Economic Evaluation of Healthcare Programmes - A Detailed Case Study
VerifiedAdded on 2023/04/23
|13
|2661
|231
Case Study
AI Summary
This document presents a comprehensive case study focusing on the economic evaluation of healthcare programmes. It addresses key concepts such as present value calculation, incremental cost-effectiveness ratio (ICER), opportunity cost, and quality-adjusted life years (QALY). The study compares different treatment options using ICER, discusses the importance of opportunity cost in healthcare investment, and explains the methodology for QALY calculation. Furthermore, it explores methods like standard gamble (SG), time trade-off (TTO), and visual analog scale (VAS) for valuing health outcomes. The document also discusses the application of cost-utility analysis (CUA) and cost-benefit analysis (CBA) in healthcare decision-making, providing insights into preventive dentistry project setup and cost-effectiveness analysis. The assignment provides a detailed overview and insights into the economic considerations vital for healthcare programme assessment. Desklib provides a platform for students to access similar solved assignments and study resources.
Questions and Answers
On
Economic Evaluation of
Healthcare Programmes
Name |
| Date
On
Economic Evaluation of
Healthcare Programmes
Name |
| Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Healthcare Programmes- an approach from the books of Economics
CASE STUDY ON ECONOMIC EVALUATION OF HEALTHCARE
PROGRAMMES
Answer to question 1a:
The present value PV = C / (1 + d)n
C-= amount whose PV is to be arrived.
D = discount rate
n = number of years.
For the current year, expenditure is € 7000
For the next year, the expenditure will be € 4500
The present value of the costs will be € 4500/(1+..03) = € 4368.93
For the third year, the costs will be € 3400
The present value of the costs will be € 3400 / (1 + .03)2 = € 3204.52
The total present value of the costs will be € 12073.45
The answer to question 1B :
“ICER” is calculated by dividing the incremental cost by incremental effect (difference in
health outcomes).
ICER A = Cost of treatment for A – Cost of treatment cost for O” ) / (Benefit of
Treatment for A – Benefit of treatment for O)
ICER for A compared to O = (€ 65000 - € 30000) / (2.7 – 2.0)
= € 35000 / 0.7 = € 50000 / QALY
ICER for B compared to A = (€ 85000 - € 65000) / (3.0 – 2.7)
1
CASE STUDY ON ECONOMIC EVALUATION OF HEALTHCARE
PROGRAMMES
Answer to question 1a:
The present value PV = C / (1 + d)n
C-= amount whose PV is to be arrived.
D = discount rate
n = number of years.
For the current year, expenditure is € 7000
For the next year, the expenditure will be € 4500
The present value of the costs will be € 4500/(1+..03) = € 4368.93
For the third year, the costs will be € 3400
The present value of the costs will be € 3400 / (1 + .03)2 = € 3204.52
The total present value of the costs will be € 12073.45
The answer to question 1B :
“ICER” is calculated by dividing the incremental cost by incremental effect (difference in
health outcomes).
ICER A = Cost of treatment for A – Cost of treatment cost for O” ) / (Benefit of
Treatment for A – Benefit of treatment for O)
ICER for A compared to O = (€ 65000 - € 30000) / (2.7 – 2.0)
= € 35000 / 0.7 = € 50000 / QALY
ICER for B compared to A = (€ 85000 - € 65000) / (3.0 – 2.7)
1
Healthcare Programmes- an approach from the books of Economics
= € 20000 / 0.3 = € 66666 /QALY
From the above calculation, ICER derived from option 2 is more than ICER derived from
option 1 which proves that option 2 is more costly.
The answer to question 1C :
Opportunity cost is one of the fundamental concepts to the view of costs from the
economics angle. Since resources are found less compared to what is required, the use of
resources in one option prevents use in other options. The opportunity cost for investment
in a healthcare intervention is calculated by the number of health benefits i.e. a number of
life years saved and QALYs gained if the money spent on other interventions. Cost-
effectiveness ratios ( €/outcome of different interventions) allow opportunity costs of
different interventions comparable.
