Schizophrenia, Atypical Antipsychotics, and Nursing Management
VerifiedAdded on 2022/09/07
|12
|2842
|22
Report
AI Summary
This report delves into the psychological disorder of schizophrenia, providing a comprehensive overview of its pathophysiology and the pharmacological treatments used to manage the condition. It begins with a definition of schizophrenia, highlighting its impact on emotions, thinking, and behavior, and discusses different types of the disorder, including catatonic, hebephrenic, and paranoid subtypes. The report then explores the disruption of homeostasis in schizophrenia, including the alteration of nitric oxide levels and purine metabolism, leading to mitochondrial dysfunction. The pathophysiology section covers genetic, dopamine, neurodevelopmental, and psychosocial theories. The report then examines the use of antipsychotic drugs, particularly atypical antipsychotics, their mechanisms of action, indications, contraindications, and potential complications. It also touches upon non-pharmacological interventions and the crucial role of nursing management in patient care. The report includes a discussion on the pharmacokinetic properties of antipsychotic drugs, the complications and risk factors associated with their use, and various non-pharmacological interventions such as individual and family therapy. Finally, the report emphasizes the role of nurses in assessing, building relationships, and supporting patients with schizophrenia, aiming to reduce symptoms and promote a normal level of function.

Running Head: SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
Schizophrenia and atypical antipsychotics
Name of the Student
Name of the University
Author Note
Schizophrenia and atypical antipsychotics
Name of the Student
Name of the University
Author Note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
Abstract
Schizophrenia is a long-lasting mixed syndrome of muddled and unusual thoughts,
hallucinations, inappropriate effect, and cognitive impairment. The primary purpose of the
below paper is to provide a brief idea about the psychological disorder named schizophrenia
along with its pathophysiology and drugs used in treating the condition. Schizophrenia is
marked by severely impaired emotions, thinking and behaviour. The patient suffering from
this state is unable to filter many sensory stimuli and have enhanced perceptions of colours,
sounds and other environmental features. There are several types of this condition like
catatonic, hebephrenic and paranoid. Catatonic condition is characterised by motor symptoms
that are the patients’ experiences severe immobility issues such as bizarre movements.
Paranoid involves cognitive impairment along with delusion signs. The disease disrupts the
homeostasis condition of the body, such as raising the nitric oxide level in the patient body.
The condition alters the purine metabolism, which in turn affects the mitochondrial
dysfunction. The main pathophysiology comprises of few theories such as genetic theory,
which states that the disease happens due to a strong genetic association. The dopamine
theory highlights the hyper and hypoactivity of the dopamine resulting in positive and
negative symptoms. Other theories are neuro-development and psychosocial. Magnetic
resonance imaging and X-ray can diagnose the condition. Antipsychotic drugs such as
chlorpromazine, haloperidol, thioridazine, trifluoperazine control this state by a different
mechanism. The drug has two generations first and second. The paper also focuses on a few
non-pharmacological interventions to reduce this condition. Lastly, the paper discusses the
nursing management of this condition.
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
Abstract
Schizophrenia is a long-lasting mixed syndrome of muddled and unusual thoughts,
hallucinations, inappropriate effect, and cognitive impairment. The primary purpose of the
below paper is to provide a brief idea about the psychological disorder named schizophrenia
along with its pathophysiology and drugs used in treating the condition. Schizophrenia is
marked by severely impaired emotions, thinking and behaviour. The patient suffering from
this state is unable to filter many sensory stimuli and have enhanced perceptions of colours,
sounds and other environmental features. There are several types of this condition like
catatonic, hebephrenic and paranoid. Catatonic condition is characterised by motor symptoms
that are the patients’ experiences severe immobility issues such as bizarre movements.
Paranoid involves cognitive impairment along with delusion signs. The disease disrupts the
homeostasis condition of the body, such as raising the nitric oxide level in the patient body.
The condition alters the purine metabolism, which in turn affects the mitochondrial
dysfunction. The main pathophysiology comprises of few theories such as genetic theory,
which states that the disease happens due to a strong genetic association. The dopamine
theory highlights the hyper and hypoactivity of the dopamine resulting in positive and
negative symptoms. Other theories are neuro-development and psychosocial. Magnetic
resonance imaging and X-ray can diagnose the condition. Antipsychotic drugs such as
chlorpromazine, haloperidol, thioridazine, trifluoperazine control this state by a different
mechanism. The drug has two generations first and second. The paper also focuses on a few
non-pharmacological interventions to reduce this condition. Lastly, the paper discusses the
nursing management of this condition.
