CNA341 Improving Health: Impact of Sepsis Protocol on Early Detection
VerifiedAdded on 2023/06/04
|7
|2791
|202
Literature Review
AI Summary
This literature review explores the impact of implementing sepsis protocol policies, specifically the 'SEPSIS KILLS' program in NSW, Australia, on the early detection and treatment of sepsis patients. The review analyzes various studies and research findings to assess the effectiveness of such protocols in improving patient outcomes, reducing mortality rates, and enhancing the overall quality of care. It highlights the role of evidence-based practice in informing clinical decision-making and emphasizes the importance of early intervention through rapid IV fluids and antibiotic administration. The review also acknowledges the challenges and barriers to implementing evidence-based practice in nursing, such as lack of time and understanding of statistical terms, and suggests strategies for overcoming these obstacles. Ultimately, the review concludes that consistent and well-implemented sepsis protocols can significantly improve early detection, leading to more effective treatment and better health outcomes for sepsis patients.

Impact of Sepsis protocol policy in early detection of
sepsis patient and their treatment
Sepsis is one of the major reasons of increasing mortality rates in the hospitals globally. Statistics
reveal that one death occurs every four seconds in the world due to sepsis (Wylie-Cheer &
Goodson, 2016). One of the studies conducted between 2000 and 2012 reported that for a total of
101,064 diagnosis of sepsis was made over the year in Australia and New Zealand. Out of those,
24,255 died, which led to a mortality rate of 24% (Kaukonen, et al., 2014). Sepsis is a fatal
illness which arises when the body's response to infection damages its own tissues and organs. It
is recognized as a medical emergency worldwide (McPherson, et al., 2013). Annually, an
estimated 18,000 people suffer from sepsis, out of those around 5000 of those die and 50% of the
surviving people suffer from a disability or impaired functioning (The George Institute for
Global Health and the Australian Sepsis Network, 2017). In spite of these, massive statistics,
awareness regarding sepsis and the need for urgent intervention is lacking. The World Health
Assembly at the WHO recognised sepsis as a global health priority in May 2017 by officially
taking up a resolution to advance the prevention, detection and treatment of sepsis golabally. The
resolution invites every member states of the United Nations to take certain measures to lower
the load of sepsis, including executing national action plans, in partnership with professional and
patient-advocacy units.
In NSW, inefficiency of not being able to recognize and respond to sepsis has been registered
often. Suitable recognition techniques and on-time treatment of patients with sepsis is a major
issue in not only NSW hospitals but also in health care institutions across the globe. Delay in
management of sepsis has been linked with increased mortality rates, substantial morbidity and
augmented financial burden to the health care system (Burrell, et al., 2016). In 2009, the Clinical
Focus Report on Recognition and Management of Sepsis identified certain inadequacies in
several clinical settings in NSW health care settings (Clinical Excellence Commission Patient
Safety Team, 2012). CEC Quality Systems Assessment also found the failure of timely
recognition and suitable management.
NSW established a protocol for sepsis called “SEPSIS KILLS” which was executed as individual
emergency divisions in 2011. Its purpose is to decrease the avoidable harm to people by
improving detection and treatment of severe infection and sepsis in emergency divisions and
inpatient wards within the NSW. The SEPSIS KILLS pathways endorse bundles of care, with
their focus on early management.
This program is primarily based on:
Recognizing the risk factors, signs and symptoms of sepsis
Resuscitating with rapid IV fluids and antibiotics administration within the first hour of
diagnosis
Referring to senior practitioners and expert teams, comprising of the retrieval as needed.
