Exploring Confidence and Competence of Nurses in Palliative Care
VerifiedAdded on 2023/01/06
|58
|11643
|98
AI Summary
This assignment explores the process of primary research to identify potential care improvements in palliative care. It focuses on the confidence and competence of nurses in private nursing homes when caring for individuals with a palliative diagnosis and receiving end of life care.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Comments on any unusual/mitigating circumstances:
ASSIGNMENT
COVER PAGE
ASSIGNMENT
COVER PAGE
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Table of Contents:
Table of Contents
ASSIGNMENT COVER PAGE.............................................................................................................1
Executive Summary:..............................................................................................................................3
Chapter One..........................................................................................................................................4
Introduction and Background:...........................................................................................................4
Chapter Two..........................................................................................................................................6
Literature Review:.............................................................................................................................6
Chapter Three......................................................................................................................................14
Methodology:..................................................................................................................................14
Chapter Four........................................................................................................................................22
Results:............................................................................................................................................22
Chapter Five........................................................................................................................................47
Summary and discussions of findings:.............................................................................................47
Chapter Six..........................................................................................................................................49
Conclusion.......................................................................................................................................49
References:..........................................................................................................................................52
Appendices:.........................................................................................................................................55
Appendix A - Consent Form............................................................................................................55
Appendix B – Questionnaire............................................................................................................56
Appendix C - Ethics Form.................................................................................................................58
Table of Contents
ASSIGNMENT COVER PAGE.............................................................................................................1
Executive Summary:..............................................................................................................................3
Chapter One..........................................................................................................................................4
Introduction and Background:...........................................................................................................4
Chapter Two..........................................................................................................................................6
Literature Review:.............................................................................................................................6
Chapter Three......................................................................................................................................14
Methodology:..................................................................................................................................14
Chapter Four........................................................................................................................................22
Results:............................................................................................................................................22
Chapter Five........................................................................................................................................47
Summary and discussions of findings:.............................................................................................47
Chapter Six..........................................................................................................................................49
Conclusion.......................................................................................................................................49
References:..........................................................................................................................................52
Appendices:.........................................................................................................................................55
Appendix A - Consent Form............................................................................................................55
Appendix B – Questionnaire............................................................................................................56
Appendix C - Ethics Form.................................................................................................................58
Executive Summary:
The aim of this assignment is to encompass and explore the process of a primary
piece of research in the anticipation that this will identify potential care
improvements. This piece of research will be formulated into a qualitative
questionnaire, targeting qualified nurses working in private nursing homes,
assessing their confidence and competence when caring for individuals with a
palliative diagnosis and receiving end of life care. From the data being collected and
analysed, this will potentially highlight if a need for further training around this subject
is required in order to improve patient care that residents are currently receiving
within the nursing homes. This has an ultimate goal to improve the patient’s journey
as they reach the end of their life but also will reduce financial pressures on the
National Health Service (NHS) organisations. This would be achieved by patients
only accessing NHS community and specialist services when they have a health
requirement that necessitates this instead of this being at a time of crisis when end
of life care cannot be achieved.
The aim of this assignment is to encompass and explore the process of a primary
piece of research in the anticipation that this will identify potential care
improvements. This piece of research will be formulated into a qualitative
questionnaire, targeting qualified nurses working in private nursing homes,
assessing their confidence and competence when caring for individuals with a
palliative diagnosis and receiving end of life care. From the data being collected and
analysed, this will potentially highlight if a need for further training around this subject
is required in order to improve patient care that residents are currently receiving
within the nursing homes. This has an ultimate goal to improve the patient’s journey
as they reach the end of their life but also will reduce financial pressures on the
National Health Service (NHS) organisations. This would be achieved by patients
only accessing NHS community and specialist services when they have a health
requirement that necessitates this instead of this being at a time of crisis when end
of life care cannot be achieved.
Protocol Title: To ascertain how confident and competent nurses working within
private nursing homes feel when caring for patients who are palliative and receiving
end of life care.
Chapter One
Introduction and Background:
This research protocol will explore and develop an opportunity for a structured
qualitative research study to be carried out, exploring how confident and competent
nurses working within private nursing homes feel when caring for patients who are
palliative and receiving end of life care. This piece of primary research supports and
further develops in conjunction with the previous project management study as part
of the MSc in Healthcare Leadership, underpinning the essential need for palliative
and end of life care changes and improvements within none national health service
(NHS) run care providers. From both a professional and personal encounter, there
has been a highlighted significant difference in the standard of care these patients
receive in comparison with those who are cared for within NHS run organisations.
This assignment will explore and potentially offer a protocol to expose the gaps and
absences in care for there to be an opportunity for care improvements. It is thought
that this can be improved by offering support, knowledge, training and skills to a set
of care providers who arguably need it the most.
Dixon (2015) describes an individual receiving ‘palliative care’ as someone who is
incurable, having a ‘palliative diagnosis’, meaning that an individual is being cared
for in their last phase of life. This can be defined as ‘end of life care’ which
categorises someone to be approximately within the last year of life. This however
can be narrowed down further to patients within the last months, weeks, days and
private nursing homes feel when caring for patients who are palliative and receiving
end of life care.
Chapter One
Introduction and Background:
This research protocol will explore and develop an opportunity for a structured
qualitative research study to be carried out, exploring how confident and competent
nurses working within private nursing homes feel when caring for patients who are
palliative and receiving end of life care. This piece of primary research supports and
further develops in conjunction with the previous project management study as part
of the MSc in Healthcare Leadership, underpinning the essential need for palliative
and end of life care changes and improvements within none national health service
(NHS) run care providers. From both a professional and personal encounter, there
has been a highlighted significant difference in the standard of care these patients
receive in comparison with those who are cared for within NHS run organisations.
This assignment will explore and potentially offer a protocol to expose the gaps and
absences in care for there to be an opportunity for care improvements. It is thought
that this can be improved by offering support, knowledge, training and skills to a set
of care providers who arguably need it the most.
Dixon (2015) describes an individual receiving ‘palliative care’ as someone who is
incurable, having a ‘palliative diagnosis’, meaning that an individual is being cared
for in their last phase of life. This can be defined as ‘end of life care’ which
categorises someone to be approximately within the last year of life. This however
can be narrowed down further to patients within the last months, weeks, days and
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
hours of life (Dixon, 2015). How long an individual has left to live has a huge
implication on preparation, decision making and what care that person requires.
Without these skills or understanding across diverse care levels, there is an increase
in the risk in ambiguity within palliative and end of life care (Wallerstedt et al., 2019).
Swami and Case (2018) explain how palliative care is exploring in detail the physical,
emotional and spiritual suffering that individuals can experience through knowledge,
understanding and effective communication. Improved outcomes for patients with a
palliative diagnosis have been identified when early integration of palliative care has
been introduced (Swami, Case, 2018).This involves care staff initiating
conversations around wishes and choices early enough so these can be actioned.
This is called Advance Care Planning (ACP). ACP is a written record of patient’s
wishes, choices and preferences whilst having capacity. ACP is an umbrella term for
many different factors which can include choices around resuscitation and
implementation of medications, fluids and nutrition and preferred places of care and
death (Hold et al., 2019).ACP is a large part of palliative care plan and treatment and
should have equal amount of skill and training when discussing this with appropriate
patients. ACP was implemented from ‘respecting patient choices’ which was
introduced within healthcare services in the 1980’s (Bradshaw, Smith & Sinclair,
2016). This then developed to become ACP where the emphasis encompassed
patients’ choices, beliefs, values and what was personally important.
implication on preparation, decision making and what care that person requires.
Without these skills or understanding across diverse care levels, there is an increase
in the risk in ambiguity within palliative and end of life care (Wallerstedt et al., 2019).
Swami and Case (2018) explain how palliative care is exploring in detail the physical,
emotional and spiritual suffering that individuals can experience through knowledge,
understanding and effective communication. Improved outcomes for patients with a
palliative diagnosis have been identified when early integration of palliative care has
been introduced (Swami, Case, 2018).This involves care staff initiating
conversations around wishes and choices early enough so these can be actioned.
This is called Advance Care Planning (ACP). ACP is a written record of patient’s
wishes, choices and preferences whilst having capacity. ACP is an umbrella term for
many different factors which can include choices around resuscitation and
implementation of medications, fluids and nutrition and preferred places of care and
death (Hold et al., 2019).ACP is a large part of palliative care plan and treatment and
should have equal amount of skill and training when discussing this with appropriate
patients. ACP was implemented from ‘respecting patient choices’ which was
introduced within healthcare services in the 1980’s (Bradshaw, Smith & Sinclair,
2016). This then developed to become ACP where the emphasis encompassed
patients’ choices, beliefs, values and what was personally important.
Chapter Two
Literature Review:
There are over 470,000 individuals that die each year within the UK from having a
palliative diagnosis and from this figure, 33 percent of these patients are currently
cared for in a nursing home. However, 92,000 people from the identified category
had no palliative care input which resulted in uncontrolled symptoms. The nurses
caring for these patients felt they were unable to meet these patients’ needs due to
the lack of competence, confidence, knowledge and skills (Dixon, 2015). The Royal
College of Nursing (2015) understand how complex caring for a patient that is dying
can be and recognises how for patients care and symptoms to be managed
effectively there requires a high level of skill, experience and knowledge. Palliative
care nursing is described as anevidence-based science that required advanced skills
and knowledge, complex assessment and compassion in equal measure, which is
sensitive, dynamic, hopeful and meaningful. For this to be achieved successfully
there needs to be a level of increased knowledge and competent training and skills
(Becker, 2009).
Owen (2008) explains how nurses working within nursing homes feel unable to offer
high standard palliative and end of life care due to lack of education and training.
Patients who have a nursing home as their main place of residence have been
described as having the most complex palliative, end of life care needs but these
requirements are not recognised or met due to the lack of palliative knowledge and
understanding (Dixon, 2015). Due to the lack of faith patients and families have in
the appropriate care being received within this environment, patients change their
minds where they wish to die as they are nearing the end of their life due to nursing
Literature Review:
There are over 470,000 individuals that die each year within the UK from having a
palliative diagnosis and from this figure, 33 percent of these patients are currently
cared for in a nursing home. However, 92,000 people from the identified category
had no palliative care input which resulted in uncontrolled symptoms. The nurses
caring for these patients felt they were unable to meet these patients’ needs due to
the lack of competence, confidence, knowledge and skills (Dixon, 2015). The Royal
College of Nursing (2015) understand how complex caring for a patient that is dying
can be and recognises how for patients care and symptoms to be managed
effectively there requires a high level of skill, experience and knowledge. Palliative
care nursing is described as anevidence-based science that required advanced skills
and knowledge, complex assessment and compassion in equal measure, which is
sensitive, dynamic, hopeful and meaningful. For this to be achieved successfully
there needs to be a level of increased knowledge and competent training and skills
(Becker, 2009).
Owen (2008) explains how nurses working within nursing homes feel unable to offer
high standard palliative and end of life care due to lack of education and training.
Patients who have a nursing home as their main place of residence have been
described as having the most complex palliative, end of life care needs but these
requirements are not recognised or met due to the lack of palliative knowledge and
understanding (Dixon, 2015). Due to the lack of faith patients and families have in
the appropriate care being received within this environment, patients change their
minds where they wish to die as they are nearing the end of their life due to nursing
staff being unable to control their symptoms. This results in only 43 per cent of the
dying population, who achieve their preferred place of death (Dixon, 2015). Nursing
staff within nursing homes have admitted to feeling unable to meet the needs of their
patients including difficulty in engaging with their patients in end of life conversations.
These barriers include nurses feeling uncomfortable and inexperienced (Towsely
and Hirschman 2018). Murphy-Jones and Timmons (2016) have highlighted the
devastating reality and consequences of nursing staff feeling unable to meet the
needs of their patients anticipated deterioration and the reality being that patients are
often being transferred from nursing homes to emergency departments and dying in
cubicle bays.
More than 405,000 individuals over the age of 65 years live in care homes in the
United Kingdom (UK). From these identified figures 17% of deaths in the UK occur in
nursing homes. The proportion of deaths occurring in care homes increases with
age, and almost 40% of people aged 90 years and over die in a care home
(Hewison, Badger & Swani, 2011).
Handley et al, (2014) explain how nursing/care homes are the main providers of
long-term health care for the older population within England. Residents within these
care environments have a limited life expectancy due to their age and frailty. Kalseth
and Antun (2016) explain how nursing homes have become an increasingly essential
setting for patients who are receiving end of life care and this has a large impact on
their quality of death and dying. With these facts in mind, investment in training and
enablement for these staff members looking after these vulnerable set of patients is
essential for effective end of life care to be delivered. These investments provide a
structure of approach to encourage advance care planning, manage signs and
symptoms, reduce unplanned admissions to acute settings and increase nursing
dying population, who achieve their preferred place of death (Dixon, 2015). Nursing
staff within nursing homes have admitted to feeling unable to meet the needs of their
patients including difficulty in engaging with their patients in end of life conversations.
These barriers include nurses feeling uncomfortable and inexperienced (Towsely
and Hirschman 2018). Murphy-Jones and Timmons (2016) have highlighted the
devastating reality and consequences of nursing staff feeling unable to meet the
needs of their patients anticipated deterioration and the reality being that patients are
often being transferred from nursing homes to emergency departments and dying in
cubicle bays.
More than 405,000 individuals over the age of 65 years live in care homes in the
United Kingdom (UK). From these identified figures 17% of deaths in the UK occur in
nursing homes. The proportion of deaths occurring in care homes increases with
age, and almost 40% of people aged 90 years and over die in a care home
(Hewison, Badger & Swani, 2011).
Handley et al, (2014) explain how nursing/care homes are the main providers of
long-term health care for the older population within England. Residents within these
care environments have a limited life expectancy due to their age and frailty. Kalseth
and Antun (2016) explain how nursing homes have become an increasingly essential
setting for patients who are receiving end of life care and this has a large impact on
their quality of death and dying. With these facts in mind, investment in training and
enablement for these staff members looking after these vulnerable set of patients is
essential for effective end of life care to be delivered. These investments provide a
structure of approach to encourage advance care planning, manage signs and
symptoms, reduce unplanned admissions to acute settings and increase nursing
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
staff’s confidence in their own ability to provide a good standard of palliative/end of
life nursing care (Handley et al, 2014). Di Giulio et al (2019) explain how there is still
so much that can be improved to increase the quality of care that palliative patients
receive. Due to these identified breaches within care, only several elements of
palliative care are partially provided or not provided at all. These barriers include
insufficient connections between specialist palliative services, lack of expertise and
lack or absence of staff training.Towsley and Hirschman (2018) describe other
barriers to these conversations, including nursing staff feeling unprepared and
uncomfortable, concerned that they will cause distress by engaging in conversations
around end of life care.
Handley et al (2014) explain how nursing staff working within care homes feel that
their level of knowledge and proficiency is undervalued.
Murphy-Jones, Timmons, (2016)have highlighted howcommon patient transfers are
occurring from a nursing home to the emergency department when patients are
nearing the end of their life. This has been described as inappropriate, having
negative consequences and losing the ability to provide dignified and appropriate
care.
Kalseth and Antun (2016) express their concerns around transfers of relocation
when patients are nearing death and state that this can be traumatic. Concerns
around frequent hospital admissions are apparent and a high proportion of hospital
deaths have been described as an inappropriate setting for end of life care.
Paramedic staff are often having to make a best interest decision weighing the risks
and benefits of hospitalisation when the patient no longer has capacity. Martin,
(2015) express how there is an increasing number of admissions to hospital when
life nursing care (Handley et al, 2014). Di Giulio et al (2019) explain how there is still
so much that can be improved to increase the quality of care that palliative patients
receive. Due to these identified breaches within care, only several elements of
palliative care are partially provided or not provided at all. These barriers include
insufficient connections between specialist palliative services, lack of expertise and
lack or absence of staff training.Towsley and Hirschman (2018) describe other
barriers to these conversations, including nursing staff feeling unprepared and
uncomfortable, concerned that they will cause distress by engaging in conversations
around end of life care.
Handley et al (2014) explain how nursing staff working within care homes feel that
their level of knowledge and proficiency is undervalued.
Murphy-Jones, Timmons, (2016)have highlighted howcommon patient transfers are
occurring from a nursing home to the emergency department when patients are
nearing the end of their life. This has been described as inappropriate, having
negative consequences and losing the ability to provide dignified and appropriate
care.
Kalseth and Antun (2016) express their concerns around transfers of relocation
when patients are nearing death and state that this can be traumatic. Concerns
around frequent hospital admissions are apparent and a high proportion of hospital
deaths have been described as an inappropriate setting for end of life care.
Paramedic staff are often having to make a best interest decision weighing the risks
and benefits of hospitalisation when the patient no longer has capacity. Martin,
(2015) express how there is an increasing number of admissions to hospital when
people are at the end of their life. This is described as a negative act and a palliative
care approach with the nursing homes is advocated. Unfortunately, this is not always
achieved and in some cases, when a person has lost capacity, a best interest
decision must be addressed. This is described as a valued judgement in what the
patient would have wanted if/when they did have capacity considering beliefs,
choices and values (Martin, 2015). Paramedics have found this increasingly
challenging to equilibrium what is in the patient’s best interest and deal with the
pressures from nursing staff working within the care homes (Murphy-Jones and
Timmons, 2016). Care at the end of life is complex, challenging,emotive and can be
uncoordinated and inconsistent. For these challenges to be accomplished theremust
be a fundamental level of training delivered and understood within nursing homes in
order for an appropriate standard of care to be delivered (Hewison, Badger and
Swani 2011).Hewison, Badger and Swani (2011) explain how the most significant
and common dominator within end of life care in the UK is the highlighted insufficient
training of staff at all levels. Staff education within nursing homes hasbeen described
as one of ten top transformations necessary to improve end-of-life care(Hewison,
Badger & Swani, 2011).The NHS long term plan (2019) states how their strategy is
to integrate services in order to support older people in keeping themout of hospital
enabling independence. This includes preventing an estimated 50,000 hospital
admissions, with hope that some of these will be patients nearing end of life care.
The communication and organisation within end-of-life care remains a challenge for
nursing homes. Nursing staff have trouble in introducing and initiating conversations
about the end of life and advance care planning but also managing the complexity of
an anticipated deteriorating patient(Hewison, Badger and Swani, 2011).
care approach with the nursing homes is advocated. Unfortunately, this is not always
achieved and in some cases, when a person has lost capacity, a best interest
decision must be addressed. This is described as a valued judgement in what the
patient would have wanted if/when they did have capacity considering beliefs,
choices and values (Martin, 2015). Paramedics have found this increasingly
challenging to equilibrium what is in the patient’s best interest and deal with the
pressures from nursing staff working within the care homes (Murphy-Jones and
Timmons, 2016). Care at the end of life is complex, challenging,emotive and can be
uncoordinated and inconsistent. For these challenges to be accomplished theremust
be a fundamental level of training delivered and understood within nursing homes in
order for an appropriate standard of care to be delivered (Hewison, Badger and
Swani 2011).Hewison, Badger and Swani (2011) explain how the most significant
and common dominator within end of life care in the UK is the highlighted insufficient
training of staff at all levels. Staff education within nursing homes hasbeen described
as one of ten top transformations necessary to improve end-of-life care(Hewison,
Badger & Swani, 2011).The NHS long term plan (2019) states how their strategy is
to integrate services in order to support older people in keeping themout of hospital
enabling independence. This includes preventing an estimated 50,000 hospital
admissions, with hope that some of these will be patients nearing end of life care.
The communication and organisation within end-of-life care remains a challenge for
nursing homes. Nursing staff have trouble in introducing and initiating conversations
about the end of life and advance care planning but also managing the complexity of
an anticipated deteriorating patient(Hewison, Badger and Swani, 2011).
Andrew and Taylor (2012) express the importance of effective communication skills
and how this is central in the formation of relationships which is the provision to
offering personal centred care to the highest of quality. Effective communication has
a focus of compassion and decision making which is essential when delivering
palliative, end of life care. Towsley and Hirschman (2018) feel that when end of life
conversations are initiated by a nursing home staff members, then these
conversations should be started with a person’s preferences for today which will then
lead to a conversation around anticipation and planning for the future. It is felt that
this approach may move the isolated conversations around end of life and dying to
more of a routine conversation that will increase patient’s participation within end of
life. However, still more work has to be done to ensure these conversations are
begun.
Nursing home staff should initiate conversations around wishes, choices and
preferences within end-of-life care. This should include supporting and when
appropriate, initiating conversations between patients and their relatives in end of life
discussions to enable choices and wishes to be achieved(Gjerberg et al.,
2015).Evenblij et al, (2009) state that end-of-life conversations are rarely introduced
by care staff in long-term care facilities such as nursing homes. A possible likelihood
is that care staff lack of self-efficacy and confidence to uphold such conversations.
Evenblij et al (2009) feel that if staff within the nursing homes had some education
around providing palliative care and training around offering end of life care within
these facilities, this will improve the delivery of end of life and the communication that
is within this.
According to Badger et al (2012), Improving end-of-life care within nursing homes is
a government health priority and highlight how collaboration between care home
and how this is central in the formation of relationships which is the provision to
offering personal centred care to the highest of quality. Effective communication has
a focus of compassion and decision making which is essential when delivering
palliative, end of life care. Towsley and Hirschman (2018) feel that when end of life
conversations are initiated by a nursing home staff members, then these
conversations should be started with a person’s preferences for today which will then
lead to a conversation around anticipation and planning for the future. It is felt that
this approach may move the isolated conversations around end of life and dying to
more of a routine conversation that will increase patient’s participation within end of
life. However, still more work has to be done to ensure these conversations are
begun.
Nursing home staff should initiate conversations around wishes, choices and
preferences within end-of-life care. This should include supporting and when
appropriate, initiating conversations between patients and their relatives in end of life
discussions to enable choices and wishes to be achieved(Gjerberg et al.,
2015).Evenblij et al, (2009) state that end-of-life conversations are rarely introduced
by care staff in long-term care facilities such as nursing homes. A possible likelihood
is that care staff lack of self-efficacy and confidence to uphold such conversations.
Evenblij et al (2009) feel that if staff within the nursing homes had some education
around providing palliative care and training around offering end of life care within
these facilities, this will improve the delivery of end of life and the communication that
is within this.
According to Badger et al (2012), Improving end-of-life care within nursing homes is
a government health priority and highlight how collaboration between care home
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
staff and NHS practitioners is vital to ensure high quality, end of life care. Brodtkorb
et al (2017)feel although palliative care is sat under the umbrella of meeting the
needs for dying patients, in nursing homes, it is felt that one of the many problems
within these care providers is the lack of a structural approach in team working. It is
felt that this supports ethical challenges which then produce undignified care. There
are 4 main groups that have been highlighted and have been categorised as regular
problematic issues within how palliative, end of life nursing care is delivered within
nursing homes. These four main groups include medication knowledge,
communication around interpersonal relations with patients and other team
members, decision making including early planning around within advance care
planning and professional development including education, training, knowledge and
skills (Gorlén, Gorlén and Neergaard, 2013). From these findings there is evidence
of lack of early planning, the appropriate use of medication and detailed knowledge
around palliative and end of life care among care staff. These essential barriers
prevent patients from living a quality life for as long as possible and achieving good
end of life care and good deaths. This prevents patients’ wishes and choices being
respected and initiated, right to the very end of their life.
The Royal College of Nursing (2015) recognizes the difficulty of complex thinking
about a passing patient and sees how patient care and symptoms must be
appropriately managed for an appropriate level of skill, knowledge and information to
be required. Nursing palliative thinking is presented as a proven based science that
requires advanced skills and knowledge, complex evaluation and empathy in equal
measure, which is delicate, dynamic, energetic and important. To achieve this
effectively, there should be an extensive amount of information and possible
preparation and capacity (Becker, 2009). Owen (2008) highlights how health care
et al (2017)feel although palliative care is sat under the umbrella of meeting the
needs for dying patients, in nursing homes, it is felt that one of the many problems
within these care providers is the lack of a structural approach in team working. It is
felt that this supports ethical challenges which then produce undignified care. There
are 4 main groups that have been highlighted and have been categorised as regular
problematic issues within how palliative, end of life nursing care is delivered within
nursing homes. These four main groups include medication knowledge,
communication around interpersonal relations with patients and other team
members, decision making including early planning around within advance care
planning and professional development including education, training, knowledge and
skills (Gorlén, Gorlén and Neergaard, 2013). From these findings there is evidence
of lack of early planning, the appropriate use of medication and detailed knowledge
around palliative and end of life care among care staff. These essential barriers
prevent patients from living a quality life for as long as possible and achieving good
end of life care and good deaths. This prevents patients’ wishes and choices being
respected and initiated, right to the very end of their life.
