Implementing Safe Work Practices in Healthcare: A Detailed Report
VerifiedAdded on 2023/06/13
|22
|4573
|378
Report
AI Summary
This report comprehensively addresses safe work practices within healthcare settings. It begins by defining hazards and risks, providing examples within client care scenarios, and detailing the implications of poor manual handling and emergency planning. The importance of hazard reporting and standard precautions like hand hygiene and PPE usage are emphasized, along with additional precautions for infectious diseases such as diarrhea and MRSA. The report further explores risks associated with long driving hours for healthcare workers and the duty of care owed by both employers and employees. Case studies illustrate practical application of these principles, including managing MRSA-infected clients and handling aggressive patient behavior. The document includes risk assessment control forms and matrices to evaluate and mitigate workplace hazards. Finally, it touches upon compliance inspections and necessary actions for non-compliance, providing a holistic view of maintaining safety standards in healthcare.
Safe work practices
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
TABLE OF CONTENT
1.1.................................................................................................................................................4
1.2.................................................................................................................................................4
1.3.................................................................................................................................................4
1.4.................................................................................................................................................4
2....................................................................................................................................................5
3 ...................................................................................................................................................5
4.1.................................................................................................................................................6
4.2.................................................................................................................................................6
6....................................................................................................................................................6
6....................................................................................................................................................7
7....................................................................................................................................................7
7.1.................................................................................................................................................7
8....................................................................................................................................................7
Task 2...............................................................................................................................................8
1....................................................................................................................................................8
2....................................................................................................................................................8
3....................................................................................................................................................8
4....................................................................................................................................................8
5....................................................................................................................................................8
6....................................................................................................................................................9
7. Hand hygiene:..........................................................................................................................9
8. Resident room:.........................................................................................................................9
9. What to report:.........................................................................................................................9
10. Personal risk:..........................................................................................................................9
11. Duty of care:........................................................................................................................10
CASE STUDY 2............................................................................................................................10
1. Report this situations:............................................................................................................10
2. Future care:............................................................................................................................10
3. Warning sign:.........................................................................................................................10
4. Risk assessment:....................................................................................................................11
1.1.................................................................................................................................................4
1.2.................................................................................................................................................4
1.3.................................................................................................................................................4
1.4.................................................................................................................................................4
2....................................................................................................................................................5
3 ...................................................................................................................................................5
4.1.................................................................................................................................................6
4.2.................................................................................................................................................6
6....................................................................................................................................................6
6....................................................................................................................................................7
7....................................................................................................................................................7
7.1.................................................................................................................................................7
8....................................................................................................................................................7
Task 2...............................................................................................................................................8
1....................................................................................................................................................8
2....................................................................................................................................................8
3....................................................................................................................................................8
4....................................................................................................................................................8
5....................................................................................................................................................8
6....................................................................................................................................................9
7. Hand hygiene:..........................................................................................................................9
8. Resident room:.........................................................................................................................9
9. What to report:.........................................................................................................................9
10. Personal risk:..........................................................................................................................9
11. Duty of care:........................................................................................................................10
CASE STUDY 2............................................................................................................................10
1. Report this situations:............................................................................................................10
2. Future care:............................................................................................................................10
3. Warning sign:.........................................................................................................................10
4. Risk assessment:....................................................................................................................11
6. reduce risk in the future:........................................................................................................11
TASK 3..........................................................................................................................................11
PART A:....................................................................................................................................11
2. Discussing each policy and procedures with relevant legislation and standards:..................11
PART B..........................................................................................................................................12
PART C..........................................................................................................................................12
TASK 4..........................................................................................................................................15
1. finding any non compliance during the inspection:...............................................................15
2. what to do with non compliance item:...................................................................................16
3. How often these area need to be inspected:..........................................................................16
TASK 5..........................................................................................................................................16
1. Risk assessment control form:...............................................................................................16
2. Risk matrix:............................................................................................................................17
3. Risk assessment control form:...............................................................................................18
CONCLUSION..............................................................................................................................20
REFERENCES................................................................................................................................1
TASK 3..........................................................................................................................................11
PART A:....................................................................................................................................11
2. Discussing each policy and procedures with relevant legislation and standards:..................11
PART B..........................................................................................................................................12
PART C..........................................................................................................................................12
TASK 4..........................................................................................................................................15
1. finding any non compliance during the inspection:...............................................................15
2. what to do with non compliance item:...................................................................................16
3. How often these area need to be inspected:..........................................................................16
TASK 5..........................................................................................................................................16
1. Risk assessment control form:...............................................................................................16
2. Risk matrix:............................................................................................................................17
3. Risk assessment control form:...............................................................................................18
CONCLUSION..............................................................................................................................20
REFERENCES................................................................................................................................1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1.1
Ans- A hazard refers to potential sources that might create harm and provide adverse health
effects over an individual.