2
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
Schizophrenia
Schizophrenia is one of the critical mental illnesses where the patients associate with,
the real-life in an atypical way (Arion et al., 2015). The patient with this illness mostly
experiences both the indications like hallucinations, delusions and a chief mood-related
disorder like depression, anxiety at a similar point of the stage (Gaebel & Zielasek,
2015).There are numerous ways by which schizophrenia can arise, these are –
Genetics- The disease can be triggered due to imperfect inherited gene from the family.
Neurological Cause- The disease can also be instigated due to the faulty secretion of
neurotransmitters, especially dopamine.
Defective development of the Brain- The structure of the brain cortex or the ventricles may
be enlarged, resulting in a schizophrenic condition (Stegmayer et al., 2016).
Homeostasis imbalance in Schizophrenia
Schizophrenia is characterised by neuropathy changes in the mechanism of the
oxidative stress mechanism. The patient with schizophrenia experiences a condition of
defective enzyme secretion as well as non-enzymatic components to defence against the free
radical noxiousness (Landek-Salgado, Faust & Sawa, 2016). It also found that defective
redox coupling most notably reduces the level of glutathione along with the reduction of
glutathione reductase activities. It is also found from previous studies that membrane
alteration and antioxidant defence system (AODS) are primarily responsible for free radical-
mediated neurotoxicity in the schizophrenia disorder. It is also observed that nitric oxide is
significantly higher in the brains of a detected patient suffering from this condition. There are
plenty of ways by which oxidative stress and free radical generation take place one such
technique is the formation of peroxynitrite by the reaction of superoxide radical and nitric
oxide. A significant rise in the level of nitric oxide is present in the brain of schizophrenia
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
Schizophrenia
Schizophrenia is one of the critical mental illnesses where the patients associate with,
the real-life in an atypical way (Arion et al., 2015). The patient with this illness mostly
experiences both the indications like hallucinations, delusions and a chief mood-related
disorder like depression, anxiety at a similar point of the stage (Gaebel & Zielasek,
2015).There are numerous ways by which schizophrenia can arise, these are –
Genetics- The disease can be triggered due to imperfect inherited gene from the family.
Neurological Cause- The disease can also be instigated due to the faulty secretion of
neurotransmitters, especially dopamine.
Defective development of the Brain- The structure of the brain cortex or the ventricles may
be enlarged, resulting in a schizophrenic condition (Stegmayer et al., 2016).
Homeostasis imbalance in Schizophrenia
Schizophrenia is characterised by neuropathy changes in the mechanism of the
oxidative stress mechanism. The patient with schizophrenia experiences a condition of
defective enzyme secretion as well as non-enzymatic components to defence against the free
radical noxiousness (Landek-Salgado, Faust & Sawa, 2016). It also found that defective
redox coupling most notably reduces the level of glutathione along with the reduction of
glutathione reductase activities. It is also found from previous studies that membrane
alteration and antioxidant defence system (AODS) are primarily responsible for free radical-
mediated neurotoxicity in the schizophrenia disorder. It is also observed that nitric oxide is
significantly higher in the brains of a detected patient suffering from this condition. There are
plenty of ways by which oxidative stress and free radical generation take place one such
technique is the formation of peroxynitrite by the reaction of superoxide radical and nitric
oxide. A significant rise in the level of nitric oxide is present in the brain of schizophrenia
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
patient—the excess production of further decreases the glutathione. Purine catabolism is
highly decreased in many diseases, which is involved in the homeostatic response and
develops mitochondrial dysfunction (Steen et al., 2020). The decrease energy level, nucleic
acid damage and purine metabolism shifts from normal response and results in the production
of xanthine and uric acid (Rajan et al., 2016). This defective mechanism results in abnormal
homeostasis in the body resulting in defective neurotransmitters from the brain, causing
schizophrenia.
Pathophysiology
The pathophysiology of this disease can be divided into four different theories such as
genetic theory, dopamine theory, Neuro-developmental theory and psychosocial theory. The
genetic theory states that there is a strong association of gene in the development of this
condition. The dopamine theory is regarded as the most important fact of this disease
development. The dopamine hyperactivity is responsible for the hyperactivity of the brain
resulting in psychotic symptoms. The hyperactivity is observed in the mesolimbic brain,
whereas the activities of the other brain parts such as frontal, prefrontal and temporal cortices
have decreased activity of this neurotransmitters (Kesbey et al., 2018). The other transmitters
that are involved are 5-hydroxytryptamine and glutamate. The receptors of these
neurotransmitters are generally G-coupled receptors which work along with ligand-gated ion
channels and thus maintaining the activity of peripheral and central nervous system along
with mediating both the inhibitory and excitatory neurotransmission. Glutamate deficiency is
also found in this state (McCutcheon et al., 2020). The neurodevelopment theory states that
schizophrenia disorders are commonly associated with utero disturbance during pregnancy.
