Cross-Sectional Survey: Vaccine Perception and Leaders' Influence
VerifiedAdded on 2022/09/14
|8
|7303
|16
Report
AI Summary
This report presents the findings of a cross-sectional survey conducted in Australia, investigating the influence of political and medical leaders on parental perceptions of vaccination. The study aimed to understand how messages from figures like Donald Trump, Pauline Hanson, and Michael Gannon impact parents' attitudes towards childhood immunizations. Participants were categorized as having 'fixed' or 'susceptible' views on vaccination. The results indicated that susceptible parents, who constituted a majority of the sample, were more likely to report a change in their willingness to vaccinate after viewing vaccine-related messages, regardless of the message's content. Furthermore, susceptible parents showed increased vaccine hesitancy after viewing negative messages. The study highlights the importance of understanding parental susceptibility to vaccine messaging and suggests categorizing parents as 'fixed-view' or 'susceptible' can be a useful strategy for designing and implementing future vaccine promotion interventions.
1Zhang EJ, et al. BMJ Open 2019;9:e025866. doi:10.1136/bmjopen-2018-025866
Open access
Influence of political and medical
leaders on parental perception of
vaccination: a cross-sectional survey
in Australia
Elissa J Zhang,1 Abrar Ahmad Chughtai,1 Anita Heywood,1
Chandini Raina MacIntyre1,2
To cite: Zhang EJ, Chughtai AA,
Heywood A, et al. Influence of
political and medical leaders
on parental perception of
vaccination: a cross-sectional
survey in Australia. BMJ Open
2019;9:e025866. doi:10.1136/
bmjopen-2018-025866
► Prepublication history and
additional material for this
paper are available online. To
view these files, please visit
the journal online (http:// dx. doi.
org/10. 1136/bmjopen- 2018-
025866).
Received 24 August 2018
Revised 13 January 2019
Accepted 14 February 2019
1School of Public Health and
Community Medicine, UNSW
Medicine, University of New
South Wales, Sydney, New South
Wales, Australia
2Kirby Institute, University of
New South Wales, Sydney, New
South Wales, Australia
Correspondence to
Abrar Ahmad Chughtai;
abrar. chughtai@unsw. edu.au
Research
© Author(s) (or their
employer(s)) 2019. Re-use
permitted under CC BY-NC. No
commercial re-use. See rights
and permissions. Published by
BMJ.
AbstrACt
Objectives The aim of this survey was to investigate
parental vaccination attitudes and responses to vaccine-
related media messages from political and medical
leaders.
Design This was a cross-sectional study using a
semiquantitative questionnaire. Data were analysed using
descriptive statistics, X2 tests and logistic regression.
setting Data were collected from a web-based
questionnaire distributed in Australia by a market research
company in May of 2017.
Participants 411 participants with at least one child
under 5 were included in this study. The sample was
designed to be representative of Australia in terms of
gender and state of residence.
Primary and secondary outcome measures The
primary outcome measures were parental attitudes
towards childhood immunisation before and after viewing
vaccine-related messages from political and medical
leaders, including Donald Trump (USA), Pauline Hanson
(Australia) and Michael Gannon (Australia). Parents were
classified as having ‘susceptible’ (not fixed) or ‘fixed’
(positive or negative) views towards vaccination based on
a series of questions.
results Parents with fixed vaccination views constituted
23.8% (n=98) of the total sample; 21.7% (n=89) were
pro-vaccination and 2.2% (n=9) were anti-vaccination.
The remaining 76.2% of participants were classified as
having susceptible views towards vaccination. Susceptible
parents were more likely to report a change in their
willingness to vaccinate after watching vaccine-related
messages compared with fixed-view parents, regardless
of whether the messaging was positive or negative (Trump
OR 2.54, 95% CI (1.29 to 5.00); Hanson OR 2.64, 95% CI
(1.26 to 5.52); Gannon OR 2.64, 95% CI (1.26 to 5.52)).
Susceptible parents were more likely than fixed-view
parents to report increased vaccine hesitancy after viewing
negative vaccine messages (Trump OR 2.14, 95% CI (1.11
to 4.14), Hanson OR 2.34, 95% CI (1.21 to 4.50)).
Conclusions The findings suggest that most parents
including the vaccinating majorty are susceptible to
vaccine messaging from political and medical leaders.
Categorising parents as ‘fixed-view’ or ‘susceptible’ can
be a useful strategy for designing and implementing future
vaccine promotion interventions.
bACkgrOunD
Vaccines are one of the greatest successes
in public health1 but have been questioned
by prominent antivaccination celebrities in
the media2 3 contributing to vaccine-related
controversy and parental vaccine hesitancy.
The added voice of political leaders in the
media such as US President Donald Trump4
and Australian Senator Pauline Hanson5 may
have additional influence on parents, but
have not been studied.
Public figures ranging from media, sports
and political celebrities have used their
fame to direct media attention towards a
diverse range of health issues including
cancer screening and treatment, HIV disclo-
sure, drug addiction, multiple sclerosis and
Alzheimer’s disease,6–12 reducing stigma
and increasingawareness.Over a quarter
of parents indicated trust in vaccine-related
information from celebrities according to a
US study.13 Most celebrities are not formally
qualified or trained to deliver health commu-
nication and their personal experiences can
be misrepresented when broadcasted on a
population level.12 Some celebritieseven
strengths and limitations of this study
► This study used a novel method of classifying pa
ents as having either ‘fixed’ or ‘susceptible’ view
towards vaccination, rather than ‘acceptance’
‘refusal’.
► The study sample was representative of Aust
in terms of gender, state residence and country
birth.
► Data on participants’ socioeconomic status were
collected and the survey was only administered
English, so there may be some degree of bias.
► Proportion of fixed antivaccine parents was t
small to determine conclusions about the impact
media messages.
copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
Open access
Influence of political and medical
leaders on parental perception of
vaccination: a cross-sectional survey
in Australia
Elissa J Zhang,1 Abrar Ahmad Chughtai,1 Anita Heywood,1
Chandini Raina MacIntyre1,2
To cite: Zhang EJ, Chughtai AA,
Heywood A, et al. Influence of
political and medical leaders
on parental perception of
vaccination: a cross-sectional
survey in Australia. BMJ Open
2019;9:e025866. doi:10.1136/
bmjopen-2018-025866
► Prepublication history and
additional material for this
paper are available online. To
view these files, please visit
the journal online (http:// dx. doi.
org/10. 1136/bmjopen- 2018-
025866).
Received 24 August 2018
Revised 13 January 2019
Accepted 14 February 2019
1School of Public Health and
Community Medicine, UNSW
Medicine, University of New
South Wales, Sydney, New South
Wales, Australia
2Kirby Institute, University of
New South Wales, Sydney, New
South Wales, Australia
Correspondence to
Abrar Ahmad Chughtai;
abrar. chughtai@unsw. edu.au
Research
© Author(s) (or their
employer(s)) 2019. Re-use
permitted under CC BY-NC. No
commercial re-use. See rights
and permissions. Published by
BMJ.
AbstrACt
Objectives The aim of this survey was to investigate
parental vaccination attitudes and responses to vaccine-
related media messages from political and medical
leaders.
Design This was a cross-sectional study using a
semiquantitative questionnaire. Data were analysed using
descriptive statistics, X2 tests and logistic regression.
setting Data were collected from a web-based
questionnaire distributed in Australia by a market research
company in May of 2017.
Participants 411 participants with at least one child
under 5 were included in this study. The sample was
designed to be representative of Australia in terms of
gender and state of residence.
Primary and secondary outcome measures The
primary outcome measures were parental attitudes
towards childhood immunisation before and after viewing
vaccine-related messages from political and medical
leaders, including Donald Trump (USA), Pauline Hanson
(Australia) and Michael Gannon (Australia). Parents were
classified as having ‘susceptible’ (not fixed) or ‘fixed’
(positive or negative) views towards vaccination based on
a series of questions.
results Parents with fixed vaccination views constituted
23.8% (n=98) of the total sample; 21.7% (n=89) were
pro-vaccination and 2.2% (n=9) were anti-vaccination.
The remaining 76.2% of participants were classified as
having susceptible views towards vaccination. Susceptible
parents were more likely to report a change in their
willingness to vaccinate after watching vaccine-related
messages compared with fixed-view parents, regardless
of whether the messaging was positive or negative (Trump
OR 2.54, 95% CI (1.29 to 5.00); Hanson OR 2.64, 95% CI
(1.26 to 5.52); Gannon OR 2.64, 95% CI (1.26 to 5.52)).
Susceptible parents were more likely than fixed-view
parents to report increased vaccine hesitancy after viewing
negative vaccine messages (Trump OR 2.14, 95% CI (1.11
to 4.14), Hanson OR 2.34, 95% CI (1.21 to 4.50)).
Conclusions The findings suggest that most parents
including the vaccinating majorty are susceptible to
vaccine messaging from political and medical leaders.
Categorising parents as ‘fixed-view’ or ‘susceptible’ can
be a useful strategy for designing and implementing future
vaccine promotion interventions.
bACkgrOunD
Vaccines are one of the greatest successes
in public health1 but have been questioned
by prominent antivaccination celebrities in
the media2 3 contributing to vaccine-related
controversy and parental vaccine hesitancy.
The added voice of political leaders in the
media such as US President Donald Trump4
and Australian Senator Pauline Hanson5 may
have additional influence on parents, but
have not been studied.
Public figures ranging from media, sports
and political celebrities have used their
fame to direct media attention towards a
diverse range of health issues including
cancer screening and treatment, HIV disclo-
sure, drug addiction, multiple sclerosis and
Alzheimer’s disease,6–12 reducing stigma
and increasingawareness.Over a quarter
of parents indicated trust in vaccine-related
information from celebrities according to a
US study.13 Most celebrities are not formally
qualified or trained to deliver health commu-
nication and their personal experiences can
be misrepresented when broadcasted on a
population level.12 Some celebritieseven
strengths and limitations of this study
► This study used a novel method of classifying pa
ents as having either ‘fixed’ or ‘susceptible’ view
towards vaccination, rather than ‘acceptance’
‘refusal’.
► The study sample was representative of Aust
in terms of gender, state residence and country
birth.
► Data on participants’ socioeconomic status were
collected and the survey was only administered
English, so there may be some degree of bias.
► Proportion of fixed antivaccine parents was t
small to determine conclusions about the impact
media messages.
copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
2 Zhang EJ, et al. BMJ Open 2019;9:e025866. doi:10.1136/bmjopen-201
Open access
actively condemn childhood vaccination, such as former
model Jenny McCarthy.2 3 Television host Katie Couric,
an established bowel cancer screening spokesperson,11
portrayed doubts14 about the safety of Human Papilloma-
virus Vaccine on her talk show.
As politicians both occupy media attention and have
the authority to direct public health policy on the
issue, their influence is potentially greater than that of
entertainment and sports celebrities. For example, the
mealses, mumps and rubella vaccine-autism controversy
sparked by the discredited Wakefield study15 in 2001 was
influenced when the UK prime minister at the time Tony
Blair refused to disclose the vaccination status of his own
child,16 contributing to parental anxiety and fear, and
impeding the efforts of public health officials.17
US President Trump’s call for a commissioninto
vaccine safety in early 2017 led by vaccine sceptics Robert
Kennedy Jr and Robert De Niro has concerned health
professionals around the world.18 In Australia, Senator
Pauline Hanson created controversyin March 2017
when she advised parents to disregard the advice of their
doctors and ‘do their own research’ into vaccine safety and
promoted a non-existent ‘vaccination reaction test’ which
she subsequently retracted.5 When such views are made
public, they are often countered by medical experts, yet
there is little research on the impact of political messages
and how best to ensure optimal public health messaging.