The Royal College of Nursing (2015) recognizes the difficulty of complex thinking
about a passing patient and sees how patient care and symptoms must be
appropriately managed for an appropriate level of skill, knowledge and information to
be required. Nursing palliative thinking is presented as a proven based science that
requires advanced skills and knowledge, complex evaluation and empathy in equal
measure, which is delicate, dynamic, energetic and important. To achieve this
effectively, there should be an extensive amount of information and possible
preparation and capacity (Becker, 2009). Owen (2008) highlights how health care
workers working in nursing homes feel inadequate to provide palliative and end-of-
life care due to lack of education and training. Patients who have a nursing home as
their primary place of residence are viewed as the most likely palliative care, end-of-
life needs, but these requirements are not seen or met due to lack of palliative
information and understanding Dixon, 2015). As patients and families do not trust the
right idea to be found in this climate, patients change their views where they want to
give it as they are approaching mental limit due to the nursing staff's inability to
control their own side effects. This results in only 43% of the population dying,
reaching their preferred place of death (Dixon, 2015). Nursing staff within nursing
homes admitted that they are inadequate to deal with their patients' problems
recalling difficulties in connecting with their patients during conversations. end of life
and managing complex symptoms by feeling strange and insecure (Towsely and
Hirschman 2018). Handley et al (2014) show that nursing staff working in nursing
homes believe that their level of knowledge and skills are underestimated.
Murphy-Jones and Timmons (2016) have described the difficult reality and
consequences of the failure of nursing staff to deal with the expected problems of
their patients weakening and the fact that patients have the constant transfer from
nursing homes to emergency departments and shifting to the narrow clinical work
area is narrowing. Murphy-Jones and Timmons, (2016) have described how basic
patient transfers from nursing home to emergency office occur when patients are
near a remarkable milestone. This has been said to be inappropriate, with negative
results and a loss of ability to consider critically and adequately. Kalseth and Antun
(2016) articulate their interests in migratory movements as patients approach death
and argue that this can be devastating. Concerns about medical clinical trials are
obvious and many clinical emergency measures have been interpreted as an
life care due to lack of education and training. Patients who have a nursing home as
their primary place of residence are viewed as the most likely palliative care, end-of-
life needs, but these requirements are not seen or met due to lack of palliative
information and understanding Dixon, 2015). As patients and families do not trust the
right idea to be found in this climate, patients change their views where they want to
give it as they are approaching mental limit due to the nursing staff's inability to
control their own side effects. This results in only 43% of the population dying,
reaching their preferred place of death (Dixon, 2015). Nursing staff within nursing
homes admitted that they are inadequate to deal with their patients' problems
recalling difficulties in connecting with their patients during conversations. end of life
and managing complex symptoms by feeling strange and insecure (Towsely and
Hirschman 2018). Handley et al (2014) show that nursing staff working in nursing
homes believe that their level of knowledge and skills are underestimated.
Murphy-Jones and Timmons (2016) have described the difficult reality and
consequences of the failure of nursing staff to deal with the expected problems of
their patients weakening and the fact that patients have the constant transfer from
nursing homes to emergency departments and shifting to the narrow clinical work
area is narrowing. Murphy-Jones and Timmons, (2016) have described how basic
patient transfers from nursing home to emergency office occur when patients are
near a remarkable milestone. This has been said to be inappropriate, with negative
results and a loss of ability to consider critically and adequately. Kalseth and Antun
(2016) articulate their interests in migratory movements as patients approach death
and argue that this can be devastating. Concerns about medical clinical trials are
obvious and many clinical emergency measures have been interpreted as an
inappropriate environment for end-of-life care. Paramedics often focus on a well-
being option that evaluates hospital risks and benefits when the patient has no more
boundaries. Martin, (2015) reports that more and more hospitals are in a medical
clinic because individuals are nearing the end of their lives, which is defined as
negative testing and an attempt to advance a palliative care approach. within nursing
homes. Unfortunately, this is not consistently achieved and, at times, when an
individual has lost the edge, a well-being choice should be made. This is presented
as an approximate judgment of what the patient would need if / when he / she was
constrained in thinking about beliefs, decisions, and attributes (Martin, 2015).
Paramedics found this inconsistent test to balance patient well-being with pressure
management by nurses working within observation homes (Murphy-Jones &
Timmons, 2016). Caring for the end of life is incredible, challenging and emotional
and can be daunting and controversial. To address these problems, there should be
a basic level of preparation and behavioral understanding within nursing homes to
achieve and ensure a correct standard of care (Hewison, Badger & Swani 2011).
Hewison, Badger and Swani (2011) highlight that the most critical and normal
landlord in end of life care in the UK reflects a lack of staff preparation at all levels.
Staff training within nursing homes is identified as one of the ten key changes
important to improve end-of-life care (Hewison, Badger & Swani, 2011). The NHS
Long-Term Slowdown Plan (2019) defines how their approach to coordinating
administrations to help more settled people keep them out of an addiction medical
clinic empowers and supports patients to live better for more. This includes the
forestry of approximately 50,000 planned clinical trials, with the goal that a portion of
these are patients approaching life care.
being option that evaluates hospital risks and benefits when the patient has no more
boundaries. Martin, (2015) reports that more and more hospitals are in a medical
clinic because individuals are nearing the end of their lives, which is defined as
negative testing and an attempt to advance a palliative care approach. within nursing
homes. Unfortunately, this is not consistently achieved and, at times, when an
individual has lost the edge, a well-being choice should be made. This is presented
as an approximate judgment of what the patient would need if / when he / she was
constrained in thinking about beliefs, decisions, and attributes (Martin, 2015).
Paramedics found this inconsistent test to balance patient well-being with pressure
management by nurses working within observation homes (Murphy-Jones &
Timmons, 2016). Caring for the end of life is incredible, challenging and emotional
and can be daunting and controversial. To address these problems, there should be
a basic level of preparation and behavioral understanding within nursing homes to
achieve and ensure a correct standard of care (Hewison, Badger & Swani 2011).
Hewison, Badger and Swani (2011) highlight that the most critical and normal
landlord in end of life care in the UK reflects a lack of staff preparation at all levels.
Staff training within nursing homes is identified as one of the ten key changes
important to improve end-of-life care (Hewison, Badger & Swani, 2011). The NHS
Long-Term Slowdown Plan (2019) defines how their approach to coordinating
administrations to help more settled people keep them out of an addiction medical
clinic empowers and supports patients to live better for more. This includes the
forestry of approximately 50,000 planned clinical trials, with the goal that a portion of
these are patients approaching life care.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Chapter Three
Methodology:
By formulating a qualitative questionnaire around palliative and end of life care,
asking several questions to underpin the level of knowledge these nurses
understand, allows there to be an opportunity for care improvement. The
questionnaire will cover different aspects of basic nursing skills that are essential and
required to offer a broad understanding around palliative and end of life care. The
formulated questions used with be open ended, meaning that the nurses will have to
elaborate on their answers as opposed to a tick box exercise. Harland and Holey
(2011) explain how open-ended questions when used within questionnaire
methodology can enhance depth and value to the results and conclusion within
research studies. The questionnaires will include a rudimentary understand of
palliative, end of life care, skills and opportunities that should encompass this
including advance care planning, preferred place of care and death considerations
and understanding of signs and symptoms and how to manage these. Three
different nursing homes, within different locations with be targeted, requesting
consent from the nursing home managers for their nurses to complete the
questionnaires in order to give a viable result and an indication of the level of
understanding and improvements that need to be made. It is felt that this will be
achieved through the offering of a qualitative research approach. Chirwatkul,
(2014)describe qualitative research as a problem-solving, culturally sensitive method
that can influence improvements in health. Qualitative study has been defined as
having the ability to increase health equity and equality and has the potential to
make a positive difference in health at a global level. Nilsson Kajermo et al (2014)
express how the creation of new knowledge is ongoing with the importance of patient
Methodology:
By formulating a qualitative questionnaire around palliative and end of life care,
asking several questions to underpin the level of knowledge these nurses
understand, allows there to be an opportunity for care improvement. The
questionnaire will cover different aspects of basic nursing skills that are essential and
required to offer a broad understanding around palliative and end of life care. The
formulated questions used with be open ended, meaning that the nurses will have to
elaborate on their answers as opposed to a tick box exercise. Harland and Holey
(2011) explain how open-ended questions when used within questionnaire
methodology can enhance depth and value to the results and conclusion within
research studies. The questionnaires will include a rudimentary understand of
palliative, end of life care, skills and opportunities that should encompass this
including advance care planning, preferred place of care and death considerations
and understanding of signs and symptoms and how to manage these. Three
different nursing homes, within different locations with be targeted, requesting
consent from the nursing home managers for their nurses to complete the
questionnaires in order to give a viable result and an indication of the level of
understanding and improvements that need to be made. It is felt that this will be
achieved through the offering of a qualitative research approach. Chirwatkul,
(2014)describe qualitative research as a problem-solving, culturally sensitive method
that can influence improvements in health. Qualitative study has been defined as
having the ability to increase health equity and equality and has the potential to
make a positive difference in health at a global level. Nilsson Kajermo et al (2014)
express how the creation of new knowledge is ongoing with the importance of patient
safety and evidence-based practice being a priority for the NHS. Most primary
research is formulated within questionnaires. Questionnaires provide an opportunity
of validity and reliability and provide a tool to monitor and reflect on clinicians’ skills
but also facilitate an opportunity for discussion (Kirkpatrick et al., 2019). From the
literature supporting this initiative, these choices of methods were introduced.
This formulated primary research questionnaire will focus on a qualitative structure to
enable a detailed, honest outlook on current levels of care that are actively been
received. Parton (2015) describes qualitative research as a powerful source of
grounded theory that is produced from investigation within the “real world” as
opposed to laboratory or academia. When using a qualitative research method, it is
helpful to utilise a design that can be followed. Parton (2015) has designed a
strategy that can be completed to support the design of a research project. The
areas to be considered are:
1) Goals:
- Why is the research worth completing and potential issues to be
considered?
- This can include clarifying what practices and policies can this research
influence.
2) Conceptual framework:
- including what theories, beliefs and prior research findings that could
influence research outcomes.
- How literature, initial studies and personal experience could support the
understanding of the research.
3) Research Question:
research is formulated within questionnaires. Questionnaires provide an opportunity
of validity and reliability and provide a tool to monitor and reflect on clinicians’ skills
but also facilitate an opportunity for discussion (Kirkpatrick et al., 2019). From the
literature supporting this initiative, these choices of methods were introduced.
This formulated primary research questionnaire will focus on a qualitative structure to
enable a detailed, honest outlook on current levels of care that are actively been
received. Parton (2015) describes qualitative research as a powerful source of
grounded theory that is produced from investigation within the “real world” as
opposed to laboratory or academia. When using a qualitative research method, it is
helpful to utilise a design that can be followed. Parton (2015) has designed a
strategy that can be completed to support the design of a research project. The
areas to be considered are:
1) Goals:
- Why is the research worth completing and potential issues to be
considered?
- This can include clarifying what practices and policies can this research
influence.
2) Conceptual framework:
- including what theories, beliefs and prior research findings that could
influence research outcomes.
- How literature, initial studies and personal experience could support the
understanding of the research.
3) Research Question:
- What can be gained from the study and what questions will be answered
to support the initial theory.
4) Methods:
- In conducting the study, which techniques will be used to collect and then
analysis the data?
5) Validity:
- How the quality of the research is factually found in suspect of credibility,
reliability and justifiability.
Using this framework as a guide to the primary research that will be completed within
this study, this will be reflected:
1) Goals:
The goal has been developed through personal and professional experience but has
been supported through identifying current literature to sustenance the concept that
qualified nursing staff working in nursing homes do not have the knowledge and
skills required to offer the best care to patients at the end of life.
2) Conceptual framework:
Evidence found within the literature review supports the need for further research to
be completed. There has been an identified level of care standard that reduces
within a nursing home setting when end of life care is given. Potential issues to be
considered could be that the nursing team do not feel that their level of care needs to
be improved and are “comfortable” with the level of care that is offered. Evidence
based practice is central to individuals’ preferences, choices, wishes and clinical
judgement. With encompassing the development within relationships and effective
communication, this allows professionals to underpin what clinical intervention will be
the most effective. However, care providers face daily challenges which prevent
to support the initial theory.
4) Methods:
- In conducting the study, which techniques will be used to collect and then
analysis the data?
5) Validity:
- How the quality of the research is factually found in suspect of credibility,
reliability and justifiability.
Using this framework as a guide to the primary research that will be completed within
this study, this will be reflected:
1) Goals:
The goal has been developed through personal and professional experience but has
been supported through identifying current literature to sustenance the concept that
qualified nursing staff working in nursing homes do not have the knowledge and
skills required to offer the best care to patients at the end of life.
2) Conceptual framework:
Evidence found within the literature review supports the need for further research to
be completed. There has been an identified level of care standard that reduces
within a nursing home setting when end of life care is given. Potential issues to be
considered could be that the nursing team do not feel that their level of care needs to
be improved and are “comfortable” with the level of care that is offered. Evidence
based practice is central to individuals’ preferences, choices, wishes and clinical
judgement. With encompassing the development within relationships and effective
communication, this allows professionals to underpin what clinical intervention will be
the most effective. However, care providers face daily challenges which prevent
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
evidence-based practice in being delivered. This includes perceptions of having lack
of training, knowledge, time and access to relevant information. The Nursing and
Midwifery Code of Conduct (NMC) (2018) states that nurses must practice with the
“best available evidence”. For this to be achieved, qualified nurses must ensure that
any information, advice, knowledge and skill is evidence based to pledge safe and
effective care.
3) Research question:
From completing the primary research there will be reliable evidence to either
support or disagree with the literature identified above. From the detailed
questionnaire, it will be evident if nurses understand the basics of palliative and end
of life care or if improvements need to be made.
4) Methods:
The method used will be a hand delivered questionnaire with a completion date. The
data will then be collected, and each question analysed and compared to their fellow
professionals who offer the same care but potentially at a different standard.
5) Validity:
The respondents will complete the questionnaires anonymously therefore offering an
unbiased and confidential response to justify that questions will be answered
honestly to remove any concerns by the respondents and support the reliability of
the research.
The participants who will be completing the questionnaires are nurses who regularly
give palliative and end of life care to their regular residents. The geographic area will
be within 10 miles of each other, all covering the northern Lancashire area which has
a natural increase in the population being over the age of 75 years. The research
conductor will liaise with the nursing home manager prior to the delivery of the
of training, knowledge, time and access to relevant information. The Nursing and
Midwifery Code of Conduct (NMC) (2018) states that nurses must practice with the
“best available evidence”. For this to be achieved, qualified nurses must ensure that
any information, advice, knowledge and skill is evidence based to pledge safe and
effective care.
3) Research question:
From completing the primary research there will be reliable evidence to either
support or disagree with the literature identified above. From the detailed
questionnaire, it will be evident if nurses understand the basics of palliative and end
of life care or if improvements need to be made.
4) Methods:
The method used will be a hand delivered questionnaire with a completion date. The
data will then be collected, and each question analysed and compared to their fellow
professionals who offer the same care but potentially at a different standard.
5) Validity:
The respondents will complete the questionnaires anonymously therefore offering an
unbiased and confidential response to justify that questions will be answered
honestly to remove any concerns by the respondents and support the reliability of
the research.
The participants who will be completing the questionnaires are nurses who regularly
give palliative and end of life care to their regular residents. The geographic area will
be within 10 miles of each other, all covering the northern Lancashire area which has
a natural increase in the population being over the age of 75 years. The research
conductor will liaise with the nursing home manager prior to the delivery of the
questionnaires to ensure informed consent (please see Appendix A) has been
gained from the care provider manager. Once gained, a clear explanation and goal
will be discussed with the manager and each nursing team member, ensuring a
trusting relationship is established, all within confidentiality boundaries. It will be
discussed in detail that participants can have the opportunity to withdraw at any time,
that none of the findings will be exploited unless a need for safeguarding escalation
is identified and all having a common goal which is to improve patient care(please
see Appendix B).
Prior to this research being introduced an ethics form has been completed (please
see Appendix C)
Validity can be described as the extent to which the understandings of the results are
warranted (Kimberlin and Winterstein, 2008).
Study Overview
To identify reduced standards of care within nursing homes due to lack of
knowledge, experience and skills. By recognising the need for additional training and
support this will untimely improve patient end of life experiences and reduce
pressures within NHS services. By conducting this piece of primary research, this will
highlight the evidence that this needs to be addressed and action planned.
Inclusion criteria:
Persons who fit the criteria will be qualified nurses with or without experiences in
palliative care. The participants must have a nursing qualification, but this does not
have to be at degree level. The professionals must be working at a nursing home
and currently on the nursing midwifery council register (NMC).
gained from the care provider manager. Once gained, a clear explanation and goal
will be discussed with the manager and each nursing team member, ensuring a
trusting relationship is established, all within confidentiality boundaries. It will be
discussed in detail that participants can have the opportunity to withdraw at any time,
that none of the findings will be exploited unless a need for safeguarding escalation
is identified and all having a common goal which is to improve patient care(please
see Appendix B).
Prior to this research being introduced an ethics form has been completed (please
see Appendix C)
Validity can be described as the extent to which the understandings of the results are
warranted (Kimberlin and Winterstein, 2008).
Study Overview
To identify reduced standards of care within nursing homes due to lack of
knowledge, experience and skills. By recognising the need for additional training and
support this will untimely improve patient end of life experiences and reduce
pressures within NHS services. By conducting this piece of primary research, this will
highlight the evidence that this needs to be addressed and action planned.
Inclusion criteria:
Persons who fit the criteria will be qualified nurses with or without experiences in
palliative care. The participants must have a nursing qualification, but this does not
have to be at degree level. The professionals must be working at a nursing home
and currently on the nursing midwifery council register (NMC).
Exclusion criteria:
Nurses who are not permanently working at the nursing home and/or have a job
within the NHS will be excluded. Carers/nursing assistants will not be permitted to
complete the questionnaires as the research is to gather a level of understanding
within staff already having a nursing qualification.
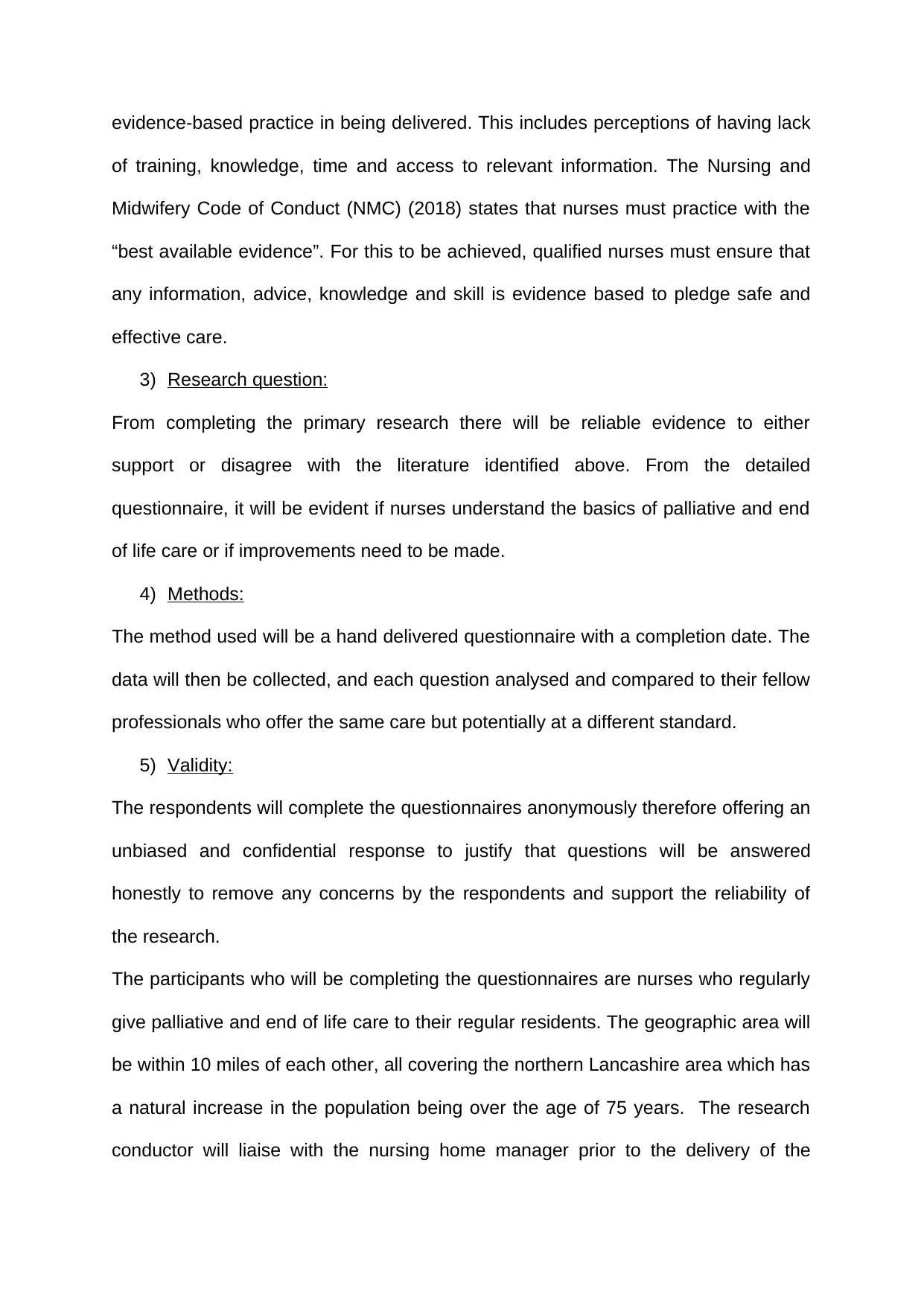
Timescales:
The research will be conducted, and data analysed between May – July 2019. This
will be presented within the completed dissertation by September 2019. The gantt
chart is a timeline used to illustrate how the research project will run. Individual tasks
can be broken down and viewed and will ensure the expected completion date is
met.
See Gant chart below for time scale breakdown:
Time Scale: May
2019
June
2019
July
2019
August
2019
September
2019
Discussion with
management
Distribution of
questionnaires
Collection of
questionnaires
Data Gathering
Collation of data
Report write up
Nurses who are not permanently working at the nursing home and/or have a job
within the NHS will be excluded. Carers/nursing assistants will not be permitted to
complete the questionnaires as the research is to gather a level of understanding
within staff already having a nursing qualification.
Timescales:
The research will be conducted, and data analysed between May – July 2019. This
will be presented within the completed dissertation by September 2019. The gantt
chart is a timeline used to illustrate how the research project will run. Individual tasks
can be broken down and viewed and will ensure the expected completion date is
met.
See Gant chart below for time scale breakdown:
Time Scale: May
2019
June
2019
July
2019
August
2019
September
2019
Discussion with
management
Distribution of
questionnaires
Collection of
questionnaires
Data Gathering
Collation of data
Report write up
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Within the timescale several tasks have been highlighted that need completing. The
first achievement is to have the initial discussion with the manager of the nursing
homes and gain consent for their staff and care home to take part within this
research project. This needs to have been achieved by the end of May. Following
consent been gained, the distribution of questionnaires will be completed by the
beginning of June, allowing the participants an achievable timescale for these to be
completed. Questionnaires will be collected by the end of June which gives the
researcher the required time for the data to be gathered throughout July and analysis
to commence. Following this the collation of data will be analysed during the middle
of July to the middle of august, with the final report being completed by the due date
in September 2019.
Ethical Considerations:
Ethical deliberations should be considered within all primary research. The factors
that will be measured within this assignment is the use of confidentiality, informed
consent and anonymity as discussed above. Clark (2019) describes ethics as a
formal procedure that is a cornerstone for formulating meaningful and effective
research and protection of participants. Ethics in relation to conducting research
achieves this protection by obtaining consent, always maintaining privacy and
confidentiality and avoiding harm (Clark, 2019).
Outcomes:
The outcomes will be defined by the results of the questionnaire.
Intervention:
Following the completion of the primary research study and dependent on at what
extent the nurses within the nursing homes require to maintain a safe and effected
first achievement is to have the initial discussion with the manager of the nursing
homes and gain consent for their staff and care home to take part within this
research project. This needs to have been achieved by the end of May. Following
consent been gained, the distribution of questionnaires will be completed by the
beginning of June, allowing the participants an achievable timescale for these to be
completed. Questionnaires will be collected by the end of June which gives the
researcher the required time for the data to be gathered throughout July and analysis
to commence. Following this the collation of data will be analysed during the middle
of July to the middle of august, with the final report being completed by the due date
in September 2019.