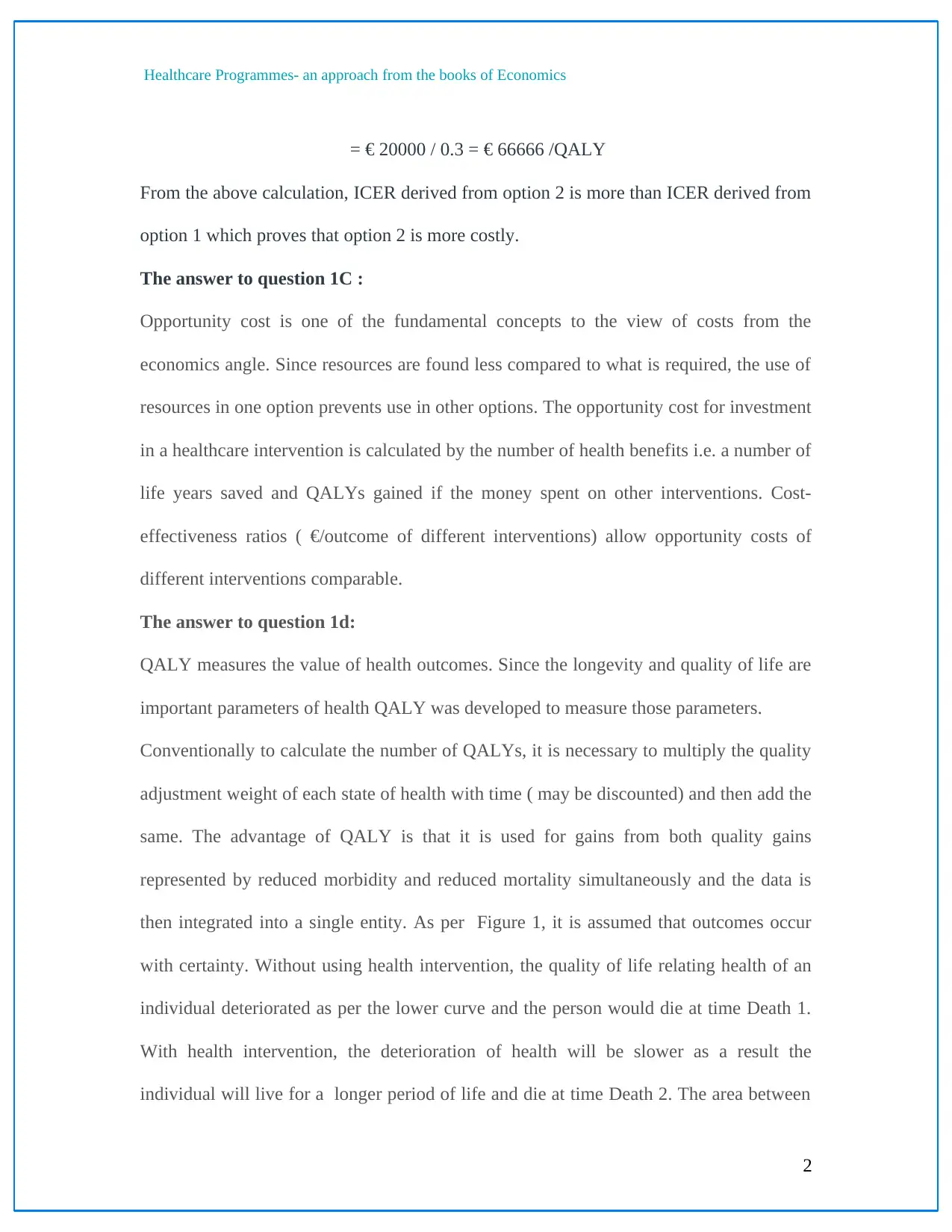
The answer to question 1d:
QALY measures the value of health outcomes. Since the longevity and quality of life are
important parameters of health QALY was developed to measure those parameters.
