Scenario-Based Writing Task: Nursing Care Plan for Mrs. Y's Fracture
VerifiedAdded on 2022/11/25
|8
|1676
|298
Report
AI Summary
This report presents a nursing care plan for Mrs. Y, who sustained a femoral fracture following a fall. The plan utilizes the clinical reasoning cycle to assess Mrs. Y's condition, including her pain levels (related to the fracture and bruising), altered vital signs (history of hypertension), and anxiety. The report prioritizes pain management, focusing on pharmacological and non-pharmacological interventions, such as positioning, traction, and diversion therapy, along with continuous pain assessment. It addresses the patient's anxiety through pharmacological and non-pharmacological methods, emphasizing the importance of patient education and support. The report also considers pre-operative monitoring and management. Evidence-based research from databases like Medline and PubMed is used to support the nursing interventions, demonstrating a commitment to patient-centered care and quality outcomes.
Scenario based writing task
Part B
Introduction
Clinical reasoning cycle is the methodology used for the assessment of the case scenario and
to plan the nursing care for Mrs.Y. Clinical reasoning cycle is the systematic way of planning
and executing the therapy for the patients. In the case scenario, Mrs Y had a fall and got a
fracture in the right head of the femur (Anakin,2019). She also had laceration over the
forehead. Nursing management for Mrs Y is planned according to clinical reasoning cycle. It
includes consideration of patient situation, collection of information, and process of
information, understands the situation of the patient, Plan the care and implement the nursing
intervention, evaluate the outcomes and learn from the clinical reasoning process.
Potential nursing problems
Nursing problem statement: Pain related to fall as evidence by signs and symptoms.
Primary, nursing problem in the case scenario is the pain caused by the fall and the fracture.
Mr.Ys present medical history states that she had a fall. On admission, she complained of
moderate pain over the right hip, arm, and face. She also had severe bruising over the right
hip, face, and arm. Wendt (2016) states that the primary consideration of the elderly patient
who had a fall and ends up in femoral fracture has to be treated for pain. Pre-operative
nursing problem is pain that is related to the fracture. Pain management has to be performed
to reduce the fear and anxiety of the patient.
Nursing problem statement: Altered vital signs caused due to the incident as evidence by
the physical examination
Part B
Introduction
Clinical reasoning cycle is the methodology used for the assessment of the case scenario and
to plan the nursing care for Mrs.Y. Clinical reasoning cycle is the systematic way of planning
and executing the therapy for the patients. In the case scenario, Mrs Y had a fall and got a
fracture in the right head of the femur (Anakin,2019). She also had laceration over the
forehead. Nursing management for Mrs Y is planned according to clinical reasoning cycle. It
includes consideration of patient situation, collection of information, and process of
information, understands the situation of the patient, Plan the care and implement the nursing
intervention, evaluate the outcomes and learn from the clinical reasoning process.
Potential nursing problems
Nursing problem statement: Pain related to fall as evidence by signs and symptoms.
Primary, nursing problem in the case scenario is the pain caused by the fall and the fracture.
Mr.Ys present medical history states that she had a fall. On admission, she complained of
moderate pain over the right hip, arm, and face. She also had severe bruising over the right
hip, face, and arm. Wendt (2016) states that the primary consideration of the elderly patient
who had a fall and ends up in femoral fracture has to be treated for pain. Pre-operative
nursing problem is pain that is related to the fracture. Pain management has to be performed
to reduce the fear and anxiety of the patient.
Nursing problem statement: Altered vital signs caused due to the incident as evidence by
the physical examination
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Second pre-operative priority for the femoral fracture in the elderly is monitoring. Vital signs
have to be monitored continuously. Wendt (2016) states that the patient needs to monitored
continuously during the pre-operative stage. On admission patient’s vital signs were altered
and she is having a history of hypertension and congestive heart failure. Her vital signs on
admission are BP 142/88, HR 110, T 37.3. Chest clear, SpO2 97% RA, AE equal to bases.
Since the patient is posted for the surgery, the nurse has to monitor the vital signs of the
patient.
Nursing problem statement: Anxiety caused due to sudden accident which is a potential
problem for the pre-operative patients.