Parental vaccine hesitancy is well studied, and gener-
ally defined as a delay in acceptance or refusal of vacci-
nation despite availabilityof vaccination services.19
This definition encompasses parents with a spectrum
of vaccine-hesitant opinions, including those with fixed
antivaccinationviews,who generallydo not change
their opinions, and uncertain parents that are not
fully compliant with vaccine schedules but could be
persuaded to change.20 While WHO SAGE definition21
refers to parents who are fully or mostly compliant with
vaccine schedules but experience caution or uncertainty
in doing so, the emphasis of research and health inter-
vention is rather focused on those who refuse some or
all vaccines. These vaccinating parents nevertheless may
be influenced to doubt childhood vaccination and delay
or refuse vaccinations in the future and may still be
susceptible to negative vaccine messages.22 While health
promotion and intervention tend to focus on parents at
the hesitant end of the spectrum, it is currently unknown
how easily influenced the silent majority of vaccinating
parents are, whose continued compliance is necessary
for upholding effective vaccination coverage rates. Hesi-
tant but compliant parents in Australia are influenced by
vaccine-related events and news coverage, contributing
to complex unresolved concerns regarding the safety
of vaccines, and could potentially reduce their future
compliance accordingly.23 The aim of this survey was to
investigate parental vaccination attitudes and responses
to vaccine-related media messages from political and
medical leaders of all types of parents through an alter-
nate model of classifying parental vaccine opinions by
susceptibility to change rather than their behaviour o
vaccine refusal.
MethODs
This study was designed to measure parental attitudes at
baseline and following viewing of vaccine messaging from
public figures through a 15–20 min online questionnaire
of parents of children aged 0–5 years in Australia. Th
questions used in the online survey were formulated by th
authors of this paper to answer the research questions of
this paper and to obtain a range of qualitative and quanti-
tative data on parental attitudes towards childhood vacci-
nations and sociodemographic information. Short video
clips and corresponding transcripts of vaccine messages
from US President Donald Trump, Australian Senator
Pauline Hanson and head of the Australian Medical
Association Michael Gannon were then shown to partic-
ipants and responses collected. The first two message
(Trump, Hanson) questionedvaccinesafety,whereas
the last message (Gannon) affirmed vaccine safety (fo
transcripts, see online supplementary appendix 1). The
impact of these messages on parental willingness to vacc
nate and perception of vaccine safety was compared
against baseline views.
recruitment
A market research company Survey Sampling Interna-
tional was employed to randomly distribute the survey lin
to representative sample (see table 1) aged 18–60 years
stratified by gender and state/territory of residence from
a database of registered panel members (n=400 000)
Distribution of points redeemable for gift cards, cash out
or charity donation provided incentive.
A total of 1727 potential participants clicked on the
survey link. A total of 1316 of these participants had no
children or only had children over 5 years of age an
were ineligible; 411 parents comprised the final eligible
sample.
sample size calculation
The study was powered for a separate study, assessi
acceptanceof a new vaccine policy. Assuming50%
support for vaccination, 385 participants were required,
with alpha=0.05 and power of 80%. The study aimed to
recruit 400 participants, with sampling designed to be
proportionate to the population of states and territories
in Australia.
Analysis
Descriptive analysis was conducted on the responses from
the population survey. Influences on parental vaccina-
tion attitudes (eg, doctors, health professionals, personal
experiences,familial/friend advice, media/internet)
were determined prior to exposure to political media
messages (see online supplementary appendix 2). X2
test and OR were used to evaluate the change in parental
views following exposure to vaccine messages from t
copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
Open access
actively condemn childhood vaccination, such as former
model Jenny McCarthy.2 3 Television host Katie Couric,
an established bowel cancer screening spokesperson,11
portrayed doubts14 about the safety of Human Papilloma-
virus Vaccine on her talk show.
As politicians both occupy media attention and have
the authority to direct public health policy on the
issue, their influence is potentially greater than that of
entertainment and sports celebrities. For example, the
mealses, mumps and rubella vaccine-autism controversy
sparked by the discredited Wakefield study15 in 2001 was
influenced when the UK prime minister at the time Tony
Blair refused to disclose the vaccination status of his own
child,16 contributing to parental anxiety and fear, and
impeding the efforts of public health officials.17
US President Trump’s call for a commissioninto
vaccine safety in early 2017 led by vaccine sceptics Robert
Kennedy Jr and Robert De Niro has concerned health
professionals around the world.18 In Australia, Senator
Pauline Hanson created controversyin March 2017
when she advised parents to disregard the advice of their
doctors and ‘do their own research’ into vaccine safety and
promoted a non-existent ‘vaccination reaction test’ which
she subsequently retracted.5 When such views are made
public, they are often countered by medical experts, yet
there is little research on the impact of political messages
and how best to ensure optimal public health messaging.
Parental vaccine hesitancy is well studied, and gener-
ally defined as a delay in acceptance or refusal of vacci-
nation despite availabilityof vaccination services.19
This definition encompasses parents with a spectrum
of vaccine-hesitant opinions, including those with fixed
antivaccinationviews,who generallydo not change
their opinions, and uncertain parents that are not
fully compliant with vaccine schedules but could be
persuaded to change.20 While WHO SAGE definition21
refers to parents who are fully or mostly compliant with
vaccine schedules but experience caution or uncertainty
in doing so, the emphasis of research and health inter-
vention is rather focused on those who refuse some or
all vaccines. These vaccinating parents nevertheless may
be influenced to doubt childhood vaccination and delay
or refuse vaccinations in the future and may still be
susceptible to negative vaccine messages.22 While health
promotion and intervention tend to focus on parents at
the hesitant end of the spectrum, it is currently unknown
how easily influenced the silent majority of vaccinating
parents are, whose continued compliance is necessary
for upholding effective vaccination coverage rates. Hesi-
tant but compliant parents in Australia are influenced by
vaccine-related events and news coverage, contributing
to complex unresolved concerns regarding the safety
of vaccines, and could potentially reduce their future
compliance accordingly.23 The aim of this survey was to
investigate parental vaccination attitudes and responses
to vaccine-related media messages from political and
medical leaders of all types of parents through an alter-
nate model of classifying parental vaccine opinions by
susceptibility to change rather than their behaviour o
vaccine refusal.
MethODs
This study was designed to measure parental attitudes at
baseline and following viewing of vaccine messaging from
public figures through a 15–20 min online questionnaire
of parents of children aged 0–5 years in Australia. Th
questions used in the online survey were formulated by th
authors of this paper to answer the research questions of
this paper and to obtain a range of qualitative and quanti-
tative data on parental attitudes towards childhood vacci-
nations and sociodemographic information. Short video
clips and corresponding transcripts of vaccine messages
from US President Donald Trump, Australian Senator
Pauline Hanson and head of the Australian Medical
Association Michael Gannon were then shown to partic-
ipants and responses collected. The first two message
(Trump, Hanson) questionedvaccinesafety,whereas
the last message (Gannon) affirmed vaccine safety (fo
transcripts, see online supplementary appendix 1). The
impact of these messages on parental willingness to vacc
nate and perception of vaccine safety was compared
against baseline views.
recruitment
A market research company Survey Sampling Interna-
tional was employed to randomly distribute the survey lin
to representative sample (see table 1) aged 18–60 years
stratified by gender and state/territory of residence from
a database of registered panel members (n=400 000)
Distribution of points redeemable for gift cards, cash out
or charity donation provided incentive.
A total of 1727 potential participants clicked on the
survey link. A total of 1316 of these participants had no
children or only had children over 5 years of age an
were ineligible; 411 parents comprised the final eligible
sample.
sample size calculation
The study was powered for a separate study, assessi
acceptanceof a new vaccine policy. Assuming50%
support for vaccination, 385 participants were required,
with alpha=0.05 and power of 80%. The study aimed to
recruit 400 participants, with sampling designed to be
proportionate to the population of states and territories
in Australia.
Analysis
Descriptive analysis was conducted on the responses from
the population survey. Influences on parental vaccina-
tion attitudes (eg, doctors, health professionals, personal
experiences,familial/friend advice, media/internet)
were determined prior to exposure to political media
messages (see online supplementary appendix 2). X2
test and OR were used to evaluate the change in parental
views following exposure to vaccine messages from t
copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
3Zhang EJ, et al. BMJ Open 2019;9:e025866. doi:10.1136/bmjopen-2018-025866
Open access
selected three public figures. All analyses were performed
with IBM SPSS Statistics V.24.0.24
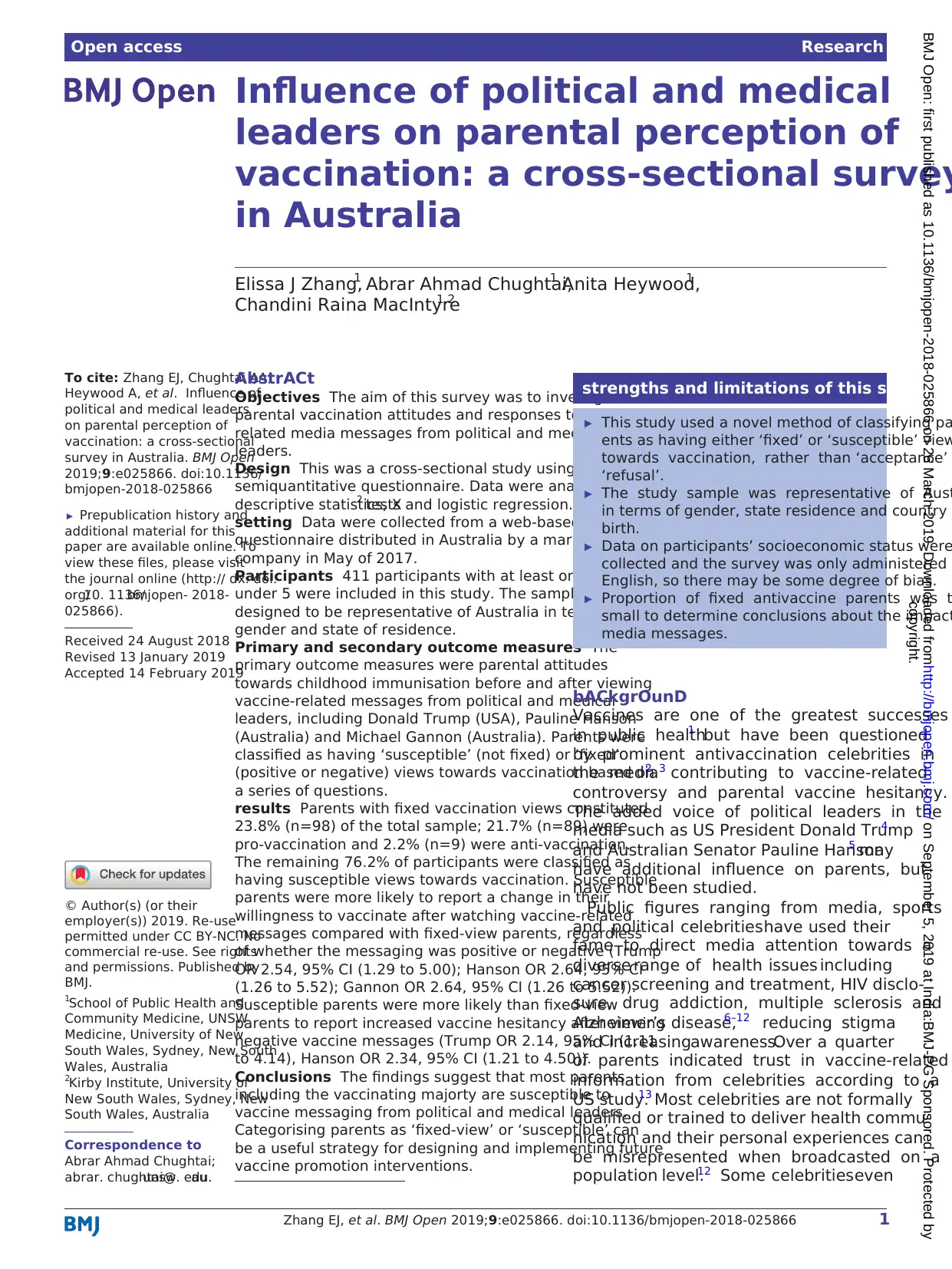
Parents were then categorised according to the fixed-
ness of their baseline vaccination views either for or
against into ‘fixed-view’ and ‘susceptible’ groups, the
rationale being that vaccine attitudes lie on a spectrum25
between complete baseline vaccine rejection and vaccine
acceptance, which we defined as fixed anti-vaccination
and pro-vaccination views (see figure 1). We defined
‘susceptible parents’ by excluding those who expresse
fixed vaccination views in the baseline questions,
including parents who expressed hesitancy or concern
towards vaccines. The remaining parents who did not
have firmly fixed views, even if they were fully vaccinating
we defined as ‘susceptible’. Parents were categorised a
fixed pro-vaccine or anti-vaccine based on their views of
childhood vaccination as ‘very important for children’ or
‘not important for children/risky for children’, respec-
tively, and these views not changing during the surve
The data from the quantitative survey were then inte
nally validated by checking against qualitative comments
in particular, the use of strong language like ‘never’ or
‘always’, and ensuring these were consistent with the cate
gorisation of fixed or susceptible by the agreement two
study authors (EJZ and AAC).
