NURS2006 Supplementary Assessment: Medication Error Project
VerifiedAdded on 2023/05/29
|11
|4526
|453
Report
AI Summary
This report presents a Clinical Practice Improvement (CPI) project focused on reducing medication errors by nurses in the acute care system. The project aims to identify individual and system issues contributing to medication errors and to review evidence-based interventions. The report emphasizes the relevance of clinical governance, outlining key stakeholders such as insurance companies, physicians, and patients. It utilizes the Plan-Do-Study-Act (PDSA) cycle as a CPI tool to analyze common medication errors, propose changes, and measure improvements. The proposed interventions include leveraging information technology, such as physician hightech and changes in working schedules. The report also addresses barriers to implementation, such as the magnitude and complexity of the change and competing demands. The report provides a comprehensive overview of the project, including the background, methodology, interventions, and challenges, offering valuable insights for healthcare professionals and students alike. The report concludes by discussing the evaluation of the project.
NURS2006 SUPPLEMENTARY ASSESSMENT
Clinical Practice Improvement Project Report on
Individual and /or system issues that can reduce or prevent medication errors
by nurses in the acute care system
Student Name, FAN and ID:
Project title;
Individual and /or system issues that can reduce or prevent medication errors by nurses in
the acute care system
Project Aim:
To identifying individuals and /or system issues that can help in reducing or
preventing medication errors by the nurses in acute care system for a period of 6
months.
To systematically review and appraise empirical evidence which is associated with
administration medication errors in acute care system.
Background and Evidence that the issue is worth solving:
The major component of health services quality in the field of healthcare provision is the patients’
safety (Hayes et al. 2015). Promoting patients’ safety level starts with identification of medical errors
and what causes them (Stavropoulou, Doherty and Tosey, 2015). Some of medical errors such as
medication errors are the most prevailing errors threatening health which has become a global
problem (Hayes et al. 2015). An important part of the treatment and care process is the execution of
medication and it is also the main part of performance in the nursing profession (Birks et al. 2016).
Understanding the causes of these errors it will be easy to design and implement the most
appropriate intervention to minimise their occurrence.
Relevance of Clinical Governance to your project
The relevance of clinical governance in this report is to promote and raise patient satisfaction,
increase efficiency and collaborative relationship inside and across clinical teams, and raise job
satisfaction level among professionals, and improve clinical outcome (Birks et al. 2016). Clinical
governance will see accountability and continuity of service quality improvement and safeguard high
standards of service through creation of an environment that attract excellence in acute care system
to thrive (Hayes et al. 2015). Clinical governance in this project will involve four pillars which
NURS2006 Supplementary Assessment for Semester Two, 2018. 1
Clinical Practice Improvement Project Report on
Individual and /or system issues that can reduce or prevent medication errors
by nurses in the acute care system
Student Name, FAN and ID:
Project title;
Individual and /or system issues that can reduce or prevent medication errors by nurses in
the acute care system
Project Aim:
To identifying individuals and /or system issues that can help in reducing or
preventing medication errors by the nurses in acute care system for a period of 6
months.
To systematically review and appraise empirical evidence which is associated with
administration medication errors in acute care system.
Background and Evidence that the issue is worth solving:
The major component of health services quality in the field of healthcare provision is the patients’
safety (Hayes et al. 2015). Promoting patients’ safety level starts with identification of medical errors
and what causes them (Stavropoulou, Doherty and Tosey, 2015). Some of medical errors such as
medication errors are the most prevailing errors threatening health which has become a global
problem (Hayes et al. 2015). An important part of the treatment and care process is the execution of
medication and it is also the main part of performance in the nursing profession (Birks et al. 2016).
Understanding the causes of these errors it will be easy to design and implement the most
appropriate intervention to minimise their occurrence.
Relevance of Clinical Governance to your project
The relevance of clinical governance in this report is to promote and raise patient satisfaction,
increase efficiency and collaborative relationship inside and across clinical teams, and raise job
satisfaction level among professionals, and improve clinical outcome (Birks et al. 2016). Clinical
governance will see accountability and continuity of service quality improvement and safeguard high
standards of service through creation of an environment that attract excellence in acute care system
to thrive (Hayes et al. 2015). Clinical governance in this project will involve four pillars which
NURS2006 Supplementary Assessment for Semester Two, 2018. 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
includes:
Clinical performance audit
Clinical assessment enables nurses, doctors, and other professionals in healthcare systems to
measure the quality services they offer (Gibson et al., 2015). It is also useful in helping them to
compare their improvement against a standard to see how they are doing. New proposals also need
further audit to test whether they have been successful.
Professional development and management
To reduce medication errors, knowledge and skills for the nurses that care for patient is important so
that a good job is done. This is why nurses need opportunities to increase their knowledge and skills
(Gibson et al. 2015). This in turn increases job satisfaction among nursing professionals,
management improved performance, and clinicians’ improved credentialing, and improved
professional development training for workforce.
Clinical risk
This would include investigating and minimizing the risks to patients by: identifying what does go
wrong, what can be done to avoid reoccurrence of errors, identifying influences of the errors during
care, and ensuring systems are put in place to prevent or reduce risks.
Consumer values
Improving trust among the patients is vital that nurses work in partnership with patients and their
carers if their goal is to offer quality care. This means, understanding of the priorities and concerns
of the consumers of the services offered by involving them in what you do including planning and
policy making. To gain their views we need to apply patients and carer councils and also monitor
their views through complaints and compliments received through PALS (Gibson et al. 2015). By
doing so there is an opportunity for improved patients outcome, enhanced health service
understanding and responsiveness to consumer need, as well as enhanced consumer and patients’
knowledge and participation in delivery of health services and management.
Key Stakeholders:
The key stakeholders in acute care systems include insurance companies, physicians, government,
pharmaceutical firms, patients and employers. Insurance companies are involved in selling health
coverage plans directly to the patients or through their employer (indirectly) or through government
intersessions (Mitchell et al. 2016). Each stakeholder is involved in one way or the other in reducing
medication errors in this project. Employers also offer health insurance coverage to their employees
deductable from their salaries.
Pharmaceutical firms are involved in the development and marketing of medications prescribed by
doctors for the patients’ treatments (Mitchell et al. 2016). Last and not least the government
NURS2006 Supplementary Assessment for Semester Two, 2018. 2
Clinical performance audit
Clinical assessment enables nurses, doctors, and other professionals in healthcare systems to
measure the quality services they offer (Gibson et al., 2015). It is also useful in helping them to
compare their improvement against a standard to see how they are doing. New proposals also need
further audit to test whether they have been successful.
Professional development and management
To reduce medication errors, knowledge and skills for the nurses that care for patient is important so
that a good job is done. This is why nurses need opportunities to increase their knowledge and skills
(Gibson et al. 2015). This in turn increases job satisfaction among nursing professionals,
management improved performance, and clinicians’ improved credentialing, and improved
professional development training for workforce.
