SNPG917 Assessment 3: Effective VAP Bundle to Reduce VAP in Patients
VerifiedAdded on 2020/11/04
|11
|3525
|148
Report
AI Summary
This report, submitted by Rasmiti Maharjan, examines the effectiveness of ventilator bundles in reducing ventilator-associated pneumonia (VAP) in intubated patients. The introduction defines VAP as a significant nosocomial infection in ICU patients, associated with increased mortality and morbidity. The research question investigates the impact of ventilator bundles on reducing VAP incidence. The report summarizes the search methodology, including databases like CINAHL, PubMed, and Google Scholar, and the key concepts used. Evidence from studies by Shahnaz et al. (2018), Gadani et al. (2010), and Osman et al. (2020) is reviewed, highlighting the impact of VAP bundles on reducing VAP rates, improving nurse competency, and identifying risk factors. The discussion emphasizes the importance of VAP bundles and nurse education in preventing VAP. The conclusion reiterates the significance of VAP as a dangerous ICU-acquired infection and the effectiveness of ventilator bundles in mitigating its impact.

RASMITA MAHARJAN SNPG917
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
Tittle
Topic: Effective use of a Ventilator bundle to decrease the frequency of ventilated
associated pneumonia in ventilated patient (VAP)
Introduction
Ventilator-associated pneumonia (VAP) is a respiratory infection that must have evolved more
than 48 h after intubation. It represents up to 47% of all pathogens in clients with ICU. About 9-
27% of all intubated cases have been identified and 86% of nosocomial pneumonia have been re
cord with VAP (Samra, Sherif & Elokda 2017). It is the most common nasocomial infection in
critically ill patients and is associated with increased length of stay, higher cost of treatment and
a greater mortality and morbidity rate in individual requiring mechanical ventilation. (Shitrit,
Meirson, Mendelson & Chowers 2015). There are a few initiatives suggested for the prevention
of breathing tube-Associated Pneumonia. The Institute of Healthcare Improvement has proposed
a VAP package of strategy to reduce Ventilator Aspirated Pneumonia. The kit is a systematic
approach that facilitates the adoption of best guidelines and evidence-based care for all patients,
thus improving health outcomes (Parisi, Gerovasili, Dimopoulos, Kampisiouli, Goga,
Perivolioti, Nanas 2016). It is not unusual for patients of any age to be intubated electively or
emergingly due to a variety of multisystem issues (Dumbre 2019). The usage of a artifical
breathing machine after intubation places patients at risk of acquiring VAP (Samra et al.,2017).
Nurses ought to remain careful in the treatment of patients on a mechanical ventilator. Although
the best solution to minimising ventilator-associated pneumonia remains unknown, findings have
shown that informing health care professionals caring for patients on mechanical ventilation will
minimise the risk of ventilator-associated pneumonia (Keyt, Faverio & Restrepo 2014). Nurses
play a vital role in avoiding certain nosocomial or hospital-acquired diseases, like VAP, through
integrating treatment with other healthcare professionals (Cakan, Demirkıran & Yardımcı 2019.
Preventing VAP in particular, using a structured, protocolized package, can help to streamline
the treatment received, resulting in reduced period of hospital as well as ICU stay, cost control
and, eventually, better outcomes (Rello, Lode, Cornaglia & Masterton 2010)
1
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
Tittle
Topic: Effective use of a Ventilator bundle to decrease the frequency of ventilated
associated pneumonia in ventilated patient (VAP)
Introduction
Ventilator-associated pneumonia (VAP) is a respiratory infection that must have evolved more
than 48 h after intubation. It represents up to 47% of all pathogens in clients with ICU. About 9-
27% of all intubated cases have been identified and 86% of nosocomial pneumonia have been re
cord with VAP (Samra, Sherif & Elokda 2017). It is the most common nasocomial infection in
critically ill patients and is associated with increased length of stay, higher cost of treatment and
a greater mortality and morbidity rate in individual requiring mechanical ventilation. (Shitrit,
Meirson, Mendelson & Chowers 2015). There are a few initiatives suggested for the prevention
of breathing tube-Associated Pneumonia. The Institute of Healthcare Improvement has proposed
a VAP package of strategy to reduce Ventilator Aspirated Pneumonia. The kit is a systematic
approach that facilitates the adoption of best guidelines and evidence-based care for all patients,
thus improving health outcomes (Parisi, Gerovasili, Dimopoulos, Kampisiouli, Goga,
Perivolioti, Nanas 2016). It is not unusual for patients of any age to be intubated electively or
emergingly due to a variety of multisystem issues (Dumbre 2019). The usage of a artifical
breathing machine after intubation places patients at risk of acquiring VAP (Samra et al.,2017).
Nurses ought to remain careful in the treatment of patients on a mechanical ventilator. Although
the best solution to minimising ventilator-associated pneumonia remains unknown, findings have
shown that informing health care professionals caring for patients on mechanical ventilation will
minimise the risk of ventilator-associated pneumonia (Keyt, Faverio & Restrepo 2014). Nurses
play a vital role in avoiding certain nosocomial or hospital-acquired diseases, like VAP, through
integrating treatment with other healthcare professionals (Cakan, Demirkıran & Yardımcı 2019.
Preventing VAP in particular, using a structured, protocolized package, can help to streamline
the treatment received, resulting in reduced period of hospital as well as ICU stay, cost control
and, eventually, better outcomes (Rello, Lode, Cornaglia & Masterton 2010)
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
RASMITA MAHARJAN SNPG917
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
Research Question
What is the impact of the ventilator package on the reduction of the incidence of ventilated
induced pneumonia in ventilated patients?
Search summary
A number of online and internet-based search engines used in this project which includes library
database, CINAHL, PubMed, Google scholar, MEDLINE etc. According to research question
the following key concepts: ventilator-associated pneumonia, VAP bundle treatment and
intervention are used in literature search. The years 2010 to 2020 were used in the selection of
articles and other types of literature. Internet searches and keywords have been defined using the
descriptive topic heading search area and the subject heading has exploded. Method, wildcards
and phrases have been used depending on each database. Ventilator acquired pneumonia
Ventilator aspiration pneumonia, VAP, kit, pack. Study was mainly focused on human, among
nurses and randomized controlled trial method were used . As for language inclusion, english
language was considered. Finally, over 650 potentially relevant report were identified. Among
them only 16 randomised control trail were checked and objectively examined after the
elimination of depletes and obsolete articles.
