NRSG263: Sedative Medications Use Controversy in Mental Health
VerifiedAdded on 2022/08/29
|12
|3231
|25
Essay
AI Summary
This essay, prepared for an NRSG263 assignment, examines the controversy surrounding the use of sedative medications, particularly psychotropic drugs, in mental health care. It focuses on the challenges of managing challenging behaviors and mental disorders in individuals with intellectual disabilities. The essay highlights concerns such as poly-pharmacy, adverse side effects, and coercive practices in medication administration. It discusses the side effects of psychotropic medicines, including metabolic and cardiac problems, and the challenges faced by registered nurses in administering these medications. The essay also explores the extensive use of psychotropic medications, sometimes without proper diagnoses, and the lack of evidence to guide changes in dispensing practices. It emphasizes the need for research to determine the efficacy and safety of these medications and the importance of adequate support for nurses to deliver optimal mental health care. The essay concludes by emphasizing the need for a nuanced approach to the use of sedative medications, considering the potential side effects and the importance of patient-centered care.

Running head: SEDATIVE MEDICATIONS 1
Controversy Related to the Use of Sedative Medications
Name
Institution
Controversy Related to the Use of Sedative Medications
Name
Institution
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
SEDATIVE MEDICATIONS 2
Controversy Related to the Use of Sedative Medications
Introduction
Psychiatric specialists prescribe sedative medicines to persons with intellectual
disabilities (ID) to manage a comorbid mental disorder or challenging behaviors, including
aggressive tendencies, self-harm habits, property destruction, and pica (Hercelinskyj &
Alexander, 2019). Such challenging situations can give caregivers difficulty in providing
mental health care. Often, with or without the presence of multiple psychiatric problems or
symptoms or challenging behaviours, overuse of sedative medicines can occur albeit in some
cases, these drugs can be justified and included in the treatment plan. Also, the overuse of
such sedative medicines, for example psychotropic drugs, is not supported within mental
health services, including across Australian states and territories. Generally, however, using
sedative medicines to manage problem behaviours is considered controversial and is
described as being highly coercive and linked to substantial side effects on caregivers and
patients.
Controversy Related to the Use of Psychotropic Medications to Control Behaviours and
Manage Symptoms for People who Experience Mental Illness.
Psychotropic medications refer to any medicines that can affect the mind, feelings as
well as behaviour, and they include antidepressants, benzodiazepines besides antipsychotics.
Crucial reasons for the concerns on psychotropic prescription for managing problem behavior
include poly-pharmacy – using higher than prescribed dosage; adverse side effects that could
be difficult to evaluate, and inappropriate medicine consumption to offset the harmful side
effects; overall little or no statistics to support the effectiveness, efficacy, and safety of
psychotropic drugs to alleviate challenging behavior such as violence; expired license use of
psychiatric drugs; and coercive medication or prescribing medicines regardless of whether a
Controversy Related to the Use of Sedative Medications
Introduction
Psychiatric specialists prescribe sedative medicines to persons with intellectual
disabilities (ID) to manage a comorbid mental disorder or challenging behaviors, including
aggressive tendencies, self-harm habits, property destruction, and pica (Hercelinskyj &
Alexander, 2019). Such challenging situations can give caregivers difficulty in providing
mental health care. Often, with or without the presence of multiple psychiatric problems or
symptoms or challenging behaviours, overuse of sedative medicines can occur albeit in some
cases, these drugs can be justified and included in the treatment plan. Also, the overuse of
such sedative medicines, for example psychotropic drugs, is not supported within mental
health services, including across Australian states and territories. Generally, however, using
sedative medicines to manage problem behaviours is considered controversial and is
described as being highly coercive and linked to substantial side effects on caregivers and
patients.
Controversy Related to the Use of Psychotropic Medications to Control Behaviours and
Manage Symptoms for People who Experience Mental Illness.
Psychotropic medications refer to any medicines that can affect the mind, feelings as
well as behaviour, and they include antidepressants, benzodiazepines besides antipsychotics.
Crucial reasons for the concerns on psychotropic prescription for managing problem behavior
include poly-pharmacy – using higher than prescribed dosage; adverse side effects that could
be difficult to evaluate, and inappropriate medicine consumption to offset the harmful side
effects; overall little or no statistics to support the effectiveness, efficacy, and safety of
psychotropic drugs to alleviate challenging behavior such as violence; expired license use of
psychiatric drugs; and coercive medication or prescribing medicines regardless of whether a
SEDATIVE MEDICATIONS 3
patient consents or not that often happens among persons with ID (Deb, 2020; Niven et al.,
2017). Thus, understanding the various concerns in detail is crucial for health practice.
a) Side Effects of Psychotropic Medicines
Poor control of the drugs’ side effects can hinder effective treatment, impair quality of
life, as well as cause several harmful health consequences in people with ID (Roughead et al.,
2017). In Australia, estimates from the 2010 National Psychosis Survey were that over 80%
of the population on psychotropic drugs experience side effects. Also, one in three lives with
moderate to severe impairments because of drug-associated side effects (Roughead et al.,
2017). More than 60% of people on antipsychotic drugs also experienced side effects such as
poor memory and losing attentiveness, and agitation, which exacerbate challenging behavior.
