University Mental Health MSE Assessment Report for Leroy
VerifiedAdded on 2022/10/10
|10
|2566
|10
Report
AI Summary
This report presents a mental state examination (MSE) assessment of a 35-year-old Caucasian male named Leroy, conducted as part of a nursing assignment. The assessment meticulously details various aspects of Leroy's mental state, including his general appearance, behavior, speech patterns, mood and affect, thought processes, thought content, perception, cognition, and judgment & insight. Leroy's presentation exhibited signs of potential mania, including a euphoric mood, rapid speech, and flight of ideas. The report further analyzes specific symptoms such as insomnia, racing thoughts, and a euphoric mood, offering detailed intervention strategies. These interventions include both pharmacological approaches, such as sedatives and atypical antipsychotics, and non-pharmacological techniques like cognitive behavioral therapy, paradoxical intention, mindfulness meditation, and recommending medication techniques. The assessment aims to provide a comprehensive overview of Leroy's mental state and propose appropriate interventions to address his symptoms.

Running head: MENTAL STATE EXAMINATION
Nursing/ mental health
Name of the Student
Name of the University
Author Note
Nursing/ mental health
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
MENTAL STATE EXAMINATION
Adult Mental Health Services
CONSUMER ASSESSMENT
Date: Time:
URN:
Family Name:
Given Name(s):
Address:
Date of Birth:
MENTAL STATE EXAMINATION
General
appearance
Although Leroy was a Caucasian male who was aged 35 years, his general
physical appearance did not match the stated age. His apparent age, as deduced
from the video was nearly 45-50 years. The fact that Leroy appeared much
elder to his actual chronological age provided a suggestion for ill-health and/or
poor self-care.pre
His dress was riotous and colourful. He had put on an orange cap with blue
shirt and green trousers that provided an indication of mania. However, his
clothes were neither unkempt nor dirty. He did not put on any accessories or
clothing that were particular of his Caucasian culture. In addition, there were
no body modifications. No signs of physical appearance were evident that
could provide an indication for drug abuse or alcoholism. However, significant
loss in body weight, since the previous session was notived, which provided an
indication of poor eating behaviour.
Behaviour
He maintained a kyphotic posture all throughout the interview, which suggests
forward curvature of the spine. Hence, his posture demonstrated weakening of
the muscles that made him slouch on the seat. All during the course of the
interview, he did not maintain direct eye contact with the counsellor. He
exchanged furtive glimpses that lasted for short time and kept looking
downwards, for most of the time. Hence, eye contact was perceived to be
MENTAL STATE EXAMINATION
Adult Mental Health Services
CONSUMER ASSESSMENT
Date: Time:
URN:
Family Name:
Given Name(s):
Address:
Date of Birth:
MENTAL STATE EXAMINATION
General
appearance
Although Leroy was a Caucasian male who was aged 35 years, his general
physical appearance did not match the stated age. His apparent age, as deduced
from the video was nearly 45-50 years. The fact that Leroy appeared much
elder to his actual chronological age provided a suggestion for ill-health and/or
poor self-care.pre
His dress was riotous and colourful. He had put on an orange cap with blue
shirt and green trousers that provided an indication of mania. However, his
clothes were neither unkempt nor dirty. He did not put on any accessories or
clothing that were particular of his Caucasian culture. In addition, there were
no body modifications. No signs of physical appearance were evident that
could provide an indication for drug abuse or alcoholism. However, significant
loss in body weight, since the previous session was notived, which provided an
indication of poor eating behaviour.
Behaviour
He maintained a kyphotic posture all throughout the interview, which suggests
forward curvature of the spine. Hence, his posture demonstrated weakening of
the muscles that made him slouch on the seat. All during the course of the
interview, he did not maintain direct eye contact with the counsellor. He
exchanged furtive glimpses that lasted for short time and kept looking
downwards, for most of the time. Hence, eye contact was perceived to be
2
MENTAL STATE EXAMINATION
intimidating to Leroy and he felt uncomfortable in doing so. In addition, on
being asked different questions, he continuously demonstrated tremor of his
hands. All throughout the interview, he demonstrated involuntary movement
of his hands and also manifested signs of stereotypies. This involved repetitive
abnormal and quasi-purposeful movement of his head, in the form of head
banging and communicated the need for reinforcement or attention or sensory
stimulation. Furthermore, on questioning him about use of medications,
substance abuse and hallucinations, psychomotor agitation was observed. His
typical manifestations included putting the hands on his head, bending his
head, and wringing his hands.