Review of Evidence
Shahnaz, A., Bhardwaj, U., Tamang, E. K., & Dwivedi, S. (2018). A comparative study to assess
the competency among ICU nurses in using ventilator associated pneumonia bundle to prevent
ventilator associated pneumonia in selected government and private hospitals of New Delhi.
International Journal of Nursing Education, 10(3), 6. https://doi.org/10.5958/0974-
9357.2018.00057.0
A study was done to determine and evaluate the degree of competency in the usage of the VAP
kit and assess the relation between expertise and skills among the competence of ICU nurses
with chosen demographic factors at selected Government and Private hospital of New Delhi . A
Quantitative (Non Experimental) research Approach with comparative descriptive research
2
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
Research Question
What is the impact of the ventilator package on the reduction of the incidence of ventilated
induced pneumonia in ventilated patients?
Search summary
A number of online and internet-based search engines used in this project which includes library
database, CINAHL, PubMed, Google scholar, MEDLINE etc. According to research question
the following key concepts: ventilator-associated pneumonia, VAP bundle treatment and
intervention are used in literature search. The years 2010 to 2020 were used in the selection of
articles and other types of literature. Internet searches and keywords have been defined using the
descriptive topic heading search area and the subject heading has exploded. Method, wildcards
and phrases have been used depending on each database. Ventilator acquired pneumonia
Ventilator aspiration pneumonia, VAP, kit, pack. Study was mainly focused on human, among
nurses and randomized controlled trial method were used . As for language inclusion, english
language was considered. Finally, over 650 potentially relevant report were identified. Among
them only 16 randomised control trail were checked and objectively examined after the
elimination of depletes and obsolete articles.
Review of Evidence
Shahnaz, A., Bhardwaj, U., Tamang, E. K., & Dwivedi, S. (2018). A comparative study to assess
the competency among ICU nurses in using ventilator associated pneumonia bundle to prevent
ventilator associated pneumonia in selected government and private hospitals of New Delhi.
International Journal of Nursing Education, 10(3), 6. https://doi.org/10.5958/0974-
9357.2018.00057.0
A study was done to determine and evaluate the degree of competency in the usage of the VAP
kit and assess the relation between expertise and skills among the competence of ICU nurses
with chosen demographic factors at selected Government and Private hospital of New Delhi . A
Quantitative (Non Experimental) research Approach with comparative descriptive research
2
RASMITA MAHARJAN SNPG917
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
design was adopted for the study. Structured questionnaire and structured observational checklist
was used. Through non probability purposive sampling technique, 60 ICU nurses were selected
among them 30 nurses from government hospital (Safdarjung) and 30 nurses fromprivate
hospital (Indraprastha Apollo) New Delhi, respectively were selected. The findings of the
analysis were enhanced after training sessions by the nurse on 8 of the 10 topics examined (P
from 0.03 to < .001). The places with the most important change is lifting the head of the bed (P
< .001), elevation of the head of the foot (P=.009), oral therapy (P=.009), residual pressure
regulation of the nasal gastric pipe (P=.008) Contraindications to the height of the head of the
bed do not occur in the nurses' experience (P=.38). The strength of the study were try to covered
the two different hospital of india. Furthermore, the study is limited to a survey of only 30 ICU
nurses in chosen hospitals, which are limited to the generalisation of findings and no effort has
been made to determine the enforcement with the VAP inspection list in specified health care
centers owing to a short timeline for data collection.
Gadani, H., Vyas, A., & Kar, A. (2010). A study of ventilator-associated pneumonia: Incidence,
outcome, risk factors and measures to be taken for prevention. Indian Journal of Anaesthesia,
54(6), 535. https://doi.org/10.4103/0019-5049.7264
A randomised control study has been performed at the Intensive Care Unit ( ICU) tertiary care
centre at CMC Hospital, Ludhiana. The goal of the analysis was to objectively evaluate the
occurrence and result, define different danger factors and determine concrete steps that could be
implemented to deter VAP from occurring. A minimum number of 100 patients who were placed
on artifical ventilator were randomly picked. Groups covered people of both sexes who had been
holding on a artificial breathing for longer than 48 h and who were > 15 years of age. Clients
who died or contracted pneumonia within 48 hours or who recovered from pneumonia at the
time of diagnosis and clients with ARDS were omitted from the survey. The level of relevance
was set at P<0.05. It was reported that 37 individuals had produced VAP. A questionnaire was
developed and each individual selected to be included in the analysis was evaluated and tracked
according to the questionnaire. Age, date of admission to ICU, date of introduction of artificial
breathing and mode of evaluation of the patients' airways, or tracheostomy, were reported. In the
3
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
design was adopted for the study. Structured questionnaire and structured observational checklist
was used. Through non probability purposive sampling technique, 60 ICU nurses were selected
among them 30 nurses from government hospital (Safdarjung) and 30 nurses fromprivate
hospital (Indraprastha Apollo) New Delhi, respectively were selected. The findings of the
analysis were enhanced after training sessions by the nurse on 8 of the 10 topics examined (P
from 0.03 to < .001). The places with the most important change is lifting the head of the bed (P
< .001), elevation of the head of the foot (P=.009), oral therapy (P=.009), residual pressure
regulation of the nasal gastric pipe (P=.008) Contraindications to the height of the head of the
bed do not occur in the nurses' experience (P=.38). The strength of the study were try to covered
the two different hospital of india. Furthermore, the study is limited to a survey of only 30 ICU
nurses in chosen hospitals, which are limited to the generalisation of findings and no effort has
been made to determine the enforcement with the VAP inspection list in specified health care
centers owing to a short timeline for data collection.