Clinical risk
This would include investigating and minimizing the risks to patients by: identifying what does go
wrong, what can be done to avoid reoccurrence of errors, identifying influences of the errors during
care, and ensuring systems are put in place to prevent or reduce risks.
Consumer values
Improving trust among the patients is vital that nurses work in partnership with patients and their
carers if their goal is to offer quality care. This means, understanding of the priorities and concerns
of the consumers of the services offered by involving them in what you do including planning and
policy making. To gain their views we need to apply patients and carer councils and also monitor
their views through complaints and compliments received through PALS (Gibson et al. 2015). By
doing so there is an opportunity for improved patients outcome, enhanced health service
understanding and responsiveness to consumer need, as well as enhanced consumer and patients’
knowledge and participation in delivery of health services and management.
Key Stakeholders:
The key stakeholders in acute care systems include insurance companies, physicians, government,
pharmaceutical firms, patients and employers. Insurance companies are involved in selling health
coverage plans directly to the patients or through their employer (indirectly) or through government
intersessions (Mitchell et al. 2016). Each stakeholder is involved in one way or the other in reducing
medication errors in this project. Employers also offer health insurance coverage to their employees
deductable from their salaries.
Pharmaceutical firms are involved in the development and marketing of medications prescribed by
doctors for the patients’ treatments (Mitchell et al. 2016). Last and not least the government
NURS2006 Supplementary Assessment for Semester Two, 2018. 2
subsidizes healthcare for the disabled, elderly and the poor. Physicians on the other hand are the
medical care providers while patient becomes the client (Mitchell et al. 2016).
CPI Tool:
The Plan-Do-Study-Act (PDSA) cycle
This model of improvement was developed by Associates in Process Improvement. It is simple,
powerful, and very effective tool for accelerating improvement. However, the tool is not meant to
replace what organizations are using today (Mitchell et al. 2016). Its main goal is improvement
acceleration. Hundreds of health care organisations have successfully used this tool to improve and
accelerate health care processes and outcomes (Birks et al. 2016). This model contains two parts:
One, three important questions, addressed in any order and two, the plan Plan-Do-Study-Act (PDSA)
cycle used to examine changes in the actual work situations (Gibson et al., 2015). The cycle is meant
to guide and determine if there is improvement on change. The following would be the focus.
What are the common medication errors done by the nurses in acute care system? What changes
can be made in those medication errors? What changes that will tell whether the improvement or
success has been achieved?
Team formation
This tool state that, for a successful improvement effort, inclusion of the right people in the
improvement team is critical in the process. No group is equal to the other and in this project teams
will be formed in ways that fits our needs. This is in the stage of planning where best team is
selected from those willing to bring change.
Model of improvement
Setting the goal
This should be measurable and time specific and address specific composition that would be affected
e.g. people or systems (Stavropoulou, Doherty and Tosey, 2015). The specific goal is to identify the
common medication errors in acute care system. This has to be done in small portion of nurses who
NURS2006 Supplementary Assessment for Semester Two, 2018. 3
How we will know change in improvement
What change we can make to result in improvement?
What is to be accomplished?
medical care providers while patient becomes the client (Mitchell et al. 2016).
CPI Tool:
The Plan-Do-Study-Act (PDSA) cycle
This model of improvement was developed by Associates in Process Improvement. It is simple,
powerful, and very effective tool for accelerating improvement. However, the tool is not meant to
replace what organizations are using today (Mitchell et al. 2016). Its main goal is improvement
acceleration. Hundreds of health care organisations have successfully used this tool to improve and
accelerate health care processes and outcomes (Birks et al. 2016). This model contains two parts:
One, three important questions, addressed in any order and two, the plan Plan-Do-Study-Act (PDSA)
cycle used to examine changes in the actual work situations (Gibson et al., 2015). The cycle is meant
to guide and determine if there is improvement on change. The following would be the focus.
What are the common medication errors done by the nurses in acute care system? What changes
can be made in those medication errors? What changes that will tell whether the improvement or
success has been achieved?
Team formation
This tool state that, for a successful improvement effort, inclusion of the right people in the
improvement team is critical in the process. No group is equal to the other and in this project teams
will be formed in ways that fits our needs. This is in the stage of planning where best team is
selected from those willing to bring change.
Model of improvement
Setting the goal
This should be measurable and time specific and address specific composition that would be affected
e.g. people or systems (Stavropoulou, Doherty and Tosey, 2015). The specific goal is to identify the
common medication errors in acute care system. This has to be done in small portion of nurses who
NURS2006 Supplementary Assessment for Semester Two, 2018. 3
How we will know change in improvement
What change we can make to result in improvement?
What is to be accomplished?
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
work in acute care system.
Establishing Measures
To determine if a specific change leads to a certain improvement the teams will use quantitative
measures. There will be determination of per cent which will have reduced from the improved
measures that are suggested.
Selecting changes
Mostly ideas originate from people working within the system or experiences of others who tried
and succeeded.
Testing of the changes
This tool (PDSA) is the shorthand for testing improvement on small scale in the real work setting
through planning, trying, observing, and acting on the learning process (Stavropoulou, Doherty and
Tosey, 2015). This represents the scientific method modified for action-oriented learning. After
determining the changes that can be adopted testing to see whether it worked will be carried out.
Implementing Changes
This is done after a change test on a small scale, learning from each test, and refining the change
through several cycles of PDSA. Thereafter, the team may opt to implement the change on larger
scale e.g. an entire unit (Stavropoulou, Doherty & Tosey, 2015). If changes have been achieved the
implementing changes will have to continue being utilized from then.
Spreading Changes
After successful implementation of a set of changes for an entire unit, the changes can be spread to
other professionals in the organization or organizations. Changes that proved to create the required
change will be shared with other professionals to adapt them so as to reduce the medication errors.
Summary of proposed intervention:
A medication error may be defined as any preventable event that may lead or cause inappropriate
use of medicine or harm to patient (Castaneda et al. 2015). The medication error may occur in any
stage of medication management process including preparation, transcription, prescription, and
administration.
Using information technology to reduce or prevent medication errors
Medication errors are injurious and costly to patients and so common in acute care system.
Reviewed literature states that, particular sets of information technology can minimize the rates of
medication errors occurrences. However, there is inadequate data in existence for different
technologies as those figures available relate to adult settings (Mitchell et al. 2016). Physician High-
tech will significantly minimise the occurrence of severe medication errors among in-patients adults
NURS2006 Supplementary Assessment for Semester Two, 2018. 4
Establishing Measures
To determine if a specific change leads to a certain improvement the teams will use quantitative
measures. There will be determination of per cent which will have reduced from the improved
measures that are suggested.