Speech
Throughout the interview, Leroy demonstrated signs of cluttering. His speech
was primarily characterised by rapid words and sentences, in addition to poor
grammar, poor syntax, erratic rhythm and speaking in a manner that made it
difficult to understand. This predominantly suggested that Leroy was nervous.
However, he did not face any difficulty in putting his thoughts into phrases,
though they became gradually disorganised at the time of speaking. He was
firstly dysfluent on the intial sounds while beginning to respond to the
questions asked, however, became more confident towards the end of the
statements. His speech was also characterised by struggle behaviour and he
also manifested signs of palilalia. There were unsolicited repetitions of words,
syllables and phrases, while replying to the counsellor. In addition, he also
demonstrated signs of pressured speech that were characterised by his
tendency to speak frenziedly and rapidly, as if he was motivated by an
earnestness not ostensible to the counsellor.
His mood was euphoric and was characterised by intense feelings of wellbeing
MENTAL STATE EXAMINATION
intimidating to Leroy and he felt uncomfortable in doing so. In addition, on
being asked different questions, he continuously demonstrated tremor of his
hands. All throughout the interview, he demonstrated involuntary movement
of his hands and also manifested signs of stereotypies. This involved repetitive
abnormal and quasi-purposeful movement of his head, in the form of head
banging and communicated the need for reinforcement or attention or sensory
stimulation. Furthermore, on questioning him about use of medications,
substance abuse and hallucinations, psychomotor agitation was observed. His
typical manifestations included putting the hands on his head, bending his
head, and wringing his hands.
Speech
Throughout the interview, Leroy demonstrated signs of cluttering. His speech
was primarily characterised by rapid words and sentences, in addition to poor
grammar, poor syntax, erratic rhythm and speaking in a manner that made it
difficult to understand. This predominantly suggested that Leroy was nervous.
However, he did not face any difficulty in putting his thoughts into phrases,
though they became gradually disorganised at the time of speaking. He was
firstly dysfluent on the intial sounds while beginning to respond to the
questions asked, however, became more confident towards the end of the
statements. His speech was also characterised by struggle behaviour and he
also manifested signs of palilalia. There were unsolicited repetitions of words,
syllables and phrases, while replying to the counsellor. In addition, he also
demonstrated signs of pressured speech that were characterised by his
tendency to speak frenziedly and rapidly, as if he was motivated by an
earnestness not ostensible to the counsellor.
His mood was euphoric and was characterised by intense feelings of wellbeing
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
MENTAL STATE EXAMINATION
Mood and
Affect
and excitement during the interview. On being asked questions about his
health, medications, substance abuse and hallucinations, he kepy on laughing
and provided replies that suggested the presence of mania. In addition, his
affect was also characterised by an enhanced expression. He did not
demonstrate any signs of blunted affect.
Thought process
Though the thought process of Leroy canot be directly understoodby observing
him, it can be inferred from his speech. He included a great deal of
inappropriate information in his responses and also made recurrent diversions,
thus demonstrating flight of ideas. This was further manifested by the
symptom that his thoughts, in relation to the individual questions were so raid
that his speech appeared incoherent. Hence, there was superficial association
between his ideas and his thoughts were expressed in the form of a
disconnection.
Thought content
On being questioned about whether he hears or watches anything while
watching the television or listening to the radio, he did not report hallucinating
any object or person. He also stated that he does not have suicidal ideations
and did not ever think of inflict harm either upon himself or others. However,
he stated that he thinks himself to be in possession of special powers regarding
business plan. These provide an indication about delusion about self that often
makes him feel overconfident, invincible and and empowered. Hence, he had
an overvalued idea about himself, concomitant with an emotionally charged
belief and also reported being preoccupied with work.
Perception
There were no signs of visual or audiotry hallucinations observed during the
interview.
MENTAL STATE EXAMINATION
Mood and
Affect
and excitement during the interview. On being asked questions about his
health, medications, substance abuse and hallucinations, he kepy on laughing
and provided replies that suggested the presence of mania. In addition, his
affect was also characterised by an enhanced expression. He did not
demonstrate any signs of blunted affect.
Thought process
Though the thought process of Leroy canot be directly understoodby observing
him, it can be inferred from his speech. He included a great deal of
inappropriate information in his responses and also made recurrent diversions,
thus demonstrating flight of ideas. This was further manifested by the
symptom that his thoughts, in relation to the individual questions were so raid
that his speech appeared incoherent. Hence, there was superficial association
between his ideas and his thoughts were expressed in the form of a
disconnection.
