Vaccination and Anaphylaxis: A Study on Risk in Children and Adults
VerifiedAdded on 2022/09/14
|11
|10788
|17
Report
AI Summary
This report presents a study on the risk of anaphylaxis after vaccination in children and adults, utilizing data from the Vaccine Safety Datalink (VSD). The study aimed to estimate the incidence of anaphylaxis after all vaccines combined and for individual vaccines, and to describe the demographic and clinical characteristics of confirmed cases. Researchers identified potential cases using ICD-9-CM codes and validated them through medical record reviews, applying the Brighton Collaboration definition for anaphylaxis. The study found a low incidence rate of anaphylaxis, approximately 1.31 cases per million vaccine doses, with no significant variation by age. The onset of symptoms was predominantly within 4 hours of vaccination. The report emphasizes that despite its rarity, anaphylaxis is a potentially life-threatening emergency that vaccine providers need to be prepared to treat. The study highlights the importance of vaccine safety monitoring and the need for preparedness in handling adverse reactions, especially given the increasing use of vaccines in broader age groups and the introduction of new vaccines.
Risk of anaphylaxis after vaccination in children and adults
Michael M. McNeil, MD, MPH,a Eric S. Weintraub, MPH,a Jonathan Duffy, MD, MPH,a Lakshmi Sukumaran, MD, MPH,a
Steven J. Jacobsen, MD, PhD,b Nicola P. Klein, MD, PhD,c Simon J. Hambidge, MD, PhD,d Grace M. Lee, MD, MPH,e
Lisa A. Jackson, MD, MPH,f Stephanie A. Irving, MHS,g Jennifer P. King, MPH,h Elyse O. Kharbanda, MD, MPH,i
Robert A. Bednarczyk, PhD,j and Frank DeStefano, MD, MPHa Atlanta, Ga, Pasadena and Oakland, Calif, Denver, Colo
Boston, Mass, Seattle, Wash, Portland, Ore, Marshfield, Wis, and Minneapolis, Minn
Background: Anaphylaxis is a potentially life-threatening
allergic reaction.The risk of anaphylaxis after vaccination has
not been well described in adults or with newer vaccines in
children.
Objective: We sought to estimate the incidence of anaphylaxis
after vaccines and describe the demographic and clinical
characteristics of confirmed cases of anaphylaxis.
Methods: Using health care data from the Vaccine Safety
Datalink,we determined rates of anaphylaxis after vaccination
in children and adults.We first identified all patients with a
vaccination record from January 2009 through December 2011
and used diagnostic and procedure codes to identify potential
anaphylaxis cases.Medical records of potential cases were
reviewed.Confirmed cases met the Brighton Collaboration
definition for anaphylaxis and had to be determined to be
vaccine triggered.We calculated the incidence of anaphylaxis
after all vaccines combined and for selected individual vaccines.
Results: We identified 33 confirmed vaccine-triggered
anaphylaxis cases that occurred after 25,173,965 vaccine doses.
The rate of anaphylaxis was 1.31 (95% CI, 0.90-1.84) per million
vaccine doses.The incidence did not vary significantly by age,
and there was a nonsignificant female predominance.Vaccine-
specific rates included 1.35 (95% CI, 0.65-2.47) per million dos
for inactivated trivalent influenza vaccine (10 cases,7,434,628
doses given alone) and 1.83 (95% CI,0.22-6.63) per million
doses for inactivated monovalent influenza vaccine (2 cases,
1,090,279 doses given alone).The onset of symptoms among
cases was within 30 minutes (8 cases),30 to less than
120 minutes (8 cases),2 to less than 4 hours (10 cases),4 to
8 hours (2 cases),the next day (1 case),and not documented
(4 cases).
Conclusion: Anaphylaxis after vaccination is rare in all age
groups.Despite its rarity,anaphylaxis is a potentially
life-threatening medical emergency that vaccine providers
need to be prepared to treat.(J Allergy Clin Immunol
2015;nnn:nnn-nnn.)
Key words:Anaphylaxis, vaccine safety, immunization
Anaphylaxisis an acute,systemic,and potentially lethal
hypersensitivityreaction with multiple organ system
involvement.1-4 Anaphylaxiscan occur after exposureto
allergens from a variety of sources, including food, venom, d
and immunizations.Virtually all vaccines have the potential to
trigger anaphylaxis.5,6Recently, a committee of the Institute of
Medicine (IOM) concluded that epidemiologic and mechanis
evidence convincingly supports a causalrelationship between
anaphylaxisand severalchildhood and adolescentvaccines
(measles,mumps,rubella [MMR]vaccine;varicella vaccine;
influenza vaccine; hepatitis B vaccine; diphtheria toxoid-, te
toxoid-, and acellular pertussis antigen-containing vaccines;
meningococcalvaccine),favors acceptanceof a causal
relationshipfor the humanpapillomavirusvaccine(HPV;
mechanisticevidenceonly), and is inadequatefor hepatitis
A vaccine (HAV).7 Vaccine componentsthat might be
allergenic include the vaccine antigen,residual animal protein,
antimicrobial agents,preservatives, stabilizers,or other vaccine
components.8 Individualvaccine componentsthathave been
implicated in acute vaccine reactions include egg protein, g
milk proteins,and potentially otheradditives.Naturalrubber
latex, which can be contained in the syringe plunger, the tip
prefilled syringes,and vialstoppers,is another potentialcause
of anaphylaxis.9
The life-threatening nature of anaphylaxis and the accept
of a causal relationship with certain vaccines make estimati
the magnitude of risk after vaccination an important priority
researchinto vaccinesafety.Currentdata are limitedfor
quantifying the risk of anaphylaxis associated with vaccinat
in general or with specific vaccines. Given the infrequency w
which anaphylaxis occurs,large populations are necessary to
Fromathe Immunization Safety Office, Division of Healthcare Quality Promotion, Na-
tionalCenter for Emerging and Zoonotic Infectious Diseases,Centers for Disease
Control and Prevention, Atlanta;bSouthern California Kaiser Permanente, Pasadena;
cKaiser PermanenteVaccineStudy Center,Oakland;dthe Institutefor Health
Research, Kaiser Permanente, Denver;ethe Department of Population Medicine, Har-
vard Medical School and the Harvard Pilgrim Health Care Institute, Boston;fGroup
Health Research Institute, Seattle;gthe Center for Health Research, Kaiser Permanente
Northwest,Portland;hthe Marshfield Clinic Research Foundation,Marshfield;ithe
HealthPartnersInstitutefor Education and Research,Minneapolis;and jKaiser
Permanente Center for Health Research,and the Rollins Schoolof Public Health,
Emory University, Atlanta.
The findings and conclusions of this report are those of the authors and do not necessarily
representthe officialpolicy orposition ofthe Centers forDisease Controland
Prevention (CDC).Use of trade names and commercial sources is for identification
only and does notimply endorsementby the CDC.The Vaccine Safety Datalink
Project is funded by the CDC. This study was supported by the CDC, and no external
funding was secured.
Disclosure of potential conflict of interest: L. Sukumaran has received research support
from the National Institutes of Health (NIH).N. P. Klein has received research and
travelsupport,as wellas paymentfor writing/reviewing the manuscript,from the
Centers for Disease Control and Prevention (CDC) and has received research support
from Sanofi Pasteur,GlaxoSmithKline,Novartis,MedImmune,Protein Science,
Merck, Pfizer, and Nuron Biotech. S. J. Hambidge has received research support from
the CDC Vaccine Safety Datalink. G. M. Lee and L. A. Jackson have received research
support from the CDC. S. A. Irving has received research and travel support from the
CDC. J. P. King has received research support from the CDC. The rest of the authors
declare that they have no relevant conflicts of interest.
Received for publication March 18, 2015; revised July 31, 2015; accepted for publication
July 31, 2015.
Corresponding author: Michael M. McNeil, MD, MPH, Centers for Disease Control and
Prevention, 1600 Clifton Road NE, MS D-26, Atlanta, GA 30333. E-mail: mmm2@
cdc.gov.
0091-6749
http://dx.doi.org/10.1016/j.jaci.2015.07.048
1
Michael M. McNeil, MD, MPH,a Eric S. Weintraub, MPH,a Jonathan Duffy, MD, MPH,a Lakshmi Sukumaran, MD, MPH,a
Steven J. Jacobsen, MD, PhD,b Nicola P. Klein, MD, PhD,c Simon J. Hambidge, MD, PhD,d Grace M. Lee, MD, MPH,e
Lisa A. Jackson, MD, MPH,f Stephanie A. Irving, MHS,g Jennifer P. King, MPH,h Elyse O. Kharbanda, MD, MPH,i
Robert A. Bednarczyk, PhD,j and Frank DeStefano, MD, MPHa Atlanta, Ga, Pasadena and Oakland, Calif, Denver, Colo
Boston, Mass, Seattle, Wash, Portland, Ore, Marshfield, Wis, and Minneapolis, Minn
Background: Anaphylaxis is a potentially life-threatening
allergic reaction.The risk of anaphylaxis after vaccination has
not been well described in adults or with newer vaccines in
children.
Objective: We sought to estimate the incidence of anaphylaxis
after vaccines and describe the demographic and clinical
characteristics of confirmed cases of anaphylaxis.
Methods: Using health care data from the Vaccine Safety
Datalink,we determined rates of anaphylaxis after vaccination
in children and adults.We first identified all patients with a
vaccination record from January 2009 through December 2011
and used diagnostic and procedure codes to identify potential
anaphylaxis cases.Medical records of potential cases were
reviewed.Confirmed cases met the Brighton Collaboration
definition for anaphylaxis and had to be determined to be
vaccine triggered.We calculated the incidence of anaphylaxis
after all vaccines combined and for selected individual vaccines.
Results: We identified 33 confirmed vaccine-triggered
anaphylaxis cases that occurred after 25,173,965 vaccine doses.
The rate of anaphylaxis was 1.31 (95% CI, 0.90-1.84) per million
vaccine doses.The incidence did not vary significantly by age,
and there was a nonsignificant female predominance.Vaccine-
specific rates included 1.35 (95% CI, 0.65-2.47) per million dos
for inactivated trivalent influenza vaccine (10 cases,7,434,628
doses given alone) and 1.83 (95% CI,0.22-6.63) per million
doses for inactivated monovalent influenza vaccine (2 cases,
1,090,279 doses given alone).The onset of symptoms among
cases was within 30 minutes (8 cases),30 to less than
120 minutes (8 cases),2 to less than 4 hours (10 cases),4 to
8 hours (2 cases),the next day (1 case),and not documented
(4 cases).
Conclusion: Anaphylaxis after vaccination is rare in all age
groups.Despite its rarity,anaphylaxis is a potentially
life-threatening medical emergency that vaccine providers
need to be prepared to treat.(J Allergy Clin Immunol
2015;nnn:nnn-nnn.)
Key words:Anaphylaxis, vaccine safety, immunization
Anaphylaxisis an acute,systemic,and potentially lethal
hypersensitivityreaction with multiple organ system
involvement.1-4 Anaphylaxiscan occur after exposureto
allergens from a variety of sources, including food, venom, d
and immunizations.Virtually all vaccines have the potential to
trigger anaphylaxis.5,6Recently, a committee of the Institute of
Medicine (IOM) concluded that epidemiologic and mechanis
evidence convincingly supports a causalrelationship between
anaphylaxisand severalchildhood and adolescentvaccines
(measles,mumps,rubella [MMR]vaccine;varicella vaccine;
influenza vaccine; hepatitis B vaccine; diphtheria toxoid-, te
toxoid-, and acellular pertussis antigen-containing vaccines;
meningococcalvaccine),favors acceptanceof a causal
relationshipfor the humanpapillomavirusvaccine(HPV;
mechanisticevidenceonly), and is inadequatefor hepatitis
A vaccine (HAV).7 Vaccine componentsthat might be
allergenic include the vaccine antigen,residual animal protein,
antimicrobial agents,preservatives, stabilizers,or other vaccine
components.8 Individualvaccine componentsthathave been
implicated in acute vaccine reactions include egg protein, g
milk proteins,and potentially otheradditives.Naturalrubber
latex, which can be contained in the syringe plunger, the tip
prefilled syringes,and vialstoppers,is another potentialcause
of anaphylaxis.9
The life-threatening nature of anaphylaxis and the accept
of a causal relationship with certain vaccines make estimati
the magnitude of risk after vaccination an important priority
researchinto vaccinesafety.Currentdata are limitedfor
quantifying the risk of anaphylaxis associated with vaccinat
in general or with specific vaccines. Given the infrequency w
which anaphylaxis occurs,large populations are necessary to
Fromathe Immunization Safety Office, Division of Healthcare Quality Promotion, Na-
tionalCenter for Emerging and Zoonotic Infectious Diseases,Centers for Disease
Control and Prevention, Atlanta;bSouthern California Kaiser Permanente, Pasadena;
cKaiser PermanenteVaccineStudy Center,Oakland;dthe Institutefor Health
Research, Kaiser Permanente, Denver;ethe Department of Population Medicine, Har-
vard Medical School and the Harvard Pilgrim Health Care Institute, Boston;fGroup
Health Research Institute, Seattle;gthe Center for Health Research, Kaiser Permanente
Northwest,Portland;hthe Marshfield Clinic Research Foundation,Marshfield;ithe
HealthPartnersInstitutefor Education and Research,Minneapolis;and jKaiser
Permanente Center for Health Research,and the Rollins Schoolof Public Health,
Emory University, Atlanta.
The findings and conclusions of this report are those of the authors and do not necessarily
representthe officialpolicy orposition ofthe Centers forDisease Controland
Prevention (CDC).Use of trade names and commercial sources is for identification
only and does notimply endorsementby the CDC.The Vaccine Safety Datalink
Project is funded by the CDC. This study was supported by the CDC, and no external
funding was secured.
Disclosure of potential conflict of interest: L. Sukumaran has received research support
from the National Institutes of Health (NIH).N. P. Klein has received research and
travelsupport,as wellas paymentfor writing/reviewing the manuscript,from the
Centers for Disease Control and Prevention (CDC) and has received research support
from Sanofi Pasteur,GlaxoSmithKline,Novartis,MedImmune,Protein Science,
Merck, Pfizer, and Nuron Biotech. S. J. Hambidge has received research support from
the CDC Vaccine Safety Datalink. G. M. Lee and L. A. Jackson have received research
support from the CDC. S. A. Irving has received research and travel support from the
CDC. J. P. King has received research support from the CDC. The rest of the authors
declare that they have no relevant conflicts of interest.
Received for publication March 18, 2015; revised July 31, 2015; accepted for publication
July 31, 2015.
Corresponding author: Michael M. McNeil, MD, MPH, Centers for Disease Control and
Prevention, 1600 Clifton Road NE, MS D-26, Atlanta, GA 30333. E-mail: mmm2@
cdc.gov.
0091-6749
http://dx.doi.org/10.1016/j.jaci.2015.07.048
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Abbreviations used
DT: Diphtheria and tetanus toxoids
DTaP and Tdap:Diphtheria, tetanus, and acellular pertussis vaccines
ED: Emergency department
HAV: Hepatitis A vaccine
HPV: Human papillomavirus vaccine
HZV: Herpes zoster vaccine
ICD-9-CM: International Classification of Diseases, Ninth
Revision, Clinical Modification
IOM: Institute of Medicine
MIV: Monovalent influenza vaccine
MMR: Measles, mumps, rubella vaccine
OPD: Outpatient department
TIV: Trivalent influenza vaccine
VSD: Vaccine Safety Datalink
study thisexposure-disease relationship.The Vaccine Safety
Datalink (VSD), a collaboration between the Centers for Disease
Control and Prevention’s Immunization Safety Office and several
integrated health care systems across the United States,offers
such a population.10The only population-based data on the risk of
anaphylaxis associated with vaccination are from a much-cited
historical VSD study conducted by Bohlke et al11 covering the
years 1991-1997. At the time of the study by Bohlke et al,11the
VSD comprised 4 sites with a population of approximately 6
million persons,and the focus was on the safety of childhood
immunizations;there was limited use ofinfluenza vaccine in
the pediatric population. Bohlke et al11used an ad hoc algorithm
in their study to classify anaphylaxis cases. Based on 5 confirmed
cases,the incidencerate of anaphylaxisin childrenand
adolescents was estimated to be 0.65 (95% CI, 0.21-1.53) cases
per million vaccine doses.11
Recently,since the report by Bohlke et al,11 there have been
changes to the recommended childhood and adult immunization
schedules,with broaderage groups recommended to receive
certain vaccines and the introduction of severalnew vaccines
and vaccine combinations.Importantly,influenza vaccine has
been generally recommended for the entire US population aged
6 months or greater, with more than 100 million doses of influenza
vaccine administered annually.Because eggs are used in the
production ofmostinfluenzavaccines,thesecontain small
amountsof ovalbumin,and potentialanaphylacticreactions
among patients with egg allergy are an important safety concern
for influenzavaccines.A recent advancein vaccinesafety
science has been the Brighton Collaboration’s developmentof
standardized case definitions and guidelines for data collection,
analysis,and presentation.In 2007,the Brighton Collaboration
published a standardized case definition foranaphylaxis after
vaccinations.12 Lastly, since the Bohlke et al report,11 VSD has
expanded to a total of 9 sites with the ability to monitor vaccine
safety in a larger and more diverse population of both children
and adults.13
Therefore we conducted a study using recentVSD data and
applied the Brighton criteria in our analysis. Our study objectives
included (1)estimating the incidence ofanaphylaxis afterall
vaccinescombined and forindividualvaccines(when dose
numberswere sufficientto allow vaccine-specificanalysis
[eg,influenza vaccines])and (2)describing the demographic
and clinical characteristics of confirmed cases of anaphylaxis.
METHODS
Study population
Our study population included all children and adults enrolled in the h
plans at 9 VSD sites who received 1 or more vaccines during the period f
January 1, 2009 through December 31, 2011. Currently, the VSD has dat
approximately 9.3 million subjects available annually, including 2.1 millio
children and 7.2 million adults.13 The participating VSD sitesmaintain
automated databasesof health care encounters,including immunization
registrieswith detailed information on vaccinesadministered;have the
capability to access written orelectronic medicalrecords and otherdata
sources to provide detailed information on specific health care encounte
and provide integrated health care services to their members so that the
spectrum of health care from outpatient department (OPD) and emergen
department (ED) visits to hospitalizations can be captured. The study pro
was approved by institutional review boards at the Centers for Disease C
and Prevention and each VSD site,and itwas determined thatinformed
consent was not required.