Zachwieja (2019) states that the patient may undergo anxiety or any kind of mental illness
during the pre-operative period. The nurse has to rule out the mental condition of the patient
and reduce her anxiety with the pharmacological intervention and non-pharmacological
interventions. Nurses have to administer anti-anxieties, provide moral and spiritual support
because anxiety may increase the blood pressure during the surgery. Encourage the patient to
express her anxiety feelings about surgery and treatment. Explain her about the surgery and
post-operative management.
Highest priority statement
Abou-Setta (2011) state that pain is the priority problem for the person who had a femoral
fracture. She is an aged person had femoral fracture which is associated with bruising over
the face and arm. She also had eight sutures over her fore head. Multiple injuries increases
the pain and for aged person the pain tolarence will be reduced.(Question 2) Patient centered
goal for the femoral fracture is formulated to ensure safe and quality nursing care for the
patient. The patient is comfortable and verbalises that the pain over the injury site is reduced.
have to be monitored continuously. Wendt (2016) states that the patient needs to monitored
continuously during the pre-operative stage. On admission patient’s vital signs were altered
and she is having a history of hypertension and congestive heart failure. Her vital signs on
admission are BP 142/88, HR 110, T 37.3. Chest clear, SpO2 97% RA, AE equal to bases.
Since the patient is posted for the surgery, the nurse has to monitor the vital signs of the
patient.
Nursing problem statement: Anxiety caused due to sudden accident which is a potential
problem for the pre-operative patients.
Zachwieja (2019) states that the patient may undergo anxiety or any kind of mental illness
during the pre-operative period. The nurse has to rule out the mental condition of the patient
and reduce her anxiety with the pharmacological intervention and non-pharmacological
interventions. Nurses have to administer anti-anxieties, provide moral and spiritual support
because anxiety may increase the blood pressure during the surgery. Encourage the patient to
express her anxiety feelings about surgery and treatment. Explain her about the surgery and
post-operative management.
Highest priority statement
Abou-Setta (2011) state that pain is the priority problem for the person who had a femoral
fracture. She is an aged person had femoral fracture which is associated with bruising over
the face and arm. She also had eight sutures over her fore head. Multiple injuries increases
the pain and for aged person the pain tolarence will be reduced.(Question 2) Patient centered
goal for the femoral fracture is formulated to ensure safe and quality nursing care for the
patient. The patient is comfortable and verbalises that the pain over the injury site is reduced.
Mrs Y said that she is aware of the pain management techniques and she will co-operate with
the nurse in pain management during post operative period. The patient had an understanding
and knowledge about post-operative pain management (Rasmussen, 2018).
Nursing interventions
Primary nursing intervention for the patient who had femoral fracture is pain management.
Pain management can be implemented by pharmacological nursing interventions. Non-
pharmacological interventions are simple and easy methods which reduce pain without any
medication (Bhandari, 2017). Pharmacological intervention can be executed by the
administration of narcotic drugs. The patient who had femoral fracture suffer from high
intensity pain and pain tolerance is less in the elderly patient. Mrs.Y had to bruise over the
face, arm, and forehead, so pain management can be achieved by the administration of the
narcotic drugs (Florschutz, 2015).
Alleviation of the pain using non pharmacological measures can be attained with the
interventions like positioning the patient; because positioning the patient reduces the pain
(Ivarsson, 2018). Support the patient with extra pillows and cushions, as it will increase the
comfort for the patient. Applying traction will reduce the pain and increases the comfort for
the patient. (Roberts, 2015). Nurse can implement diversion therapy because diversion
therapy distracts the patient’s concentration towards pain. Because non-pharmacological pain
management measures easy to apply and can be used at any time.
Implementation of the pain management techniques is the secondary nursing interventions for
the patien. Continuously assess the intensity of the pain using the pain scale. The continuous
assessment helps the nurse to identify clinical deteriotation which is a medical emergency.
Educate and demonstrate deep breathing exercise to the patient. Deep breathing exercise
the nurse in pain management during post operative period. The patient had an understanding
and knowledge about post-operative pain management (Rasmussen, 2018).
Nursing interventions
Primary nursing intervention for the patient who had femoral fracture is pain management.
Pain management can be implemented by pharmacological nursing interventions. Non-
pharmacological interventions are simple and easy methods which reduce pain without any
medication (Bhandari, 2017). Pharmacological intervention can be executed by the
administration of narcotic drugs. The patient who had femoral fracture suffer from high
intensity pain and pain tolerance is less in the elderly patient. Mrs.Y had to bruise over the
face, arm, and forehead, so pain management can be achieved by the administration of the
narcotic drugs (Florschutz, 2015).