Thought content
On being questioned about whether he hears or watches anything while
watching the television or listening to the radio, he did not report hallucinating
any object or person. He also stated that he does not have suicidal ideations
and did not ever think of inflict harm either upon himself or others. However,
he stated that he thinks himself to be in possession of special powers regarding
business plan. These provide an indication about delusion about self that often
makes him feel overconfident, invincible and and empowered. Hence, he had
an overvalued idea about himself, concomitant with an emotionally charged
belief and also reported being preoccupied with work.
Perception
There were no signs of visual or audiotry hallucinations observed during the
interview.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
MENTAL STATE EXAMINATION
Cognition
No assesments were conducted to determine his memory, attention, orientation
executive functions and language function. However, on being asked about the
last time he took his medicines, Leroy reported that perhaps he had consumed
the medications two weeks earlier.
Judgment &
Insight
He considered himself extremely busy with work, although he was currently
unemployed. He also had the perception that on consuming medicines, his
symptoms improved, thus there was no need to continue their consumption.
Therefore, he did not recognise that he was suffering from a mental illness and
thus, refused to show compliance to the treatment that had been prescribed the
local mental health service. No questions were asked that could provide an
insight into Leroy’s judgment capabilities.
MENTAL STATE EXAMINATION
Cognition
No assesments were conducted to determine his memory, attention, orientation
executive functions and language function. However, on being asked about the
last time he took his medicines, Leroy reported that perhaps he had consumed
the medications two weeks earlier.
Judgment &
Insight
He considered himself extremely busy with work, although he was currently
unemployed. He also had the perception that on consuming medicines, his
symptoms improved, thus there was no need to continue their consumption.
Therefore, he did not recognise that he was suffering from a mental illness and
thus, refused to show compliance to the treatment that had been prescribed the
local mental health service. No questions were asked that could provide an
insight into Leroy’s judgment capabilities.
5
MENTAL STATE EXAMINATION
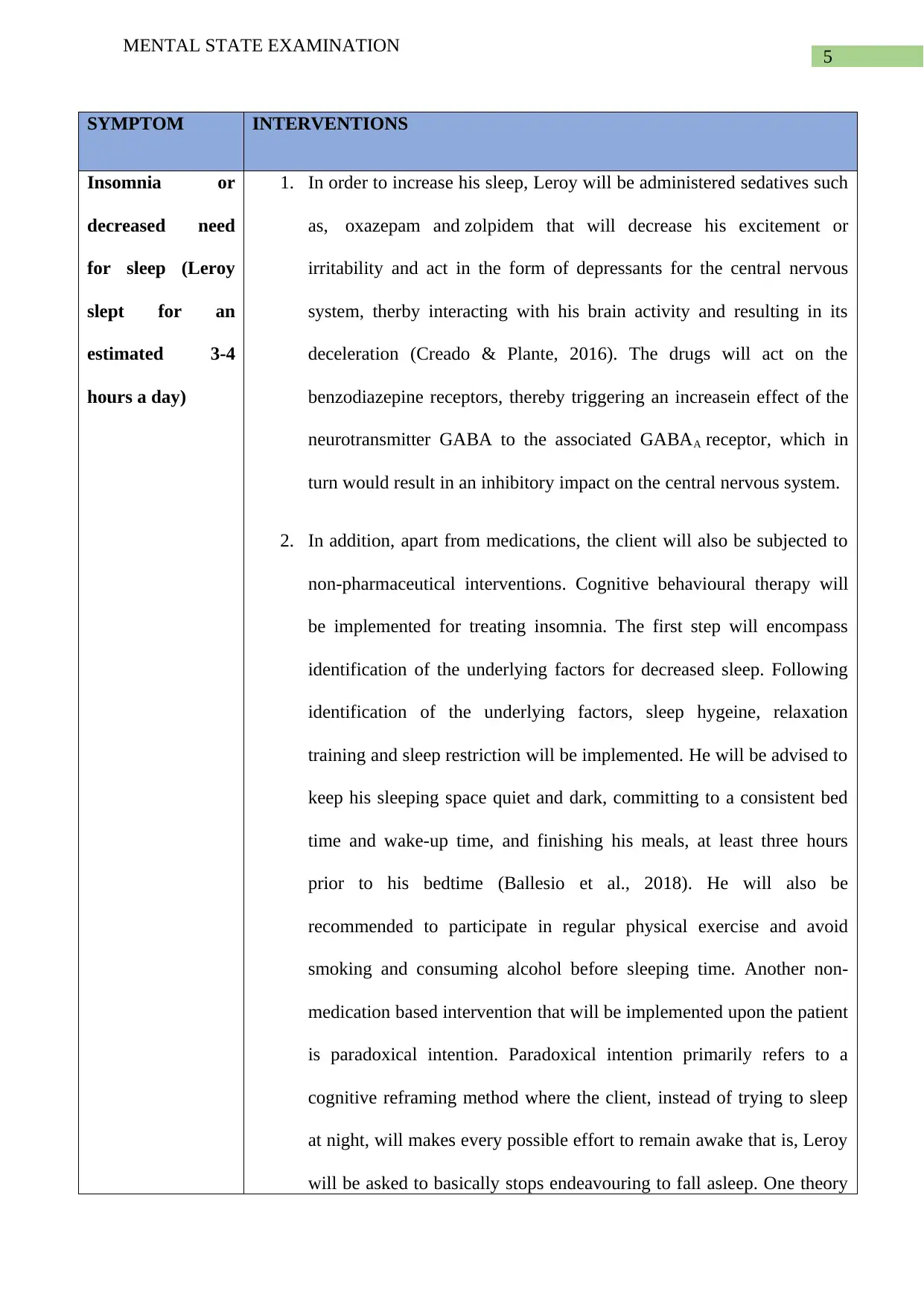
SYMPTOM INTERVENTIONS
Insomnia or
decreased need
for sleep (Leroy
slept for an
estimated 3-4
hours a day)
1. In order to increase his sleep, Leroy will be administered sedatives such
as, oxazepam and zolpidem that will decrease his excitement or
irritability and act in the form of depressants for the central nervous
system, therby interacting with his brain activity and resulting in its
deceleration (Creado & Plante, 2016). The drugs will act on the
benzodiazepine receptors, thereby triggering an increasein effect of the
neurotransmitter GABA to the associated GABAA receptor, which in
turn would result in an inhibitory impact on the central nervous system.