The cause of this system is a disturbance in the upper respiratory infections, neonatal hypoxia
and obstetric complication. The last theory of psychosocial states that it happens due to poor
interpersonal skills, excessive stress and poor socio-economic state.
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
patient—the excess production of further decreases the glutathione. Purine catabolism is
highly decreased in many diseases, which is involved in the homeostatic response and
develops mitochondrial dysfunction (Steen et al., 2020). The decrease energy level, nucleic
acid damage and purine metabolism shifts from normal response and results in the production
of xanthine and uric acid (Rajan et al., 2016). This defective mechanism results in abnormal
homeostasis in the body resulting in defective neurotransmitters from the brain, causing
schizophrenia.
Pathophysiology
The pathophysiology of this disease can be divided into four different theories such as
genetic theory, dopamine theory, Neuro-developmental theory and psychosocial theory. The
genetic theory states that there is a strong association of gene in the development of this
condition. The dopamine theory is regarded as the most important fact of this disease
development. The dopamine hyperactivity is responsible for the hyperactivity of the brain
resulting in psychotic symptoms. The hyperactivity is observed in the mesolimbic brain,
whereas the activities of the other brain parts such as frontal, prefrontal and temporal cortices
have decreased activity of this neurotransmitters (Kesbey et al., 2018). The other transmitters
that are involved are 5-hydroxytryptamine and glutamate. The receptors of these
neurotransmitters are generally G-coupled receptors which work along with ligand-gated ion
channels and thus maintaining the activity of peripheral and central nervous system along
with mediating both the inhibitory and excitatory neurotransmission. Glutamate deficiency is
also found in this state (McCutcheon et al., 2020). The neurodevelopment theory states that
schizophrenia disorders are commonly associated with utero disturbance during pregnancy.
The cause of this system is a disturbance in the upper respiratory infections, neonatal hypoxia
and obstetric complication. The last theory of psychosocial states that it happens due to poor
interpersonal skills, excessive stress and poor socio-economic state.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
On the other hand, the disease can be caused due to the abnormalities present in the
dopaminergic system. The hyper-dopaminergic activity in the brain region of the mesolimbic
system develops positive symptom and the hypo-dopaminergic activity in the brain region
results in positive symptom. Some other reasons are changes in specific brain portions such
as the hippocampus and surrounding region reduction and larger ventricular region due to the
excessive amount of fluid-filled in the spaces.
Fig 1- Brain structure changes
Pharmacological treatment and mechanism of action
The antipsychotic drugs are mainly used in curing this disease. There are numerous
kinds of antipsychotic drugs that help in dropping the indication. It chiefly inhibits the
chemical hints of the brain such as neurotransmitters like serotonin and dopamine. The
assemblies of this drug are typical drug or first-generation, and the other group is atypical
drugs or second-generation. The utmost shared drugs that are helpful for treating the patient
are- chlorpromazine, haloperidol, thioridazine, trifluoperazine, thiothixene, fluphenazine.
These medications are chiefly neuroleptic, dopamine antagonists. The medicines diminish the
affirmative as well as destructive indications of the illness by hindering the four dopamine
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
On the other hand, the disease can be caused due to the abnormalities present in the
dopaminergic system. The hyper-dopaminergic activity in the brain region of the mesolimbic
system develops positive symptom and the hypo-dopaminergic activity in the brain region
results in positive symptom. Some other reasons are changes in specific brain portions such
as the hippocampus and surrounding region reduction and larger ventricular region due to the
excessive amount of fluid-filled in the spaces.
Fig 1- Brain structure changes
Pharmacological treatment and mechanism of action
The antipsychotic drugs are mainly used in curing this disease. There are numerous
kinds of antipsychotic drugs that help in dropping the indication. It chiefly inhibits the
chemical hints of the brain such as neurotransmitters like serotonin and dopamine. The
assemblies of this drug are typical drug or first-generation, and the other group is atypical
drugs or second-generation. The utmost shared drugs that are helpful for treating the patient
are- chlorpromazine, haloperidol, thioridazine, trifluoperazine, thiothixene, fluphenazine.
