Regulatory Environment in Healthcare
VerifiedAdded on 2023/05/30
|7
|1731
|128
AI Summary
This article discusses the violation of the Referral Fee Law in the supply and value exchange process of Durable Medical Equipments (DME) in healthcare. It highlights the responsibilities of different stakeholders in maintaining compliance and preventing unethical practices.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

1Running head: REGULATORY ENVIRONMENT IN HEALTHCARE
Regulatory Environment in Healthcare
Type Your Name Here
National American University
Regulatory Environment in Healthcare
Type Your Name Here
National American University
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
2REGULATORY ENVIRONMENT IN HEALTHCARE
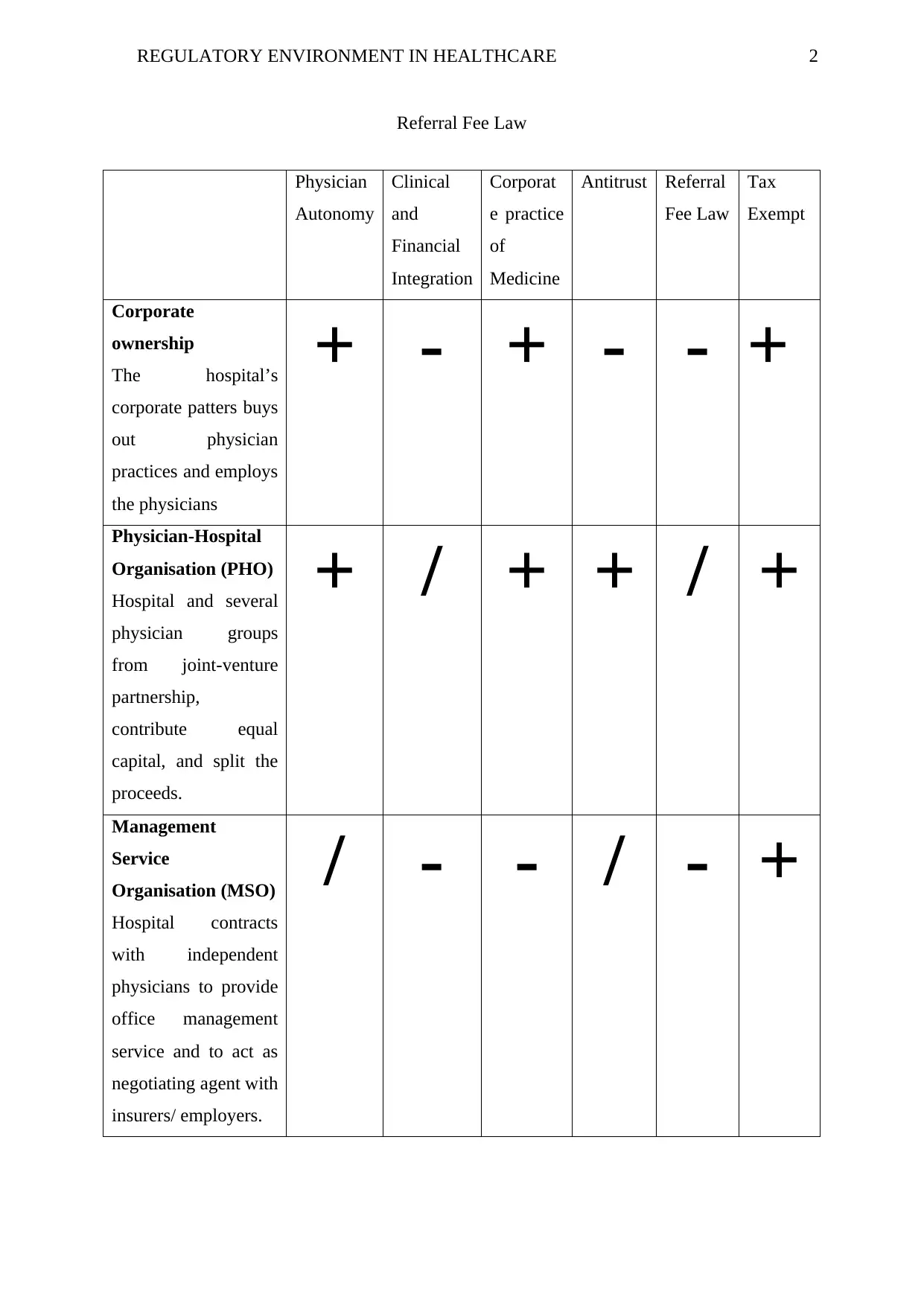
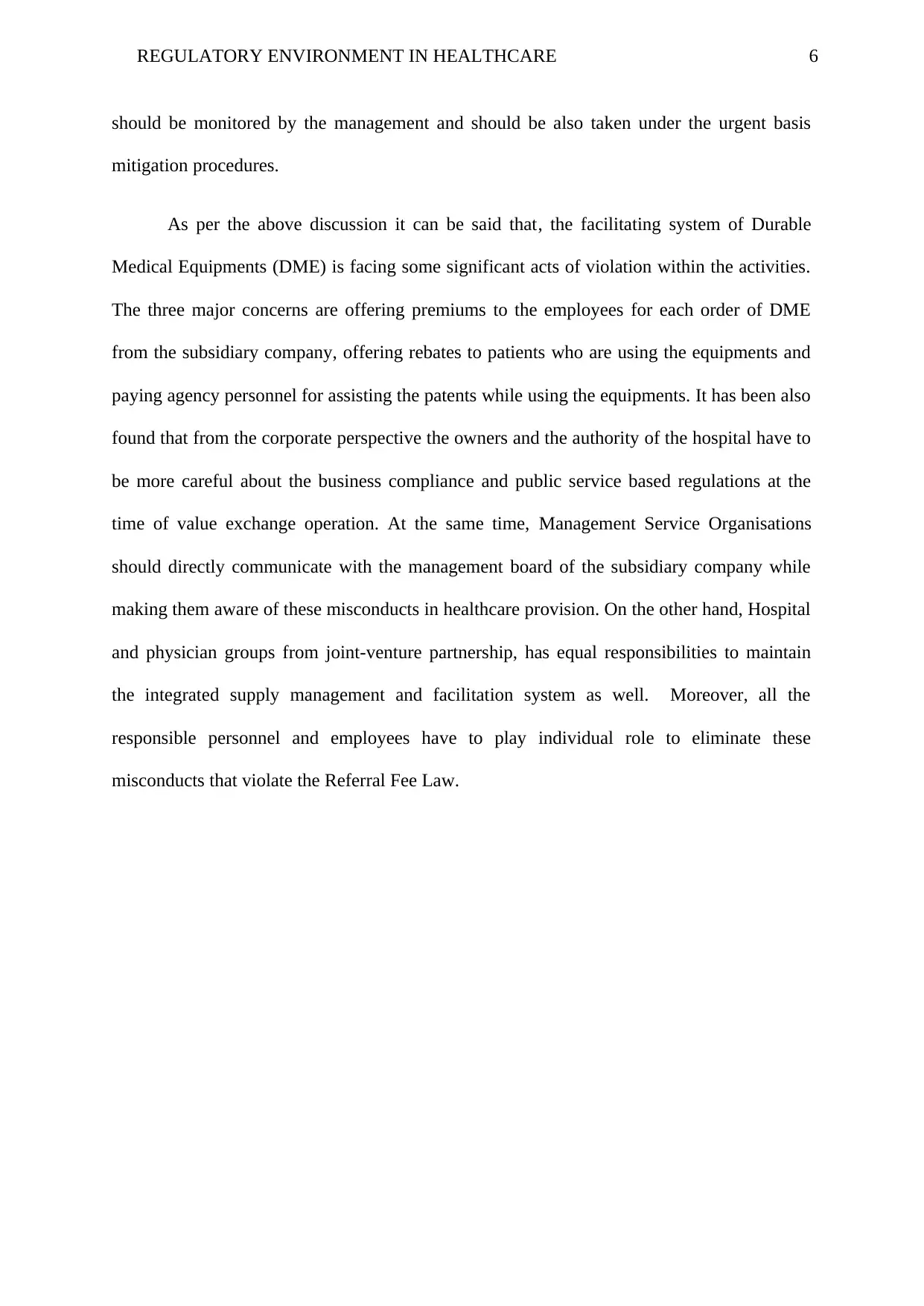
Referral Fee Law
Physician
Autonomy
Clinical
and
Financial
Integration
Corporat
e practice
of
Medicine
Antitrust Referral
Fee Law
Tax
Exempt
Corporate
ownership
The hospital’s
corporate patters buys
out physician
practices and employs
the physicians
+ - + - - +
Physician-Hospital
Organisation (PHO)
Hospital and several
physician groups
from joint-venture
partnership,
contribute equal
capital, and split the
proceeds.
+ / + + / +
Management
Service
Organisation (MSO)
Hospital contracts
with independent
physicians to provide
office management
service and to act as
negotiating agent with
insurers/ employers.
