Reduction of Fall Rates Among Elderly Population in Hospital Ward
VerifiedAdded on 2023/06/15
|11
|4768
|233
AI Summary
The aim of the project is to bring about 30% reduction in fall rates among the elderly population in a hospital ward within a six-month time frame by implementing exercise. The project is relevant to clinical governance as it involves risk assessment and management. The proposed intervention includes organizing exercise programs for the patients of the hospital ward and educating the nurses about the importance of physical therapies to reduce the fall risks among the elderly. The barriers to implementation include normalization of falls, denial, and lack of necessary resources and facilities.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
NURS2006 ASSIGNMENT 3
Clinical Practice Improvement Project Report
Student Name, FAN and ID:
Type your assignment into the white spaces in the template and the rows will
expand as much as you need them to.ie Alex Smith smit0000 ID 1234567
Project Title:
Reduction of fall rates among the elderly population in a hospital ward.
Project Aim:
The aim of the project is to bring about 30% reduction in fall rates among the elderly population in
a hospital ward within a six-month time frame by implementing exercise.
Falls are the most common causes of morbidity, mortality and disability among the elderly. Falls in
the elderly are a major concern and approximately 30% of falls occur each year (Milisen et al.
2013, pp. 495-507). Postural stability depends on the ability to coordinate the sensory and motor
nerves, which in turn helps to perceive the environment and respond accordingly by controlling
the movement of the body. Cognitive impairment has been identified as a risk factor associated
with falls among the elderly, however, other diseases like dementia, depression and Parkinson’s
disease have also been associated with falls among the elderly (Montero Odasso‐ et al. 2012, pp.
2127-2136). Subtle changes in cognition like executive function has also been associated with falls
among the elderly. Recent research has revealed the importance of impairment of executive
function is association with falls among the elderly people in hospitals. Assessments of executive
function in the elderly needs to be carried out and should be a apart of the fall risk assessment
carried out in the hospitals (Snyder 2013). There are various consequences associated with falls in
the elderly. Injuries associated with falls in the elderly involve fractures of the hip, broken bones
and broken hips, soft tissue injury, damages to the head, among others. These injuries in turn can
give rise to serious consequences. Falls among the elderly results in loss of independence and
many of the elderly population have to permanently reside in long-term care facilities. The risks
associated with falls prevent them to carry out physical activities or any other daily activities,
thereby restricting their movements. They feel isolated and this isolation can give rise to various
mental disorders like anxiety, depression, among others. They become dependent on others to
carry out their daily activities. The individuals who suffer falls have increased chances of
succumbing to falls again (Muir, Gopaul and Montero Odasso 2012, pp. 299-308; Winter, Watt and
Clinical Practice Improvement Project Report
Student Name, FAN and ID:
Type your assignment into the white spaces in the template and the rows will
expand as much as you need them to.ie Alex Smith smit0000 ID 1234567
Project Title:
Reduction of fall rates among the elderly population in a hospital ward.
Project Aim:
The aim of the project is to bring about 30% reduction in fall rates among the elderly population in
a hospital ward within a six-month time frame by implementing exercise.
Falls are the most common causes of morbidity, mortality and disability among the elderly. Falls in
the elderly are a major concern and approximately 30% of falls occur each year (Milisen et al.
2013, pp. 495-507). Postural stability depends on the ability to coordinate the sensory and motor
nerves, which in turn helps to perceive the environment and respond accordingly by controlling
the movement of the body. Cognitive impairment has been identified as a risk factor associated
with falls among the elderly, however, other diseases like dementia, depression and Parkinson’s
disease have also been associated with falls among the elderly (Montero Odasso‐ et al. 2012, pp.
2127-2136). Subtle changes in cognition like executive function has also been associated with falls
among the elderly. Recent research has revealed the importance of impairment of executive
function is association with falls among the elderly people in hospitals. Assessments of executive
function in the elderly needs to be carried out and should be a apart of the fall risk assessment
carried out in the hospitals (Snyder 2013). There are various consequences associated with falls in
the elderly. Injuries associated with falls in the elderly involve fractures of the hip, broken bones
and broken hips, soft tissue injury, damages to the head, among others. These injuries in turn can
give rise to serious consequences. Falls among the elderly results in loss of independence and
many of the elderly population have to permanently reside in long-term care facilities. The risks
associated with falls prevent them to carry out physical activities or any other daily activities,
thereby restricting their movements. They feel isolated and this isolation can give rise to various
mental disorders like anxiety, depression, among others. They become dependent on others to
carry out their daily activities. The individuals who suffer falls have increased chances of
succumbing to falls again (Muir, Gopaul and Montero Odasso 2012, pp. 299-308; Winter, Watt and
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Peel 2013, pp. 215-227). Exercises have been shown to be beneficial as it helps to attain balance
and build physical stability and strength, which is highly essential for such elderly population to
lead a healthy life. According to Sherrington and Tiedemann (2015), various multi-component
group based exrcises, gait and balance or functional training exercises have been shown to reduce
falls among the elderly. Therefore, the aim is to increase the balance and physical strength among
the elders by carrying out different strength building exercises.
Relevance of Clinical Governance to your project
Clinical Governance is a framework, which is used by the National Health Service Organizations,
who are responsible for carrying out continuous improvements in quality of service and providing
high quality care by providing an environment that encourages development of excellence in
clinical care (Brennan and Flynn 2013, pp. 114-131). The seven pillars of clinical governance are
clinical effectiveness and research, risk management, audit, education and training, involvement
of patient and public, usage of information technology and staff management. The most relevant
pillar is the pillar that deals with risk assessment and management. The nurses are required to
assess the risk factors, critically analyse them and determine the probability of occurrence of any
event that can cause harm to the patients. Moreover, they also need to implement approaches to
reduce the risks and the impacts associated with such risks. The pillar of Clinical Governance that
defines the identification of risk factors can be linked to this project as the nurses have to assess
the risk factors associated with the falls of the elderly patients and provide necessary evidence
based intervention strategies to reduce such fall rates in the hospital ward (Heyrani et al. 2012,
pp. 84). Exercise programs will enable the elderly population to regain their balance and strength
and in turn lead an active and independent life.
Evidence that the issue / problem is worth solving:
This issue is worth addressing, as exercises are known to reduce falls in the elderly. Exercises help
to maintain balance and in turn provide strength and physical stability. Exercise can also improve
heart functions and also help in maintaining good mental health, which in turn contributes to
healthy and safe living (Blake and Hawley 2012, pp. 19-27).
In 2015 and 2016, falls were the most reported incidents in acute and community care hospitals
and was the third most reported incidents in mental healthcare hospitals. About 250000 fall cases
were reported in hospital settings. Falls among the hospital patients usually range between 2.3 to
7 falls per 1000 patients. The fall associated injuries include fractures, bleeding, subdural
hematomas and death. Injuries associated with falls also increase the healthcare costs. A recent
research revealed that during the research duration, the researchers observed 315817 falls, of
and build physical stability and strength, which is highly essential for such elderly population to
lead a healthy life. According to Sherrington and Tiedemann (2015), various multi-component
group based exrcises, gait and balance or functional training exercises have been shown to reduce
falls among the elderly. Therefore, the aim is to increase the balance and physical strength among
the elders by carrying out different strength building exercises.
