Respiratory System Practice Questions
VerifiedAdded on 2023/06/13
|5
|1140
|440
AI Summary
This set of practice questions covers various topics related to the respiratory system, including alveoli, pulmonary embolism, empyema, COPD, asthma, hypertension, and cardiac valves. Each question is multiple-choice and has five options to choose from. These questions are suitable for medical students and anyone who wants to test their knowledge on the respiratory system.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Q U E S TI O N 1
1. Which of the following is FALSE regarding alveoli and alveolar ventilation?
a. Surfactant reduces the compliance of the alveoli
b. Minute ventilation refers to the amount of air inhaled and exhaled per minute, while
alveolar ventilation refers to how much inhaled air is actually reaching the alveoli for gas
exchange
c. Residual volume includes a volume of air which cannot be expelled from the alveoli as
well as the air in the airways
d. Inadequate perfusion of well-ventilated alveoli leads to a ventilation-perfusion mismatch
e. Inadequate ventilation of alveoli which are well perfused leads to a ventilation-perfusion
mismatch
Q U E S TI O N 2
1. Which of the following would BEST differentiate pulmonary embolism from
pneumonia?
a. Normal lung function with hypoxemia suggests pulmonary embolism
b. Chest pain would indicate the condition is pneumonia
c. Persistent, productive cough would suggest the condition is pulmonary embolism
d. Dyspnoea indicates the condition is pneumonia
e. Tachycardia suggests the condition is pneumonioa
Q U E S TI O N 3
1. Which of the following would differentiate
an empyema from a transudative plueral effusion ?
a. Purulent pleural fluid suggests empyema has developed
b. Protein in the pleural fluid suggests the effusion is transudative, not empyema
c. Air in the pleural space means empyema has developed
d. Hypoxemia suggests the effusion is empyema, not transudative
e. Reduced FEV1/FVC suggests the effusion is transudative, not empyema
Q U E S TI O N 4
1. Which of the following would be MOST APPROPRIATE for treating moderate
Chronic Obstructive Pulmonary Disease (COPD)?
a. Salbutamol and fluticasone for management, ipratropium as needed for acute
bronchospasm
b. Triotopium with eFormoterol for management and Salbutamol as needed for acute
bronchospasm
c. Fluticasone and ipratropium for management, salmeterol as needed for acute
bronchospasm
d. Fluticasone and salmeterol for management, eFormoterol as needed for acute brochospasm
e. Tiotropium and ciclesonide for management, salmeterol as needed for acute brochospasm
1. Which of the following is FALSE regarding alveoli and alveolar ventilation?
a. Surfactant reduces the compliance of the alveoli
b. Minute ventilation refers to the amount of air inhaled and exhaled per minute, while
alveolar ventilation refers to how much inhaled air is actually reaching the alveoli for gas
exchange
c. Residual volume includes a volume of air which cannot be expelled from the alveoli as
well as the air in the airways
d. Inadequate perfusion of well-ventilated alveoli leads to a ventilation-perfusion mismatch
e. Inadequate ventilation of alveoli which are well perfused leads to a ventilation-perfusion
mismatch
Q U E S TI O N 2
1. Which of the following would BEST differentiate pulmonary embolism from
pneumonia?
a. Normal lung function with hypoxemia suggests pulmonary embolism
b. Chest pain would indicate the condition is pneumonia
c. Persistent, productive cough would suggest the condition is pulmonary embolism
d. Dyspnoea indicates the condition is pneumonia
e. Tachycardia suggests the condition is pneumonioa
Q U E S TI O N 3
1. Which of the following would differentiate
an empyema from a transudative plueral effusion ?
a. Purulent pleural fluid suggests empyema has developed
b. Protein in the pleural fluid suggests the effusion is transudative, not empyema
c. Air in the pleural space means empyema has developed
d. Hypoxemia suggests the effusion is empyema, not transudative
e. Reduced FEV1/FVC suggests the effusion is transudative, not empyema
Q U E S TI O N 4
1. Which of the following would be MOST APPROPRIATE for treating moderate
Chronic Obstructive Pulmonary Disease (COPD)?
a. Salbutamol and fluticasone for management, ipratropium as needed for acute
bronchospasm
b. Triotopium with eFormoterol for management and Salbutamol as needed for acute
bronchospasm
c. Fluticasone and ipratropium for management, salmeterol as needed for acute
bronchospasm
d. Fluticasone and salmeterol for management, eFormoterol as needed for acute brochospasm
e. Tiotropium and ciclesonide for management, salmeterol as needed for acute brochospasm
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Q U E S TI O N 5
1. Which of the following is a decongestant which has alpha agonist actions (i.e. causes
vasoconstriction in mucus glands)?
a. Dihydrocodeine
b. Dornase alfa
c. Guaifenesin
d. Oxymetazoline
e. Dornase alfa
Q U E S TI O N 6
1. Which of the following is MOST likely to be cause immediate bronchodilation in status
asthmaticus?
a. Inhaled Ciclesonide
b
.