Similarly, individuals who practiced poly-pharmacy testified that they experienced
more side effects than people on a single antipsychotic medicine (McLaughlin-Beltz, 2015).
Another study cited that risperidone alone reduced auto-aggressive behaviour, but when
mixed with citalopram, elevated self-harm and aggressive behaviours were observed (Häβler
et al., 2014). Treating such side effects is debilitating, and can impact the quality of life if not
well-managed (Roughead et al., 2017; O’Dwyer et al., 2018).
A clinical practice guideline for the management of mental illnesses recommended for
Australia and New Zealand shows distinct differences in terms of the side effects resulting
from old generation psychotropic drugs and new generation psychotropic medications. For
instance, evidence shows that young persons are specifically vulnerable to the adverse effects
of psychiatric medications, unless the young individual has an acute mental disease, and
needs immediate medical attention (Galletly et al., 2016). Mental health specialists
recommend and prefer second-generation antipsychotic (SGA) medicines to first-generation
antipsychotics (FGA) because the former can be tolerated better than the latter, and have
better extrapyramidal side effects characteristics (Pillay, B.Sc. et al., 2017). However, SGAs
patient consents or not that often happens among persons with ID (Deb, 2020; Niven et al.,
2017). Thus, understanding the various concerns in detail is crucial for health practice.
a) Side Effects of Psychotropic Medicines
Poor control of the drugs’ side effects can hinder effective treatment, impair quality of
life, as well as cause several harmful health consequences in people with ID (Roughead et al.,
2017). In Australia, estimates from the 2010 National Psychosis Survey were that over 80%
of the population on psychotropic drugs experience side effects. Also, one in three lives with
moderate to severe impairments because of drug-associated side effects (Roughead et al.,
2017). More than 60% of people on antipsychotic drugs also experienced side effects such as
poor memory and losing attentiveness, and agitation, which exacerbate challenging behavior.
Similarly, individuals who practiced poly-pharmacy testified that they experienced
more side effects than people on a single antipsychotic medicine (McLaughlin-Beltz, 2015).
Another study cited that risperidone alone reduced auto-aggressive behaviour, but when
mixed with citalopram, elevated self-harm and aggressive behaviours were observed (Häβler
et al., 2014). Treating such side effects is debilitating, and can impact the quality of life if not
well-managed (Roughead et al., 2017; O’Dwyer et al., 2018).
A clinical practice guideline for the management of mental illnesses recommended for
Australia and New Zealand shows distinct differences in terms of the side effects resulting
from old generation psychotropic drugs and new generation psychotropic medications. For
instance, evidence shows that young persons are specifically vulnerable to the adverse effects
of psychiatric medications, unless the young individual has an acute mental disease, and
needs immediate medical attention (Galletly et al., 2016). Mental health specialists
recommend and prefer second-generation antipsychotic (SGA) medicines to first-generation
antipsychotics (FGA) because the former can be tolerated better than the latter, and have
better extrapyramidal side effects characteristics (Pillay, B.Sc. et al., 2017). However, SGAs
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
SEDATIVE MEDICATIONS 4
can still cause serious adverse effects such as metabolic besides cardiac problems. In terms of
efficacy and contraindications, each individual with a mental illness is affected differently
(Galletly et al., 2016). A close therapeutic relationship should exist between a person with
mental illness or challenging behavior and the clinicians for the best possible care.
b) Extensive Use of Psychotropic Medicines
In their findings, Sheehan et al. (2015) found out that more people with ID have been
managed with psychotropic medicines exceeding the actual number of people with a recorded
psychiatric disease in the United Kingdom. Psychotropic prescriptions are also given to
individuals without documented severe mental disorders but have experience of challenging
behavior like the destruction of property and aggressive habits (Valdovinos et al., 2016;
Sheehan et al., 2015). Equally, sometimes prescriptions are made without true psychiatric
diagnoses, and this is a primary concern, in situations where consumers size keeps increasing
(Finkelhor & Johnson, 2015). In other instances, chances of using other antipsychotic drugs
are high, for example, in people with multiple psychological problems such as ID, autism,
and dementia, among others, which will usually indicate the departing of practice from
evidence-based clinical protocols (Sheehan et al., 2015). Such prescriptions also open doors
for unnecessary medicines that may come with adverse health outcomes and a burden to
healthcare. For instance, some of these medications referred to as off-label psychotropic
practice can be prescribed for use other than their licensed purpose (Sheehan et al., 2015; Van
der Plaat et al., 2019).