sepsis patient and their treatment
Sepsis is one of the major reasons of increasing mortality rates in the hospitals globally. Statistics
reveal that one death occurs every four seconds in the world due to sepsis (Wylie-Cheer &
Goodson, 2016). One of the studies conducted between 2000 and 2012 reported that for a total of
101,064 diagnosis of sepsis was made over the year in Australia and New Zealand. Out of those,
24,255 died, which led to a mortality rate of 24% (Kaukonen, et al., 2014). Sepsis is a fatal
illness which arises when the body's response to infection damages its own tissues and organs. It
is recognized as a medical emergency worldwide (McPherson, et al., 2013). Annually, an
estimated 18,000 people suffer from sepsis, out of those around 5000 of those die and 50% of the
surviving people suffer from a disability or impaired functioning (The George Institute for
Global Health and the Australian Sepsis Network, 2017). In spite of these, massive statistics,
awareness regarding sepsis and the need for urgent intervention is lacking. The World Health
Assembly at the WHO recognised sepsis as a global health priority in May 2017 by officially
taking up a resolution to advance the prevention, detection and treatment of sepsis golabally. The
resolution invites every member states of the United Nations to take certain measures to lower
the load of sepsis, including executing national action plans, in partnership with professional and
patient-advocacy units.
In NSW, inefficiency of not being able to recognize and respond to sepsis has been registered
often. Suitable recognition techniques and on-time treatment of patients with sepsis is a major
issue in not only NSW hospitals but also in health care institutions across the globe. Delay in
management of sepsis has been linked with increased mortality rates, substantial morbidity and
augmented financial burden to the health care system (Burrell, et al., 2016). In 2009, the Clinical
Focus Report on Recognition and Management of Sepsis identified certain inadequacies in
several clinical settings in NSW health care settings (Clinical Excellence Commission Patient
Safety Team, 2012). CEC Quality Systems Assessment also found the failure of timely
recognition and suitable management.
NSW established a protocol for sepsis called “SEPSIS KILLS” which was executed as individual
emergency divisions in 2011. Its purpose is to decrease the avoidable harm to people by
improving detection and treatment of severe infection and sepsis in emergency divisions and
inpatient wards within the NSW. The SEPSIS KILLS pathways endorse bundles of care, with
their focus on early management.
This program is primarily based on:
Recognizing the risk factors, signs and symptoms of sepsis
Resuscitating with rapid IV fluids and antibiotics administration within the first hour of
diagnosis
Referring to senior practitioners and expert teams, comprising of the retrieval as needed.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
