An Analysis of Racial/Ethnic Health Disparities in Refugee Healthcare
VerifiedAdded on 2022/10/01
|13
|3894
|6
Report
AI Summary
This report delves into the critical issue of racial and ethnic health disparities affecting refugees in Australia. It highlights the vulnerability of refugees due to factors such as trauma, discrimination, and lack of protection from their native lands, emphasizing the importance of support rather than mere identification. The report examines how social determinants of health, including discrimination, racism, and distrust of the government, hinder refugees' access to the Australian healthcare system. It explores the impact of these factors on mental health, access to employment, housing, education, and the ability to afford essential needs like a balanced diet and medication. Furthermore, the report discusses health inequalities and inequities, such as differences in health status, access to basic healthcare, and affordability, which contribute to adverse health outcomes among refugees. It also addresses the role of language barriers and communication difficulties between refugees and healthcare providers. The report concludes by emphasizing the need to address these disparities and improve the healthcare experiences and outcomes for refugee populations in Australia.

Running Head: RACIAL/ETHNIC DISPARITIES IN HEALTHCARE AMONG REFUGEES
Racial/Ethnic Disparities in Healthcare among Refugees
Institution
Student name
Date
Racial/Ethnic Disparities in Healthcare among Refugees
Institution
Student name
Date
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2
Racial/Ethnic Disparities in Healthcare among Refugees
From a health and healthcare perspective, there is no doubt that asylum seekers are
among the most vulnerable groups in Australia (Silove, Ventevogel, & Rees, 2017). As an
overall proposition, it can be reasoned that refugees are per se risk since they are outside their
native country. Their susceptibility originates from the trauma, violence, and discrimination they
have experienced and the fact that their very own state cannot offer any form of protection to
them. Silove, Ventevogel, and Rees (2017), however, argue that vulnerability should not be
based merely on one’s belonging to a certain group that is considered underprivileged, but rather
as an individual. While this paper is not insinuating that the latter perspective is indecorous, it’s
worth noting that there exists a certain degree of vulnerability to any refugee irrespective of his
or her previous or current socioeconomic status and emphasis should, therefore, be based on
support rather than identification. For purposes of this essay, the author adopts the position that
all refugees in Australia are vulnerable due to the fact that they are outside the protection of their
native land. The author will rely on a number of factors such as social determinants of health,
health inequalities, health inequities and health outcomes to reinforce this standpoint.
Taylor and Haintz (2018) assert that a surfeit of factors hinder refuges in Australia from
fully utilizing the Australian healthcare system. In their research, the duo examined several
SDHs on refugees’ access to Australian healthcare services. Social norms and attitudes such as
discrimination, racism, and distrust of government ranked top among the social determinants of
refugee health in Australia. Research shows that perceived discrimination and distrust of the
government have been identified to bear huge detrimental effect on the mental health of African
refugees currently in Australia. With increasing incidences of terrorist attacks in recent years, the
fundamental rights of asylum seekers and refugees have been violated in Australia’s interest to
fight terrorism (Taylor & Haintz, 2018). This has led to increased discrimination and racism
Racial/Ethnic Disparities in Healthcare among Refugees
From a health and healthcare perspective, there is no doubt that asylum seekers are
among the most vulnerable groups in Australia (Silove, Ventevogel, & Rees, 2017). As an
overall proposition, it can be reasoned that refugees are per se risk since they are outside their
native country. Their susceptibility originates from the trauma, violence, and discrimination they
have experienced and the fact that their very own state cannot offer any form of protection to
them. Silove, Ventevogel, and Rees (2017), however, argue that vulnerability should not be
based merely on one’s belonging to a certain group that is considered underprivileged, but rather
as an individual. While this paper is not insinuating that the latter perspective is indecorous, it’s
worth noting that there exists a certain degree of vulnerability to any refugee irrespective of his
or her previous or current socioeconomic status and emphasis should, therefore, be based on
support rather than identification. For purposes of this essay, the author adopts the position that
all refugees in Australia are vulnerable due to the fact that they are outside the protection of their
native land. The author will rely on a number of factors such as social determinants of health,
health inequalities, health inequities and health outcomes to reinforce this standpoint.
Taylor and Haintz (2018) assert that a surfeit of factors hinder refuges in Australia from
fully utilizing the Australian healthcare system. In their research, the duo examined several
SDHs on refugees’ access to Australian healthcare services. Social norms and attitudes such as
discrimination, racism, and distrust of government ranked top among the social determinants of
refugee health in Australia. Research shows that perceived discrimination and distrust of the
government have been identified to bear huge detrimental effect on the mental health of African
refugees currently in Australia. With increasing incidences of terrorist attacks in recent years, the
fundamental rights of asylum seekers and refugees have been violated in Australia’s interest to
fight terrorism (Taylor & Haintz, 2018). This has led to increased discrimination and racism
3
Racial/Ethnic Disparities in Healthcare among Refugees
towards these populations. Perceived segregation has negatively impacted refugee health in
several ways including reduced access to housing, education and employment and leading to
severe emotional distress and associated psychopathology (Shishehgar et al., 2017). In addition,
findings show that emotional negativity emanating from prejudiced experiences leads to
functional and structural adjustments in several physiological systems of the victim.