The influence of messaging from the selected public
figures on susceptibleparents was determined by
comparing their views at baseline with views after being
exposed to the messaging. The analysis first noted positiv
and negative change in willingness to vaccinate. Subs
quently, change in either direction was combined into
one single variable ‘change’ and unchanged positive or
negative pre-existing attitudes into a ‘no change’ variable
for further analysis. Closed-ended questions were asked
if the media messages presented in this survey increased
vaccine safety concerns, with optional open-ended elabo-
ration. The difference in response between the subgroups
was evaluated using p values from bivariate X2 analysis and
OR. Qualitative analysis was also performed by manually
collating optional open-ended responses regarding the
persuasiveness of the public figures.
Participant involvement
Parents were not involved in the design of this study.
results
Table 1 summarises the demographic characteristics o
the participants, compared against data from the Austra-
lian Bureau of Statistics.26 27The majority of participants
were aged 25–44 years old (n=314, 76.4%).
The percentage of parents born overseas (n=89, 21.7%)
in the sample is slightly less than the population propor-
tion of 28.5%. The majority of surveyed parents (n=327,
79.6%) had completed some form of tertiary education.
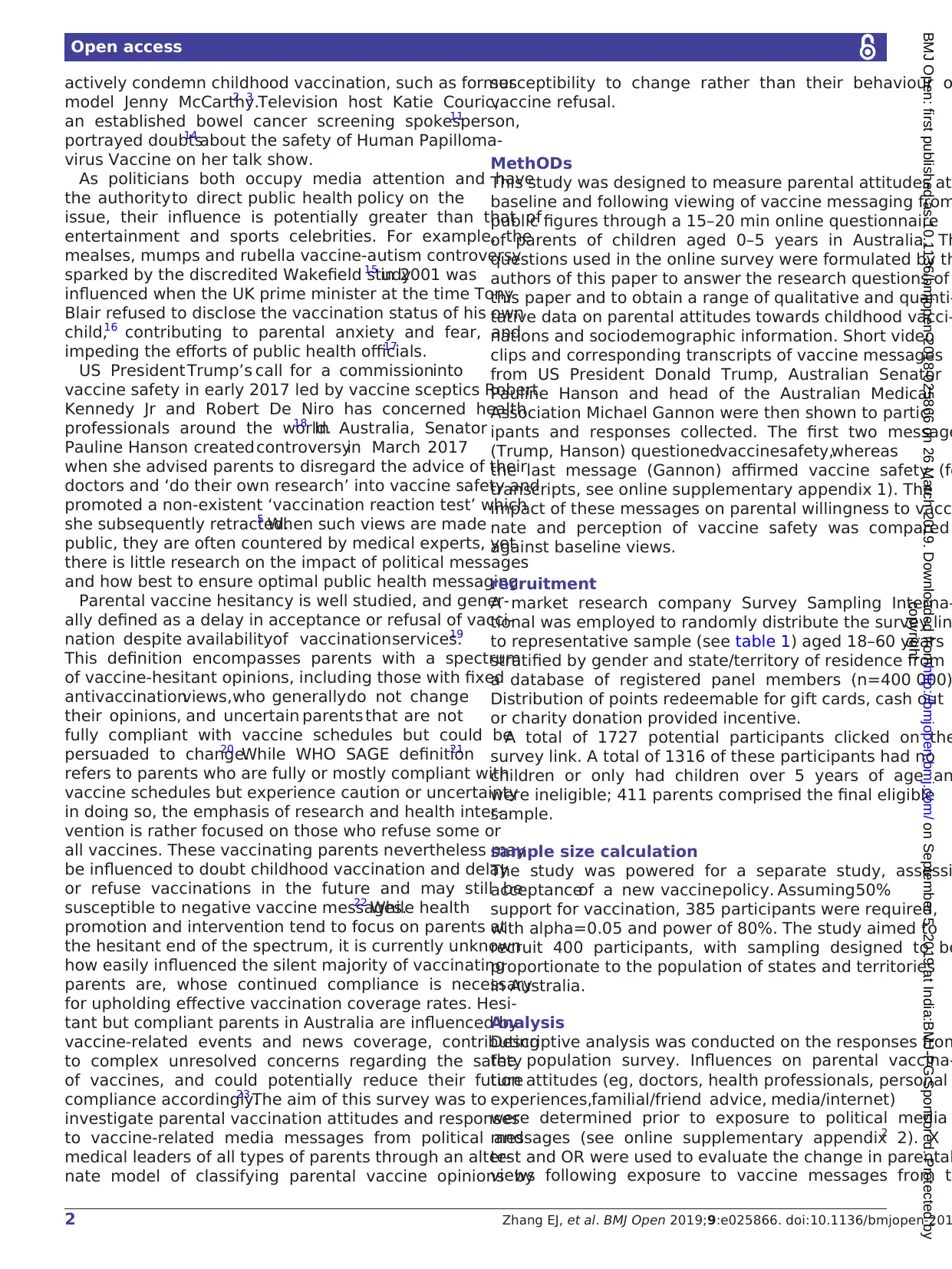
Most parents (88.6%) selected doctors as strong influ-
encers of their vaccination attitudes, and 20.2% of parent
were strongly influenced by the media and/or Internet
websites (figure 2).
Parents with fixed vaccination views constituted
23.8% (n=98/411) of the total sample − 89/411 were
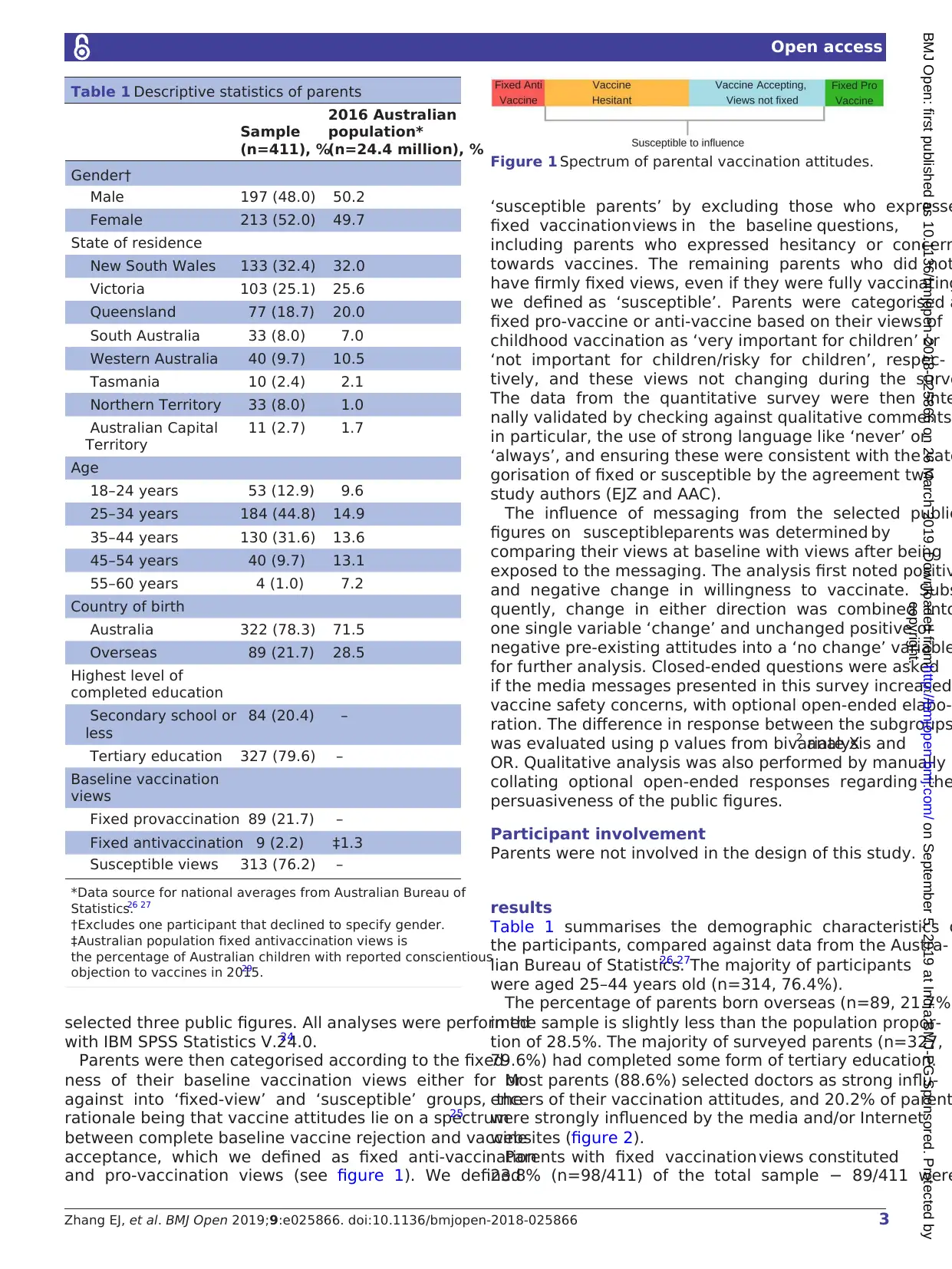
Table 1 Descriptive statistics of parents
Sample
(n=411), %
2016 Australian
population*
(n=24.4 million), %
Gender†
Male 197 (48.0) 50.2
Female 213 (52.0) 49.7
State of residence
New South Wales 133 (32.4) 32.0
Victoria 103 (25.1) 25.6
Queensland 77 (18.7) 20.0
South Australia 33 (8.0) 7.0
Western Australia 40 (9.7) 10.5
Tasmania 10 (2.4) 2.1
Northern Territory 33 (8.0) 1.0
Australian Capital
Territory
11 (2.7) 1.7
Age
18–24 years 53 (12.9) 9.6
25–34 years 184 (44.8) 14.9
35–44 years 130 (31.6) 13.6
45–54 years 40 (9.7) 13.1
55–60 years 4 (1.0) 7.2
Country of birth
Australia 322 (78.3) 71.5
Overseas 89 (21.7) 28.5
Highest level of
completed education
Secondary school or
less
84 (20.4) –
Tertiary education 327 (79.6) –
Baseline vaccination
views
Fixed provaccination 89 (21.7) –
Fixed antivaccination 9 (2.2) ‡1.3
Susceptible views 313 (76.2) –
*Data source for national averages from Australian Bureau of
Statistics.26 27
†Excludes one participant that declined to specify gender.
‡Australian population fixed antivaccination views is
the percentage of Australian children with reported conscientious
objection to vaccines in 2015.29
Figure 1 Spectrum of parental vaccination attitudes.
copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
Open access
selected three public figures. All analyses were performed
with IBM SPSS Statistics V.24.0.24
Parents were then categorised according to the fixed-
ness of their baseline vaccination views either for or
against into ‘fixed-view’ and ‘susceptible’ groups, the
rationale being that vaccine attitudes lie on a spectrum25
between complete baseline vaccine rejection and vaccine
acceptance, which we defined as fixed anti-vaccination
and pro-vaccination views (see figure 1). We defined
‘susceptible parents’ by excluding those who expresse
fixed vaccination views in the baseline questions,
including parents who expressed hesitancy or concern
towards vaccines. The remaining parents who did not
have firmly fixed views, even if they were fully vaccinating
we defined as ‘susceptible’. Parents were categorised a
fixed pro-vaccine or anti-vaccine based on their views of
childhood vaccination as ‘very important for children’ or
‘not important for children/risky for children’, respec-
tively, and these views not changing during the surve
The data from the quantitative survey were then inte
nally validated by checking against qualitative comments
in particular, the use of strong language like ‘never’ or
‘always’, and ensuring these were consistent with the cate
gorisation of fixed or susceptible by the agreement two
study authors (EJZ and AAC).
