Evaluation of Neuroblastoma Skeletal Metastases: PET vs. MIBG Accuracy
VerifiedAdded on 2023/01/18
|4
|1410
|80
Report
AI Summary
This report reviews the accuracy of Positron Emission Tomography (PET) imaging versus Iodine-123 metaiodobenzylguanidine (MIBG) scintigraphy in the evaluation of skeletal metastases of neuroblastoma (NBL) in younger children. Neuroblastoma, a common extracranial malignant solid tumor in infants and children, is staged using the INSS system. The report discusses the use of MIBG, a structural analogue taken up by neuroendocrine cells, and PET, which utilizes glucose metabolism, for NBL detection. It highlights the importance of diagnostic accuracy and the need for follow-up scans to assess treatment response. The report compares the performance of MIBG scintigraphy and PET, considering methodological and clinical variations. It also addresses the use of risk stratification for treatment protocols and the recent trends in chemotherapy dosage. The conclusion emphasizes the importance of multimodality imaging, including MRI and MIBG, for diagnosing and managing NBL.
Review of the accuracy of PET imaging vs. MIBG scintigraphy in evaluation of skeletal
metastases of neuroblastoma in younger children
Introduction
Neuroblastoma (NBL) is considered to be the tumor in embryo of the child that generally
originates from the neural crest. This is considered to be the common extracranial malignant
solid tumors in the children and infants. It generally accounts for 7% of the cancers in children
and 15% of the deaths in children. NBL is considered to be arising anywhere with the
sympathetic nervous system and has been found to be frequent in abdomen. NBL is staged
according to the stating System of INSS which highlights about the stage 1 and 2 and the stage 3
of the NBL is about the regional disease.
Accuracy of PET imaging vs MIBG scintigraphy
Considering the accuracy for the Cochrane review, there are diagnosis through use of the
Iodine 123- metaiodobenzylguanidine (MIBG) an positron emission tomography (PET) for the
detection of a neuroblastoma. MIBG is the compound with the structural analogue that has been
actively taken up in the cells of neuroendocrine cells via norepinephrine transport (NET). It has
been seen that MIBG WB has been for the metabases with two-dimensional approach. The
structures include the excrete of the catecholamines like the bladder, urinary tract and the
gastrointestinal system (Smets et al., 2018). Here, the perspectives are based on the hypertension
where the scanning of MIBG might not be reliable as well, if the patient has been treated with
the agent of antihypertensive activity.
The other imaging modality includes the diagnosis of the NBL which is PET imaging that
has been for the use of the metabolism of glucose. It is mainly for the visualization of the
primary tumor with the metastases with F-FDG. The contrast is to the normal cells with cancer
cells that are avidly able to take up the glucose and then metabolize it to the lactase with oxygen
that is abundantly present (Gauguet et al., 2017). MIBG has been including the PET, which is not
specific for the NBL, but it is effective for the imagining modality for the diagnosis of the
neuroblastoma. The rationale of the MIBG and PET is based on the accuracy which is suspected
with the testing of the urinary catecholamines, and the NBL in the children. There is a need to
metastases of neuroblastoma in younger children
Introduction
Neuroblastoma (NBL) is considered to be the tumor in embryo of the child that generally
originates from the neural crest. This is considered to be the common extracranial malignant
solid tumors in the children and infants. It generally accounts for 7% of the cancers in children
and 15% of the deaths in children. NBL is considered to be arising anywhere with the
sympathetic nervous system and has been found to be frequent in abdomen. NBL is staged
according to the stating System of INSS which highlights about the stage 1 and 2 and the stage 3
of the NBL is about the regional disease.
Accuracy of PET imaging vs MIBG scintigraphy
Considering the accuracy for the Cochrane review, there are diagnosis through use of the
Iodine 123- metaiodobenzylguanidine (MIBG) an positron emission tomography (PET) for the
detection of a neuroblastoma. MIBG is the compound with the structural analogue that has been
actively taken up in the cells of neuroendocrine cells via norepinephrine transport (NET). It has
been seen that MIBG WB has been for the metabases with two-dimensional approach. The
structures include the excrete of the catecholamines like the bladder, urinary tract and the
gastrointestinal system (Smets et al., 2018). Here, the perspectives are based on the hypertension
where the scanning of MIBG might not be reliable as well, if the patient has been treated with
the agent of antihypertensive activity.