These medications are chiefly neuroleptic, dopamine antagonists. The medicines diminish the
affirmative as well as destructive indications of the illness by hindering the four dopamine
5
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
pathway. The mesocortical route, it is a path by which the ventral tegmentum, is associated
with the prefrontal cortex, widespread action of this pathway mentions to the improvement of
destructive indications of schizophrenia. The next target pathways of these medicines are
mesolimbic pathway; overexpression of this pathway leads to the upsurge of affirmative signs
the illness amongst the patients. The antipsychotic medication mostly wedges the D2 receptor
of this mesolimbic pathway.
The next pathway that is targeted by these drugs is the nigrostriatal pathway, which is
related to extrapyramidal symptoms. Here in this path, the drug aims the D2 receptors to
reduce the indications of schizophrenia. The last path that is directed by the drugs is a
tuberoinfundibular path, and here the drug improves the level of prolactin as the dopamines
diminish the creation level of prolactin by constraining it.
Among the medicines, chlorpromazine is the uppermost anticholinergic consequence
with great hypotensive effect (Kowalski et al., 2017). Chlorpromazine (Given, 2016) is a
phenothiazine (FEEN-oh-THYE-a-zeen) employed in adolescents for the diagnosis of
psychiatric conditions such as autism and bipolar depression. The medication is used to cure
autism, and to manage nausea and vomiting. In fact it is often given during surgery to
alleviate restlessness and anxiety. For the diagnosis of extreme behavioral issues in children
(1 to 12 years of age) marked by combativeness and/or destructive hyperexcitable actions
(out of comparison to imminent provocations) and for the short-term management of
hyperactive adolescents with repetitive motor activity associated cognitive disturbances
consisting of the following symptoms such as impulsiveness. However, the contradictions
include the norms where the drugs should not be administered amongst the patients with
known hypersensitivity to phenothiazines and for patients in comatose conditions or with
significant concentrations of depressant central nervous system.
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
pathway. The mesocortical route, it is a path by which the ventral tegmentum, is associated
with the prefrontal cortex, widespread action of this pathway mentions to the improvement of
destructive indications of schizophrenia. The next target pathways of these medicines are
mesolimbic pathway; overexpression of this pathway leads to the upsurge of affirmative signs
the illness amongst the patients. The antipsychotic medication mostly wedges the D2 receptor
of this mesolimbic pathway.
The next pathway that is targeted by these drugs is the nigrostriatal pathway, which is
related to extrapyramidal symptoms. Here in this path, the drug aims the D2 receptors to
reduce the indications of schizophrenia. The last path that is directed by the drugs is a
tuberoinfundibular path, and here the drug improves the level of prolactin as the dopamines
diminish the creation level of prolactin by constraining it.
Among the medicines, chlorpromazine is the uppermost anticholinergic consequence
with great hypotensive effect (Kowalski et al., 2017). Chlorpromazine (Given, 2016) is a
phenothiazine (FEEN-oh-THYE-a-zeen) employed in adolescents for the diagnosis of
psychiatric conditions such as autism and bipolar depression. The medication is used to cure
autism, and to manage nausea and vomiting. In fact it is often given during surgery to
alleviate restlessness and anxiety. For the diagnosis of extreme behavioral issues in children
(1 to 12 years of age) marked by combativeness and/or destructive hyperexcitable actions
(out of comparison to imminent provocations) and for the short-term management of
hyperactive adolescents with repetitive motor activity associated cognitive disturbances
consisting of the following symptoms such as impulsiveness. However, the contradictions
include the norms where the drugs should not be administered amongst the patients with
known hypersensitivity to phenothiazines and for patients in comatose conditions or with
significant concentrations of depressant central nervous system.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
Considering the probability that certain patients that are regularly addicted to
antipsychotics that experience late dyskinesia, it is advised that detailed knowledge regarding
this possibility be provided to all patients with, which prolonged usage is considered and the
precautions to be observed. Obviously, the determination to advise patients and/or their
guardians must take into consideration the patient's health conditions and ability to interpret
the details received. Thorazine (chlorpromazine) (Given, 2016) should be prescribed to
individuals with coronary, kidney, or renal disorder with care. There has been indication that
patients with a history of cirrhosis-related hepatic encephalopathy have doubled susceptibility
to the CNS effects of thorazine (chlorpromazine) (i.e. impaired cerebration and abnormal
EEG slowing). Thorazine (chlorpromazine) should be used with caution in patients with
chronic respiratory disorders such as severe asthma, emphysema and acute respiratory
infections, especially in children (1 to 12 years of age) due to its CNS depressing effect. In
patients with specific medical conditions, for example, patients with mitral insufficiency or
pheochromocytoma reported extreme hypotension after prescribed doses, certain side effects
of thorazine (chlorpromazine) might be more likely to arise, or arise with greater severity.