Gadani, H., Vyas, A., & Kar, A. (2010). A study of ventilator-associated pneumonia: Incidence,
outcome, risk factors and measures to be taken for prevention. Indian Journal of Anaesthesia,
54(6), 535. https://doi.org/10.4103/0019-5049.7264
A randomised control study has been performed at the Intensive Care Unit ( ICU) tertiary care
centre at CMC Hospital, Ludhiana. The goal of the analysis was to objectively evaluate the
occurrence and result, define different danger factors and determine concrete steps that could be
implemented to deter VAP from occurring. A minimum number of 100 patients who were placed
on artifical ventilator were randomly picked. Groups covered people of both sexes who had been
holding on a artificial breathing for longer than 48 h and who were > 15 years of age. Clients
who died or contracted pneumonia within 48 hours or who recovered from pneumonia at the
time of diagnosis and clients with ARDS were omitted from the survey. The level of relevance
was set at P<0.05. It was reported that 37 individuals had produced VAP. A questionnaire was
developed and each individual selected to be included in the analysis was evaluated and tracked
according to the questionnaire. Age, date of admission to ICU, date of introduction of artificial
breathing and mode of evaluation of the patients' airways, or tracheostomy, were reported. In the
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
RASMITA MAHARJAN SNPG917
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
analysis, it was observed that those needing extended ventilator assistance (> 15 days) had a
slightly higher rate of VAP (P-value, 0.001). Supine posture and stuporous comatose cases were
considered to be contributing factors for a high prevalence of VAP which were seen to be
statistically important (P-value, 0.003 which 0.0023, respectively). Out of the 37 patients that
acquired VAP, 10 (27.02 %) acquired early-onset VAP and 27 (72.97%) developed late-onset
VAP. The average mortality rate was 46%, while the mortality rate for VAP patients was 54%.
The early-onset form mortality rate was estimated to be 20%. In the case of late-onset form,
66.67% was noticed. Late-onset VAP has a very strong correlation (P=0.0234) in terms of death
relative to early-onset pneumonia. The study were limited only to one hospital. Furthermore, the
strenghth of the study were excludation of the patient with diagnosed pneumonia.
Osman, S., Al Talhi, Y. M., AlDabbagh, M., Baksh, M., Osman, M., & Azzam, M. (2020). The
incidence of ventilator-associated pneumonia (VAP) in a tertiary-care center: Comparison
between pre- and post-VAP prevention bundle. Journal of Infection and Public Health, 13(4),
552-557. doi:10.1016/j.jiph.2019.09.015
The purpose of this analysis was to apply the established package for prevention of VAP as a
quality control method in the King's PICU Abdulaziz Medical City (KAMC) – Jeddah, Kingdom
of Saudi Arabia (KSA) with a view to rising the amount of VAP incidents over a span of one
year. A single-center, longitudinal analysis was performed between January 2015 and March
2018 and assessed the occurrence of VAP before and after the introduction of the package. The
study provided a summary of two periods of review, the first was pre-bundle rollout from
January 2015 to February 2017, and the second was post-bundle transition from March 2017 to
March 2018. The study involved 141 infants, 95 from the pre-bundle team and 36 from the
bundle section. VAP was formed in 35 per cent of the pre-bundle population compared to 31 per
cent of the bundle group (p = 0.651) with occurrence rates equivalent to 18 and 12 per 1,000
ventilation days, respectively. For the statistical analysis, descriptive statistics such as mean,
standard deviation ( SD), median, size, interquartile, or proportion were used depending on the
characteristics and the choice of variables. The VAP event incidence was calculated as a
different number per 1000 Artificial Respiratory Tube Day. Qualitative factors have been
calculated using chi-square Check or Fisher-Exact check, as appropriate. P-value (p) less than p-
value 0.05 was considered to be statistically significant. Statistical research was carried out with
4
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
analysis, it was observed that those needing extended ventilator assistance (> 15 days) had a
slightly higher rate of VAP (P-value, 0.001). Supine posture and stuporous comatose cases were
considered to be contributing factors for a high prevalence of VAP which were seen to be
statistically important (P-value, 0.003 which 0.0023, respectively). Out of the 37 patients that
acquired VAP, 10 (27.02 %) acquired early-onset VAP and 27 (72.97%) developed late-onset
VAP. The average mortality rate was 46%, while the mortality rate for VAP patients was 54%.
The early-onset form mortality rate was estimated to be 20%. In the case of late-onset form,
66.67% was noticed. Late-onset VAP has a very strong correlation (P=0.0234) in terms of death
relative to early-onset pneumonia. The study were limited only to one hospital. Furthermore, the
strenghth of the study were excludation of the patient with diagnosed pneumonia.
Osman, S., Al Talhi, Y. M., AlDabbagh, M., Baksh, M., Osman, M., & Azzam, M. (2020). The
incidence of ventilator-associated pneumonia (VAP) in a tertiary-care center: Comparison
between pre- and post-VAP prevention bundle. Journal of Infection and Public Health, 13(4),
552-557. doi:10.1016/j.jiph.2019.09.015
The purpose of this analysis was to apply the established package for prevention of VAP as a
quality control method in the King's PICU Abdulaziz Medical City (KAMC) – Jeddah, Kingdom
of Saudi Arabia (KSA) with a view to rising the amount of VAP incidents over a span of one
year. A single-center, longitudinal analysis was performed between January 2015 and March
2018 and assessed the occurrence of VAP before and after the introduction of the package. The
study provided a summary of two periods of review, the first was pre-bundle rollout from
January 2015 to February 2017, and the second was post-bundle transition from March 2017 to
March 2018. The study involved 141 infants, 95 from the pre-bundle team and 36 from the
bundle section. VAP was formed in 35 per cent of the pre-bundle population compared to 31 per
cent of the bundle group (p = 0.651) with occurrence rates equivalent to 18 and 12 per 1,000
ventilation days, respectively. For the statistical analysis, descriptive statistics such as mean,
standard deviation ( SD), median, size, interquartile, or proportion were used depending on the
characteristics and the choice of variables. The VAP event incidence was calculated as a
different number per 1000 Artificial Respiratory Tube Day. Qualitative factors have been
calculated using chi-square Check or Fisher-Exact check, as appropriate. P-value (p) less than p-
value 0.05 was considered to be statistically significant. Statistical research was carried out with
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
RASMITA MAHARJAN SNPG917
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
the Social Sciences Statistical Package ( SPSS) version 25.0. The strength of the study were
covered the large number of sample so the generalization of finding can be done. Furthermore,
the work concentrated mainly on the significance of the VAP levels in kit elimination after the
has been used. Certain ventilator related infections such as Ventilator-Aspirated Tracheitis
(VAT) have not been reported.