Alleviation of the pain using non pharmacological measures can be attained with the
interventions like positioning the patient; because positioning the patient reduces the pain
(Ivarsson, 2018). Support the patient with extra pillows and cushions, as it will increase the
comfort for the patient. Applying traction will reduce the pain and increases the comfort for
the patient. (Roberts, 2015). Nurse can implement diversion therapy because diversion
therapy distracts the patient’s concentration towards pain. Because non-pharmacological pain
management measures easy to apply and can be used at any time.
Implementation of the pain management techniques is the secondary nursing interventions for
the patien. Continuously assess the intensity of the pain using the pain scale. The continuous
assessment helps the nurse to identify clinical deteriotation which is a medical emergency.
Educate and demonstrate deep breathing exercise to the patient. Deep breathing exercise
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

relaxes the body muscles and the pain will be reduced. Education and demonstration help the
patient to understand proper exercise method (Zachwieja, 2019). Administer analgesics as per
doctor’s order. Analgesics reduce pain and promote comfort. The nurse has to educate the
patient and his family about pain management techniques. The nurse can implement
diversion therapy which is one of the non-pharmachological pain management.
Conclusion
Evidence based research is implemented in the case scenario to plan and execute the nursing
care based on the clinical reasoning cycle. Clinical reasoning cycle is the systematic way of
planning and executing the therapy for the patients. Evidence based research was executed by
the data base like Medline and pub med were used to search the evidence based literature that
supports the case scenario. Consideration of patient situation, collection of information, and
process of information, understand the situation of the patient, Plan the care and implement
the nursing intervention, evaluate the outcomes and learn are the eight steps of the clinical
reasoning cycle is implemented to care for Mrs Y. The nursing problem statement was
created and highest priority nursing interventions are critically assessed with the rationales.
Evidence from the current peer reviewed nursing literature is used to formulate the nursing
interventions based on the need of the patient.
References
Anakin, M., Petryk, T., Ladyka, V., & Dudar, S. (2019). Features of the femoral head
fractures treatment. ORTHOPAEDICS, TRAUMATOLOGY and PROSTHETICS, (2),
27-35 http://otp-journal.com.ua/article/view/172079
Abou-Setta AM, Beaupre LA, Jones CA, et al. Pain Management Interventions for Hip
Fracture [Internet]. Rockville (MD): Agency for Healthcare Research and Quality
patient to understand proper exercise method (Zachwieja, 2019). Administer analgesics as per
doctor’s order. Analgesics reduce pain and promote comfort. The nurse has to educate the
patient and his family about pain management techniques. The nurse can implement
diversion therapy which is one of the non-pharmachological pain management.
Conclusion
Evidence based research is implemented in the case scenario to plan and execute the nursing
care based on the clinical reasoning cycle. Clinical reasoning cycle is the systematic way of
planning and executing the therapy for the patients. Evidence based research was executed by
the data base like Medline and pub med were used to search the evidence based literature that
supports the case scenario. Consideration of patient situation, collection of information, and
process of information, understand the situation of the patient, Plan the care and implement
the nursing intervention, evaluate the outcomes and learn are the eight steps of the clinical
reasoning cycle is implemented to care for Mrs Y. The nursing problem statement was
created and highest priority nursing interventions are critically assessed with the rationales.
Evidence from the current peer reviewed nursing literature is used to formulate the nursing
interventions based on the need of the patient.