Discriminatory treatment as Mahimbo et al. (2017) contents, deeply affects one's self-efficacy
and self-esteem thus fettering opportunities for the victim's participation in economic and social
spheres.
The 1951 Convention on Refugee rights grants refugees employment opportunities and
participation in other economic activities. However, most host nations have been unwilling to
permit this right. Several factors influence this reluctance and include security concerns about
large numbers of refugees gaining settlement, job availability for the natives, limited capacity to
absorb labor and fear for xenophobic uprisings against the foreigners like the case of South
Africa. Although a party to the 1951 refugee convention, Australia declares reservations and the
refugee grant to work is subject to the labor market index among other stringent conditions.
Apart from mental distress, lack of access to job and economic activities bears direct
implications on refugee health as the majority are unable to afford a balanced diet due to a lack
of financial resources. Additionally, due to lack of adequate financial resources emanating from
joblessness, most refugees are unable to acquire decent housing and clean water and are thus
forced to reside in camps that are highly susceptible to airborne and infectious ailments. Lastly,
the refugee unemployed may not be able to afford proper medication in the event that they fall
sick due to a lack of monies to fund their medication (Fisher et al., 2016).
Racial/Ethnic Disparities in Healthcare among Refugees
towards these populations. Perceived segregation has negatively impacted refugee health in
several ways including reduced access to housing, education and employment and leading to
severe emotional distress and associated psychopathology (Shishehgar et al., 2017). In addition,
findings show that emotional negativity emanating from prejudiced experiences leads to
functional and structural adjustments in several physiological systems of the victim.
Discriminatory treatment as Mahimbo et al. (2017) contents, deeply affects one's self-efficacy
and self-esteem thus fettering opportunities for the victim's participation in economic and social
spheres.
The 1951 Convention on Refugee rights grants refugees employment opportunities and
participation in other economic activities. However, most host nations have been unwilling to
permit this right. Several factors influence this reluctance and include security concerns about
large numbers of refugees gaining settlement, job availability for the natives, limited capacity to
absorb labor and fear for xenophobic uprisings against the foreigners like the case of South
Africa. Although a party to the 1951 refugee convention, Australia declares reservations and the
refugee grant to work is subject to the labor market index among other stringent conditions.
Apart from mental distress, lack of access to job and economic activities bears direct
implications on refugee health as the majority are unable to afford a balanced diet due to a lack
of financial resources. Additionally, due to lack of adequate financial resources emanating from
joblessness, most refugees are unable to acquire decent housing and clean water and are thus
forced to reside in camps that are highly susceptible to airborne and infectious ailments. Lastly,
the refugee unemployed may not be able to afford proper medication in the event that they fall
sick due to a lack of monies to fund their medication (Fisher et al., 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4
Racial/Ethnic Disparities in Healthcare among Refugees
Most of the refugees in Australia use English as their second language with varying
levels of mastery of the same. Shishehgar et al. (2017) observe that some refugees especially
from West and Central Africa whom English is neither their first nor second language experience
a lot of difficulties when trying to access educational opportunities or health services in
Australia. With English being the language of instruction in Australia, the majority of refugees
opt not to attend Australian school because of the constraints involved in first learning the new
language before proceeding to their specific area of interest. With low literacy levels and
communication barriers already existing, most of these refugees miss out on opportunities to
attend school and gain much-needed health education and economic empowerment
(Nithianandan et al., 2016). Medical attendants also experience difficulties communicating with
the non-English speaking refugees without the services of an interpreter. With the refugee unable
to express oneself clearly to the medics, doctors may end up misinterpreting the symptoms and
giving wrong prescriptions that in some cases may turn out detrimental to the patient thus
making them even more vulnerable (Mahimbo et al., 2017).
Variations in health status among different groups of populations have been cited as one
of the factors contributing to the increased vulnerability of asylum seekers in Australia. Day
(2016) feels that health inequalities such as mortality and morbidity, healthy life expectancy,
differences in well-being, abuse and violence and risk of diseases put the lives of refugees at a
higher propensity of susceptibility. de Bocanegra et al. (2018) cite violence, abuse, and brutality
as one of the major stressors affecting mostly the mental health of refugees not only in Australia
but across the globe. Major, Dovidio, and Link (2018) claim that refugees who have been
through traumatic experiences in their native country are highly vulnerable to developing
psychological problems such as post traumatic stress disorder (PTSD). This reflection is
Racial/Ethnic Disparities in Healthcare among Refugees
Most of the refugees in Australia use English as their second language with varying
levels of mastery of the same. Shishehgar et al. (2017) observe that some refugees especially
from West and Central Africa whom English is neither their first nor second language experience
a lot of difficulties when trying to access educational opportunities or health services in
Australia. With English being the language of instruction in Australia, the majority of refugees
opt not to attend Australian school because of the constraints involved in first learning the new
language before proceeding to their specific area of interest. With low literacy levels and
communication barriers already existing, most of these refugees miss out on opportunities to
attend school and gain much-needed health education and economic empowerment
(Nithianandan et al., 2016). Medical attendants also experience difficulties communicating with
the non-English speaking refugees without the services of an interpreter. With the refugee unable
to express oneself clearly to the medics, doctors may end up misinterpreting the symptoms and
giving wrong prescriptions that in some cases may turn out detrimental to the patient thus
making them even more vulnerable (Mahimbo et al., 2017).