Conventionally to calculate the number of QALYs, it is necessary to multiply the quality
adjustment weight of each state of health with time ( may be discounted) and then add the
same. The advantage of QALY is that it is used for gains from both quality gains
represented by reduced morbidity and reduced mortality simultaneously and the data is
then integrated into a single entity. As per Figure 1, it is assumed that outcomes occur
with certainty. Without using health intervention, the quality of life relating health of an
individual deteriorated as per the lower curve and the person would die at time Death 1.
With health intervention, the deterioration of health will be slower as a result the
individual will live for a longer period of life and die at time Death 2. The area between
2
= € 20000 / 0.3 = € 66666 /QALY
From the above calculation, ICER derived from option 2 is more than ICER derived from
option 1 which proves that option 2 is more costly.
The answer to question 1C :
Opportunity cost is one of the fundamental concepts to the view of costs from the
economics angle. Since resources are found less compared to what is required, the use of
resources in one option prevents use in other options. The opportunity cost for investment
in a healthcare intervention is calculated by the number of health benefits i.e. a number of
life years saved and QALYs gained if the money spent on other interventions. Cost-
effectiveness ratios ( €/outcome of different interventions) allow opportunity costs of
different interventions comparable.
The answer to question 1d:
QALY measures the value of health outcomes. Since the longevity and quality of life are
important parameters of health QALY was developed to measure those parameters.
Conventionally to calculate the number of QALYs, it is necessary to multiply the quality
adjustment weight of each state of health with time ( may be discounted) and then add the
same. The advantage of QALY is that it is used for gains from both quality gains
represented by reduced morbidity and reduced mortality simultaneously and the data is
then integrated into a single entity. As per Figure 1, it is assumed that outcomes occur
with certainty. Without using health intervention, the quality of life relating health of an
individual deteriorated as per the lower curve and the person would die at time Death 1.
With health intervention, the deterioration of health will be slower as a result the
individual will live for a longer period of life and die at time Death 2. The area between
2
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Healthcare Programmes- an approach from the books of Economics
the curves denotes QALYs gained because of this intervention The area is divided into
two parts part A and part B. Part A is QALYs gained because of quality improvements
(i.e. the quality gained when the individual is alive), and part B is the QALYs gained
because of quantity improvements (i.e. the amount of extension of life).
Figure1 represents the gain of QLAYs on account of intervention
The answer to question 2a
Standard gamble (SG) is having two options 1. surviving for t years in health state h for
example, one could live for 7 years with a fractured arm, 2. the patient is having
probability p of living t1years in good health equivalent to h=1 or immediate death
(i.e.t1=0).The main purpose of using standard gamble (SG) is to find out the value of p.
3
the curves denotes QALYs gained because of this intervention The area is divided into
two parts part A and part B. Part A is QALYs gained because of quality improvements
(i.e. the quality gained when the individual is alive), and part B is the QALYs gained
because of quantity improvements (i.e. the amount of extension of life).
Figure1 represents the gain of QLAYs on account of intervention
The answer to question 2a
Standard gamble (SG) is having two options 1. surviving for t years in health state h for
example, one could live for 7 years with a fractured arm, 2. the patient is having
probability p of living t1years in good health equivalent to h=1 or immediate death
(i.e.t1=0).The main purpose of using standard gamble (SG) is to find out the value of p.
3
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Healthcare Programmes- an approach from the books of Economics
Time Trade-off (TTO). In this concept, the patient will be given an option to choose
whether he or she wants to have his left over life expectancy in the situation “live,
fractured arm” or a shorter lifespan in normal health. For example, a 60-year-old man is
being asked how many years T in a state of good health he can survive instead of is 15
years (his remaining life expectancy) in the state “alive, fractured arm ” T is a variable
here and it will be found that at a particular value of T, he is indecisive when it comes to
selecting within the two options. The most simple way to change the optimal-health
equivalent T into a utility (value between 0 and 1) is to divide T by 15.
Visual Analog Scale (VAS). This can be called a “thermometer” approach. In VAS, the
subject is asked to rate the state by inserting a mark on a 100-mm vertical or horizontal
line, anchored by good health as well as death or worst possible health. The score will be
the number of mm from the “death” anchor to the mark, divided by hundred. The VAS
does not replicate any trade-off that a subject is willing to make for obtaining better
health, neither in terms of risk nor in years of life (Wiseman et al. 2016).
