Case Study on Congestive Heart Failure (CHF) in Mrs. Sharon McKenzie
VerifiedAdded on 2023/04/25
|15
|3559
|480
AI Summary
This document is a case study on Congestive Heart Failure (CHF) in Mrs. Sharon McKenzie. It discusses the causes, risk factors, and impact of CHF on patients and their families. It also explains the pharmacokinetics and pharmacodynamics of ACE inhibitors for CHF treatment and provides a nursing care plan for Mrs. Sharon McKenzie with CHF.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

1
Running Head: Case Study
Case Study 1
Running Head: Case Study
Case Study 1
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
2
Case Study 1
Answer 1:
From the analysis of the case study, it has been found that Mrs Sharon McKenzie is suffering
from Congestive cardiac failure or Heart disease (CHF) (Zipes et al., 2018). The causes of this
disease are:
Hypertension: High blood pressure (more than 120/80mmHg) causes arteries to become
narrow as a result of which blood flow is interrupted. It leads to congestive heart failure
(Woodruffe et al., 2015).
Faulty Valve Conditions: Heart valves are responsible for regulating blood flow through
the heart in order to enable blood in and out of the chambers (O’Neil et al., 2016). When
valves do not open or close properly, it may create difficulty for ventricles to work harder
for pumping blood. It gradually leads to CHF.
Other Causes: Diabetes, Obesity, Allergic reactions, and Thyroid diseases also result in
CHF. Chronic diseases, for example, HIV, hypothyroidism, hyperthyroidism, or a
buildup of iron or protein also leads to heart failure (O’Neil et al., 2016).
Abmormal heart rate: This is called heart arrhythmias, which makes heart to beat slow or
fast. It also contributes to heart disease (Sevilla-Cazes et al., 2018).
Myocarditis: It is the swelling of the heart muscle, mainly caused by a virus that can lead
to heart disease.
Incidence of heart failure or disease: On the basis of overseas reports, it is found that around
300,000 Australians suffer from chronic heart failure (Huynh et al., 2018). Its
Case Study 1
Answer 1:
From the analysis of the case study, it has been found that Mrs Sharon McKenzie is suffering
from Congestive cardiac failure or Heart disease (CHF) (Zipes et al., 2018). The causes of this
disease are:
Hypertension: High blood pressure (more than 120/80mmHg) causes arteries to become
narrow as a result of which blood flow is interrupted. It leads to congestive heart failure
(Woodruffe et al., 2015).
Faulty Valve Conditions: Heart valves are responsible for regulating blood flow through
the heart in order to enable blood in and out of the chambers (O’Neil et al., 2016). When
valves do not open or close properly, it may create difficulty for ventricles to work harder
for pumping blood. It gradually leads to CHF.
Other Causes: Diabetes, Obesity, Allergic reactions, and Thyroid diseases also result in
CHF. Chronic diseases, for example, HIV, hypothyroidism, hyperthyroidism, or a
buildup of iron or protein also leads to heart failure (O’Neil et al., 2016).
Abmormal heart rate: This is called heart arrhythmias, which makes heart to beat slow or
fast. It also contributes to heart disease (Sevilla-Cazes et al., 2018).
Myocarditis: It is the swelling of the heart muscle, mainly caused by a virus that can lead
to heart disease.
Incidence of heart failure or disease: On the basis of overseas reports, it is found that around
300,000 Australians suffer from chronic heart failure (Huynh et al., 2018). Its
3
occurrence/incidence is approx four percent of the population aged 45 or above, with 30,000 new
heart diseases spotted every year.
Risk Factors of CHF:
Coronary artery disease: Narrowed arteries results in insufficient supply of oxygen rich
blood, thereby weakening the heart muscles (O’Neil et al., 2016).
Heart Attack: It causes damage to the heart muscle as a result of which the heart stops
pumping blood as efficiently as it should.
Certain medications: Medications may raise the chances of heart diseases. These include
anesthesia medications; nonsteroidal anti-inflammatory drugs (NSAIDs), and those
medications which are used to treat cancer, urological conditions, BP, psychiatric
conditions, and , inflammatory conditions (Sevilla-Cazes et al., 2018).
Sleep Apnea: Problem in breathing properly at sleep weakens the heart.
Congenital heart defects: Individuals who are born with structural heart faults.
Alcohol/Tobacco use: It weakens the heart muscles (O’Neil et al., 2016).
Impact of Heart disease on the patient and their family:
Heart disease greatly affects the physical as well as mental health of the patient. A bad heart
condition can disturb all aspects of patient's life, including his/her emotional health. Depression
is developed in persons with heart disease. It also hampers the rate of recovery and raises the risk
of further heart defects. In addition to this, heart disease is also a family affair. Their roles and
duties increase for the patient, and they also face the mental disturbance not less than the patient
(Nieminen et al., 2015). They also become psychologically weak and depressed, having patient's
care every time in their mind.
occurrence/incidence is approx four percent of the population aged 45 or above, with 30,000 new
heart diseases spotted every year.
Risk Factors of CHF:
Coronary artery disease: Narrowed arteries results in insufficient supply of oxygen rich
blood, thereby weakening the heart muscles (O’Neil et al., 2016).
Heart Attack: It causes damage to the heart muscle as a result of which the heart stops
pumping blood as efficiently as it should.
Certain medications: Medications may raise the chances of heart diseases. These include
anesthesia medications; nonsteroidal anti-inflammatory drugs (NSAIDs), and those
medications which are used to treat cancer, urological conditions, BP, psychiatric
conditions, and , inflammatory conditions (Sevilla-Cazes et al., 2018).
Sleep Apnea: Problem in breathing properly at sleep weakens the heart.
Congenital heart defects: Individuals who are born with structural heart faults.
Alcohol/Tobacco use: It weakens the heart muscles (O’Neil et al., 2016).
Impact of Heart disease on the patient and their family:
Heart disease greatly affects the physical as well as mental health of the patient. A bad heart
condition can disturb all aspects of patient's life, including his/her emotional health. Depression
is developed in persons with heart disease. It also hampers the rate of recovery and raises the risk
of further heart defects. In addition to this, heart disease is also a family affair. Their roles and
duties increase for the patient, and they also face the mental disturbance not less than the patient
(Nieminen et al., 2015). They also become psychologically weak and depressed, having patient's
care every time in their mind.