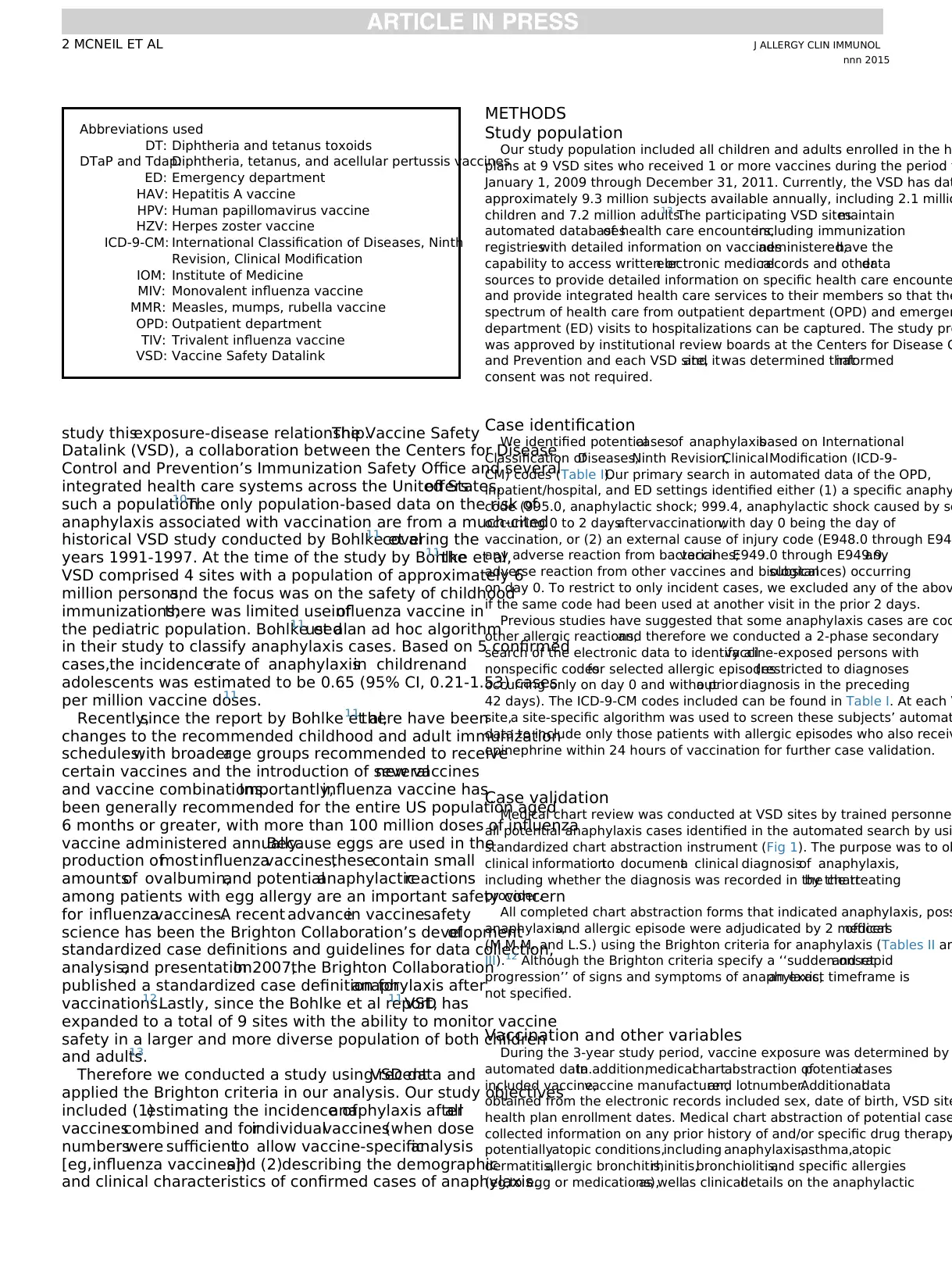
Case identification
We identified potentialcasesof anaphylaxisbased on International
Classification ofDiseases,Ninth Revision,ClinicalModification (ICD-9-
CM) codes (Table I).Our primary search in automated data of the OPD,
inpatient/hospital, and ED settings identified either (1) a specific anaphy
code (995.0, anaphylactic shock; 999.4, anaphylactic shock caused by se
occurring 0 to 2 daysaftervaccination,with day 0 being the day of
vaccination, or (2) an external cause of injury code (E948.0 through E94
any adverse reaction from bacterialvaccines;E949.0 through E949.9,any
adverse reaction from other vaccines and biologicalsubstances) occurring
on day 0. To restrict to only incident cases, we excluded any of the abov
if the same code had been used at another visit in the prior 2 days.
Previous studies have suggested that some anaphylaxis cases are cod
other allergic reactions,and therefore we conducted a 2-phase secondary
search of the electronic data to identify allvaccine-exposed persons with
nonspecific codesfor selected allergic episodes(restricted to diagnoses
occurring only on day 0 and withouta priordiagnosis in the preceding
42 days). The ICD-9-CM codes included can be found in Table I. At each V
site,a site-specific algorithm was used to screen these subjects’ automat
data to include only those patients with allergic episodes who also receiv
epinephrine within 24 hours of vaccination for further case validation.
Case validation
Medical chart review was conducted at VSD sites by trained personnel
all potential anaphylaxis cases identified in the automated search by usi
standardized chart abstraction instrument (Fig 1). The purpose was to ob
clinical informationto documenta clinical diagnosisof anaphylaxis,
including whether the diagnosis was recorded in the chartby the treating
provider.
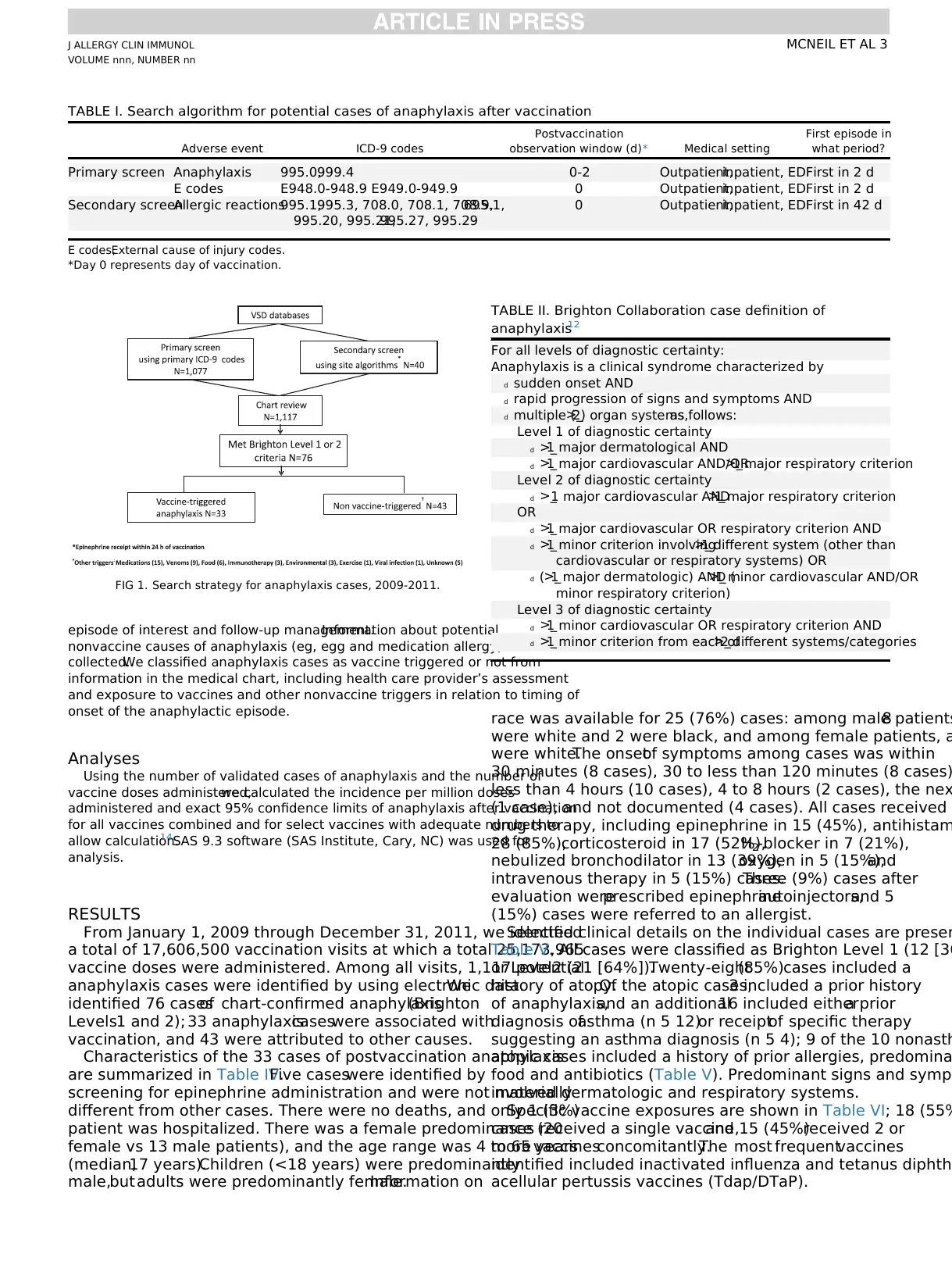
All completed chart abstraction forms that indicated anaphylaxis, poss
anaphylaxis,and allergic episode were adjudicated by 2 medicalofficers
(M.M.M. and L.S.) using the Brighton criteria for anaphylaxis (Tables II an
III). 12 Although the Brighton criteria specify a ‘‘sudden onsetand rapid
progression’’ of signs and symptoms of anaphylaxis,an exact timeframe is
not specified.
Vaccination and other variables
During the 3-year study period, vaccine exposure was determined by
automated data.In addition,medicalchartabstraction ofpotentialcases
included vaccine,vaccine manufacturer,and lotnumber.Additionaldata
obtained from the electronic records included sex, date of birth, VSD site
health plan enrollment dates. Medical chart abstraction of potential case
collected information on any prior history of and/or specific drug therapy
potentiallyatopic conditions,including anaphylaxis,asthma,atopic
dermatitis,allergic bronchitis,rhinitis,bronchiolitis,and specific allergies
(eg,to egg or medications),as wellas clinicaldetails on the anaphylactic
J ALLERGY CLIN IMMUNOL
nnn 2015
2 MCNEIL ET AL
DT: Diphtheria and tetanus toxoids
DTaP and Tdap:Diphtheria, tetanus, and acellular pertussis vaccines
ED: Emergency department
HAV: Hepatitis A vaccine
HPV: Human papillomavirus vaccine
HZV: Herpes zoster vaccine
ICD-9-CM: International Classification of Diseases, Ninth
Revision, Clinical Modification
IOM: Institute of Medicine
MIV: Monovalent influenza vaccine
MMR: Measles, mumps, rubella vaccine
OPD: Outpatient department
TIV: Trivalent influenza vaccine
VSD: Vaccine Safety Datalink
study thisexposure-disease relationship.The Vaccine Safety
Datalink (VSD), a collaboration between the Centers for Disease
Control and Prevention’s Immunization Safety Office and several
integrated health care systems across the United States,offers
such a population.10The only population-based data on the risk of
anaphylaxis associated with vaccination are from a much-cited
historical VSD study conducted by Bohlke et al11 covering the
years 1991-1997. At the time of the study by Bohlke et al,11the
VSD comprised 4 sites with a population of approximately 6
million persons,and the focus was on the safety of childhood
immunizations;there was limited use ofinfluenza vaccine in
the pediatric population. Bohlke et al11used an ad hoc algorithm
in their study to classify anaphylaxis cases. Based on 5 confirmed
cases,the incidencerate of anaphylaxisin childrenand
adolescents was estimated to be 0.65 (95% CI, 0.21-1.53) cases
per million vaccine doses.11
Recently,since the report by Bohlke et al,11 there have been
changes to the recommended childhood and adult immunization
schedules,with broaderage groups recommended to receive
certain vaccines and the introduction of severalnew vaccines
and vaccine combinations.Importantly,influenza vaccine has
been generally recommended for the entire US population aged
6 months or greater, with more than 100 million doses of influenza
vaccine administered annually.Because eggs are used in the
production ofmostinfluenzavaccines,thesecontain small
amountsof ovalbumin,and potentialanaphylacticreactions
among patients with egg allergy are an important safety concern
for influenzavaccines.A recent advancein vaccinesafety
science has been the Brighton Collaboration’s developmentof
standardized case definitions and guidelines for data collection,
analysis,and presentation.In 2007,the Brighton Collaboration
published a standardized case definition foranaphylaxis after
vaccinations.12 Lastly, since the Bohlke et al report,11 VSD has
expanded to a total of 9 sites with the ability to monitor vaccine
safety in a larger and more diverse population of both children
and adults.13
Therefore we conducted a study using recentVSD data and
applied the Brighton criteria in our analysis. Our study objectives
included (1)estimating the incidence ofanaphylaxis afterall
vaccinescombined and forindividualvaccines(when dose
numberswere sufficientto allow vaccine-specificanalysis
[eg,influenza vaccines])and (2)describing the demographic
and clinical characteristics of confirmed cases of anaphylaxis.
METHODS
Study population
Our study population included all children and adults enrolled in the h
plans at 9 VSD sites who received 1 or more vaccines during the period f
January 1, 2009 through December 31, 2011. Currently, the VSD has dat
approximately 9.3 million subjects available annually, including 2.1 millio
children and 7.2 million adults.13 The participating VSD sitesmaintain
automated databasesof health care encounters,including immunization
registrieswith detailed information on vaccinesadministered;have the
capability to access written orelectronic medicalrecords and otherdata
sources to provide detailed information on specific health care encounte
and provide integrated health care services to their members so that the
spectrum of health care from outpatient department (OPD) and emergen
department (ED) visits to hospitalizations can be captured. The study pro
was approved by institutional review boards at the Centers for Disease C
and Prevention and each VSD site,and itwas determined thatinformed
consent was not required.
Case identification
We identified potentialcasesof anaphylaxisbased on International
Classification ofDiseases,Ninth Revision,ClinicalModification (ICD-9-
CM) codes (Table I).Our primary search in automated data of the OPD,
inpatient/hospital, and ED settings identified either (1) a specific anaphy
code (995.0, anaphylactic shock; 999.4, anaphylactic shock caused by se
occurring 0 to 2 daysaftervaccination,with day 0 being the day of
vaccination, or (2) an external cause of injury code (E948.0 through E94
any adverse reaction from bacterialvaccines;E949.0 through E949.9,any
adverse reaction from other vaccines and biologicalsubstances) occurring
on day 0. To restrict to only incident cases, we excluded any of the abov
if the same code had been used at another visit in the prior 2 days.
Previous studies have suggested that some anaphylaxis cases are cod
other allergic reactions,and therefore we conducted a 2-phase secondary
search of the electronic data to identify allvaccine-exposed persons with
nonspecific codesfor selected allergic episodes(restricted to diagnoses
occurring only on day 0 and withouta priordiagnosis in the preceding
42 days). The ICD-9-CM codes included can be found in Table I. At each V
site,a site-specific algorithm was used to screen these subjects’ automat
data to include only those patients with allergic episodes who also receiv
epinephrine within 24 hours of vaccination for further case validation.
Case validation
Medical chart review was conducted at VSD sites by trained personnel
all potential anaphylaxis cases identified in the automated search by usi
standardized chart abstraction instrument (Fig 1). The purpose was to ob
clinical informationto documenta clinical diagnosisof anaphylaxis,
including whether the diagnosis was recorded in the chartby the treating
provider.
All completed chart abstraction forms that indicated anaphylaxis, poss
anaphylaxis,and allergic episode were adjudicated by 2 medicalofficers
(M.M.M. and L.S.) using the Brighton criteria for anaphylaxis (Tables II an
III). 12 Although the Brighton criteria specify a ‘‘sudden onsetand rapid
progression’’ of signs and symptoms of anaphylaxis,an exact timeframe is
not specified.
Vaccination and other variables
During the 3-year study period, vaccine exposure was determined by
automated data.In addition,medicalchartabstraction ofpotentialcases
included vaccine,vaccine manufacturer,and lotnumber.Additionaldata
obtained from the electronic records included sex, date of birth, VSD site
health plan enrollment dates. Medical chart abstraction of potential case
collected information on any prior history of and/or specific drug therapy
potentiallyatopic conditions,including anaphylaxis,asthma,atopic
dermatitis,allergic bronchitis,rhinitis,bronchiolitis,and specific allergies
(eg,to egg or medications),as wellas clinicaldetails on the anaphylactic
J ALLERGY CLIN IMMUNOL
nnn 2015
2 MCNEIL ET AL
episode of interest and follow-up management.Information about potential
nonvaccine causes of anaphylaxis (eg, egg and medication allergy) was also
collected.We classified anaphylaxis cases as vaccine triggered or not from
information in the medical chart, including health care provider’s assessment
and exposure to vaccines and other nonvaccine triggers in relation to timing of
onset of the anaphylactic episode.
Analyses
Using the number of validated cases of anaphylaxis and the number of
vaccine doses administered,we calculated the incidence per million doses
administered and exact 95% confidence limits of anaphylaxis after vaccination
for all vaccines combined and for select vaccines with adequate numbers to
allow calculation.14SAS 9.3 software (SAS Institute, Cary, NC) was used for
analysis.
RESULTS
From January 1, 2009 through December 31, 2011, we identified
a total of 17,606,500 vaccination visits at which a total 25,173,965
vaccine doses were administered. Among all visits, 1,117 potential
anaphylaxis cases were identified by using electronic data.We
identified 76 casesof chart-confirmed anaphylaxis(Brighton
Levels1 and 2); 33 anaphylaxiscaseswere associated with
vaccination, and 43 were attributed to other causes.