Dizziness may occur, normally mild to moderate, especially within the initial or second week,
following which it typically disappears.
Pharmacokinetic properties
All the antipsychotic drugs have similar pharmacokinetic properties such as good
gastrointestinal absorption but reduced systemic availability. This is due to the first passage
of drug hepatic metabolism. The hepatic cells are also very responsible for clearing the
metabolites, also known as first hepatic clearance. The distribution of this drug is also very
fast and is rapidly absorbed in the bloodstream. The drug reaches the half-life within 24hours
and is readily eliminated from the body. However, this drug has no such active metabolites
along with poor renal elimination. These drugs can be administered both orally and injectable
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
Considering the probability that certain patients that are regularly addicted to
antipsychotics that experience late dyskinesia, it is advised that detailed knowledge regarding
this possibility be provided to all patients with, which prolonged usage is considered and the
precautions to be observed. Obviously, the determination to advise patients and/or their
guardians must take into consideration the patient's health conditions and ability to interpret
the details received. Thorazine (chlorpromazine) (Given, 2016) should be prescribed to
individuals with coronary, kidney, or renal disorder with care. There has been indication that
patients with a history of cirrhosis-related hepatic encephalopathy have doubled susceptibility
to the CNS effects of thorazine (chlorpromazine) (i.e. impaired cerebration and abnormal
EEG slowing). Thorazine (chlorpromazine) should be used with caution in patients with
chronic respiratory disorders such as severe asthma, emphysema and acute respiratory
infections, especially in children (1 to 12 years of age) due to its CNS depressing effect. In
patients with specific medical conditions, for example, patients with mitral insufficiency or
pheochromocytoma reported extreme hypotension after prescribed doses, certain side effects
of thorazine (chlorpromazine) might be more likely to arise, or arise with greater severity.
Dizziness may occur, normally mild to moderate, especially within the initial or second week,
following which it typically disappears.
Pharmacokinetic properties
All the antipsychotic drugs have similar pharmacokinetic properties such as good
gastrointestinal absorption but reduced systemic availability. This is due to the first passage
of drug hepatic metabolism. The hepatic cells are also very responsible for clearing the
metabolites, also known as first hepatic clearance. The distribution of this drug is also very
fast and is rapidly absorbed in the bloodstream. The drug reaches the half-life within 24hours
and is readily eliminated from the body. However, this drug has no such active metabolites
along with poor renal elimination. These drugs can be administered both orally and injectable
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
form. Example Risperidone is used in treating schizophrenia which is administered by
injection (Fellner, 2017).
Complications and risk factors of antipsychotic drugs
There are many complications that happen due to long-term use of these drugs. Few
second-generation drugs such as clozapine and olanzapine results in the development of
metabolic disorders such as type 2 diabetes mellitus and obesity. The first generation drugs
result in some more adverse condition such as movement disorders. Other complications are
sedation, cardiac arrhythmia, postural hypotension and even cardiac arrest (Stepnicki, Kondej
& Kaczor, 2018).