4
Answer 2:
In the given case, Sharon's blood pressure is 170/110 mmHg, which is higher than normal. Her
heart rate is HR 54 bpm, which is lower than normal rate of 60 to 100.These are the clear
symptoms of CHF. In addition to this, her swollen ankles, cold skin and shortness of breath also
confirm the signs of heart disease (Boman et al., 2018). Sharon also seems to experience
attention problems, memory loss, and other cognitive problems in the case study, as she forgets
to take all of her medications. our blood potassium level is 3.6 to 5.2 millimoles per liter
(mmol/L). Moreover, her low potassium level ( 2.5 mmol/L) which is less than normal level
(3.60 to 5.2 mmol/L) shows that her condition is critical, and urgently requires medical attention.
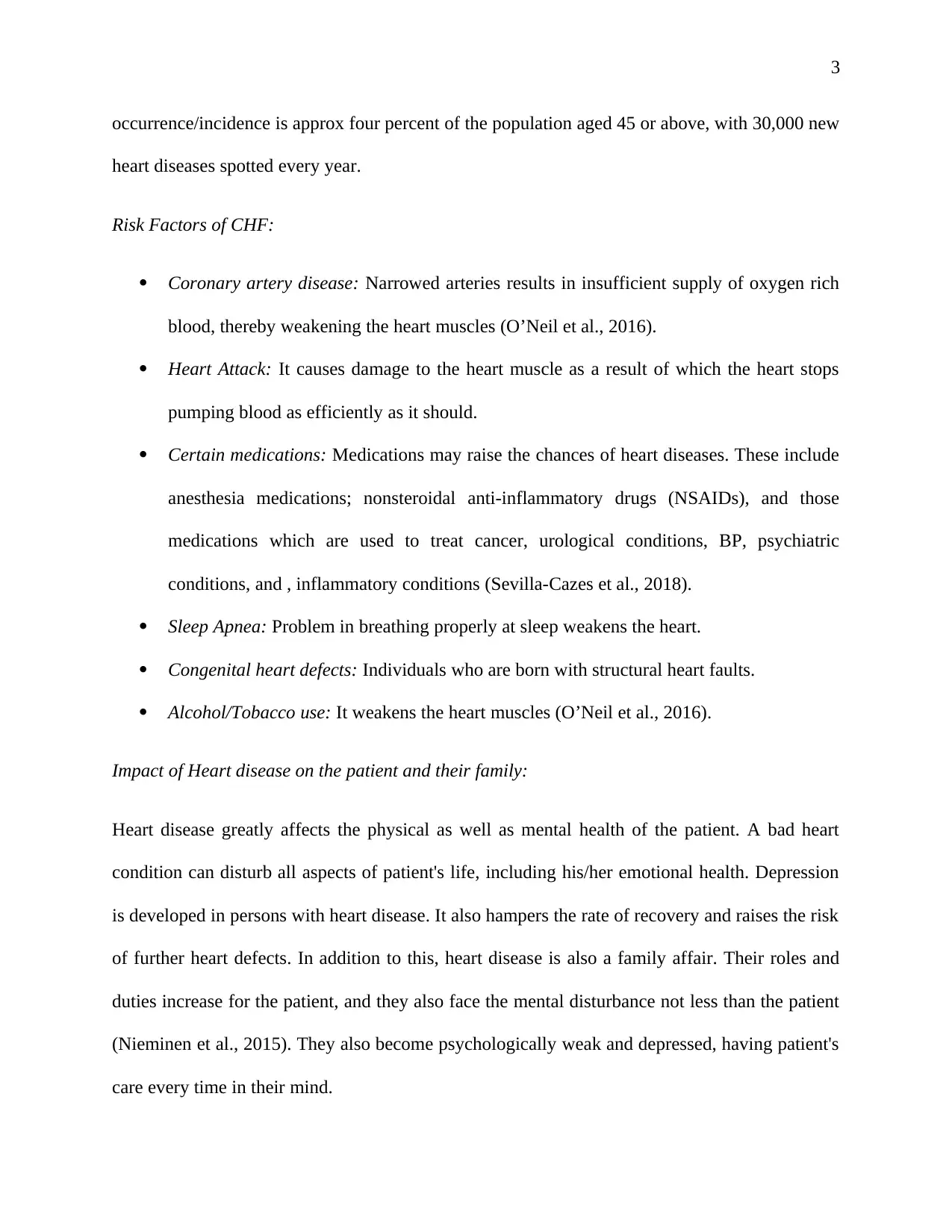
In medical, three common signs and symptoms of the Congestive cardiac/heart failure are as follow:
Symptoms that may be
observed first
Symptoms indicating that
condition has worsened
Symptoms indicating a
severe heart condition
swollen legs, ankles, and feet, cough that builds up from
congested lungs
fast breathing
fatigue slow/fast heartbeat (Horiuchi
et al., 2018)
chest pain radiating through
the upper body (Sanchis-
Gomar et al., 2016).
increased urinate, particularly
at night (Horiuchi et al.,
2018).
shortness of breath, including
pulmonary edema
fainting
weight gain wheezing skin appearing blue due to
insufficiency of oxygen in
Answer 2:
In the given case, Sharon's blood pressure is 170/110 mmHg, which is higher than normal. Her
heart rate is HR 54 bpm, which is lower than normal rate of 60 to 100.These are the clear
symptoms of CHF. In addition to this, her swollen ankles, cold skin and shortness of breath also
confirm the signs of heart disease (Boman et al., 2018). Sharon also seems to experience
attention problems, memory loss, and other cognitive problems in the case study, as she forgets
to take all of her medications. our blood potassium level is 3.6 to 5.2 millimoles per liter
(mmol/L). Moreover, her low potassium level ( 2.5 mmol/L) which is less than normal level
(3.60 to 5.2 mmol/L) shows that her condition is critical, and urgently requires medical attention.