The other imaging modality includes the diagnosis of the NBL which is PET imaging that
has been for the use of the metabolism of glucose. It is mainly for the visualization of the
primary tumor with the metastases with F-FDG. The contrast is to the normal cells with cancer
cells that are avidly able to take up the glucose and then metabolize it to the lactase with oxygen
that is abundantly present (Gauguet et al., 2017). MIBG has been including the PET, which is not
specific for the NBL, but it is effective for the imagining modality for the diagnosis of the
neuroblastoma. The rationale of the MIBG and PET is based on the accuracy which is suspected
with the testing of the urinary catecholamines, and the NBL in the children. There is a need to
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
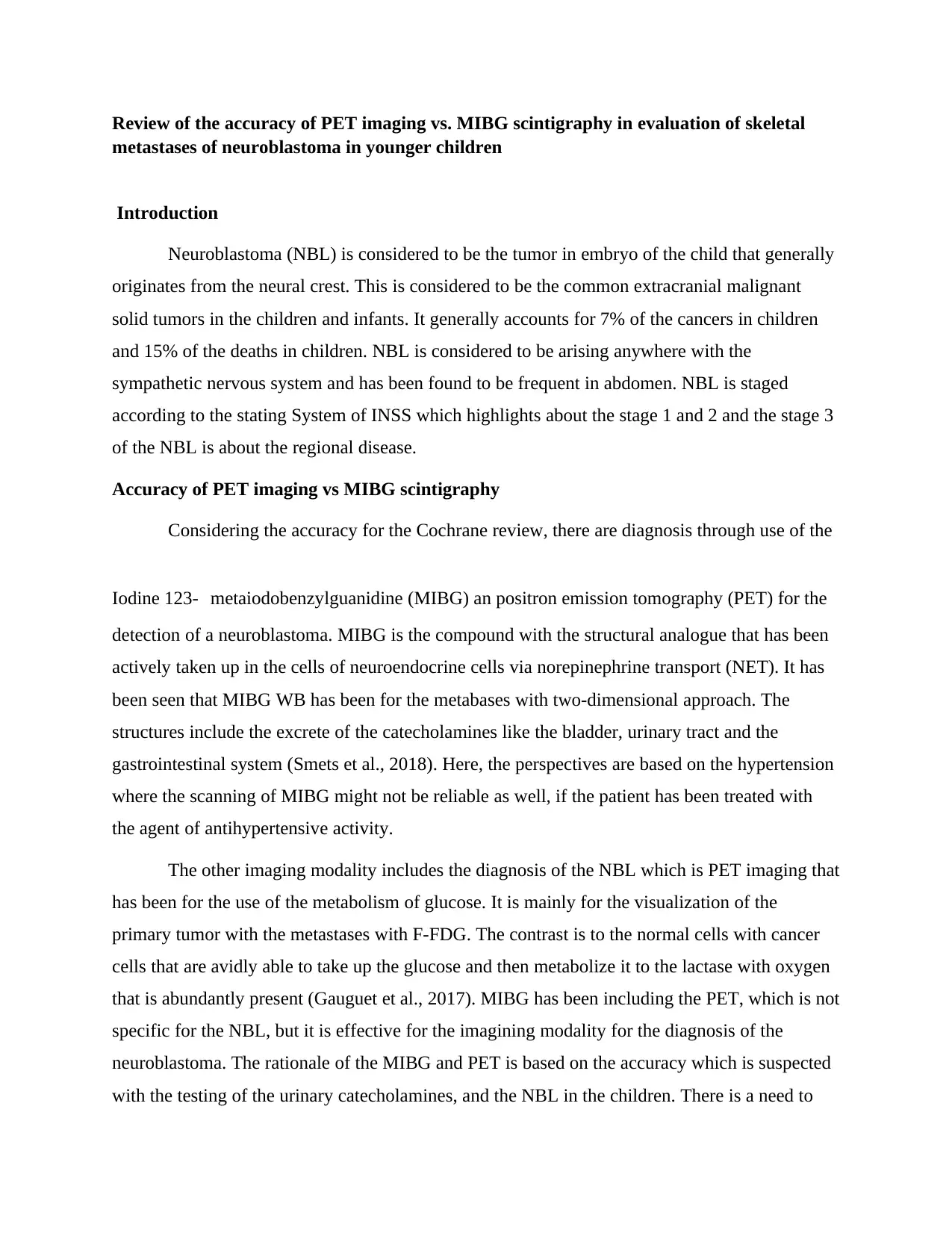
analyze about following up with the scans to assess the response to therapy. PET cases and the
scans are related to the imaging techniques where diagnostic accuracy is not yet well-established
(Uslu et al., 2015). The prognosis and the treatment is done in response to the patients who are
facing the problem of extensive scoring of scans for MIBG.