Parenteral saline
c. Parenteral
ephedrine
d
.
Inhaled eFormoterol
e. Parenteral salmeterol
Q U E S TI O N 7
1. Which of the following is a short acting beta agonist?
a. Terbutaline
b
.
Eformoterol
c. Fluticasone
d
.
Tiotropium
e. Salmeterol
Q U E S TI O N 8
1. Which of the following anti-inflammatories is classed as a mast cell stabiliser?
a. Fluticasone
b. Sodium Cromoglycate
c. Omalizumab
d. Montelukast
e. Ciclesonide
Q U E S TI O N 9
1. Which of the following most likely explains why Symbicort may be effective in
managing an acute bronchospasm (i.e. acute asthma attack) though Seretide is not?
a. The budesonide in Symbicort is a beta agonist with a rapid onset of action
1. Which of the following is a decongestant which has alpha agonist actions (i.e. causes
vasoconstriction in mucus glands)?
a. Dihydrocodeine
b. Dornase alfa
c. Guaifenesin
d. Oxymetazoline
e. Dornase alfa
Q U E S TI O N 6
1. Which of the following is MOST likely to be cause immediate bronchodilation in status
asthmaticus?
a. Inhaled Ciclesonide
b
.
Parenteral saline
c. Parenteral
ephedrine
d
.
Inhaled eFormoterol
e. Parenteral salmeterol
Q U E S TI O N 7
1. Which of the following is a short acting beta agonist?
a. Terbutaline
b
.
Eformoterol
c. Fluticasone
d
.
Tiotropium
e. Salmeterol
Q U E S TI O N 8
1. Which of the following anti-inflammatories is classed as a mast cell stabiliser?
a. Fluticasone
b. Sodium Cromoglycate
c. Omalizumab
d. Montelukast
e. Ciclesonide
Q U E S TI O N 9
1. Which of the following most likely explains why Symbicort may be effective in
managing an acute bronchospasm (i.e. acute asthma attack) though Seretide is not?
a. The budesonide in Symbicort is a beta agonist with a rapid onset of action
b. The Eformoterol in Symbicort has a rapid onset of action
c. The Eformoterol in Symbicort is a short acting beta agonist
d. Seretide does not contain a beta agonist
e. The fluticasone in Seretide causes bronchoconstriction
Q U E S TI O N 1 0
1. A patient is admitted to hospital with dyspnoea. Lung function tests show her FEV1
(forced expiratory volume in 1 second) <40% predicated for her age and height,
FEV1/FVC = 36%, haemoglobin saturation is 90%. Haemoglobin saturation did
increase with oxygen therapy but lung function did not improve with inhaled
bronchodilators. This patient MOST LIKELY has:
a. Empyema
b. Severe Chronic Obstructive Pulmonary Disease (COPD)
c. Acute respiratory distress syndrome
d. Tension Pneumothorax
e. Chronic bronchitis
Q U E S TI O N 1 1
1. Which of the following typically occurs in allergic asthma but not chronic bronchitis?
a. Bronchospasm
b. IgE mediated sensitisation of mast cells
c. Destruction of alveoli and small airways
d. Obstruction of airways with mucus
e. A chronic persistent cough
Q U E S TI O N 1 2
1. Which of the following is true regarding allergic asthma
a. Mast cells release prostaglandins to cause bronchoconstriction, which is why
leukotriene receptor antagonists are effective in treating allergic asthma
b. Sensitization typically causes bronchspasm when beta adrenergic receptors are stimulated
on airway smooth muscle
c. Where there can be chronic thickening of the airways due to oedema and inflammation
d. Mast cell degranulation will cause brionchodilation
e. Mast cells are sensitized to an allergen by IgM antibodies to the allergen
Q U E S TI O N 1 3
1. Which of the following would be the most appropriate immediate treatment for a
moderate stable pulmonary embolism
a. Prednisone
b. Aspirin
c. Warfarin
c. The Eformoterol in Symbicort is a short acting beta agonist
d. Seretide does not contain a beta agonist
e. The fluticasone in Seretide causes bronchoconstriction
Q U E S TI O N 1 0
1. A patient is admitted to hospital with dyspnoea. Lung function tests show her FEV1
(forced expiratory volume in 1 second) <40% predicated for her age and height,
FEV1/FVC = 36%, haemoglobin saturation is 90%. Haemoglobin saturation did
increase with oxygen therapy but lung function did not improve with inhaled
bronchodilators. This patient MOST LIKELY has:
a. Empyema
b. Severe Chronic Obstructive Pulmonary Disease (COPD)