In medical, three common signs and symptoms of the Congestive cardiac/heart failure are as follow:
Symptoms that may be
observed first
Symptoms indicating that
condition has worsened
Symptoms indicating a
severe heart condition
swollen legs, ankles, and feet, cough that builds up from
congested lungs
fast breathing
fatigue slow/fast heartbeat (Horiuchi
et al., 2018)
chest pain radiating through
the upper body (Sanchis-
Gomar et al., 2016).
increased urinate, particularly
at night (Horiuchi et al.,
2018).
shortness of breath, including
pulmonary edema
fainting
weight gain wheezing skin appearing blue due to
insufficiency of oxygen in
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
5
lungs (Sanchis-Gomar et al.,
2016)
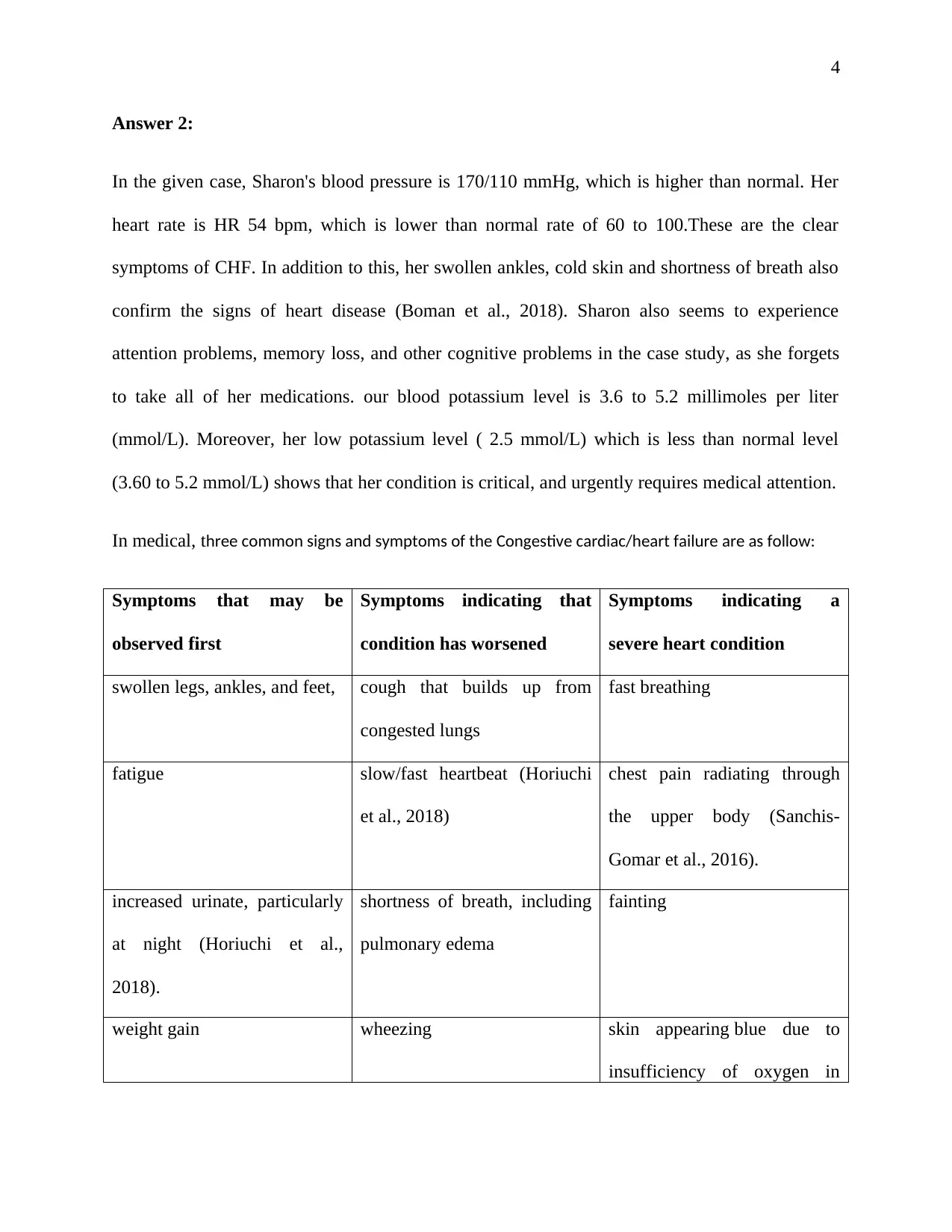
Pathophysiology of heart failure:
The major pathophysiology of heart or cardiac disease is a decrease in the working of the heart
muscle due to congestion or injury (Asgar et al., 2015). The heart of a person with heart disease
has a reduced force of contraction due to overloading of the ventricle, and thus results in
decrease in cardiac output.
Determinants of Cardiac Output
(Boman et al., 2018)
Signs & Symptoms Pathophysiology
Severe ventricular arrhythmias:
Unconsciousness or sudden cardiac death or
The pathogenesis of the arrhythmias can be
divided into two basic methods:
lungs (Sanchis-Gomar et al.,
2016)
Pathophysiology of heart failure:
The major pathophysiology of heart or cardiac disease is a decrease in the working of the heart
muscle due to congestion or injury (Asgar et al., 2015). The heart of a person with heart disease
has a reduced force of contraction due to overloading of the ventricle, and thus results in
decrease in cardiac output.