1.2
Ans- Risk illustrates the possibility of something bad happening as it involves uncertainty about
the implications that can be faced due to an activity with respect to something that valued by an
individual by often focusing towards the pessimistic and undesirable consequences (Hughes and
Afanuh, 2021).
1.3
Is this a hazard? Tick each correct answer
Working with client in their homes
A strained back ✓
Showering a client
Lifting a box ✓
Working long hours ✓
Stress ✓
1.4
(a) Poor manual handling can result into injuries, long term musculoskeletal disorders and joint
pain issues. Moreover, one can also have to face stress and anxiety.
(b) Inappropriate way of handling mobility equipment might lead to underarm crutches that also
lead towards a condition of crutch paralysis.
One can have a risk of cuts and punctures, chemical burns, electric shocks along with
exposure of excessive vibration and noise.
Ans- A hazard refers to potential sources that might create harm and provide adverse health
effects over an individual.
1.2
Ans- Risk illustrates the possibility of something bad happening as it involves uncertainty about
the implications that can be faced due to an activity with respect to something that valued by an
individual by often focusing towards the pessimistic and undesirable consequences (Hughes and
Afanuh, 2021).
1.3
Is this a hazard? Tick each correct answer
Working with client in their homes
A strained back ✓
Showering a client
Lifting a box ✓
Working long hours ✓
Stress ✓
1.4
(a) Poor manual handling can result into injuries, long term musculoskeletal disorders and joint
pain issues. Moreover, one can also have to face stress and anxiety.
(b) Inappropriate way of handling mobility equipment might lead to underarm crutches that also
lead towards a condition of crutch paralysis.
One can have a risk of cuts and punctures, chemical burns, electric shocks along with
exposure of excessive vibration and noise.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Poorly prepared plans, will lead towards disorganized evacuation or emergency responses
that resulting into injury, confu6.sion as well as property damage.
(e) The management team will unable to aid from proper risk assessment and identify effective
solutions to potential risks.
(f) Overall spreading of the infection that might lead to drastic situation.
2.
Ans- Provide adequate means of escape
Outline clear pathways to exit doors
Install smoke detection system
Conduct regular fire drills
Use flame retardant material in interiors
Keep building plans handy.
3
(a) Reporting of hazards provide an appropriate solution and ways to remove or mitigate
something from which others are highly unaware as once the hazard have been identified, they
can be handled in proper manner along with reduces or eliminate the risk of death or injury.
3.1 (a) Yes, the supervisor must report this issue as a work health and safety issue to
management because this forbidding air conditioners lead to serious hazards as the staff
members are working in front of fire which creates the whole environment hot for them which
might create harmful impacts over the workers who are working over there.
◦ (b) The supervisor must report the incident to the WHS in order to resolve the issue at
utmost priority level.
◦ (c) Initially by providing fundamental information.
Take note of any damages and injuries.
Identify affected people
Take action
that resulting into injury, confu6.sion as well as property damage.
(e) The management team will unable to aid from proper risk assessment and identify effective
solutions to potential risks.