Relevance of Clinical Governance to your project
Clinical Governance is a framework, which is used by the National Health Service Organizations,
who are responsible for carrying out continuous improvements in quality of service and providing
high quality care by providing an environment that encourages development of excellence in
clinical care (Brennan and Flynn 2013, pp. 114-131). The seven pillars of clinical governance are
clinical effectiveness and research, risk management, audit, education and training, involvement
of patient and public, usage of information technology and staff management. The most relevant
pillar is the pillar that deals with risk assessment and management. The nurses are required to
assess the risk factors, critically analyse them and determine the probability of occurrence of any
event that can cause harm to the patients. Moreover, they also need to implement approaches to
reduce the risks and the impacts associated with such risks. The pillar of Clinical Governance that
defines the identification of risk factors can be linked to this project as the nurses have to assess
the risk factors associated with the falls of the elderly patients and provide necessary evidence
based intervention strategies to reduce such fall rates in the hospital ward (Heyrani et al. 2012,
pp. 84). Exercise programs will enable the elderly population to regain their balance and strength
and in turn lead an active and independent life.
Evidence that the issue / problem is worth solving:
This issue is worth addressing, as exercises are known to reduce falls in the elderly. Exercises help
to maintain balance and in turn provide strength and physical stability. Exercise can also improve
heart functions and also help in maintaining good mental health, which in turn contributes to
healthy and safe living (Blake and Hawley 2012, pp. 19-27).
In 2015 and 2016, falls were the most reported incidents in acute and community care hospitals
and was the third most reported incidents in mental healthcare hospitals. About 250000 fall cases
were reported in hospital settings. Falls among the hospital patients usually range between 2.3 to
7 falls per 1000 patients. The fall associated injuries include fractures, bleeding, subdural
hematomas and death. Injuries associated with falls also increase the healthcare costs. A recent
research revealed that during the research duration, the researchers observed 315817 falls, of
which 26.1% gave rise to injuries. Patients above 80 years of age are more prone to succumb to
falls, however patients of 65 years of age and below have also been found to succumb to falls.
Falls are the leading causes of accidental death among the elderly population (Bouldin et al. 2013,
pp. 13). The fall related injuries in Australia are reported to be over 60 in the year 2013. Studies
have shown that exercises can decrease the rate of falls among the elderly and balance is
considered to be an essential element of physical activity programmes (Tiedemann, Sherrington
and Lord 2013, pp. 541-547).
Key Stakeholders:
The key stakeholders of the project could be the nurses or the care givers and the patients
themselves. The nurses or the care givers can participate in the project by carrying out
assessments of the risk factors of the patients that can give rise to the falls, analysis of the data
and providing necessary intervention strategies in order to reduce the risk of falls among the
elderly population. The nurses can educate the patients about the importance of exercises. The
nurse can obtain feedback from the patients about the quality of care and develop or bring about
improvements in their strategies in order to enhance patient satisfaction by giving rise to
favourable outcomes. Other stakeholders may include the doctors and physiotherapists, help in
designing the exercise program and determine the health issues during and after the exercise
program.
CPI Tool:
Clinical Practice Improvement or CPI is a method for carrying out improvements and thereby
providing high quality care. Clinical Practice Improvement ensures the quality, safety and
efficiency of the provided care, enables accountability for the care either individually or as a group
and brings about continuous improvements in the already established procedures. Clinical Practice
Improvement provides a framework, which can be used by the healthcare professionals to carry
out assessments regarding the causes associated with process failures, which in turn can cause
harm to patients and bringing about solutions in order to carry out continuous improvements in
care and patient outcomes (Rosenfeld, Shiffman and Robertson 2013, pp. S1-S55). The clinical
practice improvement tool applied in the project will be the Plan Do Study Act. Plan Do Study Act
or PDSA cycle involves undertaking small tests in order to bring about improvements. The PDSA
cycle can be used to test a change by designing a plan, then carrying out the plan and
subsequently observing and understanding the consequences of the plan. The PDSA cycle also
involves determining the modifications that can be brought about in the plan to further improve
it. The PDSA is an essential component of improvement practices in the healthcare settings. The
falls, however patients of 65 years of age and below have also been found to succumb to falls.
Falls are the leading causes of accidental death among the elderly population (Bouldin et al. 2013,
pp. 13). The fall related injuries in Australia are reported to be over 60 in the year 2013. Studies
have shown that exercises can decrease the rate of falls among the elderly and balance is
considered to be an essential element of physical activity programmes (Tiedemann, Sherrington
and Lord 2013, pp. 541-547).
Key Stakeholders:
The key stakeholders of the project could be the nurses or the care givers and the patients
themselves. The nurses or the care givers can participate in the project by carrying out
assessments of the risk factors of the patients that can give rise to the falls, analysis of the data
and providing necessary intervention strategies in order to reduce the risk of falls among the
elderly population. The nurses can educate the patients about the importance of exercises. The
nurse can obtain feedback from the patients about the quality of care and develop or bring about
improvements in their strategies in order to enhance patient satisfaction by giving rise to
favourable outcomes. Other stakeholders may include the doctors and physiotherapists, help in
designing the exercise program and determine the health issues during and after the exercise
program.
CPI Tool:
Clinical Practice Improvement or CPI is a method for carrying out improvements and thereby
providing high quality care. Clinical Practice Improvement ensures the quality, safety and
efficiency of the provided care, enables accountability for the care either individually or as a group
and brings about continuous improvements in the already established procedures. Clinical Practice
Improvement provides a framework, which can be used by the healthcare professionals to carry
out assessments regarding the causes associated with process failures, which in turn can cause
harm to patients and bringing about solutions in order to carry out continuous improvements in
care and patient outcomes (Rosenfeld, Shiffman and Robertson 2013, pp. S1-S55). The clinical
practice improvement tool applied in the project will be the Plan Do Study Act. Plan Do Study Act
or PDSA cycle involves undertaking small tests in order to bring about improvements. The PDSA
cycle can be used to test a change by designing a plan, then carrying out the plan and
subsequently observing and understanding the consequences of the plan. The PDSA cycle also
involves determining the modifications that can be brought about in the plan to further improve
it. The PDSA is an essential component of improvement practices in the healthcare settings. The
stages of the PDSA cycle involves critical analysis of data that highlights poor performance,
identifying the necessary causes associated with the poor performances, implementing small
changes and monitoring the impact of the changes. Those changes that bring about positive
outcomes are defined and established in order to be followed by all. The use of clinical practice
improvement tools is a fundamental part of clinical governance. The benefits of PDSA involves
establishment of new processes, involves the use of learning to bring about improvements, helps
to reduce the costs of resources, provides scope for continuous development and improvement,
helps to solve the problems associated with a large amount of data, increase process
understanding, bring about improvements in outcomes and enhance teamwork. It can also
provide customer or patient satisfaction and provide motivation to staff (Knudsen et al. 2017, pp.