/ - - / - +
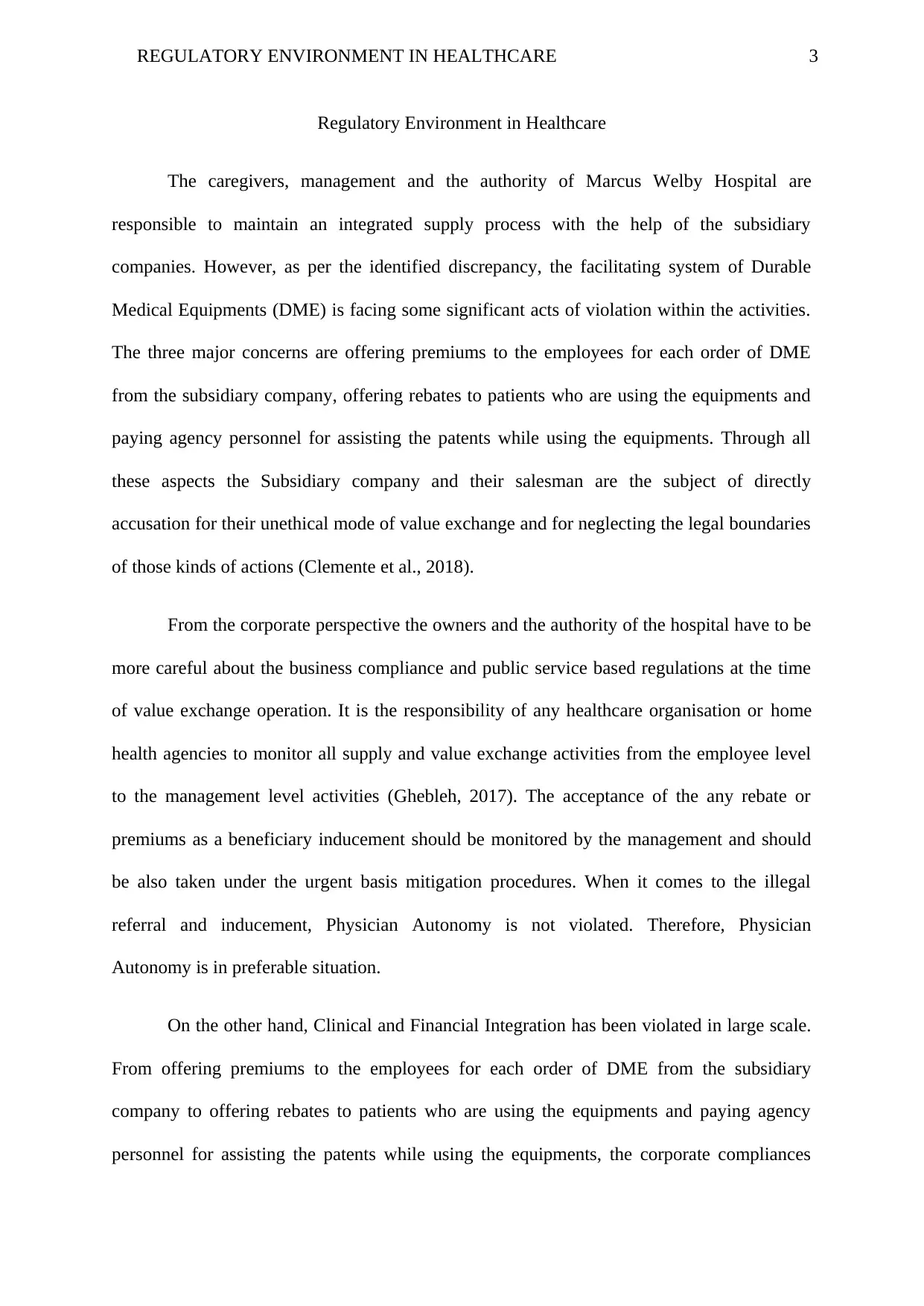
Referral Fee Law
Physician
Autonomy
Clinical
and
Financial
Integration
Corporat
e practice
of
Medicine
Antitrust Referral
Fee Law
Tax
Exempt
Corporate
ownership
The hospital’s
corporate patters buys
out physician
practices and employs
the physicians
+ - + - - +
Physician-Hospital
Organisation (PHO)
Hospital and several
physician groups
from joint-venture
partnership,
contribute equal
capital, and split the
proceeds.
+ / + + / +
Management
Service
Organisation (MSO)
Hospital contracts
with independent
physicians to provide
office management
service and to act as
negotiating agent with
insurers/ employers.