From the approaches mentioned above SG provides a higher score than TTO which in
turn gives a higher score than VAS.
The answer to question 2b
CUA permits comparison as well as assessment of different health-related
programs and policies by using a common unit which is equal to (money/QALY gained).
It offers an effective analysis of total benefits compared to normal cost-benefit analysis. It
is because of CUA taking into consideration life quality of the patient, whereas CBA
does not have that (Gray and Wilkinson 2016).
4
Time Trade-off (TTO). In this concept, the patient will be given an option to choose
whether he or she wants to have his left over life expectancy in the situation “live,
fractured arm” or a shorter lifespan in normal health. For example, a 60-year-old man is
being asked how many years T in a state of good health he can survive instead of is 15
years (his remaining life expectancy) in the state “alive, fractured arm ” T is a variable
here and it will be found that at a particular value of T, he is indecisive when it comes to
selecting within the two options. The most simple way to change the optimal-health
equivalent T into a utility (value between 0 and 1) is to divide T by 15.
Visual Analog Scale (VAS). This can be called a “thermometer” approach. In VAS, the
subject is asked to rate the state by inserting a mark on a 100-mm vertical or horizontal
line, anchored by good health as well as death or worst possible health. The score will be
the number of mm from the “death” anchor to the mark, divided by hundred. The VAS
does not replicate any trade-off that a subject is willing to make for obtaining better
health, neither in terms of risk nor in years of life (Wiseman et al. 2016).
From the approaches mentioned above SG provides a higher score than TTO which in
turn gives a higher score than VAS.
The answer to question 2b
CUA permits comparison as well as assessment of different health-related
programs and policies by using a common unit which is equal to (money/QALY gained).
It offers an effective analysis of total benefits compared to normal cost-benefit analysis. It
is because of CUA taking into consideration life quality of the patient, whereas CBA
does not have that (Gray and Wilkinson 2016).
4
Healthcare Programmes- an approach from the books of Economics
The CUA’s main purpose is to find out the ratio of cost of a health-related intervention as
well as the advantages in terms of a number of years living in sound health by the person.
So it can be called the subset of CEA, and the terms CUA and CEA are often
interchanged (Van Baal, Meltzer and Brouwer 2016).
Cost is expressed by a unit of money (euro). The benefit is expressed such a way that
gives a quantitative value to health states which are considered less preferable to sound
health. However, unlike CBA, the benefits need not be expressed in money terms. It is
expressed in QALYs.
5
The CUA’s main purpose is to find out the ratio of cost of a health-related intervention as
well as the advantages in terms of a number of years living in sound health by the person.
So it can be called the subset of CEA, and the terms CUA and CEA are often
interchanged (Van Baal, Meltzer and Brouwer 2016).
Cost is expressed by a unit of money (euro). The benefit is expressed such a way that
gives a quantitative value to health states which are considered less preferable to sound
health. However, unlike CBA, the benefits need not be expressed in money terms. It is
expressed in QALYs.
5
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Healthcare Programmes- an approach from the books of Economics
The answer to question 3
The following methodology can be adopted for decision-making for setting up an
environment for preventive dentistry.
1. an inventory is prepared for identifying and establishing actual data relating to both
health and finance.
2. well defined health objectives may be stipulated from both patient and clinical
oriented views (Donker et al. 2015).
3. To establish objectives of treatment for different categories of patients with
measures leading to a well-defined outcome that is consistent with overall health
objectives, starting with an oral disease like cavity formation and the related side
effects like pneumonia due to bacteria formation. Promotion of health, maintenance
of equipment, and treatment of disease should be taken into account and both costs
and the consequences are to be explained in detail in the time of preparation of the
budget.
4. for setting up of a project on preventive dentistry as mentioned above, a cost-benefit
analysis before the planning process is to be prepared to find out the preferences and
“willing to pay (WTP)” among adults.