The influence of messaging from the selected public
figures on susceptibleparents was determined by
comparing their views at baseline with views after being
exposed to the messaging. The analysis first noted positiv
and negative change in willingness to vaccinate. Subs
quently, change in either direction was combined into
one single variable ‘change’ and unchanged positive or
negative pre-existing attitudes into a ‘no change’ variable
for further analysis. Closed-ended questions were asked
if the media messages presented in this survey increased
vaccine safety concerns, with optional open-ended elabo-
ration. The difference in response between the subgroups
was evaluated using p values from bivariate X2 analysis and
OR. Qualitative analysis was also performed by manually
collating optional open-ended responses regarding the
persuasiveness of the public figures.
Participant involvement
Parents were not involved in the design of this study.
results
Table 1 summarises the demographic characteristics o
the participants, compared against data from the Austra-
lian Bureau of Statistics.26 27The majority of participants
were aged 25–44 years old (n=314, 76.4%).
The percentage of parents born overseas (n=89, 21.7%)
in the sample is slightly less than the population propor-
tion of 28.5%. The majority of surveyed parents (n=327,
79.6%) had completed some form of tertiary education.
Most parents (88.6%) selected doctors as strong influ-
encers of their vaccination attitudes, and 20.2% of parent
were strongly influenced by the media and/or Internet
websites (figure 2).
Parents with fixed vaccination views constituted
23.8% (n=98/411) of the total sample − 89/411 were
Table 1 Descriptive statistics of parents
Sample
(n=411), %
2016 Australian
population*
(n=24.4 million), %
Gender†
Male 197 (48.0) 50.2
Female 213 (52.0) 49.7
State of residence
New South Wales 133 (32.4) 32.0
Victoria 103 (25.1) 25.6
Queensland 77 (18.7) 20.0
South Australia 33 (8.0) 7.0
Western Australia 40 (9.7) 10.5
Tasmania 10 (2.4) 2.1
Northern Territory 33 (8.0) 1.0
Australian Capital
Territory
11 (2.7) 1.7
Age
18–24 years 53 (12.9) 9.6
25–34 years 184 (44.8) 14.9
35–44 years 130 (31.6) 13.6
45–54 years 40 (9.7) 13.1
55–60 years 4 (1.0) 7.2
Country of birth
Australia 322 (78.3) 71.5
Overseas 89 (21.7) 28.5
Highest level of
completed education
Secondary school or
less
84 (20.4) –
Tertiary education 327 (79.6) –
Baseline vaccination
views
Fixed provaccination 89 (21.7) –
Fixed antivaccination 9 (2.2) ‡1.3
Susceptible views 313 (76.2) –
*Data source for national averages from Australian Bureau of
Statistics.26 27
†Excludes one participant that declined to specify gender.
‡Australian population fixed antivaccination views is
the percentage of Australian children with reported conscientious
objection to vaccines in 2015.29
Figure 1 Spectrum of parental vaccination attitudes.
copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
4 Zhang EJ, et al. BMJ Open 2019;9:e025866. doi:10.1136/bmjopen-201
Open access
pro-vaccination and 9/411 were anti-vaccination. The
remaining 313 parents (76.2%) were defined as suscep-
tible. There were no significantdifferencesbetween
fixed-view and susceptible parents with regard to the
demographic characteristics of gender (p=0.544), age
(p=0.299), country of birth (p=0.827) and education
(p=0.247).
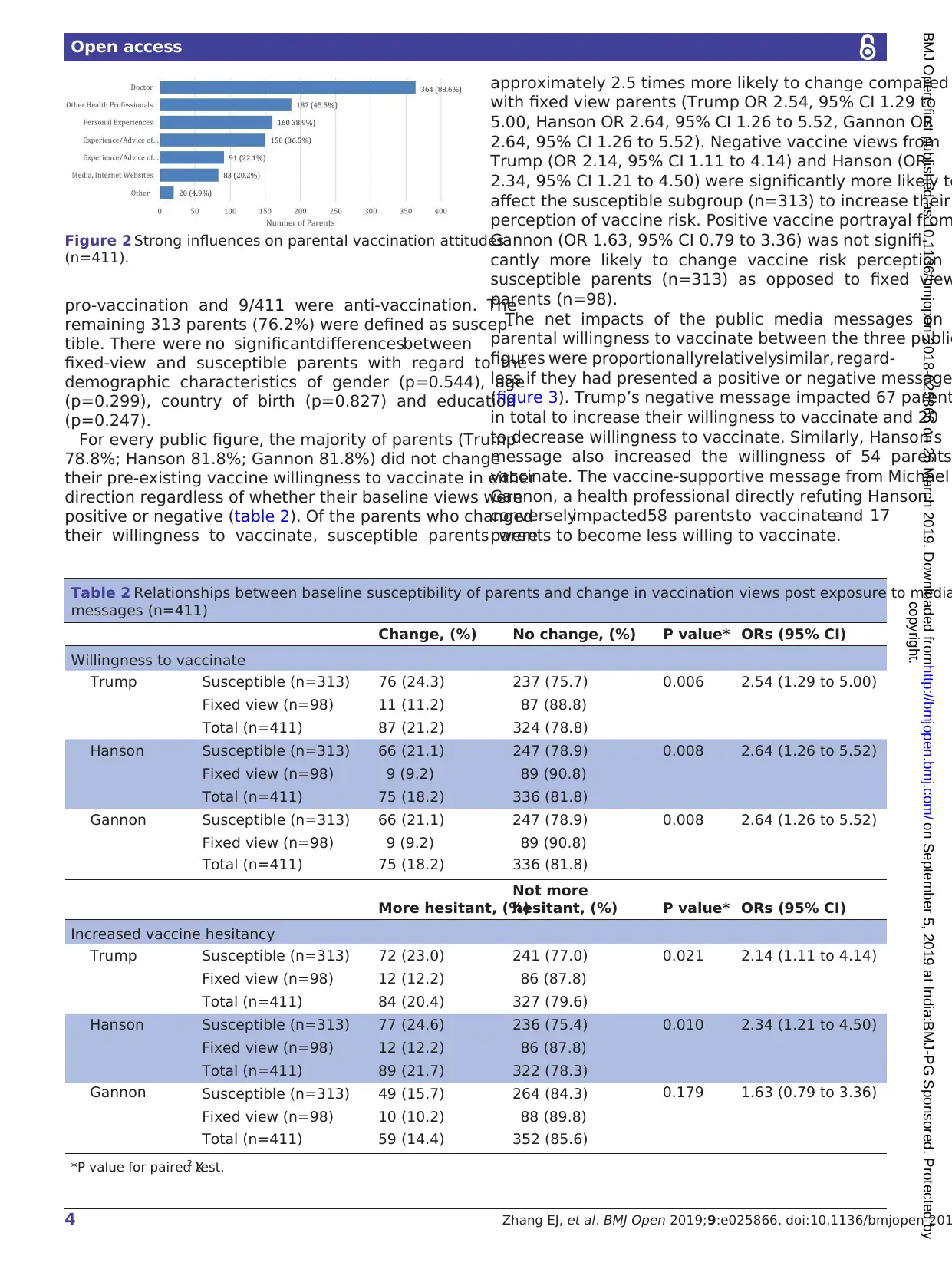
For every public figure, the majority of parents (Trump
78.8%; Hanson 81.8%; Gannon 81.8%) did not change
their pre-existing vaccine willingness to vaccinate in either
direction regardless of whether their baseline views were
positive or negative (table 2). Of the parents who changed
their willingness to vaccinate, susceptible parents were
approximately 2.5 times more likely to change compared
with fixed view parents (Trump OR 2.54, 95% CI 1.29 to
5.00, Hanson OR 2.64, 95% CI 1.26 to 5.52, Gannon OR
2.64, 95% CI 1.26 to 5.52). Negative vaccine views from
Trump (OR 2.14, 95% CI 1.11 to 4.14) and Hanson (OR
2.34, 95% CI 1.21 to 4.50) were significantly more likely to
affect the susceptible subgroup (n=313) to increase their
perception of vaccine risk. Positive vaccine portrayal from
Gannon (OR 1.63, 95% CI 0.79 to 3.36) was not signifi-
cantly more likely to change vaccine risk perception
susceptible parents (n=313) as opposed to fixed view
parents (n=98).
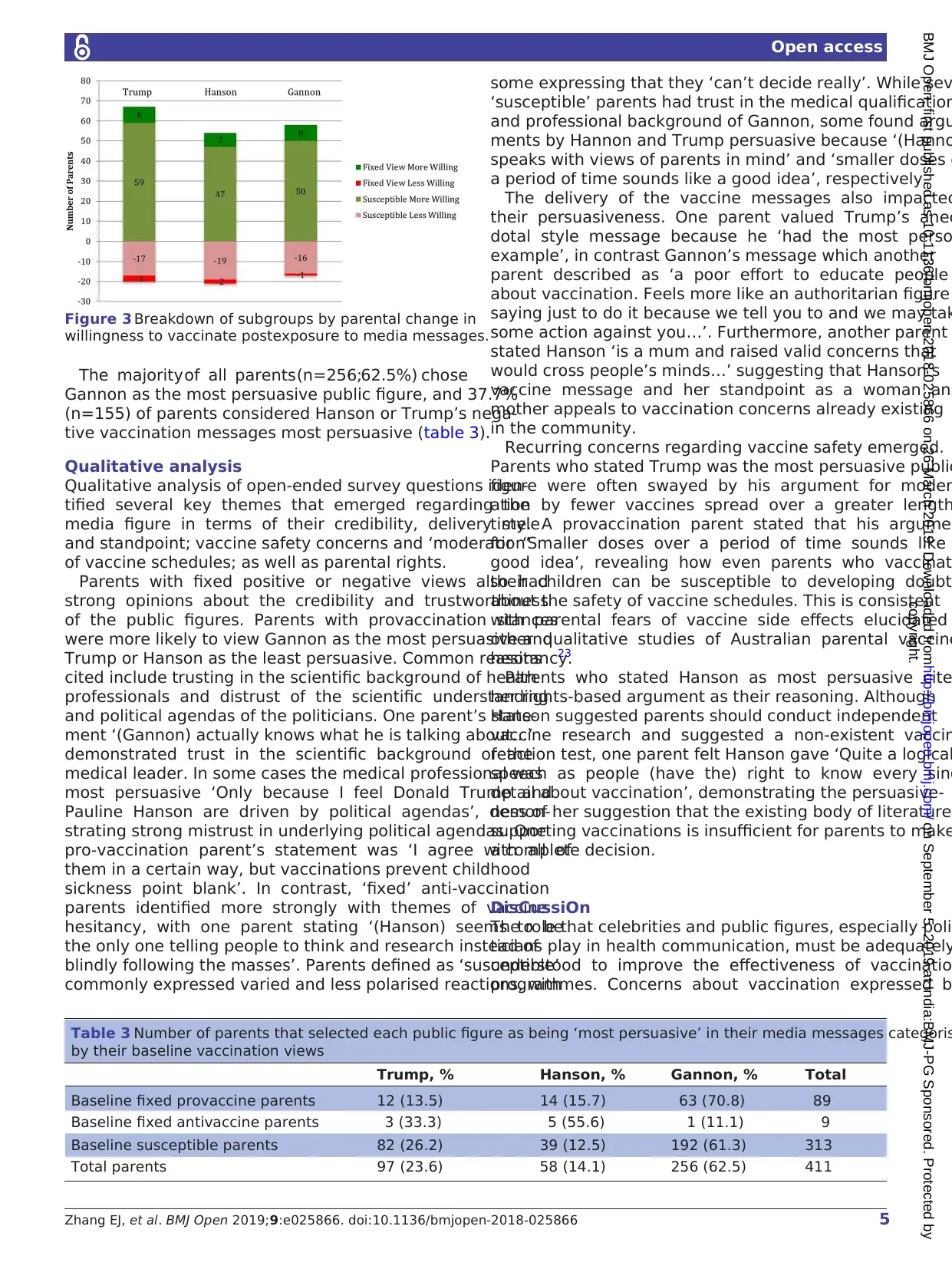
The net impacts of the public media messages on
parental willingness to vaccinate between the three public
figures were proportionallyrelativelysimilar, regard-
less if they had presented a positive or negative message
(figure 3). Trump’s negative message impacted 67 parent
in total to increase their willingness to vaccinate and 20
to decrease willingness to vaccinate. Similarly, Hanson’s
message also increased the willingness of 54 parents
vaccinate. The vaccine-supportive message from Michael
Gannon, a health professional directly refuting Hanson
converselyimpacted58 parents to vaccinateand 17
parents to become less willing to vaccinate.