The primary focus is on determining the MIBH with detection of the NBL and the
metastases in the children who are from 0 to 18 years of age. With this, there is a need to analyze
the PET imaging with neuroblastoma and the metastases which is firstly diagnosed or is at the
recurrence from 0 to 18 years There are performances which includes the MIBG scintigraphy
when compared to the testing cases (Chen et al., 2018).
The investigation and the assessment is based on the methodological and the clinical
sources which are set for the variations and defining the positive test results. There are different
factors which tend to contribute to the heterogeneity in the diagnostic performance across the
study. The review is based on the accuracy of MIBG which includes the concordance with the
literature. The study of MIBG includes the workup of the children to reduce the problems and
scans are related to the imaging techniques where diagnostic accuracy is not yet well-established
(Uslu et al., 2015). The prognosis and the treatment is done in response to the patients who are
facing the problem of extensive scoring of scans for MIBG.
The primary focus is on determining the MIBH with detection of the NBL and the
metastases in the children who are from 0 to 18 years of age. With this, there is a need to analyze
the PET imaging with neuroblastoma and the metastases which is firstly diagnosed or is at the
recurrence from 0 to 18 years There are performances which includes the MIBG scintigraphy
when compared to the testing cases (Chen et al., 2018).
The investigation and the assessment is based on the methodological and the clinical
sources which are set for the variations and defining the positive test results. There are different
factors which tend to contribute to the heterogeneity in the diagnostic performance across the
study. The review is based on the accuracy of MIBG which includes the concordance with the
literature. The study of MIBG includes the workup of the children to reduce the problems and
the incidences related to the false positive and the negative results (Lewington et al., 2017). It
has been seen that MIBG is able to offer the unique opportunity for the imaging of the NBL with
the sensitivity tracers. They are able to produce the images of a proper resolution depending
upon the cost effectiveness. MIBG has been the analogue for the catecholamine which is
concentrated in the neuroplastic cells and the other sympathetic issue. The excretions by the
kidney is not metabolized after any injection. PET has been able to work on promising the
modality with revealing NBL in the soft tissues and skeleton. It tends to exploit the aerobic
glycolysis for the malignant cells and then retention is within the cells form of FDG. The
primary tumor concentrate FDG (fluoro-2-deoxy-D-glucose) which is directly proportional to
the tumor metastatic spread. The treatment of the protocols needs to be done in accordance to the
risk stratification with the low, intermediate and the high risks sectors (Bleeker et al., 2015). The
risk grouping system is based on the aging, staging and then selecting the features which
includes the treatment in the low and intermediate risks cases where there is an increase of the
chemotherapy dose intensity for the high risks cases (Pfluger & Piccardo, 2017). There have
been recent trends which tend to reduce the treatment with the lower and the intermediate risks
cases. The increase in the chemotherapy dose leads to the increase in the high risks cases. NBL is
used for the sanitation with treatment which is done to understand about the molecular biologic
techniques that help in detecting the residue disease in the blood and the bone marrow. The
higher risk tumors are amplified with the unresectable diseases in different groups, and the 4th
stage highlights for the diseases in the different patients.
Conclusion
The course of NBL has been to prognosticate with biological character of tumor which
can be appreciated. Here, it requires to focus on the multimodality of imaging and evaluation.
Here, MRI and MIBG have a major leading role to diagnose about the problems in the infants.
has been seen that MIBG is able to offer the unique opportunity for the imaging of the NBL with
the sensitivity tracers. They are able to produce the images of a proper resolution depending
upon the cost effectiveness. MIBG has been the analogue for the catecholamine which is
concentrated in the neuroplastic cells and the other sympathetic issue. The excretions by the
kidney is not metabolized after any injection. PET has been able to work on promising the
modality with revealing NBL in the soft tissues and skeleton. It tends to exploit the aerobic
glycolysis for the malignant cells and then retention is within the cells form of FDG. The
primary tumor concentrate FDG (fluoro-2-deoxy-D-glucose) which is directly proportional to
the tumor metastatic spread. The treatment of the protocols needs to be done in accordance to the
risk stratification with the low, intermediate and the high risks sectors (Bleeker et al., 2015). The
risk grouping system is based on the aging, staging and then selecting the features which
includes the treatment in the low and intermediate risks cases where there is an increase of the
chemotherapy dose intensity for the high risks cases (Pfluger & Piccardo, 2017). There have
been recent trends which tend to reduce the treatment with the lower and the intermediate risks
cases. The increase in the chemotherapy dose leads to the increase in the high risks cases. NBL is
used for the sanitation with treatment which is done to understand about the molecular biologic
techniques that help in detecting the residue disease in the blood and the bone marrow. The
higher risk tumors are amplified with the unresectable diseases in different groups, and the 4th
stage highlights for the diseases in the different patients.