Ethical Considerations:
Ethical deliberations should be considered within all primary research. The factors
that will be measured within this assignment is the use of confidentiality, informed
consent and anonymity as discussed above. Clark (2019) describes ethics as a
formal procedure that is a cornerstone for formulating meaningful and effective
research and protection of participants. Ethics in relation to conducting research
achieves this protection by obtaining consent, always maintaining privacy and
confidentiality and avoiding harm (Clark, 2019).
Outcomes:
The outcomes will be defined by the results of the questionnaire.
Intervention:
Following the completion of the primary research study and dependent on at what
extent the nurses within the nursing homes require to maintain a safe and effected
level of nursing care, a NHS funded palliative care training programme is to be
developed and delivered within nursing homes to improve palliative and patient end
of life care. From this service opportunity it will enable patients to stay in their
preferred place of care and achieve their preferred place of death, allowing nurses to
feel confident and competent around managing complex symptoms and supporting
patients and their families during these difficult times. This will ultimately give
patients a ‘good death’, but also offer a long-term positive implication on finance
reduction in NHS services by reducing the pressures on community services. This is
in hope that those within the nursing homes will only be accessing specialist services
when their management and care becomes “complex” and requires that specialist
support.
Data Extract:
The data will be extracted and analysed once all questionnaires have been
completed and handed back. This will then lead onto the dissertation of the research
report where the results will be presented and discussed.
developed and delivered within nursing homes to improve palliative and patient end
of life care. From this service opportunity it will enable patients to stay in their
preferred place of care and achieve their preferred place of death, allowing nurses to
feel confident and competent around managing complex symptoms and supporting
patients and their families during these difficult times. This will ultimately give
patients a ‘good death’, but also offer a long-term positive implication on finance
reduction in NHS services by reducing the pressures on community services. This is
in hope that those within the nursing homes will only be accessing specialist services
when their management and care becomes “complex” and requires that specialist
support.
Data Extract:
The data will be extracted and analysed once all questionnaires have been
completed and handed back. This will then lead onto the dissertation of the research
report where the results will be presented and discussed.
Chapter Four
Results:
Prior to the final questionnaires been sent out for completion, a pilot was first
conducted. This was supplemented by participants of the scientist's current work
base. Since the first study was completed and the results of the exchange and
current research were exchanged, changes have been made to accommodate this
idea. This reminded me of the format change and the requests that were sent.
From the updates mentioned in the polls, these have been distributed to nursing
homes. Each nursing home was given a full-time scale to complete these studies to
allow time for annual leave, illnesses and other human components.
However, while it was thought to be time consuming, one of these four nursing
homes sadly did not complete as planned. Some of the classifiers had gone on
annual leave, the rest of the group had not been given the cut-off time or field of
study and so only 2 out of 10 studies had been completed. Fortunately, the other 3
nursing homes figured out how to complete all the inspections that allowed this room
to make a mistake.
Using contemporary analysis, the results were broken down and explained in detail
in pie charts. Subjective analysis is a methodological tool used to analyze and
understand internal and external information (Lawless and Chen 2019). If there is not
too much trouble, take a look below.
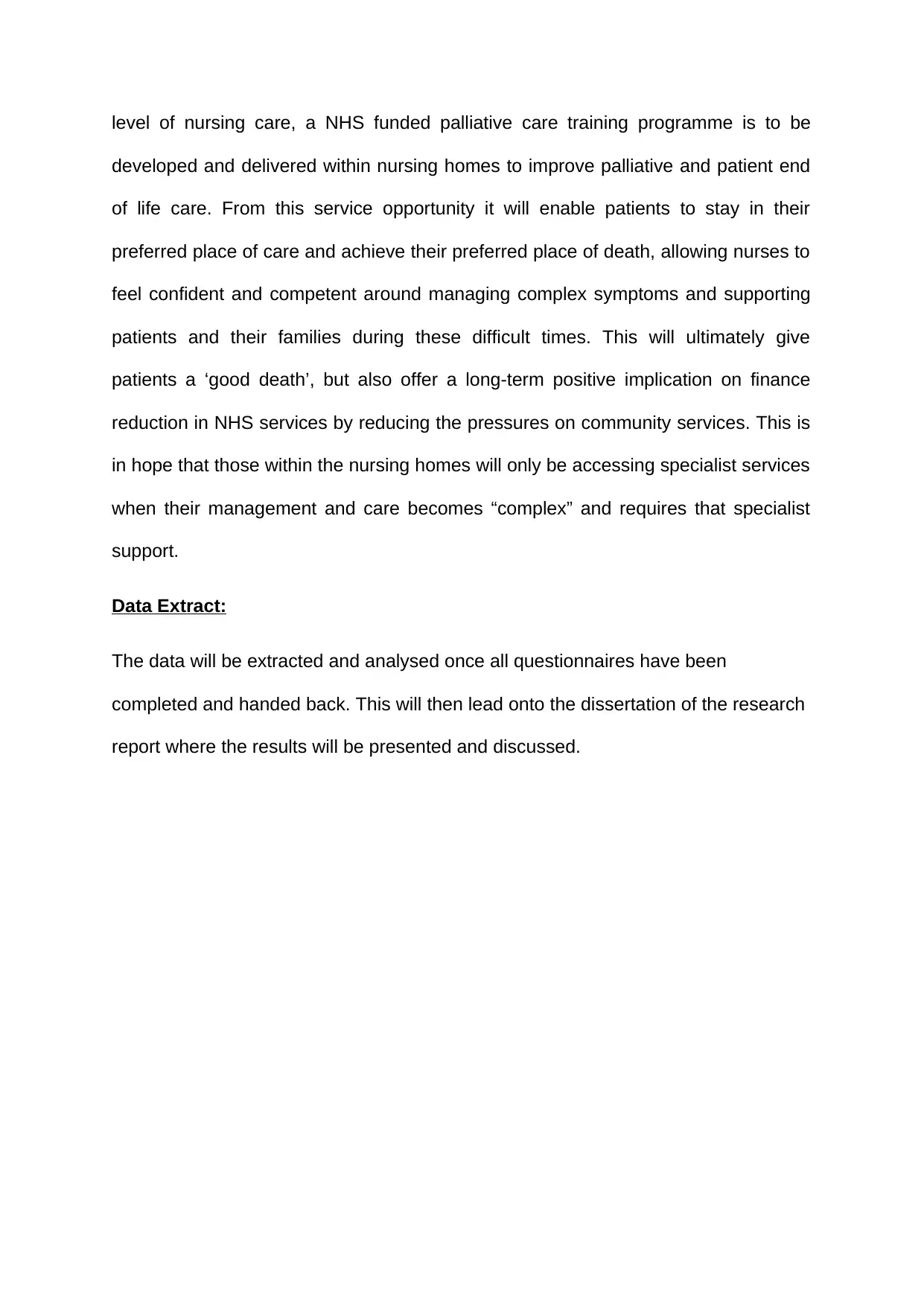
Question 1
How long have you been a qualified nurse?
Results:
Prior to the final questionnaires been sent out for completion, a pilot was first
conducted. This was supplemented by participants of the scientist's current work
base. Since the first study was completed and the results of the exchange and
current research were exchanged, changes have been made to accommodate this
idea. This reminded me of the format change and the requests that were sent.
From the updates mentioned in the polls, these have been distributed to nursing
homes. Each nursing home was given a full-time scale to complete these studies to
allow time for annual leave, illnesses and other human components.
However, while it was thought to be time consuming, one of these four nursing
homes sadly did not complete as planned. Some of the classifiers had gone on
annual leave, the rest of the group had not been given the cut-off time or field of
study and so only 2 out of 10 studies had been completed. Fortunately, the other 3
nursing homes figured out how to complete all the inspections that allowed this room
to make a mistake.
Using contemporary analysis, the results were broken down and explained in detail
in pie charts. Subjective analysis is a methodological tool used to analyze and
understand internal and external information (Lawless and Chen 2019). If there is not
too much trouble, take a look below.
Question 1
How long have you been a qualified nurse?
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1st Qtr
1-10 Years
11-20 Years
21-30 Years
31-40 Years
40+ Years
No recently qualified nurses worked at the nursing home with over 50% of the nurses
being qualified over 25 years.
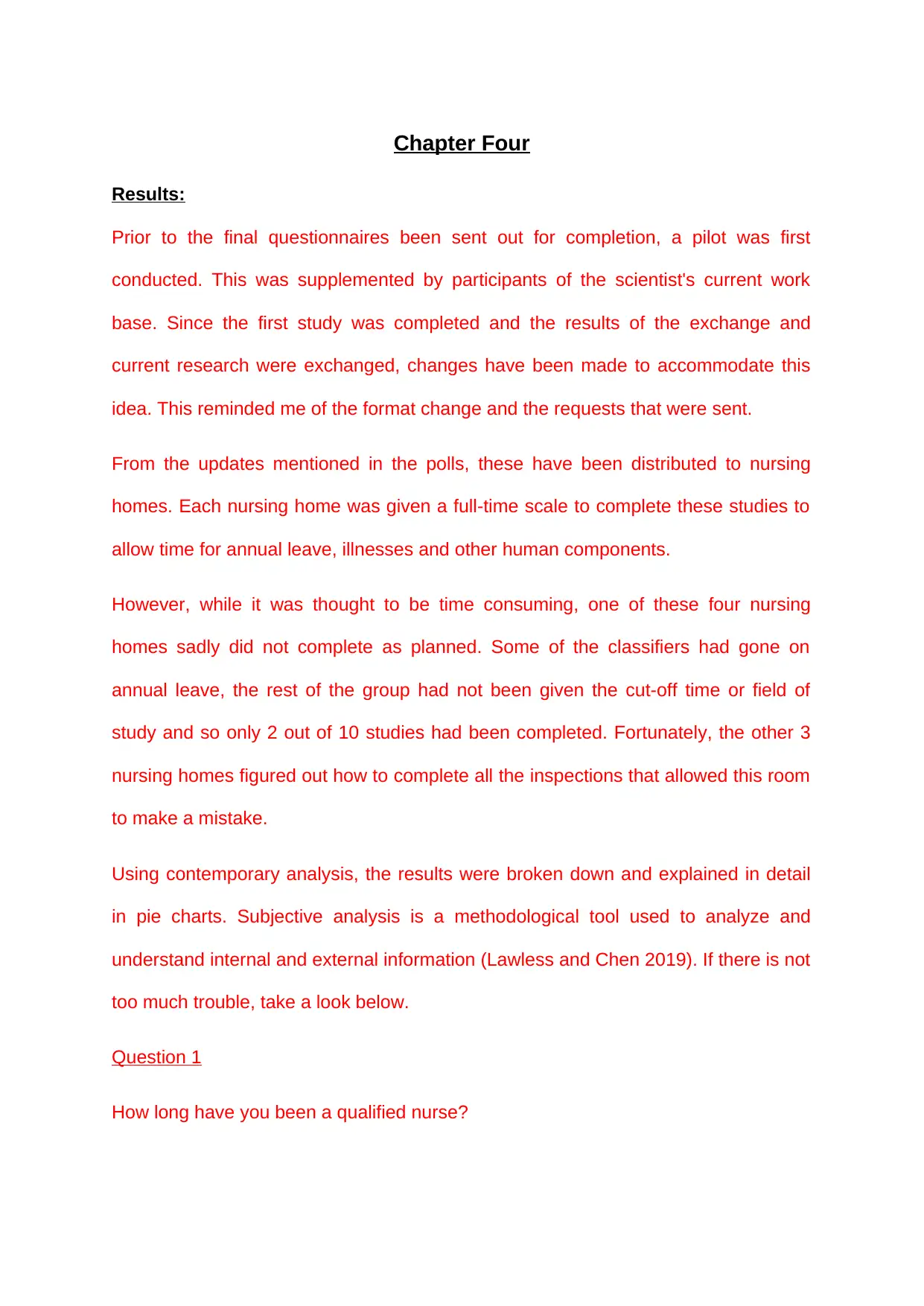
Question 2
How long have you been working within this nursing home?
Pie 1
0 - 12 Months
1-5 Years
6-10 Years
11-20 Years
21-30 Years
30+ Years
38% of nurses had worked in the nursing homes for less than 5 years, with one
nurse having worked there for 9 months. 62% of the rest of the nursing staff had
worked there for over 5 years.
1-10 Years
11-20 Years
21-30 Years
31-40 Years
40+ Years
No recently qualified nurses worked at the nursing home with over 50% of the nurses
being qualified over 25 years.
Question 2
How long have you been working within this nursing home?
Pie 1
0 - 12 Months
1-5 Years
6-10 Years
11-20 Years
21-30 Years
30+ Years
38% of nurses had worked in the nursing homes for less than 5 years, with one
nurse having worked there for 9 months. 62% of the rest of the nursing staff had
worked there for over 5 years.
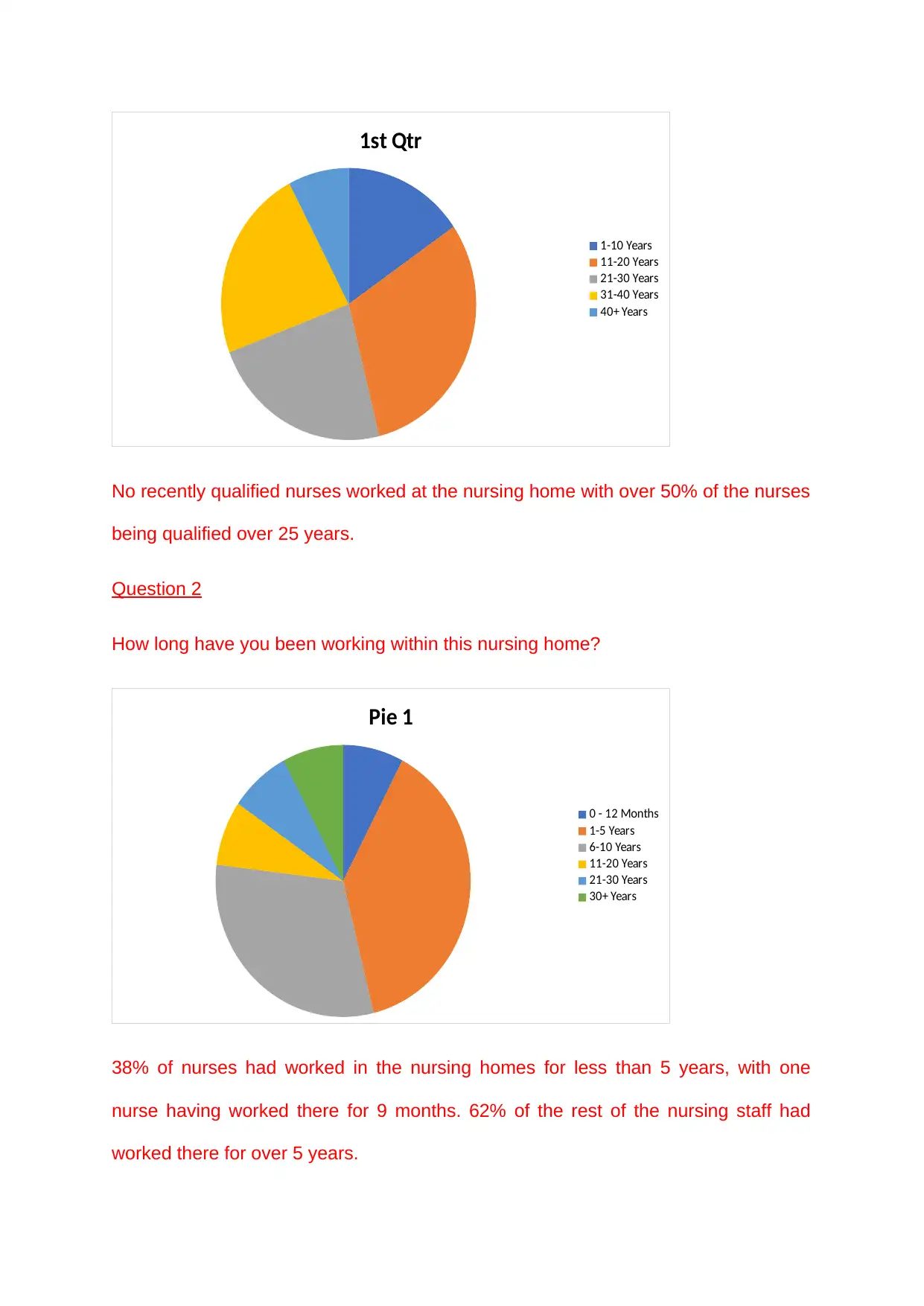
Question 3
What level of qualification do you hold? (Certificate/ diploma/ advanced diploma/
degree).
Certificate
Diploma
Advanced Diploma
Degree
More than 50% of the nurses had certificate level qualification due to the number of
years they had been qualified. Only 15% had obtained degree level.
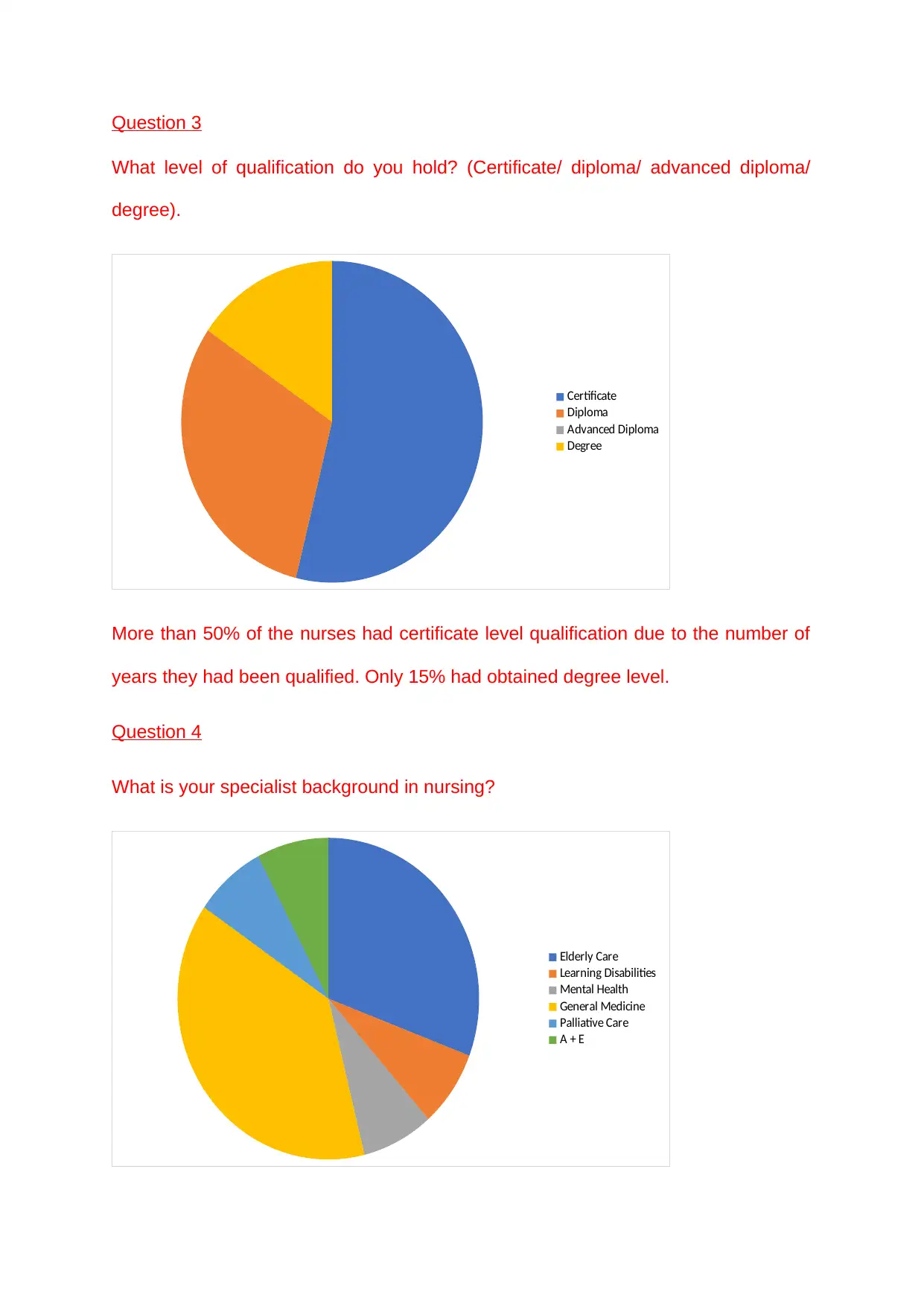
Question 4
What is your specialist background in nursing?
Elderly Care
Learning Disabilities
Mental Health
General Medicine
Palliative Care
A + E
What level of qualification do you hold? (Certificate/ diploma/ advanced diploma/
degree).
Certificate
Diploma
Advanced Diploma
Degree
More than 50% of the nurses had certificate level qualification due to the number of
years they had been qualified. Only 15% had obtained degree level.
Question 4
What is your specialist background in nursing?
Elderly Care
Learning Disabilities
Mental Health
General Medicine
Palliative Care
A + E
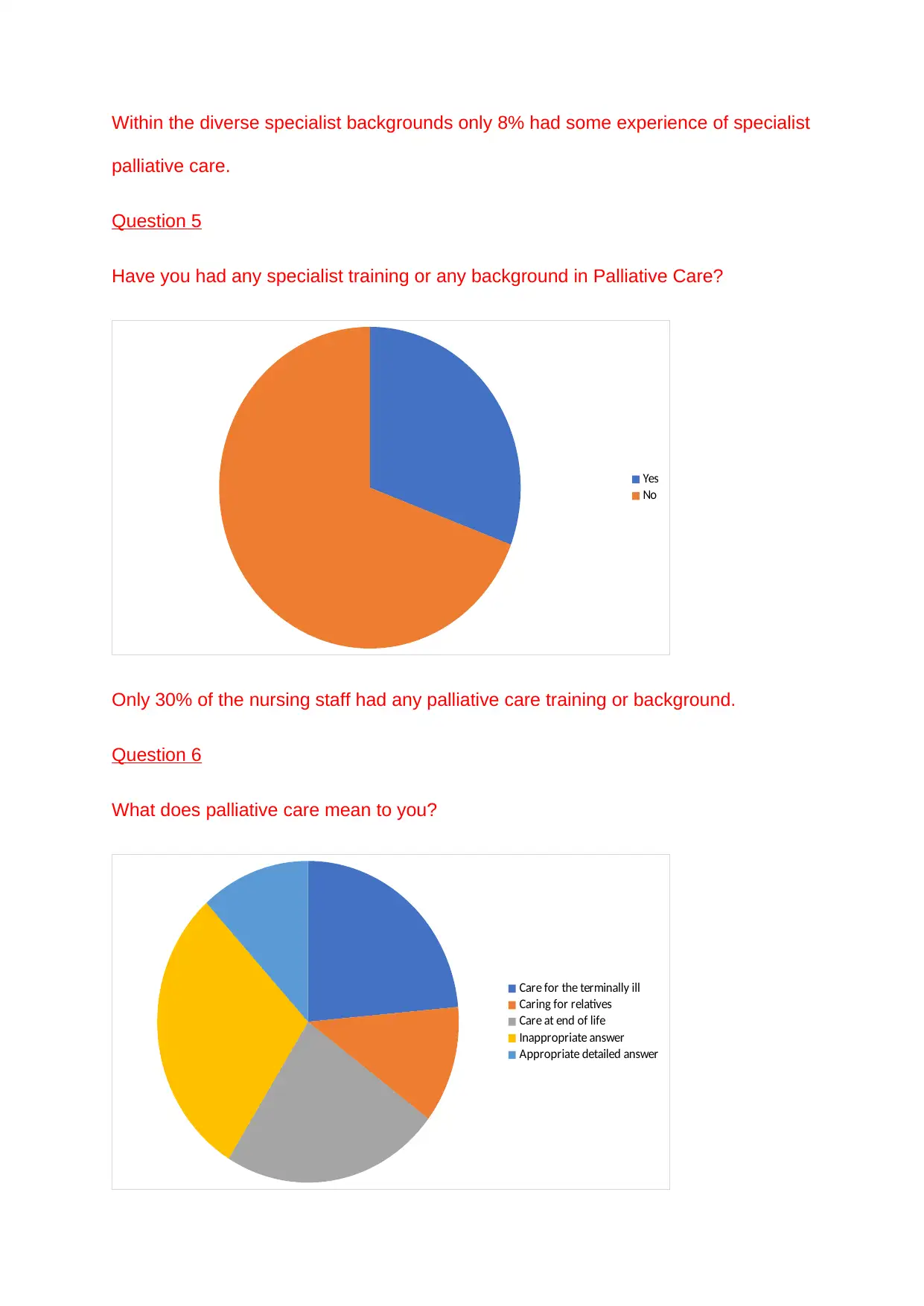
Within the diverse specialist backgrounds only 8% had some experience of specialist
palliative care.
Question 5
Have you had any specialist training or any background in Palliative Care?