Figure 2 Strong influences on parental vaccination attitudes
(n=411).
Table 2 Relationships between baseline susceptibility of parents and change in vaccination views post exposure to media
messages (n=411)
Change, (%) No change, (%) P value* ORs (95% CI)
Willingness to vaccinate
Trump Susceptible (n=313) 76 (24.3) 237 (75.7) 0.006 2.54 (1.29 to 5.00)
Fixed view (n=98) 11 (11.2) 87 (88.8)
Total (n=411) 87 (21.2) 324 (78.8)
Hanson Susceptible (n=313) 66 (21.1) 247 (78.9) 0.008 2.64 (1.26 to 5.52)
Fixed view (n=98) 9 (9.2) 89 (90.8)
Total (n=411) 75 (18.2) 336 (81.8)
Gannon Susceptible (n=313) 66 (21.1) 247 (78.9) 0.008 2.64 (1.26 to 5.52)
Fixed view (n=98) 9 (9.2) 89 (90.8)
Total (n=411) 75 (18.2) 336 (81.8)
More hesitant, (%)
Not more
hesitant, (%) P value* ORs (95% CI)
Increased vaccine hesitancy
Trump Susceptible (n=313) 72 (23.0) 241 (77.0) 0.021 2.14 (1.11 to 4.14)
Fixed view (n=98) 12 (12.2) 86 (87.8)
Total (n=411) 84 (20.4) 327 (79.6)
Hanson Susceptible (n=313) 77 (24.6) 236 (75.4) 0.010 2.34 (1.21 to 4.50)
Fixed view (n=98) 12 (12.2) 86 (87.8)
Total (n=411) 89 (21.7) 322 (78.3)
Gannon Susceptible (n=313) 49 (15.7) 264 (84.3) 0.179 1.63 (0.79 to 3.36)
Fixed view (n=98) 10 (10.2) 88 (89.8)
Total (n=411) 59 (14.4) 352 (85.6)
*P value for paired X2 test.
copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
Open access
pro-vaccination and 9/411 were anti-vaccination. The
remaining 313 parents (76.2%) were defined as suscep-
tible. There were no significantdifferencesbetween
fixed-view and susceptible parents with regard to the
demographic characteristics of gender (p=0.544), age
(p=0.299), country of birth (p=0.827) and education
(p=0.247).
For every public figure, the majority of parents (Trump
78.8%; Hanson 81.8%; Gannon 81.8%) did not change
their pre-existing vaccine willingness to vaccinate in either
direction regardless of whether their baseline views were
positive or negative (table 2). Of the parents who changed
their willingness to vaccinate, susceptible parents were
approximately 2.5 times more likely to change compared
with fixed view parents (Trump OR 2.54, 95% CI 1.29 to
5.00, Hanson OR 2.64, 95% CI 1.26 to 5.52, Gannon OR
2.64, 95% CI 1.26 to 5.52). Negative vaccine views from
Trump (OR 2.14, 95% CI 1.11 to 4.14) and Hanson (OR
2.34, 95% CI 1.21 to 4.50) were significantly more likely to
affect the susceptible subgroup (n=313) to increase their
perception of vaccine risk. Positive vaccine portrayal from
Gannon (OR 1.63, 95% CI 0.79 to 3.36) was not signifi-
cantly more likely to change vaccine risk perception
susceptible parents (n=313) as opposed to fixed view
parents (n=98).
The net impacts of the public media messages on
parental willingness to vaccinate between the three public
figures were proportionallyrelativelysimilar, regard-
less if they had presented a positive or negative message
(figure 3). Trump’s negative message impacted 67 parent
in total to increase their willingness to vaccinate and 20
to decrease willingness to vaccinate. Similarly, Hanson’s
message also increased the willingness of 54 parents
vaccinate. The vaccine-supportive message from Michael
Gannon, a health professional directly refuting Hanson
converselyimpacted58 parents to vaccinateand 17
parents to become less willing to vaccinate.
Figure 2 Strong influences on parental vaccination attitudes
(n=411).
Table 2 Relationships between baseline susceptibility of parents and change in vaccination views post exposure to media
messages (n=411)
Change, (%) No change, (%) P value* ORs (95% CI)
Willingness to vaccinate
Trump Susceptible (n=313) 76 (24.3) 237 (75.7) 0.006 2.54 (1.29 to 5.00)
Fixed view (n=98) 11 (11.2) 87 (88.8)
Total (n=411) 87 (21.2) 324 (78.8)
Hanson Susceptible (n=313) 66 (21.1) 247 (78.9) 0.008 2.64 (1.26 to 5.52)
Fixed view (n=98) 9 (9.2) 89 (90.8)
Total (n=411) 75 (18.2) 336 (81.8)
Gannon Susceptible (n=313) 66 (21.1) 247 (78.9) 0.008 2.64 (1.26 to 5.52)
Fixed view (n=98) 9 (9.2) 89 (90.8)
Total (n=411) 75 (18.2) 336 (81.8)
More hesitant, (%)
Not more
hesitant, (%) P value* ORs (95% CI)
Increased vaccine hesitancy
Trump Susceptible (n=313) 72 (23.0) 241 (77.0) 0.021 2.14 (1.11 to 4.14)
Fixed view (n=98) 12 (12.2) 86 (87.8)
Total (n=411) 84 (20.4) 327 (79.6)
Hanson Susceptible (n=313) 77 (24.6) 236 (75.4) 0.010 2.34 (1.21 to 4.50)
Fixed view (n=98) 12 (12.2) 86 (87.8)
Total (n=411) 89 (21.7) 322 (78.3)
Gannon Susceptible (n=313) 49 (15.7) 264 (84.3) 0.179 1.63 (0.79 to 3.36)
Fixed view (n=98) 10 (10.2) 88 (89.8)
Total (n=411) 59 (14.4) 352 (85.6)
*P value for paired X2 test.
copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
5Zhang EJ, et al. BMJ Open 2019;9:e025866. doi:10.1136/bmjopen-2018-025866
Open access
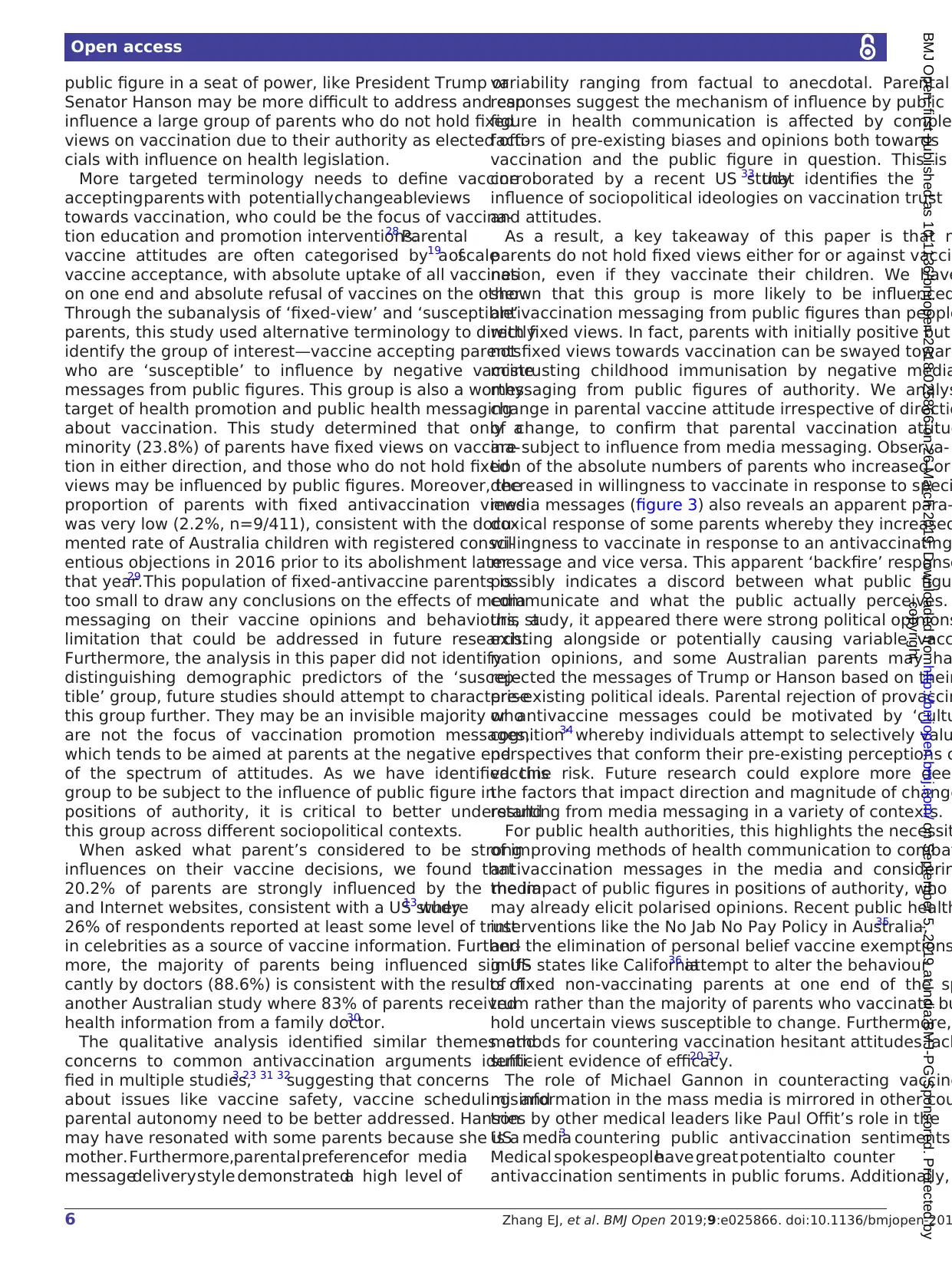
The majority of all parents (n=256;62.5%) chose
Gannon as the most persuasive public figure, and 37.7%
(n=155) of parents considered Hanson or Trump’s nega-
tive vaccination messages most persuasive (table 3).
Qualitative analysis
Qualitative analysis of open-ended survey questions iden-
tified several key themes that emerged regarding the
media figure in terms of their credibility, delivery style
and standpoint; vaccine safety concerns and ‘moderation’
of vaccine schedules; as well as parental rights.
Parents with fixed positive or negative views also had
strong opinions about the credibility and trustworthiness
of the public figures. Parents with provaccination stances
were more likely to view Gannon as the most persuasive and
Trump or Hanson as the least persuasive. Common reasons
cited include trusting in the scientific background of health
professionals and distrust of the scientific understanding
and political agendas of the politicians. One parent’s state-
ment ‘(Gannon) actually knows what he is talking about…’
demonstrated trust in the scientific background of the
medical leader. In some cases the medical professional was
most persuasive ‘Only because I feel Donald Trump and
Pauline Hanson are driven by political agendas’, demon-
strating strong mistrust in underlying political agendas. One
pro-vaccination parent’s statement was ‘I agree with all of
them in a certain way, but vaccinations prevent childhood
sickness point blank’. In contrast, ‘fixed’ anti-vaccination
parents identified more strongly with themes of vaccine
hesitancy, with one parent stating ‘(Hanson) seems to be
the only one telling people to think and research instead of
blindly following the masses’. Parents defined as ‘susceptible’
commonly expressed varied and less polarised reactions, with
some expressing that they ‘can’t decide really’. While sev
‘susceptible’ parents had trust in the medical qualification
and professional background of Gannon, some found argu
ments by Hannon and Trump persuasive because ‘(Hanno
speaks with views of parents in mind’ and ‘smaller doses o
a period of time sounds like a good idea’, respectively.