/ - - / - +
3REGULATORY ENVIRONMENT IN HEALTHCARE
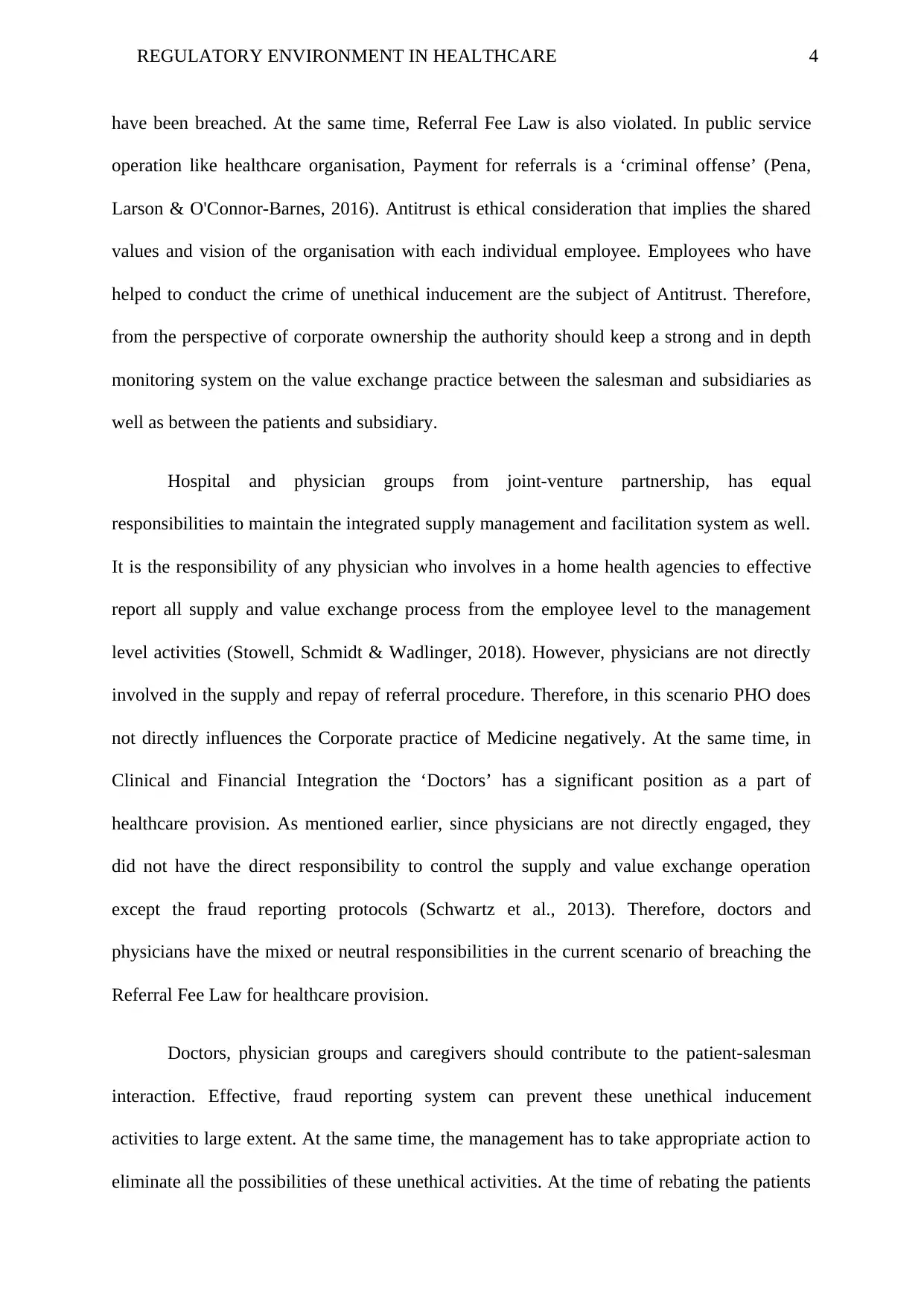
Regulatory Environment in Healthcare
The caregivers, management and the authority of Marcus Welby Hospital are
responsible to maintain an integrated supply process with the help of the subsidiary
companies. However, as per the identified discrepancy, the facilitating system of Durable
Medical Equipments (DME) is facing some significant acts of violation within the activities.
The three major concerns are offering premiums to the employees for each order of DME
from the subsidiary company, offering rebates to patients who are using the equipments and
paying agency personnel for assisting the patents while using the equipments. Through all
these aspects the Subsidiary company and their salesman are the subject of directly
accusation for their unethical mode of value exchange and for neglecting the legal boundaries
of those kinds of actions (Clemente et al., 2018).