5. different preventive measures should be in place before implementation of the
project, the following points should be given due attention to creating the best health
outcome like expected results of preventive measures, analysis of individual
preferences, resource accessibility, health objectives and allocation policy.
6
The answer to question 3
The following methodology can be adopted for decision-making for setting up an
environment for preventive dentistry.
1. an inventory is prepared for identifying and establishing actual data relating to both
health and finance.
2. well defined health objectives may be stipulated from both patient and clinical
oriented views (Donker et al. 2015).
3. To establish objectives of treatment for different categories of patients with
measures leading to a well-defined outcome that is consistent with overall health
objectives, starting with an oral disease like cavity formation and the related side
effects like pneumonia due to bacteria formation. Promotion of health, maintenance
of equipment, and treatment of disease should be taken into account and both costs
and the consequences are to be explained in detail in the time of preparation of the
budget.
4. for setting up of a project on preventive dentistry as mentioned above, a cost-benefit
analysis before the planning process is to be prepared to find out the preferences and
“willing to pay (WTP)” among adults.
5. different preventive measures should be in place before implementation of the
project, the following points should be given due attention to creating the best health
outcome like expected results of preventive measures, analysis of individual
preferences, resource accessibility, health objectives and allocation policy.
6
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Healthcare Programmes- an approach from the books of Economics
6. continuous follow-ups both centralised and local are performed in order to compare
health outcomes and costs (CEA, CBA).
The CEA is the most widely accepted method of analysis to evaluate health interventions.
The concept behind CEA is to look at expenses as well as outcomes of at least two or
more different choices between a new intervention and the existing one.CEA computes
the effective expenses of a health result, like cost-per-disease avoided, cost-per-death that
is avoided, or cost per additional year of life gained. The net expenses equal the cost of a
particular health action delivered to avoid a disease or undesirable health minus the
treatment cost along with other costs not spent due to the effects of benefits of the
intervention. The ratio of the expenses in euro as a numerator to measurable health
benefits as; the denominator is calculated on the basis of each alternative intervention.
The health benefit is expressed in terms of the gain in years of life. While CBA refers to a
popular method for decisions about the real estate projects or large scale civil or
infrastructure projects where the allocation of funds is the most important criteria, it is
less useful for estimating investments in the healthcare sector. (Tseng et al. 2018).
7
6. continuous follow-ups both centralised and local are performed in order to compare
health outcomes and costs (CEA, CBA).
The CEA is the most widely accepted method of analysis to evaluate health interventions.
The concept behind CEA is to look at expenses as well as outcomes of at least two or
more different choices between a new intervention and the existing one.CEA computes
the effective expenses of a health result, like cost-per-disease avoided, cost-per-death that
is avoided, or cost per additional year of life gained. The net expenses equal the cost of a
particular health action delivered to avoid a disease or undesirable health minus the
treatment cost along with other costs not spent due to the effects of benefits of the
intervention. The ratio of the expenses in euro as a numerator to measurable health
benefits as; the denominator is calculated on the basis of each alternative intervention.
The health benefit is expressed in terms of the gain in years of life. While CBA refers to a
popular method for decisions about the real estate projects or large scale civil or
infrastructure projects where the allocation of funds is the most important criteria, it is
less useful for estimating investments in the healthcare sector. (Tseng et al. 2018).
7
Healthcare Programmes- an approach from the books of Economics
The answer to question 4
Cost-Effectiveness Analysis (CEA) is a measure of clinical outcomes in “natural units.”
which consist of a number of endpoints like a number of years gained in lifetime, periods
that are free of symptoms, avoiding complications along with the cases that are
diagnosed. The main objective of Cost Effective Analysis is to improve health benefits of
the society while working within a tight budget.
Though CEA is having a number of advantages the major drawback is not to provide
comparisons between different diseases. So it is not able to determine the opportunity
cost of implementation of an action over another. The opportunity cost refers to the
shortage of health benefits that can be eradicated if same resources are used in other
healthcare organizations. Since opportunity cost measurement is not a direct one and
practically impossible to get accurately it is a challenge for policymakers to take effective
decisions regarding the allocation of proper costs of the resources and effects of other
alternative actions.