The delivery of the vaccine messages also impacted
their persuasiveness. One parent valued Trump’s anec
dotal style message because he ‘had the most perso
example’, in contrast Gannon’s message which another
parent described as ‘a poor effort to educate people
about vaccination. Feels more like an authoritarian figure
saying just to do it because we tell you to and we may tak
some action against you…’. Furthermore, another parent
stated Hanson ‘is a mum and raised valid concerns that
would cross people’s minds…’ suggesting that Hanson’s
vaccine message and her standpoint as a woman and
mother appeals to vaccination concerns already existing
in the community.
Recurring concerns regarding vaccine safety emerged.
Parents who stated Trump was the most persuasive public
figure were often swayed by his argument for moder
ation by fewer vaccines spread over a greater length
time. A provaccination parent stated that his argumen
for ‘Smaller doses over a period of time sounds like
good idea’, revealing how even parents who vaccinat
their children can be susceptible to developing doubt
about the safety of vaccine schedules. This is consistent
with parental fears of vaccine side effects elucidated
other qualitative studies of Australian parental vaccine
hesitancy.23
Parents who stated Hanson as most persuasive cite
her rights-based argument as their reasoning. Although
Hanson suggested parents should conduct independent
vaccine research and suggested a non-existent vaccin
reaction test, one parent felt Hanson gave ‘Quite a logical
speech as people (have the) right to know every sing
detail about vaccination’, demonstrating the persuasive-
ness of her suggestion that the existing body of literature
supporting vaccinations is insufficient for parents to make
a complete decision.
DisCussiOn
The role that celebrities and public figures, especially poli
ticians play in health communication, must be adequately
understood to improve the effectiveness of vaccinatio
programmes. Concerns about vaccination expressed b
Figure 3 Breakdown of subgroups by parental change in
willingness to vaccinate postexposure to media messages.
Table 3 Number of parents that selected each public figure as being ‘most persuasive’ in their media messages categoris
by their baseline vaccination views
Trump, % Hanson, % Gannon, % Total
Baseline fixed provaccine parents 12 (13.5) 14 (15.7) 63 (70.8) 89
Baseline fixed antivaccine parents 3 (33.3) 5 (55.6) 1 (11.1) 9
Baseline susceptible parents 82 (26.2) 39 (12.5) 192 (61.3) 313
Total parents 97 (23.6) 58 (14.1) 256 (62.5) 411
copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
Open access
The majority of all parents (n=256;62.5%) chose
Gannon as the most persuasive public figure, and 37.7%
(n=155) of parents considered Hanson or Trump’s nega-
tive vaccination messages most persuasive (table 3).
Qualitative analysis
Qualitative analysis of open-ended survey questions iden-
tified several key themes that emerged regarding the
media figure in terms of their credibility, delivery style
and standpoint; vaccine safety concerns and ‘moderation’
of vaccine schedules; as well as parental rights.
Parents with fixed positive or negative views also had
strong opinions about the credibility and trustworthiness
of the public figures. Parents with provaccination stances
were more likely to view Gannon as the most persuasive and
Trump or Hanson as the least persuasive. Common reasons
cited include trusting in the scientific background of health
professionals and distrust of the scientific understanding
and political agendas of the politicians. One parent’s state-
ment ‘(Gannon) actually knows what he is talking about…’
demonstrated trust in the scientific background of the
medical leader. In some cases the medical professional was
most persuasive ‘Only because I feel Donald Trump and
Pauline Hanson are driven by political agendas’, demon-
strating strong mistrust in underlying political agendas. One
pro-vaccination parent’s statement was ‘I agree with all of
them in a certain way, but vaccinations prevent childhood
sickness point blank’. In contrast, ‘fixed’ anti-vaccination
parents identified more strongly with themes of vaccine
hesitancy, with one parent stating ‘(Hanson) seems to be
the only one telling people to think and research instead of
blindly following the masses’. Parents defined as ‘susceptible’
commonly expressed varied and less polarised reactions, with
some expressing that they ‘can’t decide really’. While sev
‘susceptible’ parents had trust in the medical qualification
and professional background of Gannon, some found argu
ments by Hannon and Trump persuasive because ‘(Hanno
speaks with views of parents in mind’ and ‘smaller doses o
a period of time sounds like a good idea’, respectively.
The delivery of the vaccine messages also impacted
their persuasiveness. One parent valued Trump’s anec
dotal style message because he ‘had the most perso
example’, in contrast Gannon’s message which another
parent described as ‘a poor effort to educate people
about vaccination. Feels more like an authoritarian figure
saying just to do it because we tell you to and we may tak
some action against you…’. Furthermore, another parent
stated Hanson ‘is a mum and raised valid concerns that
would cross people’s minds…’ suggesting that Hanson’s
vaccine message and her standpoint as a woman and
mother appeals to vaccination concerns already existing
in the community.
Recurring concerns regarding vaccine safety emerged.
Parents who stated Trump was the most persuasive public
figure were often swayed by his argument for moder
ation by fewer vaccines spread over a greater length
time. A provaccination parent stated that his argumen
for ‘Smaller doses over a period of time sounds like
good idea’, revealing how even parents who vaccinat
their children can be susceptible to developing doubt
about the safety of vaccine schedules. This is consistent
with parental fears of vaccine side effects elucidated
other qualitative studies of Australian parental vaccine
hesitancy.23
Parents who stated Hanson as most persuasive cite
her rights-based argument as their reasoning. Although
Hanson suggested parents should conduct independent
vaccine research and suggested a non-existent vaccin
reaction test, one parent felt Hanson gave ‘Quite a logical
speech as people (have the) right to know every sing
detail about vaccination’, demonstrating the persuasive-
ness of her suggestion that the existing body of literature
supporting vaccinations is insufficient for parents to make
a complete decision.
DisCussiOn
The role that celebrities and public figures, especially poli
ticians play in health communication, must be adequately
understood to improve the effectiveness of vaccinatio
programmes. Concerns about vaccination expressed b
Figure 3 Breakdown of subgroups by parental change in
willingness to vaccinate postexposure to media messages.
Table 3 Number of parents that selected each public figure as being ‘most persuasive’ in their media messages categoris
by their baseline vaccination views
Trump, % Hanson, % Gannon, % Total
Baseline fixed provaccine parents 12 (13.5) 14 (15.7) 63 (70.8) 89
Baseline fixed antivaccine parents 3 (33.3) 5 (55.6) 1 (11.1) 9
Baseline susceptible parents 82 (26.2) 39 (12.5) 192 (61.3) 313
Total parents 97 (23.6) 58 (14.1) 256 (62.5) 411
copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
6 Zhang EJ, et al. BMJ Open 2019;9:e025866. doi:10.1136/bmjopen-201
Open access
public figure in a seat of power, like President Trump or
Senator Hanson may be more difficult to address and can
influence a large group of parents who do not hold fixed
views on vaccination due to their authority as elected offi-
cials with influence on health legislation.
More targeted terminology needs to define vaccine
accepting parents with potentially changeableviews
towards vaccination, who could be the focus of vaccina-
tion education and promotion interventions.28 Parental
vaccine attitudes are often categorised by a scale19 of
vaccine acceptance, with absolute uptake of all vaccines
on one end and absolute refusal of vaccines on the other.
Through the subanalysis of ‘fixed-view’ and ‘susceptible’
parents, this study used alternative terminology to directly
identify the group of interest—vaccine accepting parents
who are ‘susceptible’ to influence by negative vaccine
messages from public figures. This group is also a worthy
target of health promotion and public health messaging
about vaccination. This study determined that only a
minority (23.8%) of parents have fixed views on vaccina-
tion in either direction, and those who do not hold fixed
views may be influenced by public figures. Moreover, the
proportion of parents with fixed antivaccination views
was very low (2.2%, n=9/411), consistent with the docu-
mented rate of Australia children with registered consci-
entious objections in 2016 prior to its abolishment later
that year.29 This population of fixed-antivaccine parents is
too small to draw any conclusions on the effects of media
messaging on their vaccine opinions and behaviours, a
limitation that could be addressed in future research.
Furthermore, the analysis in this paper did not identify
distinguishing demographic predictors of the ‘suscep-
tible’ group, future studies should attempt to characterise
this group further. They may be an invisible majority who
are not the focus of vaccination promotion messages,
which tends to be aimed at parents at the negative end
of the spectrum of attitudes. As we have identified this
group to be subject to the influence of public figure in
positions of authority, it is critical to better understand
this group across different sociopolitical contexts.
When asked what parent’s considered to be strong
influences on their vaccine decisions, we found that
20.2% of parents are strongly influenced by the media
and Internet websites, consistent with a US study13 where
26% of respondents reported at least some level of trust
in celebrities as a source of vaccine information. Further-
more, the majority of parents being influenced signifi-
cantly by doctors (88.6%) is consistent with the results of
another Australian study where 83% of parents received
health information from a family doctor.30
The qualitative analysis identified similar themes and
concerns to common antivaccination arguments identi-
fied in multiple studies,3 23 31 32
suggesting that concerns
about issues like vaccine safety, vaccine scheduling and
parental autonomy need to be better addressed. Hanson
may have resonated with some parents because she is a
mother. Furthermore,parental preferencefor media
messagedelivery style demonstrateda high level of
variability ranging from factual to anecdotal. Parental
responses suggest the mechanism of influence by public
figure in health communication is affected by comple
factors of pre-existing biases and opinions both towards
vaccination and the public figure in question. This is
corroborated by a recent US study33 that identifies the
influence of sociopolitical ideologies on vaccination trust
and attitudes.
As a result, a key takeaway of this paper is that m
parents do not hold fixed views either for or against vacci
nation, even if they vaccinate their children. We have
shown that this group is more likely to be influenced
antivaccination messaging from public figures than people
with fixed views. In fact, parents with initially positive but
not fixed views towards vaccination can be swayed toward
mistrusting childhood immunisation by negative media
messaging from public figures of authority. We analys
change in parental vaccine attitude irrespective of directio
of change, to confirm that parental vaccination attitud
are subject to influence from media messaging. Observa-
tion of the absolute numbers of parents who increased or
decreased in willingness to vaccinate in response to speci
media messages (figure 3) also reveals an apparent para-
doxical response of some parents whereby they increased
willingness to vaccinate in response to an antivaccinating
message and vice versa. This apparent ‘backfire’ response
possibly indicates a discord between what public figu
communicate and what the public actually perceives.
this study, it appeared there were strong political opinions
existing alongside or potentially causing variable vacc
nation opinions, and some Australian parents may ha
rejected the messages of Trump or Hanson based on their
pre-existing political ideals. Parental rejection of provaccin
or antivaccine messages could be motivated by ‘cultu
cognition’34 whereby individuals attempt to selectively valu
perspectives that conform their pre-existing perceptions o
vaccine risk. Future research could explore more deep
the factors that impact direction and magnitude of change
resulting from media messaging in a variety of contexts.
For public health authorities, this highlights the necessit
of improving methods of health communication to combat
antivaccination messages in the media and considerin
the impact of public figures in positions of authority, who
may already elicit polarised opinions. Recent public health
interventions like the No Jab No Pay Policy in Australia,35
and the elimination of personal belief vaccine exemptions
in US states like California36 attempt to alter the behaviour
of fixed non-vaccinating parents at one end of the sp
trum rather than the majority of parents who vaccinate bu
hold uncertain views susceptible to change. Furthermore,
methods for countering vaccination hesitant attitudes lack
sufficient evidence of efficacy.20 37
The role of Michael Gannon in counteracting vaccine
misinformation in the mass media is mirrored in other cou
tries by other medical leaders like Paul Offit’s role in the
US media3 countering public antivaccination sentiments.
Medical spokespeoplehave great potentialto counter
antivaccination sentiments in public forums. Additionally,
copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
Open access
public figure in a seat of power, like President Trump or
Senator Hanson may be more difficult to address and can
influence a large group of parents who do not hold fixed
views on vaccination due to their authority as elected offi-
cials with influence on health legislation.
More targeted terminology needs to define vaccine
accepting parents with potentially changeableviews
towards vaccination, who could be the focus of vaccina-
tion education and promotion interventions.28 Parental
vaccine attitudes are often categorised by a scale19 of
vaccine acceptance, with absolute uptake of all vaccines
on one end and absolute refusal of vaccines on the other.