Discussion
Hospital-acquired pneumonia tends to be a challenging problem for health care staff. Among
critically ill patients in ICU (Dandagi 2010). Pneumonia is one of the biggest frequent related
hospital-acquired infections. The ventilator artificial airway or the endotracheal (ET) channel can
be transmit the microorganisms in the lungs. Therefore, the most significant obstacle to the
production of VAP is intubation itself (Cakan, Demirkıran,& Yardımcı 2019). The writers
believed that a checklist was an important resource for the health and treatment of chronically ill
patients. It is recommended that healthcare professionals who make bedside visits follow a one-
sentence memorization strategy (Dumbre 2019). The usage of the care kit, a series of primary
measures centred on the guidelines, will promote the application of the guidelines.
Nurse education has a function to be performed in the preventative measures of VAP. Various
risk factors (the use of more than three drugs, enteral intake and tracheotomy) have been strongly
correlated with VAP in the study. Nursing education improves nurses' hand hygiene and
compliance with the VAP bundle Lambert, Palomar, Agodi, Hiesmayr, Lepape, Ingenbleek &
Frank (2013). Parisi, Gerovasili, Dimopoulos, Kampisiouli,Goga, Perivolioti, Nanas (2016 also
showed the value of utilising the VAP package and workers awareness to reduce the frequency
of VAP. Some researchers noticed that package quality analysis in PICU settings is restricted.
The most specific VAP-associated organism is Pseudomonas (43.24%), led by Klebsiella
(18.91%). The overall mortality rate in the Pseudomonas group was also high (62.5 percent). In
other studies, Pseudomonas isolation varies from 15 % to 25%.
This finding was funded by Mandal A.K, (2011) a randomised study at Fortis Hospital, Punjab.
The ventilator kit solution was given to 76 patients with a supplemental oxygen in the ICU for 3
days. The research found that the post-test measurement of ventilator-aspirated pneumonia with
acute lung disease indicated a substantial decrease in ventilator aspirated lung disease in the trial
5
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
the Social Sciences Statistical Package ( SPSS) version 25.0. The strength of the study were
covered the large number of sample so the generalization of finding can be done. Furthermore,
the work concentrated mainly on the significance of the VAP levels in kit elimination after the
has been used. Certain ventilator related infections such as Ventilator-Aspirated Tracheitis
(VAT) have not been reported.
Discussion
Hospital-acquired pneumonia tends to be a challenging problem for health care staff. Among
critically ill patients in ICU (Dandagi 2010). Pneumonia is one of the biggest frequent related
hospital-acquired infections. The ventilator artificial airway or the endotracheal (ET) channel can
be transmit the microorganisms in the lungs. Therefore, the most significant obstacle to the
production of VAP is intubation itself (Cakan, Demirkıran,& Yardımcı 2019). The writers
believed that a checklist was an important resource for the health and treatment of chronically ill
patients. It is recommended that healthcare professionals who make bedside visits follow a one-
sentence memorization strategy (Dumbre 2019). The usage of the care kit, a series of primary
measures centred on the guidelines, will promote the application of the guidelines.
Nurse education has a function to be performed in the preventative measures of VAP. Various
risk factors (the use of more than three drugs, enteral intake and tracheotomy) have been strongly
correlated with VAP in the study. Nursing education improves nurses' hand hygiene and
compliance with the VAP bundle Lambert, Palomar, Agodi, Hiesmayr, Lepape, Ingenbleek &
Frank (2013). Parisi, Gerovasili, Dimopoulos, Kampisiouli,Goga, Perivolioti, Nanas (2016 also
showed the value of utilising the VAP package and workers awareness to reduce the frequency
of VAP. Some researchers noticed that package quality analysis in PICU settings is restricted.
The most specific VAP-associated organism is Pseudomonas (43.24%), led by Klebsiella
(18.91%). The overall mortality rate in the Pseudomonas group was also high (62.5 percent). In
other studies, Pseudomonas isolation varies from 15 % to 25%.
This finding was funded by Mandal A.K, (2011) a randomised study at Fortis Hospital, Punjab.
The ventilator kit solution was given to 76 patients with a supplemental oxygen in the ICU for 3
days. The research found that the post-test measurement of ventilator-aspirated pneumonia with
acute lung disease indicated a substantial decrease in ventilator aspirated lung disease in the trial
5
RASMITA MAHARJAN SNPG917
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
community 10% relative to the control community 3.6 %. The study indicates that 43 shows the
application of the ventilator kit was successful in avoiding the resulting pneumonia of the
ventilator.
This research was sponsored by Ravishankar M, et.al, (2010) and a prospective research was
undertaken at the College of Medical Sciences & Teaching Hospital, Bidar, KarnatakaThe
breathing tube package has been applied to SICU patients. VAP decreased to 3.4 cases in the
ventilator kit population and VAP was observed in a total of 10.2 cases in the non-ventilator
bundle category. The report found that the introduction of the respiratory kit was associated with
a significantly decreased rate of VAP in SICU clients.
Conclusion
Despite much study, VAP appears to be one of the most dangerous ICU-acquired infections and
is correlated with increased mortality carries substantial burdens of morbidity, antibiotic usage
and e. The research was undertaken toevaluate the effectiveness of the ventilator package in the
reduction of ventilator-aspirated pneumonia in intubated patients in chosen hospitals. The
findings the research shows that the ventilator package was successful in avoiding pneumonia
associated with the ventilator in patients with mechanical ventilator.
6
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
community 10% relative to the control community 3.6 %. The study indicates that 43 shows the
application of the ventilator kit was successful in avoiding the resulting pneumonia of the
ventilator.
This research was sponsored by Ravishankar M, et.al, (2010) and a prospective research was
undertaken at the College of Medical Sciences & Teaching Hospital, Bidar, KarnatakaThe
breathing tube package has been applied to SICU patients. VAP decreased to 3.4 cases in the
ventilator kit population and VAP was observed in a total of 10.2 cases in the non-ventilator
bundle category. The report found that the introduction of the respiratory kit was associated with
a significantly decreased rate of VAP in SICU clients.