The cost-qutility analysis is regarding measurement of the acceptance of the
healthcare service users for being in a specific state of health. The preference outcome is
expressed in the form of a utility score and is generally between 1 [perfect health] and 0
[death]. In the case of Cost-Effective Analysis, the result is demonstrated as QALY.
CUA as well as CEA are similar in good number of areas of operation (Mariño et al.
2016).
8
The answer to question 4
Cost-Effectiveness Analysis (CEA) is a measure of clinical outcomes in “natural units.”
which consist of a number of endpoints like a number of years gained in lifetime, periods
that are free of symptoms, avoiding complications along with the cases that are
diagnosed. The main objective of Cost Effective Analysis is to improve health benefits of
the society while working within a tight budget.
Though CEA is having a number of advantages the major drawback is not to provide
comparisons between different diseases. So it is not able to determine the opportunity
cost of implementation of an action over another. The opportunity cost refers to the
shortage of health benefits that can be eradicated if same resources are used in other
healthcare organizations. Since opportunity cost measurement is not a direct one and
practically impossible to get accurately it is a challenge for policymakers to take effective
decisions regarding the allocation of proper costs of the resources and effects of other
alternative actions.
The cost-qutility analysis is regarding measurement of the acceptance of the
healthcare service users for being in a specific state of health. The preference outcome is
expressed in the form of a utility score and is generally between 1 [perfect health] and 0
[death]. In the case of Cost-Effective Analysis, the result is demonstrated as QALY.
CUA as well as CEA are similar in good number of areas of operation (Mariño et al.
2016).
8