Variations in health status among different groups of populations have been cited as one
of the factors contributing to the increased vulnerability of asylum seekers in Australia. Day
(2016) feels that health inequalities such as mortality and morbidity, healthy life expectancy,
differences in well-being, abuse and violence and risk of diseases put the lives of refugees at a
higher propensity of susceptibility. de Bocanegra et al. (2018) cite violence, abuse, and brutality
as one of the major stressors affecting mostly the mental health of refugees not only in Australia
but across the globe. Major, Dovidio, and Link (2018) claim that refugees who have been
through traumatic experiences in their native country are highly vulnerable to developing
psychological problems such as post traumatic stress disorder (PTSD). This reflection is
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5
Racial/Ethnic Disparities in Healthcare among Refugees
reiterated by Hirani, Payne, Mutch, and Cherian (2019) who notice that most migrant patients in
Australia present with typical symptoms of post-traumatic stress disorder that affect how they
relate and associate with both the fellow refugees and host residents. Cullen et al. (2018) add that
poor living conditions and ardors journeys cause a myriad of health challenges and access to
primary healthcare is exceedingly difficult for those on the move. This difficulty in managing
infectious ailments implies that some asylum seekers do not get appropriate treatment which may
culminate into long term complications that significantly affect their health.
Several health inequities such as access to basic healthcare and affordability of the same
are considered another factor that makes refugee populations more vulnerable to health
complications than others. With limited opportunities for employment and stringent labor laws in
the host country, immigrants are left with wobbly means of raising enough income to cater for
their treatment and other basic needs such as proper diet (Priest et al., 2016). Access to
Australia’s insurance schemes is also made difficult due to cost implications and laborious
authentication process and paperwork needed especially from the migrant populations. Lack of
employment and refugee status makes it even more difficult for refugees to acquire these covers.
Consequently, the migrants are forced to rely on the host country’s provided healthcare services
for the refugees which is obviously not enough to meet their individual needs (Roche et al.,
2015).
The vulnerability in access to healthcare services has led to several negative health
outcomes among the refugee populations in Australia. As Tiong et al. (2006) discern,
populations are grappling with a trifle of health issues such as inadequate vaccinations, incessant
outbreaks and spread of infectious diseases such as latent tuberculosis, schistosomiasis, and
gastrointestinal infections. According to Tiong et al. (2006), out of the 258 refugee patients
Racial/Ethnic Disparities in Healthcare among Refugees
reiterated by Hirani, Payne, Mutch, and Cherian (2019) who notice that most migrant patients in
Australia present with typical symptoms of post-traumatic stress disorder that affect how they
relate and associate with both the fellow refugees and host residents. Cullen et al. (2018) add that
poor living conditions and ardors journeys cause a myriad of health challenges and access to
primary healthcare is exceedingly difficult for those on the move. This difficulty in managing
infectious ailments implies that some asylum seekers do not get appropriate treatment which may
culminate into long term complications that significantly affect their health.
Several health inequities such as access to basic healthcare and affordability of the same
are considered another factor that makes refugee populations more vulnerable to health
complications than others. With limited opportunities for employment and stringent labor laws in
the host country, immigrants are left with wobbly means of raising enough income to cater for
their treatment and other basic needs such as proper diet (Priest et al., 2016). Access to
Australia’s insurance schemes is also made difficult due to cost implications and laborious
authentication process and paperwork needed especially from the migrant populations. Lack of
employment and refugee status makes it even more difficult for refugees to acquire these covers.
Consequently, the migrants are forced to rely on the host country’s provided healthcare services
for the refugees which is obviously not enough to meet their individual needs (Roche et al.,
2015).
The vulnerability in access to healthcare services has led to several negative health
outcomes among the refugee populations in Australia. As Tiong et al. (2006) discern,
populations are grappling with a trifle of health issues such as inadequate vaccinations, incessant
outbreaks and spread of infectious diseases such as latent tuberculosis, schistosomiasis, and
gastrointestinal infections. According to Tiong et al. (2006), out of the 258 refugee patients
6
Racial/Ethnic Disparities in Healthcare among Refugees
tested for latent tuberculosis, 25% of them were confirmed positive. Most adults also exhibited
psychological, musculoskeletal and social problems which can be attributed to age, long
journeys, injuries sustained due to war, insufficient healthcare and trauma suffered both in their
home country and in the host nation.