Selecting changes
Mostly ideas originate from people working within the system or experiences of others who tried
and succeeded.
Testing of the changes
This tool (PDSA) is the shorthand for testing improvement on small scale in the real work setting
through planning, trying, observing, and acting on the learning process (Stavropoulou, Doherty and
Tosey, 2015). This represents the scientific method modified for action-oriented learning. After
determining the changes that can be adopted testing to see whether it worked will be carried out.
Implementing Changes
This is done after a change test on a small scale, learning from each test, and refining the change
through several cycles of PDSA. Thereafter, the team may opt to implement the change on larger
scale e.g. an entire unit (Stavropoulou, Doherty & Tosey, 2015). If changes have been achieved the
implementing changes will have to continue being utilized from then.
Spreading Changes
After successful implementation of a set of changes for an entire unit, the changes can be spread to
other professionals in the organization or organizations. Changes that proved to create the required
change will be shared with other professionals to adapt them so as to reduce the medication errors.
Summary of proposed intervention:
A medication error may be defined as any preventable event that may lead or cause inappropriate
use of medicine or harm to patient (Castaneda et al. 2015). The medication error may occur in any
stage of medication management process including preparation, transcription, prescription, and
administration.
Using information technology to reduce or prevent medication errors
Medication errors are injurious and costly to patients and so common in acute care system.
Reviewed literature states that, particular sets of information technology can minimize the rates of
medication errors occurrences. However, there is inadequate data in existence for different
technologies as those figures available relate to adult settings (Mitchell et al. 2016). Physician High-
tech will significantly minimise the occurrence of severe medication errors among in-patients adults
NURS2006 Supplementary Assessment for Semester Two, 2018. 4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
if combined with the assessment support (Haines, 2018). Even though there is existence of
insufficient evidence some particular information technologies for inpatients maybe significant
(Roughead, Semple and Rosenfeld, 2016). The degree of benefit could be greater in paediatrics than
in adults’ medicine since there is need for dosing based on weight. In addition, evaluation,
dissemination and application of exact paediatrics’ computerised information is very important
(D’Andreamatteo et al. 2015). This is an example of system issue that can reduce medication error. It
can also be applied in reducing medication errors in outpatient setting and inpatients setting.
The system approach usually targets hitches in methods as opposed to blaming it on separate entity.
System error is made successful by introduction of checks to capture errors before they patient is
reached, which create a blameless culture, educating personnel, and system functions
simplification.
Change in Working Schedule (CWS). This intervention has not been so much focused on to solve
medical error but one study that involved an investigation of the effects of CWS shown comparisons
being done on medication error made by medical interns who worked in traditional schedule as
compared to those errors made when extensions of work shift were removed (Runciman, Merry and
Walton, 2017).
Interns who worked on extended shift traditional schedule made several medical errors compared to
their counterparts who worked in intervention group (Haines, 2018). This was the different interns
who worked in intervention group made 82.5 errors per 1000 patient-days compared with Interns
who worked on extended shift traditional schedule who made 99.7 errors per 1000 patient-days (P=
0.03) (Hayes et al., 2015). Increasing the interns working hours is the major challenge and in
reducing the medication errors in the ICU.
Recent studies have also indicated that within hospitals, of all trainees, interns (postgraduate year 1)
work in extended hours (Runciman, Merry and Walton, 2017). This has an effect of making them
prone to fatigue-induced errors. A survey of house officers proven that by 41 per cent of them
relating fatigue with their most serious mistakes (Mitchell et al. 2016). In simple and understandable
way, simple interventions may achieve impressive reductions in error rates (Haines, 2018). There is a
need to better categorize, replicate, and test study designs to maximize protection from biasness in
evidence of medical error reduction needs.
Barriers to implementation:
Magnitude and Complexity of the Change
INTERACT (Interventions to Reduce Acute Care Transfers) is not simple but a complex program that
employs multiple tools and mostly requires change in thinking about preventability of a certain
NURS2006 Supplementary Assessment for Semester Two, 2018. 5
insufficient evidence some particular information technologies for inpatients maybe significant
(Roughead, Semple and Rosenfeld, 2016). The degree of benefit could be greater in paediatrics than
in adults’ medicine since there is need for dosing based on weight. In addition, evaluation,
dissemination and application of exact paediatrics’ computerised information is very important
(D’Andreamatteo et al. 2015). This is an example of system issue that can reduce medication error. It
can also be applied in reducing medication errors in outpatient setting and inpatients setting.
The system approach usually targets hitches in methods as opposed to blaming it on separate entity.
System error is made successful by introduction of checks to capture errors before they patient is
reached, which create a blameless culture, educating personnel, and system functions
simplification.
Change in Working Schedule (CWS). This intervention has not been so much focused on to solve
medical error but one study that involved an investigation of the effects of CWS shown comparisons
being done on medication error made by medical interns who worked in traditional schedule as
compared to those errors made when extensions of work shift were removed (Runciman, Merry and
Walton, 2017).
Interns who worked on extended shift traditional schedule made several medical errors compared to
their counterparts who worked in intervention group (Haines, 2018). This was the different interns
who worked in intervention group made 82.5 errors per 1000 patient-days compared with Interns
who worked on extended shift traditional schedule who made 99.7 errors per 1000 patient-days (P=
0.03) (Hayes et al., 2015). Increasing the interns working hours is the major challenge and in
reducing the medication errors in the ICU.
Recent studies have also indicated that within hospitals, of all trainees, interns (postgraduate year 1)
work in extended hours (Runciman, Merry and Walton, 2017). This has an effect of making them
prone to fatigue-induced errors. A survey of house officers proven that by 41 per cent of them
relating fatigue with their most serious mistakes (Mitchell et al. 2016). In simple and understandable
way, simple interventions may achieve impressive reductions in error rates (Haines, 2018). There is a
need to better categorize, replicate, and test study designs to maximize protection from biasness in
evidence of medical error reduction needs.
Barriers to implementation:
Magnitude and Complexity of the Change
INTERACT (Interventions to Reduce Acute Care Transfers) is not simple but a complex program that
employs multiple tools and mostly requires change in thinking about preventability of a certain
NURS2006 Supplementary Assessment for Semester Two, 2018. 5
hospital transfer proportion in NHs (Gibson et al., 2015). Full implementation would require an
extended effort to be effective. In one study reviewed, one respondent stated that, there is time
taken for cultural change (Schmidt, MacWilliams & Neal-Boylan, 2017). Since there are more
resources required to implement such major changes champions observe it could be a challenge
tackling other major initiatives like electronic health records at one time.
Competing Demands
What has been linked to make implementation difficult is the demand of additional major change
initiatives occurring at the same time. There were also two competing demands that were most
frequently mentioned which included implementation of an electronic health record and upcoming
state surveys (Schmidt, MacWilliams & Neal-Boylan, 2017). Implementation must be done on
priority to avoid demand overlap.