Determinants of Cardiac Output
(Boman et al., 2018)
Signs & Symptoms Pathophysiology
Severe ventricular arrhythmias:
Unconsciousness or sudden cardiac death or
The pathogenesis of the arrhythmias can be
divided into two basic methods:
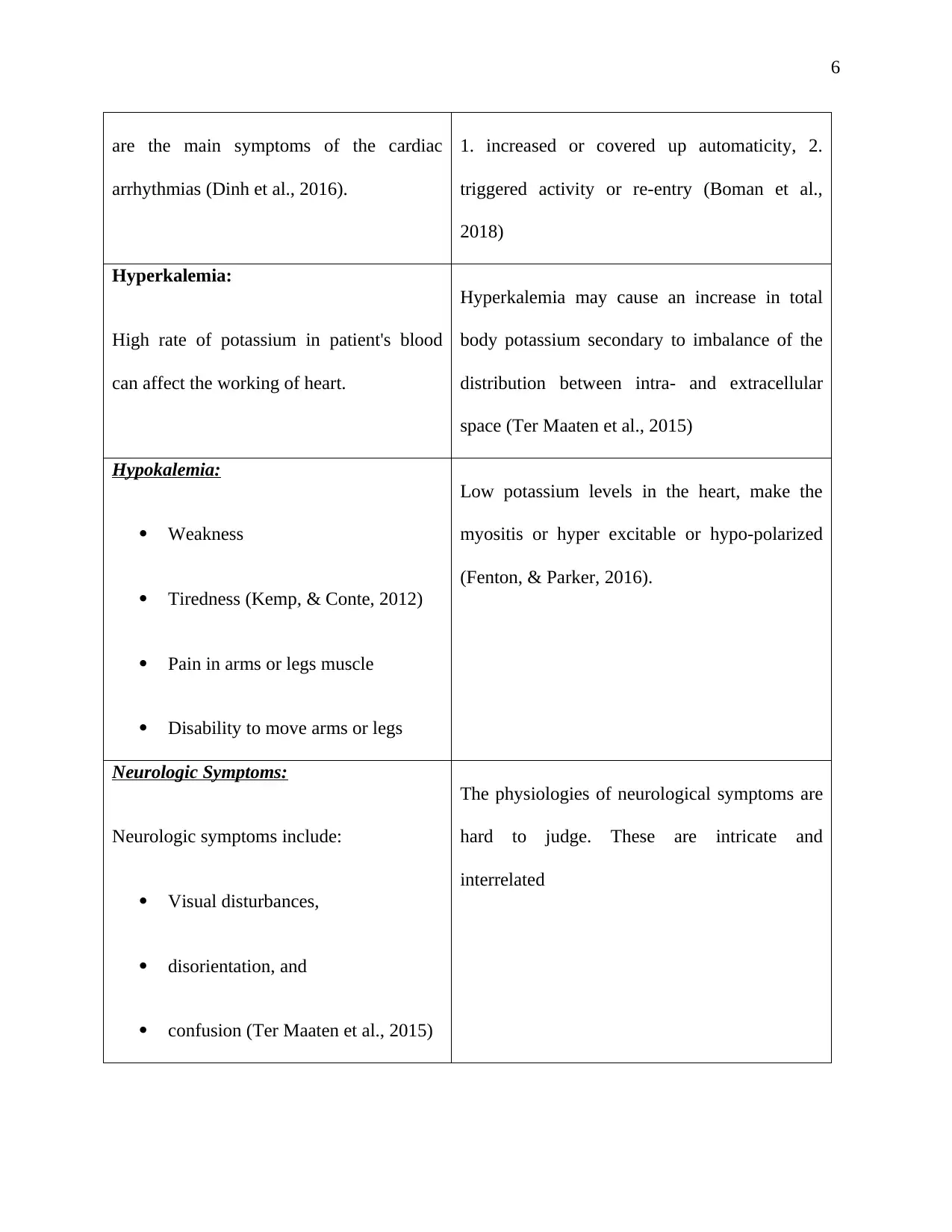
6
are the main symptoms of the cardiac
arrhythmias (Dinh et al., 2016).
1. increased or covered up automaticity, 2.
triggered activity or re-entry (Boman et al.,
2018)
Hyperkalemia:
High rate of potassium in patient's blood
can affect the working of heart.
Hyperkalemia may cause an increase in total
body potassium secondary to imbalance of the
distribution between intra- and extracellular
space (Ter Maaten et al., 2015)
Hypokalemia:
Weakness
Tiredness (Kemp, & Conte, 2012)
Pain in arms or legs muscle
Disability to move arms or legs
Low potassium levels in the heart, make the
myositis or hyper excitable or hypo-polarized
(Fenton, & Parker, 2016).
Neurologic Symptoms:
Neurologic symptoms include:
Visual disturbances,
disorientation, and
confusion (Ter Maaten et al., 2015)
The physiologies of neurological symptoms are
hard to judge. These are intricate and
interrelated
are the main symptoms of the cardiac
arrhythmias (Dinh et al., 2016).
1. increased or covered up automaticity, 2.
triggered activity or re-entry (Boman et al.,
2018)
Hyperkalemia:
High rate of potassium in patient's blood
can affect the working of heart.
Hyperkalemia may cause an increase in total
body potassium secondary to imbalance of the
distribution between intra- and extracellular
space (Ter Maaten et al., 2015)
Hypokalemia:
Weakness
Tiredness (Kemp, & Conte, 2012)
Pain in arms or legs muscle
Disability to move arms or legs
Low potassium levels in the heart, make the
myositis or hyper excitable or hypo-polarized
(Fenton, & Parker, 2016).
Neurologic Symptoms:
Neurologic symptoms include:
Visual disturbances,
disorientation, and
confusion (Ter Maaten et al., 2015)
The physiologies of neurological symptoms are
hard to judge. These are intricate and
interrelated
7
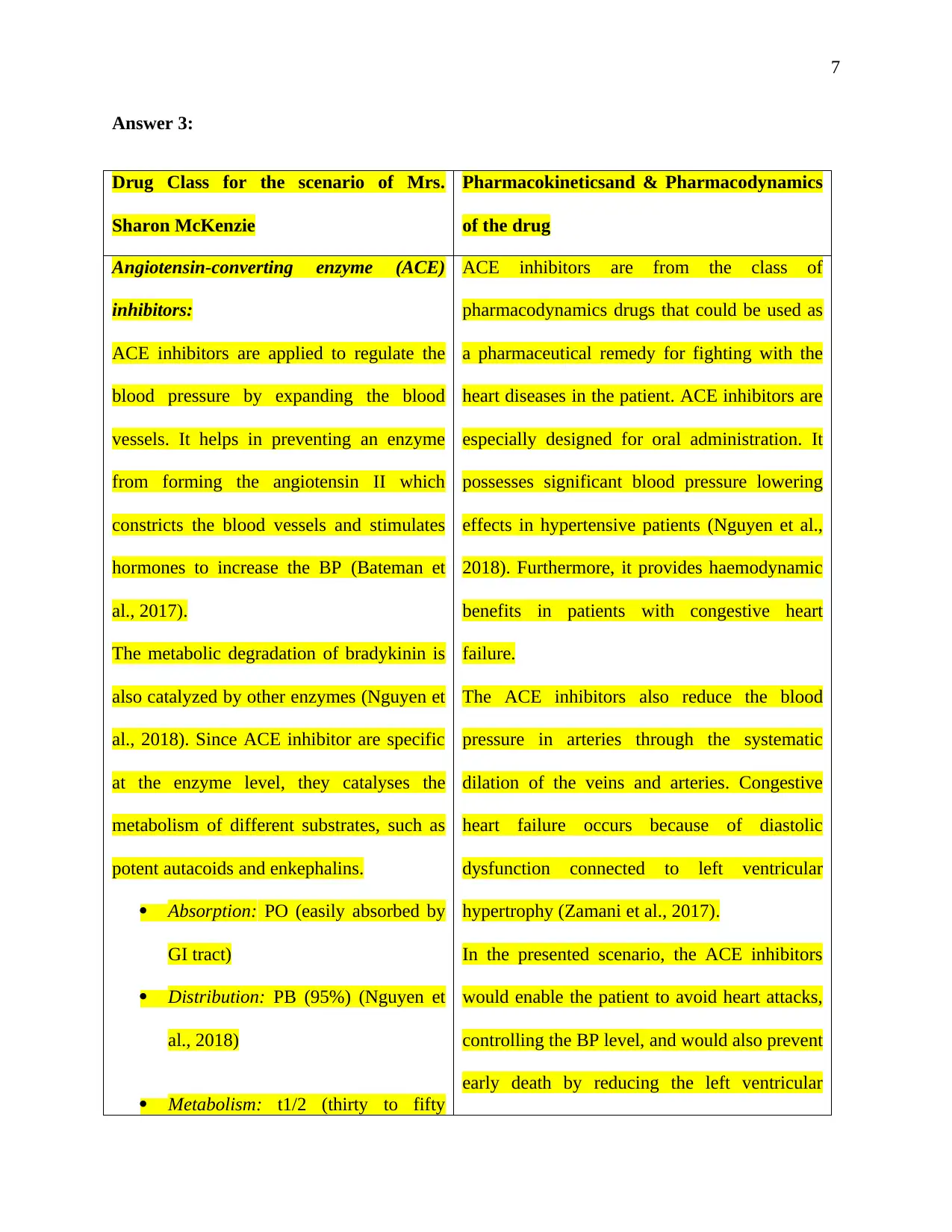
Answer 3:
Drug Class for the scenario of Mrs.