c. Acute respiratory distress syndrome
d. Tension Pneumothorax
e. Chronic bronchitis
Q U E S TI O N 1 1
1. Which of the following typically occurs in allergic asthma but not chronic bronchitis?
a. Bronchospasm
b. IgE mediated sensitisation of mast cells
c. Destruction of alveoli and small airways
d. Obstruction of airways with mucus
e. A chronic persistent cough
Q U E S TI O N 1 2
1. Which of the following is true regarding allergic asthma
a. Mast cells release prostaglandins to cause bronchoconstriction, which is why
leukotriene receptor antagonists are effective in treating allergic asthma
b. Sensitization typically causes bronchspasm when beta adrenergic receptors are stimulated
on airway smooth muscle
c. Where there can be chronic thickening of the airways due to oedema and inflammation
d. Mast cell degranulation will cause brionchodilation
e. Mast cells are sensitized to an allergen by IgM antibodies to the allergen
Q U E S TI O N 1 3
1. Which of the following would be the most appropriate immediate treatment for a
moderate stable pulmonary embolism
a. Prednisone
b. Aspirin
c. Warfarin
d. Low molecular weight heparin
e. Antiplase
Q U E S TI O N 1 4
Which of the following is the most appropriate treatment for
a severe unstable pulmonary thromboembolism
a. An anti coagulant which inhibits platelet aggregation
b. A non-steroidal anti-inflammatory
c. A thrombolytic agent
d. a corticosteroid
e. An anticoagulant which acts on the clotting cascade proteins
Q U E S TI O N 1 5
A patient is admitted to hospital with severe dyspnea, an FEV1/FVC of 34% and an
FEV1 predicted of 32%, tachycardia, dyspnea, a persistent but unproductive cough
who is currently being treated with tiotropium and salmeterol. When stable they have
FEV1/FVC of 52% and an FEV1 predicted of 39%. According to the COPD-X chart,
they most likely have:
a. severe COPD
b. mild COPD
c. Severe persistent asthma
d. Pneumonia
e. moderate COPD
Q U E S TI O N 1 6
Premature ventricular complexes, non-sinus ventricular tachycardia and ventricular
fibrillation are all caused by ___________ECTOPIC_____ pacemakers.
Q U E S TI O N 1 7
Bacterial colonies on the leaflets of the cardiac valves, encased in fibrin deposits, are called
________NON Bacterial Thrombotic ENDOCARTITIS______ .
e. Antiplase
Q U E S TI O N 1 4
Which of the following is the most appropriate treatment for
a severe unstable pulmonary thromboembolism
a. An anti coagulant which inhibits platelet aggregation
b. A non-steroidal anti-inflammatory
c. A thrombolytic agent
d. a corticosteroid
e. An anticoagulant which acts on the clotting cascade proteins
Q U E S TI O N 1 5
A patient is admitted to hospital with severe dyspnea, an FEV1/FVC of 34% and an
FEV1 predicted of 32%, tachycardia, dyspnea, a persistent but unproductive cough
who is currently being treated with tiotropium and salmeterol. When stable they have
FEV1/FVC of 52% and an FEV1 predicted of 39%. According to the COPD-X chart,
they most likely have:
a. severe COPD
b. mild COPD
c. Severe persistent asthma
d. Pneumonia
e. moderate COPD
Q U E S TI O N 1 6
Premature ventricular complexes, non-sinus ventricular tachycardia and ventricular
fibrillation are all caused by ___________ECTOPIC_____ pacemakers.
Q U E S TI O N 1 7
Bacterial colonies on the leaflets of the cardiac valves, encased in fibrin deposits, are called