Racial/Ethnic disparity ranks top among the health disparities affecting migrant
populations in Australia (Shepherd et al., 2018). The trio regret that despite the factors being
attributed to racial health disparity having been identified through research and archive literature,
little or no efforts have been done to mitigate these conditions. Further, the researchers argue that
the interaction of these factors has not been explored as it should leading to unsystematic and
uniformed approach to the little effort being done to mitigate them (Shepherd et al.,2018).
A wide range of literature documents the ethnic/racial healthcare disparities between the
racial minority who in this case are the refugees and asylum seekers and the majority who are the
host residents (Philbin et al. 2018). In what the investigators term as a health paradox, the
immigrant populations that arrive in Australia with a better status of wellbeing than average
resident Australians born lose the status privilege as time progresses. For instance, Mexican
émigrés living in Australia enter the country in a healthier status than average Australian but
within a span of 10 years, about 8 percent of them are seen to have poorer health condition as
compared to the average native. It is further witnessed that after 15 years, this percentage rises to
15, raising conerns over the nature of healthcare services provided to the refugees and the
support accorded by the international community to the host nation regarding the refugee welfare
(Priest et al., 2016).
Lack of economic support and insurance cover among the immigrant’s hints towards a
probable racial/ethnic disparity. While television stations have sign language interpreters to assist
Racial/Ethnic Disparities in Healthcare among Refugees
tested for latent tuberculosis, 25% of them were confirmed positive. Most adults also exhibited
psychological, musculoskeletal and social problems which can be attributed to age, long
journeys, injuries sustained due to war, insufficient healthcare and trauma suffered both in their
home country and in the host nation.
Racial/Ethnic disparity ranks top among the health disparities affecting migrant
populations in Australia (Shepherd et al., 2018). The trio regret that despite the factors being
attributed to racial health disparity having been identified through research and archive literature,
little or no efforts have been done to mitigate these conditions. Further, the researchers argue that
the interaction of these factors has not been explored as it should leading to unsystematic and
uniformed approach to the little effort being done to mitigate them (Shepherd et al.,2018).
A wide range of literature documents the ethnic/racial healthcare disparities between the
racial minority who in this case are the refugees and asylum seekers and the majority who are the
host residents (Philbin et al. 2018). In what the investigators term as a health paradox, the
immigrant populations that arrive in Australia with a better status of wellbeing than average
resident Australians born lose the status privilege as time progresses. For instance, Mexican
émigrés living in Australia enter the country in a healthier status than average Australian but
within a span of 10 years, about 8 percent of them are seen to have poorer health condition as
compared to the average native. It is further witnessed that after 15 years, this percentage rises to
15, raising conerns over the nature of healthcare services provided to the refugees and the
support accorded by the international community to the host nation regarding the refugee welfare
(Priest et al., 2016).
Lack of economic support and insurance cover among the immigrant’s hints towards a
probable racial/ethnic disparity. While television stations have sign language interpreters to assist
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
7
Racial/Ethnic Disparities in Healthcare among Refugees
the visually impaired during news broadcasts, Bostos and Yaradies (2018) lament that most
health facilities in Australia do not have special needs assistants and language interpreters. While
the natives easily and fluently express themselves to medics, the non-English speaking refugees
find it difficult to express themselves to the doctors since the host government does not provide
language interpreters. The communication barrier between the medics and the patients creates a
health crisis among the immigrants that is yet to be addressed by the government (Bostos &
Yaradies, 2018).