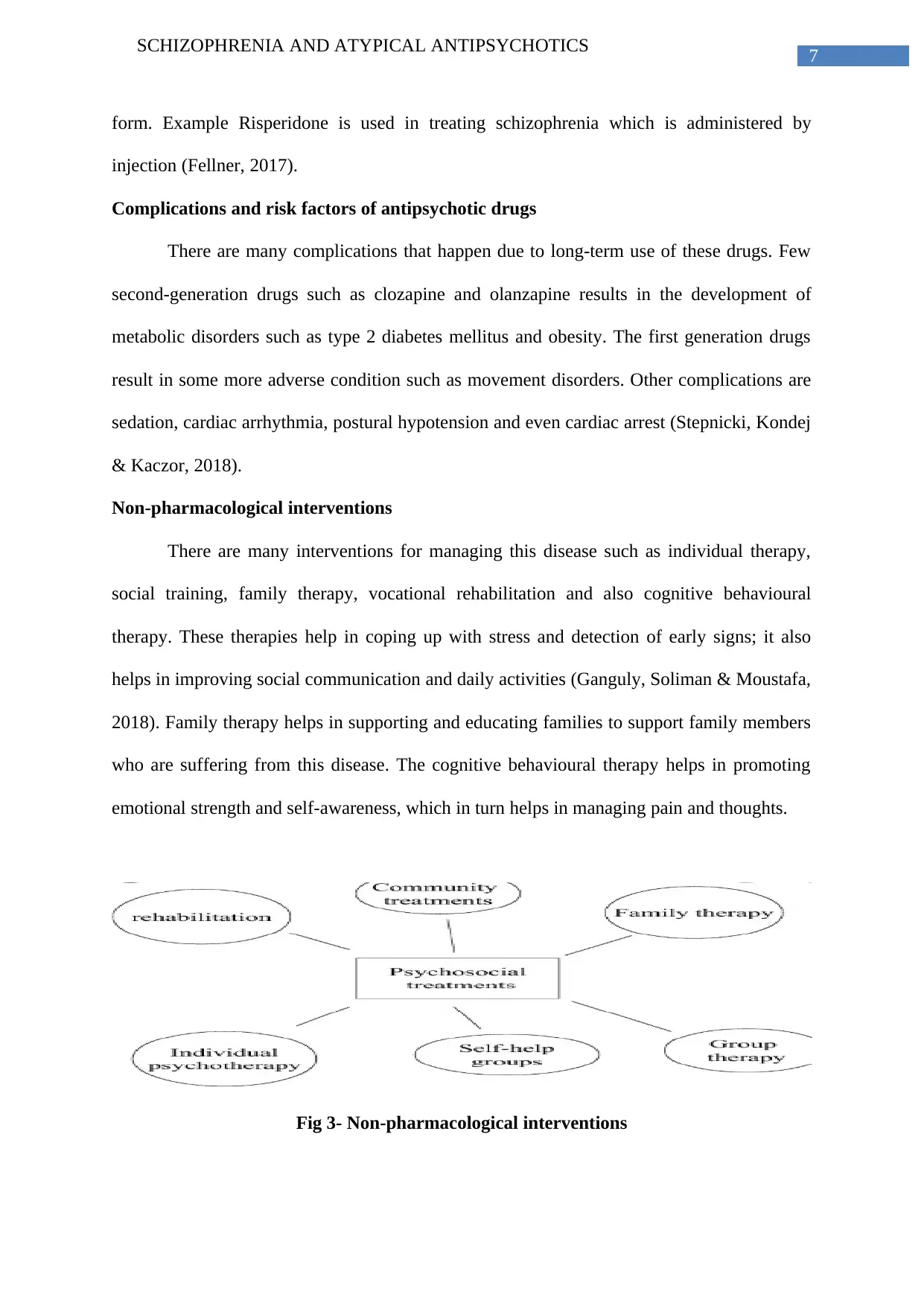
Non-pharmacological interventions
There are many interventions for managing this disease such as individual therapy,
social training, family therapy, vocational rehabilitation and also cognitive behavioural
therapy. These therapies help in coping up with stress and detection of early signs; it also
helps in improving social communication and daily activities (Ganguly, Soliman & Moustafa,
2018). Family therapy helps in supporting and educating families to support family members
who are suffering from this disease. The cognitive behavioural therapy helps in promoting
emotional strength and self-awareness, which in turn helps in managing pain and thoughts.
Fig 3- Non-pharmacological interventions
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
form. Example Risperidone is used in treating schizophrenia which is administered by
injection (Fellner, 2017).
Complications and risk factors of antipsychotic drugs
There are many complications that happen due to long-term use of these drugs. Few
second-generation drugs such as clozapine and olanzapine results in the development of
metabolic disorders such as type 2 diabetes mellitus and obesity. The first generation drugs
result in some more adverse condition such as movement disorders. Other complications are
sedation, cardiac arrhythmia, postural hypotension and even cardiac arrest (Stepnicki, Kondej
& Kaczor, 2018).
Non-pharmacological interventions
There are many interventions for managing this disease such as individual therapy,
social training, family therapy, vocational rehabilitation and also cognitive behavioural
therapy. These therapies help in coping up with stress and detection of early signs; it also
helps in improving social communication and daily activities (Ganguly, Soliman & Moustafa,
2018). Family therapy helps in supporting and educating families to support family members
who are suffering from this disease. The cognitive behavioural therapy helps in promoting
emotional strength and self-awareness, which in turn helps in managing pain and thoughts.
Fig 3- Non-pharmacological interventions
8
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
Nursing Management
The nurses play an important role in managing the patient who is suffering from this
disease. The assessment starts with recognising the sign and symptoms. It is also important
for maintaining a trustworthy relationship with the patient, along with guiding and helping
them with daily living activities and finally maintaining patient safety. The main goal is to
reduce the psychotic symptoms, prevent recurrence of acute episodes, understanding the
patient need and providing help to achieve a normal level of function (Mahone, Maphis &
Snow, 2016).