The SEPSIS KILLS protocol is a quality-upgrading plan that has been formed from universal
evidence-based practice. It provides various advantages to NSW hospitals at clinical as well as
system levels such as:
Increased practitioners skills in sepsis detection and treatment
More timely, regulated and efficient recognition and treatment of sepsis
Decreased death, morbidity and bed-stays rates associated with sepsis
Improved process and quality of care for patients with sepsis in NSW hospitals
for safer patient experience.
Role of evidence-based practice in informing effective
clinical decision making in Sepsis management
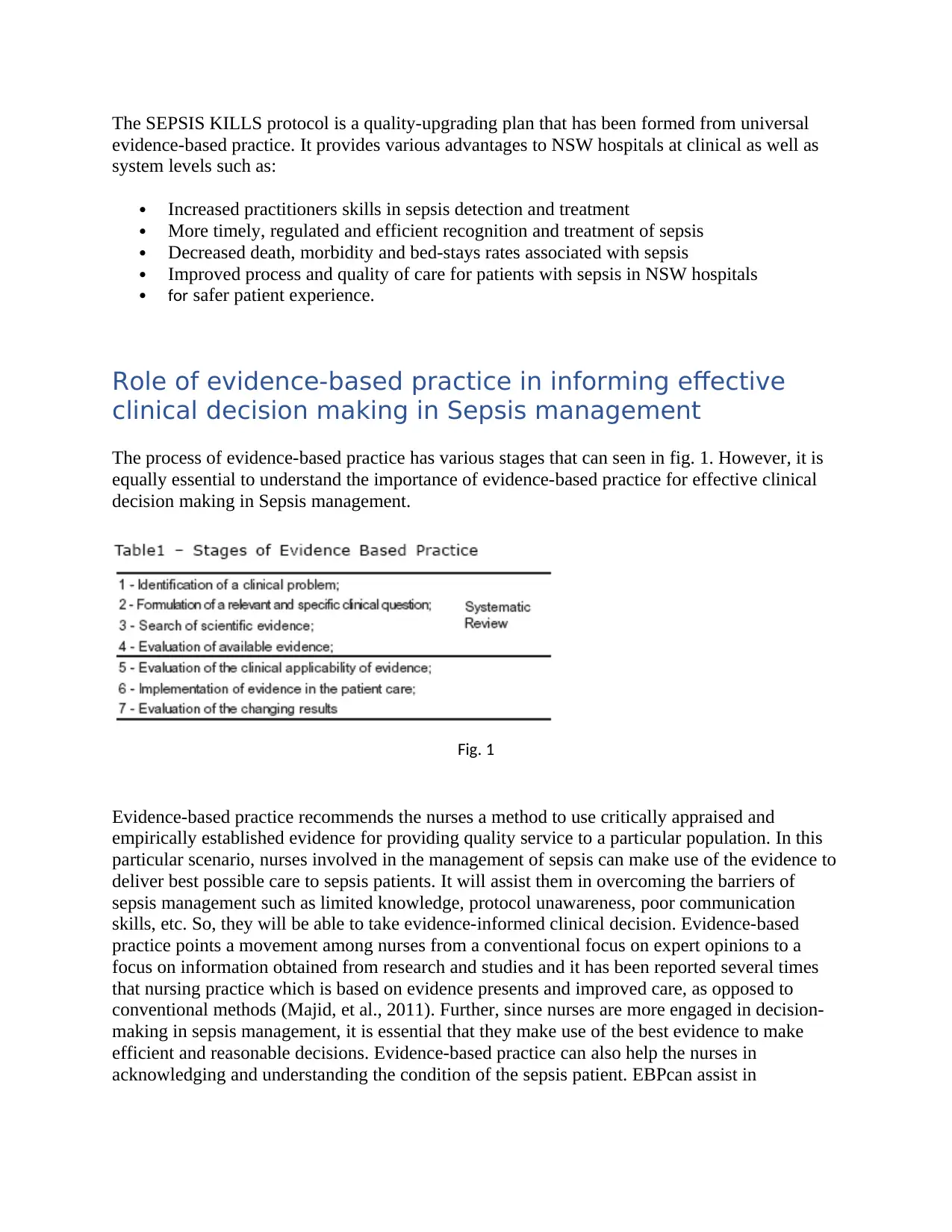
The process of evidence-based practice has various stages that can seen in fig. 1. However, it is
equally essential to understand the importance of evidence-based practice for effective clinical
decision making in Sepsis management.
Fig. 1
Evidence-based practice recommends the nurses a method to use critically appraised and
empirically established evidence for providing quality service to a particular population. In this
particular scenario, nurses involved in the management of sepsis can make use of the evidence to
deliver best possible care to sepsis patients. It will assist them in overcoming the barriers of
sepsis management such as limited knowledge, protocol unawareness, poor communication
skills, etc. So, they will be able to take evidence-informed clinical decision. Evidence-based
practice points a movement among nurses from a conventional focus on expert opinions to a
focus on information obtained from research and studies and it has been reported several times
that nursing practice which is based on evidence presents and improved care, as opposed to
conventional methods (Majid, et al., 2011). Further, since nurses are more engaged in decision-
making in sepsis management, it is essential that they make use of the best evidence to make
efficient and reasonable decisions. Evidence-based practice can also help the nurses in
acknowledging and understanding the condition of the sepsis patient. EBPcan assist in
evidence-based practice. It provides various advantages to NSW hospitals at clinical as well as
system levels such as:
Increased practitioners skills in sepsis detection and treatment
More timely, regulated and efficient recognition and treatment of sepsis
Decreased death, morbidity and bed-stays rates associated with sepsis
Improved process and quality of care for patients with sepsis in NSW hospitals
for safer patient experience.
Role of evidence-based practice in informing effective
clinical decision making in Sepsis management
The process of evidence-based practice has various stages that can seen in fig. 1. However, it is
equally essential to understand the importance of evidence-based practice for effective clinical
decision making in Sepsis management.