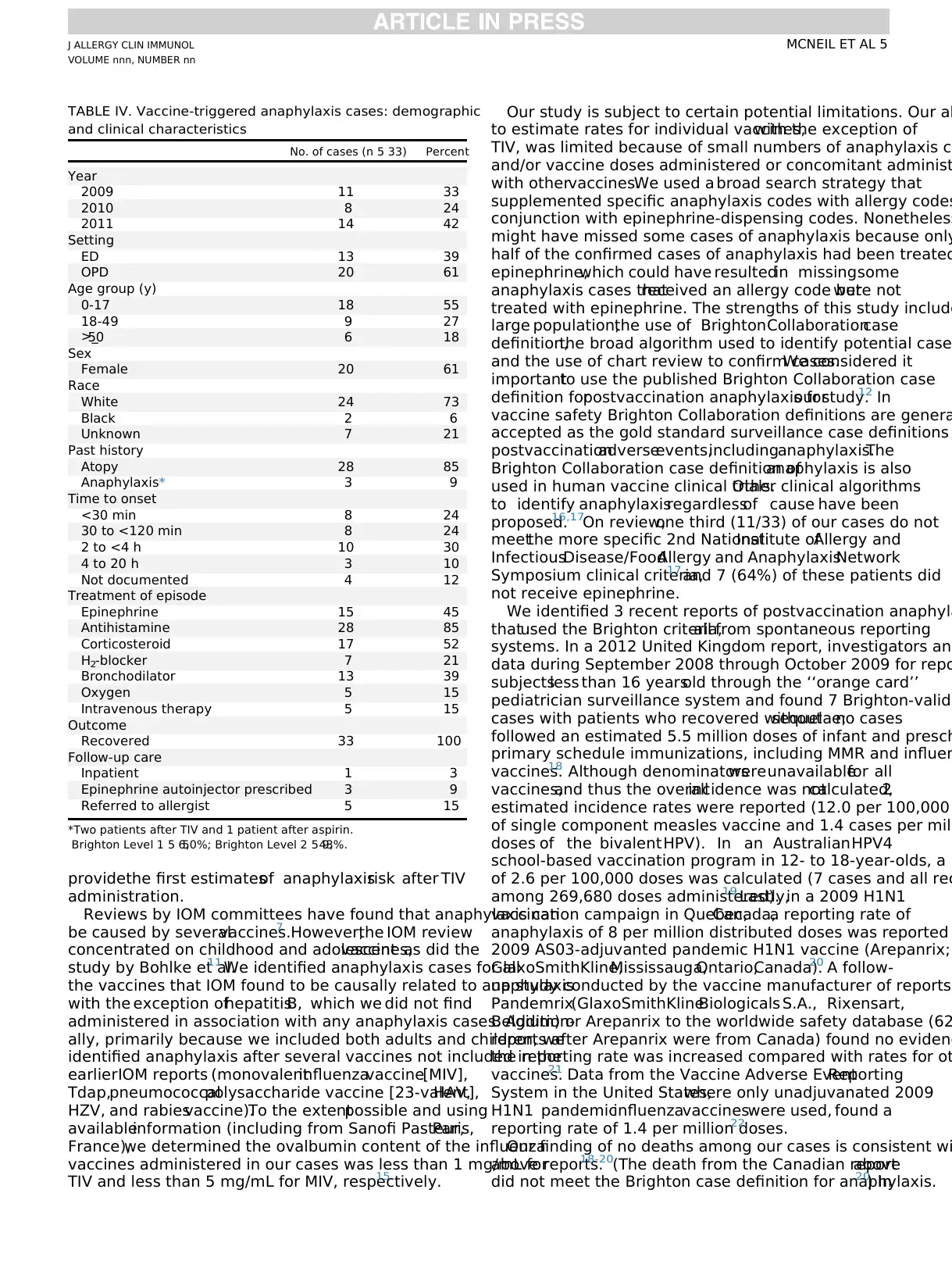
Characteristics of the 33 cases of postvaccination anaphylaxis
are summarized in Table IV.Five caseswere identified by
screening for epinephrine administration and were not materially
different from other cases. There were no deaths, and only 1 (3%)
patient was hospitalized. There was a female predominance (20
female vs 13 male patients), and the age range was 4 to 65 years
(median,17 years).Children (<18 years) were predominantly
male,but adults were predominantly female.Information on
race was available for 25 (76%) cases: among male patients8
were white and 2 were black, and among female patients, a
were white.The onsetof symptoms among cases was within
30 minutes (8 cases), 30 to less than 120 minutes (8 cases)
less than 4 hours (10 cases), 4 to 8 hours (2 cases), the nex
(1 case), and not documented (4 cases). All cases received
drug therapy, including epinephrine in 15 (45%), antihistam
28 (85%),corticosteroid in 17 (52%),H2-blocker in 7 (21%),
nebulized bronchodilator in 13 (39%),oxygen in 5 (15%),and
intravenous therapy in 5 (15%) cases.Three (9%) cases after
evaluation wereprescribed epinephrineautoinjectors,and 5
(15%) cases were referred to an allergist.
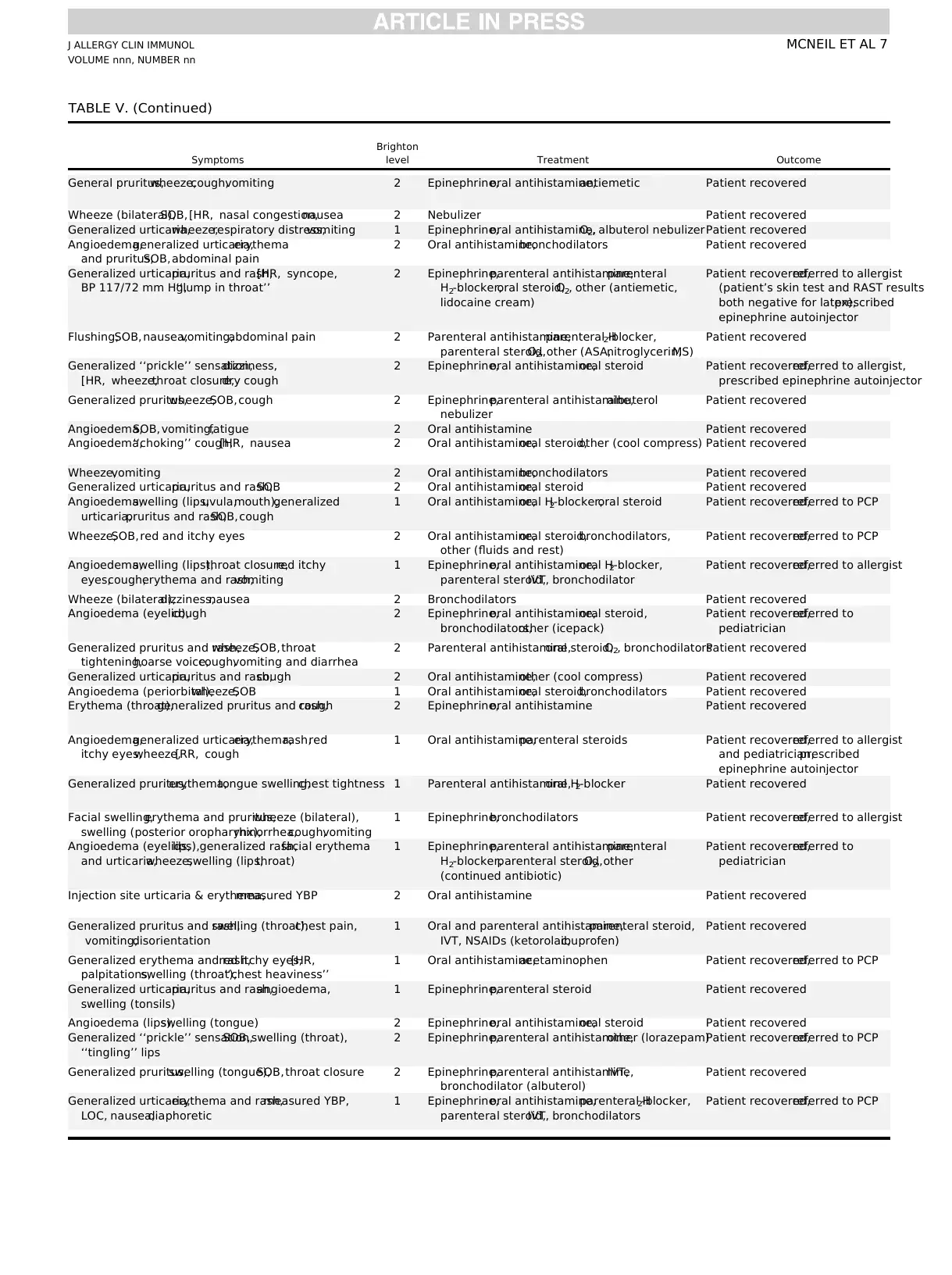
Selected clinical details on the individual cases are presen
Table V. All cases were classified as Brighton Level 1 (12 [36
or Level2 (21 [64%]).Twenty-eight(85%)cases included a
history of atopy.Of the atopic cases,3 included a prior history
of anaphylaxis,and an additional16 included eithera prior
diagnosis ofasthma (n 5 12)or receiptof specific therapy
suggesting an asthma diagnosis (n 5 4); 9 of the 10 nonasth
atopic cases included a history of prior allergies, predomina
food and antibiotics (Table V). Predominant signs and sympt
involved dermatologic and respiratory systems.
Specific vaccine exposures are shown in Table VI; 18 (55%
cases received a single vaccine,and 15 (45%)received 2 or
more vaccinesconcomitantly.The most frequentvaccines
identified included inactivated influenza and tetanus diphth
acellular pertussis vaccines (Tdap/DTaP).
TABLE I. Search algorithm for potential cases of anaphylaxis after vaccination
Adverse event ICD-9 codes
Postvaccination
observation window (d)* Medical setting
First episode in
what period?
Primary screen Anaphylaxis 995.0,999.4 0-2 Outpatient,inpatient, EDFirst in 2 d
E codes E948.0-948.9 E949.0-949.9 0 Outpatient,inpatient, EDFirst in 2 d
Secondary screenAllergic reactions995.1,995.3, 708.0, 708.1, 708.9,695.1,
995.20, 995.21,995.27, 995.29
0 Outpatient,inpatient, EDFirst in 42 d
E codes,External cause of injury codes.
*Day 0 represents day of vaccination.
FIG 1. Search strategy for anaphylaxis cases, 2009-2011.
TABLE II. Brighton Collaboration case definition of
anaphylaxis12
For all levels of diagnostic certainty:
Anaphylaxis is a clinical syndrome characterized by
d sudden onset AND
d rapid progression of signs and symptoms AND
d multiple (>_2) organ systems,as follows:
Level 1 of diagnostic certainty
d >_1 major dermatological AND
d >_1 major cardiovascular AND/OR>_1 major respiratory criterion
Level 2 of diagnostic certainty
d >_1 major cardiovascular AND>_1 major respiratory criterion
OR
d >_1 major cardiovascular OR respiratory criterion AND
d >_1 minor criterion involving>_1 different system (other than
cardiovascular or respiratory systems) OR
d (>_1 major dermatologic) AND (>_1 minor cardiovascular AND/OR
minor respiratory criterion)
Level 3 of diagnostic certainty
d >_1 minor cardiovascular OR respiratory criterion AND
d >_1 minor criterion from each of>_2 different systems/categories
J ALLERGY CLIN IMMUNOL
VOLUME nnn, NUMBER nn
MCNEIL ET AL 3
nonvaccine causes of anaphylaxis (eg, egg and medication allergy) was also
collected.We classified anaphylaxis cases as vaccine triggered or not from
information in the medical chart, including health care provider’s assessment
and exposure to vaccines and other nonvaccine triggers in relation to timing of
onset of the anaphylactic episode.
Analyses
Using the number of validated cases of anaphylaxis and the number of
vaccine doses administered,we calculated the incidence per million doses
administered and exact 95% confidence limits of anaphylaxis after vaccination
for all vaccines combined and for select vaccines with adequate numbers to
allow calculation.14SAS 9.3 software (SAS Institute, Cary, NC) was used for
analysis.
RESULTS
From January 1, 2009 through December 31, 2011, we identified
a total of 17,606,500 vaccination visits at which a total 25,173,965
vaccine doses were administered. Among all visits, 1,117 potential
anaphylaxis cases were identified by using electronic data.We
identified 76 casesof chart-confirmed anaphylaxis(Brighton
Levels1 and 2); 33 anaphylaxiscaseswere associated with
vaccination, and 43 were attributed to other causes.
Characteristics of the 33 cases of postvaccination anaphylaxis
are summarized in Table IV.Five caseswere identified by
screening for epinephrine administration and were not materially
different from other cases. There were no deaths, and only 1 (3%)
patient was hospitalized. There was a female predominance (20
female vs 13 male patients), and the age range was 4 to 65 years
(median,17 years).Children (<18 years) were predominantly
male,but adults were predominantly female.Information on
race was available for 25 (76%) cases: among male patients8
were white and 2 were black, and among female patients, a
were white.The onsetof symptoms among cases was within
30 minutes (8 cases), 30 to less than 120 minutes (8 cases)
less than 4 hours (10 cases), 4 to 8 hours (2 cases), the nex
(1 case), and not documented (4 cases). All cases received
drug therapy, including epinephrine in 15 (45%), antihistam
28 (85%),corticosteroid in 17 (52%),H2-blocker in 7 (21%),
nebulized bronchodilator in 13 (39%),oxygen in 5 (15%),and
intravenous therapy in 5 (15%) cases.Three (9%) cases after
evaluation wereprescribed epinephrineautoinjectors,and 5
(15%) cases were referred to an allergist.
Selected clinical details on the individual cases are presen
Table V. All cases were classified as Brighton Level 1 (12 [36
or Level2 (21 [64%]).Twenty-eight(85%)cases included a
history of atopy.Of the atopic cases,3 included a prior history
of anaphylaxis,and an additional16 included eithera prior
diagnosis ofasthma (n 5 12)or receiptof specific therapy
suggesting an asthma diagnosis (n 5 4); 9 of the 10 nonasth
atopic cases included a history of prior allergies, predomina
food and antibiotics (Table V). Predominant signs and sympt
involved dermatologic and respiratory systems.
Specific vaccine exposures are shown in Table VI; 18 (55%
cases received a single vaccine,and 15 (45%)received 2 or
more vaccinesconcomitantly.The most frequentvaccines
identified included inactivated influenza and tetanus diphth
acellular pertussis vaccines (Tdap/DTaP).
TABLE I. Search algorithm for potential cases of anaphylaxis after vaccination
Adverse event ICD-9 codes
Postvaccination
observation window (d)* Medical setting
First episode in
what period?
Primary screen Anaphylaxis 995.0,999.4 0-2 Outpatient,inpatient, EDFirst in 2 d
E codes E948.0-948.9 E949.0-949.9 0 Outpatient,inpatient, EDFirst in 2 d
Secondary screenAllergic reactions995.1,995.3, 708.0, 708.1, 708.9,695.1,
995.20, 995.21,995.27, 995.29
0 Outpatient,inpatient, EDFirst in 42 d
E codes,External cause of injury codes.
*Day 0 represents day of vaccination.
FIG 1. Search strategy for anaphylaxis cases, 2009-2011.
TABLE II. Brighton Collaboration case definition of
anaphylaxis12
For all levels of diagnostic certainty:
Anaphylaxis is a clinical syndrome characterized by
d sudden onset AND
d rapid progression of signs and symptoms AND
d multiple (>_2) organ systems,as follows:
Level 1 of diagnostic certainty
d >_1 major dermatological AND
d >_1 major cardiovascular AND/OR>_1 major respiratory criterion
Level 2 of diagnostic certainty
d >_1 major cardiovascular AND>_1 major respiratory criterion
OR
d >_1 major cardiovascular OR respiratory criterion AND
d >_1 minor criterion involving>_1 different system (other than
cardiovascular or respiratory systems) OR
d (>_1 major dermatologic) AND (>_1 minor cardiovascular AND/OR
minor respiratory criterion)
Level 3 of diagnostic certainty
d >_1 minor cardiovascular OR respiratory criterion AND
d >_1 minor criterion from each of>_2 different systems/categories
J ALLERGY CLIN IMMUNOL
VOLUME nnn, NUMBER nn
MCNEIL ET AL 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
The rate of postvaccination anaphylaxis for all vaccines was 33
cases per25,173,965 doses or1.31 (95% CI,0.90-1.84)per
million vaccine doses (Table VII).Rates were similar by age,
although the rate was lower in the oldest age group. The rate in
female subjects was slightly higher than in male subjects. Rates
after specific vaccines were difficultto quantify because most
were administered concomitantly with other vaccines. The cases
that followedadministrationof a single vaccineinvolved
predominantly trivalentinfluenza vaccine (TIV),for which the
rate was estimatedto be 1.35 per million vaccinedoses
(Table VIII).The highestrates followed herpes zoster vaccine
(HZV) and rabies vaccine, but these were based on only 2 and 1
case(s),respectively,and had wide CIs (Table VIII).The rate
for postvaccination anaphylaxis for cases thatdid notinvolve
TIV was 19 casesper 14,394,021 dosesor 1.32 (95% CI,
0.79-2.06) per million vaccine doses.
When analyzedbasedon vaccinationvisits ratherthan
vaccination doses,the rate of postvaccination anaphylaxis for
all vaccines was 33 cases per 17,606,500 vaccination visits or 1.87
(95% CI 1.29-2.63)per million vaccination visits.The rate
based on visits was higher than the per-dose rate because more
than 1 vaccine was often administered ata vaccination visit.
The median numberof vaccinesreceived ateach visitwas
2 (range,1-14)among 0-to 17-year-olds,1 (range,1-12)
among 18-to 49-year-olds,and 1 (range,1-12)among those
50 years and older. The rate for postvaccination anaphylaxis for
casesthatdid notinvolve TIV was19 casesper 8,857,787
vaccination visitsor 2.15 (95% CI, 1.29-3.35)per million
vaccination visits.