2. In addition, apart from medications, the client will also be subjected to
non-pharmaceutical interventions. Cognitive behavioural therapy will
be implemented for treating insomnia. The first step will encompass
identification of the underlying factors for decreased sleep. Following
identification of the underlying factors, sleep hygeine, relaxation
training and sleep restriction will be implemented. He will be advised to
keep his sleeping space quiet and dark, committing to a consistent bed
time and wake-up time, and finishing his meals, at least three hours
prior to his bedtime (Ballesio et al., 2018). He will also be
recommended to participate in regular physical exercise and avoid
smoking and consuming alcohol before sleeping time. Another non-
medication based intervention that will be implemented upon the patient
is paradoxical intention. Paradoxical intention primarily refers to a
cognitive reframing method where the client, instead of trying to sleep
at night, will makes every possible effort to remain awake that is, Leroy
will be asked to basically stops endeavouring to fall asleep. One theory
MENTAL STATE EXAMINATION
SYMPTOM INTERVENTIONS
Insomnia or
decreased need
for sleep (Leroy
slept for an
estimated 3-4
hours a day)
1. In order to increase his sleep, Leroy will be administered sedatives such
as, oxazepam and zolpidem that will decrease his excitement or
irritability and act in the form of depressants for the central nervous
system, therby interacting with his brain activity and resulting in its
deceleration (Creado & Plante, 2016). The drugs will act on the
benzodiazepine receptors, thereby triggering an increasein effect of the
neurotransmitter GABA to the associated GABAA receptor, which in
turn would result in an inhibitory impact on the central nervous system.
2. In addition, apart from medications, the client will also be subjected to
non-pharmaceutical interventions. Cognitive behavioural therapy will
be implemented for treating insomnia. The first step will encompass
identification of the underlying factors for decreased sleep. Following
identification of the underlying factors, sleep hygeine, relaxation
training and sleep restriction will be implemented. He will be advised to
keep his sleeping space quiet and dark, committing to a consistent bed
time and wake-up time, and finishing his meals, at least three hours
prior to his bedtime (Ballesio et al., 2018). He will also be
recommended to participate in regular physical exercise and avoid
smoking and consuming alcohol before sleeping time. Another non-
medication based intervention that will be implemented upon the patient
is paradoxical intention. Paradoxical intention primarily refers to a
cognitive reframing method where the client, instead of trying to sleep
at night, will makes every possible effort to remain awake that is, Leroy
will be asked to basically stops endeavouring to fall asleep. One theory
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
MENTAL STATE EXAMINATION
that can provide an explanation for the efficacy of this method is that
restricting voluntarily effort from falling asleep will help in relieving the
performance anxiety that generally arises (van Straten et al., 2018).