Another concern is that little, or no evidence exists that can guide the making of
changes required in the dispensing of psychotropic drugs for individuals with challenging
behaviour (Sheehan et al., 2015). In another study, Sheehan (2018) highlights that
psychotropic drug use for ID populations raises complicated problems, not least due to the
absence of evidence, which exists on the topic. However, psychotropic medications can only
can still cause serious adverse effects such as metabolic besides cardiac problems. In terms of
efficacy and contraindications, each individual with a mental illness is affected differently
(Galletly et al., 2016). A close therapeutic relationship should exist between a person with
mental illness or challenging behavior and the clinicians for the best possible care.
b) Extensive Use of Psychotropic Medicines
In their findings, Sheehan et al. (2015) found out that more people with ID have been
managed with psychotropic medicines exceeding the actual number of people with a recorded
psychiatric disease in the United Kingdom. Psychotropic prescriptions are also given to
individuals without documented severe mental disorders but have experience of challenging
behavior like the destruction of property and aggressive habits (Valdovinos et al., 2016;
Sheehan et al., 2015). Equally, sometimes prescriptions are made without true psychiatric
diagnoses, and this is a primary concern, in situations where consumers size keeps increasing
(Finkelhor & Johnson, 2015). In other instances, chances of using other antipsychotic drugs
are high, for example, in people with multiple psychological problems such as ID, autism,
and dementia, among others, which will usually indicate the departing of practice from
evidence-based clinical protocols (Sheehan et al., 2015). Such prescriptions also open doors
for unnecessary medicines that may come with adverse health outcomes and a burden to
healthcare. For instance, some of these medications referred to as off-label psychotropic
practice can be prescribed for use other than their licensed purpose (Sheehan et al., 2015; Van
der Plaat et al., 2019).
Another concern is that little, or no evidence exists that can guide the making of
changes required in the dispensing of psychotropic drugs for individuals with challenging
behaviour (Sheehan et al., 2015). In another study, Sheehan (2018) highlights that
psychotropic drug use for ID populations raises complicated problems, not least due to the
absence of evidence, which exists on the topic. However, psychotropic medications can only
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
SEDATIVE MEDICATIONS 5
confer health benefits to individuals with mental problems and problem behavior if they are
backed by research evidence (Sheehan, 2018; Glover et al., 2014). Thus, while using
psychotropic drugs in persons with ID for challenging behaviours, there is a need for
adequate statistics to determine the efficacy as well as safety of antipsychotic medications.
Although there is vast condemnation as well as inadequate evidence on the safety and
efficacy of simultaneous use of multiple psychotropic drugs, also known as poly-pharmacy,
this practice is still extensive. On the other hand, the benefits besides adverse effects
associated with the combination of antipsychotics with another set of psychotropics,
particularly for challenging behaviors in adults with ID, remains questionable. Through
deprescribing, for example in a pilot randomized control trial of drug minimization of 22
adults with ID managed using risperidone for challenging behaviour with no record of current
or past mental illness, 59% of the 22 individuals progressed to the next level of reduction at
the end of the research (O’Dwyer et al., 2018). However, the rest did not show clinical