45). In this project the PDSA tool can be used by the nurses to critically analyse the risk factors
associated with patient falls, identifying the causes, planning an exercise or physical therapy
program, implement the exercise programs, monitoring the success associated with the exercise
program and subsequently establishing the exercise programs in the daily routine of the elderly in
the hospital ward (Taylor et al. 2013, pp.bmjqs-2013). The small-scale strategies employed by the
nurses can be the strength and balance building exercises that they can implement in order to help
the elderly lead a health life.
Summary of proposed interventions:
The elderly patients with cognitive impairment suffer from falls on a regular basis and this is as a
result of impairment in their motor functions preventing them to properly analyse the
environment and carry out necessary changes in the body movements. This in turn affects their
balance, stability and gait (Morse, Merry and Bloswick 2016, pp. 341).
The first phase of the plan will involve the designing of the project and the necessary resources
and the finances involved with it will be provided to the necessary finance department and the
Director of the hospital, where the elderly succumb to such falls. Funds will be requested in order
to carry out the project.
Exercise programs will be organized for the patients of the hospital ward and conducted under the
supervision of physiotherapists. Exercises has been shown to reduce the risk factors associated
with falls such as impaired balance and or mobility. Exercise programs that are aimed to bring
about improvements in balance, strength and gait have been shown to reduce the occurrence of
falls among the elderly (Cameron et al. 2012, pp. 1-121; Gillespie et al. 2012, pp. 1-299). It is
necessary to educate the nurses about the importance of these approaches or intervention
strategies. The exercise program will be carried out for six months under the supervision of the
identifying the necessary causes associated with the poor performances, implementing small
changes and monitoring the impact of the changes. Those changes that bring about positive
outcomes are defined and established in order to be followed by all. The use of clinical practice
improvement tools is a fundamental part of clinical governance. The benefits of PDSA involves
establishment of new processes, involves the use of learning to bring about improvements, helps
to reduce the costs of resources, provides scope for continuous development and improvement,
helps to solve the problems associated with a large amount of data, increase process
understanding, bring about improvements in outcomes and enhance teamwork. It can also
provide customer or patient satisfaction and provide motivation to staff (Knudsen et al. 2017, pp.
45). In this project the PDSA tool can be used by the nurses to critically analyse the risk factors
associated with patient falls, identifying the causes, planning an exercise or physical therapy
program, implement the exercise programs, monitoring the success associated with the exercise
program and subsequently establishing the exercise programs in the daily routine of the elderly in
the hospital ward (Taylor et al. 2013, pp.bmjqs-2013). The small-scale strategies employed by the
nurses can be the strength and balance building exercises that they can implement in order to help
the elderly lead a health life.
Summary of proposed interventions:
The elderly patients with cognitive impairment suffer from falls on a regular basis and this is as a
result of impairment in their motor functions preventing them to properly analyse the
environment and carry out necessary changes in the body movements. This in turn affects their
balance, stability and gait (Morse, Merry and Bloswick 2016, pp. 341).
The first phase of the plan will involve the designing of the project and the necessary resources
and the finances involved with it will be provided to the necessary finance department and the
Director of the hospital, where the elderly succumb to such falls. Funds will be requested in order
to carry out the project.
Exercise programs will be organized for the patients of the hospital ward and conducted under the
supervision of physiotherapists. Exercises has been shown to reduce the risk factors associated
with falls such as impaired balance and or mobility. Exercise programs that are aimed to bring
about improvements in balance, strength and gait have been shown to reduce the occurrence of
falls among the elderly (Cameron et al. 2012, pp. 1-121; Gillespie et al. 2012, pp. 1-299). It is
necessary to educate the nurses about the importance of these approaches or intervention
strategies. The exercise program will be carried out for six months under the supervision of the
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
physiotherapists. The exercise program will be carried out 4 days a week for 1 hour and will
include various strength and balance building exercise apart from free hand exercises as well. The
improvements of the elderly people before and after the exercise programs will be monitored and
such exercises once proven to be effective will be included in the daily activities of the elderly in
order to reduce their fall rates and succumbing to injuries. The project can include an education
package for the nurses and the care givers, where information will be provided about the
importance of physical therapies to reduce the fall risks among the elderly. Moreover, the nurses
can also be given appropriate training to carry out these exercises effectively. Such education
packages can be developed by physiotherapists, fall management experts and senior doctors. The
nurses can be trained by the physiotherapists in order to carry out physical therapy programs. The
nurses should be encouraged to carry out frequent rounds of the patients and monitor their
improvements. After the training necessary feedback can be obtained from the patients about the
effectiveness of the training program. The nurses can monitor the patients by collecting their
feedbacks, analysing the data obtained and provide the necessary patient specific care.
Barriers to implementation and sustaining change:
The various barriers to implementation of strategies to reduce the risks of falls among elderly
people include normalization of falls. The elderly people perceive falls as normal according to their
age and disregard such falls. There are various stigmas associated with falls among the elderly
people. These include the fear of reporting the occurrences of falls as they believe that it will
result in them being permanently transferred to long term care facilities. The older individuals
believe that implementation of various interventions like exercises cannot prevent the occurrence
of falls. They are fatalistic as they believe that nothing can improve their health and their ultimate
fate is death. Another barrier is denial, where the elderly people refuse to understand that the
cause of their falls is muscle weakness and loss of balance and strength (Biedenweg et al. 2014,
pp. 1-11). The barriers associated with healthcare professionals include trivialization of falls,
where they do not attach much importance to the occurrences of such falls and do not determine
the causes of such falls. Many healthcare professionals lack the necessary skills and knowledge in
management of falls among the elderly. Some healthcare professionals do not understand the
value of exercising in preventing falls and are unaware of the effectiveness of exercises and
physical therapy programs. Some of the healthcare professionals do not work in groups and do not
have the relevant information needed to prevent the fatal injuries associated with falls. They do
not discuss and obtain advice from other healthcare professionals involved in the management of
falls. Thus, they do not carry out interdisciplinary approaches in order to provide patient specific
care. Thus, the patients are not referred to physiotherapists, occupational therapists and
include various strength and balance building exercise apart from free hand exercises as well. The
improvements of the elderly people before and after the exercise programs will be monitored and
such exercises once proven to be effective will be included in the daily activities of the elderly in
order to reduce their fall rates and succumbing to injuries. The project can include an education
package for the nurses and the care givers, where information will be provided about the
importance of physical therapies to reduce the fall risks among the elderly. Moreover, the nurses
can also be given appropriate training to carry out these exercises effectively. Such education
packages can be developed by physiotherapists, fall management experts and senior doctors. The
nurses can be trained by the physiotherapists in order to carry out physical therapy programs. The
nurses should be encouraged to carry out frequent rounds of the patients and monitor their
improvements. After the training necessary feedback can be obtained from the patients about the
effectiveness of the training program. The nurses can monitor the patients by collecting their
feedbacks, analysing the data obtained and provide the necessary patient specific care.