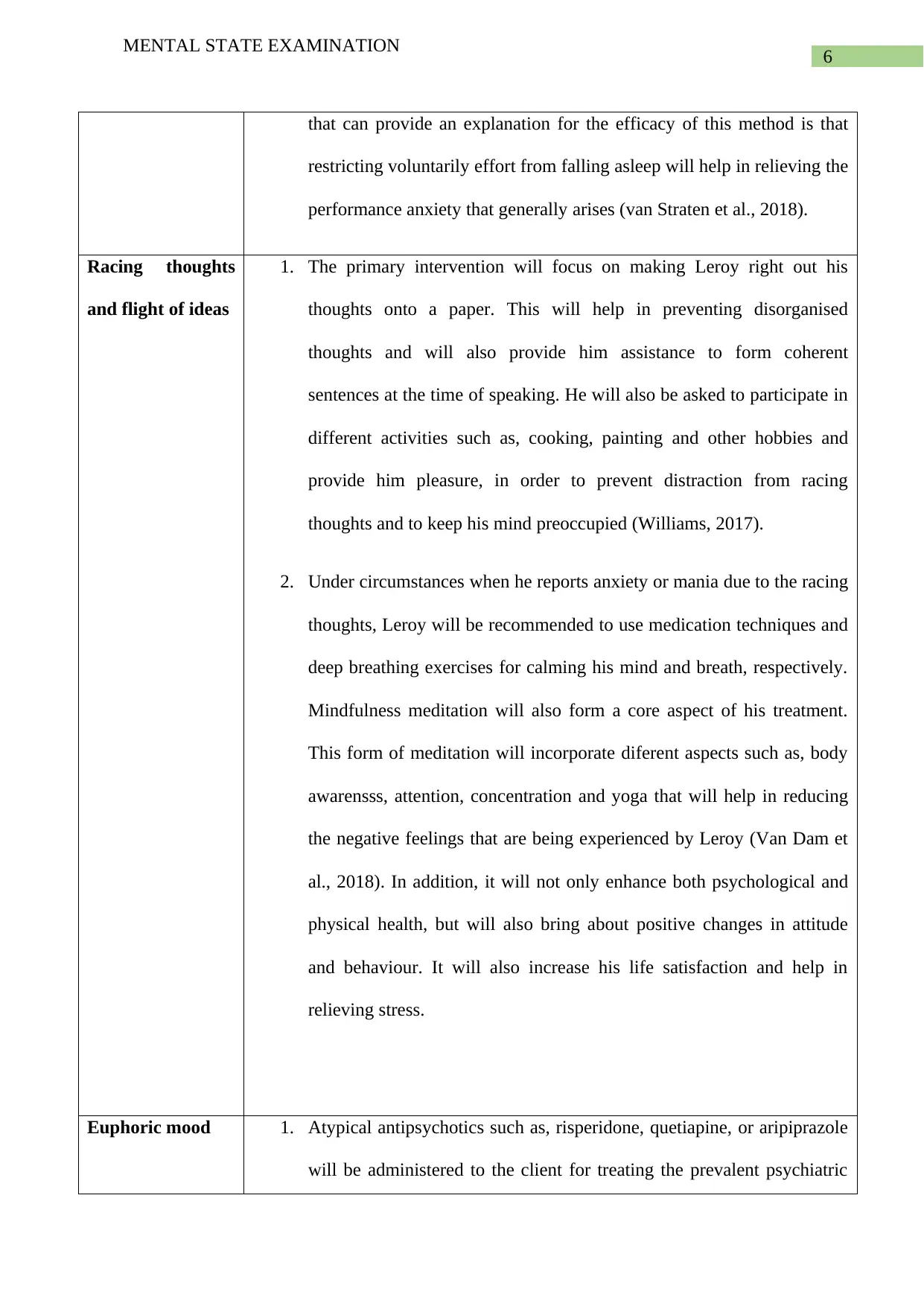
Racing thoughts
and flight of ideas
1. The primary intervention will focus on making Leroy right out his
thoughts onto a paper. This will help in preventing disorganised
thoughts and will also provide him assistance to form coherent
sentences at the time of speaking. He will also be asked to participate in
different activities such as, cooking, painting and other hobbies and
provide him pleasure, in order to prevent distraction from racing
thoughts and to keep his mind preoccupied (Williams, 2017).