References
Anakin, M., Petryk, T., Ladyka, V., & Dudar, S. (2019). Features of the femoral head
fractures treatment. ORTHOPAEDICS, TRAUMATOLOGY and PROSTHETICS, (2),
27-35 http://otp-journal.com.ua/article/view/172079
Abou-Setta AM, Beaupre LA, Jones CA, et al. Pain Management Interventions for Hip
Fracture [Internet]. Rockville (MD): Agency for Healthcare Research and Quality
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
(US); 2011 May. (Comparative Effectiveness Reviews, No. 30.) Available from:
https://www.ncbi.nlm.nih.gov/books/NBK56670/
Bhandari, M., & Swiontkowski, M. (2017). Management of acute hip fracture. New England
Journal of Medicine, 377(21), 2053-2062
https://www.nejm.org/doi/full/10.1056/NEJMcp1611090
Florschutz, A. V., Langford, J. R., Haidukewych, G. J., & Koval, K. J. (2015). Femoral neck
fractures: current management. Journal of orthopaedic trauma, 29(3), 121-129
https://journals.lww.com/jorthotrauma/Abstract/2015/03000/Femoral_Neck_Fractures
__Current_Management.2.aspx
Ivarsson, B., Hommel, A., Sandberg, M., Sjöstrand, D., & Johansson, A. (2018). The
experiences of pre-and in-hospital care in patients with hip fractures: A study based
on Critical incidents. International journal of orthopaedic and trauma nursing, 30, 8-
13 https://www.ncbi.nlm.nih.gov/pubmed/29929886
Ju, D. G., Rajaee, S. S., Mirocha, J., Lin, C. A., & Moon, C. N. (2017). A nationwide analysis
of femoral neck fractures in elderly patients: a receding tide. JBJS, 99(22), 1932-1940
https://journals.lww.com/jbjsjournal/Abstract/2017/11150/Nationwide_Analysis_of_F
emoral_Neck_Fractures_in.9.aspx
Roberts, K. C., Brox, W. T., Jevsevar, D. S., & Sevarino, K. (2015). Management of hip
fractures in the elderly. JAAOS-Journal of the American Academy of Orthopaedic
Surgeons, 23(2), 131-137
https://journals.lww.com/jaaos/Fulltext/2015/02000/Management_of_Hip_Fractures_i
n_the_Elderly.9.aspx
https://www.ncbi.nlm.nih.gov/books/NBK56670/
Bhandari, M., & Swiontkowski, M. (2017). Management of acute hip fracture. New England
Journal of Medicine, 377(21), 2053-2062
https://www.nejm.org/doi/full/10.1056/NEJMcp1611090
Florschutz, A. V., Langford, J. R., Haidukewych, G. J., & Koval, K. J. (2015). Femoral neck
fractures: current management. Journal of orthopaedic trauma, 29(3), 121-129
https://journals.lww.com/jorthotrauma/Abstract/2015/03000/Femoral_Neck_Fractures
__Current_Management.2.aspx
Ivarsson, B., Hommel, A., Sandberg, M., Sjöstrand, D., & Johansson, A. (2018). The
experiences of pre-and in-hospital care in patients with hip fractures: A study based
on Critical incidents. International journal of orthopaedic and trauma nursing, 30, 8-
13 https://www.ncbi.nlm.nih.gov/pubmed/29929886
Ju, D. G., Rajaee, S. S., Mirocha, J., Lin, C. A., & Moon, C. N. (2017). A nationwide analysis
of femoral neck fractures in elderly patients: a receding tide. JBJS, 99(22), 1932-1940
https://journals.lww.com/jbjsjournal/Abstract/2017/11150/Nationwide_Analysis_of_F
emoral_Neck_Fractures_in.9.aspx
Roberts, K. C., Brox, W. T., Jevsevar, D. S., & Sevarino, K. (2015). Management of hip
fractures in the elderly. JAAOS-Journal of the American Academy of Orthopaedic
Surgeons, 23(2), 131-137
https://journals.lww.com/jaaos/Fulltext/2015/02000/Management_of_Hip_Fractures_i
n_the_Elderly.9.aspx
Rasmussen, B., Nielsen, C. V., & Uhrenfeldt, L. (2018). Being active after hip fracture; older
people’s lived experiences of facilitators and barriers. International journal of
qualitative studies on health and well-being, 13(1), 1554024
https://www.ncbi.nlm.nih.gov/pubmed/30704373
Wendt, K., Heim, D., Josten, C., Kdolsky, R., Oestern, H. J., Palm, H., ... & Copuroglu, C.