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Healthcare Programmes- an approach from the books of Economics
Cost-benefit analysis is one of the most comprehensive methods for economic evaluation
and is based on traditional economic theory. During a cost-benefit analysis, the
consequences due to intervention are expressed in money terms; therefore, it places
values in terms of currency on both inputs (costs) and outputs (benefits) of health care.
Since outcomes are expressed in units of money, it is the best suited for the mechanism of
allocation decisions. Policymakers can assess the ROI from health rather than
investments in other sectors of the economy, like real estate, industry and other
investments. (Drummond et al., 2015)
9
Cost-benefit analysis is one of the most comprehensive methods for economic evaluation
and is based on traditional economic theory. During a cost-benefit analysis, the
consequences due to intervention are expressed in money terms; therefore, it places
values in terms of currency on both inputs (costs) and outputs (benefits) of health care.
Since outcomes are expressed in units of money, it is the best suited for the mechanism of
allocation decisions. Policymakers can assess the ROI from health rather than
investments in other sectors of the economy, like real estate, industry and other
investments. (Drummond et al., 2015)
9
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Healthcare Programmes- an approach from the books of Economics
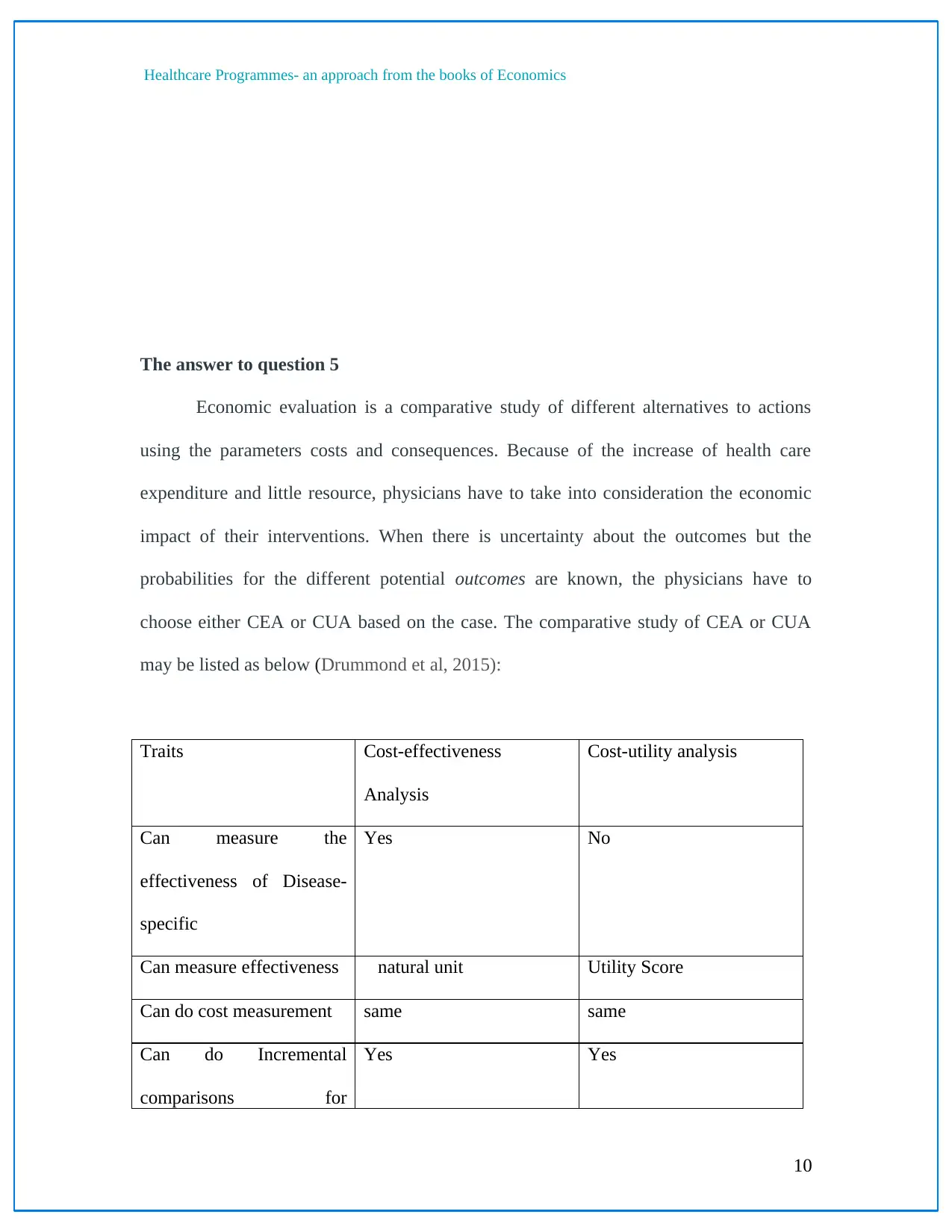
The answer to question 5
Economic evaluation is a comparative study of different alternatives to actions
using the parameters costs and consequences. Because of the increase of health care
expenditure and little resource, physicians have to take into consideration the economic
impact of their interventions. When there is uncertainty about the outcomes but the