2. Under circumstances when he reports anxiety or mania due to the racing
thoughts, Leroy will be recommended to use medication techniques and
deep breathing exercises for calming his mind and breath, respectively.
Mindfulness meditation will also form a core aspect of his treatment.
This form of meditation will incorporate diferent aspects such as, body
awarensss, attention, concentration and yoga that will help in reducing
the negative feelings that are being experienced by Leroy (Van Dam et
al., 2018). In addition, it will not only enhance both psychological and
physical health, but will also bring about positive changes in attitude
and behaviour. It will also increase his life satisfaction and help in
relieving stress.
Euphoric mood 1. Atypical antipsychotics such as, risperidone, quetiapine, or aripiprazole
will be administered to the client for treating the prevalent psychiatric
MENTAL STATE EXAMINATION
that can provide an explanation for the efficacy of this method is that
restricting voluntarily effort from falling asleep will help in relieving the
performance anxiety that generally arises (van Straten et al., 2018).
Racing thoughts
and flight of ideas
1. The primary intervention will focus on making Leroy right out his
thoughts onto a paper. This will help in preventing disorganised
thoughts and will also provide him assistance to form coherent
sentences at the time of speaking. He will also be asked to participate in
different activities such as, cooking, painting and other hobbies and
provide him pleasure, in order to prevent distraction from racing
thoughts and to keep his mind preoccupied (Williams, 2017).
2. Under circumstances when he reports anxiety or mania due to the racing
thoughts, Leroy will be recommended to use medication techniques and
deep breathing exercises for calming his mind and breath, respectively.
Mindfulness meditation will also form a core aspect of his treatment.
This form of meditation will incorporate diferent aspects such as, body
awarensss, attention, concentration and yoga that will help in reducing
the negative feelings that are being experienced by Leroy (Van Dam et
al., 2018). In addition, it will not only enhance both psychological and
physical health, but will also bring about positive changes in attitude
and behaviour. It will also increase his life satisfaction and help in
relieving stress.
Euphoric mood 1. Atypical antipsychotics such as, risperidone, quetiapine, or aripiprazole
will be administered to the client for treating the prevalent psychiatric
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
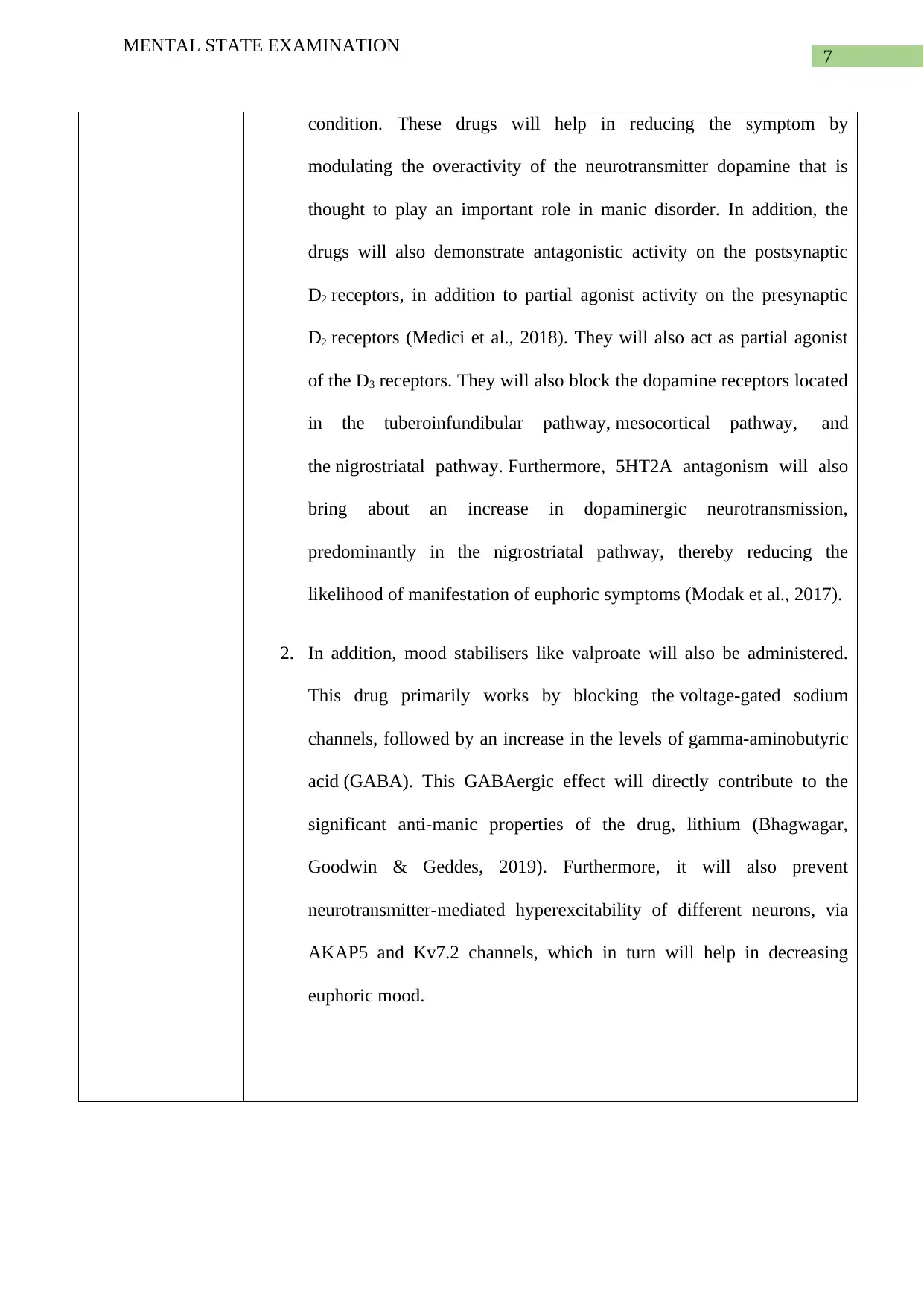
MENTAL STATE EXAMINATION
condition. These drugs will help in reducing the symptom by