Fig. 1
Evidence-based practice recommends the nurses a method to use critically appraised and
empirically established evidence for providing quality service to a particular population. In this
particular scenario, nurses involved in the management of sepsis can make use of the evidence to
deliver best possible care to sepsis patients. It will assist them in overcoming the barriers of
sepsis management such as limited knowledge, protocol unawareness, poor communication
skills, etc. So, they will be able to take evidence-informed clinical decision. Evidence-based
practice points a movement among nurses from a conventional focus on expert opinions to a
focus on information obtained from research and studies and it has been reported several times
that nursing practice which is based on evidence presents and improved care, as opposed to
conventional methods (Majid, et al., 2011). Further, since nurses are more engaged in decision-
making in sepsis management, it is essential that they make use of the best evidence to make
efficient and reasonable decisions. Evidence-based practice can also help the nurses in
acknowledging and understanding the condition of the sepsis patient. EBPcan assist in
identifying the gaps in the knowledge about sepsis recognition and management and construct
questions to bridge those gaps.
However, there are certain barriers to EBP for nursing practice, mainly lack of time due to heavy
workload and inadequacy to understand statistical terms and jargons that are used in literature.
The situation can be improved by an EBP orientation, time availability, and tutoring by nurses
with EBP experience.
Development of a searchable clinical question using a
recognized clinical question formula
PICO format has been used to develop a searchable clinical research question (Aslam &
Emmanuel, 2010).
Population: Sepsis patients
Intervention: Sepsis protocol policy- “SEPSIS KILLS”
Control: Non-evidence based practice
Outcome- Early detection and management
Therefore, the research question is “Impact of Sepsis protocol policy in early detection of sepsis
patient and their treatment”.
Evidence of a systematic literature search strategy
As a well-formed search strategy is the core of the research activity, an organized search strategy
has been utilized for searching the literature to find answer to the research questions.
Keywords
1. Early detection- On searching various databases, 381696 articles were found out with this
keyword. 50359 met the inclusion criteria. Were found relevant to the research question.
2. Sepsis protocol policy – 54 articles were identified for this keyword. 12 of them met the
inclusion criteria. Were found to be relevant to the study.
3. Sepsis kills- 112 articles were found for this key word. 16 of them met the inclusion
criteria. Were found relevant to the study.
4. Sepsis patient and their treatment- 59082 articles were identified for this keyword. 5978
met the inclusion criteria. Were relevant to be included in the research.
5. Evidence based practice and sepsis- 998 articles were identified for this keyword. 97 of
them met the inclusion criteria and were found relevant for the research inclusion.
6. Early detection of sepsis patient and their treatment- 4232 articles were found for this
keyword on searching various databases. 580 of them met the inclusion criteria and were
found relevant to be included in the research.
Inclusion criteria
1. English language
questions to bridge those gaps.
However, there are certain barriers to EBP for nursing practice, mainly lack of time due to heavy
workload and inadequacy to understand statistical terms and jargons that are used in literature.
The situation can be improved by an EBP orientation, time availability, and tutoring by nurses
with EBP experience.
Development of a searchable clinical question using a
recognized clinical question formula
PICO format has been used to develop a searchable clinical research question (Aslam &
Emmanuel, 2010).
Population: Sepsis patients
Intervention: Sepsis protocol policy- “SEPSIS KILLS”
Control: Non-evidence based practice
Outcome- Early detection and management
Therefore, the research question is “Impact of Sepsis protocol policy in early detection of sepsis
patient and their treatment”.
Evidence of a systematic literature search strategy
As a well-formed search strategy is the core of the research activity, an organized search strategy
has been utilized for searching the literature to find answer to the research questions.
Keywords
1. Early detection- On searching various databases, 381696 articles were found out with this
keyword. 50359 met the inclusion criteria. Were found relevant to the research question.
2. Sepsis protocol policy – 54 articles were identified for this keyword. 12 of them met the
inclusion criteria. Were found to be relevant to the study.
3. Sepsis kills- 112 articles were found for this key word. 16 of them met the inclusion
criteria. Were found relevant to the study.
4. Sepsis patient and their treatment- 59082 articles were identified for this keyword. 5978
met the inclusion criteria. Were relevant to be included in the research.