(f) Overall spreading of the infection that might lead to drastic situation.
2.
Ans- Provide adequate means of escape
Outline clear pathways to exit doors
Install smoke detection system
Conduct regular fire drills
Use flame retardant material in interiors
Keep building plans handy.
3
(a) Reporting of hazards provide an appropriate solution and ways to remove or mitigate
something from which others are highly unaware as once the hazard have been identified, they
can be handled in proper manner along with reduces or eliminate the risk of death or injury.
3.1 (a) Yes, the supervisor must report this issue as a work health and safety issue to
management because this forbidding air conditioners lead to serious hazards as the staff
members are working in front of fire which creates the whole environment hot for them which
might create harmful impacts over the workers who are working over there.
◦ (b) The supervisor must report the incident to the WHS in order to resolve the issue at
utmost priority level.
◦ (c) Initially by providing fundamental information.
Take note of any damages and injuries.
Identify affected people
Take action
4.1
Standard precautions are the primal level of infection control that should be utilized in the care of
the patients for all the time (Baguma, 2021). This will enable to reduce risks of transmission of
microorganisms from recognized and non-recognized sources of infection. It has been used for
all patient care as they are based upon risk assessment and make use of common sense practices
and personal protection equipments to protect healthcare providers from infection. For example
hand hygiene before and after patient contact, use personal protective equipments such as gloves,
gowns, etc. and safe use and disposal of sharps.
4.2
Additional precautions are infection prevention and control measures as well as practices
required in addition to routine practices. It has been applied when patients have a known and
suspected infectious agent that might not be contained using standard precaution alone. Three
examples of additional precautions are contact precaution, droplet precaution and airborne
precaution.
◦ The client has the responsibility to avoid contacting the worker as she is suffering
from diarrhoea and not allowed him to do home visit as well.
◦ The symptoms show the disease of diarrhoea.
◦ The risk of spreading diarrhoea should be minimized by washing hands often, taking
good hygiene and using improved sanitization measures.
◦ Getting entry within the home premises of the client create risk to the worker as she is
suffering from diarrhoea which is a communicable disease that can be easily spread
specially through direct contact with vomit and faeces from infected people (Beutel,
2018). It can also spread through contact with contaminated surface or object.
6.
Ans- Three things that help an individual to remain updated with safe work practices are:
Keeping tidy work space
Inspection of equipments
Standard precautions are the primal level of infection control that should be utilized in the care of
the patients for all the time (Baguma, 2021). This will enable to reduce risks of transmission of
microorganisms from recognized and non-recognized sources of infection. It has been used for
all patient care as they are based upon risk assessment and make use of common sense practices
and personal protection equipments to protect healthcare providers from infection. For example
hand hygiene before and after patient contact, use personal protective equipments such as gloves,
gowns, etc. and safe use and disposal of sharps.
4.2
Additional precautions are infection prevention and control measures as well as practices
required in addition to routine practices. It has been applied when patients have a known and
suspected infectious agent that might not be contained using standard precaution alone. Three
examples of additional precautions are contact precaution, droplet precaution and airborne
precaution.
◦ The client has the responsibility to avoid contacting the worker as she is suffering
from diarrhoea and not allowed him to do home visit as well.
◦ The symptoms show the disease of diarrhoea.
◦ The risk of spreading diarrhoea should be minimized by washing hands often, taking
good hygiene and using improved sanitization measures.
◦ Getting entry within the home premises of the client create risk to the worker as she is
suffering from diarrhoea which is a communicable disease that can be easily spread
specially through direct contact with vomit and faeces from infected people (Beutel,
2018). It can also spread through contact with contaminated surface or object.
6.
Ans- Three things that help an individual to remain updated with safe work practices are:
Keeping tidy work space
Inspection of equipments
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Record keeping
6.
7.
Ans- Risks associated with long driving hours are:
Risk 1: Damage to musculoskeletal system which can be controlled by maintaining erect
position of back and neck, keep wrists as neutral as possible, avoid neck bending and avoiding
static position for prolonged period.