From the corporate perspective the owners and the authority of the hospital have to be
more careful about the business compliance and public service based regulations at the time
of value exchange operation. It is the responsibility of any healthcare organisation or home
health agencies to monitor all supply and value exchange activities from the employee level
to the management level activities (Ghebleh, 2017). The acceptance of the any rebate or
premiums as a beneficiary inducement should be monitored by the management and should
be also taken under the urgent basis mitigation procedures. When it comes to the illegal
referral and inducement, Physician Autonomy is not violated. Therefore, Physician
Autonomy is in preferable situation.
On the other hand, Clinical and Financial Integration has been violated in large scale.
From offering premiums to the employees for each order of DME from the subsidiary
company to offering rebates to patients who are using the equipments and paying agency
personnel for assisting the patents while using the equipments, the corporate compliances
Regulatory Environment in Healthcare
The caregivers, management and the authority of Marcus Welby Hospital are
responsible to maintain an integrated supply process with the help of the subsidiary
companies. However, as per the identified discrepancy, the facilitating system of Durable
Medical Equipments (DME) is facing some significant acts of violation within the activities.
The three major concerns are offering premiums to the employees for each order of DME
from the subsidiary company, offering rebates to patients who are using the equipments and
paying agency personnel for assisting the patents while using the equipments. Through all
these aspects the Subsidiary company and their salesman are the subject of directly
accusation for their unethical mode of value exchange and for neglecting the legal boundaries
of those kinds of actions (Clemente et al., 2018).
From the corporate perspective the owners and the authority of the hospital have to be
more careful about the business compliance and public service based regulations at the time
of value exchange operation. It is the responsibility of any healthcare organisation or home
health agencies to monitor all supply and value exchange activities from the employee level
to the management level activities (Ghebleh, 2017). The acceptance of the any rebate or
premiums as a beneficiary inducement should be monitored by the management and should
be also taken under the urgent basis mitigation procedures. When it comes to the illegal
referral and inducement, Physician Autonomy is not violated. Therefore, Physician
Autonomy is in preferable situation.
On the other hand, Clinical and Financial Integration has been violated in large scale.
From offering premiums to the employees for each order of DME from the subsidiary
company to offering rebates to patients who are using the equipments and paying agency
personnel for assisting the patents while using the equipments, the corporate compliances
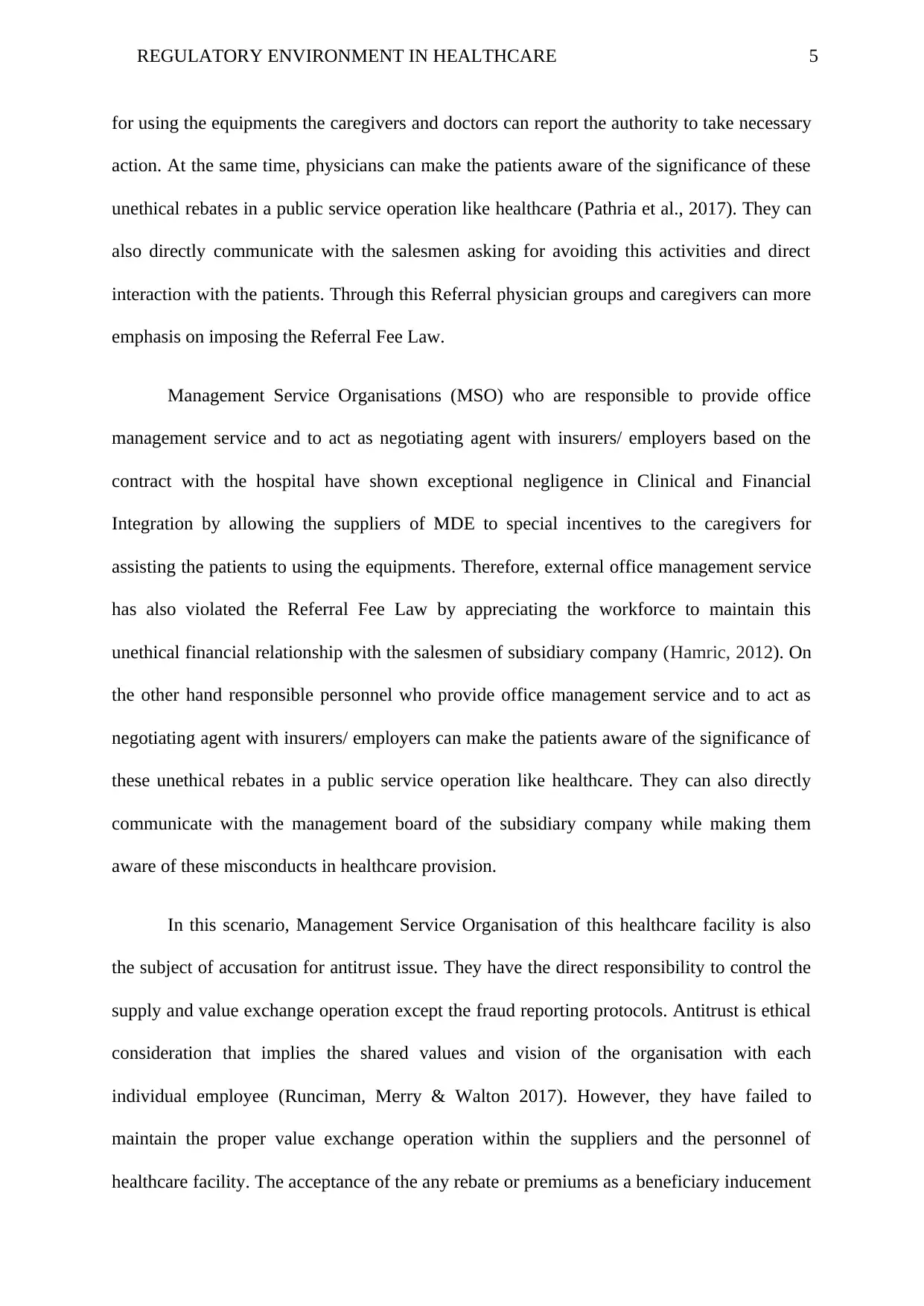
4REGULATORY ENVIRONMENT IN HEALTHCARE
have been breached. At the same time, Referral Fee Law is also violated. In public service
operation like healthcare organisation, Payment for referrals is a ‘criminal offense’ (Pena,
Larson & O'Connor-Barnes, 2016). Antitrust is ethical consideration that implies the shared
values and vision of the organisation with each individual employee. Employees who have
helped to conduct the crime of unethical inducement are the subject of Antitrust. Therefore,