improvement in levels of aggressive behaviour (O’Dwyer et al., 2018). Haider et al. (2014)
found out that poly-pharmacy was linked to a more significant number of visits to general
practitioners and moderately or poorly reported health status. For such cases, there is a need
to regularly review medication in people with ID, and particularly when poly-pharmacy
presents.
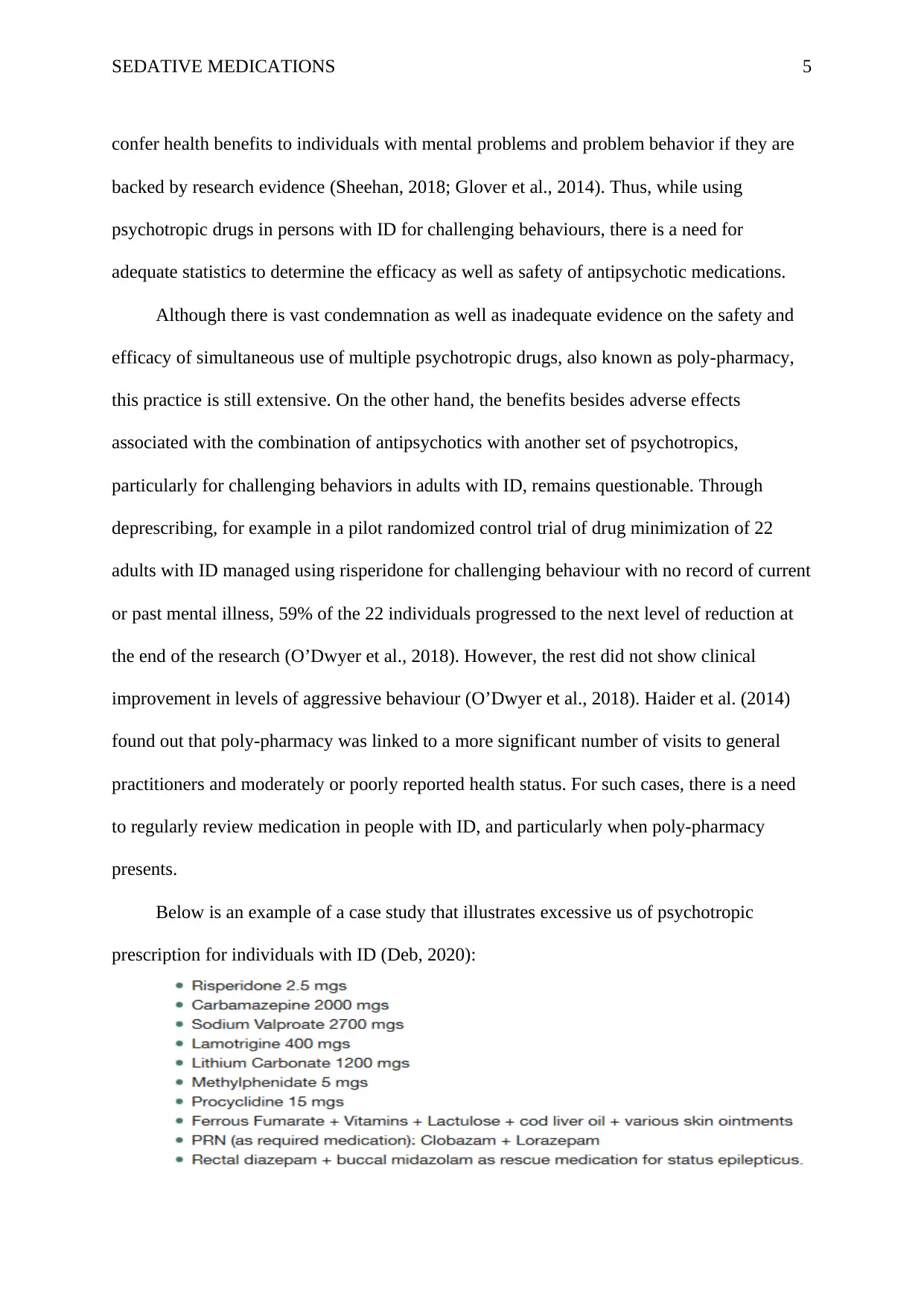
Below is an example of a case study that illustrates excessive us of psychotropic
prescription for individuals with ID (Deb, 2020):
confer health benefits to individuals with mental problems and problem behavior if they are
backed by research evidence (Sheehan, 2018; Glover et al., 2014). Thus, while using
psychotropic drugs in persons with ID for challenging behaviours, there is a need for
adequate statistics to determine the efficacy as well as safety of antipsychotic medications.
Although there is vast condemnation as well as inadequate evidence on the safety and
efficacy of simultaneous use of multiple psychotropic drugs, also known as poly-pharmacy,
this practice is still extensive. On the other hand, the benefits besides adverse effects
associated with the combination of antipsychotics with another set of psychotropics,
particularly for challenging behaviors in adults with ID, remains questionable. Through
deprescribing, for example in a pilot randomized control trial of drug minimization of 22
adults with ID managed using risperidone for challenging behaviour with no record of current
or past mental illness, 59% of the 22 individuals progressed to the next level of reduction at
the end of the research (O’Dwyer et al., 2018). However, the rest did not show clinical
improvement in levels of aggressive behaviour (O’Dwyer et al., 2018). Haider et al. (2014)
found out that poly-pharmacy was linked to a more significant number of visits to general
practitioners and moderately or poorly reported health status. For such cases, there is a need
to regularly review medication in people with ID, and particularly when poly-pharmacy
presents.
Below is an example of a case study that illustrates excessive us of psychotropic
prescription for individuals with ID (Deb, 2020):
SEDATIVE MEDICATIONS 6
This case study presents a list containing a daily dosage of drugs for adults with ID.
The use of sodium valproate besides carbamazepine is beyond the recommended dosage
(Jackson et al., 2015; Gierbolini et al., 2016). When taken together with sodium valproate,
then the lamotrigine dosage must be lower. Risperidone, besides the four antiepileptics
(carbamazepine, lamotrigine, and sodium valproate), are already prescribed, so lithium
should not be needed in the list to manage problem behavior. The formulation of these
prescriptions is improper, and it looks like this is a desperate combination to avert
challenging behavior (Deb, 2020).
c) Coercive Means during Psychotropic Medication for Challenging Behavior or Mental
Illness or Both
Coercive drug administration is allowed in mental health services, albeit under strict
conditions. However, use of such means during care has been criticized because of the nature
of its use without patient’s consent and being invasive. Patients with challenging behavior
including aggression may become the root of fear, stigma and isolation, and coercive
situations during psychotropic drug administration (Slemon et al., 2017). Forced medication
can also result from the assaultive or threats of such acts. In another study, patients with risky
behavior like violence were put under chemical restraint through rapid tranquilization
(Parker, C., 2015). However, the controversy related to coercive treatment emanates from the
fact that there is a dearth of data in coercive drug prescription as well as literature on every
aspect concerning this contentious practice.