Risk 2: Heart problems as long sitting hours create stress over the body that fluctuates the blood
pressure and create heart problems. In order to mitigate the damages from prolonged driving, one
should take rests in between the drives and keep focus towards their posture.
7.1
Risk 1: As Kellie works as transporting client with disabilities, she has a risk of fall from the
vehicle which is due to mobility issues, balance disorder, chronic illness and impaired vision.
The risk can be controlled by staying physically fit, getting enough sleep and stand up slowly.
Risk 2: Risk of getting delay also might be faced by the Kellie and for this she have to manage
their time accordingly so that she can reach to their clients within appropriate time duration. She
must prioritize things in planned manner.
8.
Ans- Appropriate lifting of heavy objects in a way which has been shown in the above diagram
enables an individual to reduce the risks of injury. It also promoted back health and ensures that
the work will be completed in highly safe manner.
◦ No, the employer does not show a duty of care towards care worker as a care worker
have to fulfil the role which is about assist to vulnerable people to live comfortably as
6.
7.
Ans- Risks associated with long driving hours are:
Risk 1: Damage to musculoskeletal system which can be controlled by maintaining erect
position of back and neck, keep wrists as neutral as possible, avoid neck bending and avoiding
static position for prolonged period.
Risk 2: Heart problems as long sitting hours create stress over the body that fluctuates the blood
pressure and create heart problems. In order to mitigate the damages from prolonged driving, one
should take rests in between the drives and keep focus towards their posture.
7.1
Risk 1: As Kellie works as transporting client with disabilities, she has a risk of fall from the
vehicle which is due to mobility issues, balance disorder, chronic illness and impaired vision.
The risk can be controlled by staying physically fit, getting enough sleep and stand up slowly.
Risk 2: Risk of getting delay also might be faced by the Kellie and for this she have to manage
their time accordingly so that she can reach to their clients within appropriate time duration. She
must prioritize things in planned manner.
8.
Ans- Appropriate lifting of heavy objects in a way which has been shown in the above diagram
enables an individual to reduce the risks of injury. It also promoted back health and ensures that
the work will be completed in highly safe manner.
◦ No, the employer does not show a duty of care towards care worker as a care worker
have to fulfil the role which is about assist to vulnerable people to live comfortably as
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
well as providing appropriate assistance to the workers in order to avoid any
damages.
◦ No, the care worker also does not fulfil the duty of care as she have to ask about the
manual or for training requirements before handling the client with a disability in
order to avoid accident or injury.
Task 2
1.
Ans- MRSA is a kind of infection which is occurred when there is a cut or break within the skin.
It is highly contagious and can be spread through direct contact with infectious person. This
spread through contact with a contaminated wound or by sharing personal items such as towels,
razors, etc. that have touched infected skin or surface (Xiaojun and Ken, 2020).
2.
Ans- The procedures for working with MRSA infection client is available at the hospitals and
healthcare settings which include nursing homes and dialysis centres.
3.
Ans- Yes the standard precautions has been utilized within the MRSA infection issues. For
example using contact precautions from personal touchable things such as gloves, gowns, etc.
and by using hand sanitizer. On the other hand, the additional precautions could not be used for
MRSA patient as it is not airborne virus. The care provider have to use contact precautions while
caring for patient with MRSA.
4.
Ans- The care provider must wash their hands before and after providing care to the MRSA
resident and during all the five moments of hand hygiene.
damages.
◦ No, the care worker also does not fulfil the duty of care as she have to ask about the
manual or for training requirements before handling the client with a disability in
order to avoid accident or injury.
Task 2
1.
Ans- MRSA is a kind of infection which is occurred when there is a cut or break within the skin.
It is highly contagious and can be spread through direct contact with infectious person. This
spread through contact with a contaminated wound or by sharing personal items such as towels,
razors, etc. that have touched infected skin or surface (Xiaojun and Ken, 2020).