Conclusion
The course of NBL has been to prognosticate with biological character of tumor which
can be appreciated. Here, it requires to focus on the multimodality of imaging and evaluation.
Here, MRI and MIBG have a major leading role to diagnose about the problems in the infants.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
References
Bleeker, G., Tytgat, G.A., Adam, J.A., Caron, H.N., Kremer, L.C., Hooft, L. and van Dalen,
E.C., 2015. 123I‐MIBG scintigraphy and 18F‐FDG‐PET imaging for diagnosing
neuroblastoma. Cochrane Database of Systematic Reviews, (9).
Chen, A.M., Trout, A.T. and Towbin, A.J., 2018. A review of neuroblastoma image-defined risk
factors on magnetic resonance imaging. Pediatric radiology, 48(9), pp.1337-1347.
Gauguet, J.M., Pace‐Emerson, T., Grant, F.D., Shusterman, S., DuBois, S.G., Frazier, A.L. and
Voss, S.D., 2017. Evaluation of the utility of 99mTc‐MDP bone scintigraphy versus MIBG
scintigraphy and cross‐sectional imaging for staging patients with neuroblastoma. Pediatric
blood & cancer, 64(11), p.e26601.
Lewington, V., Lambert, B., Poetschger, U., Sever, Z.B., Giammarile, F., McEwan, A.J.,
Castellani, R., Lynch, T., Shulkin, B., Drobics, M. and Staudenherz, A., 2017. 123 I-mIBG
scintigraphy in neuroblastoma: development of a SIOPEN semi-quantitative reporting, method
by an international panel. European journal of nuclear medicine and molecular imaging, 44(2),
pp.234-241.
Pfluger, T. and Piccardo, A., 2017, March. Neuroblastoma: MIBG imaging and new tracers.
In Seminars in nuclear medicine (Vol. 47, No. 2, pp. 143-157). WB Saunders.
Smets, A.M., Deurloo, E.E., Slager, T.J.E., Stoker, J. and Bipat, S., 2018. Whole-body magnetic
resonance imaging for detection of skeletal metastases in children and young people with
primary solid tumors-systematic review. Pediatric radiology, 48(2), pp.241-252.
Uslu, L., Donig, J., Link, M., Rosenberg, J., Quon, A. and Daldrup-Link, H.E., 2015. Value of
18F-FDG PET and PET/CT for evaluation of pediatric malignancies. Journal of Nuclear
Medicine, 56(2), pp.274-286.
Bleeker, G., Tytgat, G.A., Adam, J.A., Caron, H.N., Kremer, L.C., Hooft, L. and van Dalen,
E.C., 2015. 123I‐MIBG scintigraphy and 18F‐FDG‐PET imaging for diagnosing
neuroblastoma. Cochrane Database of Systematic Reviews, (9).
Chen, A.M., Trout, A.T. and Towbin, A.J., 2018. A review of neuroblastoma image-defined risk
factors on magnetic resonance imaging. Pediatric radiology, 48(9), pp.1337-1347.
Gauguet, J.M., Pace‐Emerson, T., Grant, F.D., Shusterman, S., DuBois, S.G., Frazier, A.L. and
Voss, S.D., 2017. Evaluation of the utility of 99mTc‐MDP bone scintigraphy versus MIBG
scintigraphy and cross‐sectional imaging for staging patients with neuroblastoma. Pediatric
blood & cancer, 64(11), p.e26601.
Lewington, V., Lambert, B., Poetschger, U., Sever, Z.B., Giammarile, F., McEwan, A.J.,
Castellani, R., Lynch, T., Shulkin, B., Drobics, M. and Staudenherz, A., 2017. 123 I-mIBG
scintigraphy in neuroblastoma: development of a SIOPEN semi-quantitative reporting, method
by an international panel. European journal of nuclear medicine and molecular imaging, 44(2),
pp.234-241.
Pfluger, T. and Piccardo, A., 2017, March. Neuroblastoma: MIBG imaging and new tracers.
In Seminars in nuclear medicine (Vol. 47, No. 2, pp. 143-157). WB Saunders.
Smets, A.M., Deurloo, E.E., Slager, T.J.E., Stoker, J. and Bipat, S., 2018. Whole-body magnetic
resonance imaging for detection of skeletal metastases in children and young people with
primary solid tumors-systematic review. Pediatric radiology, 48(2), pp.241-252.
Uslu, L., Donig, J., Link, M., Rosenberg, J., Quon, A. and Daldrup-Link, H.E., 2015. Value of
18F-FDG PET and PET/CT for evaluation of pediatric malignancies. Journal of Nuclear
Medicine, 56(2), pp.274-286.
1 out of 4
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