probabilities for the different potential outcomes are known, the physicians have to
choose either CEA or CUA based on the case. The comparative study of CEA or CUA
may be listed as below (Drummond et al, 2015):
Traits Cost-effectiveness
Analysis
Cost-utility analysis
Can measure the
effectiveness of Disease-
specific
Yes No
Can measure effectiveness natural unit Utility Score
Can do cost measurement same same
Can do Incremental
comparisons for
Yes Yes
10
The answer to question 5
Economic evaluation is a comparative study of different alternatives to actions
using the parameters costs and consequences. Because of the increase of health care
expenditure and little resource, physicians have to take into consideration the economic
impact of their interventions. When there is uncertainty about the outcomes but the
probabilities for the different potential outcomes are known, the physicians have to
choose either CEA or CUA based on the case. The comparative study of CEA or CUA
may be listed as below (Drummond et al, 2015):
Traits Cost-effectiveness
Analysis
Cost-utility analysis
Can measure the
effectiveness of Disease-
specific
Yes No
Can measure effectiveness natural unit Utility Score
Can do cost measurement same same
Can do Incremental
comparisons for
Yes Yes
10
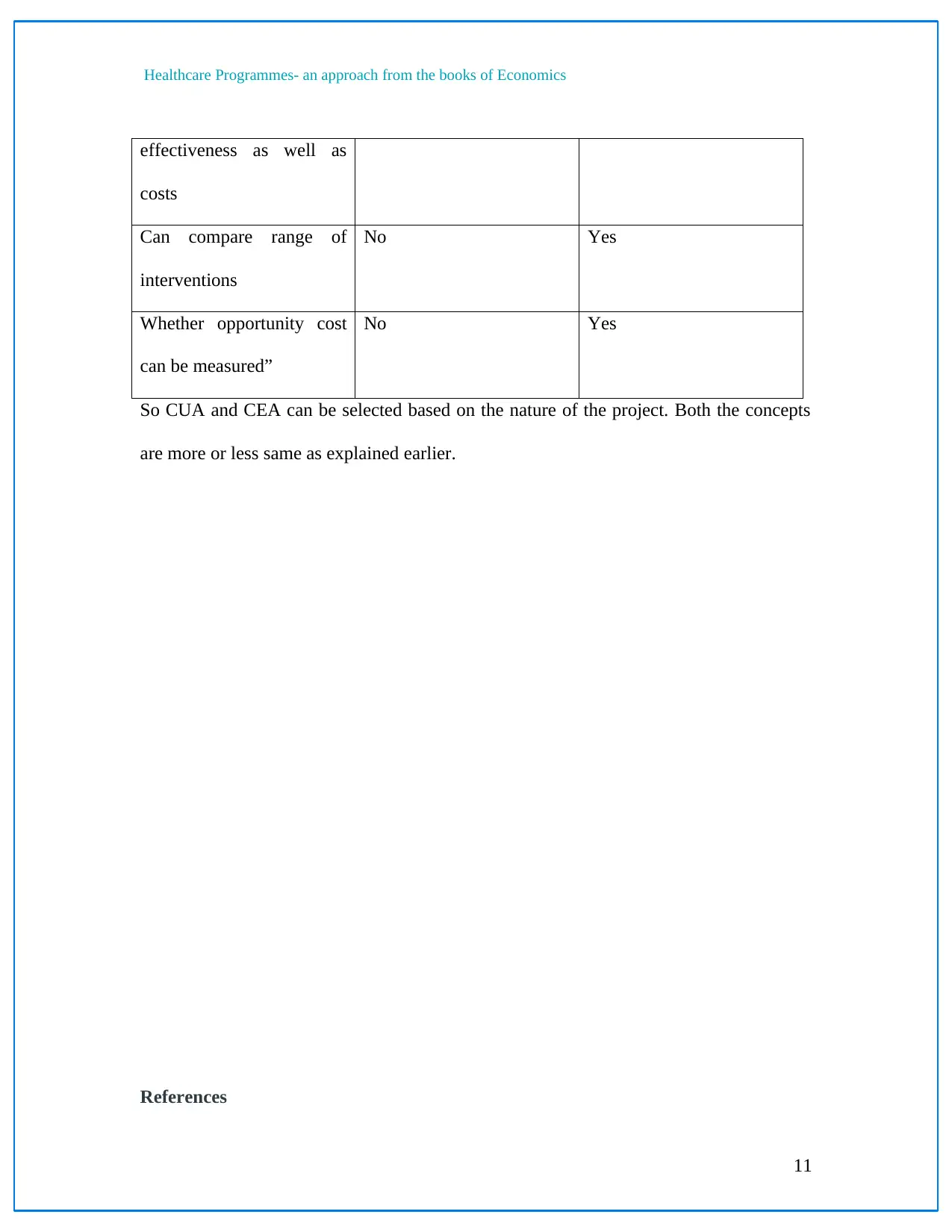
Healthcare Programmes- an approach from the books of Economics
effectiveness as well as
costs
Can compare range of
interventions
No Yes
Whether opportunity cost
can be measured”
No Yes
So CUA and CEA can be selected based on the nature of the project. Both the concepts
are more or less same as explained earlier.
References
11
effectiveness as well as
costs
Can compare range of
interventions
No Yes
Whether opportunity cost
can be measured”
No Yes
So CUA and CEA can be selected based on the nature of the project. Both the concepts
are more or less same as explained earlier.
References
11
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