2.
Ans- The procedures for working with MRSA infection client is available at the hospitals and
healthcare settings which include nursing homes and dialysis centres.
3.
Ans- Yes the standard precautions has been utilized within the MRSA infection issues. For
example using contact precautions from personal touchable things such as gloves, gowns, etc.
and by using hand sanitizer. On the other hand, the additional precautions could not be used for
MRSA patient as it is not airborne virus. The care provider have to use contact precautions while
caring for patient with MRSA.
4.
Ans- The care provider must wash their hands before and after providing care to the MRSA
resident and during all the five moments of hand hygiene.
5.
Ans- The personal protective equipments required at the time of handling MRSA patient include
gloves and gowns provided by healthcare personnel is highly recommended avoiding further
infection to care provider.
6.
Ans- The correct procedure to remove PPE is if mask is used, remove gloves using glove to
glove technique and skin to skin technique and discard immediately. Perform hand hygiene. If a
gown is used untie necktie's first, then waist ties over the gown (Bouchaut and et.al., 2021).
7. Hand hygiene:
At first resident and her visitor should avoid social contacting and try to avoid visiting them in
their home. Secondly they need to wear PPE kits and other safety equipments such as gloves,
mask and hand sanitizer to stop spread of MARS.
8. Resident room:
Resident room should be clean in proper manner, there are certain steps:
At first, room cleaner have to wear PPE and other personal safety equipment to ensure
safety.
Secondly, worker or cleaner need to find transmission of infection and identify those
droplets that can be dangerous.
At last, worker or cleaner need to use cleaning chemical like disinfectants, concentration
and other chemical that reduce power of infection and then room should be cleaned with
dust and aerosols control procedure.
9. What to report:
In this situation safety protocol need to be recorded, worker and healthcare professional need to
ensure personal as well as safety of patient. Patient health and status need to be recorded, this
simply means care worker need to report health status of patient.
Ans- The personal protective equipments required at the time of handling MRSA patient include
gloves and gowns provided by healthcare personnel is highly recommended avoiding further
infection to care provider.
6.
Ans- The correct procedure to remove PPE is if mask is used, remove gloves using glove to
glove technique and skin to skin technique and discard immediately. Perform hand hygiene. If a
gown is used untie necktie's first, then waist ties over the gown (Bouchaut and et.al., 2021).
7. Hand hygiene:
At first resident and her visitor should avoid social contacting and try to avoid visiting them in
their home. Secondly they need to wear PPE kits and other safety equipments such as gloves,
mask and hand sanitizer to stop spread of MARS.
8. Resident room:
Resident room should be clean in proper manner, there are certain steps:
At first, room cleaner have to wear PPE and other personal safety equipment to ensure
safety.
Secondly, worker or cleaner need to find transmission of infection and identify those
droplets that can be dangerous.
At last, worker or cleaner need to use cleaning chemical like disinfectants, concentration
and other chemical that reduce power of infection and then room should be cleaned with
dust and aerosols control procedure.
9. What to report:
In this situation safety protocol need to be recorded, worker and healthcare professional need to
ensure personal as well as safety of patient. Patient health and status need to be recorded, this
simply means care worker need to report health status of patient.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

10. Personal risk:
Risk of infection: taking care of infectious person have certain risk associated, this means
worker personal will going to feel fear while working this resident and their performance
might be impacted.
Exposure: risk of exposure, this simply Salih, F.I., Bakar, N.A.A., Hassan, N.H., Yahya,
F., Kama, N. and Shah, J., 2019. IOT security risk management model for healthcare
industry. Malaysian Journal of Computer Science, pp.131-144.means worker might
exposure to infectious environment and get sick, personally it is very risk for worker
because one small mistake can impact their personal life and health.
11. Duty of care:
Fair treatment: fair treatment is one of the most import duty which care worker need to provide
to resident, this simply means fairly taking care and avoiding any kind of unethical behaviour
that might impact health of resident (Lancet, 2020).