from the perspective of corporate ownership the authority should keep a strong and in depth
monitoring system on the value exchange practice between the salesman and subsidiaries as
well as between the patients and subsidiary.
Hospital and physician groups from joint-venture partnership, has equal
responsibilities to maintain the integrated supply management and facilitation system as well.
It is the responsibility of any physician who involves in a home health agencies to effective
report all supply and value exchange process from the employee level to the management
level activities (Stowell, Schmidt & Wadlinger, 2018). However, physicians are not directly
involved in the supply and repay of referral procedure. Therefore, in this scenario PHO does
not directly influences the Corporate practice of Medicine negatively. At the same time, in
Clinical and Financial Integration the ‘Doctors’ has a significant position as a part of
healthcare provision. As mentioned earlier, since physicians are not directly engaged, they
did not have the direct responsibility to control the supply and value exchange operation
except the fraud reporting protocols (Schwartz et al., 2013). Therefore, doctors and
physicians have the mixed or neutral responsibilities in the current scenario of breaching the
Referral Fee Law for healthcare provision.
Doctors, physician groups and caregivers should contribute to the patient-salesman
interaction. Effective, fraud reporting system can prevent these unethical inducement
activities to large extent. At the same time, the management has to take appropriate action to
eliminate all the possibilities of these unethical activities. At the time of rebating the patients
have been breached. At the same time, Referral Fee Law is also violated. In public service
operation like healthcare organisation, Payment for referrals is a ‘criminal offense’ (Pena,
Larson & O'Connor-Barnes, 2016). Antitrust is ethical consideration that implies the shared
values and vision of the organisation with each individual employee. Employees who have
helped to conduct the crime of unethical inducement are the subject of Antitrust. Therefore,
from the perspective of corporate ownership the authority should keep a strong and in depth
monitoring system on the value exchange practice between the salesman and subsidiaries as
well as between the patients and subsidiary.
Hospital and physician groups from joint-venture partnership, has equal
responsibilities to maintain the integrated supply management and facilitation system as well.
It is the responsibility of any physician who involves in a home health agencies to effective
report all supply and value exchange process from the employee level to the management
level activities (Stowell, Schmidt & Wadlinger, 2018). However, physicians are not directly
involved in the supply and repay of referral procedure. Therefore, in this scenario PHO does
not directly influences the Corporate practice of Medicine negatively. At the same time, in
Clinical and Financial Integration the ‘Doctors’ has a significant position as a part of
healthcare provision. As mentioned earlier, since physicians are not directly engaged, they
did not have the direct responsibility to control the supply and value exchange operation
except the fraud reporting protocols (Schwartz et al., 2013). Therefore, doctors and
physicians have the mixed or neutral responsibilities in the current scenario of breaching the
Referral Fee Law for healthcare provision.