Conclusion
Despite much study, VAP appears to be one of the most dangerous ICU-acquired infections and
is correlated with increased mortality carries substantial burdens of morbidity, antibiotic usage
and e. The research was undertaken toevaluate the effectiveness of the ventilator package in the
reduction of ventilator-aspirated pneumonia in intubated patients in chosen hospitals. The
findings the research shows that the ventilator package was successful in avoiding pneumonia
associated with the ventilator in patients with mechanical ventilator.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

RASMITA MAHARJAN SNPG917
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
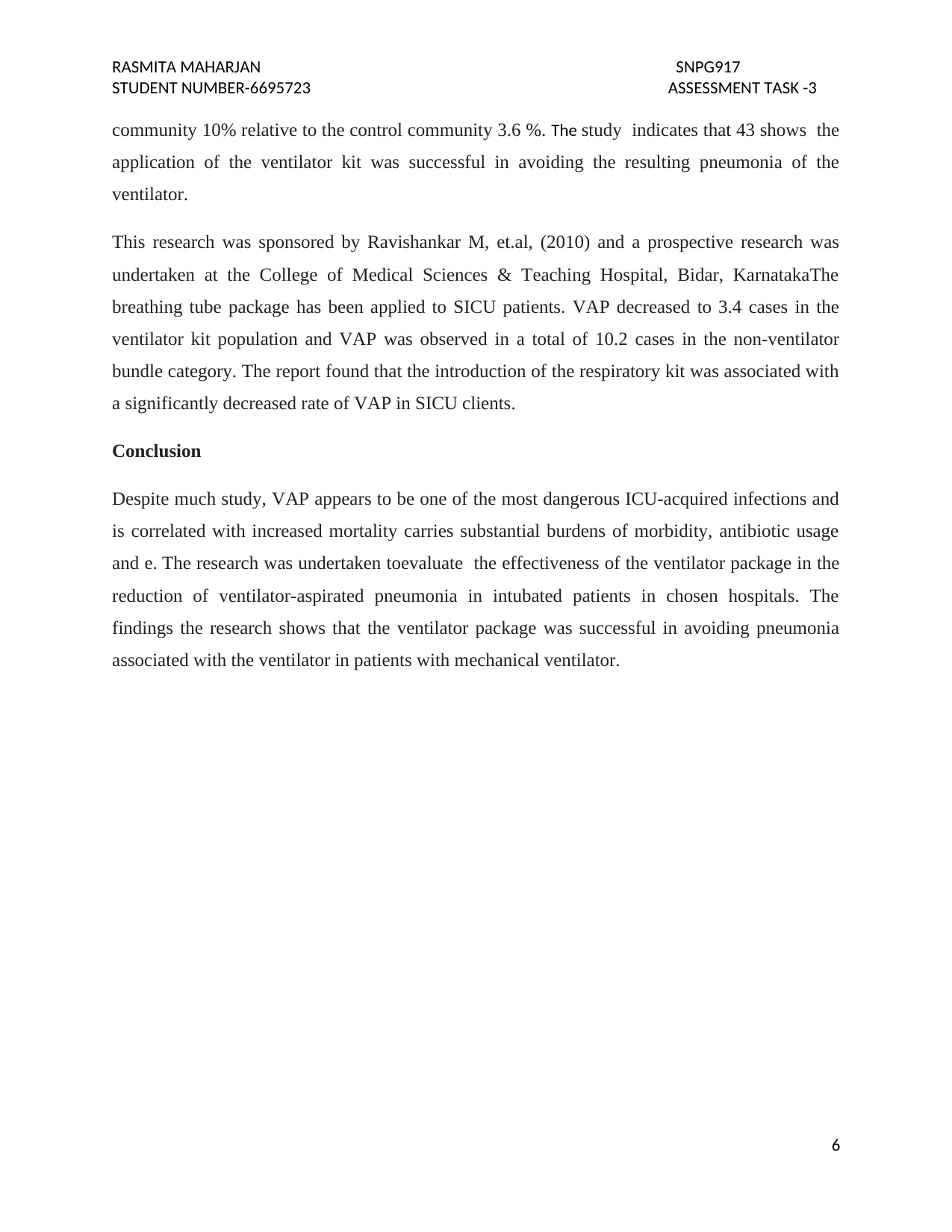
Appraisal tool for Article 1
Shahnaz, A., Bhardwaj, U., Tamang, E. K., & Dwivedi, S. (2018). A comparative study to assess
the competency among ICU nurses in using ventilator associated pneumonia bundle to prevent
ventilator associated pneumonia in selected government and private hospitals of New Delhi.
International Journal of Nursing Education, 10(3), 6. https://doi.org/10.5958/0974-
9357.2018.00057.0
Critical appraisal guidelines – quantitative research (Comparable cohort & case control studies)
Criteria Yes No Unclear N/A
1. Is the sample representative of people in the population
as a whole?
2. Are the participants at a similar point in the course of
their condition / illness?
3. Has bias been minimised in relation to the selection of
cases and of controls?
4. Are confounding factors identified and strategies to deal
with them stated?
5. Are the outcomes assessed using objective criteria?
6. Was follow up carried out over a sufficient time period?
7. Were the outcomes of people who withdrew described
and included in the analysis?
8. Were outcomes measured in a reliable way?
9. Was appropriate statistical analysis used?
7
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
Appraisal tool for Article 1
Shahnaz, A., Bhardwaj, U., Tamang, E. K., & Dwivedi, S. (2018). A comparative study to assess
the competency among ICU nurses in using ventilator associated pneumonia bundle to prevent
ventilator associated pneumonia in selected government and private hospitals of New Delhi.
International Journal of Nursing Education, 10(3), 6. https://doi.org/10.5958/0974-
9357.2018.00057.0
Critical appraisal guidelines – quantitative research (Comparable cohort & case control studies)
Criteria Yes No Unclear N/A
1. Is the sample representative of people in the population
as a whole?
2. Are the participants at a similar point in the course of
their condition / illness?
3. Has bias been minimised in relation to the selection of
cases and of controls?
4. Are confounding factors identified and strategies to deal
with them stated?
5. Are the outcomes assessed using objective criteria?
6. Was follow up carried out over a sufficient time period?
7. Were the outcomes of people who withdrew described
and included in the analysis?