Safeguarding: safeguarding is another important duty of care provider which they need to
provide, this means care provider will ensure patient's safety and safeguarding them from any
kind of risk including risk of getting infection or exposure.
CASE STUDY 2
1. Report this situations:
Taking immediate situations: care provider need to take action immediate and report this
situation to manager and inform them about aggressive behaviour of patient.
Report to the authorities: after informing to manager, care provider need to inform and report
these situations to authorities who has sent them for care and dressing of patient. Reporting
should include aggressive behaviours of patient and immediate help to control this situation.
2. Future care:
Care provider need to record observation of these situations and behaviour of patient to avoid
any future incident that might impact patient and care provider. Recording of observation will
help them in certain ways, these are:Card, A.J. and Klein, V.R., 2016
More careful: observation of previous incident will allow care provider to be careful in next
operation and allow them to be effective.
Handling: if care provider is aware about aggressive behaviours of patient then they will be more
serious and handle patient with care and other ethical procedures.
Risk of infection: taking care of infectious person have certain risk associated, this means
worker personal will going to feel fear while working this resident and their performance
might be impacted.
Exposure: risk of exposure, this simply Salih, F.I., Bakar, N.A.A., Hassan, N.H., Yahya,
F., Kama, N. and Shah, J., 2019. IOT security risk management model for healthcare
industry. Malaysian Journal of Computer Science, pp.131-144.means worker might
exposure to infectious environment and get sick, personally it is very risk for worker
because one small mistake can impact their personal life and health.
11. Duty of care:
Fair treatment: fair treatment is one of the most import duty which care worker need to provide
to resident, this simply means fairly taking care and avoiding any kind of unethical behaviour
that might impact health of resident (Lancet, 2020).
Safeguarding: safeguarding is another important duty of care provider which they need to
provide, this means care provider will ensure patient's safety and safeguarding them from any
kind of risk including risk of getting infection or exposure.
CASE STUDY 2
1. Report this situations:
Taking immediate situations: care provider need to take action immediate and report this
situation to manager and inform them about aggressive behaviour of patient.
Report to the authorities: after informing to manager, care provider need to inform and report
these situations to authorities who has sent them for care and dressing of patient. Reporting
should include aggressive behaviours of patient and immediate help to control this situation.
2. Future care:
Care provider need to record observation of these situations and behaviour of patient to avoid
any future incident that might impact patient and care provider. Recording of observation will
help them in certain ways, these are:Card, A.J. and Klein, V.R., 2016
More careful: observation of previous incident will allow care provider to be careful in next
operation and allow them to be effective.
Handling: if care provider is aware about aggressive behaviours of patient then they will be more
serious and handle patient with care and other ethical procedures.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
3. Warning sign:
Warming from wife: wife of client warned care provider about aggressive behaviours of client
and highlighted that he is in angry mood that impact care provider. Her wife informed that he
remain gentle throughout the day but today he is aggressive and might harm care provider (Card
and Klein, 2016).
Warning from client: client have given warning to care provider before dressing, this should be
taken seriously because person with aggressive behaviour only provide one warning and their
behaviour become aggressive.