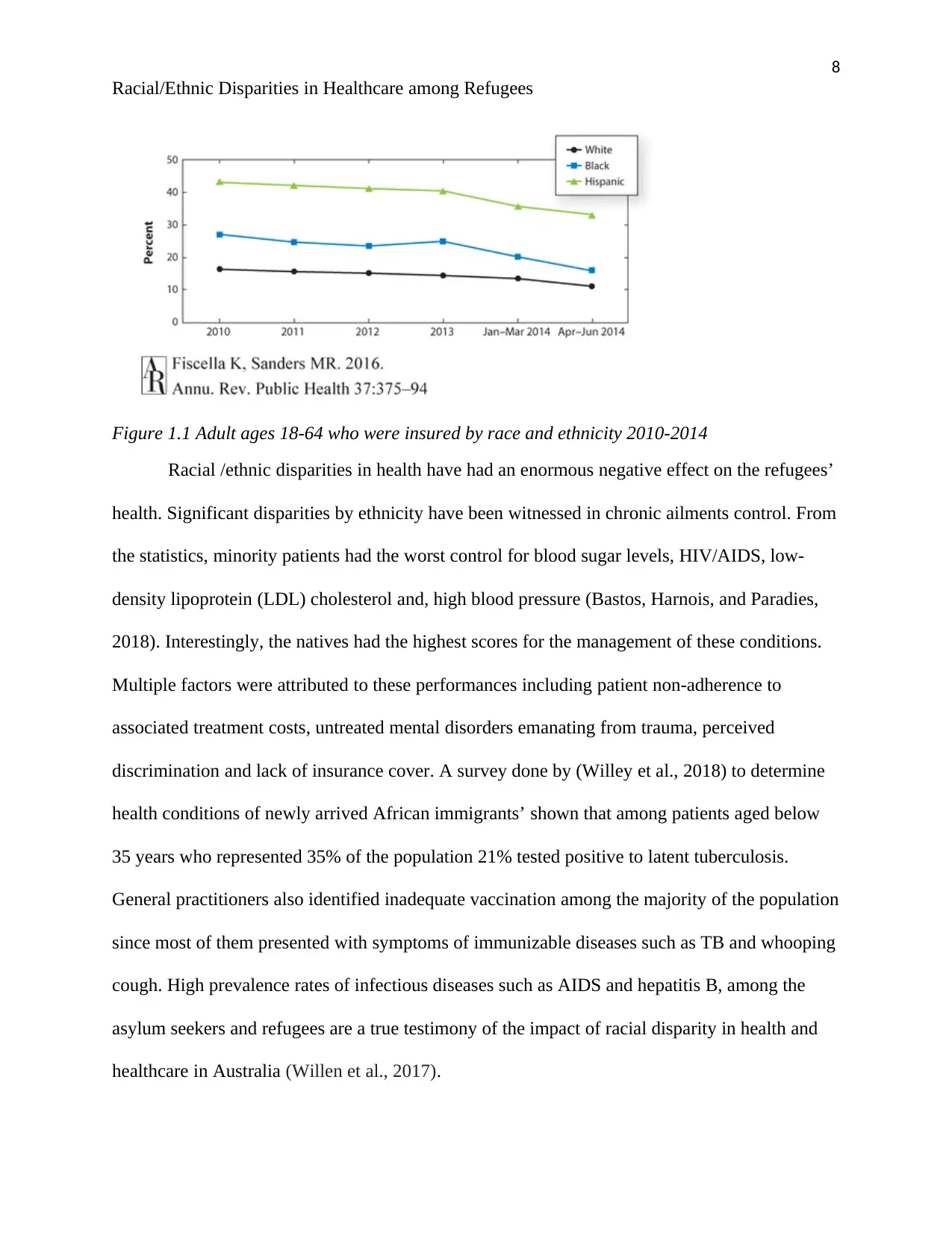
The Australian policy for protection has since early 90s restricted access to healthcare
services by refugees and asylum seekers with stringent conditions and terms to be fulfilled by the
applicant (Roche et al., 2015). While the natives have quick and efficient insurance cover
application and enrolment procedure, the immigrants are subjected to a lengthy and laborious
multiple-stage processes that only see a handful gain access to the country’s healthcare system.
While this paper is not blaming the country’s measures on security background, it is worth
noting that from a humanitarian background, much still needs to be achieved more so on access
to insurance policies. Fiscella and Sanders (2016) revealed that the majority of uninsured adults
between the age of 18 and 64 years were immigrants. According to their findings, blacks were
the least insured while Hispanic immigrants were the highest among the immigrants. However,
none of the immigrant groups had 50 % of its population insured as attested in Figure 1.1.
Racial/Ethnic Disparities in Healthcare among Refugees
the visually impaired during news broadcasts, Bostos and Yaradies (2018) lament that most
health facilities in Australia do not have special needs assistants and language interpreters. While
the natives easily and fluently express themselves to medics, the non-English speaking refugees
find it difficult to express themselves to the doctors since the host government does not provide
language interpreters. The communication barrier between the medics and the patients creates a
health crisis among the immigrants that is yet to be addressed by the government (Bostos &
Yaradies, 2018).
The Australian policy for protection has since early 90s restricted access to healthcare
services by refugees and asylum seekers with stringent conditions and terms to be fulfilled by the
applicant (Roche et al., 2015). While the natives have quick and efficient insurance cover
application and enrolment procedure, the immigrants are subjected to a lengthy and laborious
multiple-stage processes that only see a handful gain access to the country’s healthcare system.
While this paper is not blaming the country’s measures on security background, it is worth
noting that from a humanitarian background, much still needs to be achieved more so on access
to insurance policies. Fiscella and Sanders (2016) revealed that the majority of uninsured adults
between the age of 18 and 64 years were immigrants. According to their findings, blacks were
the least insured while Hispanic immigrants were the highest among the immigrants. However,
none of the immigrant groups had 50 % of its population insured as attested in Figure 1.1.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
Racial/Ethnic Disparities in Healthcare among Refugees
Figure 1.1 Adult ages 18-64 who were insured by race and ethnicity 2010-2014
Racial /ethnic disparities in health have had an enormous negative effect on the refugees’
health. Significant disparities by ethnicity have been witnessed in chronic ailments control. From
the statistics, minority patients had the worst control for blood sugar levels, HIV/AIDS, low-
density lipoprotein (LDL) cholesterol and, high blood pressure (Bastos, Harnois, and Paradies,
2018). Interestingly, the natives had the highest scores for the management of these conditions.