Resistance to Change
Resistance is said to come from many directions and several stakeholders. One of the respondent in
a reviewed study noted that, since champion is the one leading the change, unit manager are not
interested in the process (Fairbrother et al. 2016). Some medical providers lacked confidence in the
staff nurses’ evaluations of acute changes in condition and others continued to be concerned about
liability issues (Gibson et al., 2015). This barrier can be overcome by INTERACT SBAR tool. It was also
stated that some of the families still believed that NHs could provide only very limited levels of care
(Schmidt, MacWilliams & Neal-Boylan, 2017). This in turn fuelled their insistence on hospital transfer
if change never occurred in the residence.
Scarce Resources
This is the other barrier which was often cited as significant during implementation. INTERACT
training was necessitated by nursing staff turnover (Gibson et al., 2015). Workload for the champion
remained a concern also (Schmidt, MacWilliams & Neal-Boylan, 2017). One hinted that they were
doing the same job as the same time. Another complained of lack of not having a staff development
person which made it very challenging for them to get their regular work completed PLUS getting
necessary training (Fairbrother et al. 2016). Several respondents also mentioned increases in acutely
ill residents.
Technical Problems
An abundant range of technical barriers were mentioned. It was mentioned that it was difficult to
NURS2006 Supplementary Assessment for Semester Two, 2018. 6
extended effort to be effective. In one study reviewed, one respondent stated that, there is time
taken for cultural change (Schmidt, MacWilliams & Neal-Boylan, 2017). Since there are more
resources required to implement such major changes champions observe it could be a challenge
tackling other major initiatives like electronic health records at one time.
Competing Demands
What has been linked to make implementation difficult is the demand of additional major change
initiatives occurring at the same time. There were also two competing demands that were most
frequently mentioned which included implementation of an electronic health record and upcoming
state surveys (Schmidt, MacWilliams & Neal-Boylan, 2017). Implementation must be done on
priority to avoid demand overlap.
Resistance to Change
Resistance is said to come from many directions and several stakeholders. One of the respondent in
a reviewed study noted that, since champion is the one leading the change, unit manager are not
interested in the process (Fairbrother et al. 2016). Some medical providers lacked confidence in the
staff nurses’ evaluations of acute changes in condition and others continued to be concerned about
liability issues (Gibson et al., 2015). This barrier can be overcome by INTERACT SBAR tool. It was also
stated that some of the families still believed that NHs could provide only very limited levels of care
(Schmidt, MacWilliams & Neal-Boylan, 2017). This in turn fuelled their insistence on hospital transfer
if change never occurred in the residence.
Scarce Resources
This is the other barrier which was often cited as significant during implementation. INTERACT
training was necessitated by nursing staff turnover (Gibson et al., 2015). Workload for the champion
remained a concern also (Schmidt, MacWilliams & Neal-Boylan, 2017). One hinted that they were
doing the same job as the same time. Another complained of lack of not having a staff development
person which made it very challenging for them to get their regular work completed PLUS getting
necessary training (Fairbrother et al. 2016). Several respondents also mentioned increases in acutely
ill residents.
Technical Problems
An abundant range of technical barriers were mentioned. It was mentioned that it was difficult to
NURS2006 Supplementary Assessment for Semester Two, 2018. 6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
access online INTERACT training when computer resources were not enough or were not update
(Dekker, 2016). The use of own computers was rampant among many champions to complete their
online training. It was also difficult entering data into INTERACT online hospitalization rate tracker
among many champions even though they would eventually master it (Dekker, 2016).
Many champions can able to overcome barriers through technical assistance from members of the
research team (Dekker, 2016). There is mostly a double entry instances among when completing one
of the SBAR communication tool or core tools. This problem would be later resolved when INTERAC
was being integrated into their electronic health record.
The Continuous Professional Development points (CPD)
To sustain improvement, there should be training goals for new staff despite their turnover.
Putting in place methods that are transparent to audit and measure performance of the staff
(Mitchell et al. 2016).
There should be another visual management tool put in place that differentiates normal and
abnormal work (Mitchell et al. 2016).
There should be a clear definition of starting point for ongoing improvement (Mitchell et al.
2016).
Handling rejection
Rejection can be handled by doing the following: Involving all the stakeholders including
patients to clinical decision making and implementation as well as planning for sustainability
early so as to continue the work after the first enthusiasm has dissipated. Also visual
management or transparency must be considered so that every staff member can
differentiate between normal and unusual as first as possible among others.
Evaluation of the project:
This systematic review scrutinized the various effects of interventions that reduce medication errors
in acute care system (Castaneda, et al., 2015). Most of the studies included single-arm before and
after designs without any control group to do comparison.
Quality assessment results indicated some aspect were not well addressed, lack of statistical
consideration of the clustering effect involving patients experiencing the error, lack of blinding of the
NURS2006 Supplementary Assessment for Semester Two, 2018. 7
(Dekker, 2016). The use of own computers was rampant among many champions to complete their
online training. It was also difficult entering data into INTERACT online hospitalization rate tracker
among many champions even though they would eventually master it (Dekker, 2016).
Many champions can able to overcome barriers through technical assistance from members of the
research team (Dekker, 2016). There is mostly a double entry instances among when completing one
of the SBAR communication tool or core tools. This problem would be later resolved when INTERAC
was being integrated into their electronic health record.
The Continuous Professional Development points (CPD)
To sustain improvement, there should be training goals for new staff despite their turnover.
Putting in place methods that are transparent to audit and measure performance of the staff
(Mitchell et al. 2016).
There should be another visual management tool put in place that differentiates normal and
abnormal work (Mitchell et al. 2016).
There should be a clear definition of starting point for ongoing improvement (Mitchell et al.
2016).
Handling rejection
Rejection can be handled by doing the following: Involving all the stakeholders including
patients to clinical decision making and implementation as well as planning for sustainability
early so as to continue the work after the first enthusiasm has dissipated. Also visual
management or transparency must be considered so that every staff member can
differentiate between normal and unusual as first as possible among others.
Evaluation of the project:
This systematic review scrutinized the various effects of interventions that reduce medication errors
in acute care system (Castaneda, et al., 2015). Most of the studies included single-arm before and
after designs without any control group to do comparison.
Quality assessment results indicated some aspect were not well addressed, lack of statistical
consideration of the clustering effect involving patients experiencing the error, lack of blinding of the
NURS2006 Supplementary Assessment for Semester Two, 2018. 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
assessor, or lack of subgroup and adjusted statistical analyses and health professionals committing
the error (Castaneda, et al., 2015).
All of the interventions mentioned in this review demonstrate reduced medication errors in post-
intervention (Castaneda, et al., 2015). However, it is not possible to say these interventions are as
positive models for safety in patients care because the reviewed work does not present evidence
and quality of the research with a particular type.