8. Were outcomes measured in a reliable way?
9. Was appropriate statistical analysis used?
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
RASMITA MAHARJAN SNPG917
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
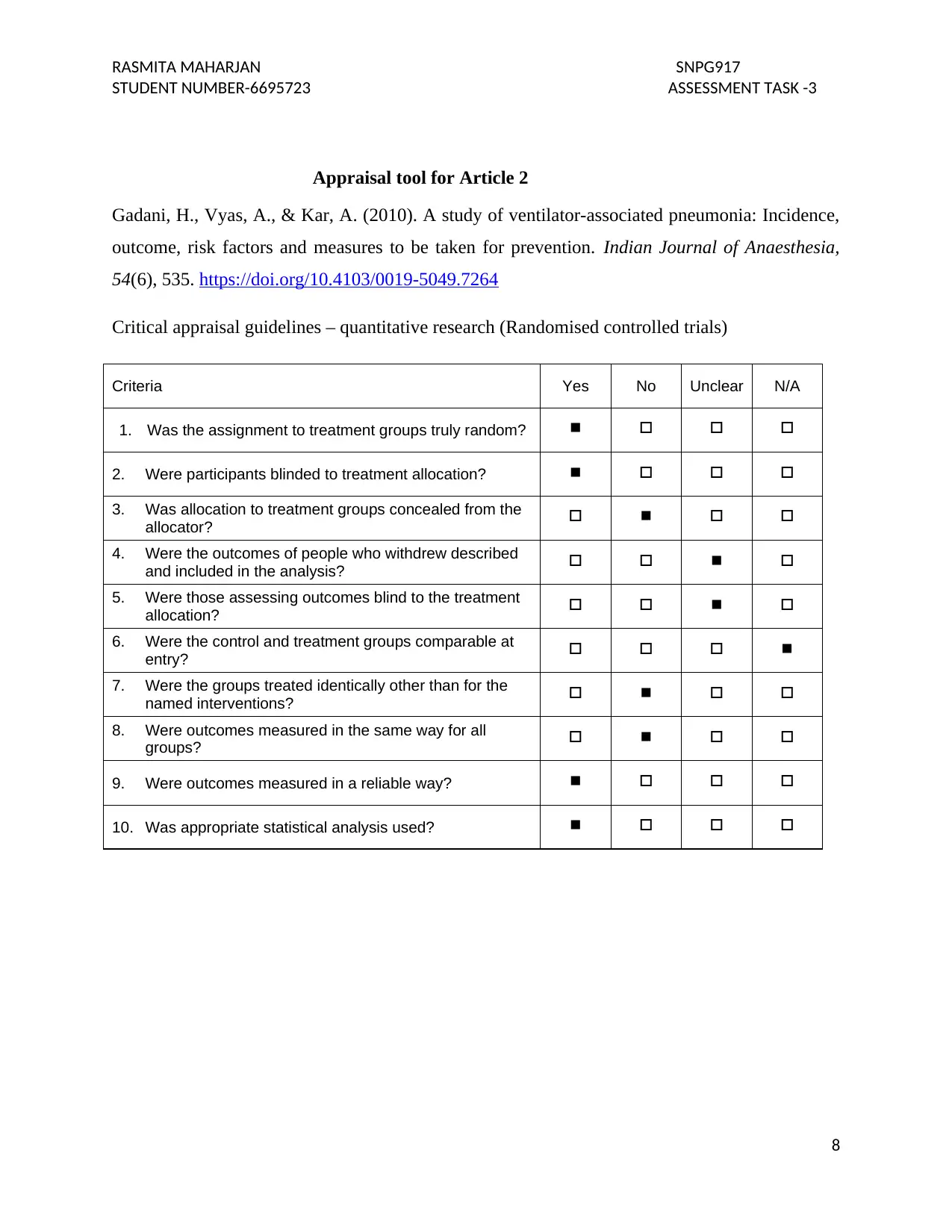
Appraisal tool for Article 2
Gadani, H., Vyas, A., & Kar, A. (2010). A study of ventilator-associated pneumonia: Incidence,
outcome, risk factors and measures to be taken for prevention. Indian Journal of Anaesthesia,
54(6), 535. https://doi.org/10.4103/0019-5049.7264
Critical appraisal guidelines – quantitative research (Randomised controlled trials)
Criteria Yes No Unclear N/A
1. Was the assignment to treatment groups truly random?
2. Were participants blinded to treatment allocation?
3. Was allocation to treatment groups concealed from the
allocator?
4. Were the outcomes of people who withdrew described
and included in the analysis?
5. Were those assessing outcomes blind to the treatment
allocation?
6. Were the control and treatment groups comparable at
entry?
7. Were the groups treated identically other than for the
named interventions?
8. Were outcomes measured in the same way for all
groups?
9. Were outcomes measured in a reliable way?
10. Was appropriate statistical analysis used?
8
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
Appraisal tool for Article 2
Gadani, H., Vyas, A., & Kar, A. (2010). A study of ventilator-associated pneumonia: Incidence,
outcome, risk factors and measures to be taken for prevention. Indian Journal of Anaesthesia,
54(6), 535. https://doi.org/10.4103/0019-5049.7264
Critical appraisal guidelines – quantitative research (Randomised controlled trials)
Criteria Yes No Unclear N/A
1. Was the assignment to treatment groups truly random?
2. Were participants blinded to treatment allocation?
3. Was allocation to treatment groups concealed from the
allocator?
4. Were the outcomes of people who withdrew described
and included in the analysis?
5. Were those assessing outcomes blind to the treatment
allocation?
6. Were the control and treatment groups comparable at
entry?
7. Were the groups treated identically other than for the
named interventions?
8. Were outcomes measured in the same way for all
groups?