Barriers to implementation and sustaining change:
The various barriers to implementation of strategies to reduce the risks of falls among elderly
people include normalization of falls. The elderly people perceive falls as normal according to their
age and disregard such falls. There are various stigmas associated with falls among the elderly
people. These include the fear of reporting the occurrences of falls as they believe that it will
result in them being permanently transferred to long term care facilities. The older individuals
believe that implementation of various interventions like exercises cannot prevent the occurrence
of falls. They are fatalistic as they believe that nothing can improve their health and their ultimate
fate is death. Another barrier is denial, where the elderly people refuse to understand that the
cause of their falls is muscle weakness and loss of balance and strength (Biedenweg et al. 2014,
pp. 1-11). The barriers associated with healthcare professionals include trivialization of falls,
where they do not attach much importance to the occurrences of such falls and do not determine
the causes of such falls. Many healthcare professionals lack the necessary skills and knowledge in
management of falls among the elderly. Some healthcare professionals do not understand the
value of exercising in preventing falls and are unaware of the effectiveness of exercises and
physical therapy programs. Some of the healthcare professionals do not work in groups and do not
have the relevant information needed to prevent the fatal injuries associated with falls. They do
not discuss and obtain advice from other healthcare professionals involved in the management of
falls. Thus, they do not carry out interdisciplinary approaches in order to provide patient specific
care. Thus, the patients are not referred to physiotherapists, occupational therapists and

pharmacists in order to obtain favourable outcomes. Other barriers to implementation include
inability to acquire the necessary resources and facilities in order to provide necessary care to
elderly patients. Lack of equipments, facilities, staff and experts can also act as potential barriers
to implementation (Loganathan et al. 2015, p. E008460).
Evaluation of the project:
Various evaluation strategies can be applied to determine the success of the project. A before and
after strategy can be carried out, where the knowledge of the nurses can be determined before
the implementation of the education program and compare it with the knowledge after the end of
the implementation program. Moreover, the rates of falls among the elderly can be measured
before and after the implementation of the project. The rates of the falls before and after the
project can be statistically represented in the forms of bar charts and other graphs in order to
evaluate the success of the program. Moreover, feedbacks can be collected from the patients
about the efficacy of the exercise programs and whether such strategies are providing them with
favourable outcomes. The success of the implementation of the education package can be
evaluated by obtaining feedback from the nurses about how these education and training
programs helped them to provide effective care to the patients. Moreover, questionnaires can
also be used to evaluate the knowledge of the nurses about effective exercise strategies with the
aim to reduce the risk of falls among the elderly. The data obtained from the questionnaires can
be used to evaluate the knowledge improvement of the nurses and percentage of the
improvement can be obtained by comparing it with the evaluation done at the initial stages of the
project (Singh and Okeke 2016, pp.u210921-w4741).
inability to acquire the necessary resources and facilities in order to provide necessary care to
elderly patients. Lack of equipments, facilities, staff and experts can also act as potential barriers
to implementation (Loganathan et al. 2015, p. E008460).
Evaluation of the project:
Various evaluation strategies can be applied to determine the success of the project. A before and
after strategy can be carried out, where the knowledge of the nurses can be determined before
the implementation of the education program and compare it with the knowledge after the end of
the implementation program. Moreover, the rates of falls among the elderly can be measured
before and after the implementation of the project. The rates of the falls before and after the
project can be statistically represented in the forms of bar charts and other graphs in order to
evaluate the success of the program. Moreover, feedbacks can be collected from the patients
about the efficacy of the exercise programs and whether such strategies are providing them with
favourable outcomes. The success of the implementation of the education package can be
evaluated by obtaining feedback from the nurses about how these education and training
programs helped them to provide effective care to the patients. Moreover, questionnaires can
also be used to evaluate the knowledge of the nurses about effective exercise strategies with the
aim to reduce the risk of falls among the elderly. The data obtained from the questionnaires can
be used to evaluate the knowledge improvement of the nurses and percentage of the
improvement can be obtained by comparing it with the evaluation done at the initial stages of the
project (Singh and Okeke 2016, pp.u210921-w4741).
Reference List
Biedenweg, K., Meischke, H., Bohl, A., Hammerback, K., Williams, B., Poe, P. and Phelan, E.A., 2014.
Understanding older adults’ motivators and barriers to participating in organized programs
supporting exercise behaviors. The journal of primary prevention, 35(1), pp.1-11.
Blake, H. and Hawley, H., 2012. Effects of Tai Chi exercise on physical and psychological health of
older people. Current aging science, 5(1), pp.19-27.
Bouldin, E.D., Andresen, E.M., Dunton, N.E., Simon, M., Waters, T.M., Liu, M., Daniels, M.J., Mion,
L.C. and Shorr, R.I., 2013. Falls among adult patients hospitalized in the United States: prevalence
and trends. Journal of patient safety, 9(1), p.13.
Brennan, N.M. and Flynn, M.A., 2013. Differentiating clinical governance, clinical management and
clinical practice. Clinical Governance: An International Journal, 18(2), pp.114-131.
Cameron, I.D., Gillespie, L.D., Robertson, M.C., Murray, G.R., Hill, K.D., Cumming, R.G. and Kerse, N.,
2012. Interventions for preventing falls in older people in care facilities and hospitals. The Cochrane
Library, pp. 1-121.
Gillespie, L.D., Robertson, M.C., Gillespie, W.J., Sherrington, C., Gates, S., Clemson, L.M. and Lamb,
S.E., 2012. Interventions for preventing falls in older people living in the community. The Cochrane
Library, pp. 1-299.
Heyrani, A., Maleki, M., Marnani, A.B., Ravaghi, H., Sedaghat, M., Jabbari, M., Farsi, D., Khajavi, A.
and Abdi, Z., 2012. Clinical governance implementation in a selected teaching emergency
department: a systems approach. Implementation science, 7(1), p.84.
Knudsen, S.V., Laursen, H.B., Ehlers, L.H. and Mainz, J., 2017. ISQUA17-3217 There is need for
improvement of quality improvement-a systematic review of the PDSA method in QI
studies. International Journal for Quality in Health Care, 29(suppl_1), pp.45-45.
Loganathan, A., Ng, C.J., Tan, M.P. and Low, W.Y., 2015. Barriers faced by healthcare professionals
when managing falls in older people in Kuala Lumpur, Malaysia: a qualitative study. BMJ open, 5(11),
p.e008460.
Milisen, K., Coussement, J., Arnout, H., Vanlerberghe, V., De Paepe, L., Schoevaerdts, D., Lambert,
M., Van Den Noortgate, N., Delbaere, K., Boonen, S. and Dejaeger, E., 2013. Feasibility of
implementing a practice guideline for fall prevention on geriatric wards: A multicentre
study. International journal of nursing studies, 50(4), pp.495-507.
Biedenweg, K., Meischke, H., Bohl, A., Hammerback, K., Williams, B., Poe, P. and Phelan, E.A., 2014.
Understanding older adults’ motivators and barriers to participating in organized programs
supporting exercise behaviors. The journal of primary prevention, 35(1), pp.1-11.
Blake, H. and Hawley, H., 2012. Effects of Tai Chi exercise on physical and psychological health of
older people. Current aging science, 5(1), pp.19-27.