Through the subanalysis of ‘fixed-view’ and ‘susceptible’
parents, this study used alternative terminology to directly
identify the group of interest—vaccine accepting parents
who are ‘susceptible’ to influence by negative vaccine
messages from public figures. This group is also a worthy
target of health promotion and public health messaging
about vaccination. This study determined that only a
minority (23.8%) of parents have fixed views on vaccina-
tion in either direction, and those who do not hold fixed
views may be influenced by public figures. Moreover, the
proportion of parents with fixed antivaccination views
was very low (2.2%, n=9/411), consistent with the docu-
mented rate of Australia children with registered consci-
entious objections in 2016 prior to its abolishment later
that year.29 This population of fixed-antivaccine parents is
too small to draw any conclusions on the effects of media
messaging on their vaccine opinions and behaviours, a
limitation that could be addressed in future research.
Furthermore, the analysis in this paper did not identify
distinguishing demographic predictors of the ‘suscep-
tible’ group, future studies should attempt to characterise
this group further. They may be an invisible majority who
are not the focus of vaccination promotion messages,
which tends to be aimed at parents at the negative end
of the spectrum of attitudes. As we have identified this
group to be subject to the influence of public figure in
positions of authority, it is critical to better understand
this group across different sociopolitical contexts.
When asked what parent’s considered to be strong
influences on their vaccine decisions, we found that
20.2% of parents are strongly influenced by the media
and Internet websites, consistent with a US study13 where
26% of respondents reported at least some level of trust
in celebrities as a source of vaccine information. Further-
more, the majority of parents being influenced signifi-
cantly by doctors (88.6%) is consistent with the results of
another Australian study where 83% of parents received
health information from a family doctor.30
The qualitative analysis identified similar themes and
concerns to common antivaccination arguments identi-
fied in multiple studies,3 23 31 32
suggesting that concerns
about issues like vaccine safety, vaccine scheduling and
parental autonomy need to be better addressed. Hanson
may have resonated with some parents because she is a
mother. Furthermore,parental preferencefor media
messagedelivery style demonstrateda high level of
variability ranging from factual to anecdotal. Parental
responses suggest the mechanism of influence by public
figure in health communication is affected by comple
factors of pre-existing biases and opinions both towards
vaccination and the public figure in question. This is
corroborated by a recent US study33 that identifies the
influence of sociopolitical ideologies on vaccination trust
and attitudes.
As a result, a key takeaway of this paper is that m
parents do not hold fixed views either for or against vacci
nation, even if they vaccinate their children. We have
shown that this group is more likely to be influenced
antivaccination messaging from public figures than people
with fixed views. In fact, parents with initially positive but
not fixed views towards vaccination can be swayed toward
mistrusting childhood immunisation by negative media
messaging from public figures of authority. We analys
change in parental vaccine attitude irrespective of directio
of change, to confirm that parental vaccination attitud
are subject to influence from media messaging. Observa-
tion of the absolute numbers of parents who increased or
decreased in willingness to vaccinate in response to speci
media messages (figure 3) also reveals an apparent para-
doxical response of some parents whereby they increased
willingness to vaccinate in response to an antivaccinating
message and vice versa. This apparent ‘backfire’ response
possibly indicates a discord between what public figu
communicate and what the public actually perceives.
this study, it appeared there were strong political opinions
existing alongside or potentially causing variable vacc
nation opinions, and some Australian parents may ha
rejected the messages of Trump or Hanson based on their
pre-existing political ideals. Parental rejection of provaccin
or antivaccine messages could be motivated by ‘cultu
cognition’34 whereby individuals attempt to selectively valu
perspectives that conform their pre-existing perceptions o
vaccine risk. Future research could explore more deep
the factors that impact direction and magnitude of change
resulting from media messaging in a variety of contexts.
For public health authorities, this highlights the necessit
of improving methods of health communication to combat
antivaccination messages in the media and considerin
the impact of public figures in positions of authority, who
may already elicit polarised opinions. Recent public health
interventions like the No Jab No Pay Policy in Australia,35
and the elimination of personal belief vaccine exemptions
in US states like California36 attempt to alter the behaviour
of fixed non-vaccinating parents at one end of the sp
trum rather than the majority of parents who vaccinate bu
hold uncertain views susceptible to change. Furthermore,
methods for countering vaccination hesitant attitudes lack
sufficient evidence of efficacy.20 37
The role of Michael Gannon in counteracting vaccine
misinformation in the mass media is mirrored in other cou
tries by other medical leaders like Paul Offit’s role in the
US media3 countering public antivaccination sentiments.
Medical spokespeoplehave great potentialto counter
antivaccination sentiments in public forums. Additionally,
copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

7Zhang EJ, et al. BMJ Open 2019;9:e025866. doi:10.1136/bmjopen-2018-025866
Open access
other politicians may counter the antivaccination senti-
ments publicly, such as Barack Obama’s public response38
to the 2015 multistate US outbreak of measles, and the
bipartisan refutal of Hansons’ antivaccination comments by
Australian prime minister Malcolm Turnbull and opposi-
tion leader Bill Shorten.39 In our study, Gannon’s provacci-
nation message did not make parents more hesitant about
vaccine safety, indicating that there is no significant back-
fire effect from provaccine messaging on these parents.
For parents with fixed views, positive vaccine messages
can backfire, causing vaccine-hesitant parents to entrench
their views, and conversely,antivaccinationmessages
can strengthen the views of vaccine-supporting parents,
confirmed by our study. Furthermore, many parents have
strong personal opinions regarding childhood vaccinations
and vaccination attitudes may be linked to the expression
of broader political and social views. It appears that political
polarisation plays a role in influencing vaccination attitudes
and behaviours in some parents.
COnClusiOn
Vaccine hesitancy research has focused on parents at one
end of the spectrum, with negative vaccination views. We
have shown that even vaccine-accepting parents with posi-
tive views can be influenced negatively by public figures
in positions of authority. Health communication should
be designed to target parents without fixed views, even
if they vaccinate their children. We suggest a different
lens through which to view parents and plan vaccination
messaging, as ‘fixed view’ and ‘susceptible’, respectively.
Politicians and public figures can influence parents’ views
of vaccination and are in a unique position of also being
able to directly influence health policy. They, therefore,
have a responsibility to provide carefully informed health
information. Politicians play a crucial role in upholding
community confidence in public health policies including
childhood vaccination.
Contributors We confirm that the manuscript has been read and approved by all
named authors and that there are no other persons who satisfied the criteria for
authorship but are not listed. We further confirm that the order of authors listed
in the manuscript has been approved by all of us. We confirm that we have given
due consideration to the protection of intellectual property associated with this
work and that there are no impediments to publication, including the timing of
publication, with respect to intellectual property. In so doing we confirm that we
have followed the regulations of our institutions concerning intellectual property.
EJZ contributed to conception and design of the study, overseeing the whole study,
data management and writing the first draft of manuscript report; AAC and AH
contributed to statistical analysis and manuscript writing; CRM was responsible for
conception and design of the study, survey design, data analysis and manuscript
writing; All authors reviewed the final draft of manuscript.
Funding This study was supported by the NHMRC Centre for Research Excellence,
Integrated Systems for Epidemic Response (ISER).
Competing interests None declared.
Patient consent for publication Not required.
ethics approval The University of New South Wales ethics committee approved
(approval number: HC17045) the survey instrument and study protocol prior to data
collection.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement No additional data are available.
Open access This is an open access article distributed in accordance w
Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license,
permits others to distribute, remix, adapt, build upon this work non-com
and license their derivative works on different terms, provided the origin
properly cited, appropriate credit is given, any changes made indicated
is non-commercial. See: http:// creativecommons.org/ licenses/by- nc/4. 0/.
reFerenCes
1. Salmon DA, Teret SP, MacIntyre CR, et al. Compulsory vaccination
and conscientious or philosophical exemptions: past, present, and
future. Lancet 2006;367:436–42.
2. Greenfeld KT. Who's afraid of Jenny McCarthy? Time 2010;175:40-5.
3. Gottlieb SD. Vaccine resistances reconsidered: Vaccine skeptics and
the Jenny McCarthy effect. Biosocieties 2016;11:152–74.
4. Beckwith RT. Transcript: Read the Full Text of the Second Republican
Debate. 2015 http:// time. com/ 4037239/ second- republican- debate-
transcript- cnn/.
5. Hanson P. In: Cassidy B, ed. Pauline Hanson joins Insiders: ABC
Insiders: Australian Broadcasting Company, 2017.
6. Beck CS, Aubuchon SM, McKenna TP, et al. Blurring personal health
and public priorities: an analysis of celebrity health narratives in the
public sphere. Health Commun 2014;29:244–56.
7. Noar SM, Willoughby JF, Myrick JG, et al. Public figure
announcements about cancer and opportunities for cancer
communication: a review and research agenda. Health Commun
2014;29:445–61.
8. Evans DGR, Barwell J, Eccles DM, et al. The Angelina Jolie effect:
how high celebrity profile can have a major impact on provision of
cancer related services. Breast Cancer Research 2014;16.
9. Brown WJ, Basil MD. Media Celebrities and Public Health:
Responses to 'Magic' Johnson's HIV Disclosure and Its Impact on
AIDS Risk and High-Risk Behaviors. Health Commun 1995;7:345–70.
10. Chapman S, McLeod K, Wakefield M, et al. Impact of news of
celebrity illness on breast cancer screening: Kylie Minogue's breast
cancer diagnosis. Med J Aust 2005;183:247–50.
11. Cram P, Fendrick AM, Inadomi J, et al. The impact of a celebrity
promotional campaign on the use of colon cancer screening: the
Katie Couric effect. Arch Intern Med 2003;163:1601–5.
12. Borzekowski DL, Guan Y, Smith KC, et al. The Angelina effect:
immediate reach, grasp, and impact of going public. Genet Med
2014;16:516–21.
13. Freed GL, Clark SJ, Butchart AT, et al. Sources and perceived
credibility of vaccine-safety information for parents. Pediatrics
2011;127(Suppl 1):S107–12.
14. Hiltzik M. Katie Couric backs off from her anti-vaccine show-but not
enough. Los Angeles Times 2013.
15. Wakefield AJ, Murch SH, Anthony A, et al. Ileal-lymphoid-nodular
hyperplasia, non-specific colitis, and pervasive developmental
disorder in children. Lancet 1998;351:637–41.
16. Womack S. Blair silent over Leo's MMR jab. The Telegraph 2001.
17. Meikle J. Tony Blair should have gone public over Leo's MMR jab,
says Sir Liam Donaldson. The Guardian 2013.
18. Phillip A, Sun LH, Bernstein L. Vaccine skeptic Robert Kennedy Jr.
says Trump asked him to lead commission on ‘vaccine safety’. The
Washington Post 2017.
19. MacDonald NE. SAGE Working Group on Vaccine Hesitancy. Vaccine
hesitancy: Definition, scope and determinants. Vaccine 2015;33:4161–4
20. Nyhan B, Reifler J, Richey S, et al. Effective messages in vaccine
promotion: a randomized trial. Pediatrics 2014;133:e835–42.
21. SAGE Working Group. Report of the SAGE working group on vaccine
hesitancy: WHO, 2014.
22. Bedford H, Attwell K, Danchin M, et al. Vaccine hesitancy, refusal
and access barriers: The need for clarity in terminology. Vaccine
2018;36:6556–8.
23. Enkel SL, Attwell K, Snelling TL, et al. 'Hesitant compliers':
Qualitative analysis of concerned fully-vaccinating parents. Vaccine
2018;36:6459–63.
24. IBM Corp. IBM SPSS Statistics for Windows Version 24.0. Armonk,
NY: IBM Corp, 2016.
25. Gowda C, Dempsey AF. The rise (and fall?) of parental vaccine
hesitancy. Hum Vaccin Immunother 2013;9:1755–62.
26. Statistics ABo. Australian Demographic Statistics. Canberra:
Commonwealth of Australia, 2017:36–8.