9. Were outcomes measured in a reliable way?
10. Was appropriate statistical analysis used?
8
RASMITA MAHARJAN SNPG917
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
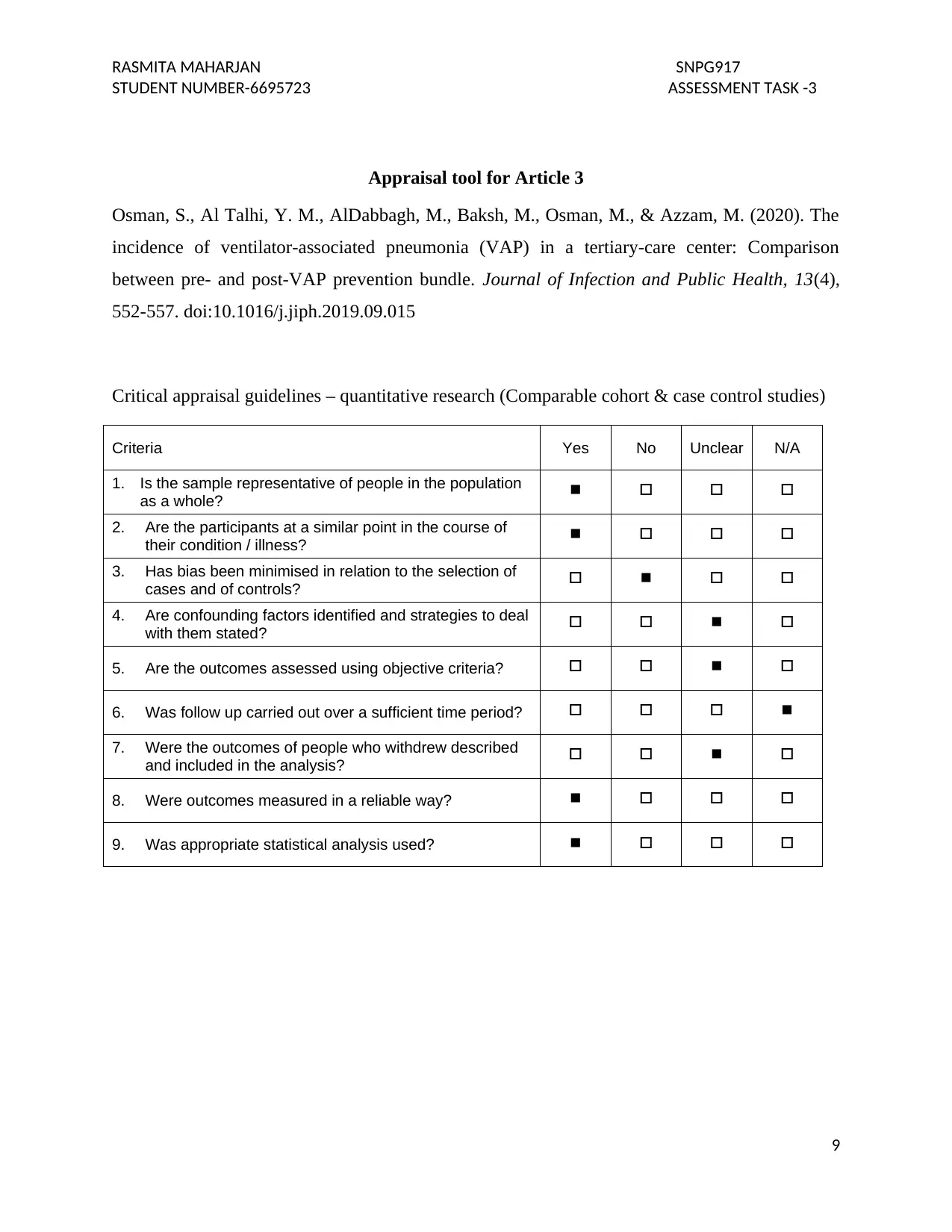
Appraisal tool for Article 3
Osman, S., Al Talhi, Y. M., AlDabbagh, M., Baksh, M., Osman, M., & Azzam, M. (2020). The
incidence of ventilator-associated pneumonia (VAP) in a tertiary-care center: Comparison
between pre- and post-VAP prevention bundle. Journal of Infection and Public Health, 13(4),
552-557. doi:10.1016/j.jiph.2019.09.015
Critical appraisal guidelines – quantitative research (Comparable cohort & case control studies)
Criteria Yes No Unclear N/A
1. Is the sample representative of people in the population
as a whole?
2. Are the participants at a similar point in the course of
their condition / illness?
3. Has bias been minimised in relation to the selection of
cases and of controls?
4. Are confounding factors identified and strategies to deal
with them stated?
5. Are the outcomes assessed using objective criteria?
6. Was follow up carried out over a sufficient time period?
7. Were the outcomes of people who withdrew described
and included in the analysis?
8. Were outcomes measured in a reliable way?
9. Was appropriate statistical analysis used?
9
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
Appraisal tool for Article 3
Osman, S., Al Talhi, Y. M., AlDabbagh, M., Baksh, M., Osman, M., & Azzam, M. (2020). The
incidence of ventilator-associated pneumonia (VAP) in a tertiary-care center: Comparison
between pre- and post-VAP prevention bundle. Journal of Infection and Public Health, 13(4),
552-557. doi:10.1016/j.jiph.2019.09.015
Critical appraisal guidelines – quantitative research (Comparable cohort & case control studies)
Criteria Yes No Unclear N/A
1. Is the sample representative of people in the population
as a whole?
2. Are the participants at a similar point in the course of
their condition / illness?
3. Has bias been minimised in relation to the selection of
cases and of controls?
4. Are confounding factors identified and strategies to deal
with them stated?
5. Are the outcomes assessed using objective criteria?
6. Was follow up carried out over a sufficient time period?
7. Were the outcomes of people who withdrew described
and included in the analysis?
8. Were outcomes measured in a reliable way?
9. Was appropriate statistical analysis used?
9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
RASMITA MAHARJAN SNPG917
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
Reference list
Cakan, M. Z., Demirkıran, H., & Yardımcı, C. (2019). Training healthcare staff on ventilator-
associated pneumonia (VAP) prevention bundle and its effects on VAP bundle on VAP.
Eastern Journal Of Medicine, 24(4), 530-535. https://doi.org/10.5505/ejm.2019.63626
Dandagi, G. (2010). Nosocomial pneumonia in critically ill patients. Lung India, 27(3), 149.
doi:10.4103/0970-2113.68321
Dumbre, D. U. (2019). A study to assess the knowledge and compliance of critical care nurses
regarding ventilator care bundle in prevention of ventilator associated pneumonia.