Multiple factors were attributed to these performances including patient non-adherence to
associated treatment costs, untreated mental disorders emanating from trauma, perceived
discrimination and lack of insurance cover. A survey done by (Willey et al., 2018) to determine
health conditions of newly arrived African immigrants’ shown that among patients aged below
35 years who represented 35% of the population 21% tested positive to latent tuberculosis.
General practitioners also identified inadequate vaccination among the majority of the population
since most of them presented with symptoms of immunizable diseases such as TB and whooping
cough. High prevalence rates of infectious diseases such as AIDS and hepatitis B, among the
asylum seekers and refugees are a true testimony of the impact of racial disparity in health and
healthcare in Australia (Willen et al., 2017).
Racial/Ethnic Disparities in Healthcare among Refugees
Figure 1.1 Adult ages 18-64 who were insured by race and ethnicity 2010-2014
Racial /ethnic disparities in health have had an enormous negative effect on the refugees’
health. Significant disparities by ethnicity have been witnessed in chronic ailments control. From
the statistics, minority patients had the worst control for blood sugar levels, HIV/AIDS, low-
density lipoprotein (LDL) cholesterol and, high blood pressure (Bastos, Harnois, and Paradies,
2018). Interestingly, the natives had the highest scores for the management of these conditions.
Multiple factors were attributed to these performances including patient non-adherence to
associated treatment costs, untreated mental disorders emanating from trauma, perceived
discrimination and lack of insurance cover. A survey done by (Willey et al., 2018) to determine
health conditions of newly arrived African immigrants’ shown that among patients aged below
35 years who represented 35% of the population 21% tested positive to latent tuberculosis.
General practitioners also identified inadequate vaccination among the majority of the population
since most of them presented with symptoms of immunizable diseases such as TB and whooping
cough. High prevalence rates of infectious diseases such as AIDS and hepatitis B, among the
asylum seekers and refugees are a true testimony of the impact of racial disparity in health and
healthcare in Australia (Willen et al., 2017).
9
Racial/Ethnic Disparities in Healthcare among Refugees
The selected audience for this insight is the Bangladesh Rural and Advancement
Committee (BRAC) Australian chapter. BRAC is arguably the largest non-governmental
organization in the world with its headquarters in Dhaka, Bangladesh and reaches out to over
126million people across the planet. Established in 1972 the organization is said to employee
over 100000 people across the world and received over 212.7 million from AusAID (Gramling et
al., 2016). It is against this background that the author settled on BRAC as it is believed to
possess both financial and manpower capacity to address the issue of immigration racial
disparities. Although there are already existing mechanisms by several other organizations, this
paper assumes the position of a new initiative since the approach and strategies to be employed
herein are different from the normal. As such it is presumed that there is not even a single
resource allocated towards mitigating the racial disparity in Australian healthcare. In addition,
BRAC is an accredited NGO in Australia and has a reputation to influence the government
towards making adjustments to its existing policies on refugee healthcare (Salami et al., 2017).
This proposal, therefore, seeks to solicit for both financial and human resource support from the
exchequer.
In order to successfully execute the initiative, this paper suggests the approach of
working for and with the refugees. Since most of the problems affecting refugee healthcare
emanate from financial constraints, perhaps it is a time the NGO management considered
recruiting refugee nurses to work with its existing nursing personne. This will change the
dimension of the public towards them and in the long run, minimize the much haunting
discrimination and inequities. In addition, the organization management could think of
employing volunteer language interpreters in all of its facilities to aid the practitioners and
refugee communication. The interpreters could as well be the refugees themselves since we have
Racial/Ethnic Disparities in Healthcare among Refugees
The selected audience for this insight is the Bangladesh Rural and Advancement
Committee (BRAC) Australian chapter. BRAC is arguably the largest non-governmental
organization in the world with its headquarters in Dhaka, Bangladesh and reaches out to over
126million people across the planet. Established in 1972 the organization is said to employee
over 100000 people across the world and received over 212.7 million from AusAID (Gramling et
al., 2016). It is against this background that the author settled on BRAC as it is believed to
possess both financial and manpower capacity to address the issue of immigration racial
disparities. Although there are already existing mechanisms by several other organizations, this
paper assumes the position of a new initiative since the approach and strategies to be employed
herein are different from the normal. As such it is presumed that there is not even a single
resource allocated towards mitigating the racial disparity in Australian healthcare. In addition,
BRAC is an accredited NGO in Australia and has a reputation to influence the government
towards making adjustments to its existing policies on refugee healthcare (Salami et al., 2017).
This proposal, therefore, seeks to solicit for both financial and human resource support from the
exchequer.