Doctors, physician groups and caregivers should contribute to the patient-salesman
interaction. Effective, fraud reporting system can prevent these unethical inducement
activities to large extent. At the same time, the management has to take appropriate action to
eliminate all the possibilities of these unethical activities. At the time of rebating the patients
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
5REGULATORY ENVIRONMENT IN HEALTHCARE
for using the equipments the caregivers and doctors can report the authority to take necessary
action. At the same time, physicians can make the patients aware of the significance of these
unethical rebates in a public service operation like healthcare (Pathria et al., 2017). They can
also directly communicate with the salesmen asking for avoiding this activities and direct
interaction with the patients. Through this Referral physician groups and caregivers can more
emphasis on imposing the Referral Fee Law.
Management Service Organisations (MSO) who are responsible to provide office
management service and to act as negotiating agent with insurers/ employers based on the
contract with the hospital have shown exceptional negligence in Clinical and Financial
Integration by allowing the suppliers of MDE to special incentives to the caregivers for
assisting the patients to using the equipments. Therefore, external office management service
has also violated the Referral Fee Law by appreciating the workforce to maintain this
unethical financial relationship with the salesmen of subsidiary company (Hamric, 2012). On
the other hand responsible personnel who provide office management service and to act as
negotiating agent with insurers/ employers can make the patients aware of the significance of
these unethical rebates in a public service operation like healthcare. They can also directly
communicate with the management board of the subsidiary company while making them
aware of these misconducts in healthcare provision.
In this scenario, Management Service Organisation of this healthcare facility is also
the subject of accusation for antitrust issue. They have the direct responsibility to control the
supply and value exchange operation except the fraud reporting protocols. Antitrust is ethical
consideration that implies the shared values and vision of the organisation with each
individual employee (Runciman, Merry & Walton 2017). However, they have failed to
maintain the proper value exchange operation within the suppliers and the personnel of
healthcare facility. The acceptance of the any rebate or premiums as a beneficiary inducement
for using the equipments the caregivers and doctors can report the authority to take necessary
action. At the same time, physicians can make the patients aware of the significance of these
unethical rebates in a public service operation like healthcare (Pathria et al., 2017). They can
also directly communicate with the salesmen asking for avoiding this activities and direct
interaction with the patients. Through this Referral physician groups and caregivers can more
emphasis on imposing the Referral Fee Law.
Management Service Organisations (MSO) who are responsible to provide office
management service and to act as negotiating agent with insurers/ employers based on the
contract with the hospital have shown exceptional negligence in Clinical and Financial
Integration by allowing the suppliers of MDE to special incentives to the caregivers for
assisting the patients to using the equipments. Therefore, external office management service
has also violated the Referral Fee Law by appreciating the workforce to maintain this
unethical financial relationship with the salesmen of subsidiary company (Hamric, 2012). On
the other hand responsible personnel who provide office management service and to act as
negotiating agent with insurers/ employers can make the patients aware of the significance of
these unethical rebates in a public service operation like healthcare. They can also directly
communicate with the management board of the subsidiary company while making them
aware of these misconducts in healthcare provision.
In this scenario, Management Service Organisation of this healthcare facility is also
the subject of accusation for antitrust issue. They have the direct responsibility to control the
supply and value exchange operation except the fraud reporting protocols. Antitrust is ethical
consideration that implies the shared values and vision of the organisation with each
individual employee (Runciman, Merry & Walton 2017). However, they have failed to
maintain the proper value exchange operation within the suppliers and the personnel of
healthcare facility. The acceptance of the any rebate or premiums as a beneficiary inducement
6REGULATORY ENVIRONMENT IN HEALTHCARE
should be monitored by the management and should be also taken under the urgent basis
mitigation procedures.
As per the above discussion it can be said that, the facilitating system of Durable
Medical Equipments (DME) is facing some significant acts of violation within the activities.