DISCUSSION
In a large population-based study with extensive case findi
we identified 33 confirmed cases of anaphylaxis after admini
tration of 25,173,965 vaccine doses or 1.31 (95% CI, 0.90-1.8
cases per million vaccine doses. With the largest number of d
and the largest number of cases, inactivated TIV was the ma
contributor to the number of vaccine-triggered anaphylaxis c
in the population,although the rate (1.35 [95% CI,0.65-2.47]
cases per million vaccine doses of TIV given alone) was simil
the rate forall vaccines.Our overallrate ofpostvaccination
anaphylaxiswas slightly higher than the previousstudy
conducted in the VSD by Bohlke et al,11which identified 5 cases
of vaccine-associatedanaphylaxisafter administrationof
7,644,049 vaccine doses or 0.65 (95% CI,0.21-1.53) cases per
million doses.However,that study was limited to children and
adolescentsand lackedoutpatientdata on a majorityof
subjects.11The changes to the recommended childhood and ad
immunization schedules and the introduction of new vaccine
vaccine combinations since the study by Bohlke et al11stimulated
our systematic re-evaluation of postvaccination anaphylaxis
in the VSD. We used the same ICD-9-CM codes for anaphylax
but supplemented oursearch strategy with allergy codesin
conjunction with epinephrine-dispensing codes.In addition, we
used the Brighton criteria,which facilitates comparison of our
results with those of other studies of anaphylaxis.12 Our study
population was considerably larger than the previous VSD st
and data on adults and the OPD setting at all sites were inclu
In recentyears,TIV has become by farthe mostcommonly
administered vaccine in the United States,and we were able to
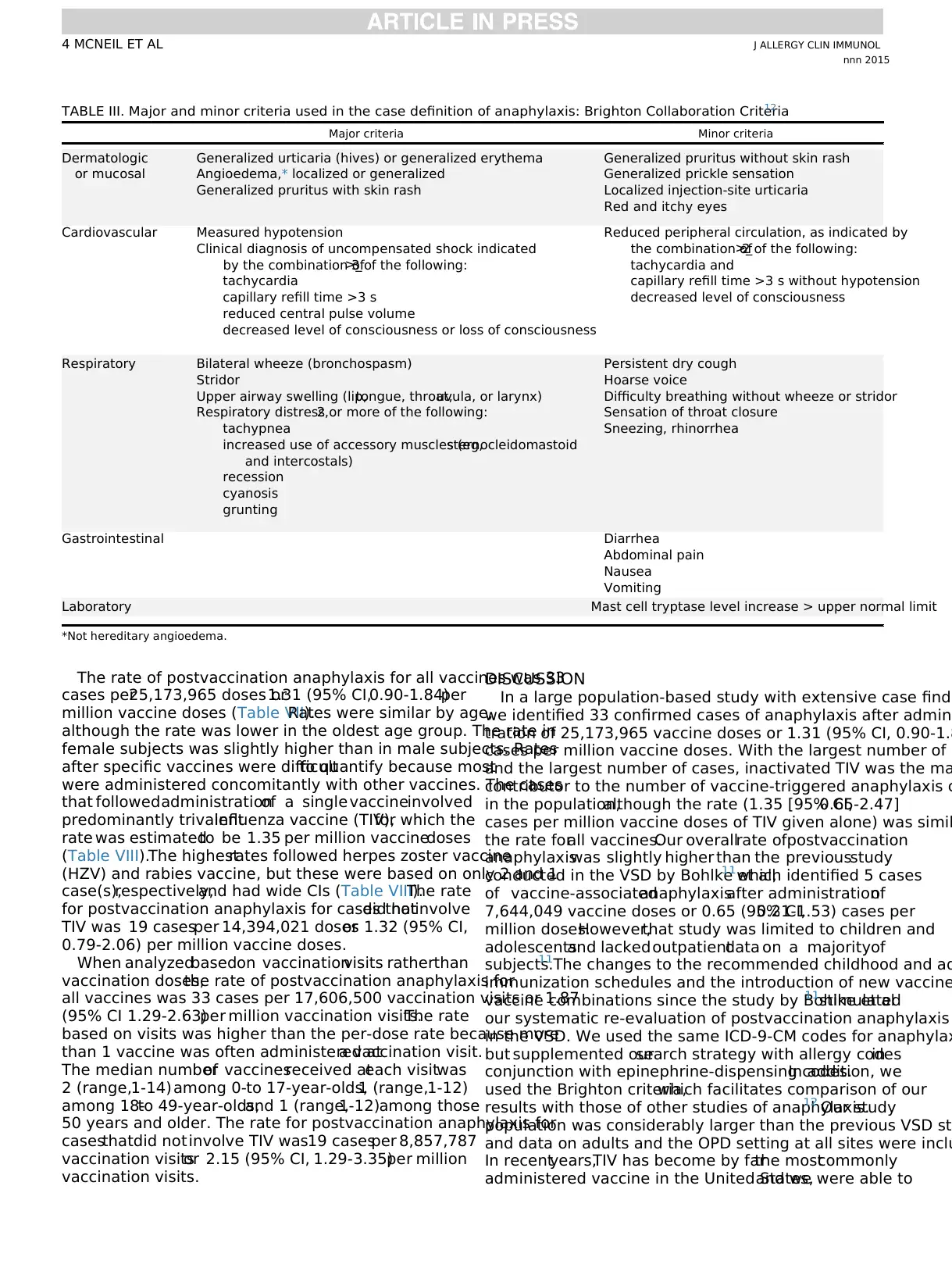
TABLE III. Major and minor criteria used in the case definition of anaphylaxis: Brighton Collaboration Criteria12
Major criteria Minor criteria
Dermatologic
or mucosal
Generalized urticaria (hives) or generalized erythema
Angioedema,* localized or generalized
Generalized pruritus with skin rash
Generalized pruritus without skin rash
Generalized prickle sensation
Localized injection-site urticaria
Red and itchy eyes
Cardiovascular Measured hypotension
Clinical diagnosis of uncompensated shock indicated
by the combination of>_3 of the following:
tachycardia
capillary refill time >3 s
reduced central pulse volume
decreased level of consciousness or loss of consciousness
Reduced peripheral circulation, as indicated by
the combination of>_2 of the following:
tachycardia and
capillary refill time >3 s without hypotension
decreased level of consciousness
Respiratory Bilateral wheeze (bronchospasm)
Stridor
Upper airway swelling (lip,tongue, throat,uvula, or larynx)
Respiratory distress,2 or more of the following:
tachypnea
increased use of accessory muscles (eg,sternocleidomastoid
and intercostals)
recession
cyanosis
grunting
Persistent dry cough
Hoarse voice
Difficulty breathing without wheeze or stridor
Sensation of throat closure
Sneezing, rhinorrhea
Gastrointestinal Diarrhea
Abdominal pain
Nausea
Vomiting
Laboratory Mast cell tryptase level increase > upper normal limit
*Not hereditary angioedema.
J ALLERGY CLIN IMMUNOL
nnn 2015
4 MCNEIL ET AL
cases per25,173,965 doses or1.31 (95% CI,0.90-1.84)per
million vaccine doses (Table VII).Rates were similar by age,
although the rate was lower in the oldest age group. The rate in
female subjects was slightly higher than in male subjects. Rates
after specific vaccines were difficultto quantify because most
were administered concomitantly with other vaccines. The cases
that followedadministrationof a single vaccineinvolved
predominantly trivalentinfluenza vaccine (TIV),for which the
rate was estimatedto be 1.35 per million vaccinedoses
(Table VIII).The highestrates followed herpes zoster vaccine
(HZV) and rabies vaccine, but these were based on only 2 and 1
case(s),respectively,and had wide CIs (Table VIII).The rate
for postvaccination anaphylaxis for cases thatdid notinvolve
TIV was 19 casesper 14,394,021 dosesor 1.32 (95% CI,
0.79-2.06) per million vaccine doses.
When analyzedbasedon vaccinationvisits ratherthan
vaccination doses,the rate of postvaccination anaphylaxis for
all vaccines was 33 cases per 17,606,500 vaccination visits or 1.87
(95% CI 1.29-2.63)per million vaccination visits.The rate
based on visits was higher than the per-dose rate because more
than 1 vaccine was often administered ata vaccination visit.
The median numberof vaccinesreceived ateach visitwas
2 (range,1-14)among 0-to 17-year-olds,1 (range,1-12)
among 18-to 49-year-olds,and 1 (range,1-12)among those
50 years and older. The rate for postvaccination anaphylaxis for
casesthatdid notinvolve TIV was19 casesper 8,857,787
vaccination visitsor 2.15 (95% CI, 1.29-3.35)per million
vaccination visits.
DISCUSSION
In a large population-based study with extensive case findi
we identified 33 confirmed cases of anaphylaxis after admini
tration of 25,173,965 vaccine doses or 1.31 (95% CI, 0.90-1.8
cases per million vaccine doses. With the largest number of d
and the largest number of cases, inactivated TIV was the ma
contributor to the number of vaccine-triggered anaphylaxis c
in the population,although the rate (1.35 [95% CI,0.65-2.47]
cases per million vaccine doses of TIV given alone) was simil
the rate forall vaccines.Our overallrate ofpostvaccination
anaphylaxiswas slightly higher than the previousstudy
conducted in the VSD by Bohlke et al,11which identified 5 cases
of vaccine-associatedanaphylaxisafter administrationof
7,644,049 vaccine doses or 0.65 (95% CI,0.21-1.53) cases per
million doses.However,that study was limited to children and
adolescentsand lackedoutpatientdata on a majorityof
subjects.11The changes to the recommended childhood and ad
immunization schedules and the introduction of new vaccine
vaccine combinations since the study by Bohlke et al11stimulated
our systematic re-evaluation of postvaccination anaphylaxis
in the VSD. We used the same ICD-9-CM codes for anaphylax
but supplemented oursearch strategy with allergy codesin
conjunction with epinephrine-dispensing codes.In addition, we
used the Brighton criteria,which facilitates comparison of our
results with those of other studies of anaphylaxis.12 Our study
population was considerably larger than the previous VSD st
and data on adults and the OPD setting at all sites were inclu
In recentyears,TIV has become by farthe mostcommonly
administered vaccine in the United States,and we were able to
TABLE III. Major and minor criteria used in the case definition of anaphylaxis: Brighton Collaboration Criteria12
Major criteria Minor criteria
Dermatologic
or mucosal
Generalized urticaria (hives) or generalized erythema
Angioedema,* localized or generalized
Generalized pruritus with skin rash
Generalized pruritus without skin rash
Generalized prickle sensation
Localized injection-site urticaria
Red and itchy eyes
Cardiovascular Measured hypotension
Clinical diagnosis of uncompensated shock indicated
by the combination of>_3 of the following:
tachycardia
capillary refill time >3 s
reduced central pulse volume
decreased level of consciousness or loss of consciousness
Reduced peripheral circulation, as indicated by
the combination of>_2 of the following:
tachycardia and
capillary refill time >3 s without hypotension
decreased level of consciousness
Respiratory Bilateral wheeze (bronchospasm)
Stridor
Upper airway swelling (lip,tongue, throat,uvula, or larynx)
Respiratory distress,2 or more of the following:
tachypnea
increased use of accessory muscles (eg,sternocleidomastoid
and intercostals)
recession
cyanosis
grunting
Persistent dry cough
Hoarse voice
Difficulty breathing without wheeze or stridor
Sensation of throat closure
Sneezing, rhinorrhea
Gastrointestinal Diarrhea
Abdominal pain
Nausea
Vomiting
Laboratory Mast cell tryptase level increase > upper normal limit
*Not hereditary angioedema.
J ALLERGY CLIN IMMUNOL
nnn 2015
4 MCNEIL ET AL
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
providethe first estimatesof anaphylaxisrisk after TIV
administration.
Reviews by IOM committees have found that anaphylaxis can
be caused by severalvaccines.7 However,the IOM review
concentrated on childhood and adolescentvaccines,as did the
study by Bohlke et al.11 We identified anaphylaxis cases for all
the vaccines that IOM found to be causally related to anaphylaxis
with the exception ofhepatitisB, which we did not find
administered in association with any anaphylaxis cases. Addition-
ally, primarily because we included both adults and children, we
identified anaphylaxis after several vaccines not included in the
earlierIOM reports (monovalentinfluenzavaccine[MIV],
Tdap,pneumococcalpolysaccharide vaccine [23-valent],HAV,
HZV, and rabiesvaccine).To the extentpossible and using
availableinformation (including from Sanofi Pasteur,Paris,
France),we determined the ovalbumin content of the influenza
vaccines administered in our cases was less than 1 mg/mL for
TIV and less than 5 mg/mL for MIV, respectively.15
Our study is subject to certain potential limitations. Our ab
to estimate rates for individual vaccines,with the exception of
TIV, was limited because of small numbers of anaphylaxis ca
and/or vaccine doses administered or concomitant administ
with othervaccines.We used a broad search strategy that
supplemented specific anaphylaxis codes with allergy codes
conjunction with epinephrine-dispensing codes. Nonetheless
might have missed some cases of anaphylaxis because only
half of the confirmed cases of anaphylaxis had been treated
epinephrine,which could have resultedin missingsome
anaphylaxis cases thatreceived an allergy code butwere not
treated with epinephrine. The strengths of this study include
large population,the use of BrightonCollaborationcase
definition,the broad algorithm used to identify potential case
and the use of chart review to confirm cases.We considered it
importantto use the published Brighton Collaboration case
definition forpostvaccination anaphylaxis forour study.12 In
vaccine safety Brighton Collaboration definitions are genera
accepted as the gold standard surveillance case definitions
postvaccinationadverseevents,includinganaphylaxis.The
Brighton Collaboration case definition ofanaphylaxis is also
used in human vaccine clinical trials.Other clinical algorithms
to identify anaphylaxisregardlessof cause have been
proposed.16,17On review,one third (11/33) of our cases do not
meetthe more specific 2nd NationalInstitute ofAllergy and
InfectiousDisease/FoodAllergy and AnaphylaxisNetwork
Symposium clinical criteria,17 and 7 (64%) of these patients did
not receive epinephrine.
We identified 3 recent reports of postvaccination anaphyla
thatused the Brighton criteria,all from spontaneous reporting
systems. In a 2012 United Kingdom report, investigators ana
data during September 2008 through October 2009 for repo
subjectsless than 16 yearsold through the ‘‘orange card’’
pediatrician surveillance system and found 7 Brighton-valida
cases with patients who recovered withoutsequelae;no cases
followed an estimated 5.5 million doses of infant and presch
primary schedule immunizations, including MMR and influen
vaccines.18 Although denominatorswereunavailablefor all
vaccines,and thus the overallincidence was notcalculated,2
estimated incidence rates were reported (12.0 per 100,000
of single component measles vaccine and 1.4 cases per mill
doses of the bivalentHPV). In an AustralianHPV4
school-based vaccination program in 12- to 18-year-olds, a r
of 2.6 per 100,000 doses was calculated (7 cases and all rec
among 269,680 doses administered).19 Lastly,in a 2009 H1N1
vaccination campaign in Quebec,Canada,a reporting rate of
anaphylaxis of 8 per million distributed doses was reported
2009 AS03-adjuvanted pandemic H1N1 vaccine (Arepanrix;
GlaxoSmithKline,Mississauga,Ontario,Canada).20 A follow-
up study conducted by the vaccine manufacturer of reports
Pandemrix(GlaxoSmithKlineBiologicals S.A., Rixensart,
Belgium) or Arepanrix to the worldwide safety database (62
reports after Arepanrix were from Canada) found no evidenc
the reporting rate was increased compared with rates for ot
vaccines.21 Data from the Vaccine Adverse EventReporting
System in the United States,where only unadjuvanated 2009
H1N1 pandemicinfluenzavaccineswere used, found a
reporting rate of 1.4 per million doses.22
Our finding of no deaths among our cases is consistent wi
above reports.18-20(The death from the Canadian reportabove
did not meet the Brighton case definition for anaphylaxis.20
) In
TABLE IV. Vaccine-triggered anaphylaxis cases: demographic
and clinical characteristics
No. of cases (n 5 33) Percent
Year
2009 11 33
2010 8 24
2011 14 42
Setting
ED 13 39
OPD 20 61
Age group (y)
0-17 18 55
18-49 9 27
>_50 6 18
Sex
Female 20 61
Race
White 24 73
Black 2 6
Unknown 7 21
Past history
Atopy 28 85
Anaphylaxis* 3 9
Time to onset
<30 min 8 24
30 to <120 min 8 24
2 to <4 h 10 30
4 to 20 h 3 10
Not documented 4 12
Treatment of episode
Epinephrine 15 45
Antihistamine 28 85
Corticosteroid 17 52
H2-blocker 7 21
Bronchodilator 13 39
Oxygen 5 15
Intravenous therapy 5 15
Outcome
Recovered 33 100
Follow-up care
Inpatient 1 3
Epinephrine autoinjector prescribed 3 9
Referred to allergist 5 15
*Two patients after TIV and 1 patient after aspirin.
Brighton Level 1 5 6,50%; Brighton Level 2 5 9,43%.
J ALLERGY CLIN IMMUNOL
VOLUME nnn, NUMBER nn
MCNEIL ET AL 5
administration.
Reviews by IOM committees have found that anaphylaxis can
be caused by severalvaccines.7 However,the IOM review
concentrated on childhood and adolescentvaccines,as did the
study by Bohlke et al.11 We identified anaphylaxis cases for all
the vaccines that IOM found to be causally related to anaphylaxis
with the exception ofhepatitisB, which we did not find
administered in association with any anaphylaxis cases. Addition-
ally, primarily because we included both adults and children, we
identified anaphylaxis after several vaccines not included in the
earlierIOM reports (monovalentinfluenzavaccine[MIV],
Tdap,pneumococcalpolysaccharide vaccine [23-valent],HAV,
HZV, and rabiesvaccine).To the extentpossible and using
availableinformation (including from Sanofi Pasteur,Paris,
France),we determined the ovalbumin content of the influenza
vaccines administered in our cases was less than 1 mg/mL for
TIV and less than 5 mg/mL for MIV, respectively.15
Our study is subject to certain potential limitations. Our ab
to estimate rates for individual vaccines,with the exception of
TIV, was limited because of small numbers of anaphylaxis ca
and/or vaccine doses administered or concomitant administ
with othervaccines.We used a broad search strategy that
supplemented specific anaphylaxis codes with allergy codes
conjunction with epinephrine-dispensing codes. Nonetheless
might have missed some cases of anaphylaxis because only
half of the confirmed cases of anaphylaxis had been treated
epinephrine,which could have resultedin missingsome
anaphylaxis cases thatreceived an allergy code butwere not
treated with epinephrine. The strengths of this study include
large population,the use of BrightonCollaborationcase
definition,the broad algorithm used to identify potential case
and the use of chart review to confirm cases.We considered it
importantto use the published Brighton Collaboration case
definition forpostvaccination anaphylaxis forour study.12 In
vaccine safety Brighton Collaboration definitions are genera
accepted as the gold standard surveillance case definitions
postvaccinationadverseevents,includinganaphylaxis.The
Brighton Collaboration case definition ofanaphylaxis is also
used in human vaccine clinical trials.Other clinical algorithms
to identify anaphylaxisregardlessof cause have been
proposed.16,17On review,one third (11/33) of our cases do not
meetthe more specific 2nd NationalInstitute ofAllergy and
InfectiousDisease/FoodAllergy and AnaphylaxisNetwork
Symposium clinical criteria,17 and 7 (64%) of these patients did
not receive epinephrine.
We identified 3 recent reports of postvaccination anaphyla
thatused the Brighton criteria,all from spontaneous reporting
systems. In a 2012 United Kingdom report, investigators ana
data during September 2008 through October 2009 for repo
subjectsless than 16 yearsold through the ‘‘orange card’’
pediatrician surveillance system and found 7 Brighton-valida
cases with patients who recovered withoutsequelae;no cases
followed an estimated 5.5 million doses of infant and presch
primary schedule immunizations, including MMR and influen
vaccines.18 Although denominatorswereunavailablefor all
vaccines,and thus the overallincidence was notcalculated,2
estimated incidence rates were reported (12.0 per 100,000
of single component measles vaccine and 1.4 cases per mill
doses of the bivalentHPV). In an AustralianHPV4
school-based vaccination program in 12- to 18-year-olds, a r
of 2.6 per 100,000 doses was calculated (7 cases and all rec
among 269,680 doses administered).19 Lastly,in a 2009 H1N1
vaccination campaign in Quebec,Canada,a reporting rate of
anaphylaxis of 8 per million distributed doses was reported
2009 AS03-adjuvanted pandemic H1N1 vaccine (Arepanrix;
GlaxoSmithKline,Mississauga,Ontario,Canada).20 A follow-
up study conducted by the vaccine manufacturer of reports
Pandemrix(GlaxoSmithKlineBiologicals S.A., Rixensart,
Belgium) or Arepanrix to the worldwide safety database (62
reports after Arepanrix were from Canada) found no evidenc
the reporting rate was increased compared with rates for ot
vaccines.21 Data from the Vaccine Adverse EventReporting
System in the United States,where only unadjuvanated 2009
H1N1 pandemicinfluenzavaccineswere used, found a
reporting rate of 1.4 per million doses.22
Our finding of no deaths among our cases is consistent wi
above reports.18-20(The death from the Canadian reportabove
did not meet the Brighton case definition for anaphylaxis.20
) In
TABLE IV. Vaccine-triggered anaphylaxis cases: demographic
and clinical characteristics
No. of cases (n 5 33) Percent
Year
2009 11 33
2010 8 24
2011 14 42
Setting
ED 13 39
OPD 20 61
Age group (y)
0-17 18 55
18-49 9 27
>_50 6 18
Sex
Female 20 61
Race
White 24 73
Black 2 6
Unknown 7 21
Past history
Atopy 28 85
Anaphylaxis* 3 9
Time to onset
<30 min 8 24
30 to <120 min 8 24
2 to <4 h 10 30
4 to 20 h 3 10
Not documented 4 12
Treatment of episode
Epinephrine 15 45
Antihistamine 28 85
Corticosteroid 17 52
H2-blocker 7 21
Bronchodilator 13 39
Oxygen 5 15
Intravenous therapy 5 15
Outcome
Recovered 33 100
Follow-up care
Inpatient 1 3
Epinephrine autoinjector prescribed 3 9
Referred to allergist 5 15
*Two patients after TIV and 1 patient after aspirin.