In order to successfully execute the initiative, this paper suggests the approach of
working for and with the refugees. Since most of the problems affecting refugee healthcare
emanate from financial constraints, perhaps it is a time the NGO management considered
recruiting refugee nurses to work with its existing nursing personne. This will change the
dimension of the public towards them and in the long run, minimize the much haunting
discrimination and inequities. In addition, the organization management could think of
employing volunteer language interpreters in all of its facilities to aid the practitioners and
refugee communication. The interpreters could as well be the refugees themselves since we have
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
10
Racial/Ethnic Disparities in Healthcare among Refugees
some of them who are multilingual. Offering employment opportunities to refugees will go a
long way in mitigating racial discrimination and enhancing their economic status.
By allowing the organizations' Australian nurses to work with refugee nurses or
community health personnel, both BRAC and the Australian government stand to win big on the
war against ethnic/racial segregation in Australian health services. The government will gain an
opportunity to boost its already stretched healthcare workforce since most of the refugee
healthcare services are not usually part of the government’s healthcare workforce plan. Of all the
winners in this arrangement, the greatest of them is the medical practitioners from the host
country moreso the nurses working with the refugee nurses. The nurses will get an opportunity to
share knowledge and experiences with foreign nurses thus practising in line to standard 2.7 of the
Australia’s nursing and midwifery board professional standards for registered nurse which
provides that a registered nurse “actively fosters a culture of safety and learning that includes
engaging with health professionals and others, to share knowledge and practice that supports
person-centered care”. By working with nursing from different professional and cultural
background, the native nurses will have a rare opportunity to appreciate the practice of nursing
from different cultural background as provided for in standard 1.3 that requires nursing personnel
to respect all cultures and experiences for the people they are offering support to and colleagues.
Besides, this integration will foster cohesion among the natives and the immigrants thus
gradually changing the perception of the public towards the refugees and in the long run avert
ethnic/racial disparities in healthcare.
Racial/Ethnic Disparities in Healthcare among Refugees
some of them who are multilingual. Offering employment opportunities to refugees will go a
long way in mitigating racial discrimination and enhancing their economic status.
By allowing the organizations' Australian nurses to work with refugee nurses or
community health personnel, both BRAC and the Australian government stand to win big on the
war against ethnic/racial segregation in Australian health services. The government will gain an
opportunity to boost its already stretched healthcare workforce since most of the refugee
healthcare services are not usually part of the government’s healthcare workforce plan. Of all the
winners in this arrangement, the greatest of them is the medical practitioners from the host
country moreso the nurses working with the refugee nurses. The nurses will get an opportunity to
share knowledge and experiences with foreign nurses thus practising in line to standard 2.7 of the
Australia’s nursing and midwifery board professional standards for registered nurse which
provides that a registered nurse “actively fosters a culture of safety and learning that includes
engaging with health professionals and others, to share knowledge and practice that supports
person-centered care”. By working with nursing from different professional and cultural
background, the native nurses will have a rare opportunity to appreciate the practice of nursing
from different cultural background as provided for in standard 1.3 that requires nursing personnel
to respect all cultures and experiences for the people they are offering support to and colleagues.
Besides, this integration will foster cohesion among the natives and the immigrants thus
gradually changing the perception of the public towards the refugees and in the long run avert
ethnic/racial disparities in healthcare.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
11
Racial/Ethnic Disparities in Healthcare among Refugees
References
Bastos, J. L., Harnois, C. E., & Paradies, Y. C. (2018). Health care barriers, racism, and
intersectionality in Australia. Social Science & Medicine, 199, 209-218.
Cullen, P., Clapham, K., Hunter, K., Porykali, B., & Ivers, R. (2018). PW 1898 Embedding
multi-sectoral solutions to address transport injury and social determinants of health in
aboriginal communities in australia.
Day, G. E. (2016). Migrant and Refugee Health: Advance Australia Fair?. Australian Health
Review, 40(1), 1-2.
de Bocanegra, H. T., Carter-Pokras, O., Ingleby, J. D., Pottie, K., Tchangalova, N., Allen, S.
I., ... & Hidalgo, B. (2018). Addressing refugee health through evidence-based policies: a
case study. Annals of epidemiology, 28(6), 411-419.
Fiscella, K., & Sanders, M. R. (2016). Racial and ethnic disparities in the quality of health
care. Annual review of public health, 37, 375-394.
Fisher, M., Baum, F. E., MacDougall, C., Newman, L., & McDermott, D. (2016). To what extent
do Australian health policy documents address social determinants of health and health
equity?. Journal of Social Policy, 45(3), 545-564.
Gramling, R., Fiscella, K., Xing, G., Hoerger, M., Duberstein, P., Plumb, S., & Epstein, R. M.
(2016). Determinants of patient-oncologist prognostic discordance in advanced
cancer. JAMA oncology, 2(11), 1421-1426.
Hirani, K., Payne, D. N., Mutch, R., & Cherian, S. (2019). Medical needs of adolescent refugees
resettling in Western Australia. Archives of disease in childhood, 104(9), 880-883.
Racial/Ethnic Disparities in Healthcare among Refugees
References
Bastos, J. L., Harnois, C. E., & Paradies, Y. C. (2018). Health care barriers, racism, and
intersectionality in Australia. Social Science & Medicine, 199, 209-218.