Yes
No
Only 30% of the nursing staff had any palliative care training or background.
Question 6
What does palliative care mean to you?
Care for the terminally ill
Caring for relatives
Care at end of life
Inappropriate answer
Appropriate detailed answer
palliative care.
Question 5
Have you had any specialist training or any background in Palliative Care?
Yes
No
Only 30% of the nursing staff had any palliative care training or background.
Question 6
What does palliative care mean to you?
Care for the terminally ill
Caring for relatives
Care at end of life
Inappropriate answer
Appropriate detailed answer
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
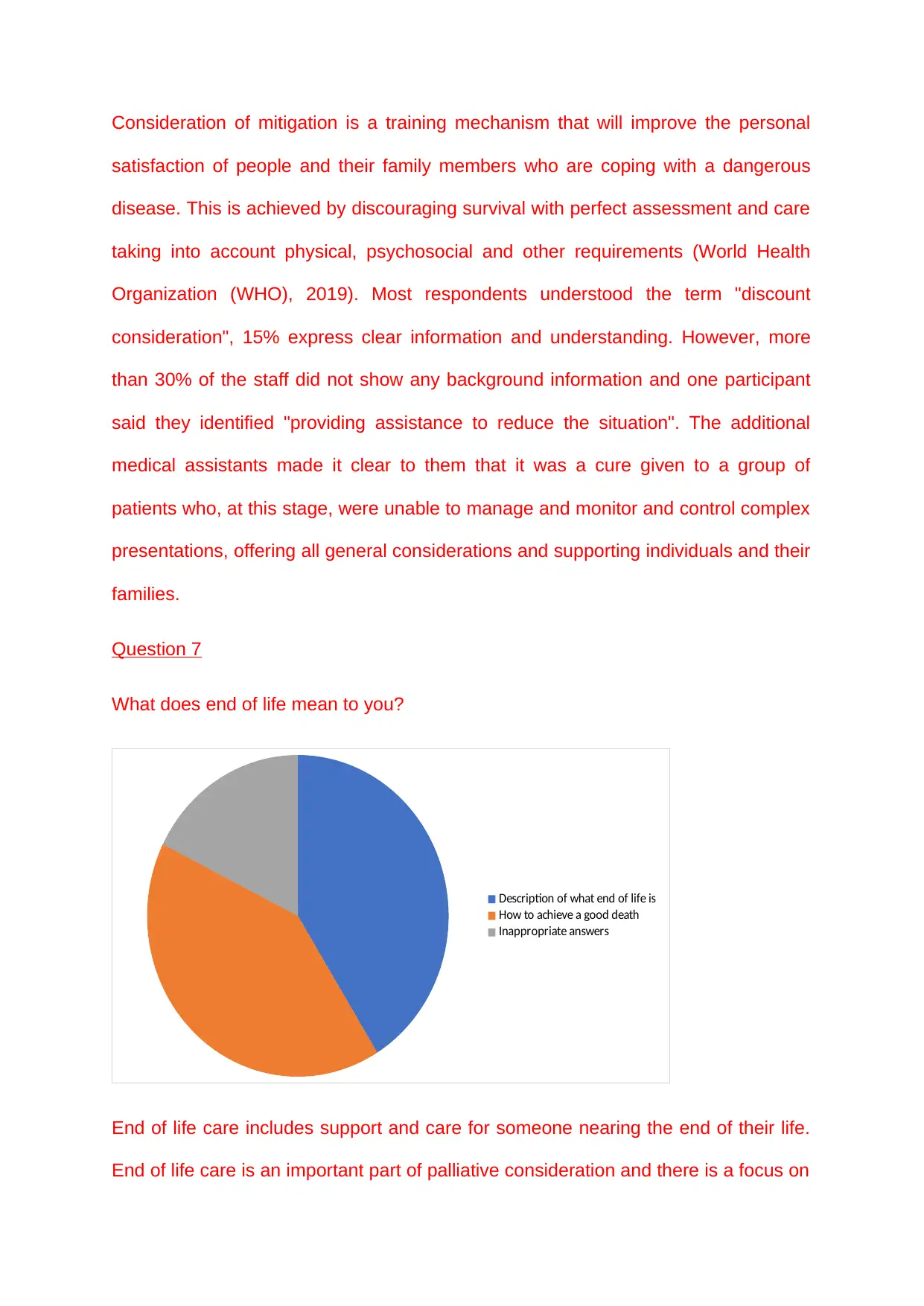
Consideration of mitigation is a training mechanism that will improve the personal
satisfaction of people and their family members who are coping with a dangerous
disease. This is achieved by discouraging survival with perfect assessment and care
taking into account physical, psychosocial and other requirements (World Health
Organization (WHO), 2019). Most respondents understood the term "discount
consideration", 15% express clear information and understanding. However, more
than 30% of the staff did not show any background information and one participant
said they identified "providing assistance to reduce the situation". The additional
medical assistants made it clear to them that it was a cure given to a group of
patients who, at this stage, were unable to manage and monitor and control complex
presentations, offering all general considerations and supporting individuals and their
families.
Question 7
What does end of life mean to you?
Description of what end of life is
How to achieve a good death
Inappropriate answers
End of life care includes support and care for someone nearing the end of their life.
End of life care is an important part of palliative consideration and there is a focus on
satisfaction of people and their family members who are coping with a dangerous
disease. This is achieved by discouraging survival with perfect assessment and care
taking into account physical, psychosocial and other requirements (World Health
Organization (WHO), 2019). Most respondents understood the term "discount
consideration", 15% express clear information and understanding. However, more
than 30% of the staff did not show any background information and one participant
said they identified "providing assistance to reduce the situation". The additional
medical assistants made it clear to them that it was a cure given to a group of
patients who, at this stage, were unable to manage and monitor and control complex
presentations, offering all general considerations and supporting individuals and their
families.
Question 7
What does end of life mean to you?
Description of what end of life is
How to achieve a good death
Inappropriate answers
End of life care includes support and care for someone nearing the end of their life.
End of life care is an important part of palliative consideration and there is a focus on
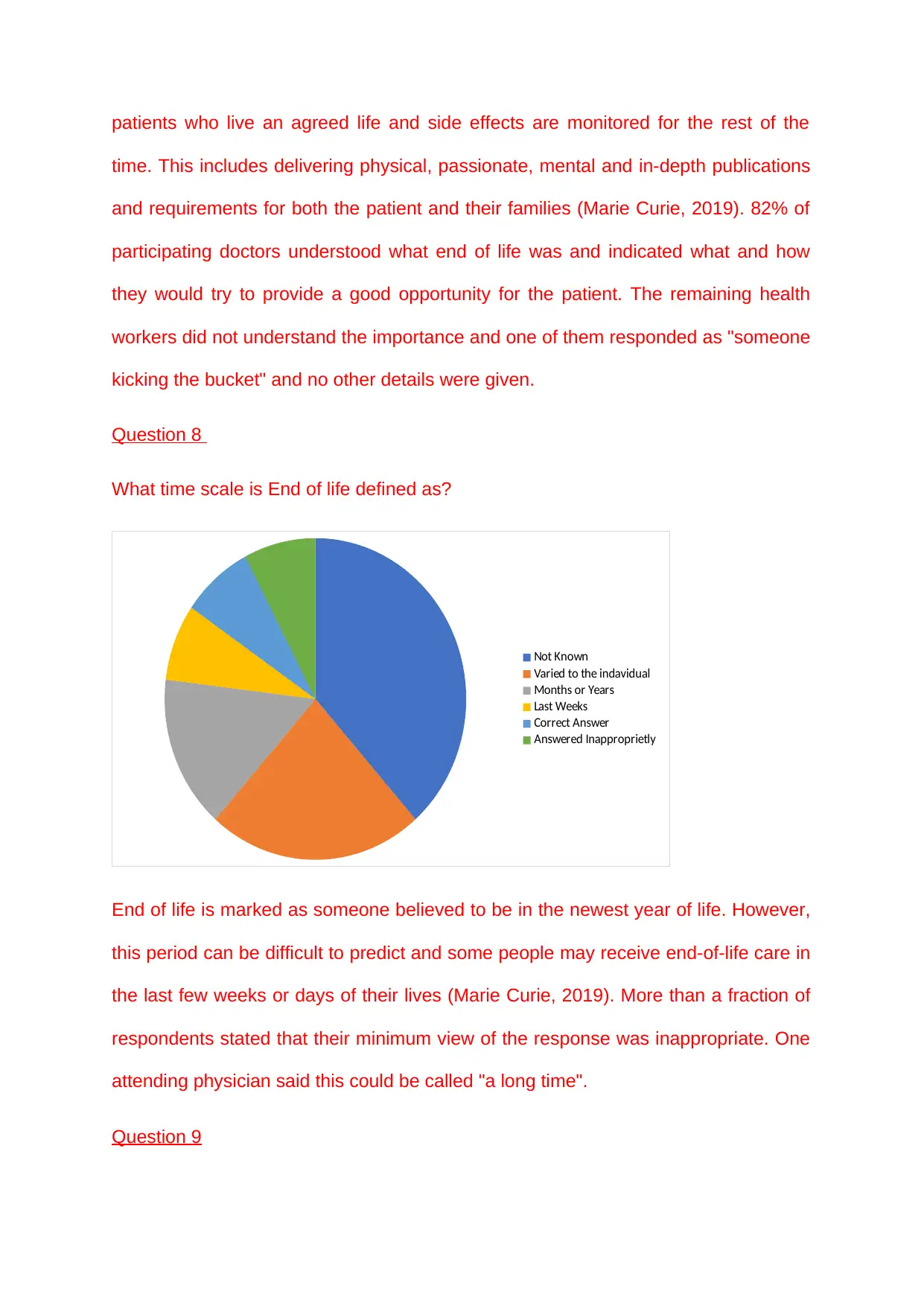
patients who live an agreed life and side effects are monitored for the rest of the
time. This includes delivering physical, passionate, mental and in-depth publications
and requirements for both the patient and their families (Marie Curie, 2019). 82% of
participating doctors understood what end of life was and indicated what and how
they would try to provide a good opportunity for the patient. The remaining health
workers did not understand the importance and one of them responded as "someone
kicking the bucket" and no other details were given.
Question 8
What time scale is End of life defined as?
Not Known
Varied to the indavidual
Months or Years
Last Weeks
Correct Answer
Answered Inapproprietly
End of life is marked as someone believed to be in the newest year of life. However,
this period can be difficult to predict and some people may receive end-of-life care in
the last few weeks or days of their lives (Marie Curie, 2019). More than a fraction of
respondents stated that their minimum view of the response was inappropriate. One
attending physician said this could be called "a long time".
Question 9
time. This includes delivering physical, passionate, mental and in-depth publications
and requirements for both the patient and their families (Marie Curie, 2019). 82% of
participating doctors understood what end of life was and indicated what and how
they would try to provide a good opportunity for the patient. The remaining health
workers did not understand the importance and one of them responded as "someone
kicking the bucket" and no other details were given.
Question 8
What time scale is End of life defined as?
Not Known
Varied to the indavidual
Months or Years
Last Weeks
Correct Answer
Answered Inapproprietly
End of life is marked as someone believed to be in the newest year of life. However,
this period can be difficult to predict and some people may receive end-of-life care in
the last few weeks or days of their lives (Marie Curie, 2019). More than a fraction of
respondents stated that their minimum view of the response was inappropriate. One
attending physician said this could be called "a long time".
Question 9
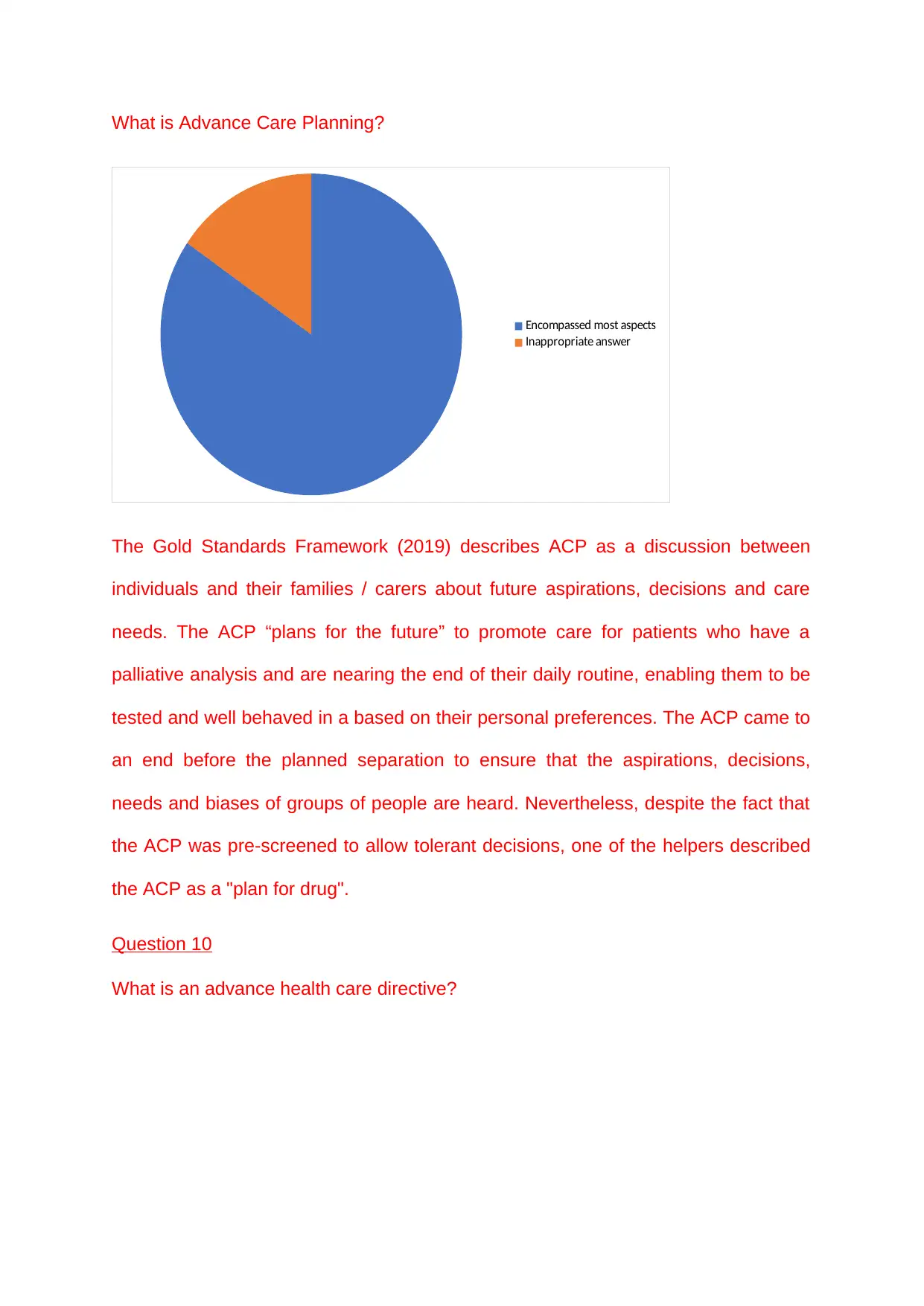
What is Advance Care Planning?
Encompassed most aspects
Inappropriate answer
The Gold Standards Framework (2019) describes ACP as a discussion between
individuals and their families / carers about future aspirations, decisions and care
needs. The ACP “plans for the future” to promote care for patients who have a
palliative analysis and are nearing the end of their daily routine, enabling them to be
tested and well behaved in a based on their personal preferences. The ACP came to
an end before the planned separation to ensure that the aspirations, decisions,
needs and biases of groups of people are heard. Nevertheless, despite the fact that
the ACP was pre-screened to allow tolerant decisions, one of the helpers described
the ACP as a "plan for drug".
Question 10
What is an advance health care directive?
Encompassed most aspects
Inappropriate answer
The Gold Standards Framework (2019) describes ACP as a discussion between
individuals and their families / carers about future aspirations, decisions and care
needs. The ACP “plans for the future” to promote care for patients who have a
palliative analysis and are nearing the end of their daily routine, enabling them to be
tested and well behaved in a based on their personal preferences. The ACP came to
an end before the planned separation to ensure that the aspirations, decisions,
needs and biases of groups of people are heard. Nevertheless, despite the fact that
the ACP was pre-screened to allow tolerant decisions, one of the helpers described
the ACP as a "plan for drug".
Question 10
What is an advance health care directive?
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
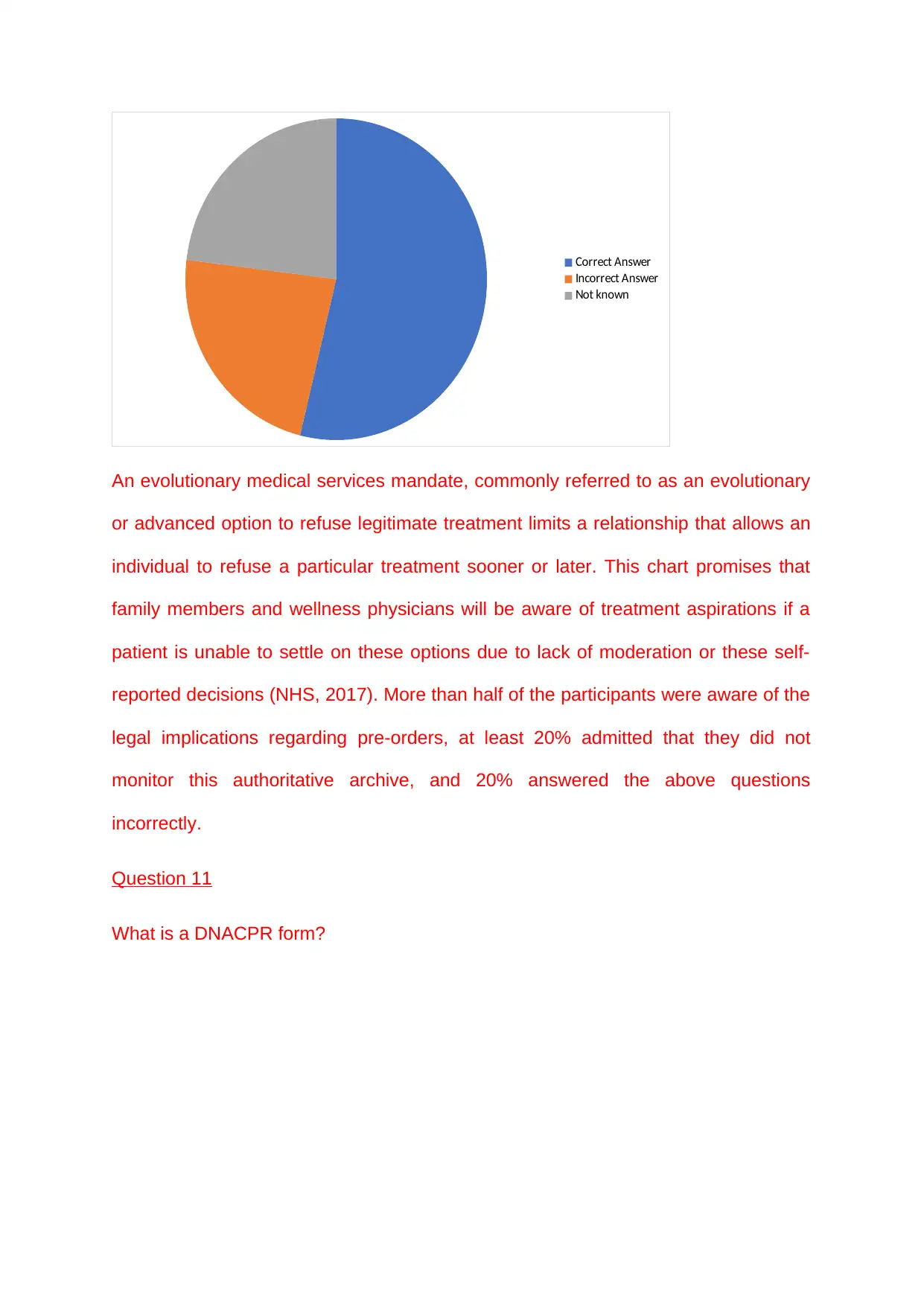
Correct Answer
Incorrect Answer
Not known
An evolutionary medical services mandate, commonly referred to as an evolutionary
or advanced option to refuse legitimate treatment limits a relationship that allows an
individual to refuse a particular treatment sooner or later. This chart promises that
family members and wellness physicians will be aware of treatment aspirations if a
patient is unable to settle on these options due to lack of moderation or these self-
reported decisions (NHS, 2017). More than half of the participants were aware of the
legal implications regarding pre-orders, at least 20% admitted that they did not
monitor this authoritative archive, and 20% answered the above questions
incorrectly.
Question 11
What is a DNACPR form?
Incorrect Answer
Not known
An evolutionary medical services mandate, commonly referred to as an evolutionary
or advanced option to refuse legitimate treatment limits a relationship that allows an
individual to refuse a particular treatment sooner or later. This chart promises that
family members and wellness physicians will be aware of treatment aspirations if a
patient is unable to settle on these options due to lack of moderation or these self-
reported decisions (NHS, 2017). More than half of the participants were aware of the
legal implications regarding pre-orders, at least 20% admitted that they did not
monitor this authoritative archive, and 20% answered the above questions
incorrectly.
Question 11
What is a DNACPR form?
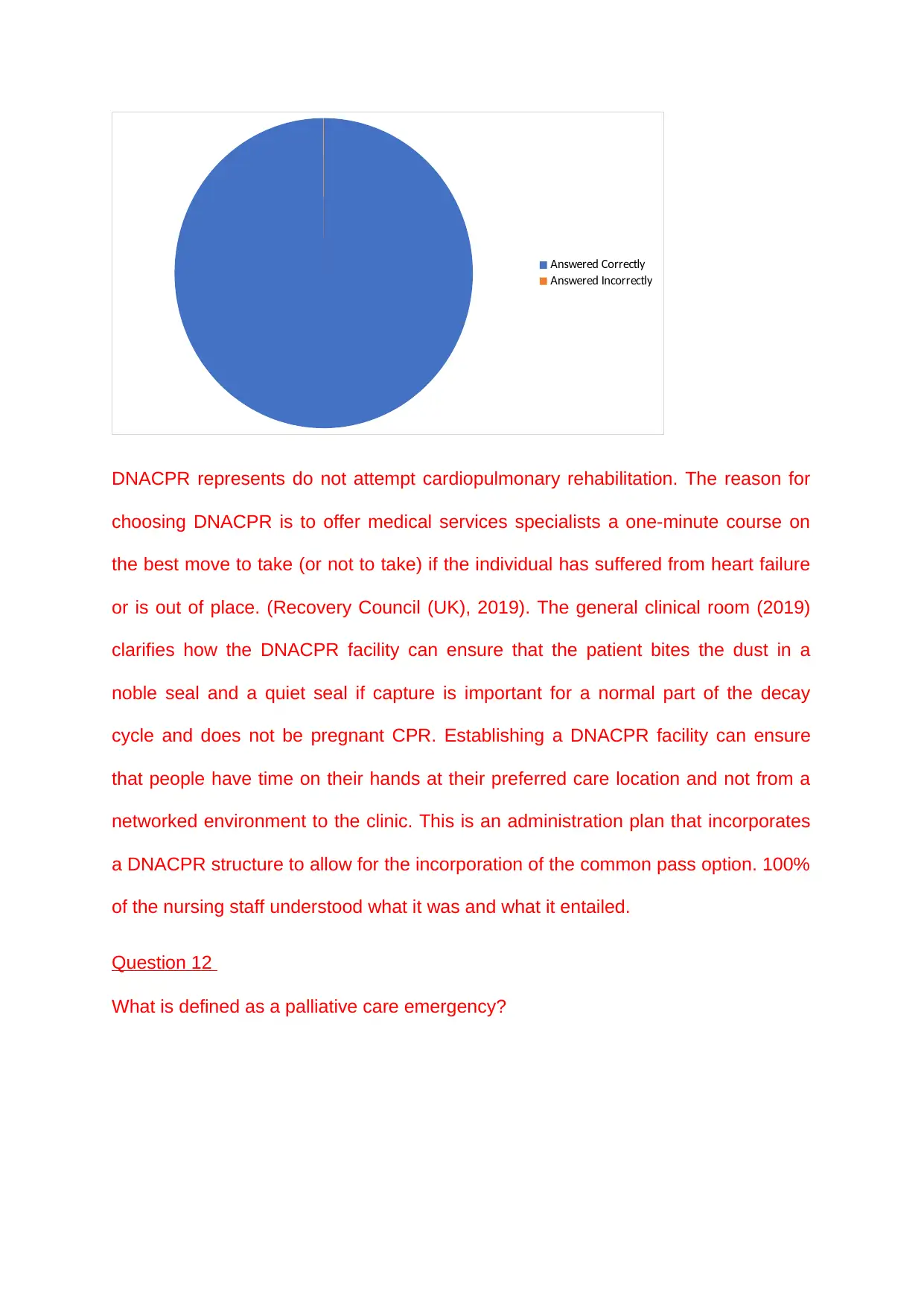
Answered Correctly
Answered Incorrectly
DNACPR represents do not attempt cardiopulmonary rehabilitation. The reason for
choosing DNACPR is to offer medical services specialists a one-minute course on
the best move to take (or not to take) if the individual has suffered from heart failure
or is out of place. (Recovery Council (UK), 2019). The general clinical room (2019)
clarifies how the DNACPR facility can ensure that the patient bites the dust in a
noble seal and a quiet seal if capture is important for a normal part of the decay
cycle and does not be pregnant CPR. Establishing a DNACPR facility can ensure
that people have time on their hands at their preferred care location and not from a
networked environment to the clinic. This is an administration plan that incorporates
a DNACPR structure to allow for the incorporation of the common pass option. 100%
of the nursing staff understood what it was and what it entailed.