Sharon McKenzie
Pharmacokineticsand & Pharmacodynamics
of the drug
Angiotensin-converting enzyme (ACE)
inhibitors:
ACE inhibitors are applied to regulate the
blood pressure by expanding the blood
vessels. It helps in preventing an enzyme
from forming the angiotensin II which
constricts the blood vessels and stimulates
hormones to increase the BP (Bateman et
al., 2017).
The metabolic degradation of bradykinin is
also catalyzed by other enzymes (Nguyen et
al., 2018). Since ACE inhibitor are specific
at the enzyme level, they catalyses the
metabolism of different substrates, such as
potent autacoids and enkephalins.
Absorption: PO (easily absorbed by
GI tract)
Distribution: PB (95%) (Nguyen et
al., 2018)
Metabolism: t1/2 (thirty to fifty
ACE inhibitors are from the class of
pharmacodynamics drugs that could be used as
a pharmaceutical remedy for fighting with the
heart diseases in the patient. ACE inhibitors are
especially designed for oral administration. It
possesses significant blood pressure lowering
effects in hypertensive patients (Nguyen et al.,
2018). Furthermore, it provides haemodynamic
benefits in patients with congestive heart
failure.
The ACE inhibitors also reduce the blood
pressure in arteries through the systematic
dilation of the veins and arteries. Congestive
heart failure occurs because of diastolic
dysfunction connected to left ventricular
hypertrophy (Zamani et al., 2017).
In the presented scenario, the ACE inhibitors
would enable the patient to avoid heart attacks,
controlling the BP level, and would also prevent
early death by reducing the left ventricular
Answer 3:
Drug Class for the scenario of Mrs.
Sharon McKenzie
Pharmacokineticsand & Pharmacodynamics
of the drug
Angiotensin-converting enzyme (ACE)
inhibitors:
ACE inhibitors are applied to regulate the
blood pressure by expanding the blood
vessels. It helps in preventing an enzyme
from forming the angiotensin II which
constricts the blood vessels and stimulates
hormones to increase the BP (Bateman et
al., 2017).
The metabolic degradation of bradykinin is
also catalyzed by other enzymes (Nguyen et
al., 2018). Since ACE inhibitor are specific
at the enzyme level, they catalyses the
metabolism of different substrates, such as
potent autacoids and enkephalins.
Absorption: PO (easily absorbed by
GI tract)
Distribution: PB (95%) (Nguyen et
al., 2018)
Metabolism: t1/2 (thirty to fifty
ACE inhibitors are from the class of
pharmacodynamics drugs that could be used as
a pharmaceutical remedy for fighting with the
heart diseases in the patient. ACE inhibitors are
especially designed for oral administration. It
possesses significant blood pressure lowering
effects in hypertensive patients (Nguyen et al.,
2018). Furthermore, it provides haemodynamic
benefits in patients with congestive heart
failure.
The ACE inhibitors also reduce the blood
pressure in arteries through the systematic
dilation of the veins and arteries. Congestive
heart failure occurs because of diastolic
dysfunction connected to left ventricular
hypertrophy (Zamani et al., 2017).
In the presented scenario, the ACE inhibitors
would enable the patient to avoid heart attacks,
controlling the BP level, and would also prevent
early death by reducing the left ventricular
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
8
minutes)
Excretion: through feces and urine
(Cohen‐Solal et al., 2017)
hypertrophy in the patient. ACE would also
ensure the balance between the vasodilatory and
natriuretic charactertics of bradykinin and the
vasoconstrictive as well as salt-retentive
properties of Ang II in the patient (Mangoni et
al., 2019)
Answer 4:
A nursing care plan for your Mrs Sharon is given below:
1. Check heart beat, and ECG:
Since Sharon has a low voltage ECG. it is important for the nurse to inform the doctor on the
availability of the outcomes for punctual initiation of medical treatment, in order to prevent the
heart failure (Verweij et al., 2018).
2. Regulate sodium intake:
Since water follows salt, being a heart patient, Sharon needs to get rid of excess fluid on board.
The nurse is also required to educate the patient on proper diet that should incorporate 300 to 600
minutes)
Excretion: through feces and urine
(Cohen‐Solal et al., 2017)
hypertrophy in the patient. ACE would also
ensure the balance between the vasodilatory and
natriuretic charactertics of bradykinin and the
vasoconstrictive as well as salt-retentive
properties of Ang II in the patient (Mangoni et
al., 2019)
Answer 4:
A nursing care plan for your Mrs Sharon is given below:
1. Check heart beat, and ECG:
Since Sharon has a low voltage ECG. it is important for the nurse to inform the doctor on the
availability of the outcomes for punctual initiation of medical treatment, in order to prevent the
heart failure (Verweij et al., 2018).