References
Birks, M., Davis, J., Smithson, J. and Cant, R., 2016. Registered nurse scope of practice in Australia:
an integrative review of the literature. Contemporary Nurse, 52(5), pp.522-543.
Castaneda, C., Nalley, K., Mannion, C., Bhattacharyya, P., Blake, P., Pecora, A., Goy, A. and Suh,
K.S., 2015. Clinical decision support systems for improving diagnostic accuracy and achieving
precision medicine. Journal of clinical bioinformatics, 5(1), p.4.
D’Andreamatteo, A., Ianni, L., Lega, F. and Sargiacomo, M., 2015. Lean in healthcare: A
comprehensive review. Health policy, 119(9), pp.1197-1209.
Dekker, S., 2016. Just culture: Balancing safety and accountability. CRC Press.
Fairbrother, G., Cashin, A., Conway, M.R., Symes, M.A. and Graham, I., 2016. Evidence based
nursing and midwifery practice in a regional Australian healthcare setting: Behaviours, skills and
barriers. Collegian, 23(1), pp.29-37.
Gibson, O., Lisy, K., Davy, C., Aromataris, E., Kite, E., Lockwood, C., Riitano, D., McBride, K. and
Brown, A., 2015. Enablers and barriers to the implementation of primary health care interventions for
Indigenous people with chronic diseases: a systematic review. Implementation Science, 10(1), p.71.
Haines, S.T., 2018. It’s Time to Dismantle CE and Build a CPI System. American Journal of
Pharmaceutical Education, p.ajpe6985.
Hayes, C., Jackson, D., Davidson, P.M. and Power, T., 2015. Medication errors in hospitals: a
literature review of disruptions to nursing practice during medication administration. Journal of clinical
nursing, 24(21-22), pp.3063-3076.
Hunt, L., Frost, S.A., Newton, P.J., Salamonson, Y. and Davidson, P.M., 2017. A survey of critical
care nurses’ knowledge of intra-abdominal hypertension and abdominal compartment
NURS2006 Supplementary Assessment for Semester Two, 2018. 8
the error (Castaneda, et al., 2015).
All of the interventions mentioned in this review demonstrate reduced medication errors in post-
intervention (Castaneda, et al., 2015). However, it is not possible to say these interventions are as
positive models for safety in patients care because the reviewed work does not present evidence
and quality of the research with a particular type.
References
Birks, M., Davis, J., Smithson, J. and Cant, R., 2016. Registered nurse scope of practice in Australia:
an integrative review of the literature. Contemporary Nurse, 52(5), pp.522-543.
Castaneda, C., Nalley, K., Mannion, C., Bhattacharyya, P., Blake, P., Pecora, A., Goy, A. and Suh,
K.S., 2015. Clinical decision support systems for improving diagnostic accuracy and achieving
precision medicine. Journal of clinical bioinformatics, 5(1), p.4.
D’Andreamatteo, A., Ianni, L., Lega, F. and Sargiacomo, M., 2015. Lean in healthcare: A
comprehensive review. Health policy, 119(9), pp.1197-1209.
Dekker, S., 2016. Just culture: Balancing safety and accountability. CRC Press.
Fairbrother, G., Cashin, A., Conway, M.R., Symes, M.A. and Graham, I., 2016. Evidence based
nursing and midwifery practice in a regional Australian healthcare setting: Behaviours, skills and
barriers. Collegian, 23(1), pp.29-37.
Gibson, O., Lisy, K., Davy, C., Aromataris, E., Kite, E., Lockwood, C., Riitano, D., McBride, K. and
Brown, A., 2015. Enablers and barriers to the implementation of primary health care interventions for
Indigenous people with chronic diseases: a systematic review. Implementation Science, 10(1), p.71.
Haines, S.T., 2018. It’s Time to Dismantle CE and Build a CPI System. American Journal of
Pharmaceutical Education, p.ajpe6985.
Hayes, C., Jackson, D., Davidson, P.M. and Power, T., 2015. Medication errors in hospitals: a
literature review of disruptions to nursing practice during medication administration. Journal of clinical
nursing, 24(21-22), pp.3063-3076.
Hunt, L., Frost, S.A., Newton, P.J., Salamonson, Y. and Davidson, P.M., 2017. A survey of critical
care nurses’ knowledge of intra-abdominal hypertension and abdominal compartment
NURS2006 Supplementary Assessment for Semester Two, 2018. 8
syndrome. Australian Critical Care, 30(1), pp.21-27.
Jacob, E.R., McKenna, L. and D’Amore, A., 2017. Role expectations of different levels of nurse on
graduation: A mixed methods approach. Collegian, 24(2), pp.135-145.
Mitchell, I., Schuster, A., Smith, K., Pronovost, P. and Wu, A., 2016. Patient safety incident reporting:
a qualitative study of thoughts and perceptions of experts 15 years after ‘To Err is Human’. BMJ Qual
Saf, 25(2), pp.92-99.
Purvis, T., Moss, K., Francis, L., Borschmann, K., Kilkenny, M.F., Denisenko, S., Bladin, C.F. and
Cadilhac, D.A., 2017. Benefits of clinical facilitators on improving stroke care in acute hospitals: a new
programme for Australia. Internal medicine journal, 47(7), pp.775-784.
Runciman, B., Merry, A. and Walton, M., 2017. Safety and ethics in healthcare: a guide to getting it
right. CRC Press.
Roughead, E.E., Semple, S.J. and Rosenfeld, E., 2016. The extent of medication errors and adverse
drug reactions throughout the patient journey in acute care in Australia. International journal of
evidence-based healthcare, 14(3-4), pp.113-122.
Scanlon, A., Cashin, A., Bryce, J., Kelly, J.G. and Buckely, T., 2016. The complexities of defining
nurse practitioner scope of practice in the Australian context. Collegian, 23(1), pp.129-142.
Schmidt, B.J., MacWilliams, B.R. and Neal-Boylan, L., 2017. Becoming inclusive: a code of conduct
for inclusion and diversity. Journal of Professional Nursing, 33(2), pp.102-107.
Stavropoulou, C., Doherty, C. and Tosey, P., 2015. How effective are incident‐reporting systems for
improving patient safety? a systematic literature review. The Milbank Quarterly, 93(4), pp.826-866.