Question 12
What is defined as a palliative care emergency?
Answered Incorrectly
DNACPR represents do not attempt cardiopulmonary rehabilitation. The reason for
choosing DNACPR is to offer medical services specialists a one-minute course on
the best move to take (or not to take) if the individual has suffered from heart failure
or is out of place. (Recovery Council (UK), 2019). The general clinical room (2019)
clarifies how the DNACPR facility can ensure that the patient bites the dust in a
noble seal and a quiet seal if capture is important for a normal part of the decay
cycle and does not be pregnant CPR. Establishing a DNACPR facility can ensure
that people have time on their hands at their preferred care location and not from a
networked environment to the clinic. This is an administration plan that incorporates
a DNACPR structure to allow for the incorporation of the common pass option. 100%
of the nursing staff understood what it was and what it entailed.
Question 12
What is defined as a palliative care emergency?

Spinal Cord Compression
Superior vena cava obstruction
hypercalcaemia
neutropenic sepsis
Haemorrhage
Unknown
Inappropriate answer
Palliative care emergencies that require urgent medical treatment include: spinal
pressure, normal vena cava obstruction, hypocalcaemia, neutropenic sepsis, and
secretion. Medical services specialists have a responsibility to be able to differentiate
the signs and manifestations of palliative care arrests and should be prepared for
how they should seek urgent clinical consideration (Marie Curie, 2019) . In the
results, a facilitator was not able to identify all 4 situations and only 38% had the
ability to differentiate at least one. 22% admitted that they have no knowledge or
understanding of these emergencies, which is a major concern.
Question 13
What is GSF?
Superior vena cava obstruction
hypercalcaemia
neutropenic sepsis
Haemorrhage
Unknown
Inappropriate answer
Palliative care emergencies that require urgent medical treatment include: spinal
pressure, normal vena cava obstruction, hypocalcaemia, neutropenic sepsis, and
secretion. Medical services specialists have a responsibility to be able to differentiate
the signs and manifestations of palliative care arrests and should be prepared for
how they should seek urgent clinical consideration (Marie Curie, 2019) . In the
results, a facilitator was not able to identify all 4 situations and only 38% had the
ability to differentiate at least one. 22% admitted that they have no knowledge or
understanding of these emergencies, which is a major concern.
Question 13
What is GSF?
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
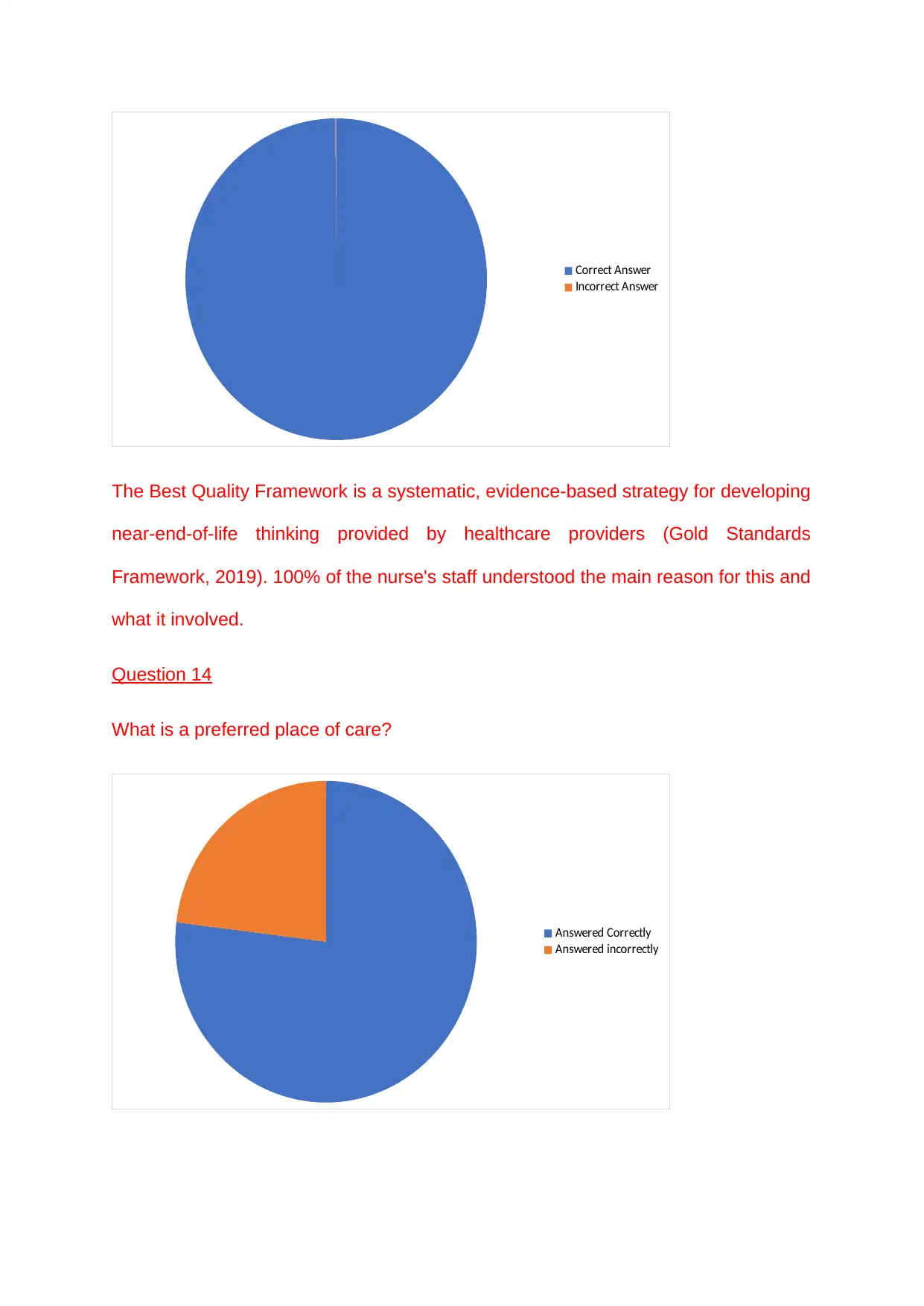
Correct Answer
Incorrect Answer
The Best Quality Framework is a systematic, evidence-based strategy for developing
near-end-of-life thinking provided by healthcare providers (Gold Standards
Framework, 2019). 100% of the nurse's staff understood the main reason for this and
what it involved.
Question 14
What is a preferred place of care?
Answered Correctly
Answered incorrectly
Incorrect Answer
The Best Quality Framework is a systematic, evidence-based strategy for developing
near-end-of-life thinking provided by healthcare providers (Gold Standards
Framework, 2019). 100% of the nurse's staff understood the main reason for this and
what it involved.
Question 14
What is a preferred place of care?
Answered Correctly
Answered incorrectly
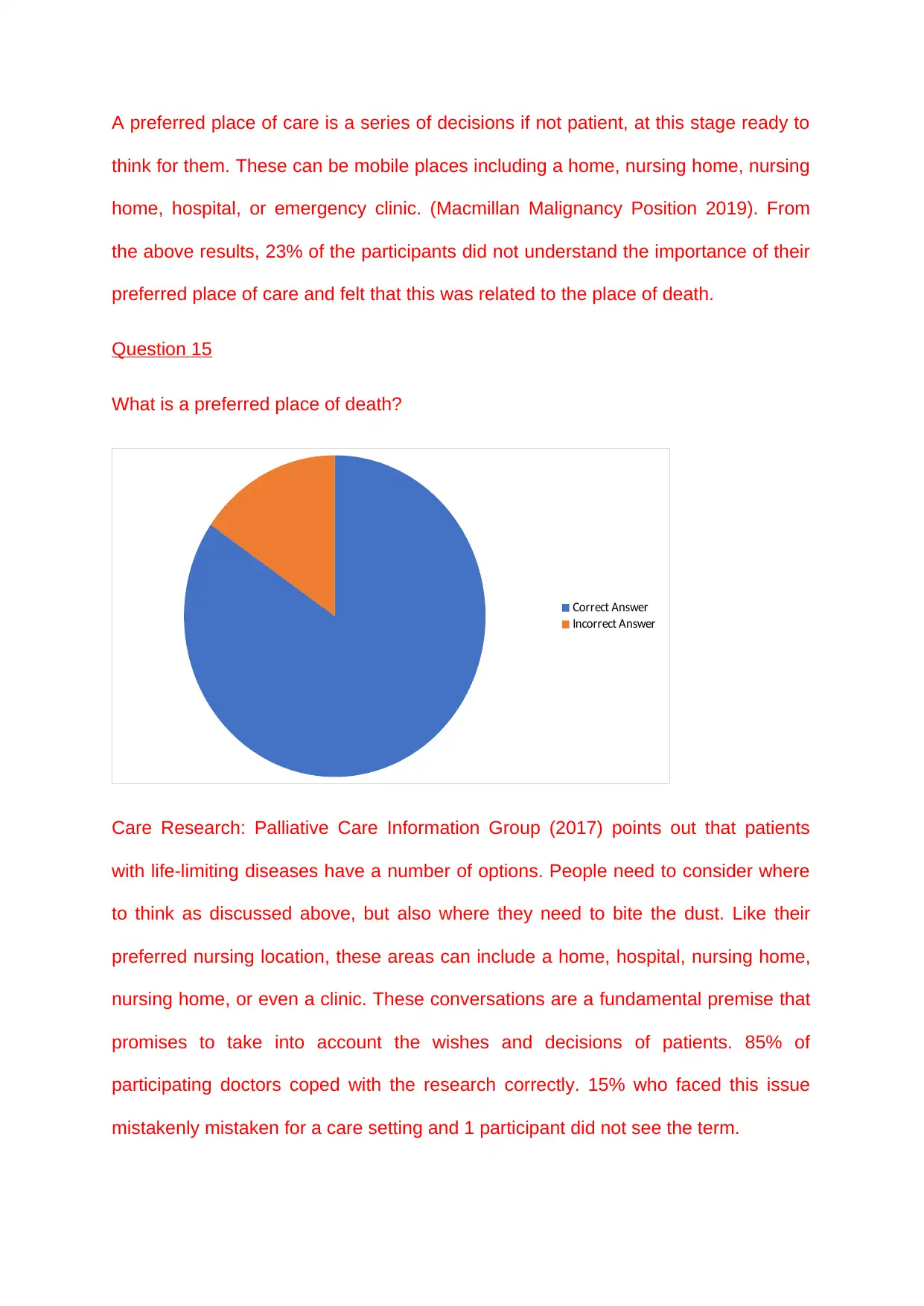
A preferred place of care is a series of decisions if not patient, at this stage ready to
think for them. These can be mobile places including a home, nursing home, nursing
home, hospital, or emergency clinic. (Macmillan Malignancy Position 2019). From
the above results, 23% of the participants did not understand the importance of their
preferred place of care and felt that this was related to the place of death.
Question 15
What is a preferred place of death?
Correct Answer
Incorrect Answer
Care Research: Palliative Care Information Group (2017) points out that patients
with life-limiting diseases have a number of options. People need to consider where
to think as discussed above, but also where they need to bite the dust. Like their
preferred nursing location, these areas can include a home, hospital, nursing home,
nursing home, or even a clinic. These conversations are a fundamental premise that
promises to take into account the wishes and decisions of patients. 85% of
participating doctors coped with the research correctly. 15% who faced this issue
mistakenly mistaken for a care setting and 1 participant did not see the term.
think for them. These can be mobile places including a home, nursing home, nursing
home, hospital, or emergency clinic. (Macmillan Malignancy Position 2019). From
the above results, 23% of the participants did not understand the importance of their
preferred place of care and felt that this was related to the place of death.
Question 15
What is a preferred place of death?
Correct Answer
Incorrect Answer
Care Research: Palliative Care Information Group (2017) points out that patients
with life-limiting diseases have a number of options. People need to consider where
to think as discussed above, but also where they need to bite the dust. Like their
preferred nursing location, these areas can include a home, hospital, nursing home,
nursing home, or even a clinic. These conversations are a fundamental premise that
promises to take into account the wishes and decisions of patients. 85% of
participating doctors coped with the research correctly. 15% who faced this issue
mistakenly mistaken for a care setting and 1 participant did not see the term.
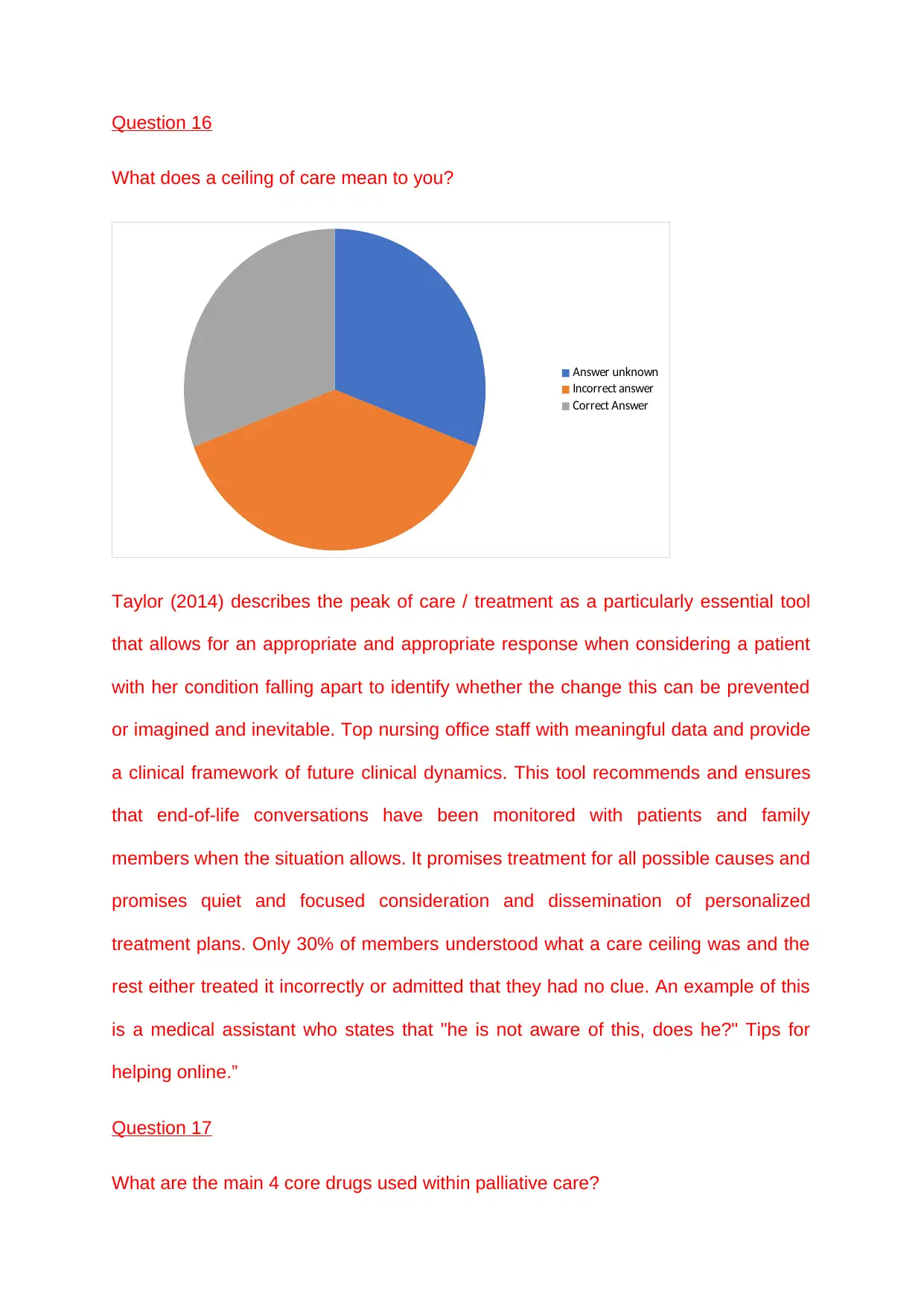
Question 16
What does a ceiling of care mean to you?
Answer unknown
Incorrect answer
Correct Answer
Taylor (2014) describes the peak of care / treatment as a particularly essential tool
that allows for an appropriate and appropriate response when considering a patient
with her condition falling apart to identify whether the change this can be prevented
or imagined and inevitable. Top nursing office staff with meaningful data and provide
a clinical framework of future clinical dynamics. This tool recommends and ensures
that end-of-life conversations have been monitored with patients and family
members when the situation allows. It promises treatment for all possible causes and
promises quiet and focused consideration and dissemination of personalized
treatment plans. Only 30% of members understood what a care ceiling was and the
rest either treated it incorrectly or admitted that they had no clue. An example of this
is a medical assistant who states that "he is not aware of this, does he?" Tips for
helping online.”
Question 17
What are the main 4 core drugs used within palliative care?
What does a ceiling of care mean to you?
Answer unknown
Incorrect answer
Correct Answer
Taylor (2014) describes the peak of care / treatment as a particularly essential tool
that allows for an appropriate and appropriate response when considering a patient
with her condition falling apart to identify whether the change this can be prevented
or imagined and inevitable. Top nursing office staff with meaningful data and provide
a clinical framework of future clinical dynamics. This tool recommends and ensures
that end-of-life conversations have been monitored with patients and family
members when the situation allows. It promises treatment for all possible causes and
promises quiet and focused consideration and dissemination of personalized
treatment plans. Only 30% of members understood what a care ceiling was and the
rest either treated it incorrectly or admitted that they had no clue. An example of this
is a medical assistant who states that "he is not aware of this, does he?" Tips for
helping online.”
Question 17
What are the main 4 core drugs used within palliative care?
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
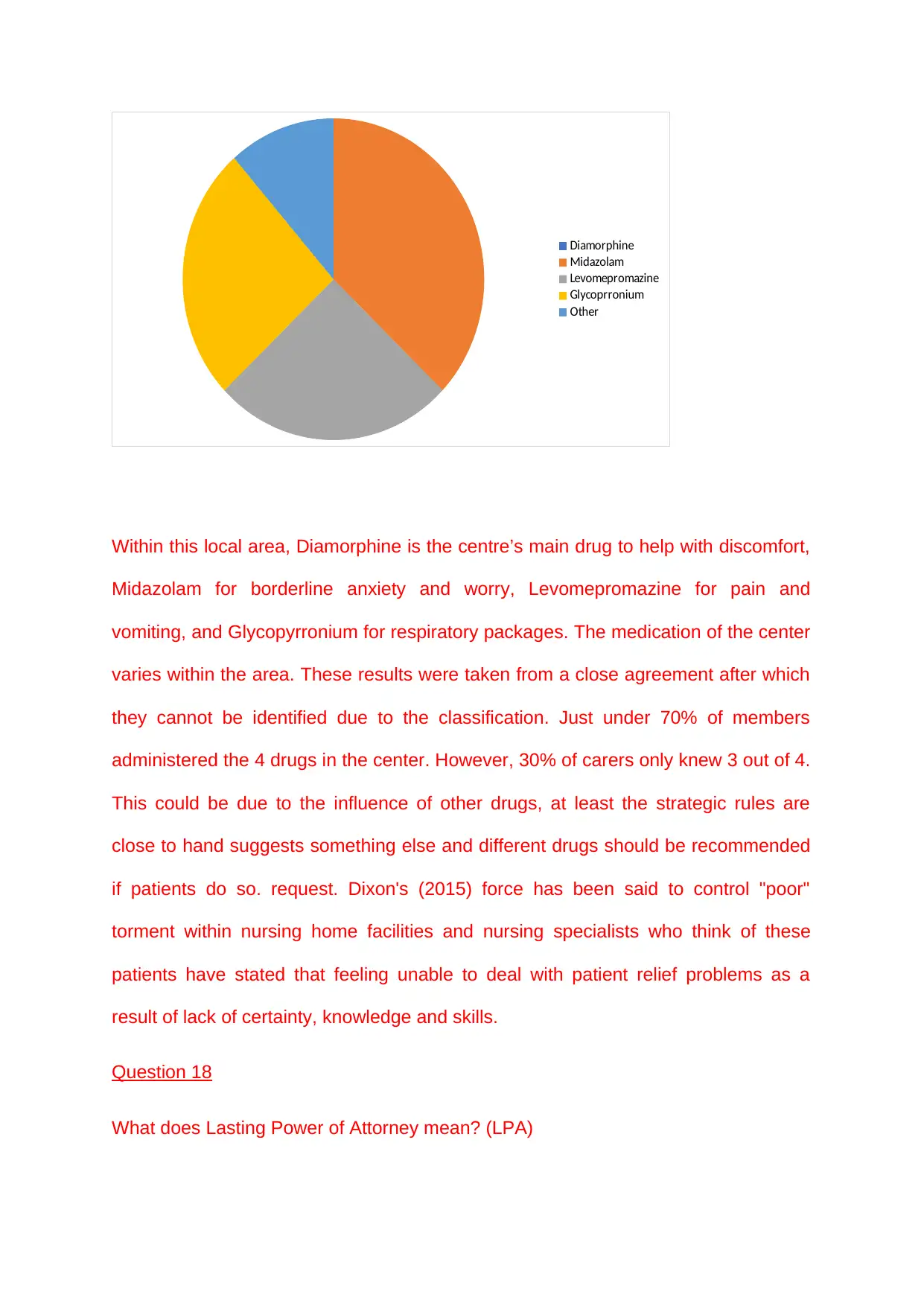
Diamorphine
Midazolam
Levomepromazine
Glycoprronium
Other
Within this local area, Diamorphine is the centre’s main drug to help with discomfort,
Midazolam for borderline anxiety and worry, Levomepromazine for pain and
vomiting, and Glycopyrronium for respiratory packages. The medication of the center
varies within the area. These results were taken from a close agreement after which
they cannot be identified due to the classification. Just under 70% of members
administered the 4 drugs in the center. However, 30% of carers only knew 3 out of 4.
This could be due to the influence of other drugs, at least the strategic rules are
close to hand suggests something else and different drugs should be recommended
if patients do so. request. Dixon's (2015) force has been said to control "poor"
torment within nursing home facilities and nursing specialists who think of these
patients have stated that feeling unable to deal with patient relief problems as a
result of lack of certainty, knowledge and skills.
Question 18
What does Lasting Power of Attorney mean? (LPA)
Midazolam
Levomepromazine
Glycoprronium
Other
Within this local area, Diamorphine is the centre’s main drug to help with discomfort,
Midazolam for borderline anxiety and worry, Levomepromazine for pain and
vomiting, and Glycopyrronium for respiratory packages. The medication of the center
varies within the area. These results were taken from a close agreement after which
they cannot be identified due to the classification. Just under 70% of members
administered the 4 drugs in the center. However, 30% of carers only knew 3 out of 4.
This could be due to the influence of other drugs, at least the strategic rules are
close to hand suggests something else and different drugs should be recommended
if patients do so. request. Dixon's (2015) force has been said to control "poor"
torment within nursing home facilities and nursing specialists who think of these
patients have stated that feeling unable to deal with patient relief problems as a
result of lack of certainty, knowledge and skills.