Bouldin, E.D., Andresen, E.M., Dunton, N.E., Simon, M., Waters, T.M., Liu, M., Daniels, M.J., Mion,
L.C. and Shorr, R.I., 2013. Falls among adult patients hospitalized in the United States: prevalence
and trends. Journal of patient safety, 9(1), p.13.
Brennan, N.M. and Flynn, M.A., 2013. Differentiating clinical governance, clinical management and
clinical practice. Clinical Governance: An International Journal, 18(2), pp.114-131.
Cameron, I.D., Gillespie, L.D., Robertson, M.C., Murray, G.R., Hill, K.D., Cumming, R.G. and Kerse, N.,
2012. Interventions for preventing falls in older people in care facilities and hospitals. The Cochrane
Library, pp. 1-121.
Gillespie, L.D., Robertson, M.C., Gillespie, W.J., Sherrington, C., Gates, S., Clemson, L.M. and Lamb,
S.E., 2012. Interventions for preventing falls in older people living in the community. The Cochrane
Library, pp. 1-299.
Heyrani, A., Maleki, M., Marnani, A.B., Ravaghi, H., Sedaghat, M., Jabbari, M., Farsi, D., Khajavi, A.
and Abdi, Z., 2012. Clinical governance implementation in a selected teaching emergency
department: a systems approach. Implementation science, 7(1), p.84.
Knudsen, S.V., Laursen, H.B., Ehlers, L.H. and Mainz, J., 2017. ISQUA17-3217 There is need for
improvement of quality improvement-a systematic review of the PDSA method in QI
studies. International Journal for Quality in Health Care, 29(suppl_1), pp.45-45.
Loganathan, A., Ng, C.J., Tan, M.P. and Low, W.Y., 2015. Barriers faced by healthcare professionals
when managing falls in older people in Kuala Lumpur, Malaysia: a qualitative study. BMJ open, 5(11),
p.e008460.
Milisen, K., Coussement, J., Arnout, H., Vanlerberghe, V., De Paepe, L., Schoevaerdts, D., Lambert,
M., Van Den Noortgate, N., Delbaere, K., Boonen, S. and Dejaeger, E., 2013. Feasibility of
implementing a practice guideline for fall prevention on geriatric wards: A multicentre
study. International journal of nursing studies, 50(4), pp.495-507.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Montero Odasso, M., Verghese, J., Beauchet, O. and Hausdorff, J.M., 2012. Gait and cognition: a‐
complementary approach to understanding brain function and the risk of falling. Journal of the
American Geriatrics Society, 60(11), pp.2127-2136.
Morse, J., Merry, A. and Bloswick, D., 2016. Research Approaches to the Prevention and Protection
of Patient Falls. Fall Prevention and Protection: Principles, Guidelines, and Practices, p.341.
Muir, S.W., Gopaul, K. and Montero Odasso, M.M., 2012. The role of cognitive impairment in fall risk
among older adults: a systematic review and meta-analysis. Age and ageing, 41(3), pp.299-308.
Rosenfeld, R.M., Shiffman, R.N. and Robertson, P., 2013. Clinical practice guideline development
manual: a quality-driven approach for translating evidence into action. Otolaryngology—Head and
Neck Surgery, 148(1_suppl), pp.S1-S55.
Sherrington, C. and Tiedemann, A., 2015. Physiotherapy in the prevention of falls in older
people. Journal of physiotherapy, 61(2), pp.54-60.
Singh, I. and Okeke, J., 2016. Reducing inpatient falls in a 100% single room elderly care
environment: evaluation of the impact of a systematic nurse training programme on falls risk
assessment (FRA). BMJ quality improvement reports, 5(1), pp.u210921-w4741.
Snyder, H.R., 2013. Major depressive disorder is associated with broad impairments on
neuropsychological measures of executive function: A meta-analysis and review.
Taylor, M.J., McNicholas, C., Nicolay, C., Darzi, A., Bell, D. and Reed, J.E., 2013. Systematic review of
the application of the plan–do–study–act method to improve quality in healthcare. BMJ Qual Saf,
pp.bmjqs-2013.
Tiedemann, A., Sherrington, C. and Lord, S.R., 2013. The role of exercise for fall prevention in older
age. Motriz: Revista de Educação Física, 19(3), pp.541-547.
Winter, H., Watt, K. and Peel, N.M., 2013. Falls prevention interventions for community-dwelling
older persons with cognitive impairment: a systematic review. International psychogeriatrics, 25(2),
pp.215-227.
complementary approach to understanding brain function and the risk of falling. Journal of the
American Geriatrics Society, 60(11), pp.2127-2136.
Morse, J., Merry, A. and Bloswick, D., 2016. Research Approaches to the Prevention and Protection
of Patient Falls. Fall Prevention and Protection: Principles, Guidelines, and Practices, p.341.
Muir, S.W., Gopaul, K. and Montero Odasso, M.M., 2012. The role of cognitive impairment in fall risk
among older adults: a systematic review and meta-analysis. Age and ageing, 41(3), pp.299-308.
Rosenfeld, R.M., Shiffman, R.N. and Robertson, P., 2013. Clinical practice guideline development
manual: a quality-driven approach for translating evidence into action. Otolaryngology—Head and
Neck Surgery, 148(1_suppl), pp.S1-S55.
Sherrington, C. and Tiedemann, A., 2015. Physiotherapy in the prevention of falls in older
people. Journal of physiotherapy, 61(2), pp.54-60.
Singh, I. and Okeke, J., 2016. Reducing inpatient falls in a 100% single room elderly care
environment: evaluation of the impact of a systematic nurse training programme on falls risk
assessment (FRA). BMJ quality improvement reports, 5(1), pp.u210921-w4741.
Snyder, H.R., 2013. Major depressive disorder is associated with broad impairments on
neuropsychological measures of executive function: A meta-analysis and review.
Taylor, M.J., McNicholas, C., Nicolay, C., Darzi, A., Bell, D. and Reed, J.E., 2013. Systematic review of
the application of the plan–do–study–act method to improve quality in healthcare. BMJ Qual Saf,
pp.bmjqs-2013.
Tiedemann, A., Sherrington, C. and Lord, S.R., 2013. The role of exercise for fall prevention in older
age. Motriz: Revista de Educação Física, 19(3), pp.541-547.
Winter, H., Watt, K. and Peel, N.M., 2013. Falls prevention interventions for community-dwelling
older persons with cognitive impairment: a systematic review. International psychogeriatrics, 25(2),
pp.215-227.