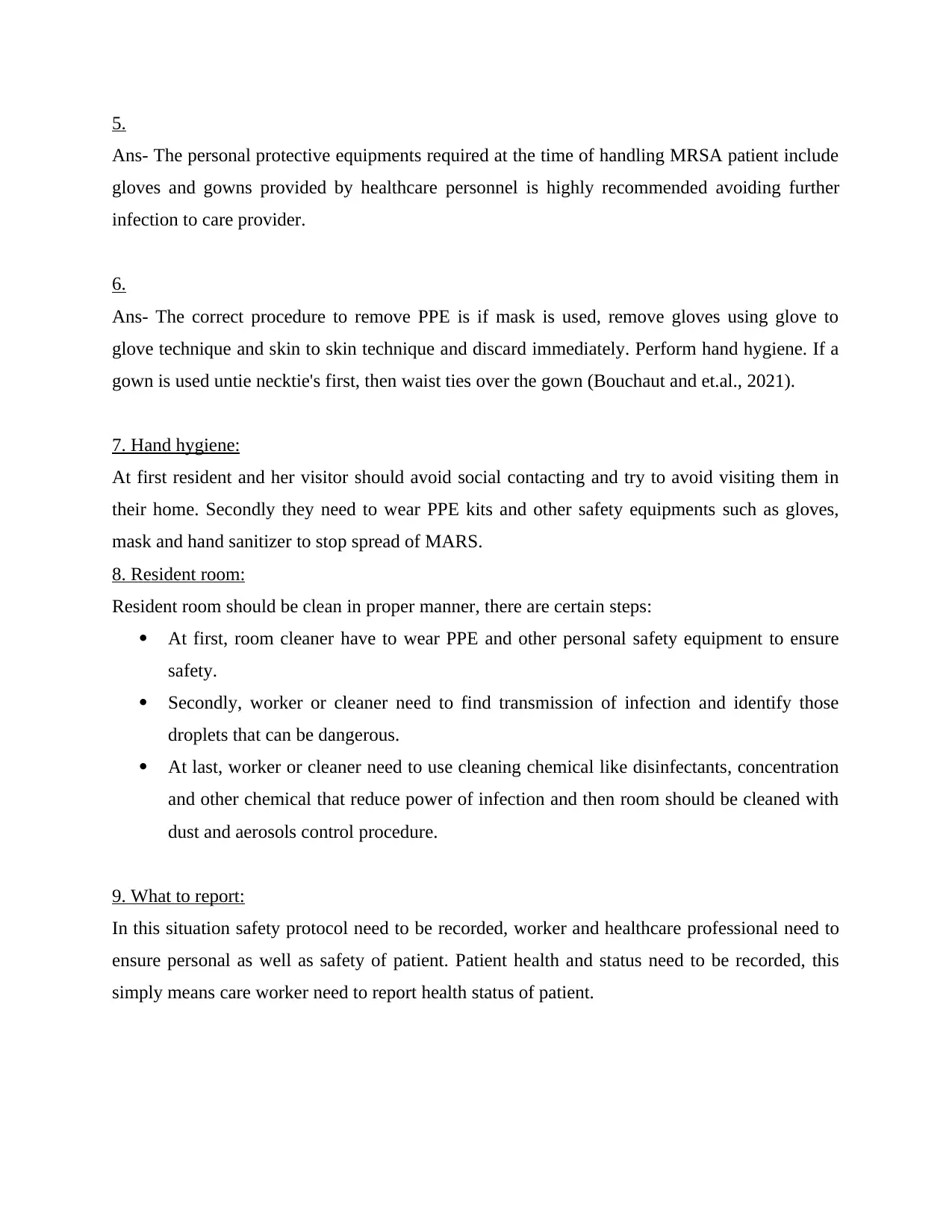
4. Risk assessment:
Rare Unlikely Possible Likely Almost
Aggressive
behaviour
low Medium High Very high Extremely
high
Violent
behaviour
Low Medium High Very high Extremely
high
Mental illness Low Medium High Very high Extremely
high
6. reduce risk in the future:
Visiting client in the future have certain risk associated, care provider need to take certain
measure to control risk in the future, these are:
Ask for appointment: care provider need to often ask client or need to take permission before
visiting their home, this will allow them to understand whether client have aggressive mood or
he is ready to take medical process.
Inform authority: care provider need to inform authority about visit to client, this will allow them
to alert authority and provide help in tough situations and allow care provider to be safe from any
kind of obligation from client.
Warming from wife: wife of client warned care provider about aggressive behaviours of client
and highlighted that he is in angry mood that impact care provider. Her wife informed that he
remain gentle throughout the day but today he is aggressive and might harm care provider (Card
and Klein, 2016).