Challenging Aspects for Registered Nurses who Administer Psychotropic Medication
to Patients with Challenging Behaviours
According to (Hercelinskyj & Alexander, 2019), challenging behaviors include
aggression, self-harm, or harm towards other people. Sometimes such actions may appear
spontaneous, having no identifiable cause; however, challenging behavior always occurs; as a
This case study presents a list containing a daily dosage of drugs for adults with ID.
The use of sodium valproate besides carbamazepine is beyond the recommended dosage
(Jackson et al., 2015; Gierbolini et al., 2016). When taken together with sodium valproate,
then the lamotrigine dosage must be lower. Risperidone, besides the four antiepileptics
(carbamazepine, lamotrigine, and sodium valproate), are already prescribed, so lithium
should not be needed in the list to manage problem behavior. The formulation of these
prescriptions is improper, and it looks like this is a desperate combination to avert
challenging behavior (Deb, 2020).
c) Coercive Means during Psychotropic Medication for Challenging Behavior or Mental
Illness or Both
Coercive drug administration is allowed in mental health services, albeit under strict
conditions. However, use of such means during care has been criticized because of the nature
of its use without patient’s consent and being invasive. Patients with challenging behavior
including aggression may become the root of fear, stigma and isolation, and coercive
situations during psychotropic drug administration (Slemon et al., 2017). Forced medication
can also result from the assaultive or threats of such acts. In another study, patients with risky
behavior like violence were put under chemical restraint through rapid tranquilization
(Parker, C., 2015). However, the controversy related to coercive treatment emanates from the
fact that there is a dearth of data in coercive drug prescription as well as literature on every
aspect concerning this contentious practice.
Challenging Aspects for Registered Nurses who Administer Psychotropic Medication
to Patients with Challenging Behaviours
According to (Hercelinskyj & Alexander, 2019), challenging behaviors include
aggression, self-harm, or harm towards other people. Sometimes such actions may appear
spontaneous, having no identifiable cause; however, challenging behavior always occurs; as a
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
SEDATIVE MEDICATIONS 7
result, some underlying reason. For example, Parker (2015) indicates that some of the causes
include; physical (ineffective medicines that cause problems, pain, epilepsy), cognitive (any
reason hindering proper communication, autism besides dementia), substance abuse (alcohol
intoxication); and psychological stress and fear. A causal factor like the adverse effects of
psychotropic drugs raise controversies on the use of such drugs in the first place. Therefore,
registered nurses (RNs) will experience challenges while administering psychiatric medicines
and care to individuals who pose a significant risk of harm to themselves and others.
Research shows that some of the critical challenges faced by the psychiatric nursing practice
include; consumers of mental health care sometimes deny being mentally ill; problems
related to exposure to mental health care users’ unpredictable behavior, which make patient
care difficult; increased incidences of aggressive behaviors and violence; psychiatric nurses
experiencing feelings of irritation besides frustrations, besides burnout (Joubert & Bhagwan,
2018; Parker, 2015). Joubert & Bhagwan (2018) also cited that in Australian psychiatric
institutions, which operated in unpredictable ambient, reported feeling emotionally exhausted
(Joubert & Bhagwan, 2018). While administering drugs, health caregivers must evaluate the
risks to either the user or to other persons, the implications of a potentially intensifying
violent situation, and risks linked to potential harmful contraindications of drugs (Parker,
2015). In such circumstances, nurses must receive adequate support to deliver optimal mental
health care by applying principles of recovery-oriented care, even though they are trained
professionally to withstand such challenging environments.
Conclusion
Overall, sedative medications to manage challenging behaviors and/or mental illnesses
among people raises are considered controversial and linked to substantial side effects on
patients and health practitioners. Concerns arising from the psychotropic prescriptions
emanate from various issues surrounding psychiatric care, and they include poly-pharmacy,
result, some underlying reason. For example, Parker (2015) indicates that some of the causes
include; physical (ineffective medicines that cause problems, pain, epilepsy), cognitive (any
reason hindering proper communication, autism besides dementia), substance abuse (alcohol
intoxication); and psychological stress and fear. A causal factor like the adverse effects of
psychotropic drugs raise controversies on the use of such drugs in the first place. Therefore,
registered nurses (RNs) will experience challenges while administering psychiatric medicines
and care to individuals who pose a significant risk of harm to themselves and others.
Research shows that some of the critical challenges faced by the psychiatric nursing practice
include; consumers of mental health care sometimes deny being mentally ill; problems
related to exposure to mental health care users’ unpredictable behavior, which make patient
care difficult; increased incidences of aggressive behaviors and violence; psychiatric nurses
experiencing feelings of irritation besides frustrations, besides burnout (Joubert & Bhagwan,
2018; Parker, 2015). Joubert & Bhagwan (2018) also cited that in Australian psychiatric
institutions, which operated in unpredictable ambient, reported feeling emotionally exhausted
(Joubert & Bhagwan, 2018). While administering drugs, health caregivers must evaluate the
risks to either the user or to other persons, the implications of a potentially intensifying
violent situation, and risks linked to potential harmful contraindications of drugs (Parker,
2015). In such circumstances, nurses must receive adequate support to deliver optimal mental
health care by applying principles of recovery-oriented care, even though they are trained
professionally to withstand such challenging environments.