2. Regulate sodium intake:
Since water follows salt, being a heart patient, Sharon needs to get rid of excess fluid on board.
The nurse is also required to educate the patient on proper diet that should incorporate 300 to 600
9
mg of salt in every serving (Sahlen et al., 2016). Moreover, the patient should be instructed to
stay away from processed foods, and salt in daily meals.
3. Check BNP:
At the stage of chronic heart disease, BP measurement becomes important due to increased SVR.
This would assist Sharon heart to compensate, and prevent hypotension (Verweij et al., 2018).
4. Monitor urine output:
Kidneys reacts to decreased cardiac output by retaining sodium and water. Urine output goes
down during the day because fluid moves into tissues, and goes high at night because fluid
returns to movement when patient is recumbent (Inamdar, & Inamdar, A. 2016). The nurse
should regularly observe decreasing output and intense urine of Sharon.
5. Monitor calf tenderness, swelling, local redness, diminished pedal pulses, or pallor of
extremity:
Venous pooling, Decreased cardiac output, and enforced bed rest raise the threat of
thrombophlebitis in the heart patient. Therefore, the nurse should regularly check on the swelling
and pedal pulses of Sharon.
6. Check supplemental oxygen regularly:
The nurse should ensure the availability of increased oxygen for myocardial update. This would
aid the heart of Sharon to fight adverse impacts of hypoxia (Inamdar, & Inamdar, A. 2016).
7. Check and replace electrolytes:
mg of salt in every serving (Sahlen et al., 2016). Moreover, the patient should be instructed to
stay away from processed foods, and salt in daily meals.
3. Check BNP:
At the stage of chronic heart disease, BP measurement becomes important due to increased SVR.
This would assist Sharon heart to compensate, and prevent hypotension (Verweij et al., 2018).
4. Monitor urine output:
Kidneys reacts to decreased cardiac output by retaining sodium and water. Urine output goes
down during the day because fluid moves into tissues, and goes high at night because fluid
returns to movement when patient is recumbent (Inamdar, & Inamdar, A. 2016). The nurse
should regularly observe decreasing output and intense urine of Sharon.
5. Monitor calf tenderness, swelling, local redness, diminished pedal pulses, or pallor of
extremity:
Venous pooling, Decreased cardiac output, and enforced bed rest raise the threat of
thrombophlebitis in the heart patient. Therefore, the nurse should regularly check on the swelling
and pedal pulses of Sharon.
6. Check supplemental oxygen regularly:
The nurse should ensure the availability of increased oxygen for myocardial update. This would
aid the heart of Sharon to fight adverse impacts of hypoxia (Inamdar, & Inamdar, A. 2016).
7. Check and replace electrolytes:
10
In Cardiac failure, the fluid moves and use of diuretics can change electrolytes (such as chloride
and potassium), which affect heart rate and contractility.
8. Check X-ray:
The chest x-ray of Sharon should be done on regular basis in order to rule out the enlargement of
the cardiac and congestion of pulmonary (Stamp et al., 2018). This would combat the left heart
failure.
9. Check skin for cyanosis and pallor:
Pallor is the sign of reduced peripheral perfusion secondary to insufficient cardiac output, and
anemia. Therefore, the nurse should check Sharon's skin condition on dailybasis (Rogers et al.,
2017).
10. Provide rest, and semirecumbent on chair or in bed.
The nurse should take proper physical care of Sharon in order to improve the efficiency and
functioning of heart, and to reduce the consumption of myocardial oxygen (Sidebottom et al.,
2015.
11. Provide peaceful environment:
The nurse should ensure that Sharon is surrounded by calm atmosphere and respond to the
expression of feelings (Albert, 2016). This would help decreasing her emotional stress,
increasing heart rhythm, and elevate BP.
In Cardiac failure, the fluid moves and use of diuretics can change electrolytes (such as chloride
and potassium), which affect heart rate and contractility.
8. Check X-ray:
The chest x-ray of Sharon should be done on regular basis in order to rule out the enlargement of
the cardiac and congestion of pulmonary (Stamp et al., 2018). This would combat the left heart
failure.
9. Check skin for cyanosis and pallor:
Pallor is the sign of reduced peripheral perfusion secondary to insufficient cardiac output, and
anemia. Therefore, the nurse should check Sharon's skin condition on dailybasis (Rogers et al.,
2017).
10. Provide rest, and semirecumbent on chair or in bed.
The nurse should take proper physical care of Sharon in order to improve the efficiency and
functioning of heart, and to reduce the consumption of myocardial oxygen (Sidebottom et al.,
2015.
11. Provide peaceful environment:
The nurse should ensure that Sharon is surrounded by calm atmosphere and respond to the
expression of feelings (Albert, 2016). This would help decreasing her emotional stress,
increasing heart rhythm, and elevate BP.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
11
References
Albert, N. M. (2016). A systematic review of transitional-care strategies to reduce
rehospitalization in patients with heart failure. Heart & Lung, 45(2), 100-113.
Asgar, A. W., Mack, M. J., & Stone, G. W. (2015). Secondary mitral regurgitation in heart
failure: pathophysiology, prognosis, and therapeutic considerations. Journal of the
American College of Cardiology, 65(12), 1231-1248.
Bateman, Brian T., Elisabetta Patorno, Rishi J. Desai, Ellen W. Seely, Helen Mogun, Sara Z.
Dejene, Michael A. Fischer, Alexander M. Friedman, Sonia Hernandez-Diaz, and Krista
F. Huybrechts. "Angiotensin-converting enzyme inhibitors and the risk of congenital
malformations." Obstetrics and gynecology 129, no. 1 (2017): 174.
Boman, K., Thormark Fröst, F., Bergman, A. C. R., & Olofsson, M. (2018). NTproBNP and ST2
as predictors for all-cause and cardiovascular mortality in elderly patients with symptoms
suggestive for heart failure. Biomarkers, 23(4), 373-379.
Cohen‐Solal, A., Jacobson, A. F., & Piña, I. L. (2017). Beta blocker dose and markers of
sympathetic activation in heart failure patients: interrelationships and prognostic
significance. ESC heart failure, 4(4), 499-506.
Dinh, T. T. H., Bonner, A., Clark, R., Ramsbotham, J., & Hines, S. (2016). The effectiveness of
the teach-back method on adherence and self-management in health education for people
with chronic disease: a systematic review. JBI database of systematic reviews and
implementation reports, 14(1), 210-247.