Warning from client: client have given warning to care provider before dressing, this should be
taken seriously because person with aggressive behaviour only provide one warning and their
behaviour become aggressive.
4. Risk assessment:
Rare Unlikely Possible Likely Almost
Aggressive
behaviour
low Medium High Very high Extremely
high
Violent
behaviour
Low Medium High Very high Extremely
high
Mental illness Low Medium High Very high Extremely
high
6. reduce risk in the future:
Visiting client in the future have certain risk associated, care provider need to take certain
measure to control risk in the future, these are:
Ask for appointment: care provider need to often ask client or need to take permission before
visiting their home, this will allow them to understand whether client have aggressive mood or
he is ready to take medical process.
Inform authority: care provider need to inform authority about visit to client, this will allow them
to alert authority and provide help in tough situations and allow care provider to be safe from any
kind of obligation from client.
TASK 3
PART A:
2. Discussing each policy and procedures with relevant legislation and standards:
Infection control: National Health and Medical Research Council (NHMRC) jointly with
Australia health guideline has provide policy and procedures to control infection; this include:
every healthcare provider need to ensure all precaution to avoid spillage on floor that can spread
infection to worker. Medical clinic need to use chemical substance and cleaning material to clean
spillage properly and place safety sign board to avoid accident.
Emergency management: under Emergency Management Australia department, government of
Australia have certain guideline to manage emergency related to health and medical. To address
any medical emergency, healthcare organization have to activate National Incident Room to
actively respond to health emergency. Under Biosecurity Act 2015, health professional need to
respond to emergency with precaution.
Manual handling: manual handling is activity that allow health professional to avoid any kind of
issue that may arrive due to lack of manual guide causing accident. Under National Manual
Task, health professional have to ensure lifting of chemical and other medical substances need to
be done in proper manner to avoid incident.
Incident reporting: every healthcare professional and organization have to follow legal and
legislative procedures to report incident, they can not avoid reporting of incident as this will
consider against professional practice. Under National Safety and Quality Health Service
(NSQHS) standard healthcare professional need to report in formal manner including setting of
the incident and impact on work or any other person.
PART B
Verbal question Write response
What are manual handling hazard did you have
to deal with?
In fire scenario, there are certain manual
handling hazard impacting worker. Smoke is
one of the most dangerous hazard but more
dangerous was asbestos and vapour that
contain chemical and can impact life of
worker.
PART A:
2. Discussing each policy and procedures with relevant legislation and standards:
Infection control: National Health and Medical Research Council (NHMRC) jointly with
Australia health guideline has provide policy and procedures to control infection; this include:
every healthcare provider need to ensure all precaution to avoid spillage on floor that can spread
infection to worker. Medical clinic need to use chemical substance and cleaning material to clean
spillage properly and place safety sign board to avoid accident.
Emergency management: under Emergency Management Australia department, government of
Australia have certain guideline to manage emergency related to health and medical. To address
any medical emergency, healthcare organization have to activate National Incident Room to
actively respond to health emergency. Under Biosecurity Act 2015, health professional need to
respond to emergency with precaution.
Manual handling: manual handling is activity that allow health professional to avoid any kind of
issue that may arrive due to lack of manual guide causing accident. Under National Manual
Task, health professional have to ensure lifting of chemical and other medical substances need to
be done in proper manner to avoid incident.
Incident reporting: every healthcare professional and organization have to follow legal and
legislative procedures to report incident, they can not avoid reporting of incident as this will
consider against professional practice. Under National Safety and Quality Health Service
(NSQHS) standard healthcare professional need to report in formal manner including setting of
the incident and impact on work or any other person.
PART B
Verbal question Write response
What are manual handling hazard did you have
to deal with?
In fire scenario, there are certain manual
handling hazard impacting worker. Smoke is
one of the most dangerous hazard but more
dangerous was asbestos and vapour that
contain chemical and can impact life of
worker.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 22