Brighton Level 1 5 6,50%; Brighton Level 2 5 9,43%.
J ALLERGY CLIN IMMUNOL
VOLUME nnn, NUMBER nn
MCNEIL ET AL 5
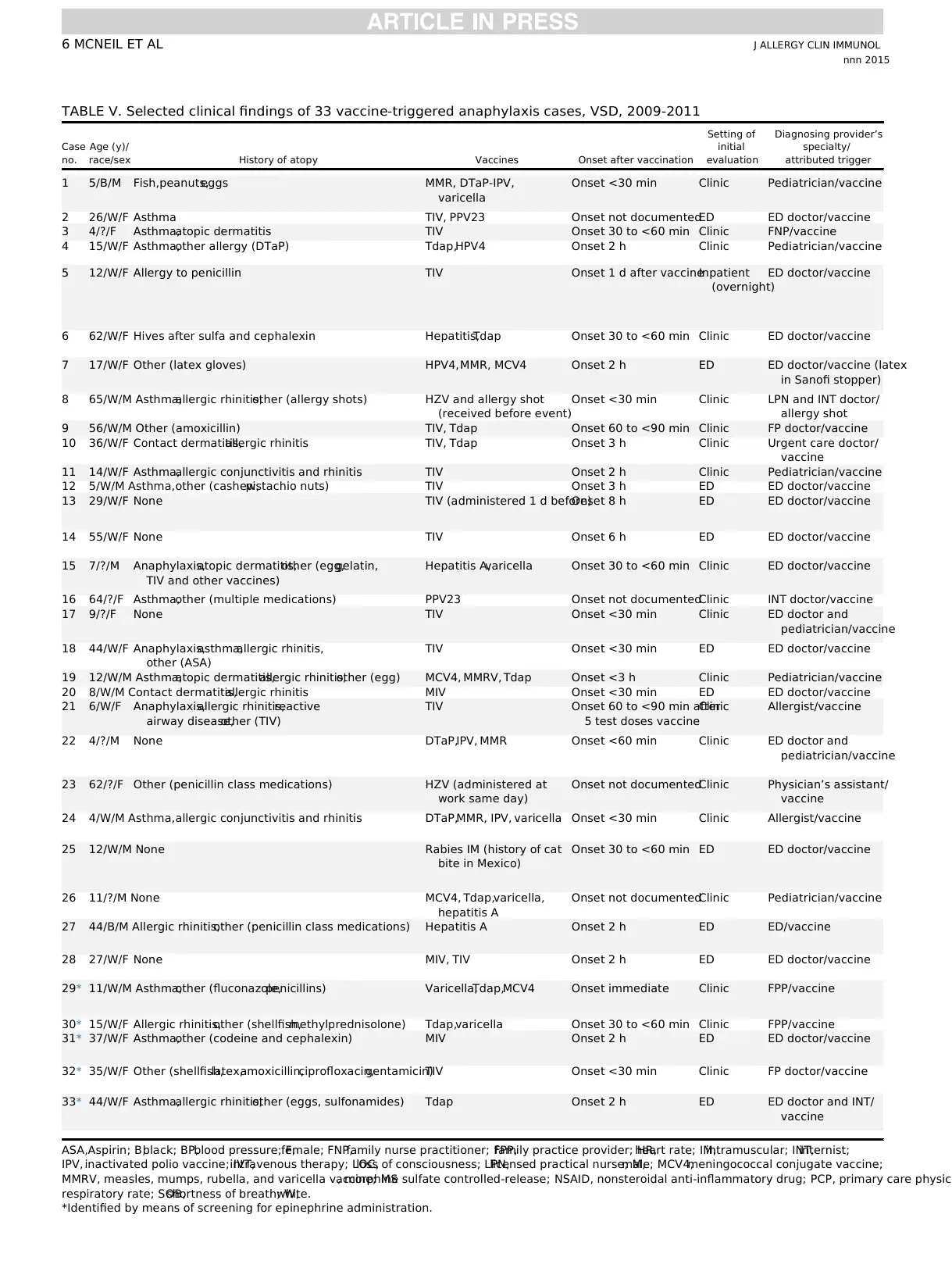
TABLE V. Selected clinical findings of 33 vaccine-triggered anaphylaxis cases, VSD, 2009-2011
Case
no.
Age (y)/
race/sex History of atopy Vaccines Onset after vaccination
Setting of
initial
evaluation
Diagnosing provider’s
specialty/
attributed trigger
1 5/B/M Fish,peanuts,eggs MMR, DTaP-IPV,
varicella
Onset <30 min Clinic Pediatrician/vaccine
2 26/W/F Asthma TIV, PPV23 Onset not documentedED ED doctor/vaccine
3 4/?/F Asthma,atopic dermatitis TIV Onset 30 to <60 min Clinic FNP/vaccine
4 15/W/F Asthma,other allergy (DTaP) Tdap,HPV4 Onset 2 h Clinic Pediatrician/vaccine
5 12/W/F Allergy to penicillin TIV Onset 1 d after vaccineInpatient
(overnight)
ED doctor/vaccine
6 62/W/F Hives after sulfa and cephalexin Hepatitis,Tdap Onset 30 to <60 min Clinic ED doctor/vaccine
7 17/W/F Other (latex gloves) HPV4,MMR, MCV4 Onset 2 h ED ED doctor/vaccine (latex
in Sanofi stopper)
8 65/W/M Asthma,allergic rhinitis,other (allergy shots) HZV and allergy shot
(received before event)
Onset <30 min Clinic LPN and INT doctor/
allergy shot
9 56/W/M Other (amoxicillin) TIV, Tdap Onset 60 to <90 min Clinic FP doctor/vaccine
10 36/W/F Contact dermatitis,allergic rhinitis TIV, Tdap Onset 3 h Clinic Urgent care doctor/
vaccine
11 14/W/F Asthma,allergic conjunctivitis and rhinitis TIV Onset 2 h Clinic Pediatrician/vaccine
12 5/W/M Asthma,other (cashew,pistachio nuts) TIV Onset 3 h ED ED doctor/vaccine
13 29/W/F None TIV (administered 1 d before)Onset 8 h ED ED doctor/vaccine
14 55/W/F None TIV Onset 6 h ED ED doctor/vaccine
15 7/?/M Anaphylaxis,atopic dermatitis,other (egg,gelatin,
TIV and other vaccines)
Hepatitis A,varicella Onset 30 to <60 min Clinic ED doctor/vaccine
16 64/?/F Asthma,other (multiple medications) PPV23 Onset not documentedClinic INT doctor/vaccine
17 9/?/F None TIV Onset <30 min Clinic ED doctor and
pediatrician/vaccine
18 44/W/F Anaphylaxis,asthma,allergic rhinitis,
other (ASA)
TIV Onset <30 min ED ED doctor/vaccine
19 12/W/M Asthma,atopic dermatitis,allergic rhinitis,other (egg) MCV4, MMRV, Tdap Onset <3 h Clinic Pediatrician/vaccine
20 8/W/M Contact dermatitis,allergic rhinitis MIV Onset <30 min ED ED doctor/vaccine
21 6/W/F Anaphylaxis,allergic rhinitis,reactive
airway disease,other (TIV)
TIV Onset 60 to <90 min after
5 test doses vaccine
Clinic Allergist/vaccine
22 4/?/M None DTaP,IPV, MMR Onset <60 min Clinic ED doctor and
pediatrician/vaccine
23 62/?/F Other (penicillin class medications) HZV (administered at
work same day)
Onset not documentedClinic Physician’s assistant/
vaccine
24 4/W/M Asthma,allergic conjunctivitis and rhinitis DTaP,MMR, IPV, varicella Onset <30 min Clinic Allergist/vaccine
25 12/W/M None Rabies IM (history of cat
bite in Mexico)
Onset 30 to <60 min ED ED doctor/vaccine
26 11/?/M None MCV4, Tdap,varicella,
hepatitis A
Onset not documentedClinic Pediatrician/vaccine
27 44/B/M Allergic rhinitis,other (penicillin class medications) Hepatitis A Onset 2 h ED ED/vaccine
28 27/W/F None MIV, TIV Onset 2 h ED ED doctor/vaccine
29* 11/W/M Asthma,other (fluconazole,penicillins) Varicella,Tdap,MCV4 Onset immediate Clinic FPP/vaccine
30* 15/W/F Allergic rhinitis,other (shellfish,methylprednisolone) Tdap,varicella Onset 30 to <60 min Clinic FPP/vaccine
31* 37/W/F Asthma,other (codeine and cephalexin) MIV Onset 2 h ED ED doctor/vaccine
32* 35/W/F Other (shellfish,latex,amoxicillin,ciprofloxacin,gentamicin)TIV Onset <30 min Clinic FP doctor/vaccine
33* 44/W/F Asthma,allergic rhinitis,other (eggs, sulfonamides) Tdap Onset 2 h ED ED doctor and INT/
vaccine
ASA,Aspirin; B,black; BP,blood pressure; F,female; FNP,family nurse practitioner; FPP,family practice provider; HR,heart rate; IM,intramuscular; INT,internist;
IPV, inactivated polio vaccine; IVT,intravenous therapy; LOC,loss of consciousness; LPN,licensed practical nurse; M,male; MCV4,meningococcal conjugate vaccine;
MMRV, measles, mumps, rubella, and varicella vaccine; MS, morphine sulfate controlled-release; NSAID, nonsteroidal anti-inflammatory drug; PCP, primary care physici
respiratory rate; SOB,shortness of breath; W,white.
*Identified by means of screening for epinephrine administration.
J ALLERGY CLIN IMMUNOL
nnn 2015
6 MCNEIL ET AL
Case
no.
Age (y)/
race/sex History of atopy Vaccines Onset after vaccination
Setting of
initial
evaluation
Diagnosing provider’s
specialty/
attributed trigger
1 5/B/M Fish,peanuts,eggs MMR, DTaP-IPV,
varicella
Onset <30 min Clinic Pediatrician/vaccine
2 26/W/F Asthma TIV, PPV23 Onset not documentedED ED doctor/vaccine
3 4/?/F Asthma,atopic dermatitis TIV Onset 30 to <60 min Clinic FNP/vaccine
4 15/W/F Asthma,other allergy (DTaP) Tdap,HPV4 Onset 2 h Clinic Pediatrician/vaccine
5 12/W/F Allergy to penicillin TIV Onset 1 d after vaccineInpatient
(overnight)
ED doctor/vaccine
6 62/W/F Hives after sulfa and cephalexin Hepatitis,Tdap Onset 30 to <60 min Clinic ED doctor/vaccine
7 17/W/F Other (latex gloves) HPV4,MMR, MCV4 Onset 2 h ED ED doctor/vaccine (latex
in Sanofi stopper)
8 65/W/M Asthma,allergic rhinitis,other (allergy shots) HZV and allergy shot
(received before event)
Onset <30 min Clinic LPN and INT doctor/
allergy shot
9 56/W/M Other (amoxicillin) TIV, Tdap Onset 60 to <90 min Clinic FP doctor/vaccine
10 36/W/F Contact dermatitis,allergic rhinitis TIV, Tdap Onset 3 h Clinic Urgent care doctor/
vaccine
11 14/W/F Asthma,allergic conjunctivitis and rhinitis TIV Onset 2 h Clinic Pediatrician/vaccine
12 5/W/M Asthma,other (cashew,pistachio nuts) TIV Onset 3 h ED ED doctor/vaccine
13 29/W/F None TIV (administered 1 d before)Onset 8 h ED ED doctor/vaccine
14 55/W/F None TIV Onset 6 h ED ED doctor/vaccine
15 7/?/M Anaphylaxis,atopic dermatitis,other (egg,gelatin,
TIV and other vaccines)
Hepatitis A,varicella Onset 30 to <60 min Clinic ED doctor/vaccine
16 64/?/F Asthma,other (multiple medications) PPV23 Onset not documentedClinic INT doctor/vaccine
17 9/?/F None TIV Onset <30 min Clinic ED doctor and
pediatrician/vaccine
18 44/W/F Anaphylaxis,asthma,allergic rhinitis,
other (ASA)
TIV Onset <30 min ED ED doctor/vaccine
19 12/W/M Asthma,atopic dermatitis,allergic rhinitis,other (egg) MCV4, MMRV, Tdap Onset <3 h Clinic Pediatrician/vaccine
20 8/W/M Contact dermatitis,allergic rhinitis MIV Onset <30 min ED ED doctor/vaccine
21 6/W/F Anaphylaxis,allergic rhinitis,reactive
airway disease,other (TIV)
TIV Onset 60 to <90 min after
5 test doses vaccine
Clinic Allergist/vaccine
22 4/?/M None DTaP,IPV, MMR Onset <60 min Clinic ED doctor and
pediatrician/vaccine
23 62/?/F Other (penicillin class medications) HZV (administered at
work same day)
Onset not documentedClinic Physician’s assistant/
vaccine
24 4/W/M Asthma,allergic conjunctivitis and rhinitis DTaP,MMR, IPV, varicella Onset <30 min Clinic Allergist/vaccine
25 12/W/M None Rabies IM (history of cat
bite in Mexico)
Onset 30 to <60 min ED ED doctor/vaccine
26 11/?/M None MCV4, Tdap,varicella,
hepatitis A
Onset not documentedClinic Pediatrician/vaccine
27 44/B/M Allergic rhinitis,other (penicillin class medications) Hepatitis A Onset 2 h ED ED/vaccine
28 27/W/F None MIV, TIV Onset 2 h ED ED doctor/vaccine
29* 11/W/M Asthma,other (fluconazole,penicillins) Varicella,Tdap,MCV4 Onset immediate Clinic FPP/vaccine
30* 15/W/F Allergic rhinitis,other (shellfish,methylprednisolone) Tdap,varicella Onset 30 to <60 min Clinic FPP/vaccine
31* 37/W/F Asthma,other (codeine and cephalexin) MIV Onset 2 h ED ED doctor/vaccine
32* 35/W/F Other (shellfish,latex,amoxicillin,ciprofloxacin,gentamicin)TIV Onset <30 min Clinic FP doctor/vaccine
33* 44/W/F Asthma,allergic rhinitis,other (eggs, sulfonamides) Tdap Onset 2 h ED ED doctor and INT/
vaccine
ASA,Aspirin; B,black; BP,blood pressure; F,female; FNP,family nurse practitioner; FPP,family practice provider; HR,heart rate; IM,intramuscular; INT,internist;
IPV, inactivated polio vaccine; IVT,intravenous therapy; LOC,loss of consciousness; LPN,licensed practical nurse; M,male; MCV4,meningococcal conjugate vaccine;
MMRV, measles, mumps, rubella, and varicella vaccine; MS, morphine sulfate controlled-release; NSAID, nonsteroidal anti-inflammatory drug; PCP, primary care physici
respiratory rate; SOB,shortness of breath; W,white.
*Identified by means of screening for epinephrine administration.