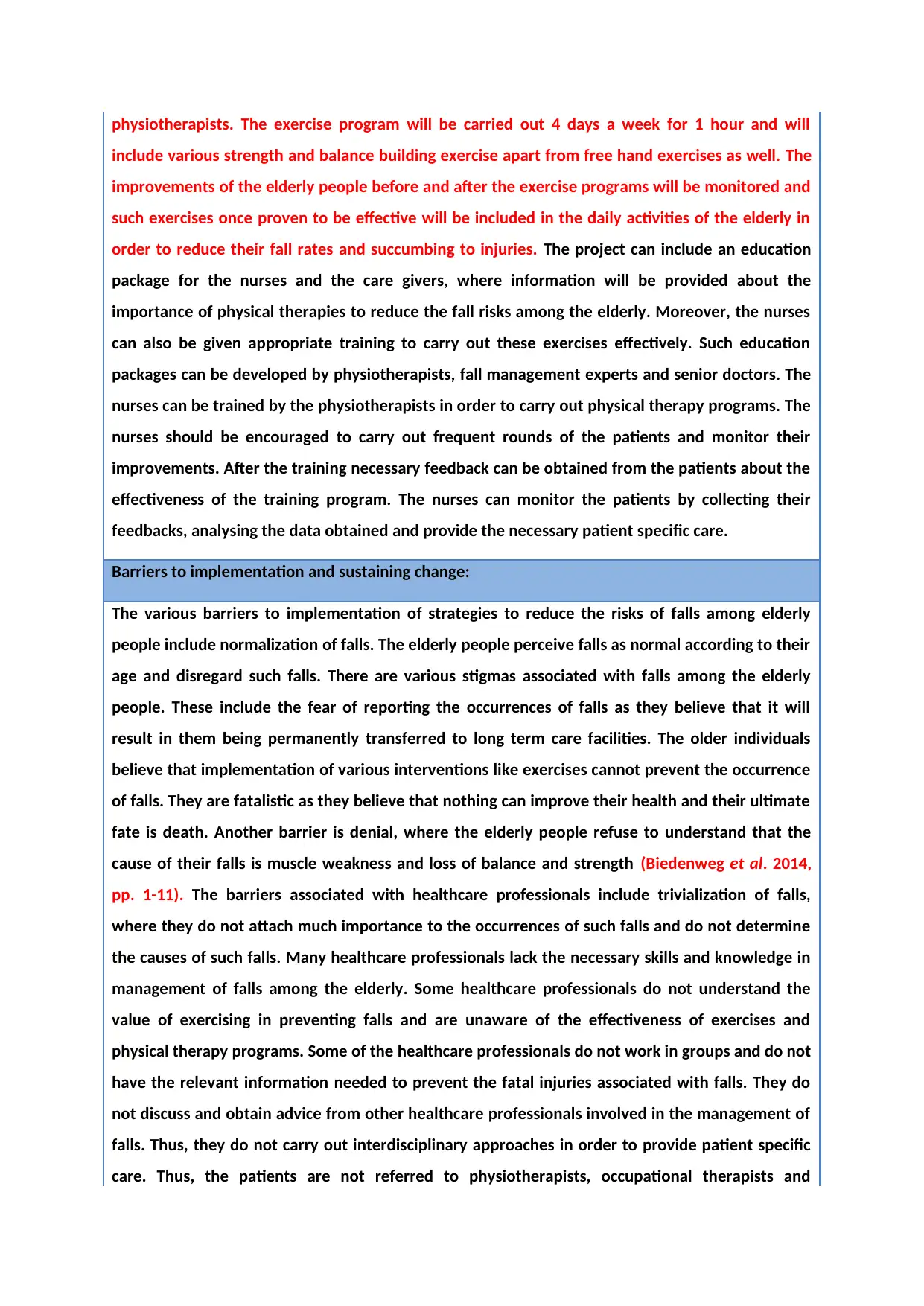
NURS2006 Assignment 3 - CPI paper Marking Rubric
PERFORMANCE STANDARD
CATEGORY &
WEIGHTING Excellent Work Good Work Passing Work Unsatisfactory work
Project Aim
and Evidence
the issue is
worth solving
20%
Aim succinct & clearly
defined. All evidence
relevant & rigorous.
Shows a very high level of
insight & relevance to the
issue.
(17-20)
Aim well defined.
Some irrelevant
information but most
evidence relevant &
rigorous. Shows a very
good level of insight &
relevance to the issue.
(13-16.5)
Aim stated with some
ambiguity. Some evidence
relevant and rigorous,
Acceptable level of
insight.
Quite a lot of irrelevant
information is present.
May be overlong/ too
brief
(10-12.5)
Aim not clearly stated
Most evidence is not
relevant or rigorous.
Poor level of insight &
relevance to the issue.
Significant amount of
irrelevant/ missing
information.
(0–9.5)
Relevance of
Clinical
Governance to
your project
10%
Succinct and highly
relevant discussion of the
relevant pillar of clinical
governance related to the
chosen clinical issue.
(9-10)
Succinct and mostly
relevant discussion of the
relevant pillar of clinical
governance related to the
chosen clinical issue.
(7-8.5)
Adequate discussion of
the relevant pillar of
clinical governance
related to the chosen
clinical issue.
Some parts not relevant
Overlong / too brief, may
be missing relevant
information.
(5-6.5)
Inadequate discussion of
the relevant pillar of
clinical governance
related to the chosen
clinical issue. Overlong /
too brief, may be missing
a significant amount of
relevant information
(0-4.5)
Key
Stakeholders
5%
Identifies most relevant
key stakeholders.
Discusses clearly how they
could be involved in the
project.
Succinctly and expertly
written. Very high level of
insight into the role of
stakeholders.
(4.5 - 5)
Identifies some relevant
key stakeholders and
adequately discusses how
they could be involved in
the project.
Very well written. Good
level of insight into the
role of stakeholders.
(3.5-4.25)
Identifies a few relevant
key stakeholders.
Mentions briefly how they
could be involved. Quite
well written but contains
some irrelevant
information, or minor
information is missing.
Adequate level of insight
into the stakeholder role.
(2.5 – 3.25- )
Contains irrelevant
information, or major
information is missing.
Inappropriate or no key
stakeholders are
identified Poor insight
into the stakeholder role.
(0-2)
Clinical Practice
Improvement
Tool
20%
Describes a relevant CPI
tool Very clearly discusses
how it could be used to
address the aim and
implement the
interventions. Succinctly
and expertly written with
no omissions of relevant
information.
(17-20)
Describes a relevant CPI
tool Discusses quite
clearly how the tool could
be used to address the
aim and implement the
interventions. Well
written but may contain
some irrelevant
information, or some
minor information is
missing
(13-16.5)
Describes a relevant CPI
tool and adequately
discusses how the tool
could be used to address
the aim and implement
the interventions.
Not succinct, contains
irrelevant information,
significant information is
missing
(10-12.5)
A relevant CPI tool is not
identified. There is no
adequate discussion of
how the tool could be
used to meet the aim or
implement the
interventions.
Contains irrelevant
information or some
major information is
missing.
(0–9.5)
Summary of
proposed
interventions
20%
All relevant interventions
are discussed very well.
Project outline is very
clear and the relevance to
clinical practice is very
high.
Most relevant
interventions discussed
quite well.
Project outline is clear &
relevance to clinical
practice is good. Contains
some irrelevant
information, minor
information may be
missing.
Acceptable level of
relevant interventions
discussed.
Project outline mostly
clear, although it may be
unclear how the project
would actually be
implemented in clinical
practice due to
irrelevant/missing info
Some elements missing or
incomplete. May contain
large amounts of
irrelevant information.
Project poorly described
and it is unclear what the
project actually entails or
its relevance to clinical
practice.