Conclusion
Overall, sedative medications to manage challenging behaviors and/or mental illnesses
among people raises are considered controversial and linked to substantial side effects on
patients and health practitioners. Concerns arising from the psychotropic prescriptions
emanate from various issues surrounding psychiatric care, and they include poly-pharmacy,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
SEDATIVE MEDICATIONS 8
adverse side effects, coercive psychotropic medication, inappropriate medications which
deemed unnecessary, and little or no evidence to guide practice. Research shows that
psychotropic medications are accompanied by several adverse effects, including metabolic
and cardiac problems such as high and low blood pressure, weight gain, and constipation.
Also, extensive use of psychotropic medications, including poly-pharmacy, is linked to
adverse health consequences, but its benefits remain questionable. On the other hand,
research shows that some of the critical challenges faced by the psychiatric nursing practice
include; consumers of mental health care sometimes deny being mentally ill; problems
related to exposure to mental health care users' unpredictable behavior, which make patient
care difficult; increased incidences of aggressive behaviors and violence; psychiatric nurses
experiencing feelings of irritation besides frustrations, besides burnout. Therefore, adequate
research is needed for effective use of sedative medications, and nurses need sufficient
support to deliver optimal mental health care by applying principles of recovery-oriented
care.
References
adverse side effects, coercive psychotropic medication, inappropriate medications which
deemed unnecessary, and little or no evidence to guide practice. Research shows that
psychotropic medications are accompanied by several adverse effects, including metabolic
and cardiac problems such as high and low blood pressure, weight gain, and constipation.
Also, extensive use of psychotropic medications, including poly-pharmacy, is linked to
adverse health consequences, but its benefits remain questionable. On the other hand,
research shows that some of the critical challenges faced by the psychiatric nursing practice
include; consumers of mental health care sometimes deny being mentally ill; problems
related to exposure to mental health care users' unpredictable behavior, which make patient
care difficult; increased incidences of aggressive behaviors and violence; psychiatric nurses
experiencing feelings of irritation besides frustrations, besides burnout. Therefore, adequate
research is needed for effective use of sedative medications, and nurses need sufficient
support to deliver optimal mental health care by applying principles of recovery-oriented
care.
References
SEDATIVE MEDICATIONS 9
Aged Care Quality and Safety Commission. (2020). Psychotropic medications used in
Australia - information for aged care. Retrieved March 28, 2020, from
https://www.agedcarequality.gov.au/resources/psychotropic-medications-used-
australia-information-aged-care
Deb, S. (2020). The Use of Medication for the Management of Problem (Challenging)
Behaviour in Adults who have Intellectual Disabilities. Understanding Intellectual
Disability and Health | Intellectual Disability and Health. Retrieved March 27, 2020,
from https://www.intellectualdisability.info/mental-health/articles/the-use-of-
medications-for-the-management-of-problem-behaviours-in-adults-who-have-
intellectual-disabilities
Finkelhor, D., & Johnson, M. (2015). Has Psychiatric Medication Reduced Crime and
Delinquency? Trauma, Violence, & Abuse, 18(3), 339-347.
https://doi.org/10.1177/1524838015620817
Galletly, C., Castle, D., Dark, F., Humberstone, V., Jablensky, A., Killackey, E.,
Kulkarni, J., McGorry, P., Nielssen, O., & Tran, N. (2016). Royal Australian and New
Zealand College of Psychiatrists clinical practice guidelines for the management of
schizophrenia and related disorders. Australian & New Zealand Journal of Psychiatry,
50(5), 410-472. https://doi.org/10.1177/0004867416641195
Gierbolini, J., Giarratano, M., & Benbadis, S. R. (2016). Carbamazepine-related antiepileptic
drugs for the treatment of epilepsy - a comparative review. Expert Opinion on
Pharmacotherapy, 17(7), 885-888. https://doi.org/10.1517/14656566.2016.1168399
Glover, G., Bernard, S., Branford, D., Holland, A., & Strydom, A. (2014). Use of medication
for challenging behaviour in people with intellectual disability. British Journal of
Psychiatry, 205(1), 6-7. https://doi.org/10.1192/bjp.bp.113.141267
Aged Care Quality and Safety Commission. (2020). Psychotropic medications used in
Australia - information for aged care. Retrieved March 28, 2020, from
https://www.agedcarequality.gov.au/resources/psychotropic-medications-used-
australia-information-aged-care
Deb, S. (2020). The Use of Medication for the Management of Problem (Challenging)
Behaviour in Adults who have Intellectual Disabilities. Understanding Intellectual
Disability and Health | Intellectual Disability and Health. Retrieved March 27, 2020,
from https://www.intellectualdisability.info/mental-health/articles/the-use-of-
medications-for-the-management-of-problem-behaviours-in-adults-who-have-
intellectual-disabilities
Finkelhor, D., & Johnson, M. (2015). Has Psychiatric Medication Reduced Crime and
Delinquency? Trauma, Violence, & Abuse, 18(3), 339-347.