(2016). Recommendations on hip fractures. European Journal of Trauma and
Emergency Surgery, 42(4), 425-431 https://link.springer.com/article/10.1007/s00068-
016-0684-3
Zachwieja, E., Butler, A. J., Grau, L. C., Summers, S., Massel, D., Orozco, F., & Hernandez,
V. H. (2019). The association of mental health disease with perioperative outcomes
following femoral neck fractures. Journal of Clinical Orthopaedics and
Traumahttps://www.sciencedirect.com/science/article/pii/S0976566218306374
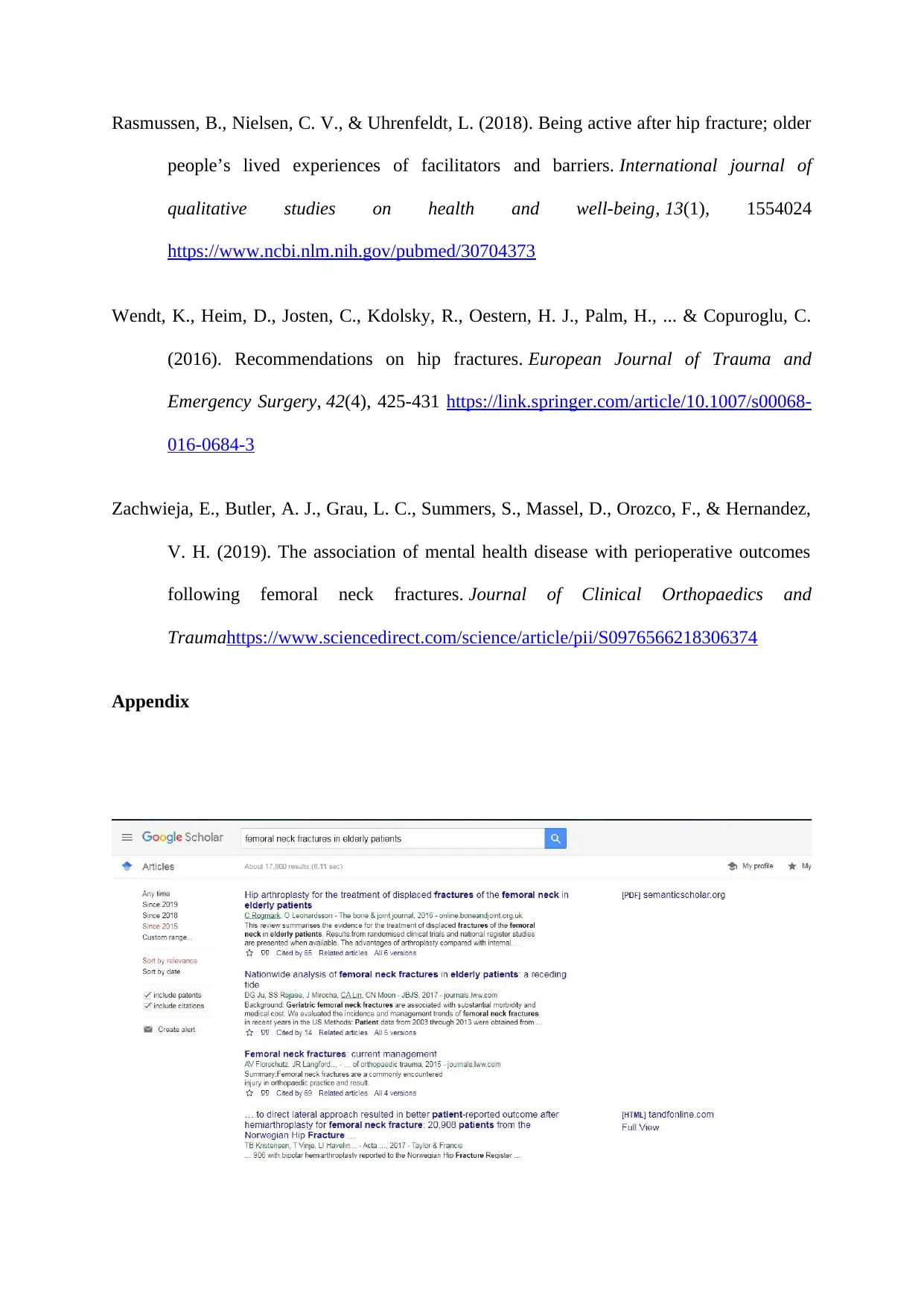
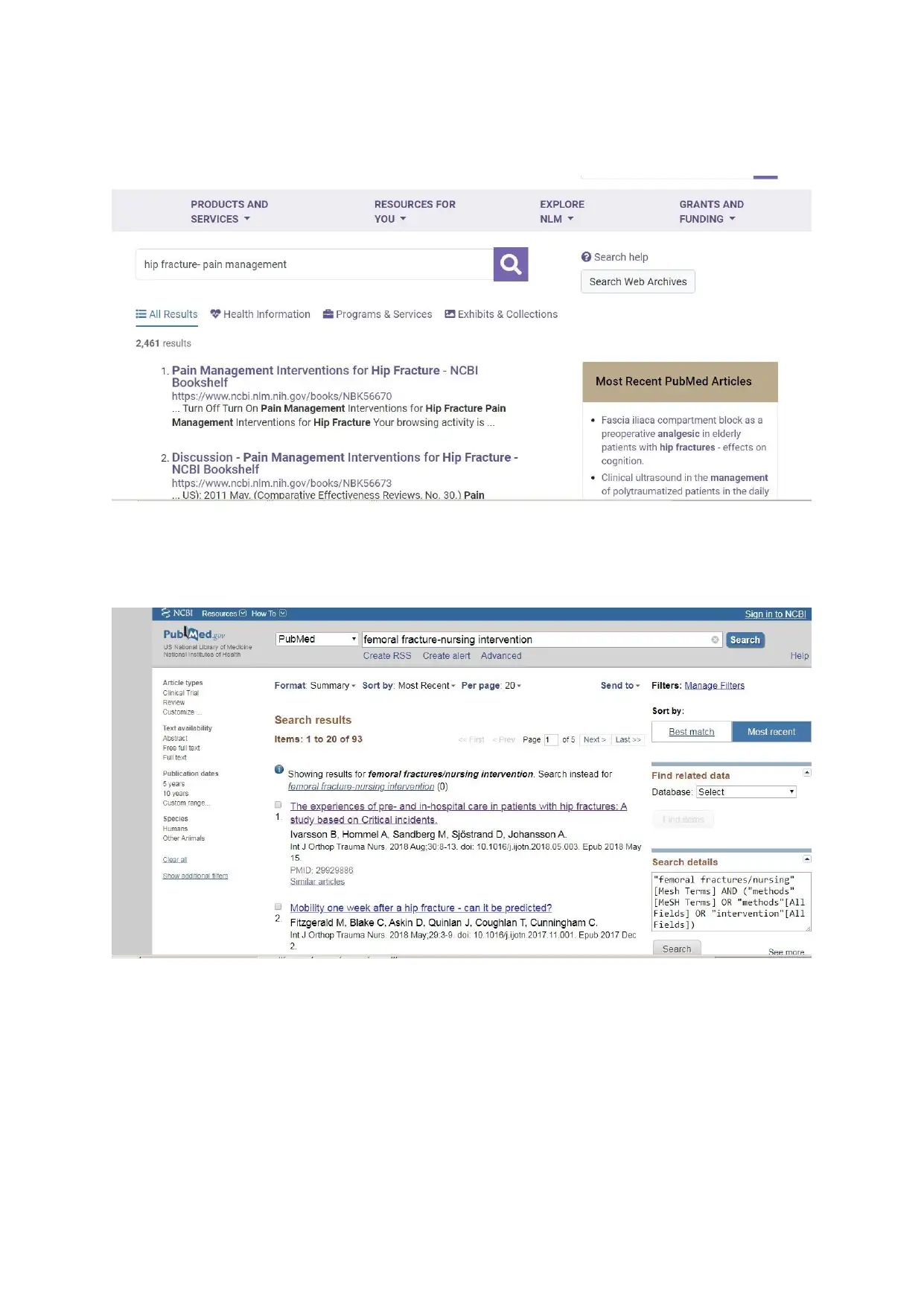
Appendix
people’s lived experiences of facilitators and barriers. International journal of
qualitative studies on health and well-being, 13(1), 1554024
https://www.ncbi.nlm.nih.gov/pubmed/30704373
Wendt, K., Heim, D., Josten, C., Kdolsky, R., Oestern, H. J., Palm, H., ... & Copuroglu, C.
(2016). Recommendations on hip fractures. European Journal of Trauma and
Emergency Surgery, 42(4), 425-431 https://link.springer.com/article/10.1007/s00068-
016-0684-3
Zachwieja, E., Butler, A. J., Grau, L. C., Summers, S., Massel, D., Orozco, F., & Hernandez,
V. H. (2019). The association of mental health disease with perioperative outcomes
following femoral neck fractures. Journal of Clinical Orthopaedics and
Traumahttps://www.sciencedirect.com/science/article/pii/S0976566218306374
Appendix
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1 out of 8
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