References
Albert, N. M. (2016). A systematic review of transitional-care strategies to reduce
rehospitalization in patients with heart failure. Heart & Lung, 45(2), 100-113.
Asgar, A. W., Mack, M. J., & Stone, G. W. (2015). Secondary mitral regurgitation in heart
failure: pathophysiology, prognosis, and therapeutic considerations. Journal of the
American College of Cardiology, 65(12), 1231-1248.
Bateman, Brian T., Elisabetta Patorno, Rishi J. Desai, Ellen W. Seely, Helen Mogun, Sara Z.
Dejene, Michael A. Fischer, Alexander M. Friedman, Sonia Hernandez-Diaz, and Krista
F. Huybrechts. "Angiotensin-converting enzyme inhibitors and the risk of congenital
malformations." Obstetrics and gynecology 129, no. 1 (2017): 174.
Boman, K., Thormark Fröst, F., Bergman, A. C. R., & Olofsson, M. (2018). NTproBNP and ST2
as predictors for all-cause and cardiovascular mortality in elderly patients with symptoms
suggestive for heart failure. Biomarkers, 23(4), 373-379.
Cohen‐Solal, A., Jacobson, A. F., & Piña, I. L. (2017). Beta blocker dose and markers of
sympathetic activation in heart failure patients: interrelationships and prognostic
significance. ESC heart failure, 4(4), 499-506.
Dinh, T. T. H., Bonner, A., Clark, R., Ramsbotham, J., & Hines, S. (2016). The effectiveness of
the teach-back method on adherence and self-management in health education for people
with chronic disease: a systematic review. JBI database of systematic reviews and
implementation reports, 14(1), 210-247.
12
Fenton, K. E., & Parker, M. M. (2016). Cardiac function and dysfunction in sepsis. Clinics in
chest medicine, 37(2), 289-298.
Horiuchi, Y., Tanimoto, S., Latif, A. M., Urayama, K. Y., Aoki, J., Yahagi, K., ... & Komiyama,
K. (2018). Identifying novel phenotypes of acute heart failure using cluster analysis of
clinical variables. International journal of cardiology, 262, 57-63.
Huynh, Q. L., Blizzard, C. L., Marwick, T. H., & Negishi, K. (2018). Association of ambient
particulate matter with heart failure incidence and all-cause readmissions in Tasmania: an
observational study. BMJ open, 8(5), e021798.
Inamdar, A., & Inamdar, A. (2016). Heart failure: diagnosis, management and
utilization. Journal of clinical medicine, 5(7), 62.
Kemp, C. D., & Conte, J. V. (2012). The pathophysiology of heart failure. Cardiovascular
Pathology, 21(5), 365-371.
Mangoni, A. A., & Jarmuzewska, E. A. (2019). The influence of heart failure on the
pharmacokinetics of cardiovascular and non‐cardiovascular drugs: a critical appraisal of
the evidence. British journal of clinical pharmacology, 85(1), 20-36.
Nguyen, T., Lanh, N. V., Viet, V. M., Phuc, L. H., Pham, T. N., Duong, K., ... & Rigatelli, G.
(2018). Advanced Strategies in the Diagnosis and Treatment of Patients with Coronary
Artery Disease and Heart Failure: When Heart Failure Causes Ischemia and Angiotensin
Converting Enzyme Inhibitor and Betablockers Helps in Diuresis. Current
pharmaceutical design, 24(4), 511-516.
Fenton, K. E., & Parker, M. M. (2016). Cardiac function and dysfunction in sepsis. Clinics in
chest medicine, 37(2), 289-298.
Horiuchi, Y., Tanimoto, S., Latif, A. M., Urayama, K. Y., Aoki, J., Yahagi, K., ... & Komiyama,
K. (2018). Identifying novel phenotypes of acute heart failure using cluster analysis of
clinical variables. International journal of cardiology, 262, 57-63.
Huynh, Q. L., Blizzard, C. L., Marwick, T. H., & Negishi, K. (2018). Association of ambient
particulate matter with heart failure incidence and all-cause readmissions in Tasmania: an
observational study. BMJ open, 8(5), e021798.
Inamdar, A., & Inamdar, A. (2016). Heart failure: diagnosis, management and
utilization. Journal of clinical medicine, 5(7), 62.
Kemp, C. D., & Conte, J. V. (2012). The pathophysiology of heart failure. Cardiovascular
Pathology, 21(5), 365-371.
Mangoni, A. A., & Jarmuzewska, E. A. (2019). The influence of heart failure on the
pharmacokinetics of cardiovascular and non‐cardiovascular drugs: a critical appraisal of
the evidence. British journal of clinical pharmacology, 85(1), 20-36.
Nguyen, T., Lanh, N. V., Viet, V. M., Phuc, L. H., Pham, T. N., Duong, K., ... & Rigatelli, G.
(2018). Advanced Strategies in the Diagnosis and Treatment of Patients with Coronary
Artery Disease and Heart Failure: When Heart Failure Causes Ischemia and Angiotensin
Converting Enzyme Inhibitor and Betablockers Helps in Diuresis. Current
pharmaceutical design, 24(4), 511-516.
13
Nieminen, M. S., Dickstein, K., Fonseca, C., Serrano, J. M., Parissis, J., Fedele, F., ... & Brito, D.
(2015). The patient perspective: quality of life in advanced heart failure with frequent
hospitalisations. International journal of cardiology, 191, 256-264.
O’Neil, A., Fisher, A. J., Kibbey, K. J., Jacka, F. N., Kotowicz, M. A., Williams, L. J., ... &
Pasco, J. A. (2016). Depression is a risk factor for incident coronary heart disease in
women: An 18-year longitudinal study. Journal of affective disorders, 196, 117-124.
Rogers, J. G., Patel, C. B., Mentz, R. J., Granger, B. B., Steinhauser, K. E., Fiuzat, M., ... &
Yang, H. (2017). Palliative care in heart failure: the PAL-HF randomized, controlled
clinical trial. Journal of the American College of Cardiology, 70(3), 331-341.
Sahlen, K. G., Boman, K., & Brännström, M. (2016). A cost-effectiveness study of person-
centered integrated heart failure and palliative home care: based on a randomized
controlled trial. Palliative medicine, 30(3), 296-302.
Sanchis-Gomar, F., Perez-Quilis, C., Leischik, R., & Lucia, A. (2016). Epidemiology of
coronary heart disease and acute coronary syndrome. Annals of translational
medicine, 4(13).