https://doi.org/10.1177/1524838015620817
Galletly, C., Castle, D., Dark, F., Humberstone, V., Jablensky, A., Killackey, E.,
Kulkarni, J., McGorry, P., Nielssen, O., & Tran, N. (2016). Royal Australian and New
Zealand College of Psychiatrists clinical practice guidelines for the management of
schizophrenia and related disorders. Australian & New Zealand Journal of Psychiatry,
50(5), 410-472. https://doi.org/10.1177/0004867416641195
Gierbolini, J., Giarratano, M., & Benbadis, S. R. (2016). Carbamazepine-related antiepileptic
drugs for the treatment of epilepsy - a comparative review. Expert Opinion on
Pharmacotherapy, 17(7), 885-888. https://doi.org/10.1517/14656566.2016.1168399
Glover, G., Bernard, S., Branford, D., Holland, A., & Strydom, A. (2014). Use of medication
for challenging behaviour in people with intellectual disability. British Journal of
Psychiatry, 205(1), 6-7. https://doi.org/10.1192/bjp.bp.113.141267
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
SEDATIVE MEDICATIONS 10
Häβler, F., Thome, J., & Reis, O. (2014). Polypharmacy in the treatment of subjects with
intellectual disability. Journal of Neural Transmission, 122(S1), 93-100.
https://doi.org/10.1007/s00702-014-1219-x
Haider, S. I., Ansari, Z., Vaughan, L., Matters, H., & Emerson, E. (2014). Prevalence and
factors associated with polypharmacy in Victorian adults with intellectual disability.
Research in Developmental Disabilities, 35(11), 3071-3080.
https://doi.org/10.1016/j.ridd.2014.07.060
Hercelinskyj, G., & Alexander, L. (2019). Mental Health Nursing: Applying Theory to
Practice. Cengage AU.
Jackson, J., McCollum, B., Ognibene, J., Diaz, F. J., & De Leon, J. (2015). Three Patients
Needing High Doses of Valproic Acid to Get Therapeutic Concentrations. Case
Reports in Psychiatry, 2015, 1-12. https://doi.org/10.1155/2015/542862
Joubert, P. D., & Bhagwan, R. (2018). An empirical study of the challenging roles of
psychiatric nurses at in-patient psychiatric facilities and its implications for nursing
education. International Journal of Africa Nursing Sciences, 9, 49-56.
https://doi.org/10.1016/j.ijans.2018.08.001
McLaughlin-Beltz, S. (2015). Polypharmacy in Individuals with Intellectual Disability.
Journal of Psychology & Clinical Psychiatry, 3(2).
https://doi.org/10.15406/jpcpy.2015.03.00126
Niven, A., Goodey, R., Webb, A., & Shankar, R. (2017). The use of psychotropic
medication for people with intellectual disabilities and behaviours that challenge in the
context of a community multidisciplinary team approach. British Journal of Learning
Disabilities, 46(1), 4-9. https://doi.org/10.1111/bld.12206
O’Dwyer, M., McCallion, P., McCarron, M., & Henman, M. (2018). Medication use and
potentially inappropriate prescribing in older adults with intellectual disabilities: a
Häβler, F., Thome, J., & Reis, O. (2014). Polypharmacy in the treatment of subjects with
intellectual disability. Journal of Neural Transmission, 122(S1), 93-100.
https://doi.org/10.1007/s00702-014-1219-x
Haider, S. I., Ansari, Z., Vaughan, L., Matters, H., & Emerson, E. (2014). Prevalence and
factors associated with polypharmacy in Victorian adults with intellectual disability.
Research in Developmental Disabilities, 35(11), 3071-3080.
https://doi.org/10.1016/j.ridd.2014.07.060
Hercelinskyj, G., & Alexander, L. (2019). Mental Health Nursing: Applying Theory to
Practice. Cengage AU.
Jackson, J., McCollum, B., Ognibene, J., Diaz, F. J., & De Leon, J. (2015). Three Patients
Needing High Doses of Valproic Acid to Get Therapeutic Concentrations. Case
Reports in Psychiatry, 2015, 1-12. https://doi.org/10.1155/2015/542862
Joubert, P. D., & Bhagwan, R. (2018). An empirical study of the challenging roles of
psychiatric nurses at in-patient psychiatric facilities and its implications for nursing
education. International Journal of Africa Nursing Sciences, 9, 49-56.
https://doi.org/10.1016/j.ijans.2018.08.001
McLaughlin-Beltz, S. (2015). Polypharmacy in Individuals with Intellectual Disability.