Question 18
What does Lasting Power of Attorney mean? (LPA)
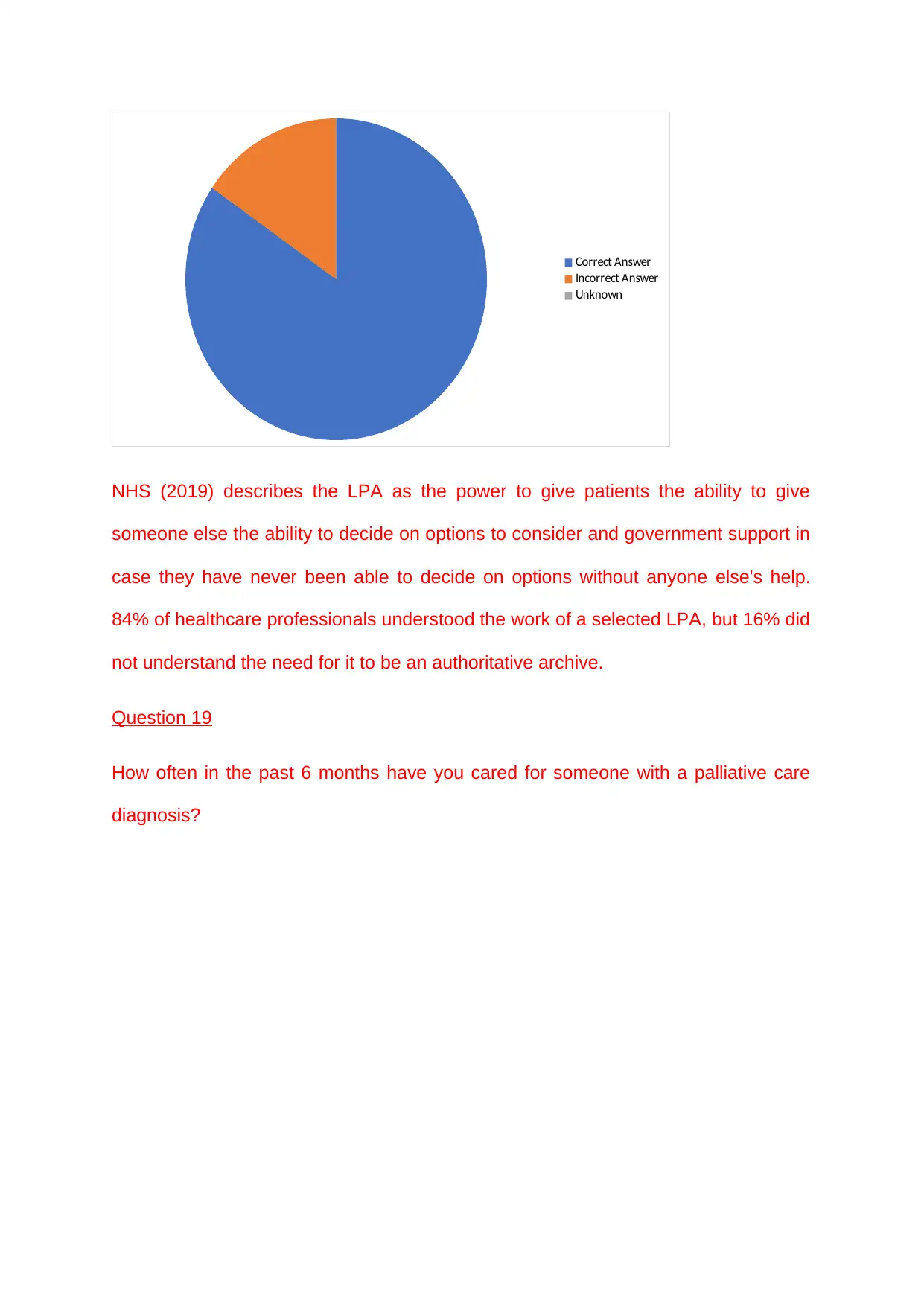
Correct Answer
Incorrect Answer
Unknown
NHS (2019) describes the LPA as the power to give patients the ability to give
someone else the ability to decide on options to consider and government support in
case they have never been able to decide on options without anyone else's help.
84% of healthcare professionals understood the work of a selected LPA, but 16% did
not understand the need for it to be an authoritative archive.
Question 19
How often in the past 6 months have you cared for someone with a palliative care
diagnosis?
Incorrect Answer
Unknown
NHS (2019) describes the LPA as the power to give patients the ability to give
someone else the ability to decide on options to consider and government support in
case they have never been able to decide on options without anyone else's help.
84% of healthcare professionals understood the work of a selected LPA, but 16% did
not understand the need for it to be an authoritative archive.
Question 19
How often in the past 6 months have you cared for someone with a palliative care
diagnosis?
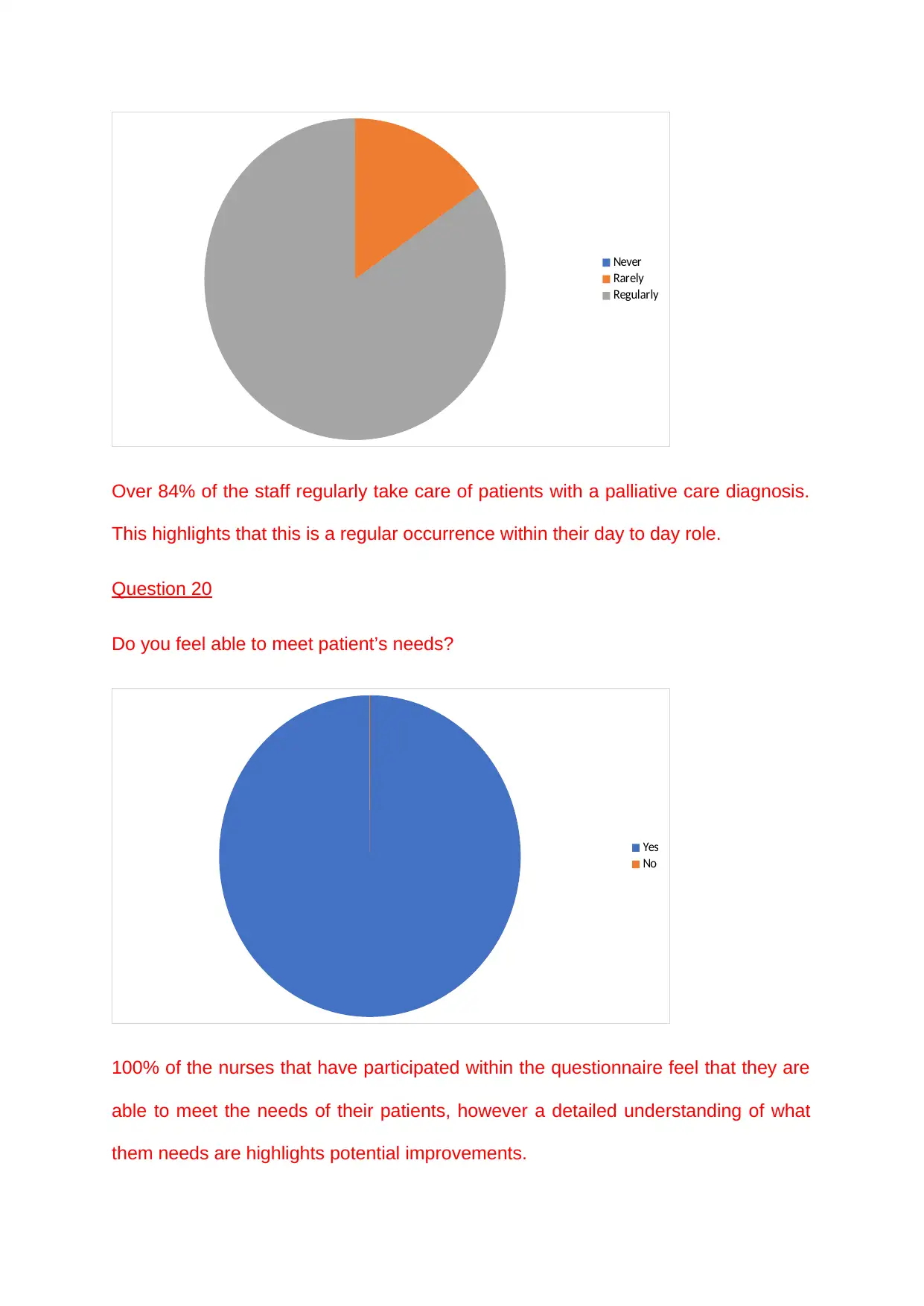
Never
Rarely
Regularly
Over 84% of the staff regularly take care of patients with a palliative care diagnosis.
This highlights that this is a regular occurrence within their day to day role.
Question 20
Do you feel able to meet patient’s needs?
Yes
No
100% of the nurses that have participated within the questionnaire feel that they are
able to meet the needs of their patients, however a detailed understanding of what
them needs are highlights potential improvements.
Rarely
Regularly
Over 84% of the staff regularly take care of patients with a palliative care diagnosis.
This highlights that this is a regular occurrence within their day to day role.
Question 20
Do you feel able to meet patient’s needs?
Yes
No
100% of the nurses that have participated within the questionnaire feel that they are
able to meet the needs of their patients, however a detailed understanding of what
them needs are highlights potential improvements.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
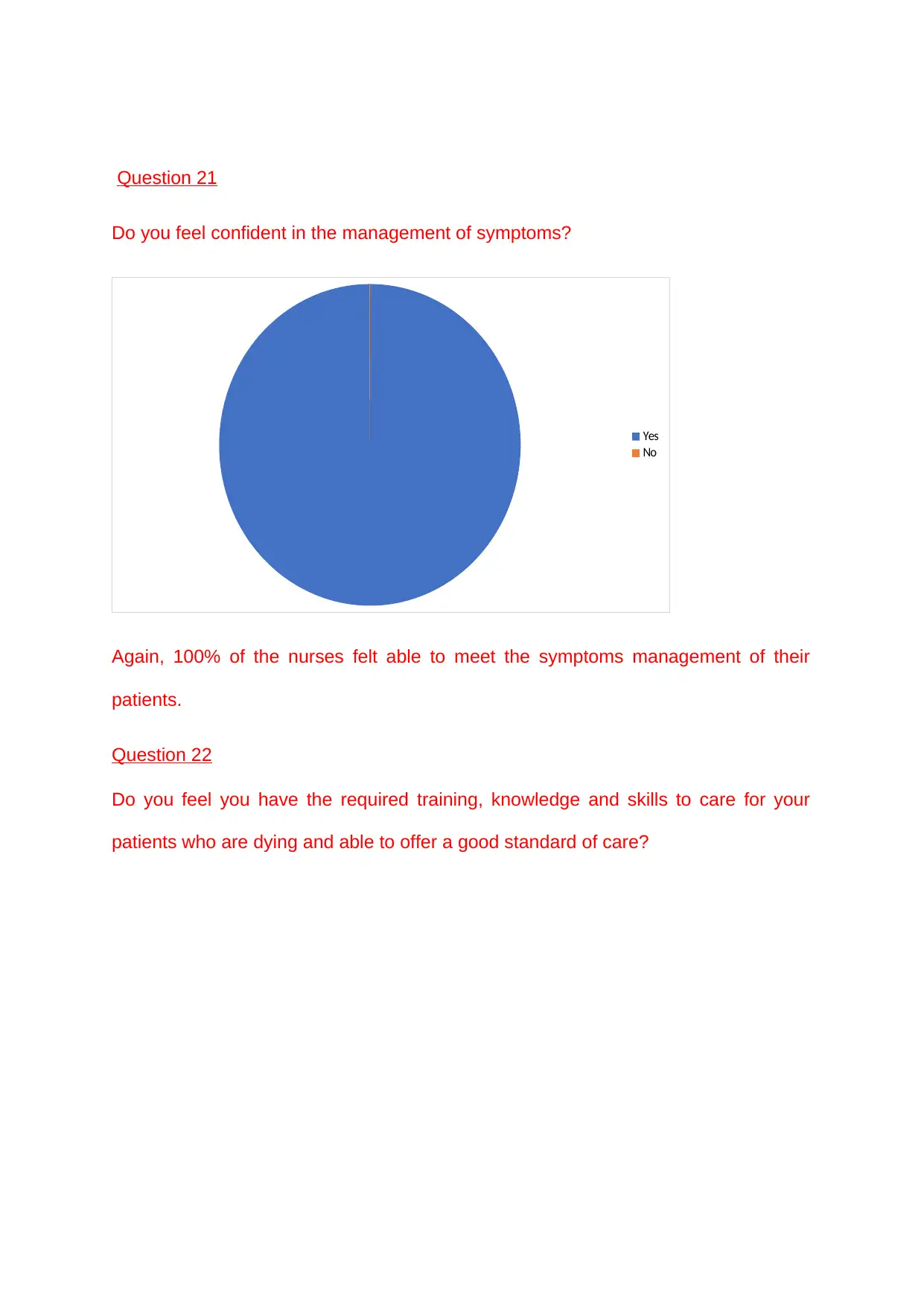
Question 21
Do you feel confident in the management of symptoms?
Yes
No
Again, 100% of the nurses felt able to meet the symptoms management of their
patients.
Question 22
Do you feel you have the required training, knowledge and skills to care for your
patients who are dying and able to offer a good standard of care?
Do you feel confident in the management of symptoms?
Yes
No
Again, 100% of the nurses felt able to meet the symptoms management of their
patients.
Question 22
Do you feel you have the required training, knowledge and skills to care for your
patients who are dying and able to offer a good standard of care?
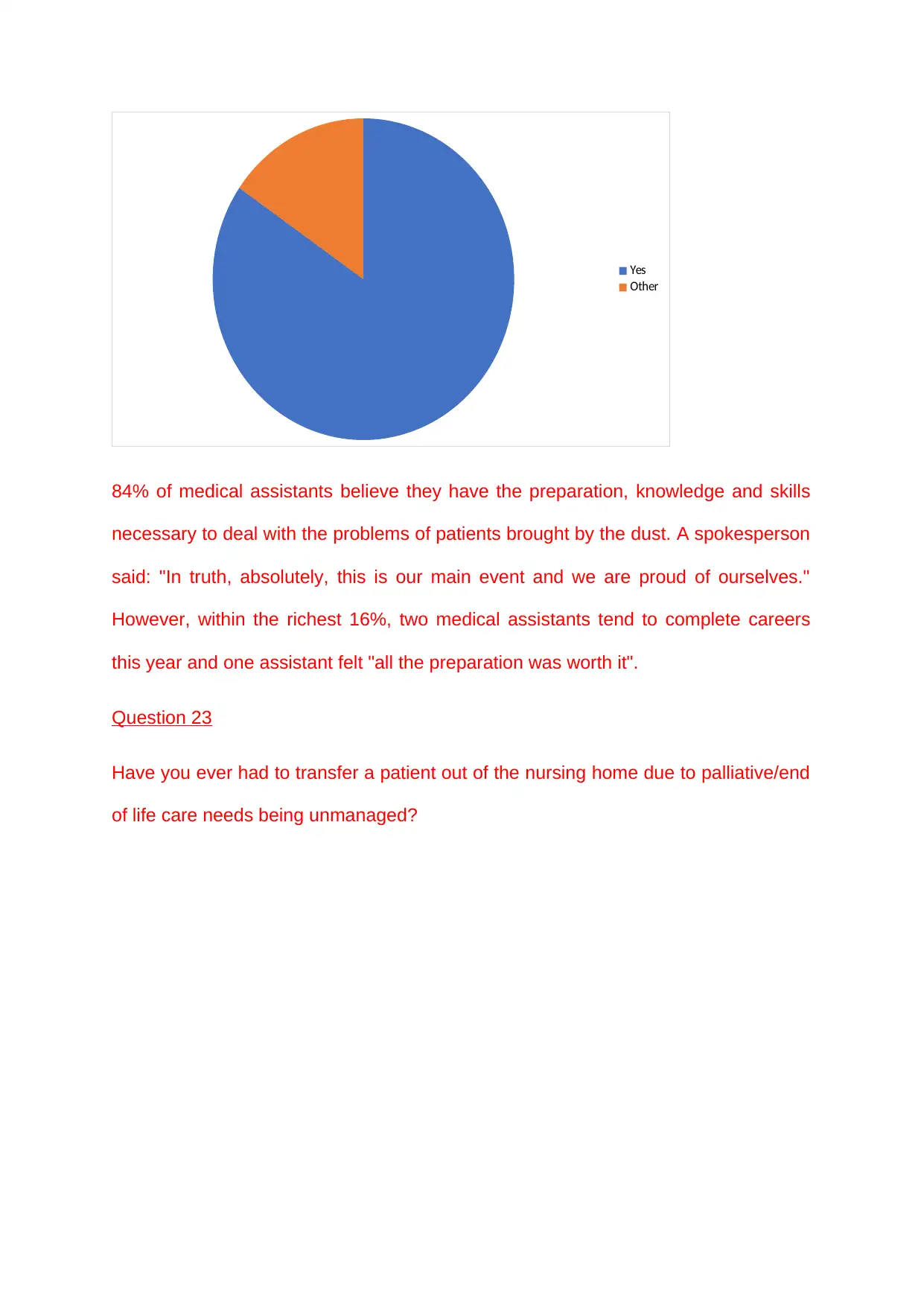
Yes
Other
84% of medical assistants believe they have the preparation, knowledge and skills
necessary to deal with the problems of patients brought by the dust. A spokesperson
said: "In truth, absolutely, this is our main event and we are proud of ourselves."
However, within the richest 16%, two medical assistants tend to complete careers
this year and one assistant felt "all the preparation was worth it".
Question 23
Have you ever had to transfer a patient out of the nursing home due to palliative/end
of life care needs being unmanaged?
Other
84% of medical assistants believe they have the preparation, knowledge and skills
necessary to deal with the problems of patients brought by the dust. A spokesperson
said: "In truth, absolutely, this is our main event and we are proud of ourselves."
However, within the richest 16%, two medical assistants tend to complete careers
this year and one assistant felt "all the preparation was worth it".
Question 23
Have you ever had to transfer a patient out of the nursing home due to palliative/end
of life care needs being unmanaged?
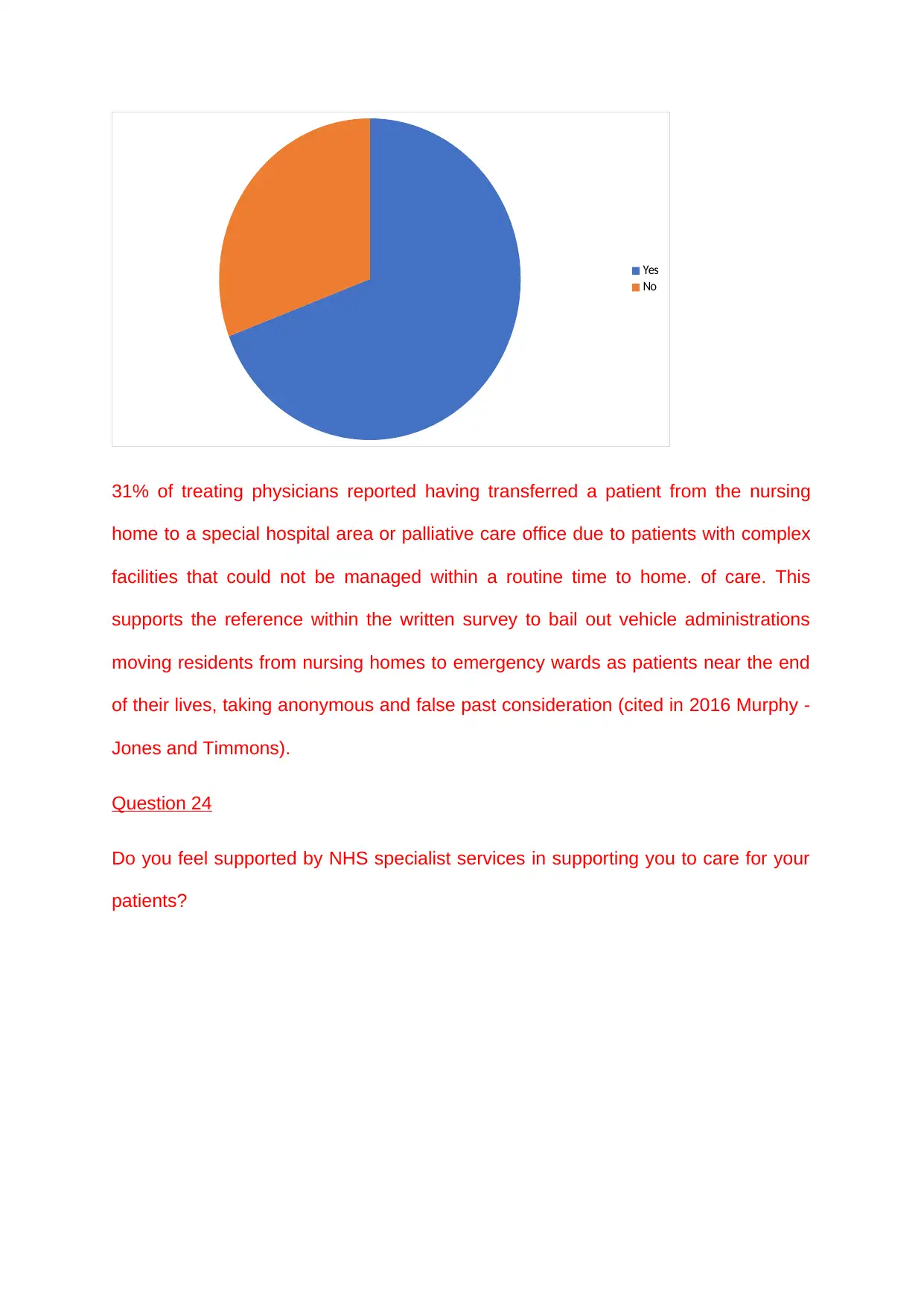
Yes
No
31% of treating physicians reported having transferred a patient from the nursing
home to a special hospital area or palliative care office due to patients with complex
facilities that could not be managed within a routine time to home. of care. This
supports the reference within the written survey to bail out vehicle administrations
moving residents from nursing homes to emergency wards as patients near the end
of their lives, taking anonymous and false past consideration (cited in 2016 Murphy -
Jones and Timmons).
Question 24
Do you feel supported by NHS specialist services in supporting you to care for your
patients?
No
31% of treating physicians reported having transferred a patient from the nursing
home to a special hospital area or palliative care office due to patients with complex
facilities that could not be managed within a routine time to home. of care. This
supports the reference within the written survey to bail out vehicle administrations
moving residents from nursing homes to emergency wards as patients near the end
of their lives, taking anonymous and false past consideration (cited in 2016 Murphy -
Jones and Timmons).
Question 24
Do you feel supported by NHS specialist services in supporting you to care for your
patients?
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
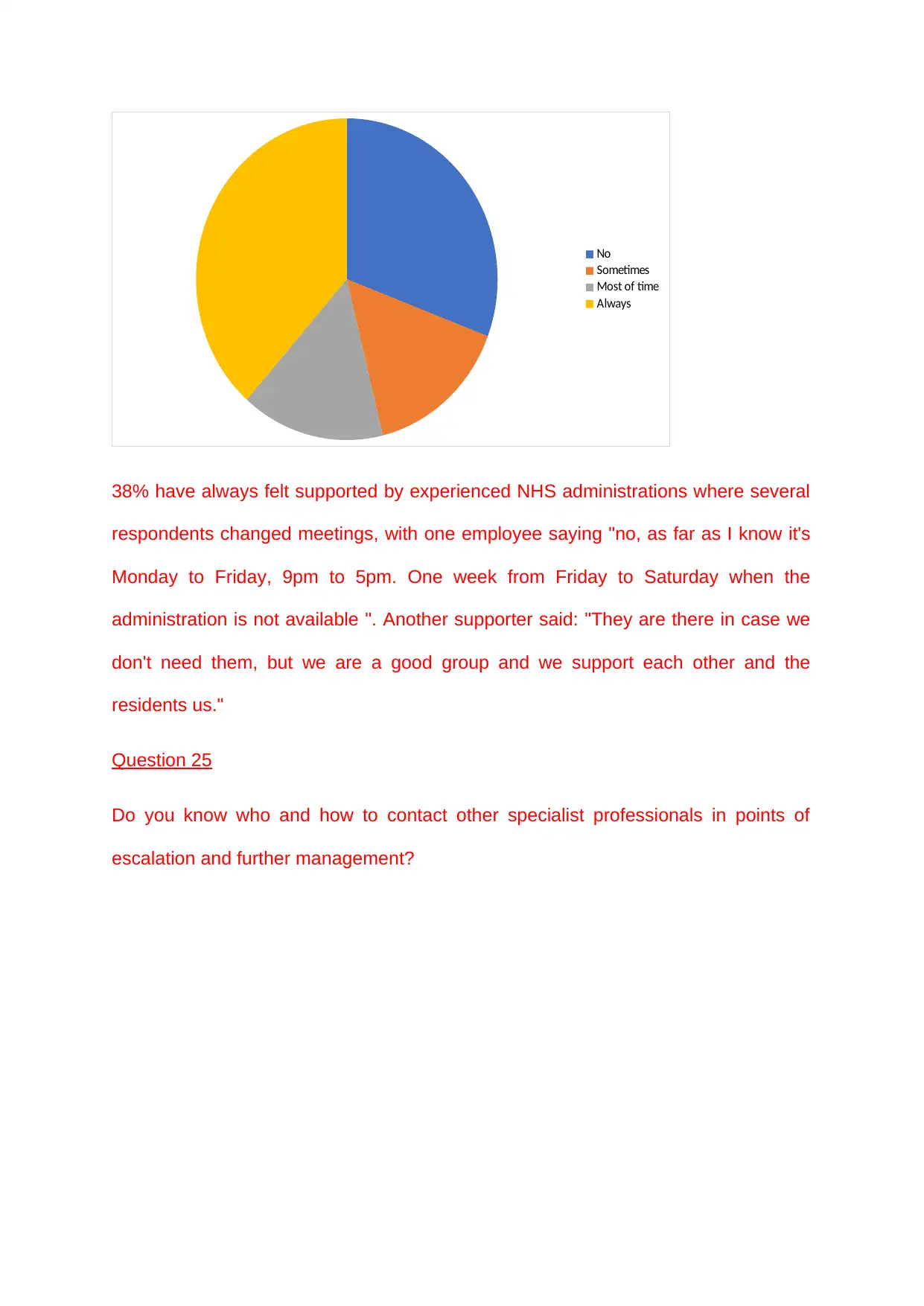
No
Sometimes
Most of time
Always
38% have always felt supported by experienced NHS administrations where several
respondents changed meetings, with one employee saying "no, as far as I know it's
Monday to Friday, 9pm to 5pm. One week from Friday to Saturday when the
administration is not available ". Another supporter said: "They are there in case we
don't need them, but we are a good group and we support each other and the
residents us."