27. Perreault L. Obesity in adults: Overview of management: UpToDate.
2017 https://www.uptodate. com/ contents/ obesity- in- adults-
overview- of- management? search=obesity& source= search_ result&
selectedTitle= 2~ 150& usage_ type= default& display_ rank= 2.copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
Open access
other politicians may counter the antivaccination senti-
ments publicly, such as Barack Obama’s public response38
to the 2015 multistate US outbreak of measles, and the
bipartisan refutal of Hansons’ antivaccination comments by
Australian prime minister Malcolm Turnbull and opposi-
tion leader Bill Shorten.39 In our study, Gannon’s provacci-
nation message did not make parents more hesitant about
vaccine safety, indicating that there is no significant back-
fire effect from provaccine messaging on these parents.
For parents with fixed views, positive vaccine messages
can backfire, causing vaccine-hesitant parents to entrench
their views, and conversely,antivaccinationmessages
can strengthen the views of vaccine-supporting parents,
confirmed by our study. Furthermore, many parents have
strong personal opinions regarding childhood vaccinations
and vaccination attitudes may be linked to the expression
of broader political and social views. It appears that political
polarisation plays a role in influencing vaccination attitudes
and behaviours in some parents.
COnClusiOn
Vaccine hesitancy research has focused on parents at one
end of the spectrum, with negative vaccination views. We
have shown that even vaccine-accepting parents with posi-
tive views can be influenced negatively by public figures
in positions of authority. Health communication should
be designed to target parents without fixed views, even
if they vaccinate their children. We suggest a different
lens through which to view parents and plan vaccination
messaging, as ‘fixed view’ and ‘susceptible’, respectively.
Politicians and public figures can influence parents’ views
of vaccination and are in a unique position of also being
able to directly influence health policy. They, therefore,
have a responsibility to provide carefully informed health
information. Politicians play a crucial role in upholding
community confidence in public health policies including
childhood vaccination.
Contributors We confirm that the manuscript has been read and approved by all
named authors and that there are no other persons who satisfied the criteria for
authorship but are not listed. We further confirm that the order of authors listed
in the manuscript has been approved by all of us. We confirm that we have given
due consideration to the protection of intellectual property associated with this
work and that there are no impediments to publication, including the timing of
publication, with respect to intellectual property. In so doing we confirm that we
have followed the regulations of our institutions concerning intellectual property.
EJZ contributed to conception and design of the study, overseeing the whole study,
data management and writing the first draft of manuscript report; AAC and AH
contributed to statistical analysis and manuscript writing; CRM was responsible for
conception and design of the study, survey design, data analysis and manuscript
writing; All authors reviewed the final draft of manuscript.
Funding This study was supported by the NHMRC Centre for Research Excellence,
Integrated Systems for Epidemic Response (ISER).
Competing interests None declared.
Patient consent for publication Not required.
ethics approval The University of New South Wales ethics committee approved
(approval number: HC17045) the survey instrument and study protocol prior to data
collection.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement No additional data are available.
Open access This is an open access article distributed in accordance w
Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license,
permits others to distribute, remix, adapt, build upon this work non-com
and license their derivative works on different terms, provided the origin
properly cited, appropriate credit is given, any changes made indicated
is non-commercial. See: http:// creativecommons.org/ licenses/by- nc/4. 0/.
reFerenCes
1. Salmon DA, Teret SP, MacIntyre CR, et al. Compulsory vaccination
and conscientious or philosophical exemptions: past, present, and
future. Lancet 2006;367:436–42.
2. Greenfeld KT. Who's afraid of Jenny McCarthy? Time 2010;175:40-5.
3. Gottlieb SD. Vaccine resistances reconsidered: Vaccine skeptics and
the Jenny McCarthy effect. Biosocieties 2016;11:152–74.
4. Beckwith RT. Transcript: Read the Full Text of the Second Republican
Debate. 2015 http:// time. com/ 4037239/ second- republican- debate-
transcript- cnn/.
5. Hanson P. In: Cassidy B, ed. Pauline Hanson joins Insiders: ABC
Insiders: Australian Broadcasting Company, 2017.
6. Beck CS, Aubuchon SM, McKenna TP, et al. Blurring personal health
and public priorities: an analysis of celebrity health narratives in the
public sphere. Health Commun 2014;29:244–56.
7. Noar SM, Willoughby JF, Myrick JG, et al. Public figure
announcements about cancer and opportunities for cancer
communication: a review and research agenda. Health Commun
2014;29:445–61.
8. Evans DGR, Barwell J, Eccles DM, et al. The Angelina Jolie effect:
how high celebrity profile can have a major impact on provision of
cancer related services. Breast Cancer Research 2014;16.
9. Brown WJ, Basil MD. Media Celebrities and Public Health:
Responses to 'Magic' Johnson's HIV Disclosure and Its Impact on
AIDS Risk and High-Risk Behaviors. Health Commun 1995;7:345–70.
10. Chapman S, McLeod K, Wakefield M, et al. Impact of news of
celebrity illness on breast cancer screening: Kylie Minogue's breast
cancer diagnosis. Med J Aust 2005;183:247–50.
11. Cram P, Fendrick AM, Inadomi J, et al. The impact of a celebrity
promotional campaign on the use of colon cancer screening: the
Katie Couric effect. Arch Intern Med 2003;163:1601–5.
12. Borzekowski DL, Guan Y, Smith KC, et al. The Angelina effect:
immediate reach, grasp, and impact of going public. Genet Med
2014;16:516–21.
13. Freed GL, Clark SJ, Butchart AT, et al. Sources and perceived
credibility of vaccine-safety information for parents. Pediatrics
2011;127(Suppl 1):S107–12.
14. Hiltzik M. Katie Couric backs off from her anti-vaccine show-but not
enough. Los Angeles Times 2013.
15. Wakefield AJ, Murch SH, Anthony A, et al. Ileal-lymphoid-nodular
hyperplasia, non-specific colitis, and pervasive developmental
disorder in children. Lancet 1998;351:637–41.
16. Womack S. Blair silent over Leo's MMR jab. The Telegraph 2001.
17. Meikle J. Tony Blair should have gone public over Leo's MMR jab,
says Sir Liam Donaldson. The Guardian 2013.
18. Phillip A, Sun LH, Bernstein L. Vaccine skeptic Robert Kennedy Jr.
says Trump asked him to lead commission on ‘vaccine safety’. The
Washington Post 2017.
19. MacDonald NE. SAGE Working Group on Vaccine Hesitancy. Vaccine
hesitancy: Definition, scope and determinants. Vaccine 2015;33:4161–4
20. Nyhan B, Reifler J, Richey S, et al. Effective messages in vaccine
promotion: a randomized trial. Pediatrics 2014;133:e835–42.
21. SAGE Working Group. Report of the SAGE working group on vaccine
hesitancy: WHO, 2014.
22. Bedford H, Attwell K, Danchin M, et al. Vaccine hesitancy, refusal
and access barriers: The need for clarity in terminology. Vaccine
2018;36:6556–8.
23. Enkel SL, Attwell K, Snelling TL, et al. 'Hesitant compliers':
Qualitative analysis of concerned fully-vaccinating parents. Vaccine
2018;36:6459–63.
24. IBM Corp. IBM SPSS Statistics for Windows Version 24.0. Armonk,
NY: IBM Corp, 2016.
25. Gowda C, Dempsey AF. The rise (and fall?) of parental vaccine
hesitancy. Hum Vaccin Immunother 2013;9:1755–62.
26. Statistics ABo. Australian Demographic Statistics. Canberra:
Commonwealth of Australia, 2017:36–8.
27. Perreault L. Obesity in adults: Overview of management: UpToDate.
2017 https://www.uptodate. com/ contents/ obesity- in- adults-
overview- of- management? search=obesity& source= search_ result&
selectedTitle= 2~ 150& usage_ type= default& display_ rank= 2.copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

8 Zhang EJ, et al. BMJ Open 2019;9:e025866. doi:10.1136/bmjopen-201
Open access
28. Leask J. Target the fence-sitters. Nature 2011;473:443–5.
29. Immunise Australia Program. ACIR- National Vaccine Objection
(Conscientious Objection) Data. 2016 http://www. immunise. health.
gov.au/ internet/ immunise/ publishing. nsf/ Content/ acir-cons- object-
hist.htm.
30. My C, Danchin M, Willaby HW, et al. Parental attitudes, beliefs,
behaviours and concerns towards childhood vaccinations
in Australia: A national online survey. Aust Fam Physician
2017;46:145–51.
31. Gerber JS, Offit PA. Vaccines and autism: a tale of shifting
hypotheses. Clin Infect Dis 2009;48:456–61.
32. Kata A. Anti-vaccine activists, Web 2.0, and the postmodern
paradigm--an overview of tactics and tropes used online by the anti-
vaccination movement. Vaccine 2012;30:3778–89.
33. Baumgaertner B, Carlisle JE, Justwan F. The influence of political
ideology and trust on willingness to vaccinate. PLoS One
2018;13:e0191728.
34. Kahan DM. Social science. A risky science communication
environment for vaccines. Science 2013;342:53–4.
35. Parliament of the Commonwealth of Australia. Social Services
Legislation Amendment (No Jab, No Pay) Bill Canberra. 2015 http://
www. aph.gov. au/ Parliamentary_ Business/ Bills_Legislation/ Bills_
Search_ Results/Result? bId= r5540.
36. Delamater PL, Leslie TF, Yang YT. Change in Medical Exemptions
From Immunization in California After Elimination of Personal Belief
Exemptions. JAMA 2017;318:863–4.
37. Dubé E, Gagnon D, MacDonald NE. SAGE Working Group
on Vaccine Hesitancy. Strategies intended to address
vaccine hesitancy: Review of published reviews. Vaccine
2015;33:4191–203.
38. Philip A. Obama to parents doubting ‘indisputable’ science: ‘Get
your kids vaccinated’. The Washington Post 2015.
39. Sharaz D, Armstrong K, Winsor B. Hanson refuses to back down
from vaccination comments as furore rises. SBS News 2017.
copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
Open access
28. Leask J. Target the fence-sitters. Nature 2011;473:443–5.
29. Immunise Australia Program. ACIR- National Vaccine Objection
(Conscientious Objection) Data. 2016 http://www. immunise. health.
gov.au/ internet/ immunise/ publishing. nsf/ Content/ acir-cons- object-
hist.htm.
30. My C, Danchin M, Willaby HW, et al. Parental attitudes, beliefs,
behaviours and concerns towards childhood vaccinations
in Australia: A national online survey. Aust Fam Physician
2017;46:145–51.
31. Gerber JS, Offit PA. Vaccines and autism: a tale of shifting
hypotheses. Clin Infect Dis 2009;48:456–61.
32. Kata A. Anti-vaccine activists, Web 2.0, and the postmodern
paradigm--an overview of tactics and tropes used online by the anti-
vaccination movement. Vaccine 2012;30:3778–89.
33. Baumgaertner B, Carlisle JE, Justwan F. The influence of political
ideology and trust on willingness to vaccinate. PLoS One
2018;13:e0191728.
34. Kahan DM. Social science. A risky science communication
environment for vaccines. Science 2013;342:53–4.
35. Parliament of the Commonwealth of Australia. Social Services
Legislation Amendment (No Jab, No Pay) Bill Canberra. 2015 http://
www. aph.gov. au/ Parliamentary_ Business/ Bills_Legislation/ Bills_
Search_ Results/Result? bId= r5540.
36. Delamater PL, Leslie TF, Yang YT. Change in Medical Exemptions
From Immunization in California After Elimination of Personal Belief
Exemptions. JAMA 2017;318:863–4.
37. Dubé E, Gagnon D, MacDonald NE. SAGE Working Group
on Vaccine Hesitancy. Strategies intended to address
vaccine hesitancy: Review of published reviews. Vaccine
2015;33:4191–203.
38. Philip A. Obama to parents doubting ‘indisputable’ science: ‘Get
your kids vaccinated’. The Washington Post 2015.
39. Sharaz D, Armstrong K, Winsor B. Hanson refuses to back down
from vaccination comments as furore rises. SBS News 2017.
copyright.
on September 5, 2019 at India:BMJ-PG Sponsored. Protected byhttp://bmjopen.bmj.com/BMJ Open: first published as 10.1136/bmjopen-2018-025866 on 26 March 2019. Downloaded from
1 out of 8
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.