________NON Bacterial Thrombotic ENDOCARTITIS______ .
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
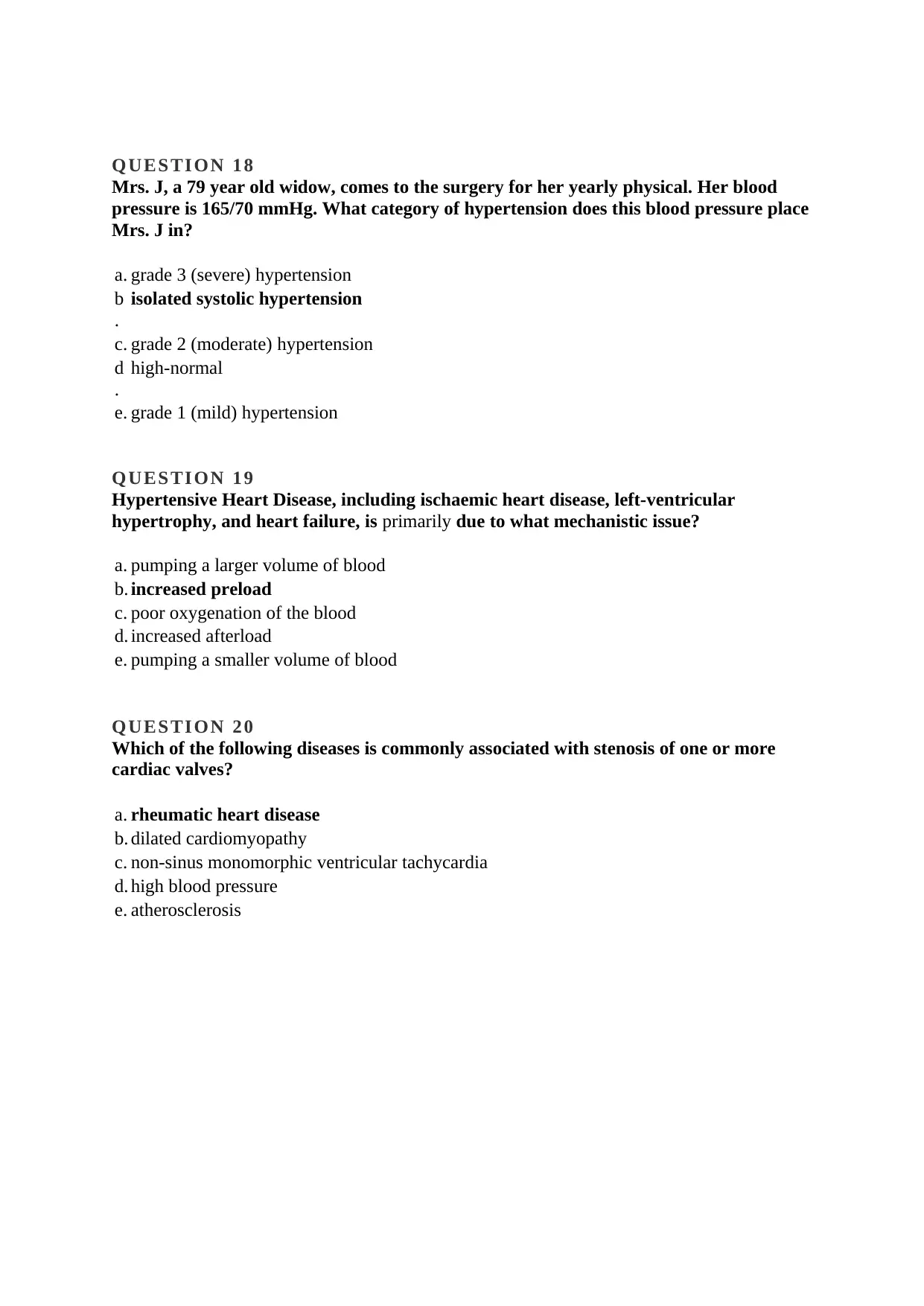
Q U E S TI O N 1 8
Mrs. J, a 79 year old widow, comes to the surgery for her yearly physical. Her blood
pressure is 165/70 mmHg. What category of hypertension does this blood pressure place
Mrs. J in?
a. grade 3 (severe) hypertension
b
.
isolated systolic hypertension
c. grade 2 (moderate) hypertension
d
.
high-normal
e. grade 1 (mild) hypertension
Q U E S TI O N 1 9
Hypertensive Heart Disease, including ischaemic heart disease, left-ventricular
hypertrophy, and heart failure, is primarily due to what mechanistic issue?
a. pumping a larger volume of blood
b. increased preload
c. poor oxygenation of the blood
d. increased afterload
e. pumping a smaller volume of blood
Q U E S TI O N 2 0
Which of the following diseases is commonly associated with stenosis of one or more
cardiac valves?
a. rheumatic heart disease
b. dilated cardiomyopathy
c. non-sinus monomorphic ventricular tachycardia
d. high blood pressure
e. atherosclerosis
Mrs. J, a 79 year old widow, comes to the surgery for her yearly physical. Her blood
pressure is 165/70 mmHg. What category of hypertension does this blood pressure place
Mrs. J in?
a. grade 3 (severe) hypertension
b
.
isolated systolic hypertension
c. grade 2 (moderate) hypertension
d
.
high-normal
e. grade 1 (mild) hypertension
Q U E S TI O N 1 9
Hypertensive Heart Disease, including ischaemic heart disease, left-ventricular
hypertrophy, and heart failure, is primarily due to what mechanistic issue?
a. pumping a larger volume of blood
b. increased preload
c. poor oxygenation of the blood
d. increased afterload
e. pumping a smaller volume of blood
Q U E S TI O N 2 0
Which of the following diseases is commonly associated with stenosis of one or more
cardiac valves?
a. rheumatic heart disease
b. dilated cardiomyopathy
c. non-sinus monomorphic ventricular tachycardia
d. high blood pressure
e. atherosclerosis
1 out of 5
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.