J ALLERGY CLIN IMMUNOL
nnn 2015
6 MCNEIL ET AL
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Symptoms
Brighton
level Treatment Outcome
General pruritus,wheeze,cough,vomiting 2 Epinephrine,oral antihistamine,antiemetic Patient recovered
Wheeze (bilateral),SOB, [HR, nasal congestion,nausea 2 Nebulizer Patient recovered
Generalized urticaria,wheeze,respiratory distress,vomiting 1 Epinephrine,oral antihistamine,O2, albuterol nebulizerPatient recovered
Angioedema,generalized urticaria,erythema
and pruritus,SOB, abdominal pain
2 Oral antihistamine,bronchodilators Patient recovered
Generalized urticaria,pruritus and rash,[HR, syncope,
BP 117/72 mm Hg,‘‘lump in throat’’
2 Epinephrine,parenteral antihistamine,parenteral
H2-blocker,oral steroid,O2, other (antiemetic,
lidocaine cream)
Patient recovered,referred to allergist
(patient’s skin test and RAST results
both negative for latex),prescribed
epinephrine autoinjector
Flushing,SOB, nausea,vomiting,abdominal pain 2 Parenteral antihistamine,parenteral H2-blocker,
parenteral steroid,O2, other (ASA,nitroglycerin,MS)
Patient recovered
Generalized ‘‘prickle’’ sensation,dizziness,
[HR, wheeze,throat closure,dry cough
2 Epinephrine,oral antihistamine,oral steroid Patient recovered,referred to allergist,
prescribed epinephrine autoinjector
Generalized pruritus,wheeze,SOB, cough 2 Epinephrine,parenteral antihistamine,albuterol
nebulizer
Patient recovered
Angioedema,SOB, vomiting,fatigue 2 Oral antihistamine Patient recovered
Angioedema,‘‘choking’’ cough,[HR, nausea 2 Oral antihistamine,oral steroid,other (cool compress) Patient recovered
Wheeze,vomiting 2 Oral antihistamine,bronchodilators Patient recovered
Generalized urticaria,pruritus and rash,SOB 2 Oral antihistamine,oral steroid Patient recovered
Angioedema,swelling (lips,uvula,mouth),generalized
urticaria,pruritus and rash,SOB, cough
1 Oral antihistamine,oral H2-blocker,oral steroid Patient recovered,referred to PCP
Wheeze,SOB, red and itchy eyes 2 Oral antihistamine,oral steroid,bronchodilators,
other (fluids and rest)
Patient recovered,referred to PCP
Angioedema,swelling (lips),throat closure,red itchy
eyes,cough,erythema and rash,vomiting
1 Epinephrine,oral antihistamine,oral H2-blocker,
parenteral steroid,IVT, bronchodilator
Patient recovered,referred to allergist
Wheeze (bilateral),dizziness,nausea 2 Bronchodilators Patient recovered
Angioedema (eyelid),cough 2 Epinephrine,oral antihistamine,oral steroid,
bronchodilators,other (icepack)
Patient recovered,referred to
pediatrician
Generalized pruritus and rash,wheeze,SOB, throat
tightening,hoarse voice,cough,vomiting and diarrhea
2 Parenteral antihistamine,oral steroid,O2, bronchodilatorsPatient recovered
Generalized urticaria,pruritus and rash,cough 2 Oral antihistamine,other (cool compress) Patient recovered
Angioedema (periorbital),wheeze,SOB 1 Oral antihistamine,oral steroid,bronchodilators Patient recovered
Erythema (throat),generalized pruritus and rash,cough 2 Epinephrine,oral antihistamine Patient recovered
Angioedema,generalized urticaria,erythema,rash,red
itchy eyes,wheeze,[RR, cough
1 Oral antihistamine,parenteral steroids Patient recovered,referred to allergist
and pediatrician,prescribed
epinephrine autoinjector
Generalized pruritus,erythema,tongue swelling,chest tightness 1 Parenteral antihistamine,oral H2-blocker Patient recovered
Facial swelling,erythema and pruritus,wheeze (bilateral),
swelling (posterior oropharynx),rhinorrhea,cough,vomiting
1 Epinephrine,bronchodilators Patient recovered,referred to allergist
Angioedema (eyelids,lips),generalized rash,facial erythema
and urticaria,wheeze,swelling (lips,throat)
1 Epinephrine,parenteral antihistamine,parenteral
H2-blocker,parenteral steroid,O2, other
(continued antibiotic)
Patient recovered,referred to
pediatrician
Injection site urticaria & erythema,measured YBP 2 Oral antihistamine Patient recovered
Generalized pruritus and rash,swelling (throat),chest pain,
vomiting,disorientation
1 Oral and parenteral antihistamine,parenteral steroid,
IVT, NSAIDs (ketorolac,ibuprofen)
Patient recovered
Generalized erythema and rash,red itchy eyes,[HR,
palpitations,swelling (throat),‘‘chest heaviness’’
1 Oral antihistamine,acetaminophen Patient recovered,referred to PCP
Generalized urticaria,pruritus and rash,angioedema,
swelling (tonsils)
1 Epinephrine,parenteral steroid Patient recovered
Angioedema (lips),swelling (tongue) 2 Epinephrine,oral antihistamine,oral steroid Patient recovered
Generalized ‘‘prickle’’ sensation,SOB,swelling (throat),
‘‘tingling’’ lips
2 Epinephrine,parenteral antihistamine,other (lorazepam)Patient recovered,referred to PCP
Generalized pruritus,swelling (tongue),SOB, throat closure 2 Epinephrine,parenteral antihistamine,IVT,
bronchodilator (albuterol)
Patient recovered
Generalized urticaria,erythema and rash,measured YBP,
LOC, nausea,diaphoretic
1 Epinephrine,oral antihistamine,parenteral H2-blocker,
parenteral steroid,IVT, bronchodilators
Patient recovered,referred to PCP
TABLE V. (Continued)
J ALLERGY CLIN IMMUNOL
VOLUME nnn, NUMBER nn
MCNEIL ET AL 7
Brighton
level Treatment Outcome
General pruritus,wheeze,cough,vomiting 2 Epinephrine,oral antihistamine,antiemetic Patient recovered
Wheeze (bilateral),SOB, [HR, nasal congestion,nausea 2 Nebulizer Patient recovered
Generalized urticaria,wheeze,respiratory distress,vomiting 1 Epinephrine,oral antihistamine,O2, albuterol nebulizerPatient recovered
Angioedema,generalized urticaria,erythema
and pruritus,SOB, abdominal pain
2 Oral antihistamine,bronchodilators Patient recovered
Generalized urticaria,pruritus and rash,[HR, syncope,
BP 117/72 mm Hg,‘‘lump in throat’’
2 Epinephrine,parenteral antihistamine,parenteral
H2-blocker,oral steroid,O2, other (antiemetic,
lidocaine cream)
Patient recovered,referred to allergist
(patient’s skin test and RAST results
both negative for latex),prescribed
epinephrine autoinjector
Flushing,SOB, nausea,vomiting,abdominal pain 2 Parenteral antihistamine,parenteral H2-blocker,
parenteral steroid,O2, other (ASA,nitroglycerin,MS)
Patient recovered
Generalized ‘‘prickle’’ sensation,dizziness,
[HR, wheeze,throat closure,dry cough
2 Epinephrine,oral antihistamine,oral steroid Patient recovered,referred to allergist,
prescribed epinephrine autoinjector
Generalized pruritus,wheeze,SOB, cough 2 Epinephrine,parenteral antihistamine,albuterol
nebulizer
Patient recovered
Angioedema,SOB, vomiting,fatigue 2 Oral antihistamine Patient recovered
Angioedema,‘‘choking’’ cough,[HR, nausea 2 Oral antihistamine,oral steroid,other (cool compress) Patient recovered
Wheeze,vomiting 2 Oral antihistamine,bronchodilators Patient recovered
Generalized urticaria,pruritus and rash,SOB 2 Oral antihistamine,oral steroid Patient recovered
Angioedema,swelling (lips,uvula,mouth),generalized
urticaria,pruritus and rash,SOB, cough
1 Oral antihistamine,oral H2-blocker,oral steroid Patient recovered,referred to PCP
Wheeze,SOB, red and itchy eyes 2 Oral antihistamine,oral steroid,bronchodilators,
other (fluids and rest)
Patient recovered,referred to PCP
Angioedema,swelling (lips),throat closure,red itchy
eyes,cough,erythema and rash,vomiting
1 Epinephrine,oral antihistamine,oral H2-blocker,
parenteral steroid,IVT, bronchodilator
Patient recovered,referred to allergist
Wheeze (bilateral),dizziness,nausea 2 Bronchodilators Patient recovered
Angioedema (eyelid),cough 2 Epinephrine,oral antihistamine,oral steroid,
bronchodilators,other (icepack)
Patient recovered,referred to
pediatrician
Generalized pruritus and rash,wheeze,SOB, throat
tightening,hoarse voice,cough,vomiting and diarrhea
2 Parenteral antihistamine,oral steroid,O2, bronchodilatorsPatient recovered
Generalized urticaria,pruritus and rash,cough 2 Oral antihistamine,other (cool compress) Patient recovered
Angioedema (periorbital),wheeze,SOB 1 Oral antihistamine,oral steroid,bronchodilators Patient recovered
Erythema (throat),generalized pruritus and rash,cough 2 Epinephrine,oral antihistamine Patient recovered
Angioedema,generalized urticaria,erythema,rash,red
itchy eyes,wheeze,[RR, cough
1 Oral antihistamine,parenteral steroids Patient recovered,referred to allergist
and pediatrician,prescribed
epinephrine autoinjector
Generalized pruritus,erythema,tongue swelling,chest tightness 1 Parenteral antihistamine,oral H2-blocker Patient recovered
Facial swelling,erythema and pruritus,wheeze (bilateral),
swelling (posterior oropharynx),rhinorrhea,cough,vomiting
1 Epinephrine,bronchodilators Patient recovered,referred to allergist
Angioedema (eyelids,lips),generalized rash,facial erythema
and urticaria,wheeze,swelling (lips,throat)
1 Epinephrine,parenteral antihistamine,parenteral
H2-blocker,parenteral steroid,O2, other
(continued antibiotic)
Patient recovered,referred to
pediatrician
Injection site urticaria & erythema,measured YBP 2 Oral antihistamine Patient recovered
Generalized pruritus and rash,swelling (throat),chest pain,
vomiting,disorientation
1 Oral and parenteral antihistamine,parenteral steroid,
IVT, NSAIDs (ketorolac,ibuprofen)
Patient recovered
Generalized erythema and rash,red itchy eyes,[HR,
palpitations,swelling (throat),‘‘chest heaviness’’
1 Oral antihistamine,acetaminophen Patient recovered,referred to PCP
Generalized urticaria,pruritus and rash,angioedema,
swelling (tonsils)
1 Epinephrine,parenteral steroid Patient recovered
Angioedema (lips),swelling (tongue) 2 Epinephrine,oral antihistamine,oral steroid Patient recovered
Generalized ‘‘prickle’’ sensation,SOB,swelling (throat),
‘‘tingling’’ lips
2 Epinephrine,parenteral antihistamine,other (lorazepam)Patient recovered,referred to PCP
Generalized pruritus,swelling (tongue),SOB, throat closure 2 Epinephrine,parenteral antihistamine,IVT,
bronchodilator (albuterol)
Patient recovered
Generalized urticaria,erythema and rash,measured YBP,
LOC, nausea,diaphoretic
1 Epinephrine,oral antihistamine,parenteral H2-blocker,
parenteral steroid,IVT, bronchodilators
Patient recovered,referred to PCP
TABLE V. (Continued)
J ALLERGY CLIN IMMUNOL
VOLUME nnn, NUMBER nn
MCNEIL ET AL 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

a review of reports after TIV in adults to the US Vaccine Adverse
Event Reporting System from 1990-2005, of 371 deaths, 4 were
reported as anaphylaxis; during this period,an estimated 747.1
million doses of TIV were administered.23 In addition, a recent
review offatal anaphylaxiscasesduring 1999-2010,which
used the National Center for Health Statistics Multiple Cause of
Death Database,found 1446 (58%) 2458 anaphylaxis-
related deathswereattributableto medications.24 However,
most(74%)drug-induced anaphylaxis-related deathshad no
identified culprit drug.Among the 368 in which the implicated
medication was specified, in only 10 (3%) was this categorized
as ‘‘serum’’;postvaccinationanaphylaxisdeathswere not
identified separately.24
Contrary to Bohlke et al,11who found patients in 4 of 5 cases
were aged less than 2 years,we identified no cases in children
less than 4 years old, and the median age of the patients in our
cases was 17 years (range, 4-65 years). Of the total 1117 charts
reviewed,380 wereidentified provisionally asanaphylaxis,
possible anaphylaxis,or allergy,and 135 (36%) of these cases
were among children 5 years or younger. Only 2 were validated
anaphylaxiscases(both Brighton Level2), and neitherwas
attributed to vaccine.A 1-year-old healthyfemalesubject
48 hours after receipt of DTaP and HAV vaccines had anaphylaxis
3 hoursafterreceiving amoxicillin foran earinfection and
recovered afterparenteralantihistamine.A 1-year-old male
subjectwith a history ofchronic urticaria had anaphylaxis
24 hours after receipt of DTaP, TIV, MMR, and varicella vaccines
and recovered afterepinephrine,antihistamine,and oraland
topicalcorticosteroids;however,anaphylaxis was attributed to
milk allergy and on follow-up by an allergist,he was found to
have positive skin testresults for eggs,peanuts,and almonds.
Our finding of no validated postvaccination anaphylaxis cases
among children less than 2 years old is consistent with the re
United Kingdom experience,which reported no anaphylaxis
eventsafter routineinfant and preschoolimmunizations.18
Factors potentially contributing to the lack of infants and tod
among our cases might include difficulty making a diagnosis
anaphylaxis and/or applying Brighton criteria in these age gr
Sargant et al25suggested the tendency for anaphylaxis in childr
to presentmostfrequently with respiratory features has raised
concern about the potential for diagnostic confusion with acu
asthma,and consideration of the diagnosis is recommended in
all children presenting with severe asthma.
Our study identified a female predominance among adults
Bohlke et al11 and Erlewyn-Lajeunesse et al18studies had small
case numbers and did not report cases’ sex,and the Brotherton
et al19 report was an HPV4 vaccination campaign that targete
female subjects only. However, the Rouleau et al20 safety study
of 2009 pandemic H1N1 influenza vaccine found after adjust
for doses administered thatfemale subjects were represented
3.9-fold more often than male subjects among their anaphyla
reports,and among reportsincluded in Tavareset al,21 the
proportion of anaphylaxis cases,which metBrighton Levels 1
to 3 was higher in female compared with male subjects (84%
16%).In these 2 reports the rates were highestin women of
childbearing age,and although the effectof a greaterfemale
tendency to reportcould notbe ruled outin these passive
surveillance studies,a biologic basisfor the difference was
hypothesized.20,21Importantly,in our population-based study
female preponderance was seen only in adults and not in chi
Fourteen (70%) of 20 female subjects were of childbearing a
(ie,aged 10-50 years).In general,anaphylaxis and immediate
hypersensitivity, particularly drug allergy, occur more freque
in women of childbearing age.26-32Sex-specific differences in
innate, humoral, and cell-mediated immune responses to vac
tion have also been reported.33-35In addition, sex differences in
adverse events (fever, pain, and inflammation) after immuni
have been noted for several vaccines, including influenza36,37
and
MMR 38,39vaccines.Although precise biologicalmechanisms
underlying sex-specificresponsesto vaccinesare unknown,
genetic and hormonalfactors are considered important.33 Sex
hormones have been shown to modulate immune responses40,41
and Hox et al42 recently found that sex-specific differences in a
mouse modelof anaphylaxis were due to the female steroid
estradiol.
The finding that 28 (85%) cases had pre-existing atopic dis
(3 with prior anaphylaxis,16 with asthma,and 9 with specific
priorallergies)is consistentwith earlierreports emphasizing
coexisting atopic disease,particularly asthma,as being clinical
risk factorsfor anaphylaxis.29,30,43Although epinephrineis
recommended as the drug ofchoice foranaphylaxis,3,44 this
therapy, as documented in the medical records, was adminis
in only 15 (45%) of our cases compared with antihistamines
(85%) cases and corticosteroids in 17 (52%) cases. Only 3 (9
caseswere documented to have been prescribed epinephrine
autoinjectors, and only 5 (15%) were known to have been re
to an allergist/allergy clinicfor follow-up.The 2010 Joint
AmericanAcademyof Allergy, Asthma& Immunology/
American College ofAllergy,Asthma & Immunology/Joint
Councilof Allergy,Asthma & Immunology Task Force on
Practice Parameters for the management of anaphylaxis clea
state thatif initialassessmentsupports potentialanaphylaxis,
the immediate intervention isto assessthe patient’sairway,
TABLE VI. Vaccination-triggered anaphylaxis cases by vaccine
exposures (n 5 33)
Vaccine Alone
With
other
vaccines Other concomitant vaccine(s)*
TIV 10 4 MIV, Tdap (2),PPSV23
MIV 2 1 TIV
Tdap 1 8 TIV (2), HPV4,HAV,VAR, MCV41MMRV,
MCV41VAR, MCV41VAR1HAV
PPSV23 1 1 TIV
HAV 1 3 Tdap,Tdap1MCV41VAR,VAR
HZV 2 0 —
Rabies 1 0 —
HPV4 — 2 Tdap,MMR1MCV4
MMR — 3 DTaP-IPV1VAR,DTaP1IPV1VAR, HPV41
MCV4
MMRV — 2 Tdap1MCV4, DTaP1IPV
MCV4 — 4 Tdap1MMRV,Tdap1VAR,Tdap1VAR1
HAV,HPV41MMR
VAR — 5 Tdap,Tdap1MCV41HAV,DTaP-IPV1
MMR, HAV,Tdap1MCV4
DTaP-IPV — 1 MMR1VAR
DTaP — 2 MMRV1IPV, MMR1IPV1VAR
IPV — 2 DTaP1MMRV,DTaP1MMR1VAR
IPV, Inactivated polio vaccine; MCV4,meningococcal conjugate vaccine;
MMRV,measles,mumps,rubella,and varicella vaccine; PPSV23,pneumococcal
polysaccharide vaccine (23-valent); VAR,varicella vaccine.
*A total of 15 (45%) cases received 2 or more concomitant vaccines.
J ALLERGY CLIN IMMUNOL
nnn 2015
8 MCNEIL ET AL
Event Reporting System from 1990-2005, of 371 deaths, 4 were
reported as anaphylaxis; during this period,an estimated 747.1
million doses of TIV were administered.23 In addition, a recent
review offatal anaphylaxiscasesduring 1999-2010,which
used the National Center for Health Statistics Multiple Cause of
Death Database,found 1446 (58%) 2458 anaphylaxis-
related deathswereattributableto medications.24 However,
most(74%)drug-induced anaphylaxis-related deathshad no
identified culprit drug.Among the 368 in which the implicated
medication was specified, in only 10 (3%) was this categorized
as ‘‘serum’’;postvaccinationanaphylaxisdeathswere not
identified separately.24
Contrary to Bohlke et al,11who found patients in 4 of 5 cases
were aged less than 2 years,we identified no cases in children
less than 4 years old, and the median age of the patients in our
cases was 17 years (range, 4-65 years). Of the total 1117 charts
reviewed,380 wereidentified provisionally asanaphylaxis,
possible anaphylaxis,or allergy,and 135 (36%) of these cases
were among children 5 years or younger. Only 2 were validated
anaphylaxiscases(both Brighton Level2), and neitherwas
attributed to vaccine.A 1-year-old healthyfemalesubject
48 hours after receipt of DTaP and HAV vaccines had anaphylaxis
3 hoursafterreceiving amoxicillin foran earinfection and
recovered afterparenteralantihistamine.A 1-year-old male
subjectwith a history ofchronic urticaria had anaphylaxis
24 hours after receipt of DTaP, TIV, MMR, and varicella vaccines
and recovered afterepinephrine,antihistamine,and oraland
topicalcorticosteroids;however,anaphylaxis was attributed to
milk allergy and on follow-up by an allergist,he was found to
have positive skin testresults for eggs,peanuts,and almonds.
Our finding of no validated postvaccination anaphylaxis cases
among children less than 2 years old is consistent with the re
United Kingdom experience,which reported no anaphylaxis
eventsafter routineinfant and preschoolimmunizations.18
Factors potentially contributing to the lack of infants and tod
among our cases might include difficulty making a diagnosis
anaphylaxis and/or applying Brighton criteria in these age gr
Sargant et al25suggested the tendency for anaphylaxis in childr
to presentmostfrequently with respiratory features has raised
concern about the potential for diagnostic confusion with acu
asthma,and consideration of the diagnosis is recommended in
all children presenting with severe asthma.
Our study identified a female predominance among adults
Bohlke et al11 and Erlewyn-Lajeunesse et al18studies had small
case numbers and did not report cases’ sex,and the Brotherton
et al19 report was an HPV4 vaccination campaign that targete
female subjects only. However, the Rouleau et al20 safety study
of 2009 pandemic H1N1 influenza vaccine found after adjust
for doses administered thatfemale subjects were represented
3.9-fold more often than male subjects among their anaphyla
reports,and among reportsincluded in Tavareset al,21 the
proportion of anaphylaxis cases,which metBrighton Levels 1
to 3 was higher in female compared with male subjects (84%
16%).In these 2 reports the rates were highestin women of
childbearing age,and although the effectof a greaterfemale
tendency to reportcould notbe ruled outin these passive
surveillance studies,a biologic basisfor the difference was
hypothesized.20,21Importantly,in our population-based study
female preponderance was seen only in adults and not in chi
Fourteen (70%) of 20 female subjects were of childbearing a
(ie,aged 10-50 years).In general,anaphylaxis and immediate
hypersensitivity, particularly drug allergy, occur more freque
in women of childbearing age.26-32Sex-specific differences in
innate, humoral, and cell-mediated immune responses to vac
tion have also been reported.33-35In addition, sex differences in
adverse events (fever, pain, and inflammation) after immuni
have been noted for several vaccines, including influenza36,37
and
MMR 38,39vaccines.Although precise biologicalmechanisms
underlying sex-specificresponsesto vaccinesare unknown,
genetic and hormonalfactors are considered important.33 Sex
hormones have been shown to modulate immune responses40,41
and Hox et al42 recently found that sex-specific differences in a
mouse modelof anaphylaxis were due to the female steroid
estradiol.