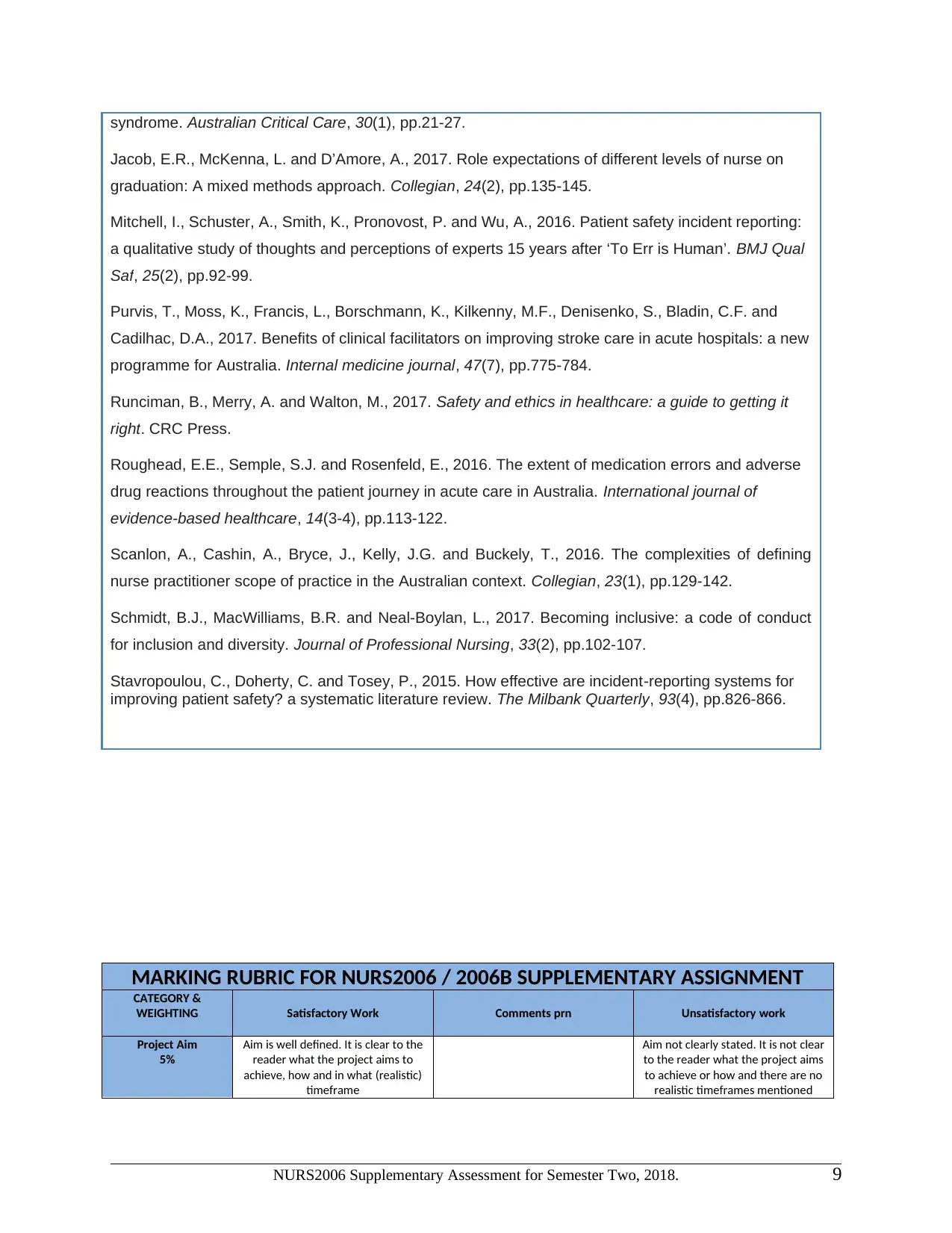
MARKING RUBRIC FOR NURS2006 / 2006B SUPPLEMENTARY ASSIGNMENT
CATEGORY &
WEIGHTING Satisfactory Work Comments prn Unsatisfactory work
Project Aim
5%
Aim is well defined. It is clear to the
reader what the project aims to
achieve, how and in what (realistic)
timeframe
Aim not clearly stated. It is not clear
to the reader what the project aims
to achieve or how and there are no
realistic timeframes mentioned
NURS2006 Supplementary Assessment for Semester Two, 2018. 9
Jacob, E.R., McKenna, L. and D’Amore, A., 2017. Role expectations of different levels of nurse on
graduation: A mixed methods approach. Collegian, 24(2), pp.135-145.
Mitchell, I., Schuster, A., Smith, K., Pronovost, P. and Wu, A., 2016. Patient safety incident reporting:
a qualitative study of thoughts and perceptions of experts 15 years after ‘To Err is Human’. BMJ Qual
Saf, 25(2), pp.92-99.
Purvis, T., Moss, K., Francis, L., Borschmann, K., Kilkenny, M.F., Denisenko, S., Bladin, C.F. and
Cadilhac, D.A., 2017. Benefits of clinical facilitators on improving stroke care in acute hospitals: a new
programme for Australia. Internal medicine journal, 47(7), pp.775-784.
Runciman, B., Merry, A. and Walton, M., 2017. Safety and ethics in healthcare: a guide to getting it
right. CRC Press.
Roughead, E.E., Semple, S.J. and Rosenfeld, E., 2016. The extent of medication errors and adverse
drug reactions throughout the patient journey in acute care in Australia. International journal of
evidence-based healthcare, 14(3-4), pp.113-122.
Scanlon, A., Cashin, A., Bryce, J., Kelly, J.G. and Buckely, T., 2016. The complexities of defining
nurse practitioner scope of practice in the Australian context. Collegian, 23(1), pp.129-142.
Schmidt, B.J., MacWilliams, B.R. and Neal-Boylan, L., 2017. Becoming inclusive: a code of conduct
for inclusion and diversity. Journal of Professional Nursing, 33(2), pp.102-107.
Stavropoulou, C., Doherty, C. and Tosey, P., 2015. How effective are incident‐reporting systems for
improving patient safety? a systematic literature review. The Milbank Quarterly, 93(4), pp.826-866.