modulating the overactivity of the neurotransmitter dopamine that is
thought to play an important role in manic disorder. In addition, the
drugs will also demonstrate antagonistic activity on the postsynaptic
D2 receptors, in addition to partial agonist activity on the presynaptic
D2 receptors (Medici et al., 2018). They will also act as partial agonist
of the D3 receptors. They will also block the dopamine receptors located
in the tuberoinfundibular pathway, mesocortical pathway, and
the nigrostriatal pathway. Furthermore, 5HT2A antagonism will also
bring about an increase in dopaminergic neurotransmission,
predominantly in the nigrostriatal pathway, thereby reducing the
likelihood of manifestation of euphoric symptoms (Modak et al., 2017).
2. In addition, mood stabilisers like valproate will also be administered.
This drug primarily works by blocking the voltage-gated sodium
channels, followed by an increase in the levels of gamma-aminobutyric
acid (GABA). This GABAergic effect will directly contribute to the
significant anti-manic properties of the drug, lithium (Bhagwagar,
Goodwin & Geddes, 2019). Furthermore, it will also prevent
neurotransmitter-mediated hyperexcitability of different neurons, via
AKAP5 and Kv7.2 channels, which in turn will help in decreasing
euphoric mood.
MENTAL STATE EXAMINATION
condition. These drugs will help in reducing the symptom by
modulating the overactivity of the neurotransmitter dopamine that is
thought to play an important role in manic disorder. In addition, the
drugs will also demonstrate antagonistic activity on the postsynaptic
D2 receptors, in addition to partial agonist activity on the presynaptic
D2 receptors (Medici et al., 2018). They will also act as partial agonist
of the D3 receptors. They will also block the dopamine receptors located
in the tuberoinfundibular pathway, mesocortical pathway, and
the nigrostriatal pathway. Furthermore, 5HT2A antagonism will also
bring about an increase in dopaminergic neurotransmission,
predominantly in the nigrostriatal pathway, thereby reducing the
likelihood of manifestation of euphoric symptoms (Modak et al., 2017).
2. In addition, mood stabilisers like valproate will also be administered.
This drug primarily works by blocking the voltage-gated sodium
channels, followed by an increase in the levels of gamma-aminobutyric
acid (GABA). This GABAergic effect will directly contribute to the
significant anti-manic properties of the drug, lithium (Bhagwagar,
Goodwin & Geddes, 2019). Furthermore, it will also prevent
neurotransmitter-mediated hyperexcitability of different neurons, via
AKAP5 and Kv7.2 channels, which in turn will help in decreasing
euphoric mood.