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
Nursing Management
The nurses play an important role in managing the patient who is suffering from this
disease. The assessment starts with recognising the sign and symptoms. It is also important
for maintaining a trustworthy relationship with the patient, along with guiding and helping
them with daily living activities and finally maintaining patient safety. The main goal is to
reduce the psychotic symptoms, prevent recurrence of acute episodes, understanding the
patient need and providing help to achieve a normal level of function (Mahone, Maphis &
Snow, 2016).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
References
Arion, D., Corradi, J. P., Tang, S., Datta, D., Boothe, F., He, A., ... & Lewis, D. A. (2015).
Distinctive transcriptome alterations of prefrontal pyramidal neurons in schizophrenia
and schizoaffective disorder. Molecular psychiatry, 20(11), 1397-1405.
https://doi.org/10.1038/mp.2014.171
Fellner C. (2017). New Schizophrenia Treatments Address Unmet Clinical Needs. P & T : a
peer-reviewed journal for formulary management, 42(2), 130–134. PMID: 28163559
Gaebel, W., & Zielasek, J. (2015). Schizophrenia in 2020: Trends in diagnosis and
therapy. Psychiatry and clinical neurosciences, 69(11), 661-673.
https://doi.org/10.1111/pcn.12322
Ganguly, P., Soliman, A., & Moustafa, A. A. (2018). Holistic Management of Schizophrenia
Symptoms Using Pharmacological and Non-pharmacological Treatment. Frontiers in
public health, 6, 166. https://doi.org/10.3389/fpubh.2018.00166
Givens, C. J. (2016). Adverse drug reactions associated with antipsychotics, antidepressants,
mood stabilizers, and stimulants. Nursing Clinics, 51(2), 309-321.
doi.org/10.1016/j.cnur.2016.01.013
Kesby, J. P., Eyles, D. W., McGrath, J. J., & Scott, J. G. (2018). Dopamine, psychosis and
schizophrenia: the widening gap between basic and clinical
neuroscience. Translational psychiatry, 8(1), 30. https://doi.org/10.1038/s41398-017-
0071-9
Kowalski, J., Pankowski, D., Lew-Starowicz, M., & Gawęda, Ł. (2017). Do specific
metacognitive training modules lead to specific cognitive changes among patients
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
References
Arion, D., Corradi, J. P., Tang, S., Datta, D., Boothe, F., He, A., ... & Lewis, D. A. (2015).
Distinctive transcriptome alterations of prefrontal pyramidal neurons in schizophrenia
and schizoaffective disorder. Molecular psychiatry, 20(11), 1397-1405.
https://doi.org/10.1038/mp.2014.171
Fellner C. (2017). New Schizophrenia Treatments Address Unmet Clinical Needs. P & T : a
peer-reviewed journal for formulary management, 42(2), 130–134. PMID: 28163559
Gaebel, W., & Zielasek, J. (2015). Schizophrenia in 2020: Trends in diagnosis and
therapy. Psychiatry and clinical neurosciences, 69(11), 661-673.
https://doi.org/10.1111/pcn.12322
Ganguly, P., Soliman, A., & Moustafa, A. A. (2018). Holistic Management of Schizophrenia
Symptoms Using Pharmacological and Non-pharmacological Treatment. Frontiers in
public health, 6, 166. https://doi.org/10.3389/fpubh.2018.00166
Givens, C. J. (2016). Adverse drug reactions associated with antipsychotics, antidepressants,
mood stabilizers, and stimulants. Nursing Clinics, 51(2), 309-321.
doi.org/10.1016/j.cnur.2016.01.013
Kesby, J. P., Eyles, D. W., McGrath, J. J., & Scott, J. G. (2018). Dopamine, psychosis and
schizophrenia: the widening gap between basic and clinical
neuroscience. Translational psychiatry, 8(1), 30. https://doi.org/10.1038/s41398-017-
0071-9
Kowalski, J., Pankowski, D., Lew-Starowicz, M., & Gawęda, Ł. (2017). Do specific
metacognitive training modules lead to specific cognitive changes among patients
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
diagnosed with schizophrenia? A single module effectiveness pilot
study. Psychosis, 9(3), 254-259. https://doi.org/10.1080/17522439.2017.1300186
Landek-Salgado, M. A., Faust, T. E., & Sawa, A. (2016). Molecular substrates of
schizophrenia: homeostatic signaling to connectivity. Molecular psychiatry, 21(1),
10–28. https://doi.org/10.1038/mp.2015.141
Mahone, I. H., Maphis, C. F., & Snow, D. E. (2016). Effective Strategies for Nurses
Empowering Clients With Schizophrenia: Medication Use as a Tool in
Recovery. Issues in mental health nursing, 37(5), 372–379.