Medico-Legal Update, 19(1), 176. doi:10.5958/0974-1283.2019.00035.5
Lambert, M. L., Palomar, M., Agodi, A., Hiesmayr,M., Lepape, A., Ingenbleek, A., ... & Frank,
U.(2013). Prevention of ventilator-associated pneumonia in intensive care units: an
international online survey. Antimicrobial resistance and infection control, 2(1), 9.
doiI: 10.1186/2047-2994-2-9
Lawrence, P., & Fulbrook, P. (2011). The ventilator care bundle and its impact on ventilator-
associated pneumonia: A review of the evidence. Nursing in Critical Care, 16(5), 222-
234. doi:10.1111/j.1478-5153.2010.00430.x
Mandal, A, K. (2011). “Implementation of a ventilator care bundle to reduce the incidence of
ventilator acquired pneumonia”. Journal of BMC, 5(6): 71- 75
Keyt, H., Faverio, P., & Restrepo, M. I. (2014). Prevention of ventilator-associated pneumonia in
the intensive care unit: a review of the clinically relevant recent advancements. The
Indian journal of medical research, 139(6), 814–821.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4164993/
Parisi, M., Gerovasili, V., Dimopoulos, S., Kampisiouli, E., Goga, C., Perivolioti, E., … Nanas,
S. (2016). Use of ventilator bundle and staff education to decrease ventilator-associated
10
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
Reference list
Cakan, M. Z., Demirkıran, H., & Yardımcı, C. (2019). Training healthcare staff on ventilator-
associated pneumonia (VAP) prevention bundle and its effects on VAP bundle on VAP.
Eastern Journal Of Medicine, 24(4), 530-535. https://doi.org/10.5505/ejm.2019.63626
Dandagi, G. (2010). Nosocomial pneumonia in critically ill patients. Lung India, 27(3), 149.
doi:10.4103/0970-2113.68321
Dumbre, D. U. (2019). A study to assess the knowledge and compliance of critical care nurses
regarding ventilator care bundle in prevention of ventilator associated pneumonia.
Medico-Legal Update, 19(1), 176. doi:10.5958/0974-1283.2019.00035.5
Lambert, M. L., Palomar, M., Agodi, A., Hiesmayr,M., Lepape, A., Ingenbleek, A., ... & Frank,
U.(2013). Prevention of ventilator-associated pneumonia in intensive care units: an
international online survey. Antimicrobial resistance and infection control, 2(1), 9.
doiI: 10.1186/2047-2994-2-9
Lawrence, P., & Fulbrook, P. (2011). The ventilator care bundle and its impact on ventilator-
associated pneumonia: A review of the evidence. Nursing in Critical Care, 16(5), 222-
234. doi:10.1111/j.1478-5153.2010.00430.x
Mandal, A, K. (2011). “Implementation of a ventilator care bundle to reduce the incidence of
ventilator acquired pneumonia”. Journal of BMC, 5(6): 71- 75
Keyt, H., Faverio, P., & Restrepo, M. I. (2014). Prevention of ventilator-associated pneumonia in
the intensive care unit: a review of the clinically relevant recent advancements. The
Indian journal of medical research, 139(6), 814–821.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4164993/
Parisi, M., Gerovasili, V., Dimopoulos, S., Kampisiouli, E., Goga, C., Perivolioti, E., … Nanas,
S. (2016). Use of ventilator bundle and staff education to decrease ventilator-associated
10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
RASMITA MAHARJAN SNPG917
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
pneumonia in intensive care patients. Critical Care Nurse, 36(5), e1-e7.
doi:10.4037/ccn2016520
Rello, J., Lode, H., Cornaglia, G., & Masterton, R. (2010). A European care bundle for prevention of
ventilator-associated pneumonia. Intensive Care Medicine, 36(5), 773-780.
https://doi.org/10.1007/s00134-010-1841-5
Samra, S. R., Sherif, D. M., & Elokda, S. A. (2017). Impact of VAP bundle adherence among ventilated
critically ill patients and its effectiveness in adult ICU. Egyptian Journal of Chest Diseases and
Tuberculosis, 66(1), 81-86. https://doi.org/10.1016/j.ejcdt.2016.08.010
Shahnaz, A., Bhardwaj, U., Tamang, E. K., & Dwivedi, S. (2018). A comparative study to assess the
competency among ICU nurses in using ventilator associated pneumonia bundle to prevent
ventilator associated pneumonia in selected government and private hospitals of New Delhi.
International Journal of Nursing Education, 10(3), 6. https://doi.org/10.5958/0974-
9357.2018.00057.0
Shitrit, P., Meirson, M., Mendelson, G., & Chowers, M. (2015). Intervention to reduce
ventilator-associated pneumonia in individuals on long-term ventilation by introducing a
customized bundle. Journal of the American Geriatrics Society, 63(10), 2089-2093.
https://doi.org/10.1111/jgs.13646
11
STUDENT NUMBER-6695723 ASSESSMENT TASK -3
pneumonia in intensive care patients. Critical Care Nurse, 36(5), e1-e7.
doi:10.4037/ccn2016520
Rello, J., Lode, H., Cornaglia, G., & Masterton, R. (2010). A European care bundle for prevention of
ventilator-associated pneumonia. Intensive Care Medicine, 36(5), 773-780.
https://doi.org/10.1007/s00134-010-1841-5
Samra, S. R., Sherif, D. M., & Elokda, S. A. (2017). Impact of VAP bundle adherence among ventilated
critically ill patients and its effectiveness in adult ICU. Egyptian Journal of Chest Diseases and
Tuberculosis, 66(1), 81-86. https://doi.org/10.1016/j.ejcdt.2016.08.010
Shahnaz, A., Bhardwaj, U., Tamang, E. K., & Dwivedi, S. (2018). A comparative study to assess the
competency among ICU nurses in using ventilator associated pneumonia bundle to prevent
ventilator associated pneumonia in selected government and private hospitals of New Delhi.
International Journal of Nursing Education, 10(3), 6. https://doi.org/10.5958/0974-
9357.2018.00057.0
Shitrit, P., Meirson, M., Mendelson, G., & Chowers, M. (2015). Intervention to reduce
ventilator-associated pneumonia in individuals on long-term ventilation by introducing a
customized bundle. Journal of the American Geriatrics Society, 63(10), 2089-2093.
https://doi.org/10.1111/jgs.13646
11
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