8
MENTAL STATE EXAMINATION
References
Ballesio, A., Aquino, M. R. J. V., Feige, B., Johann, A. F., Kyle, S. D., Spiegelhalder, K., ...
& Baglioni, C. (2018). The effectiveness of behavioural and cognitive behavioural
therapies for insomnia on depressive and fatigue symptoms: a systematic review and
network meta-analysis. Sleep Medicine Reviews, 37, 114-129.
Bhagwagar, Z., Goodwin, G., & Geddes, J. (2019). Lithium for acute mania. Cochrane
Database of Systematic Reviews, (5).
Creado, S., & Plante, D. T. (2016). An update on the use of sedative-hypnotic medications in
psychiatric disorders. Current psychiatry reports, 18(9), 78.
Medici, C. R., Kai, L. M., Kristensen, S. B., Kirkedal, C., Munk-Jørgensen, P., & Straszek, S.
(2018). Typical Versus Atypical Antipsychotics for Acute Mania. American journal
of therapeutics.
Modak, T., Kumar, S., Pal, A., Gupta, R., Pattanayak, R. D., & Khandelwal, S. K. (2017).
Chlorpromazine as prophylaxis for bipolar disorder with treatment-and
electroconvulsive therapy-refractory mania: Old horse, new trick. Indian journal of
psychological medicine, 39(4), 539.
Van Dam, N. T., van Vugt, M. K., Vago, D. R., Schmalzl, L., Saron, C. D., Olendzki, A., ...
& Fox, K. C. (2018). Mind the hype: A critical evaluation and prescriptive agenda for
research on mindfulness and meditation. Perspectives on Psychological
Science, 13(1), 36-61.
van Straten, A., van der Zweerde, T., Kleiboer, A., Cuijpers, P., Morin, C. M., & Lancee, J.
(2018). Cognitive and behavioral therapies in the treatment of insomnia: A meta-
analysis. Sleep Medicine Reviews, 38, 3-16.
MENTAL STATE EXAMINATION
References
Ballesio, A., Aquino, M. R. J. V., Feige, B., Johann, A. F., Kyle, S. D., Spiegelhalder, K., ...
& Baglioni, C. (2018). The effectiveness of behavioural and cognitive behavioural
therapies for insomnia on depressive and fatigue symptoms: a systematic review and
network meta-analysis. Sleep Medicine Reviews, 37, 114-129.
Bhagwagar, Z., Goodwin, G., & Geddes, J. (2019). Lithium for acute mania. Cochrane
Database of Systematic Reviews, (5).
Creado, S., & Plante, D. T. (2016). An update on the use of sedative-hypnotic medications in
psychiatric disorders. Current psychiatry reports, 18(9), 78.
Medici, C. R., Kai, L. M., Kristensen, S. B., Kirkedal, C., Munk-Jørgensen, P., & Straszek, S.
(2018). Typical Versus Atypical Antipsychotics for Acute Mania. American journal
of therapeutics.
Modak, T., Kumar, S., Pal, A., Gupta, R., Pattanayak, R. D., & Khandelwal, S. K. (2017).
Chlorpromazine as prophylaxis for bipolar disorder with treatment-and
electroconvulsive therapy-refractory mania: Old horse, new trick. Indian journal of
psychological medicine, 39(4), 539.
Van Dam, N. T., van Vugt, M. K., Vago, D. R., Schmalzl, L., Saron, C. D., Olendzki, A., ...
& Fox, K. C. (2018). Mind the hype: A critical evaluation and prescriptive agenda for
research on mindfulness and meditation. Perspectives on Psychological
Science, 13(1), 36-61.
van Straten, A., van der Zweerde, T., Kleiboer, A., Cuijpers, P., Morin, C. M., & Lancee, J.
(2018). Cognitive and behavioral therapies in the treatment of insomnia: A meta-
analysis. Sleep Medicine Reviews, 38, 3-16.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

9
MENTAL STATE EXAMINATION
Williams, R. (2017). Bipolar Q&A. Mental Health Matters, 4(6), 12-14.
MENTAL STATE EXAMINATION
Williams, R. (2017). Bipolar Q&A. Mental Health Matters, 4(6), 12-14.
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