Sevilla-Cazes, J., Ahmad, F. S., Bowles, K. H., Jaskowiak, A., Gallagher, T., Goldberg, L. R., ...
& Kimmel, S. E. (2018). Heart Failure Home Management Challenges and Reasons for
Readmission: a Qualitative Study to Understand the Patient’s Perspective. Journal of
general internal medicine, 33(10), 1700-1707.
Nieminen, M. S., Dickstein, K., Fonseca, C., Serrano, J. M., Parissis, J., Fedele, F., ... & Brito, D.
(2015). The patient perspective: quality of life in advanced heart failure with frequent
hospitalisations. International journal of cardiology, 191, 256-264.
O’Neil, A., Fisher, A. J., Kibbey, K. J., Jacka, F. N., Kotowicz, M. A., Williams, L. J., ... &
Pasco, J. A. (2016). Depression is a risk factor for incident coronary heart disease in
women: An 18-year longitudinal study. Journal of affective disorders, 196, 117-124.
Rogers, J. G., Patel, C. B., Mentz, R. J., Granger, B. B., Steinhauser, K. E., Fiuzat, M., ... &
Yang, H. (2017). Palliative care in heart failure: the PAL-HF randomized, controlled
clinical trial. Journal of the American College of Cardiology, 70(3), 331-341.
Sahlen, K. G., Boman, K., & Brännström, M. (2016). A cost-effectiveness study of person-
centered integrated heart failure and palliative home care: based on a randomized
controlled trial. Palliative medicine, 30(3), 296-302.
Sanchis-Gomar, F., Perez-Quilis, C., Leischik, R., & Lucia, A. (2016). Epidemiology of
coronary heart disease and acute coronary syndrome. Annals of translational
medicine, 4(13).
Sevilla-Cazes, J., Ahmad, F. S., Bowles, K. H., Jaskowiak, A., Gallagher, T., Goldberg, L. R., ...
& Kimmel, S. E. (2018). Heart Failure Home Management Challenges and Reasons for
Readmission: a Qualitative Study to Understand the Patient’s Perspective. Journal of
general internal medicine, 33(10), 1700-1707.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
14
Sidebottom, A. C., Jorgenson, A., Richards, H., Kirven, J., & Sillah, A. (2015). Inpatient
palliative care for patients with acute heart failure: outcomes from a randomized
trial. Journal of palliative medicine, 18(2), 134-142.
Stamp, K. D., Prasun, M., Lee, C. S., Jaarsma, T., Piano, M. R., & Albert, N. M. (2018). Nursing
research in heart failure care: a position statement of the american association of heart
failure nurses (AAHFN). Heart & Lung, 47(2), 169-175.
Ter Maaten, J. M., Valente, M. A., Damman, K., Hillege, H. L., Navis, G., & Voors, A. A.
(2015). Diuretic response in acute heart failure—pathophysiology, evaluation, and
therapy. Nature Reviews Cardiology, 12(3), 184.
Verweij, L., Jepma, P., Buurman, B. M., Latour, C. H. M., Engelbert, R. H. H., Ter Riet, G., ... &
op Reimer, W. S. (2018). The cardiac care bridge program: design of a randomized trial
of nurse-coordinated transitional care in older hospitalized cardiac patients at high risk of
readmission and mortality. BMC health services research, 18(1), 508.
Woodruffe, S., Neubeck, L., Clark, R. A., Gray, K., Ferry, C., Finan, J., ... & Briffa, T. G.
(2015). Australian Cardiovascular Health and Rehabilitation Association (ACRA) core
components of cardiovascular disease secondary prevention and cardiac rehabilitation
2014. Heart, Lung and Circulation, 24(5), 430-441.
Zamani, P., Tan, V., Soto-Calderon, H., Beraun, M., Brandimarto, J. A., Trieu, L., ... &
Margulies, K. B. (2017). Pharmacokinetics and pharmacodynamics of inorganic nitrate in
heart failure with preserved ejection fraction. Circulation research, 120(7), 1151-1161.
Sidebottom, A. C., Jorgenson, A., Richards, H., Kirven, J., & Sillah, A. (2015). Inpatient
palliative care for patients with acute heart failure: outcomes from a randomized
trial. Journal of palliative medicine, 18(2), 134-142.
Stamp, K. D., Prasun, M., Lee, C. S., Jaarsma, T., Piano, M. R., & Albert, N. M. (2018). Nursing
research in heart failure care: a position statement of the american association of heart
failure nurses (AAHFN). Heart & Lung, 47(2), 169-175.
Ter Maaten, J. M., Valente, M. A., Damman, K., Hillege, H. L., Navis, G., & Voors, A. A.
(2015). Diuretic response in acute heart failure—pathophysiology, evaluation, and
therapy. Nature Reviews Cardiology, 12(3), 184.
Verweij, L., Jepma, P., Buurman, B. M., Latour, C. H. M., Engelbert, R. H. H., Ter Riet, G., ... &
op Reimer, W. S. (2018). The cardiac care bridge program: design of a randomized trial
of nurse-coordinated transitional care in older hospitalized cardiac patients at high risk of
readmission and mortality. BMC health services research, 18(1), 508.
Woodruffe, S., Neubeck, L., Clark, R. A., Gray, K., Ferry, C., Finan, J., ... & Briffa, T. G.
(2015). Australian Cardiovascular Health and Rehabilitation Association (ACRA) core
components of cardiovascular disease secondary prevention and cardiac rehabilitation
2014. Heart, Lung and Circulation, 24(5), 430-441.
Zamani, P., Tan, V., Soto-Calderon, H., Beraun, M., Brandimarto, J. A., Trieu, L., ... &
Margulies, K. B. (2017). Pharmacokinetics and pharmacodynamics of inorganic nitrate in
heart failure with preserved ejection fraction. Circulation research, 120(7), 1151-1161.

15
Zipes, D. P., Libby, P., Bonow, R. O., Mann, D. L., & Tomaselli, G. F. (2018). Braunwald's
Heart Disease E-Book: A Textbook of Cardiovascular Medicine. USA: Elsevier Health
Sciences.
Zipes, D. P., Libby, P., Bonow, R. O., Mann, D. L., & Tomaselli, G. F. (2018). Braunwald's
Heart Disease E-Book: A Textbook of Cardiovascular Medicine. USA: Elsevier Health
Sciences.
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.