The three major concerns are offering premiums to the employees for each order of DME
from the subsidiary company, offering rebates to patients who are using the equipments and
paying agency personnel for assisting the patents while using the equipments. It has been also
found that from the corporate perspective the owners and the authority of the hospital have to
be more careful about the business compliance and public service based regulations at the
time of value exchange operation. At the same time, Management Service Organisations
should directly communicate with the management board of the subsidiary company while
making them aware of these misconducts in healthcare provision. On the other hand, Hospital
and physician groups from joint-venture partnership, has equal responsibilities to maintain
the integrated supply management and facilitation system as well. Moreover, all the
responsible personnel and employees have to play individual role to eliminate these
misconducts that violate the Referral Fee Law.
should be monitored by the management and should be also taken under the urgent basis
mitigation procedures.
As per the above discussion it can be said that, the facilitating system of Durable
Medical Equipments (DME) is facing some significant acts of violation within the activities.
The three major concerns are offering premiums to the employees for each order of DME
from the subsidiary company, offering rebates to patients who are using the equipments and
paying agency personnel for assisting the patents while using the equipments. It has been also
found that from the corporate perspective the owners and the authority of the hospital have to
be more careful about the business compliance and public service based regulations at the
time of value exchange operation. At the same time, Management Service Organisations
should directly communicate with the management board of the subsidiary company while
making them aware of these misconducts in healthcare provision. On the other hand, Hospital
and physician groups from joint-venture partnership, has equal responsibilities to maintain
the integrated supply management and facilitation system as well. Moreover, all the
responsible personnel and employees have to play individual role to eliminate these
misconducts that violate the Referral Fee Law.
7REGULATORY ENVIRONMENT IN HEALTHCARE
Reference
Clemente, S., McGrady, R., Repass, R., Paul III, D. P., & Coustasse, A. (2018). Medicare and
the affordable care act: fraud control efforts and results. International Journal of
Healthcare Management, 11(4), 356-362.
Ghebleh, S. (2017). No VIP treatment: ACOs should not get waiver protection from the
prohibition on beneficiary inducement. Vand. L. Rev., 70, 737.
Hamric, A. B. (2012, March). Empirical research on moral distress: issues, challenges, and
opportunities. In Hec Forum(Vol. 24, No. 1, pp. 39-49). Springer Netherlands.
Pathria, A. K., Allmon, A. L., De Traversay, J., Ianakiev, K. G., Suresh, N., & Tyler, M. K.
(2014). U.S. Patent No. 8,639,522. Washington, DC: U.S. Patent and Trademark
Office.
Pena, J. A., Larson, J. C., & O'Connor-Barnes, E. (2016). Parallel Investigations and
Prosecutions in Anti-Kickback Cases Involving Healthcare Providers. US Att'ys Bull.,
64, 47.
Runciman, B., Merry, A., & Walton, M. (2017). Safety and ethics in healthcare: a guide to
getting it right. CRC Press.
Schwartz, R. L., Furrow, B. R., Greaney, T. L., Johnson, S. H., & Stoltzfus Jost, T.
(2013). Health law: cases, materials and problems. West Academic Publishing.
Stowell, N. F., Schmidt, M., & Wadlinger, N. (2018). Healthcare fraud under the microscope:
improving its prevention. Journal of Financial Crime, (just-accepted), 00-00.
Reference
Clemente, S., McGrady, R., Repass, R., Paul III, D. P., & Coustasse, A. (2018). Medicare and
the affordable care act: fraud control efforts and results. International Journal of
Healthcare Management, 11(4), 356-362.
Ghebleh, S. (2017). No VIP treatment: ACOs should not get waiver protection from the
prohibition on beneficiary inducement. Vand. L. Rev., 70, 737.
Hamric, A. B. (2012, March). Empirical research on moral distress: issues, challenges, and
opportunities. In Hec Forum(Vol. 24, No. 1, pp. 39-49). Springer Netherlands.
Pathria, A. K., Allmon, A. L., De Traversay, J., Ianakiev, K. G., Suresh, N., & Tyler, M. K.
(2014). U.S. Patent No. 8,639,522. Washington, DC: U.S. Patent and Trademark
Office.
Pena, J. A., Larson, J. C., & O'Connor-Barnes, E. (2016). Parallel Investigations and
Prosecutions in Anti-Kickback Cases Involving Healthcare Providers. US Att'ys Bull.,
64, 47.
Runciman, B., Merry, A., & Walton, M. (2017). Safety and ethics in healthcare: a guide to
getting it right. CRC Press.
Schwartz, R. L., Furrow, B. R., Greaney, T. L., Johnson, S. H., & Stoltzfus Jost, T.
(2013). Health law: cases, materials and problems. West Academic Publishing.
Stowell, N. F., Schmidt, M., & Wadlinger, N. (2018). Healthcare fraud under the microscope:
improving its prevention. Journal of Financial Crime, (just-accepted), 00-00.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.