https://doi.org/10.3109/01612840.2016.1157228
McCutcheon, R. A., Krystal, J. H., & Howes, O. D. (2020). Dopamine and glutamate in
schizophrenia: biology, symptoms and treatment. World psychiatry : official journal
of the World Psychiatric Association (WPA), 19(1), 15–33.
https://doi.org/10.1002/wps.20693
Rajan, S., Zalpuri, I., Harrington, A., Cimpeanu, C., Song, X., & Fan, X. (2016). Relationship
between serum uric acid level and cardiometabolic risks in nondiabetic patients with
schizophrenia. International clinical psychopharmacology, 31(1), 51-56.
DOI: https://doi.org/10.1097/YIC.0000000000000107
Steen, N. E., Dieset, I., Hope, S., Vedal, T. S., Smeland, O. B., Matson, W., ... & Jönsson, E.
G. (2020). Metabolic dysfunctions in the kynurenine pathway, noradrenergic and
purine metabolism in schizophrenia and bipolar disorders. Psychological
Medicine, 50(4), 595-606. DOI: https://doi.org/10.1017/S0033291719000400
Stegmayer, K., Bohlhalter, S., Vanbellingen, T., Federspiel, A., Moor, J., Wiest, R., ... &
Walther, S. (2016). Structural brain correlates of defective gesture performance in
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
diagnosed with schizophrenia? A single module effectiveness pilot
study. Psychosis, 9(3), 254-259. https://doi.org/10.1080/17522439.2017.1300186
Landek-Salgado, M. A., Faust, T. E., & Sawa, A. (2016). Molecular substrates of
schizophrenia: homeostatic signaling to connectivity. Molecular psychiatry, 21(1),
10–28. https://doi.org/10.1038/mp.2015.141
Mahone, I. H., Maphis, C. F., & Snow, D. E. (2016). Effective Strategies for Nurses
Empowering Clients With Schizophrenia: Medication Use as a Tool in
Recovery. Issues in mental health nursing, 37(5), 372–379.
https://doi.org/10.3109/01612840.2016.1157228
McCutcheon, R. A., Krystal, J. H., & Howes, O. D. (2020). Dopamine and glutamate in
schizophrenia: biology, symptoms and treatment. World psychiatry : official journal
of the World Psychiatric Association (WPA), 19(1), 15–33.
https://doi.org/10.1002/wps.20693
Rajan, S., Zalpuri, I., Harrington, A., Cimpeanu, C., Song, X., & Fan, X. (2016). Relationship
between serum uric acid level and cardiometabolic risks in nondiabetic patients with
schizophrenia. International clinical psychopharmacology, 31(1), 51-56.
DOI: https://doi.org/10.1097/YIC.0000000000000107
Steen, N. E., Dieset, I., Hope, S., Vedal, T. S., Smeland, O. B., Matson, W., ... & Jönsson, E.
G. (2020). Metabolic dysfunctions in the kynurenine pathway, noradrenergic and
purine metabolism in schizophrenia and bipolar disorders. Psychological
Medicine, 50(4), 595-606. DOI: https://doi.org/10.1017/S0033291719000400
Stegmayer, K., Bohlhalter, S., Vanbellingen, T., Federspiel, A., Moor, J., Wiest, R., ... &
Walther, S. (2016). Structural brain correlates of defective gesture performance in

11
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
schizophrenia. Cortex, 78, 125-137. Retrieved from
https://doi.org/10.1016/j.cortex.2016.02.014
Stępnicki, P., Kondej, M., & Kaczor, A. A. (2018). Current Concepts and Treatments of
Schizophrenia. Molecules (Basel, Switzerland), 23(8), 2087.
https://doi.org/10.3390/molecules23082087
SCHIZOPHRENIA AND ATYPICAL ANTIPSYCHOTICS
schizophrenia. Cortex, 78, 125-137. Retrieved from
https://doi.org/10.1016/j.cortex.2016.02.014
Stępnicki, P., Kondej, M., & Kaczor, A. A. (2018). Current Concepts and Treatments of
Schizophrenia. Molecules (Basel, Switzerland), 23(8), 2087.
https://doi.org/10.3390/molecules23082087
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