Cullen, P., Clapham, K., Hunter, K., Porykali, B., & Ivers, R. (2018). PW 1898 Embedding
multi-sectoral solutions to address transport injury and social determinants of health in
aboriginal communities in australia.
Day, G. E. (2016). Migrant and Refugee Health: Advance Australia Fair?. Australian Health
Review, 40(1), 1-2.
de Bocanegra, H. T., Carter-Pokras, O., Ingleby, J. D., Pottie, K., Tchangalova, N., Allen, S.
I., ... & Hidalgo, B. (2018). Addressing refugee health through evidence-based policies: a
case study. Annals of epidemiology, 28(6), 411-419.
Fiscella, K., & Sanders, M. R. (2016). Racial and ethnic disparities in the quality of health
care. Annual review of public health, 37, 375-394.
Fisher, M., Baum, F. E., MacDougall, C., Newman, L., & McDermott, D. (2016). To what extent
do Australian health policy documents address social determinants of health and health
equity?. Journal of Social Policy, 45(3), 545-564.
Gramling, R., Fiscella, K., Xing, G., Hoerger, M., Duberstein, P., Plumb, S., & Epstein, R. M.
(2016). Determinants of patient-oncologist prognostic discordance in advanced
cancer. JAMA oncology, 2(11), 1421-1426.
Hirani, K., Payne, D. N., Mutch, R., & Cherian, S. (2019). Medical needs of adolescent refugees
resettling in Western Australia. Archives of disease in childhood, 104(9), 880-883.
12
Racial/Ethnic Disparities in Healthcare among Refugees
Mahimbo, A., Seale, H., Smith, M., & Heywood, A. (2017). Challenges in immunisation service
delivery for refugees in Australia: a health system perspective. Vaccine, 35(38), 5148-
5155.
Major, B., Dovidio, J. F., & Link, B. G. (Eds.). (2018). The oxford handbook of stigma,
discrimination, and health. Oxford University Press.
Nithianandan, N., Gibson-Helm, M., McBride, J., Binny, A., Gray, K. M., East, C., & Boyle, J.
A. (2016). Factors affecting implementation of perinatal mental health screening in women
of refugee background. Implementation Science, 11(1), 150.
Philbin, M. M., Flake, M., Hatzenbuehler, M. L., & Hirsch, J. S. (2018). State-level immigration
and immigrant-focused policies as drivers of Latino health disparities in the United
States. Social Science & Medicine, 199, 29-38.
Priest, N., King, T., Bécares, L., & Kavanagh, A. M. (2016). Bullying victimization and racial
discrimination among Australian children. American journal of public health, 106(10),
1882-1884.
Roche, A., Kostadinov, V., Fischer, J., & Nicholas, R. (2015). Evidence review: The social
determinants of inequities in alcohol consumption and alcohol-related health
outcomes. Australian's National Research Centre on AOD Workforce Development and
Flinders University.
Salami, B., Yaskina, M., Hegadoren, K., Diaz, E., Meherali, S., Rammohan, A., & Ben-Shlomo,
Y. (2017). Migration and social determinants of mental health: results from the Canadian
health measures survey. Canadian Journal of Public Health, 108(4), 362-367.
Racial/Ethnic Disparities in Healthcare among Refugees
Mahimbo, A., Seale, H., Smith, M., & Heywood, A. (2017). Challenges in immunisation service
delivery for refugees in Australia: a health system perspective. Vaccine, 35(38), 5148-
5155.
Major, B., Dovidio, J. F., & Link, B. G. (Eds.). (2018). The oxford handbook of stigma,
discrimination, and health. Oxford University Press.
Nithianandan, N., Gibson-Helm, M., McBride, J., Binny, A., Gray, K. M., East, C., & Boyle, J.
A. (2016). Factors affecting implementation of perinatal mental health screening in women
of refugee background. Implementation Science, 11(1), 150.
Philbin, M. M., Flake, M., Hatzenbuehler, M. L., & Hirsch, J. S. (2018). State-level immigration
and immigrant-focused policies as drivers of Latino health disparities in the United
States. Social Science & Medicine, 199, 29-38.
Priest, N., King, T., Bécares, L., & Kavanagh, A. M. (2016). Bullying victimization and racial
discrimination among Australian children. American journal of public health, 106(10),
1882-1884.
Roche, A., Kostadinov, V., Fischer, J., & Nicholas, R. (2015). Evidence review: The social
determinants of inequities in alcohol consumption and alcohol-related health
outcomes. Australian's National Research Centre on AOD Workforce Development and
Flinders University.
Salami, B., Yaskina, M., Hegadoren, K., Diaz, E., Meherali, S., Rammohan, A., & Ben-Shlomo,
Y. (2017). Migration and social determinants of mental health: results from the Canadian
health measures survey. Canadian Journal of Public Health, 108(4), 362-367.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