PERFORMANCE STANDARD
CATEGORY &
WEIGHTING Excellent Work Good Work Passing Work Unsatisfactory work
Project Aim
and Evidence
the issue is
worth solving
20%
Aim succinct & clearly
defined. All evidence
relevant & rigorous.
Shows a very high level of
insight & relevance to the
issue.
(17-20)
Aim well defined.
Some irrelevant
information but most
evidence relevant &
rigorous. Shows a very
good level of insight &
relevance to the issue.
(13-16.5)
Aim stated with some
ambiguity. Some evidence
relevant and rigorous,
Acceptable level of
insight.
Quite a lot of irrelevant
information is present.
May be overlong/ too
brief
(10-12.5)
Aim not clearly stated
Most evidence is not
relevant or rigorous.
Poor level of insight &
relevance to the issue.
Significant amount of
irrelevant/ missing
information.
(0–9.5)
Relevance of
Clinical
Governance to
your project
10%
Succinct and highly
relevant discussion of the
relevant pillar of clinical
governance related to the
chosen clinical issue.
(9-10)
Succinct and mostly
relevant discussion of the
relevant pillar of clinical
governance related to the
chosen clinical issue.
(7-8.5)
Adequate discussion of
the relevant pillar of
clinical governance
related to the chosen
clinical issue.
Some parts not relevant
Overlong / too brief, may
be missing relevant
information.
(5-6.5)
Inadequate discussion of
the relevant pillar of
clinical governance
related to the chosen
clinical issue. Overlong /
too brief, may be missing
a significant amount of
relevant information
(0-4.5)
Key
Stakeholders
5%
Identifies most relevant
key stakeholders.
Discusses clearly how they
could be involved in the
project.
Succinctly and expertly
written. Very high level of
insight into the role of
stakeholders.
(4.5 - 5)
Identifies some relevant
key stakeholders and
adequately discusses how
they could be involved in
the project.
Very well written. Good
level of insight into the
role of stakeholders.
(3.5-4.25)
Identifies a few relevant
key stakeholders.
Mentions briefly how they
could be involved. Quite
well written but contains
some irrelevant
information, or minor
information is missing.
Adequate level of insight
into the stakeholder role.
(2.5 – 3.25- )
Contains irrelevant
information, or major
information is missing.
Inappropriate or no key
stakeholders are
identified Poor insight
into the stakeholder role.
(0-2)
Clinical Practice
Improvement
Tool
20%
Describes a relevant CPI
tool Very clearly discusses
how it could be used to
address the aim and
implement the
interventions. Succinctly
and expertly written with
no omissions of relevant
information.
(17-20)
Describes a relevant CPI
tool Discusses quite
clearly how the tool could
be used to address the
aim and implement the
interventions. Well
written but may contain
some irrelevant
information, or some
minor information is
missing
(13-16.5)
Describes a relevant CPI
tool and adequately
discusses how the tool
could be used to address
the aim and implement
the interventions.
Not succinct, contains
irrelevant information,
significant information is
missing
(10-12.5)
A relevant CPI tool is not
identified. There is no
adequate discussion of
how the tool could be
used to meet the aim or
implement the
interventions.
Contains irrelevant
information or some
major information is
missing.
(0–9.5)
Summary of
proposed
interventions
20%
All relevant interventions
are discussed very well.
Project outline is very
clear and the relevance to
clinical practice is very
high.
Most relevant
interventions discussed