The finding that 28 (85%) cases had pre-existing atopic dis
(3 with prior anaphylaxis,16 with asthma,and 9 with specific
priorallergies)is consistentwith earlierreports emphasizing
coexisting atopic disease,particularly asthma,as being clinical
risk factorsfor anaphylaxis.29,30,43Although epinephrineis
recommended as the drug ofchoice foranaphylaxis,3,44 this
therapy, as documented in the medical records, was adminis
in only 15 (45%) of our cases compared with antihistamines
(85%) cases and corticosteroids in 17 (52%) cases. Only 3 (9
caseswere documented to have been prescribed epinephrine
autoinjectors, and only 5 (15%) were known to have been re
to an allergist/allergy clinicfor follow-up.The 2010 Joint
AmericanAcademyof Allergy, Asthma& Immunology/
American College ofAllergy,Asthma & Immunology/Joint
Councilof Allergy,Asthma & Immunology Task Force on
Practice Parameters for the management of anaphylaxis clea
state thatif initialassessmentsupports potentialanaphylaxis,
the immediate intervention isto assessthe patient’sairway,
TABLE VI. Vaccination-triggered anaphylaxis cases by vaccine
exposures (n 5 33)
Vaccine Alone
With
other
vaccines Other concomitant vaccine(s)*
TIV 10 4 MIV, Tdap (2),PPSV23
MIV 2 1 TIV
Tdap 1 8 TIV (2), HPV4,HAV,VAR, MCV41MMRV,
MCV41VAR, MCV41VAR1HAV
PPSV23 1 1 TIV
HAV 1 3 Tdap,Tdap1MCV41VAR,VAR
HZV 2 0 —
Rabies 1 0 —
HPV4 — 2 Tdap,MMR1MCV4
MMR — 3 DTaP-IPV1VAR,DTaP1IPV1VAR, HPV41
MCV4
MMRV — 2 Tdap1MCV4, DTaP1IPV
MCV4 — 4 Tdap1MMRV,Tdap1VAR,Tdap1VAR1
HAV,HPV41MMR
VAR — 5 Tdap,Tdap1MCV41HAV,DTaP-IPV1
MMR, HAV,Tdap1MCV4
DTaP-IPV — 1 MMR1VAR
DTaP — 2 MMRV1IPV, MMR1IPV1VAR
IPV — 2 DTaP1MMRV,DTaP1MMR1VAR
IPV, Inactivated polio vaccine; MCV4,meningococcal conjugate vaccine;
MMRV,measles,mumps,rubella,and varicella vaccine; PPSV23,pneumococcal
polysaccharide vaccine (23-valent); VAR,varicella vaccine.
*A total of 15 (45%) cases received 2 or more concomitant vaccines.
J ALLERGY CLIN IMMUNOL
nnn 2015
8 MCNEIL ET AL
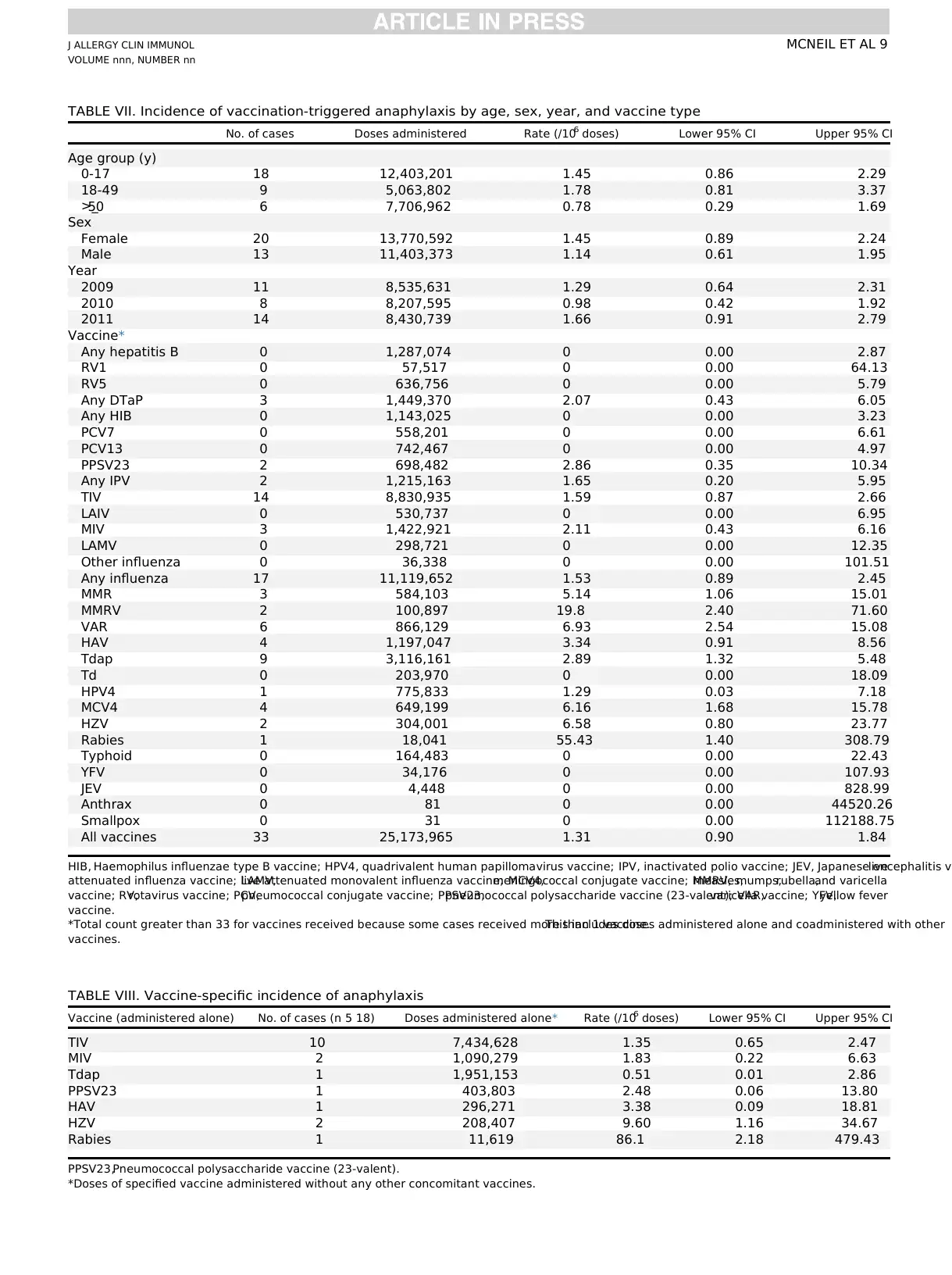
TABLE VII. Incidence of vaccination-triggered anaphylaxis by age, sex, year, and vaccine type
No. of cases Doses administered Rate (/106 doses) Lower 95% CI Upper 95% CI
Age group (y)
0-17 18 12,403,201 1.45 0.86 2.29
18-49 9 5,063,802 1.78 0.81 3.37
>_50 6 7,706,962 0.78 0.29 1.69
Sex
Female 20 13,770,592 1.45 0.89 2.24
Male 13 11,403,373 1.14 0.61 1.95
Year
2009 11 8,535,631 1.29 0.64 2.31
2010 8 8,207,595 0.98 0.42 1.92
2011 14 8,430,739 1.66 0.91 2.79
Vaccine*
Any hepatitis B 0 1,287,074 0 0.00 2.87
RV1 0 57,517 0 0.00 64.13
RV5 0 636,756 0 0.00 5.79
Any DTaP 3 1,449,370 2.07 0.43 6.05
Any HIB 0 1,143,025 0 0.00 3.23
PCV7 0 558,201 0 0.00 6.61
PCV13 0 742,467 0 0.00 4.97
PPSV23 2 698,482 2.86 0.35 10.34
Any IPV 2 1,215,163 1.65 0.20 5.95
TIV 14 8,830,935 1.59 0.87 2.66
LAIV 0 530,737 0 0.00 6.95
MIV 3 1,422,921 2.11 0.43 6.16
LAMV 0 298,721 0 0.00 12.35
Other influenza 0 36,338 0 0.00 101.51
Any influenza 17 11,119,652 1.53 0.89 2.45
MMR 3 584,103 5.14 1.06 15.01
MMRV 2 100,897 19.8 2.40 71.60
VAR 6 866,129 6.93 2.54 15.08
HAV 4 1,197,047 3.34 0.91 8.56
Tdap 9 3,116,161 2.89 1.32 5.48
Td 0 203,970 0 0.00 18.09
HPV4 1 775,833 1.29 0.03 7.18
MCV4 4 649,199 6.16 1.68 15.78
HZV 2 304,001 6.58 0.80 23.77
Rabies 1 18,041 55.43 1.40 308.79
Typhoid 0 164,483 0 0.00 22.43
YFV 0 34,176 0 0.00 107.93
JEV 0 4,448 0 0.00 828.99
Anthrax 0 81 0 0.00 44520.26
Smallpox 0 31 0 0.00 112188.75
All vaccines 33 25,173,965 1.31 0.90 1.84
HIB, Haemophilus influenzae type B vaccine; HPV4, quadrivalent human papillomavirus vaccine; IPV, inactivated polio vaccine; JEV, Japanese encephalitis valive
attenuated influenza vaccine; LAMV,live attenuated monovalent influenza vaccine; MCV4,meningococcal conjugate vaccine; MMRV,measles,mumps,rubella,and varicella
vaccine; RV,rotavirus vaccine; PCV,pneumococcal conjugate vaccine; PPSV23,pneumococcal polysaccharide vaccine (23-valent); VAR,varicella vaccine; YFV,yellow fever
vaccine.
*Total count greater than 33 for vaccines received because some cases received more than 1 vaccine.This includes doses administered alone and coadministered with other
vaccines.
TABLE VIII. Vaccine-specific incidence of anaphylaxis
Vaccine (administered alone) No. of cases (n 5 18) Doses administered alone* Rate (/106 doses) Lower 95% CI Upper 95% CI
TIV 10 7,434,628 1.35 0.65 2.47
MIV 2 1,090,279 1.83 0.22 6.63
Tdap 1 1,951,153 0.51 0.01 2.86
PPSV23 1 403,803 2.48 0.06 13.80
HAV 1 296,271 3.38 0.09 18.81
HZV 2 208,407 9.60 1.16 34.67
Rabies 1 11,619 86.1 2.18 479.43
PPSV23,Pneumococcal polysaccharide vaccine (23-valent).
*Doses of specified vaccine administered without any other concomitant vaccines.
J ALLERGY CLIN IMMUNOL
VOLUME nnn, NUMBER nn
MCNEIL ET AL 9
No. of cases Doses administered Rate (/106 doses) Lower 95% CI Upper 95% CI
Age group (y)
0-17 18 12,403,201 1.45 0.86 2.29
18-49 9 5,063,802 1.78 0.81 3.37
>_50 6 7,706,962 0.78 0.29 1.69
Sex
Female 20 13,770,592 1.45 0.89 2.24
Male 13 11,403,373 1.14 0.61 1.95
Year
2009 11 8,535,631 1.29 0.64 2.31
2010 8 8,207,595 0.98 0.42 1.92
2011 14 8,430,739 1.66 0.91 2.79
Vaccine*
Any hepatitis B 0 1,287,074 0 0.00 2.87
RV1 0 57,517 0 0.00 64.13
RV5 0 636,756 0 0.00 5.79
Any DTaP 3 1,449,370 2.07 0.43 6.05
Any HIB 0 1,143,025 0 0.00 3.23
PCV7 0 558,201 0 0.00 6.61
PCV13 0 742,467 0 0.00 4.97
PPSV23 2 698,482 2.86 0.35 10.34
Any IPV 2 1,215,163 1.65 0.20 5.95
TIV 14 8,830,935 1.59 0.87 2.66
LAIV 0 530,737 0 0.00 6.95
MIV 3 1,422,921 2.11 0.43 6.16
LAMV 0 298,721 0 0.00 12.35
Other influenza 0 36,338 0 0.00 101.51
Any influenza 17 11,119,652 1.53 0.89 2.45
MMR 3 584,103 5.14 1.06 15.01
MMRV 2 100,897 19.8 2.40 71.60
VAR 6 866,129 6.93 2.54 15.08
HAV 4 1,197,047 3.34 0.91 8.56
Tdap 9 3,116,161 2.89 1.32 5.48
Td 0 203,970 0 0.00 18.09
HPV4 1 775,833 1.29 0.03 7.18
MCV4 4 649,199 6.16 1.68 15.78
HZV 2 304,001 6.58 0.80 23.77
Rabies 1 18,041 55.43 1.40 308.79
Typhoid 0 164,483 0 0.00 22.43
YFV 0 34,176 0 0.00 107.93
JEV 0 4,448 0 0.00 828.99
Anthrax 0 81 0 0.00 44520.26
Smallpox 0 31 0 0.00 112188.75
All vaccines 33 25,173,965 1.31 0.90 1.84
HIB, Haemophilus influenzae type B vaccine; HPV4, quadrivalent human papillomavirus vaccine; IPV, inactivated polio vaccine; JEV, Japanese encephalitis valive
attenuated influenza vaccine; LAMV,live attenuated monovalent influenza vaccine; MCV4,meningococcal conjugate vaccine; MMRV,measles,mumps,rubella,and varicella
vaccine; RV,rotavirus vaccine; PCV,pneumococcal conjugate vaccine; PPSV23,pneumococcal polysaccharide vaccine (23-valent); VAR,varicella vaccine; YFV,yellow fever
vaccine.
*Total count greater than 33 for vaccines received because some cases received more than 1 vaccine.This includes doses administered alone and coadministered with other
vaccines.
TABLE VIII. Vaccine-specific incidence of anaphylaxis
Vaccine (administered alone) No. of cases (n 5 18) Doses administered alone* Rate (/106 doses) Lower 95% CI Upper 95% CI
TIV 10 7,434,628 1.35 0.65 2.47
MIV 2 1,090,279 1.83 0.22 6.63
Tdap 1 1,951,153 0.51 0.01 2.86
PPSV23 1 403,803 2.48 0.06 13.80
HAV 1 296,271 3.38 0.09 18.81
HZV 2 208,407 9.60 1.16 34.67
Rabies 1 11,619 86.1 2.18 479.43
PPSV23,Pneumococcal polysaccharide vaccine (23-valent).
*Doses of specified vaccine administered without any other concomitant vaccines.
J ALLERGY CLIN IMMUNOL
VOLUME nnn, NUMBER nn
MCNEIL ET AL 9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

breathing,circulation,and mentation;injectepinephrine;and
re-evaluate for repeatinjection,if necessary.3 After resolution,
the patient should be provided with autoinjectable epinephrine,
and in circumstances in which an allergist/immunologist is not
alreadyinvolved,it is stronglyrecommendedthat such
consultation should be obtained.3 Lack of use ofepinephrine
and these otherrecommendations is notspecific to ourstudy
and has been commented on by other investigators.3,45-48
Our study, which is based on a very large population receiving
currently used vaccines,confirms the rarity of postvaccination
anaphylaxisoverall and after specificvaccines.Although
anaphylaxisafterimmunization israre,its immediate onset
(usually within minutes) and life-threatening nature require that
all personneland facilities providingvaccinationshave
procedures in place foranaphylaxis management.Additional
providereducation concerning currentrecommendationsfor
treatment and follow-up appears to be warranted.
Clinical implications: Anaphylaxis after vaccination is rare in
all age groups.Despite its rarity,anaphylaxis is a potentially
life-threatening medicalemergency thatvaccineproviders
need to be prepared to treat.
REFERENCES
1. Austen KF. Diseaseof immediatetype hypersensitivity.In: IsselbacherKJ,
Braunwald E,Wilson JD,Martin JB,FauciAS, Kasper DL,editors.Harrison’s
principlesof internalmedicine.13th ed.New York: McGraw-Hill;1994.pp.
1630-8.
2. Simmons FE.Anaphylaxis.J Allergy Immunol 2010;125(suppl):S161-81.
3. Lieberman P,Nicklas RA,OppenheimerJ, Kemp SF,Lang DM,Bernstein DI,
et al. The diagnosis and managementof anaphylaxis practice parameter:2010
update.J Allergy Clin Immunol 2010;126:477-80,e1-42.
4. Simons FE, Ardusso LR, Bilo B, El-Gamal YM, Ledford DK, Ring J, et al. World
Allergy Organization guidelines for the assessmentand managementof anaphy-
laxis.J Allergy Clin Immunol 2011;127(593):e1-22.
5. Centers for Disease Control and Prevention. General recommendations on immu-
nization—recommendations of the Advisory Committee on Immunization Prac-
tices (ACIP).MMWR Recomm Rep 2011;60:1-64.
6. Kelso JM, Li JT, Nicklas RA, Blessing-Moore J, Cox L, Lang DM, et al. Adverse
reactions to vaccines. Ann Allergy Asthma Immunol 2009;103(4 Suppl 2):S1-14 .
7. Stratton K,Ford A,Rusch E,Clayton EW,editors.Adverse effects of vaccines:
evidenceand causality.Instituteof Medicine.Washington(DC): National
Academies Press; 2011.
8. Grabenstein JD. Clinical management of hypersensitivities to vaccine components.
Hospital Pharmacy 1997;32:77-87.
9. Lear JT,English JS.Anaphylaxis after hepatitis B vaccination.Lancet 1995;345:
1249.
10. Baggs J,Gee J,Lewis E,Fowler G,Benson P,Lieu T,et al.The Vaccine Safety
Datalink:a modelfor monitoring vaccine safety.Pediatrics2011;127(suppl):
S45-53.
11. Bohlke K, Davis RL, Marcy SM, Braun MM, DeStefano F, Black SB, et al. Risk of
anaphylaxis aftervaccination ofchildren and adolescents.Pediatrics 2003;112:
815-20.
12. Ruggeberg JU, Gold MS, Bayas JM, Blum MD, Bonhoeffer J, Friedlander S, et al.
Anaphylaxis:case definition and guidelinesfor data collection,analysisand
presentation of immunization safety data.Vaccine 2007;25:5675-84.
13. McNeil MM, Gee J,Weintraub ES,Belongia EA,Lee GM,Glanz JM,et al.The
Vaccine Safety Datalink:successesand challengesmonitoring vaccine safety.
Vaccine 2014;32:5390-8.
14. Rothman KJ, Boice JD Jr. Epidemiologic analysis with a programmable calculator.
Bethesda (MD):NationalInstitutes of Health;1979;31-2,NIH publication no.
79-1649.
15. GrohskopfLA, Olsen SJ,Sokolow LZ,Bresee JS,Cox NJ, BroderKR, et al.
Prevention and controlof seasonalinfluenza with vaccines:recommendations of
the Advisory Committeeon Immunization Practices(ACIP)—United States,
2014-15 influenza season.MMWR Morb Mortal Wkly Rep 2014;63:691-7.
16. Sampson HA,Mu~noz-Furlong A,Bock SA,Schmitt C,Bass R,Chowdhury BA,
et al. Symposium on the definition and managementof anaphylaxis:summary
report.J Allergy Clin Immunol 2005;115:584-92.
17. Sampson HA, Mu~noz-Furlong A, Campbell RL, Adkinson NF, Bock SA, Branum
A, et al. Second symposium on the definition and managementof anaphylaxis:
summary report—second National Institute of Allergy and Infectious Disease/Fo
Allergy and Anaphylaxis Network Symposium. J Allergy Clin Immunol 2006;117:
391-7.