Question 25
Do you know who and how to contact other specialist professionals in points of
escalation and further management?
Sometimes
Most of time
Always
38% have always felt supported by experienced NHS administrations where several
respondents changed meetings, with one employee saying "no, as far as I know it's
Monday to Friday, 9pm to 5pm. One week from Friday to Saturday when the
administration is not available ". Another supporter said: "They are there in case we
don't need them, but we are a good group and we support each other and the
residents us."
Question 25
Do you know who and how to contact other specialist professionals in points of
escalation and further management?
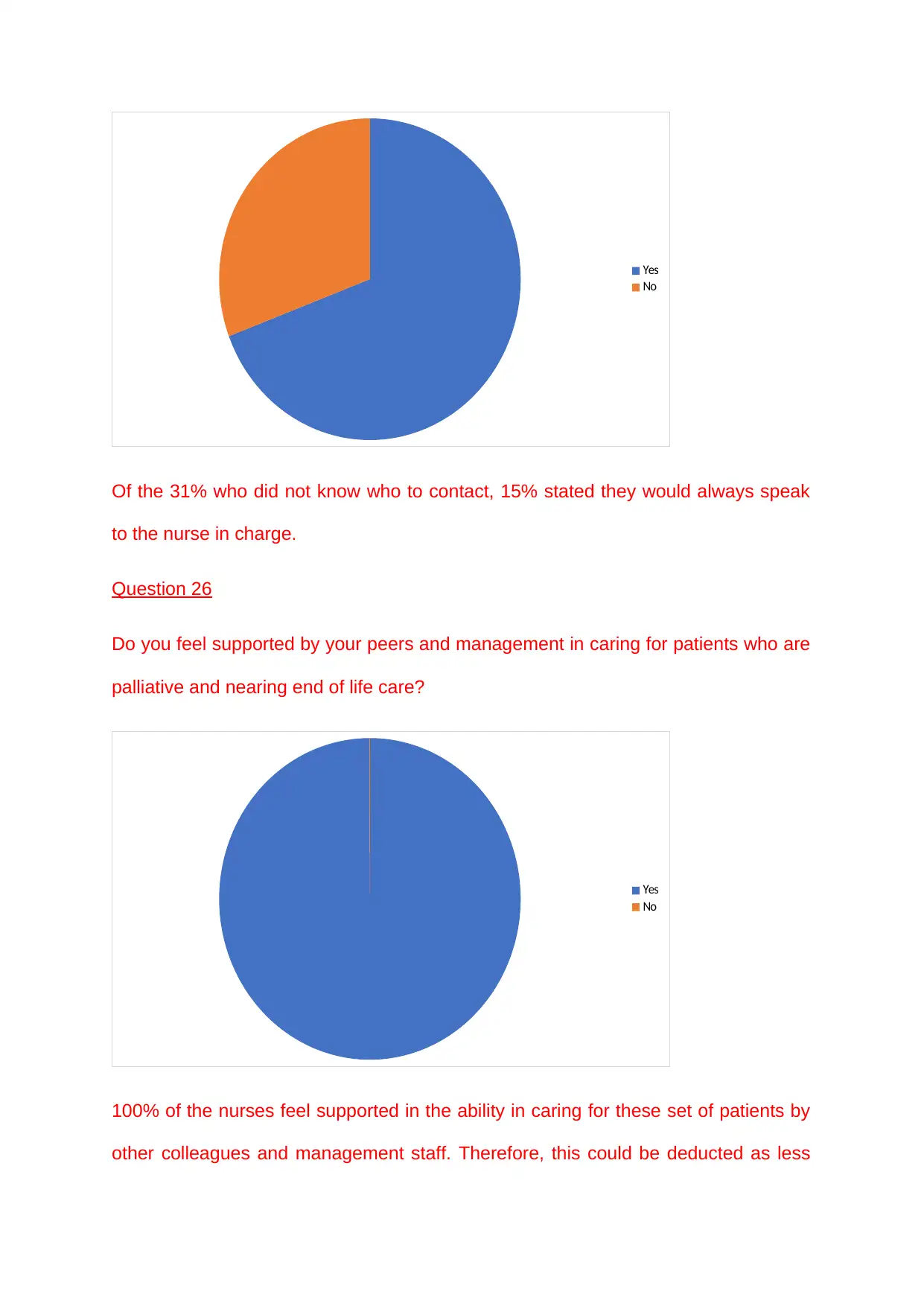
Yes
No
Of the 31% who did not know who to contact, 15% stated they would always speak
to the nurse in charge.
Question 26
Do you feel supported by your peers and management in caring for patients who are
palliative and nearing end of life care?
Yes
No
100% of the nurses feel supported in the ability in caring for these set of patients by
other colleagues and management staff. Therefore, this could be deducted as less
No
Of the 31% who did not know who to contact, 15% stated they would always speak
to the nurse in charge.
Question 26
Do you feel supported by your peers and management in caring for patients who are
palliative and nearing end of life care?
Yes
No
100% of the nurses feel supported in the ability in caring for these set of patients by
other colleagues and management staff. Therefore, this could be deducted as less
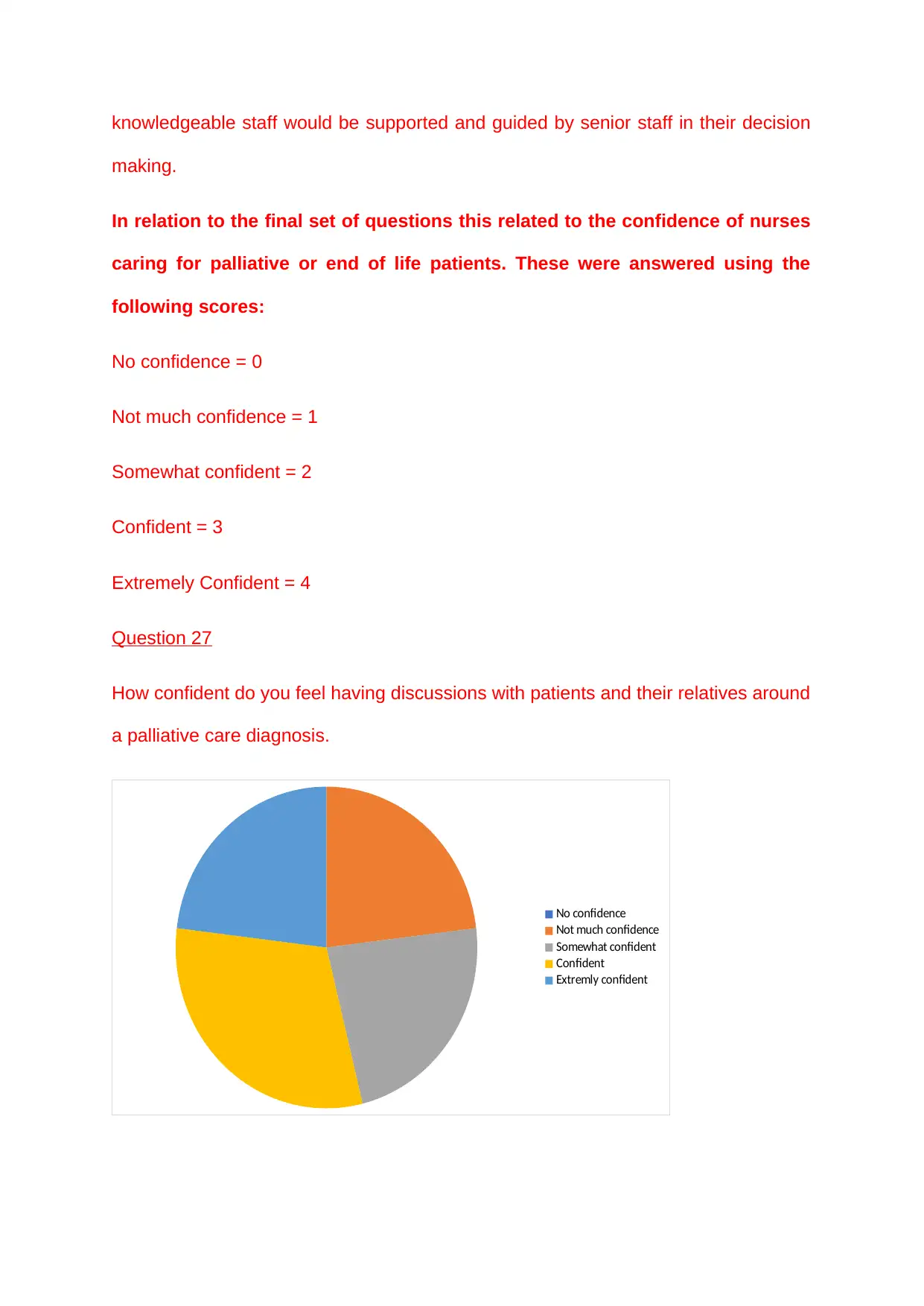
knowledgeable staff would be supported and guided by senior staff in their decision
making.
In relation to the final set of questions this related to the confidence of nurses
caring for palliative or end of life patients. These were answered using the
following scores:
No confidence = 0
Not much confidence = 1
Somewhat confident = 2
Confident = 3
Extremely Confident = 4
Question 27
How confident do you feel having discussions with patients and their relatives around
a palliative care diagnosis.
No confidence
Not much confidence
Somewhat confident
Confident
Extremly confident
making.
In relation to the final set of questions this related to the confidence of nurses
caring for palliative or end of life patients. These were answered using the
following scores:
No confidence = 0
Not much confidence = 1
Somewhat confident = 2
Confident = 3
Extremely Confident = 4
Question 27
How confident do you feel having discussions with patients and their relatives around
a palliative care diagnosis.
No confidence
Not much confidence
Somewhat confident
Confident
Extremly confident
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
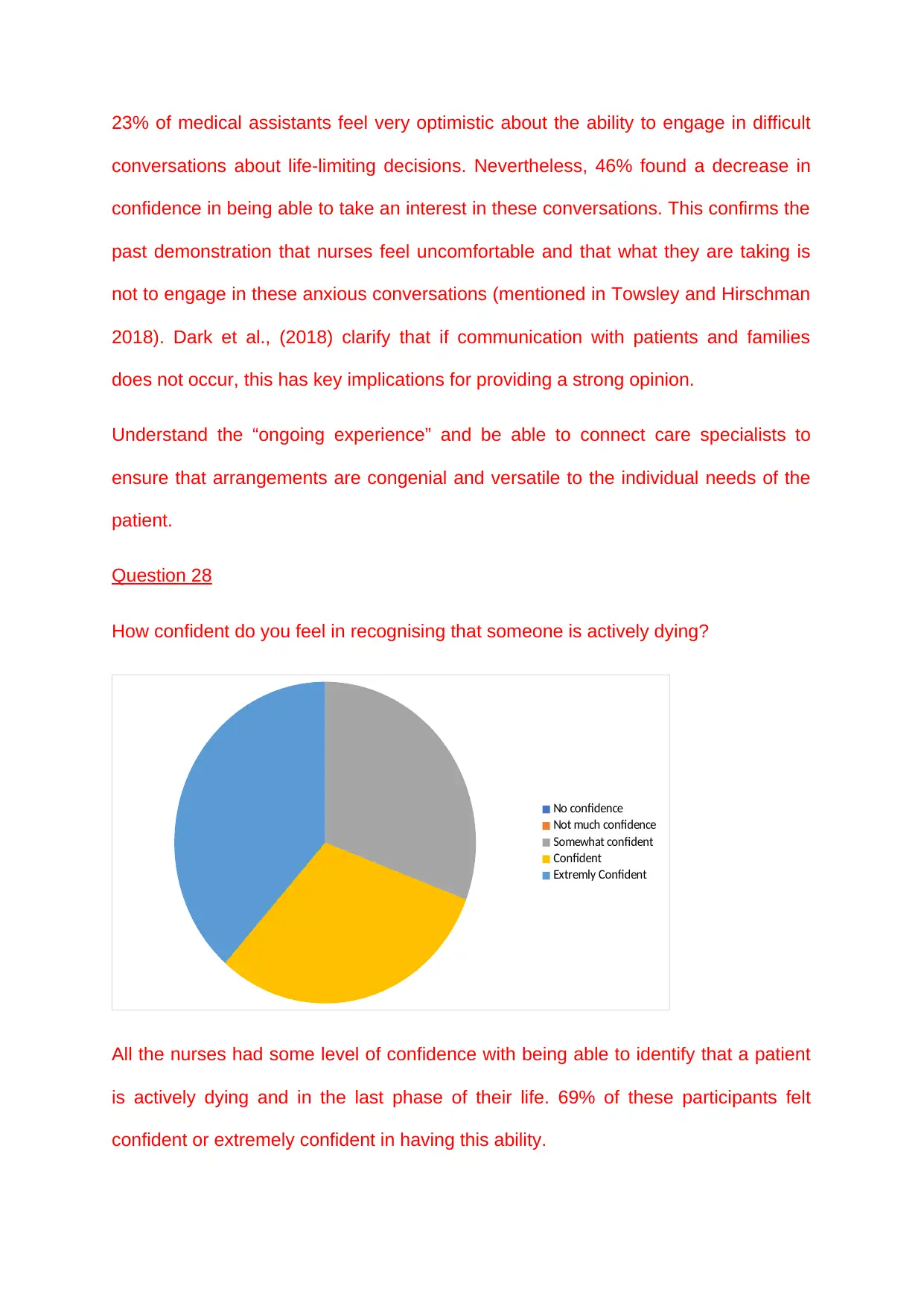
23% of medical assistants feel very optimistic about the ability to engage in difficult
conversations about life-limiting decisions. Nevertheless, 46% found a decrease in
confidence in being able to take an interest in these conversations. This confirms the
past demonstration that nurses feel uncomfortable and that what they are taking is
not to engage in these anxious conversations (mentioned in Towsley and Hirschman
2018). Dark et al., (2018) clarify that if communication with patients and families
does not occur, this has key implications for providing a strong opinion.
Understand the “ongoing experience” and be able to connect care specialists to
ensure that arrangements are congenial and versatile to the individual needs of the
patient.
Question 28
How confident do you feel in recognising that someone is actively dying?
No confidence
Not much confidence
Somewhat confident
Confident
Extremly Confident
All the nurses had some level of confidence with being able to identify that a patient
is actively dying and in the last phase of their life. 69% of these participants felt
confident or extremely confident in having this ability.
conversations about life-limiting decisions. Nevertheless, 46% found a decrease in
confidence in being able to take an interest in these conversations. This confirms the
past demonstration that nurses feel uncomfortable and that what they are taking is
not to engage in these anxious conversations (mentioned in Towsley and Hirschman
2018). Dark et al., (2018) clarify that if communication with patients and families
does not occur, this has key implications for providing a strong opinion.
Understand the “ongoing experience” and be able to connect care specialists to
ensure that arrangements are congenial and versatile to the individual needs of the
patient.
Question 28
How confident do you feel in recognising that someone is actively dying?
No confidence
Not much confidence
Somewhat confident
Confident
Extremly Confident
All the nurses had some level of confidence with being able to identify that a patient
is actively dying and in the last phase of their life. 69% of these participants felt
confident or extremely confident in having this ability.
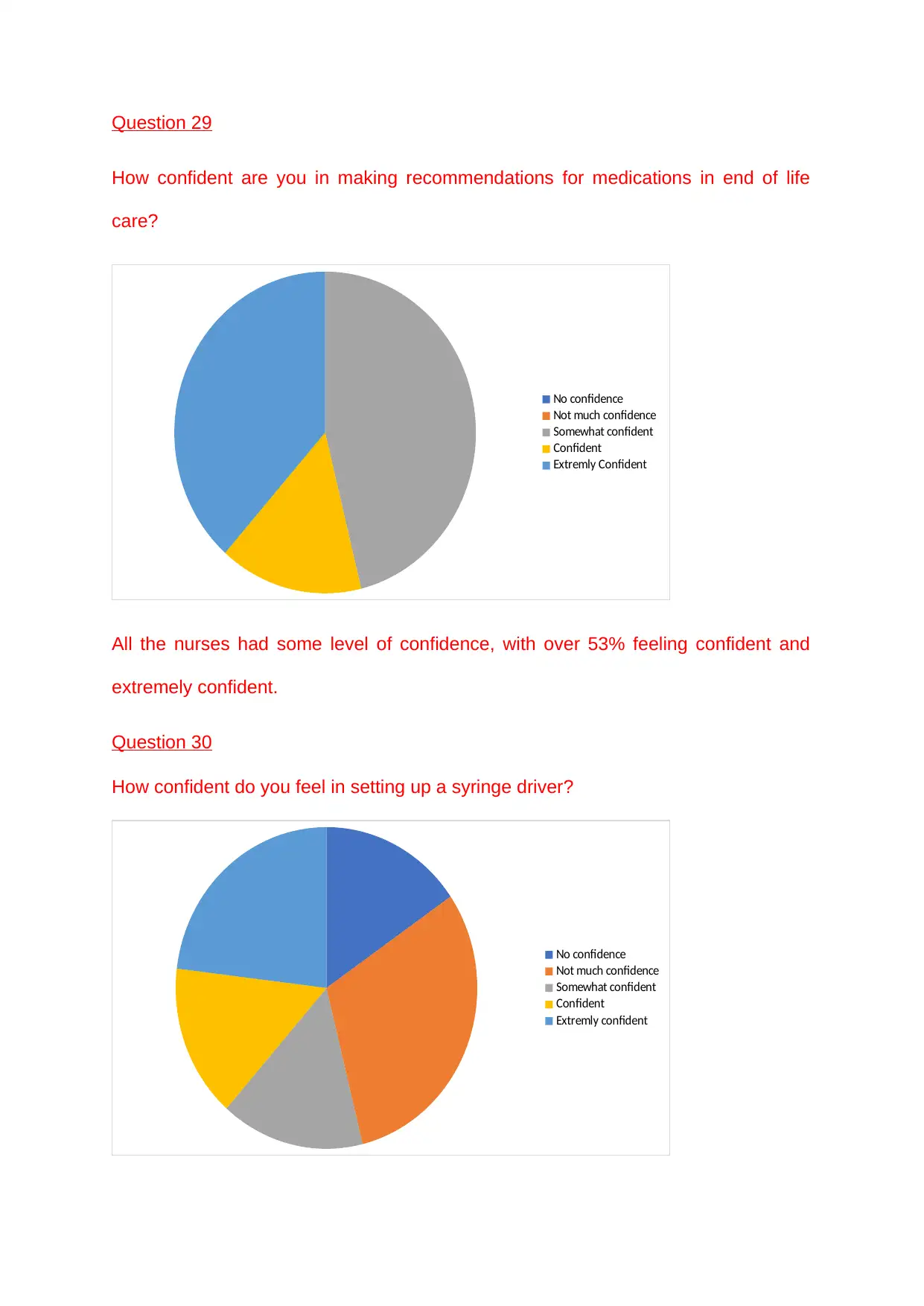
Question 29
How confident are you in making recommendations for medications in end of life
care?
No confidence
Not much confidence
Somewhat confident
Confident
Extremly Confident
All the nurses had some level of confidence, with over 53% feeling confident and
extremely confident.
Question 30
How confident do you feel in setting up a syringe driver?
No confidence
Not much confidence
Somewhat confident
Confident
Extremly confident
How confident are you in making recommendations for medications in end of life
care?
No confidence
Not much confidence
Somewhat confident
Confident
Extremly Confident
All the nurses had some level of confidence, with over 53% feeling confident and
extremely confident.
Question 30
How confident do you feel in setting up a syringe driver?
No confidence
Not much confidence
Somewhat confident
Confident
Extremly confident
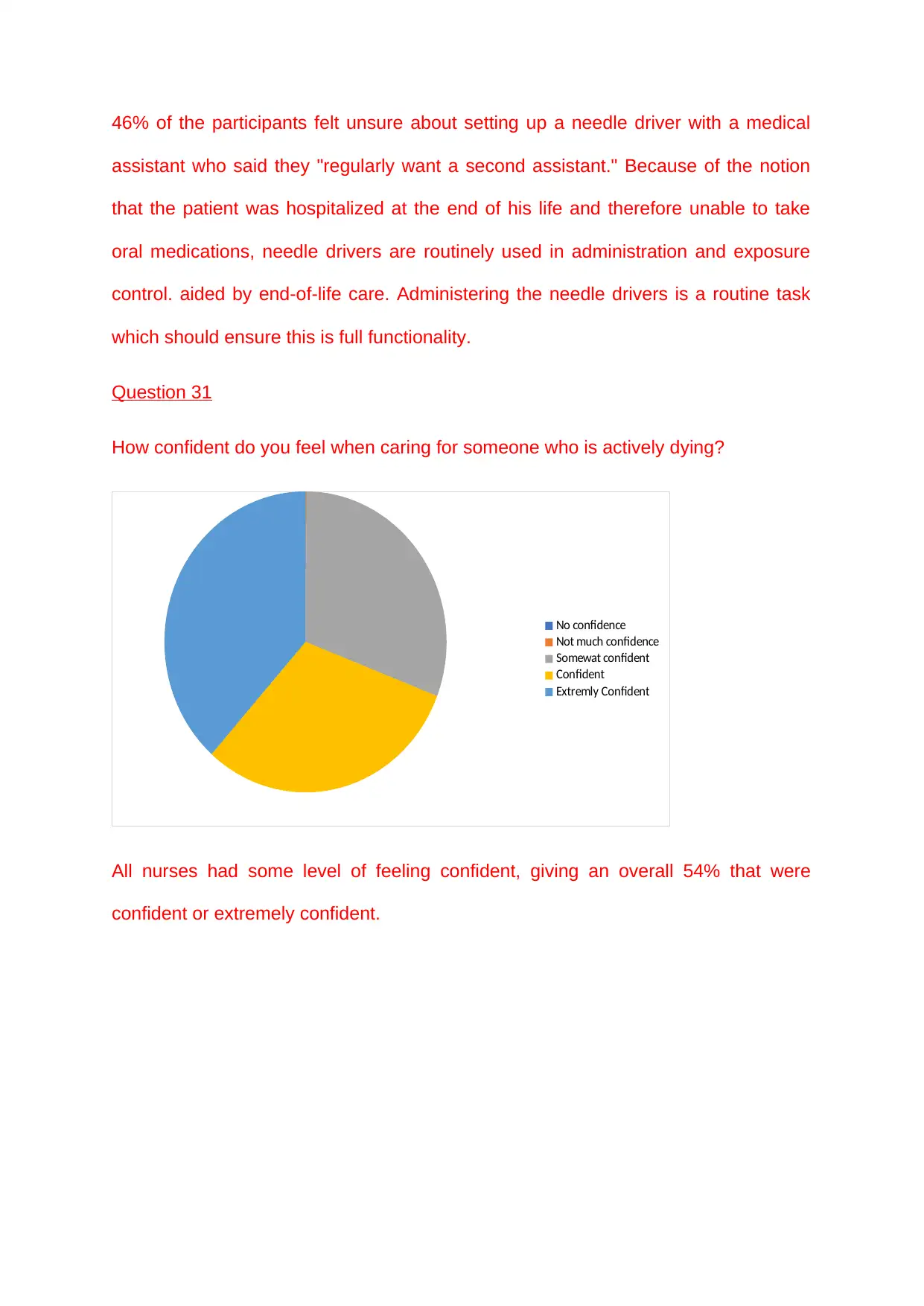
46% of the participants felt unsure about setting up a needle driver with a medical
assistant who said they "regularly want a second assistant." Because of the notion
that the patient was hospitalized at the end of his life and therefore unable to take
oral medications, needle drivers are routinely used in administration and exposure
control. aided by end-of-life care. Administering the needle drivers is a routine task
which should ensure this is full functionality.