Journal of Psychology & Clinical Psychiatry, 3(2).
https://doi.org/10.15406/jpcpy.2015.03.00126
Niven, A., Goodey, R., Webb, A., & Shankar, R. (2017). The use of psychotropic
medication for people with intellectual disabilities and behaviours that challenge in the
context of a community multidisciplinary team approach. British Journal of Learning
Disabilities, 46(1), 4-9. https://doi.org/10.1111/bld.12206
O’Dwyer, M., McCallion, P., McCarron, M., & Henman, M. (2018). Medication use and
potentially inappropriate prescribing in older adults with intellectual disabilities: a
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
SEDATIVE MEDICATIONS 11
neglected area of research. Therapeutic Advances in Drug Safety, 9(9), 535-557.
https://doi.org/10.1177/2042098618782785
Parker, C. (2015). Tranquillisation of patients with aggressive or challenging behaviour. The
Pharmaceutical Journal. https://doi.org/10.1211/pj.2015.20068706
Pillay, B.Sc., J., Boylan, M.D., Ph.D., FRCPC, K., & Carrey, FRCPC, N. (2017). First- and
Second-Generation Antipsychotics in Children and Young Adults: Systematic Review
Update. https://doi.org/10.23970/ahrqepccer184
Roughead, L., Proctor, N., Westaway, K., Sluggett, J., & Alderman, C. (2017). Medication
safety in mental health. Sydney: ACSQHC.
https://www.safetyandquality.gov.au/sites/default/files/migrated/Medication-Safety-in-
Mental-Health-final-report-2017.pdf
Sheehan, R. (2018). Optimising psychotropic medication use. Tizard Learning Disability
Review, 23(1), 22-26. https://doi.org/10.1108/tldr-07-2017-0031
Sheehan, R., Hassiotis, A., Walters, K., Osborn, D., Strydom, A., & Horsfall, L. (2015).
Mental illness, challenging behaviour, and psychotropic drug prescribing in people
with intellectual disability: UK population based cohort study. BMJ, h4326.
https://doi.org/10.1136/bmj.h4326
Slemon, A., Jenkins, E., & Bungay, V. (2017). Safety in psychiatric inpatient care: The
impact of risk management culture on mental health nursing practice. Nursing Inquiry,
24(4), e12199. https://doi.org/10.1111/nin.12199
Valdovinos, M. G., Henninger-McMahon, M., Schieber, E., Beard, L., Conley, B., &
Haas, A. (2016). Assessing the impact of psychotropic medication changes on
challenging behavior of individuals with intellectual disabilities. International Journal
of Developmental Disabilities, 62(3), 200-211.
https://doi.org/10.1080/20473869.2016.1177301
neglected area of research. Therapeutic Advances in Drug Safety, 9(9), 535-557.
https://doi.org/10.1177/2042098618782785
Parker, C. (2015). Tranquillisation of patients with aggressive or challenging behaviour. The
Pharmaceutical Journal. https://doi.org/10.1211/pj.2015.20068706
Pillay, B.Sc., J., Boylan, M.D., Ph.D., FRCPC, K., & Carrey, FRCPC, N. (2017). First- and
Second-Generation Antipsychotics in Children and Young Adults: Systematic Review
Update. https://doi.org/10.23970/ahrqepccer184
Roughead, L., Proctor, N., Westaway, K., Sluggett, J., & Alderman, C. (2017). Medication
safety in mental health. Sydney: ACSQHC.
https://www.safetyandquality.gov.au/sites/default/files/migrated/Medication-Safety-in-
Mental-Health-final-report-2017.pdf
Sheehan, R. (2018). Optimising psychotropic medication use. Tizard Learning Disability
Review, 23(1), 22-26. https://doi.org/10.1108/tldr-07-2017-0031
Sheehan, R., Hassiotis, A., Walters, K., Osborn, D., Strydom, A., & Horsfall, L. (2015).
Mental illness, challenging behaviour, and psychotropic drug prescribing in people
with intellectual disability: UK population based cohort study. BMJ, h4326.
https://doi.org/10.1136/bmj.h4326
Slemon, A., Jenkins, E., & Bungay, V. (2017). Safety in psychiatric inpatient care: The
impact of risk management culture on mental health nursing practice. Nursing Inquiry,
24(4), e12199. https://doi.org/10.1111/nin.12199
Valdovinos, M. G., Henninger-McMahon, M., Schieber, E., Beard, L., Conley, B., &
Haas, A. (2016). Assessing the impact of psychotropic medication changes on
challenging behavior of individuals with intellectual disabilities. International Journal
of Developmental Disabilities, 62(3), 200-211.
https://doi.org/10.1080/20473869.2016.1177301
SEDATIVE MEDICATIONS 12
Van der Plaat, A., Can Dooren, D. D., Van der Bijl, J., Oppewal, A., & Mergler, S. (2019).
Antipsychotic drug use in people with intellectual disability and comorbid autism.
Tijdschrift voor Artsen Verstandelijke Gehandicapten, 37(1), 23-28.
Van der Plaat, A., Can Dooren, D. D., Van der Bijl, J., Oppewal, A., & Mergler, S. (2019).
Antipsychotic drug use in people with intellectual disability and comorbid autism.
Tijdschrift voor Artsen Verstandelijke Gehandicapten, 37(1), 23-28.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 12
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