quite well.
Project outline is clear &
relevance to clinical
practice is good. Contains
some irrelevant
information, minor
information may be
missing.
Acceptable level of
relevant interventions
discussed.
Project outline mostly
clear, although it may be
unclear how the project
would actually be
implemented in clinical
practice due to
irrelevant/missing info
Some elements missing or
incomplete. May contain
large amounts of
irrelevant information.
Project poorly described
and it is unclear what the
project actually entails or
its relevance to clinical
practice.
(17-20) (13-16.5) (10-12.5) (0–9.5)
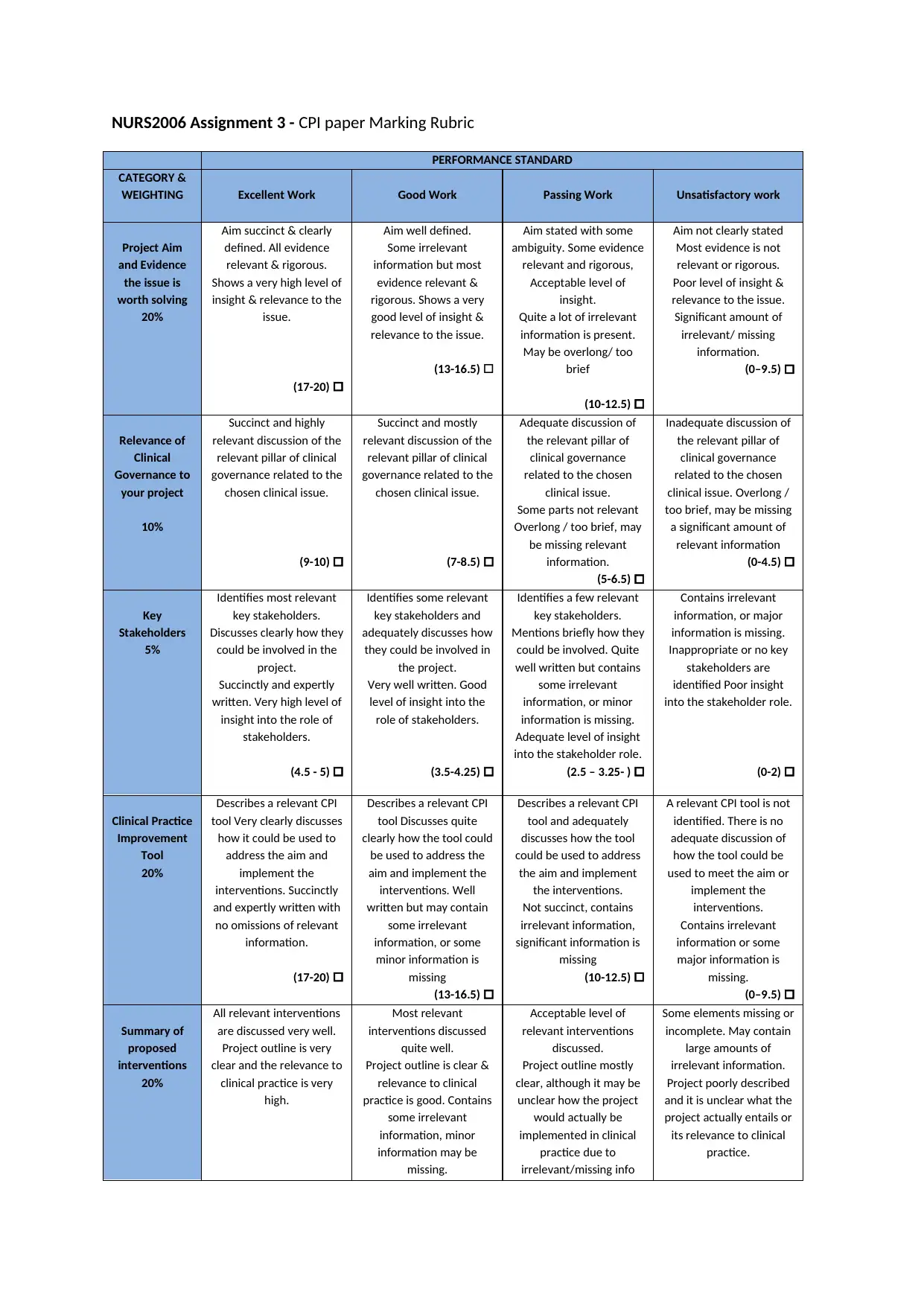
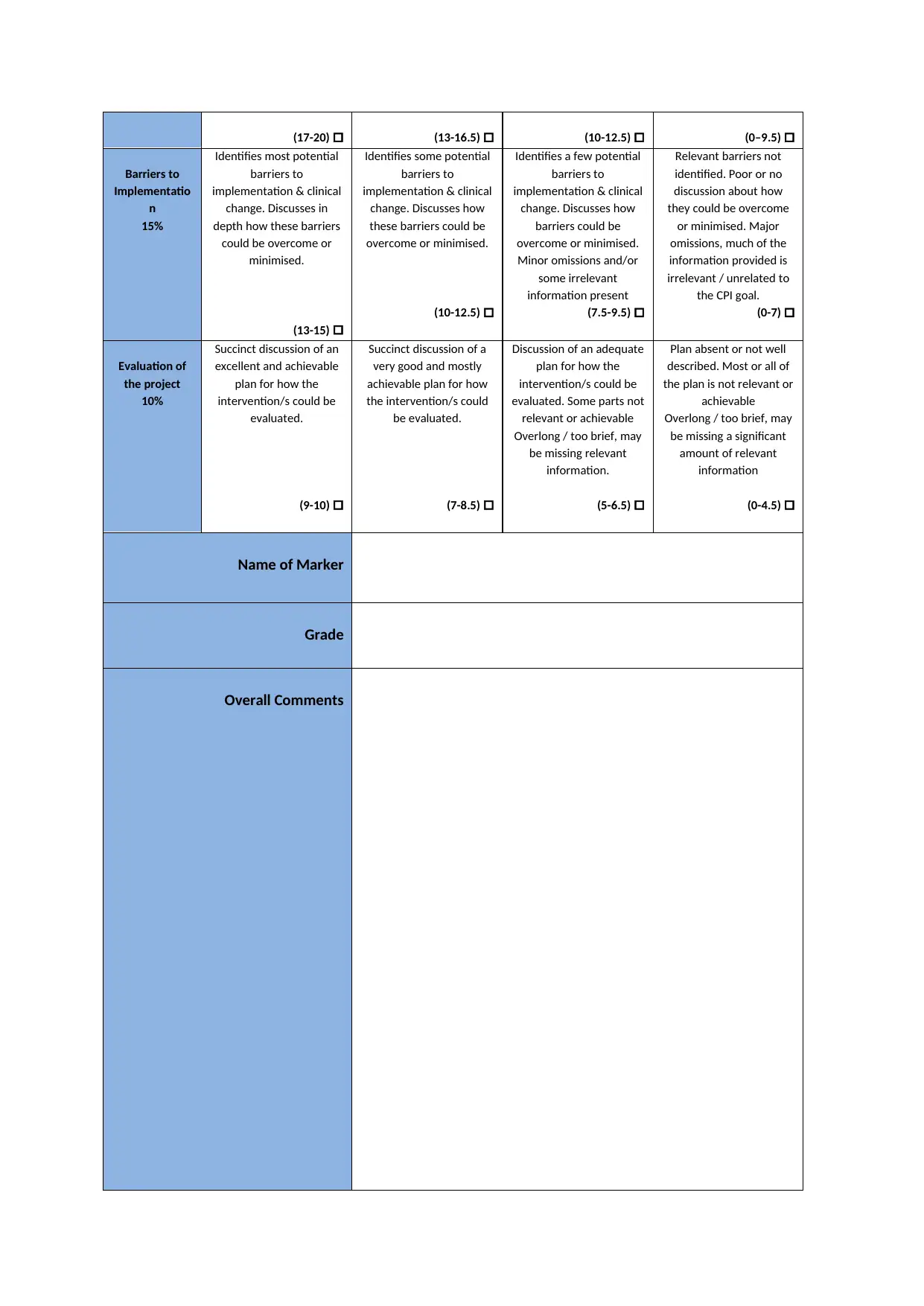
Barriers to
Implementatio
n
15%
Identifies most potential
barriers to
implementation & clinical
change. Discusses in
depth how these barriers
could be overcome or
minimised.
(13-15)
Identifies some potential
barriers to
implementation & clinical
change. Discusses how
these barriers could be
overcome or minimised.
(10-12.5)
Identifies a few potential
barriers to
implementation & clinical
change. Discusses how
barriers could be
overcome or minimised.
Minor omissions and/or
some irrelevant
information present
(7.5-9.5)
Relevant barriers not
identified. Poor or no
discussion about how
they could be overcome
or minimised. Major
omissions, much of the
information provided is
irrelevant / unrelated to
the CPI goal.
(0-7)
Evaluation of
the project
10%
Succinct discussion of an
excellent and achievable
plan for how the
intervention/s could be
evaluated.
(9-10)
Succinct discussion of a
very good and mostly
achievable plan for how
the intervention/s could
be evaluated.
(7-8.5)
Discussion of an adequate
plan for how the
intervention/s could be
evaluated. Some parts not
relevant or achievable
Overlong / too brief, may
be missing relevant
information.
(5-6.5)
Plan absent or not well
described. Most or all of
the plan is not relevant or
achievable
Overlong / too brief, may
be missing a significant
amount of relevant
information
(0-4.5)
Name of Marker
Grade
Overall Comments
Barriers to
Implementatio
n
15%
Identifies most potential
barriers to
implementation & clinical
change. Discusses in
depth how these barriers
could be overcome or
minimised.
(13-15)
Identifies some potential
barriers to
implementation & clinical
change. Discusses how
these barriers could be
overcome or minimised.
(10-12.5)
Identifies a few potential
barriers to
implementation & clinical
change. Discusses how
barriers could be
overcome or minimised.
Minor omissions and/or
some irrelevant
information present
(7.5-9.5)
Relevant barriers not
identified. Poor or no
discussion about how
they could be overcome
or minimised. Major
omissions, much of the
information provided is
irrelevant / unrelated to
the CPI goal.
(0-7)
Evaluation of
the project
10%
Succinct discussion of an
excellent and achievable
plan for how the
intervention/s could be
evaluated.
(9-10)
Succinct discussion of a
very good and mostly
achievable plan for how
the intervention/s could
be evaluated.
(7-8.5)
Discussion of an adequate
plan for how the
intervention/s could be
evaluated. Some parts not
relevant or achievable
Overlong / too brief, may
be missing relevant
information.
(5-6.5)
Plan absent or not well
described. Most or all of
the plan is not relevant or
achievable
Overlong / too brief, may
be missing a significant
amount of relevant
information
(0-4.5)
Name of Marker
Grade
Overall Comments
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