18. Erlewyn-Lajeunesse M,HuntLP, Heath PT,Finn A. Anaphylaxis as an adverse
eventfollowing immunization in the UK and Ireland.Arch Dis Child 2012;97:
487-90.
19. Brotherton JM, Gold MS, Kemp AS, McIntyre PB, Burgess MA, Campbell-Lloyd
S, et al. Anaphylaxis following quadrivalenthuman papillomavirus vaccination.
CMAJ 2008;179:525-33.
20. Rouleau I,De Serres G,DroletJP, SkowronskiDM, OuakkiM, Toth A, et al.
Increased risk of anaphylaxis following administration of 2009 AS03-adjuvanted
monovalent pandemic A/H1N1 (H1N1pdm09) vaccine. Vaccine 2013;31:5989-9
21. Tavares F,Delaigle A,Slavin D,Bauchau V,Fries L, SiefertH. Anaphylaxis
following H1N1 pandemic vaccines: safety data in perspective.Vaccine 2011;29:
6402-7.
22. Vellozzi C, Broder KR, Haber P, Guh A, Nguyen M, Cano M, et al. Adverse events
following influenzaA (H1N1) monovalentvaccinesreported to theVaccine
Adverse EventReporting System,United States,October1, 2009-January 31,
2010.Vaccine 2010;28:7248-55.
23. Vellozzi C, Burwen DR,Dobardzic A,Ball R, HaberP. Safety oftrivalent
inactivated influenzavaccinesin adults:background forpandemicinfluenza
vaccine safety monitoring. Vaccine 2009;27:2114-20.
24. Jershow E,Lin RY, Scaperotti MM,McGinn AP.Fatal anaphylaxis in the United
States,1999-2010:temporalpatternsand demographic association.J Allergy
Clin Immunol 2014;134:1318-28.
25. SargantN, Erlewyn-Lajeunesse M,BengerJ. Does anaphylaxis masquerade as
asthma in children? Emerg Med J 2015;32:83-4.
26. Erlwyn-Lajeunesse M,Dymond S,Slade I,Mansfield HL,Fish R,Jones O, et al.
Diagnostic utility oftwo case definitions foranaphylaxis:a comparison using
retrospective case notes analysis in the UK.Drug Saf 2010;33:57-64.
27. Lieberman PL.Anaphylaxis.In: Adkinson N,Bochner B,Busse W,Holgate S,
Lemanske R,SimonsF, editors.Middleton’sallergy:principlesand practice.
7th ed.Philadelphia:Mosby;2008.pp.1027-50.
28. Sheikh A,Hippisley-Cox J,Newton J,Fenty J. Trendsin nationalincidence,
lifetime prevalence and adrenaline prescribing foranaphylaxis in England.J R
Soc Med 2008;101:139-43.
29. Gonzalez-Perez A, Aponte Z, VidaurreCF, RodriguezLA. Anaphylaxis
epidemiology in patients with and patients withoutasthma:a United Kingdom
database review.J Allergy Clin Immunol 2010;125:1098-104.
30. Clark S, Wei W, Rudders SA, Camargo CA Jr. Risk factors for severe anaphylaxis
in patients receiving anaphylaxis treatmentin US emergency departments and
hospitals.J Allergy Clin Immunol 2014;134:1125-30.
31. Chen W,MempelM, SchoberW, BehrendtH, Ring J. Genderdifference,sex
hormones,and immediatetype hypersensitivityreactions.Allergy 2008;63:
1418-27.
32. Decker WW, Campbell RL, Manivannan V, Luke A, St Sauver JL, Weaver A, et al.
The etiology and incidence ofanaphylaxisin Rochester,Minnesota:a report
from the RochesterEpidemiology Project.J Allergy Clin Immunol2008;122:
1161-5.
33. Cook IF. Sexual dimorphism of humoral immunity with human vaccines. Vaccine
2008;26:3551-5.
34. Cook IF. Sex differences in injection site reactions with human vaccines.Hum
Vaccin 2009;5:441-9.
35. Klein SL, Jedlicka A,Pekosz A.The Xs and Y ofimmune responses to viral
vaccines. Lancet Infect Dis 2010;10:338-49.
36. Engler RJ, Nelson MR, Klote MM, VanRaden MJ, Haang CY, Cox NJ, et al. Half-
vs full- dose trivalent inactivated influenza vaccine (2004-2005): age, dose, and
effects on immune responses.Arch Intern Med 2008;156:1546-50.
37. Nichol KL, Margolis KL, Lind A, Murdoch M, McFadden R, Hauge M, et al. Side
effectsassociatedwith influenzavaccinationin healthyworking adults:a
randomized placebo-controlled trial.Arch Intern Med 1996;156:1546-50.
38. Khalil MK, Al-Mazrou YY, Al-Ghamdi YS, Tumsah S, Al-Jeffri M, Meshkhas A.
Effectof genderon reporting ofMMR adverse eventsin SaudiArabia.East
Mediter Health J 2003;9:152-8.
39. Benjamin CM,Chew GC,Silman AJ.Joint and limb symptoms in children after
immunization with measles,mumps,and rubella vaccine.BMJ 1992;304:1075-8.
40. Pennell LM, Galligan CL, Fish EN. Sex affects immunity. J Autoimmun 2012;38:
1075-8.
41. VerthelyiD. Sex hormonesas immunomodulatorsin health and disease.Int
Immunopharmacol 2001;1:983-93.
42. Hox V, DesaiA, Bandara G,Gilfillan AM, Metcalfe DD,Olivera A.Estrogen
increases the severity of anaphylaxis in female mice through enhanced endoth
J ALLERGY CLIN IMMUNOL
nnn 2015
10 MCNEIL ET AL
re-evaluate for repeatinjection,if necessary.3 After resolution,
the patient should be provided with autoinjectable epinephrine,
and in circumstances in which an allergist/immunologist is not
alreadyinvolved,it is stronglyrecommendedthat such
consultation should be obtained.3 Lack of use ofepinephrine
and these otherrecommendations is notspecific to ourstudy
and has been commented on by other investigators.3,45-48
Our study, which is based on a very large population receiving
currently used vaccines,confirms the rarity of postvaccination
anaphylaxisoverall and after specificvaccines.Although
anaphylaxisafterimmunization israre,its immediate onset
(usually within minutes) and life-threatening nature require that
all personneland facilities providingvaccinationshave
procedures in place foranaphylaxis management.Additional
providereducation concerning currentrecommendationsfor
treatment and follow-up appears to be warranted.
Clinical implications: Anaphylaxis after vaccination is rare in
all age groups.Despite its rarity,anaphylaxis is a potentially
life-threatening medicalemergency thatvaccineproviders
need to be prepared to treat.
REFERENCES
1. Austen KF. Diseaseof immediatetype hypersensitivity.In: IsselbacherKJ,
Braunwald E,Wilson JD,Martin JB,FauciAS, Kasper DL,editors.Harrison’s
principlesof internalmedicine.13th ed.New York: McGraw-Hill;1994.pp.
1630-8.
2. Simmons FE.Anaphylaxis.J Allergy Immunol 2010;125(suppl):S161-81.
3. Lieberman P,Nicklas RA,OppenheimerJ, Kemp SF,Lang DM,Bernstein DI,
et al. The diagnosis and managementof anaphylaxis practice parameter:2010
update.J Allergy Clin Immunol 2010;126:477-80,e1-42.
4. Simons FE, Ardusso LR, Bilo B, El-Gamal YM, Ledford DK, Ring J, et al. World
Allergy Organization guidelines for the assessmentand managementof anaphy-
laxis.J Allergy Clin Immunol 2011;127(593):e1-22.
5. Centers for Disease Control and Prevention. General recommendations on immu-
nization—recommendations of the Advisory Committee on Immunization Prac-
tices (ACIP).MMWR Recomm Rep 2011;60:1-64.
6. Kelso JM, Li JT, Nicklas RA, Blessing-Moore J, Cox L, Lang DM, et al. Adverse
reactions to vaccines. Ann Allergy Asthma Immunol 2009;103(4 Suppl 2):S1-14 .
7. Stratton K,Ford A,Rusch E,Clayton EW,editors.Adverse effects of vaccines:
evidenceand causality.Instituteof Medicine.Washington(DC): National
Academies Press; 2011.
8. Grabenstein JD. Clinical management of hypersensitivities to vaccine components.
Hospital Pharmacy 1997;32:77-87.
9. Lear JT,English JS.Anaphylaxis after hepatitis B vaccination.Lancet 1995;345:
1249.
10. Baggs J,Gee J,Lewis E,Fowler G,Benson P,Lieu T,et al.The Vaccine Safety
Datalink:a modelfor monitoring vaccine safety.Pediatrics2011;127(suppl):
S45-53.
11. Bohlke K, Davis RL, Marcy SM, Braun MM, DeStefano F, Black SB, et al. Risk of
anaphylaxis aftervaccination ofchildren and adolescents.Pediatrics 2003;112:
815-20.
12. Ruggeberg JU, Gold MS, Bayas JM, Blum MD, Bonhoeffer J, Friedlander S, et al.
Anaphylaxis:case definition and guidelinesfor data collection,analysisand
presentation of immunization safety data.Vaccine 2007;25:5675-84.
13. McNeil MM, Gee J,Weintraub ES,Belongia EA,Lee GM,Glanz JM,et al.The
Vaccine Safety Datalink:successesand challengesmonitoring vaccine safety.
Vaccine 2014;32:5390-8.
14. Rothman KJ, Boice JD Jr. Epidemiologic analysis with a programmable calculator.
Bethesda (MD):NationalInstitutes of Health;1979;31-2,NIH publication no.
79-1649.
15. GrohskopfLA, Olsen SJ,Sokolow LZ,Bresee JS,Cox NJ, BroderKR, et al.
Prevention and controlof seasonalinfluenza with vaccines:recommendations of
the Advisory Committeeon Immunization Practices(ACIP)—United States,
2014-15 influenza season.MMWR Morb Mortal Wkly Rep 2014;63:691-7.
16. Sampson HA,Mu~noz-Furlong A,Bock SA,Schmitt C,Bass R,Chowdhury BA,
et al. Symposium on the definition and managementof anaphylaxis:summary
report.J Allergy Clin Immunol 2005;115:584-92.
17. Sampson HA, Mu~noz-Furlong A, Campbell RL, Adkinson NF, Bock SA, Branum
A, et al. Second symposium on the definition and managementof anaphylaxis:
summary report—second National Institute of Allergy and Infectious Disease/Fo
Allergy and Anaphylaxis Network Symposium. J Allergy Clin Immunol 2006;117:
391-7.
18. Erlewyn-Lajeunesse M,HuntLP, Heath PT,Finn A. Anaphylaxis as an adverse
eventfollowing immunization in the UK and Ireland.Arch Dis Child 2012;97:
487-90.
19. Brotherton JM, Gold MS, Kemp AS, McIntyre PB, Burgess MA, Campbell-Lloyd
S, et al. Anaphylaxis following quadrivalenthuman papillomavirus vaccination.
CMAJ 2008;179:525-33.
20. Rouleau I,De Serres G,DroletJP, SkowronskiDM, OuakkiM, Toth A, et al.
Increased risk of anaphylaxis following administration of 2009 AS03-adjuvanted
monovalent pandemic A/H1N1 (H1N1pdm09) vaccine. Vaccine 2013;31:5989-9
21. Tavares F,Delaigle A,Slavin D,Bauchau V,Fries L, SiefertH. Anaphylaxis
following H1N1 pandemic vaccines: safety data in perspective.Vaccine 2011;29:
6402-7.
22. Vellozzi C, Broder KR, Haber P, Guh A, Nguyen M, Cano M, et al. Adverse events
following influenzaA (H1N1) monovalentvaccinesreported to theVaccine
Adverse EventReporting System,United States,October1, 2009-January 31,
2010.Vaccine 2010;28:7248-55.
23. Vellozzi C, Burwen DR,Dobardzic A,Ball R, HaberP. Safety oftrivalent
inactivated influenzavaccinesin adults:background forpandemicinfluenza
vaccine safety monitoring. Vaccine 2009;27:2114-20.
24. Jershow E,Lin RY, Scaperotti MM,McGinn AP.Fatal anaphylaxis in the United
States,1999-2010:temporalpatternsand demographic association.J Allergy
Clin Immunol 2014;134:1318-28.
25. SargantN, Erlewyn-Lajeunesse M,BengerJ. Does anaphylaxis masquerade as
asthma in children? Emerg Med J 2015;32:83-4.
26. Erlwyn-Lajeunesse M,Dymond S,Slade I,Mansfield HL,Fish R,Jones O, et al.
Diagnostic utility oftwo case definitions foranaphylaxis:a comparison using
retrospective case notes analysis in the UK.Drug Saf 2010;33:57-64.
27. Lieberman PL.Anaphylaxis.In: Adkinson N,Bochner B,Busse W,Holgate S,
Lemanske R,SimonsF, editors.Middleton’sallergy:principlesand practice.
7th ed.Philadelphia:Mosby;2008.pp.1027-50.
28. Sheikh A,Hippisley-Cox J,Newton J,Fenty J. Trendsin nationalincidence,
lifetime prevalence and adrenaline prescribing foranaphylaxis in England.J R
Soc Med 2008;101:139-43.
29. Gonzalez-Perez A, Aponte Z, VidaurreCF, RodriguezLA. Anaphylaxis
epidemiology in patients with and patients withoutasthma:a United Kingdom
database review.J Allergy Clin Immunol 2010;125:1098-104.
30. Clark S, Wei W, Rudders SA, Camargo CA Jr. Risk factors for severe anaphylaxis
in patients receiving anaphylaxis treatmentin US emergency departments and
hospitals.J Allergy Clin Immunol 2014;134:1125-30.
31. Chen W,MempelM, SchoberW, BehrendtH, Ring J. Genderdifference,sex
hormones,and immediatetype hypersensitivityreactions.Allergy 2008;63:
1418-27.
32. Decker WW, Campbell RL, Manivannan V, Luke A, St Sauver JL, Weaver A, et al.
The etiology and incidence ofanaphylaxisin Rochester,Minnesota:a report
from the RochesterEpidemiology Project.J Allergy Clin Immunol2008;122:
1161-5.
33. Cook IF. Sexual dimorphism of humoral immunity with human vaccines. Vaccine
2008;26:3551-5.
34. Cook IF. Sex differences in injection site reactions with human vaccines.Hum
Vaccin 2009;5:441-9.
35. Klein SL, Jedlicka A,Pekosz A.The Xs and Y ofimmune responses to viral
vaccines. Lancet Infect Dis 2010;10:338-49.
36. Engler RJ, Nelson MR, Klote MM, VanRaden MJ, Haang CY, Cox NJ, et al. Half-
vs full- dose trivalent inactivated influenza vaccine (2004-2005): age, dose, and
effects on immune responses.Arch Intern Med 2008;156:1546-50.
37. Nichol KL, Margolis KL, Lind A, Murdoch M, McFadden R, Hauge M, et al. Side
effectsassociatedwith influenzavaccinationin healthyworking adults:a
randomized placebo-controlled trial.Arch Intern Med 1996;156:1546-50.
38. Khalil MK, Al-Mazrou YY, Al-Ghamdi YS, Tumsah S, Al-Jeffri M, Meshkhas A.
Effectof genderon reporting ofMMR adverse eventsin SaudiArabia.East
Mediter Health J 2003;9:152-8.
39. Benjamin CM,Chew GC,Silman AJ.Joint and limb symptoms in children after
immunization with measles,mumps,and rubella vaccine.BMJ 1992;304:1075-8.
40. Pennell LM, Galligan CL, Fish EN. Sex affects immunity. J Autoimmun 2012;38:
1075-8.
41. VerthelyiD. Sex hormonesas immunomodulatorsin health and disease.Int
Immunopharmacol 2001;1:983-93.
42. Hox V, DesaiA, Bandara G,Gilfillan AM, Metcalfe DD,Olivera A.Estrogen
increases the severity of anaphylaxis in female mice through enhanced endoth
J ALLERGY CLIN IMMUNOL
nnn 2015
10 MCNEIL ET AL
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
nitric acid oxide synthetase expression and nitric oxide production. J Allergy Clin
Immunol 2015;135:729-36.e5.
43. Iribarren C, Tolstykh IV, Miller MK, Eisner MD. Asthma and the
prospective risk ofanaphylactic shock and otherallergy diagnosesin a large
integrated health care delivery system.Ann Allergy Asthma Immunol 2010;104:
371-7.
44. Simons FER.Pharmacologic treatment of anaphylaxis:can the evidence base be
strengthened? Curr Opin Allergy Clin Immunol 2010;10:384-93.
45. CampbellRL, Luke A, Weaver AL,St SauverJL, Bergstralh EJ,Li JT, et al.
Prescriptions for self-injectable epinephrine and follow-up referralin emergency
departmentpatients presenting with anaphylaxis.Ann Allergy Asthma Immunol
2008;101:631-6.
46. Campbell RL,Park MA,Kieber MA,SangilL, Hagan JB.Outcomes of allergy/
immunology follow-up after an emergency department evaluation for anaphyl
J Allergy Clin Immunol Pract 2015;3:88-93.
47. Rudders SA,Clark S,Wei W, Camargo CA.Longitudinalstudy of 954 patients
with stinginginsectanaphylaxis.Ann Allergy AsthmaImmunol2013;111:
199-204.e1.
48. Dudley LS,Mansour MI,Merlin MA.Epinephrine for anaphylaxis: underutilized
and unavailable.West J Emerg Med 2015;16:385-7.
J ALLERGY CLIN IMMUNOL
VOLUME nnn, NUMBER nn
MCNEIL ET AL 11
Immunol 2015;135:729-36.e5.
43. Iribarren C, Tolstykh IV, Miller MK, Eisner MD. Asthma and the
prospective risk ofanaphylactic shock and otherallergy diagnosesin a large
integrated health care delivery system.Ann Allergy Asthma Immunol 2010;104:
371-7.
44. Simons FER.Pharmacologic treatment of anaphylaxis:can the evidence base be
strengthened? Curr Opin Allergy Clin Immunol 2010;10:384-93.
45. CampbellRL, Luke A, Weaver AL,St SauverJL, Bergstralh EJ,Li JT, et al.
Prescriptions for self-injectable epinephrine and follow-up referralin emergency
departmentpatients presenting with anaphylaxis.Ann Allergy Asthma Immunol
2008;101:631-6.
46. Campbell RL,Park MA,Kieber MA,SangilL, Hagan JB.Outcomes of allergy/
immunology follow-up after an emergency department evaluation for anaphyl
J Allergy Clin Immunol Pract 2015;3:88-93.
47. Rudders SA,Clark S,Wei W, Camargo CA.Longitudinalstudy of 954 patients
with stinginginsectanaphylaxis.Ann Allergy AsthmaImmunol2013;111:
199-204.e1.
48. Dudley LS,Mansour MI,Merlin MA.Epinephrine for anaphylaxis: underutilized
and unavailable.West J Emerg Med 2015;16:385-7.
J ALLERGY CLIN IMMUNOL
VOLUME nnn, NUMBER nn
MCNEIL ET AL 11
1 out of 11
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.