Question 31
How confident do you feel when caring for someone who is actively dying?
No confidence
Not much confidence
Somewat confident
Confident
Extremly Confident
All nurses had some level of feeling confident, giving an overall 54% that were
confident or extremely confident.
assistant who said they "regularly want a second assistant." Because of the notion
that the patient was hospitalized at the end of his life and therefore unable to take
oral medications, needle drivers are routinely used in administration and exposure
control. aided by end-of-life care. Administering the needle drivers is a routine task
which should ensure this is full functionality.
Question 31
How confident do you feel when caring for someone who is actively dying?
No confidence
Not much confidence
Somewat confident
Confident
Extremly Confident
All nurses had some level of feeling confident, giving an overall 54% that were
confident or extremely confident.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Chapter Five
Summary and discussions of findings:
Using a thematic approach to collate the responses from the questionnaire facilitated
the analysis. In the area, 4 nursing homes were identified, all run by medical
assistants. 42 polls were broadcast. As recently stated, only 2 votes were returned in
a nursing home as a result of communications within a bombing. This resulted in the
last of 27 completed surveys returned.
Within the nursing homes there were many skilled carers who had been listed for a
long time and had worked in similar nursing homes for much of that time. Despite the
fact that these care meetings were very much about palliative care and end-of-life
thinking, the depth of their knowledge did not coordinate skills acquisition within this
department. 30% did not have the slightest idea about the importance of mitigation
consideration and despite the findings showing that carers felt able to monitor issues
-fold, this was not confirmed by the evidence because patients were always
transferred to more experienced administrations.
One the patterns discovered was one nursing home was clearly more proficient and
gifted than the other nursing homes distinguished. This perceived nursing home had
a lead medical caretaker of expert palliative consideration foundation who was inside
an administration job and lead for the best quality levels structure (GSF). These
medical caretakers felt they were more upheld and had open doors for in house
preparing which grew more abilities and information.
From the information gathered it was featured that the attendants working inside the
homes didn't feel upheld by NHS expert administrations inside palliative
consideration and didn't have a clue how or who to contact for expert exhortation and
Summary and discussions of findings:
Using a thematic approach to collate the responses from the questionnaire facilitated
the analysis. In the area, 4 nursing homes were identified, all run by medical
assistants. 42 polls were broadcast. As recently stated, only 2 votes were returned in
a nursing home as a result of communications within a bombing. This resulted in the
last of 27 completed surveys returned.
Within the nursing homes there were many skilled carers who had been listed for a
long time and had worked in similar nursing homes for much of that time. Despite the
fact that these care meetings were very much about palliative care and end-of-life
thinking, the depth of their knowledge did not coordinate skills acquisition within this
department. 30% did not have the slightest idea about the importance of mitigation
consideration and despite the findings showing that carers felt able to monitor issues
-fold, this was not confirmed by the evidence because patients were always
transferred to more experienced administrations.
One the patterns discovered was one nursing home was clearly more proficient and
gifted than the other nursing homes distinguished. This perceived nursing home had
a lead medical caretaker of expert palliative consideration foundation who was inside
an administration job and lead for the best quality levels structure (GSF). These
medical caretakers felt they were more upheld and had open doors for in house
preparing which grew more abilities and information.
From the information gathered it was featured that the attendants working inside the
homes didn't feel upheld by NHS expert administrations inside palliative
consideration and didn't have a clue how or who to contact for expert exhortation and
acceleration of care. Nonetheless, by remarks archived inside the returned surveys,
the attendants appeared to be hesitant in tolerating outside help.
The members felt positive about suggesting meds for complex frameworks yet didn't
know about 4 centre medications suggested by their nearby rules inside finish of life
care.
All the medical attendants comprehended what GSF and DNACPR were however
didn't comprehend the contrast between favored spot of care and favored spot of
death.
The huge concern featured was that not all the medical caretakers understood what
the palliative consideration crises were. This region of concern would be taken care
of back to the nursing home chief for regions of basic preparing that would should be
actualized.
Inside the outcomes all the medical attendants expressed that they felt upheld by
their companions and directors. This might bring up an issue of legitimacy in that do
the medical caretakers feel ready to be straightforward with their answers around
this subject.
the attendants appeared to be hesitant in tolerating outside help.
The members felt positive about suggesting meds for complex frameworks yet didn't
know about 4 centre medications suggested by their nearby rules inside finish of life
care.
All the medical attendants comprehended what GSF and DNACPR were however
didn't comprehend the contrast between favored spot of care and favored spot of
death.
The huge concern featured was that not all the medical caretakers understood what
the palliative consideration crises were. This region of concern would be taken care
of back to the nursing home chief for regions of basic preparing that would should be
actualized.
Inside the outcomes all the medical attendants expressed that they felt upheld by
their companions and directors. This might bring up an issue of legitimacy in that do
the medical caretakers feel ready to be straightforward with their answers around
this subject.
Chapter Six
Conclusion
From this large study it was determined that there is a need and a visible hole
designed for further event reversal and preparation in nursing home facilities. The
confirmation identified that there is a lack of knowledge and skills in some areas and
how this is affecting the perception of patients receiving palliative and end of life
care. There is an open door for developing links between NHS administrations and
external consideration providers to develop passive consideration. The study seeks
to confirm the expected profitability and challenging potential of a proposed
preparation program, provided by NHS palliative care physicians to qualified medical
participants who are qualified. work in nursing homes. When this study began, it
wanted to determine how confident and qualified participants felt when they thought
about patients serving and accepting end-of-life care. inside nursing homes. From
this an NHS preparedness system would be provided by experienced NHS palliative
care experts who aim to work together to develop silent consideration to any extent
to reduce pressure on NHS administrations, with financial impact. After the study
was conducted, despite the clear changes that could occur, the results were
generally less troubling than in past public scrutiny. was identified within the writing
studio. The results guided within this study by the ethnology and nursing base of
specialists can be influential if the majority of studies are completed.
Be that as it may, what is seen as the relationship and culture between NHS care
providers and any NHS care providers and how joint activity should be supported.
Conclusion
From this large study it was determined that there is a need and a visible hole
designed for further event reversal and preparation in nursing home facilities. The
confirmation identified that there is a lack of knowledge and skills in some areas and
how this is affecting the perception of patients receiving palliative and end of life
care. There is an open door for developing links between NHS administrations and
external consideration providers to develop passive consideration. The study seeks
to confirm the expected profitability and challenging potential of a proposed
preparation program, provided by NHS palliative care physicians to qualified medical
participants who are qualified. work in nursing homes. When this study began, it
wanted to determine how confident and qualified participants felt when they thought
about patients serving and accepting end-of-life care. inside nursing homes. From
this an NHS preparedness system would be provided by experienced NHS palliative
care experts who aim to work together to develop silent consideration to any extent
to reduce pressure on NHS administrations, with financial impact. After the study
was conducted, despite the clear changes that could occur, the results were
generally less troubling than in past public scrutiny. was identified within the writing
studio. The results guided within this study by the ethnology and nursing base of
specialists can be influential if the majority of studies are completed.
Be that as it may, what is seen as the relationship and culture between NHS care
providers and any NHS care providers and how joint activity should be supported.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
This topic is of particular interest to the analyst and to the specialist topic. After the
end of this document and the beginning of September 2019, the scientist will start an
aces course for advanced clinical specialists and within this movement will create
areas around the future development of the authority's work, with focus on society
development without an NHS care provider, for example, nursing homes, social
development and embarrassment reduction.
Owen (2008) state that the quality of care residents receives in care homes should be a
priority for everyone, not just the care home professionals. There are multiple benefits to
widening the health and social care systems and allowing home care staff to have the same
access to training as being offered to NHS professionals. This would have an immediate
effect on patient care and provide confidence and competence within nursing home staff but
also lead to a reduction in hospital admissions and inappropriate referrals to primary care
teams. Owen (2008) recognises that we need to aid care homes and support them to
recognise their own potential and build upon their own expertise that they already have..
Becker (2009) highlights that people die in many different environments but should
all have a right to supportive and palliative care, regardless of diagnosis or
circumstances. With nursing home staff feeling able to be open about their lack in
confidence and competence, this is an opportunity for NHS services to aid care
homes and support them in building upon their own expertise (Owen 2008). By
allowing nursing home staff to have access to the same standard of training that is
offered to NHS clinicians, this enables a higher standard of care to be delivered
within confidence and competence but also having multiple benefits within the NHS
service. One main advantage would be in the reduction in inappropriate hospital
admissions and unsuitable referrals to primary care teams, reducing pressures and
caseloads, ultimately having a positive financial implication. If health professionals
feel incompetently and inadequately equipped to support and care for patients during
end of this document and the beginning of September 2019, the scientist will start an
aces course for advanced clinical specialists and within this movement will create
areas around the future development of the authority's work, with focus on society
development without an NHS care provider, for example, nursing homes, social
development and embarrassment reduction.
Owen (2008) state that the quality of care residents receives in care homes should be a
priority for everyone, not just the care home professionals. There are multiple benefits to
widening the health and social care systems and allowing home care staff to have the same
access to training as being offered to NHS professionals. This would have an immediate
effect on patient care and provide confidence and competence within nursing home staff but
also lead to a reduction in hospital admissions and inappropriate referrals to primary care
teams. Owen (2008) recognises that we need to aid care homes and support them to
recognise their own potential and build upon their own expertise that they already have..
Becker (2009) highlights that people die in many different environments but should
all have a right to supportive and palliative care, regardless of diagnosis or
circumstances. With nursing home staff feeling able to be open about their lack in
confidence and competence, this is an opportunity for NHS services to aid care
homes and support them in building upon their own expertise (Owen 2008). By
allowing nursing home staff to have access to the same standard of training that is
offered to NHS clinicians, this enables a higher standard of care to be delivered
within confidence and competence but also having multiple benefits within the NHS
service. One main advantage would be in the reduction in inappropriate hospital
admissions and unsuitable referrals to primary care teams, reducing pressures and
caseloads, ultimately having a positive financial implication. If health professionals
feel incompetently and inadequately equipped to support and care for patients during
increasingly emotive and susceptible times, this can perpetuate barriers and
anxieties for both patients and clinicians during a time that is already at its most
vulnerable (Andrew, Taylor, 2012).
anxieties for both patients and clinicians during a time that is already at its most
vulnerable (Andrew, Taylor, 2012).
References:
Andrew, J. & Taylor, C. 2012, "Follow-up evaluation of a course to develop effective
communication and relationship skills for palliative care", International journal of
palliative nursing, vol. 18, no. 9, pp. 457-463.
Badger, F., Plumridge, G., Hewison, A., Shaw, K.L., Thomas, K., and Clifford, C.,
2012. An evaluation of the impact of the Gold Standards Framework on collaboration
in end-of-life care in nursing homes: A qualitative and quantitative evaluation.
International journal of nursing studies, 49(5), pp. 586-595.
Becker, R., 2009. Palliative care 1: Principles of palliative care nursing and end-of-
life care. Nursing times, 105(3), pp. 14-16.
Black, A., McGlinchey, T., Gambles, M., Ellershaw, J., and Mayland, C.R., 2018. The
lived experience of palliative care patients in one acute hospital setting: A qualitative
study. BMC Palliative Care, 17(1), pp. 1-4.
Bowers, B. 2018, "Evidence-based practice in community nursing", British journal of
community nursing, vol. 23, no. 7, pp. 336-337.
Bradshaw, W., Smith, K. & Sinclair, P.M. 2016, "Advance care planning innephrology
care", Renal Society of Australasia Journal, vol. 12, no. 1, pp. 26-30.
Brodtkorb, K., Skisland, A.V., Slettebø, Å & Skaar, R. 2017, "Preserving dignity in
end-of-life nursing home care: Some ethical challenges", Nordic Journal of Nursing
Research, vol. 37, no. 2, pp. 78-84.
Chirwatkul, S. 2014, "Editorial: Using Qualitative Research Findings", Pacific Rim
International Journal of Nursing Research, vol. 18, no. 3, pp. 171-172.
Clark, K.R. 2019, "Ethics in Research", Radiologic technology, vol. 90, no. 4, pp.
394-397.
Di Giulio, P., Finetti, S., Giunco, F., Basso, I., Rosa, D., Pettenati, F., Bussotti, A.,
Villani, D., Gentile, S., Boncinelli, L., Monti, M., Spinsanti, S., Piazza, M., Charrier, L.
& Toscani, F. 2019, "The Impact of Nursing Homes Staff Education on End-of-Life
Care in Residents With Advanced Dementia: A Quality Improvement Study", Journal
of Pain & Symptom Management, vol. 57, no. 1, pp. 93-99.
Dixon J, King D., Matosevic, T., Clark, M. and Knapp, M. (2015). Equity in the
Provision of Palliative Care the UK: Review of Evidence. [online] Available at:
https://www.mariecurie.org.uk/globalassets/media/documents/policy/campaigns/
equity-palliative-care-uk-report-full-lse.pdf/ [Accessed 2nd December 2018].
Andrew, J. & Taylor, C. 2012, "Follow-up evaluation of a course to develop effective
communication and relationship skills for palliative care", International journal of
palliative nursing, vol. 18, no. 9, pp. 457-463.
Badger, F., Plumridge, G., Hewison, A., Shaw, K.L., Thomas, K., and Clifford, C.,
2012. An evaluation of the impact of the Gold Standards Framework on collaboration
in end-of-life care in nursing homes: A qualitative and quantitative evaluation.
International journal of nursing studies, 49(5), pp. 586-595.
Becker, R., 2009. Palliative care 1: Principles of palliative care nursing and end-of-
life care. Nursing times, 105(3), pp. 14-16.
Black, A., McGlinchey, T., Gambles, M., Ellershaw, J., and Mayland, C.R., 2018. The
lived experience of palliative care patients in one acute hospital setting: A qualitative
study. BMC Palliative Care, 17(1), pp. 1-4.
Bowers, B. 2018, "Evidence-based practice in community nursing", British journal of
community nursing, vol. 23, no. 7, pp. 336-337.
Bradshaw, W., Smith, K. & Sinclair, P.M. 2016, "Advance care planning innephrology
care", Renal Society of Australasia Journal, vol. 12, no. 1, pp. 26-30.
Brodtkorb, K., Skisland, A.V., Slettebø, Å & Skaar, R. 2017, "Preserving dignity in
end-of-life nursing home care: Some ethical challenges", Nordic Journal of Nursing
Research, vol. 37, no. 2, pp. 78-84.
Chirwatkul, S. 2014, "Editorial: Using Qualitative Research Findings", Pacific Rim
International Journal of Nursing Research, vol. 18, no. 3, pp. 171-172.
Clark, K.R. 2019, "Ethics in Research", Radiologic technology, vol. 90, no. 4, pp.
394-397.
Di Giulio, P., Finetti, S., Giunco, F., Basso, I., Rosa, D., Pettenati, F., Bussotti, A.,
Villani, D., Gentile, S., Boncinelli, L., Monti, M., Spinsanti, S., Piazza, M., Charrier, L.
& Toscani, F. 2019, "The Impact of Nursing Homes Staff Education on End-of-Life
Care in Residents With Advanced Dementia: A Quality Improvement Study", Journal
of Pain & Symptom Management, vol. 57, no. 1, pp. 93-99.
Dixon J, King D., Matosevic, T., Clark, M. and Knapp, M. (2015). Equity in the
Provision of Palliative Care the UK: Review of Evidence. [online] Available at:
https://www.mariecurie.org.uk/globalassets/media/documents/policy/campaigns/
equity-palliative-care-uk-report-full-lse.pdf/ [Accessed 2nd December 2018].
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Gjerberg, E., Lillemoen, L., Førde, R. & Pedersen, R. 2015, "End-of-life care
communications and shared decision-making in Norwegian nursing homes--
experiences and perspectives of patients and relatives", BMC Geriatrics, vol. 15, no.
1, pp. 103.
Gorlén, T.F., Gorlén, T. & Neergaard, M.A. 2013, "Death in nursing homes: a Danish
qualitative study", International journal of palliative nursing, vol. 19, no. 5, pp. 236-
242.
Handley, M., Goodman, C., Froggatt, K., Mathie, E., Gage, H., Manthorpe, J.,
Barclay, S., Crang, C. & Iliffe, S. 2014, "Living and dying: responsibility for end-of-life
care in care homes without on-site nursing provision - a prospective study", Health &
Social Care in the Community, vol. 22, no. 1, pp. 22-29
Hewison, A., Badger, F. & Swani, T. 2011, "Leading end-of-life care: an action
learning set approach in nursing homes", International journal of palliative nursing,
vol. 17, no. 3, pp. 135-141.
Hold, J., Payne, C., Lesandrini, J. & Glover, A.C. 2019, "Successful Advance Care
Planning in a Rural Nursing Home", American Journal of Hospice & Palliative
Medicine, vol. 36, no. 5, pp. 357-361.
Kimberlin, C.L. & Winterstein, A.G. 2008, "Validity and reliability of measurement
instruments used in research", American Journal of Health-System Pharmacy, vol.
65, no. 23, pp. 2276-2284.
Kirkpatrick, S., Harding, S., Pollard, K. & Tacchi, P. 2019, "Preliminary piloting and
validation of a questionnaire identifying basic clinical skills practised by research
nurses", British Journal of Nursing, vol. 28, no. 3, pp. 162-167.
Martin, S. 2015, "Best interest clinical decision making for care home residents with
advanced dementia", British Journal of General Practice, vol. 65, no. 637, pp. 427-
428.
Maxwell, J., (2015). Qualitative Research Design: an Interactive Approach. 3rd ed.
London. Sage Publications.
Murphy-Jones, G. & Timmons, S. 2016, "Paramedics' experiences of end-of-life care
decision making with regard to nursing home residents: an exploration of influential
issues and factors", Emergency Medicine Journal, vol. 33, no. 10, pp. 722-726.
NHS England (2019), NHS long term plan. NHS UK. 06th May 2019.
https://www.england.nhs.uk/2019/01/long-term-plan/
Owen, T. (2008) Healthcare in care homes: a vision for improvement. Journal of
Community Nursing. 22(5): 10–14.
Paton, M., (2015). Qualitative Research and Evaluation. 4th ed. London. Sage
Publications.
communications and shared decision-making in Norwegian nursing homes--
experiences and perspectives of patients and relatives", BMC Geriatrics, vol. 15, no.
1, pp. 103.
Gorlén, T.F., Gorlén, T. & Neergaard, M.A. 2013, "Death in nursing homes: a Danish
qualitative study", International journal of palliative nursing, vol. 19, no. 5, pp. 236-
242.
Handley, M., Goodman, C., Froggatt, K., Mathie, E., Gage, H., Manthorpe, J.,
Barclay, S., Crang, C. & Iliffe, S. 2014, "Living and dying: responsibility for end-of-life
care in care homes without on-site nursing provision - a prospective study", Health &
Social Care in the Community, vol. 22, no. 1, pp. 22-29
Hewison, A., Badger, F. & Swani, T. 2011, "Leading end-of-life care: an action
learning set approach in nursing homes", International journal of palliative nursing,
vol. 17, no. 3, pp. 135-141.
Hold, J., Payne, C., Lesandrini, J. & Glover, A.C. 2019, "Successful Advance Care
Planning in a Rural Nursing Home", American Journal of Hospice & Palliative
Medicine, vol. 36, no. 5, pp. 357-361.
Kimberlin, C.L. & Winterstein, A.G. 2008, "Validity and reliability of measurement
instruments used in research", American Journal of Health-System Pharmacy, vol.
65, no. 23, pp. 2276-2284.
Kirkpatrick, S., Harding, S., Pollard, K. & Tacchi, P. 2019, "Preliminary piloting and
validation of a questionnaire identifying basic clinical skills practised by research
nurses", British Journal of Nursing, vol. 28, no. 3, pp. 162-167.
Martin, S. 2015, "Best interest clinical decision making for care home residents with
advanced dementia", British Journal of General Practice, vol. 65, no. 637, pp. 427-
428.
Maxwell, J., (2015). Qualitative Research Design: an Interactive Approach. 3rd ed.
London. Sage Publications.
Murphy-Jones, G. & Timmons, S. 2016, "Paramedics' experiences of end-of-life care
decision making with regard to nursing home residents: an exploration of influential
issues and factors", Emergency Medicine Journal, vol. 33, no. 10, pp. 722-726.
NHS England (2019), NHS long term plan. NHS UK. 06th May 2019.
https://www.england.nhs.uk/2019/01/long-term-plan/
Owen, T. (2008) Healthcare in care homes: a vision for improvement. Journal of
Community Nursing. 22(5): 10–14.
Paton, M., (2015). Qualitative Research and Evaluation. 4th ed. London. Sage
Publications.
Royal College of Nursing (2015). Getting it right every time: Fundamentals of nursing
care at end of life. [online] Available at: http://rcnendoflife.org.uk/my-role/"
http://rcnendoflife.org.uk/my-role/ [Accessed 1st December 2018)
Swami, M. & Case, A.A. 2018, "Effective Palliative Care: What Is Involved?",
Oncology (08909091), vol. 32, no. 4, pp. 180-184.
Towsley, G.L. & Hirschman, K.B. 2018, "Talking about end-of-life care: Perspectives
of nursing home residents", Geriatric nursing, vol. 39, no. 1, pp. 72-76.
Wallerstedt, B., Benzein, E., Schildmeijer, K. & Sandgren, A. 2019, "What is
palliative care? Perceptions of healthcare professionals", Scandinavian Journal of
Caring Sciences, vol. 33, no. 1, pp. 77-84.
care at end of life. [online] Available at: http://rcnendoflife.org.uk/my-role/"
http://rcnendoflife.org.uk/my-role/ [Accessed 1st December 2018)
Swami, M. & Case, A.A. 2018, "Effective Palliative Care: What Is Involved?",
Oncology (08909091), vol. 32, no. 4, pp. 180-184.
Towsley, G.L. & Hirschman, K.B. 2018, "Talking about end-of-life care: Perspectives
of nursing home residents", Geriatric nursing, vol. 39, no. 1, pp. 72-76.
Wallerstedt, B., Benzein, E., Schildmeijer, K. & Sandgren, A. 2019, "What is
palliative care? Perceptions of healthcare professionals", Scandinavian Journal of
Caring Sciences, vol. 33, no. 1, pp. 77-84.
Appendices:
Appendix A - Consent Form
Date:
Nursing Home Manager:
I am a student at BPP University currently undertaking a Masters in Healthcare
Leadership.
As part of this course I am conducting a piece of primary research to ascertain how
competent and confident registered nurses working in private nursing homes feel
when managing the care of palliative/end of life patients.
I am requesting permission to undertake a questionnaire with your qualified nursing
staff within your nursing home.
All the information will be anonymised and destroyed following the data collection
process and completing the questionnaire is completely voluntary.
If you require any further information, please do not hesitate to contact me
Yours sincerely
Appendix A - Consent Form
Date:
Nursing Home Manager:
I am a student at BPP University currently undertaking a Masters in Healthcare
Leadership.
As part of this course I am conducting a piece of primary research to ascertain how
competent and confident registered nurses working in private nursing homes feel
when managing the care of palliative/end of life patients.
I am requesting permission to undertake a questionnaire with your qualified nursing
staff within your nursing home.
All the information will be anonymised and destroyed following the data collection
process and completing the questionnaire is completely voluntary.
If you require any further information, please do not hesitate to contact me
Yours sincerely
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Appendix B – Questionnaire
Palliative and end of life care questionnaire
Please read and answer the questionnaires around palliative and end of life care as
honest as you can without researching or gaining information prior. This questionnaire
set out to identify any opportunities for development and support. This questionnaire i
confidential, stored within a safe, locked place and will be destroyed following the data
been collected.
Please complete before end of June 2019
Thank you for your time and participation.
A little bit about you:
How long have you been a qualified nurse?
What is your background in nursing?
How long have you been working within this nursing home?
What level of nursing qualification do you hold?
Please read and answer the questionnaires around palliative and end of life care as
honest as you can without researching or gaining information prior. This questionnaire
set out to identify any opportunities for development and support. This questionnaire i
confidential, stored within a safe, locked place and will be destroyed following the data
been collected.
Please complete before end of June 2019
Thank you for your time and participation.
A little bit about you:
How long have you been a qualified nurse?
What is your background in nursing?
How long have you been working within this nursing home?
What level of nursing qualification do you hold?

Appendix C - Ethics Form
1 out of 58
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.