MARKING RUBRIC FOR NURS2006 / 2006B SUPPLEMENTARY ASSIGNMENT
CATEGORY &
WEIGHTING Satisfactory Work Comments prn Unsatisfactory work
Project Aim
5%
Aim is well defined. It is clear to the
reader what the project aims to
achieve, how and in what (realistic)
timeframe
Aim not clearly stated. It is not clear
to the reader what the project aims
to achieve or how and there are no
realistic timeframes mentioned
NURS2006 Supplementary Assessment for Semester Two, 2018. 9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
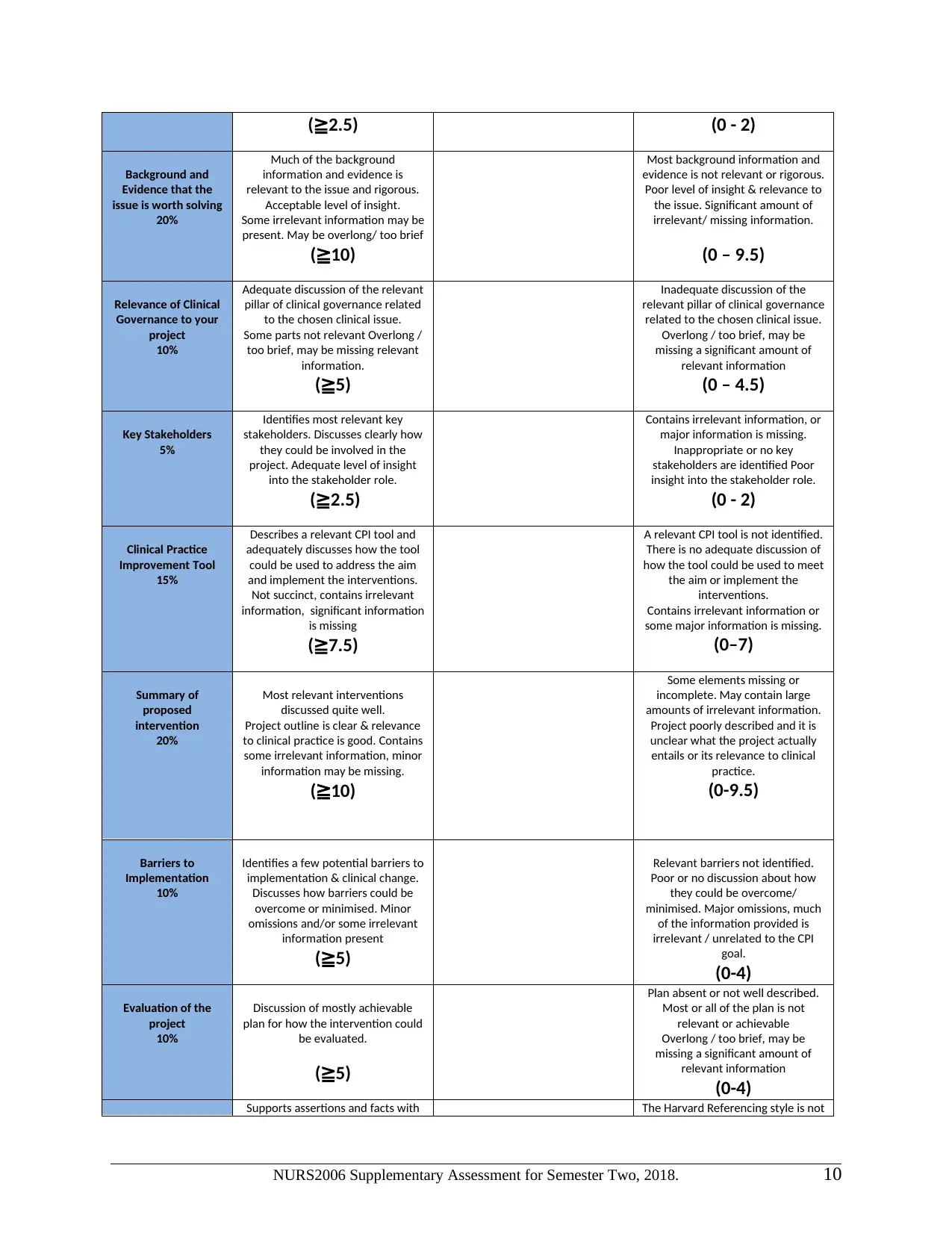
(≧2.5) (0 - 2)
Background and
Evidence that the
issue is worth solving
20%
Much of the background
information and evidence is
relevant to the issue and rigorous.
Acceptable level of insight.
Some irrelevant information may be
present. May be overlong/ too brief
(≧10)
Most background information and
evidence is not relevant or rigorous.
Poor level of insight & relevance to
the issue. Significant amount of
irrelevant/ missing information.
(0 – 9.5)
Relevance of Clinical
Governance to your
project
10%
Adequate discussion of the relevant
pillar of clinical governance related
to the chosen clinical issue.
Some parts not relevant Overlong /
too brief, may be missing relevant
information.
(≧5)
Inadequate discussion of the
relevant pillar of clinical governance
related to the chosen clinical issue.
Overlong / too brief, may be
missing a significant amount of
relevant information
(0 – 4.5)
Key Stakeholders
5%
Identifies most relevant key
stakeholders. Discusses clearly how
they could be involved in the
project. Adequate level of insight
into the stakeholder role.
(≧2.5)
Contains irrelevant information, or
major information is missing.
Inappropriate or no key
stakeholders are identified Poor
insight into the stakeholder role.
(0 - 2)
Clinical Practice
Improvement Tool
15%
Describes a relevant CPI tool and
adequately discusses how the tool
could be used to address the aim
and implement the interventions.
Not succinct, contains irrelevant
information, significant information
is missing
(≧7.5)
A relevant CPI tool is not identified.
There is no adequate discussion of
how the tool could be used to meet
the aim or implement the
interventions.
Contains irrelevant information or
some major information is missing.
(0–7)
Summary of
proposed
intervention
20%
Most relevant interventions
discussed quite well.
Project outline is clear & relevance
to clinical practice is good. Contains
some irrelevant information, minor
information may be missing.
(≧10)
Some elements missing or
incomplete. May contain large
amounts of irrelevant information.
Project poorly described and it is
unclear what the project actually
entails or its relevance to clinical
practice.
(0-9.5)
Barriers to
Implementation
10%
Identifies a few potential barriers to
implementation & clinical change.
Discusses how barriers could be
overcome or minimised. Minor
omissions and/or some irrelevant
information present
(≧5)
Relevant barriers not identified.
Poor or no discussion about how
they could be overcome/
minimised. Major omissions, much
of the information provided is
irrelevant / unrelated to the CPI
goal.
(0-4)
Evaluation of the
project
10%
Discussion of mostly achievable
plan for how the intervention could
be evaluated.
(≧5)
Plan absent or not well described.
Most or all of the plan is not
relevant or achievable
Overlong / too brief, may be
missing a significant amount of
relevant information
(0-4)
Supports assertions and facts with The Harvard Referencing style is not
NURS2006 Supplementary Assessment for Semester Two, 2018. 10
Background and
Evidence that the
issue is worth solving
20%
Much of the background
information and evidence is
relevant to the issue and rigorous.
Acceptable level of insight.
Some irrelevant information may be
present. May be overlong/ too brief
(≧10)
Most background information and
evidence is not relevant or rigorous.
Poor level of insight & relevance to
the issue. Significant amount of
irrelevant/ missing information.
(0 – 9.5)
Relevance of Clinical
Governance to your
project
10%
Adequate discussion of the relevant
pillar of clinical governance related
to the chosen clinical issue.
Some parts not relevant Overlong /
too brief, may be missing relevant
information.
(≧5)
Inadequate discussion of the
relevant pillar of clinical governance
related to the chosen clinical issue.
Overlong / too brief, may be
missing a significant amount of
relevant information
(0 – 4.5)
Key Stakeholders
5%
Identifies most relevant key
stakeholders. Discusses clearly how
they could be involved in the
project. Adequate level of insight
into the stakeholder role.
(≧2.5)
Contains irrelevant information, or
major information is missing.
Inappropriate or no key
stakeholders are identified Poor
insight into the stakeholder role.
(0 - 2)
Clinical Practice
Improvement Tool
15%
Describes a relevant CPI tool and
adequately discusses how the tool
could be used to address the aim
and implement the interventions.
Not succinct, contains irrelevant
information, significant information
is missing
(≧7.5)
A relevant CPI tool is not identified.
There is no adequate discussion of
how the tool could be used to meet
the aim or implement the
interventions.
Contains irrelevant information or
some major information is missing.
(0–7)
Summary of
proposed
intervention
20%
Most relevant interventions
discussed quite well.
Project outline is clear & relevance
to clinical practice is good. Contains
some irrelevant information, minor
information may be missing.
(≧10)
Some elements missing or
incomplete. May contain large
amounts of irrelevant information.
Project poorly described and it is
unclear what the project actually
entails or its relevance to clinical
practice.
(0-9.5)
Barriers to
Implementation
10%
Identifies a few potential barriers to
implementation & clinical change.
Discusses how barriers could be
overcome or minimised. Minor
omissions and/or some irrelevant
information present
(≧5)
Relevant barriers not identified.
Poor or no discussion about how
they could be overcome/
minimised. Major omissions, much
of the information provided is
irrelevant / unrelated to the CPI
goal.
(0-4)
Evaluation of the
project
10%
Discussion of mostly achievable
plan for how the intervention could
be evaluated.
(≧5)
Plan absent or not well described.
Most or all of the plan is not
relevant or achievable
Overlong / too brief, may be
missing a significant amount of
relevant information
(0-4)
Supports assertions and facts with The Harvard Referencing style is not
NURS2006 Supplementary Assessment for Semester Two, 2018. 10
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
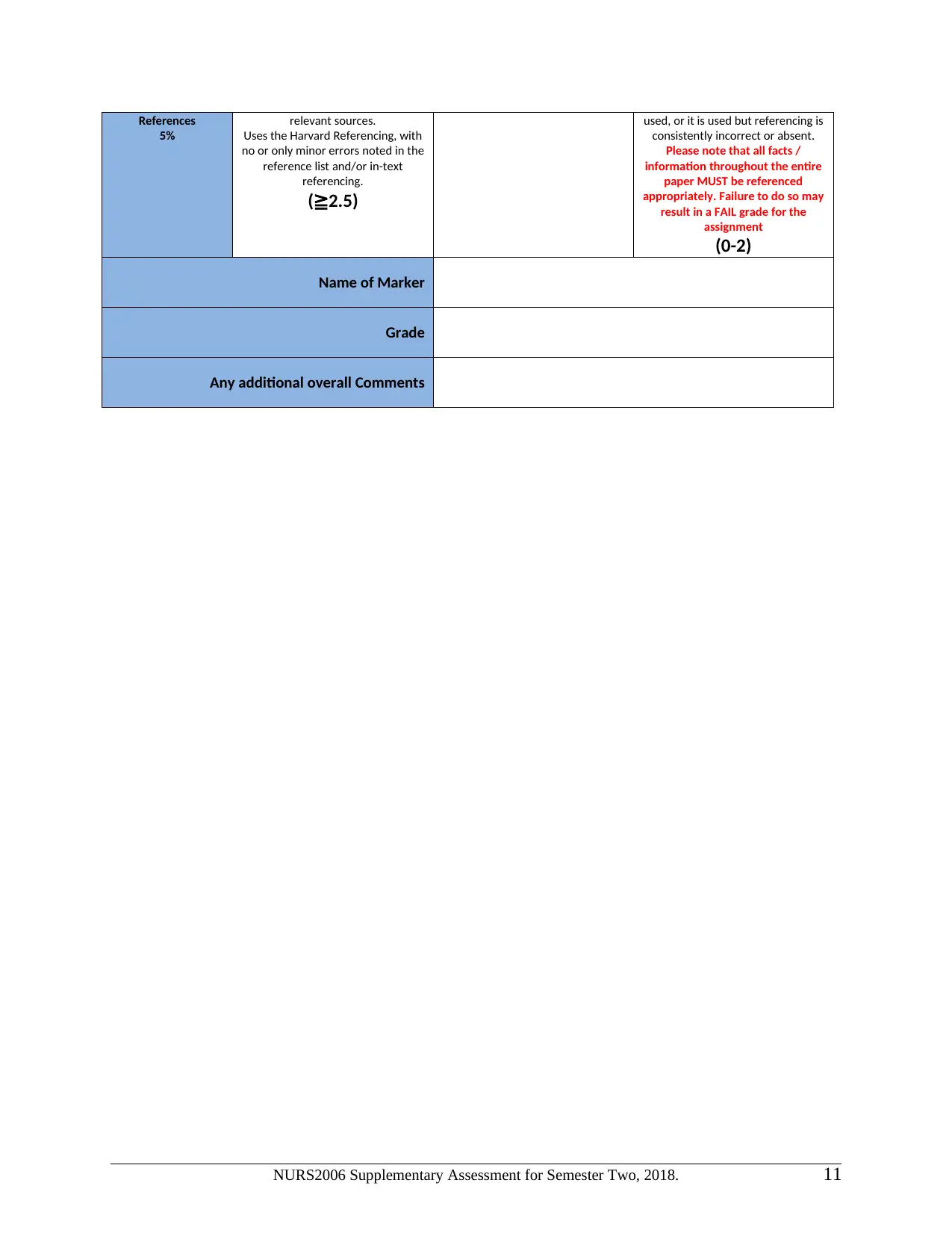
References
5%
relevant sources.
Uses the Harvard Referencing, with
no or only minor errors noted in the
reference list and/or in-text
referencing.
(≧2.5)
used, or it is used but referencing is
consistently incorrect or absent.
Please note that all facts /
information throughout the entire
paper MUST be referenced
appropriately. Failure to do so may
result in a FAIL grade for the
assignment
(0-2)
Name of Marker
Grade
Any additional overall Comments
NURS2006 Supplementary Assessment for Semester Two, 2018. 11
5%
relevant sources.
Uses the Harvard Referencing, with
no or only minor errors noted in the
reference list and/or in-text
referencing.
(≧2.5)
used, or it is used but referencing is
consistently incorrect or absent.
Please note that all facts /
information throughout the entire
paper MUST be referenced
appropriately. Failure to do so may
result in a FAIL grade for the
assignment
(0-2)
Name of Marker
Grade
Any additional overall Comments
NURS2006 Supplementary Assessment for Semester Two, 2018. 11
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