5. Evidence based practice and sepsis- 998 articles were identified for this keyword. 97 of
them met the inclusion criteria and were found relevant for the research inclusion.
6. Early detection of sepsis patient and their treatment- 4232 articles were found for this
keyword on searching various databases. 580 of them met the inclusion criteria and were
found relevant to be included in the research.
Inclusion criteria
1. English language
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
2. Published within 5 years
3. Full-text available
Exclusion criteria
1. Unsuitable target population
2. Irrelevant information
3. Outdated
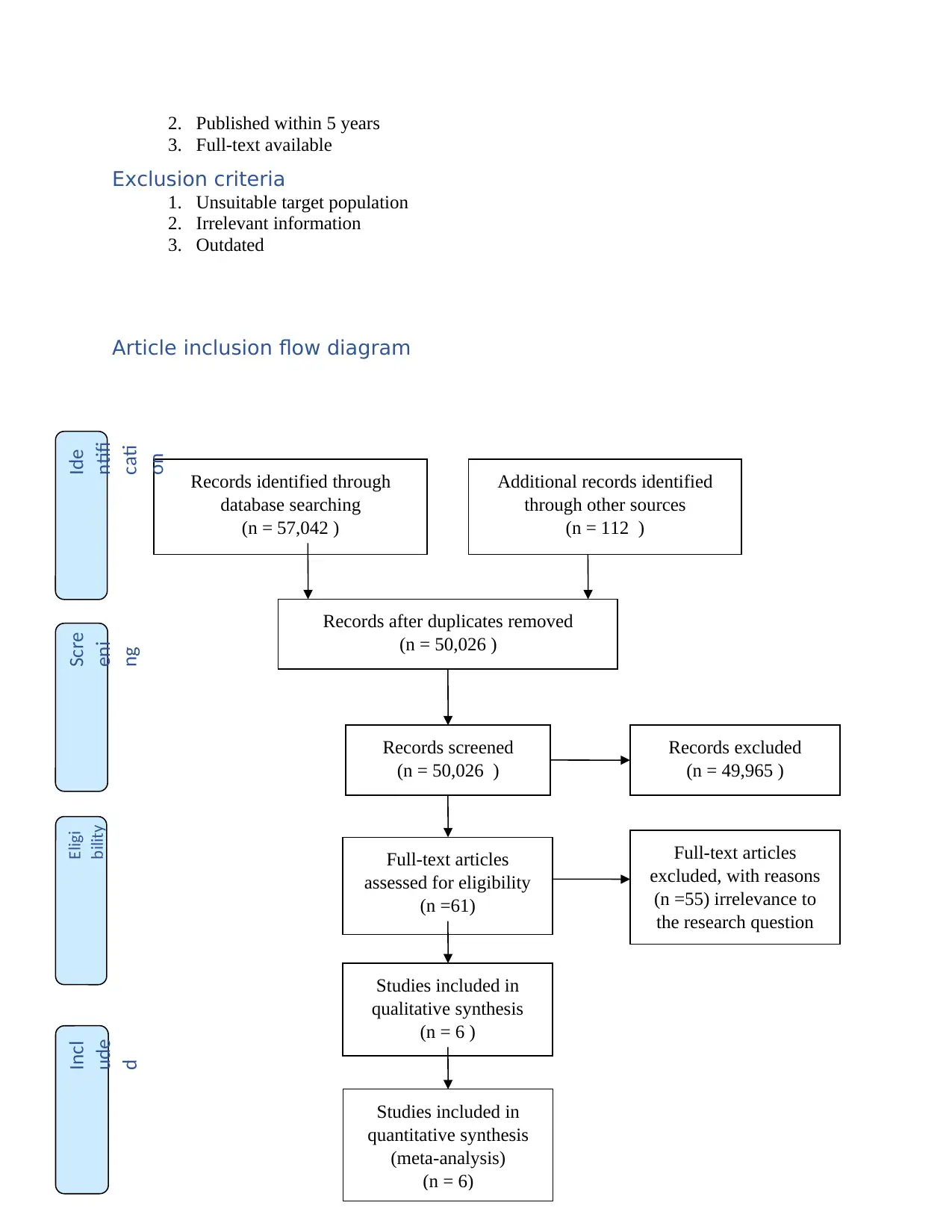
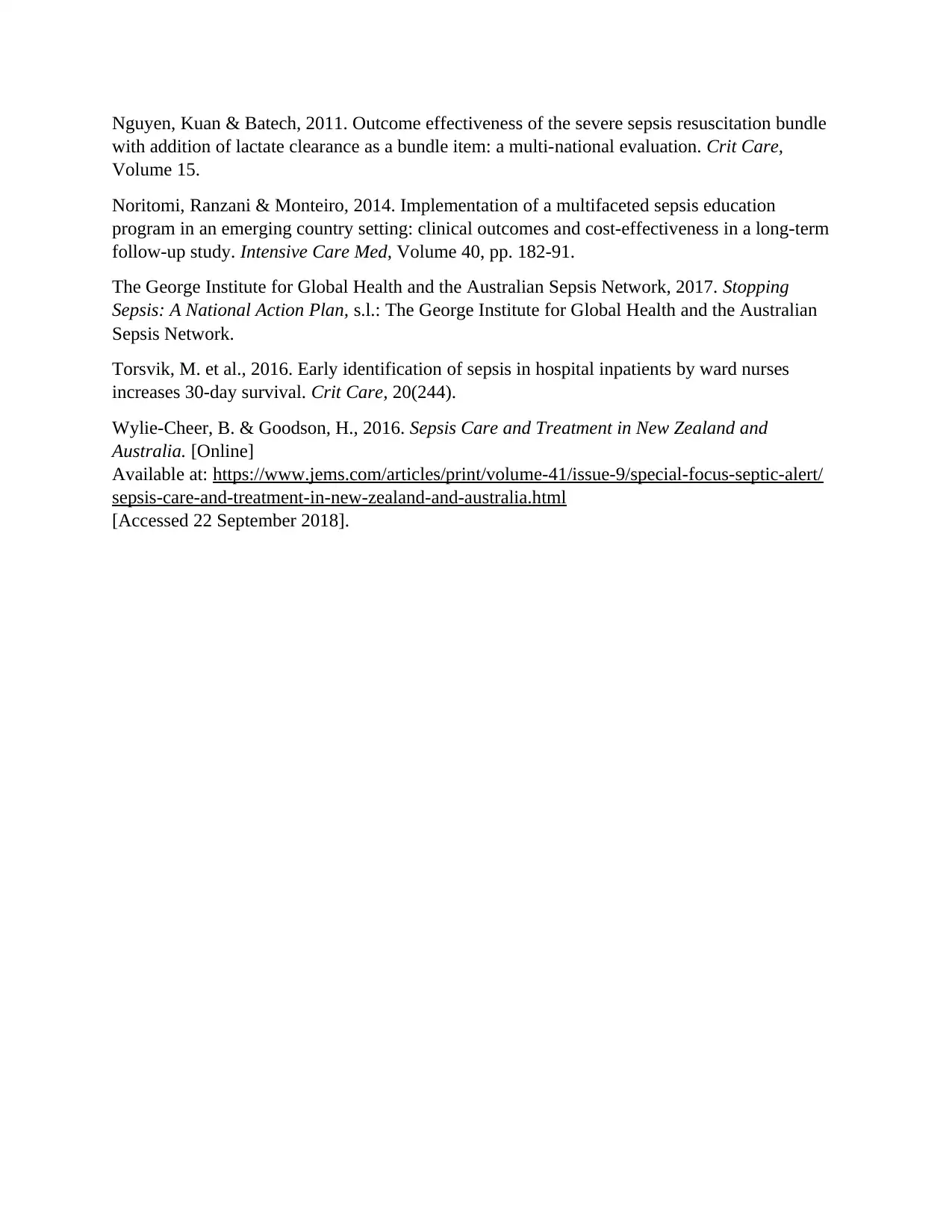
Article inclusion flow diagram
Records identified through
database searching
(n = 57,042 )
Scre
eni
ng
Incl
ude
d
Eligi
bility
Ide
ntifi
cati
on
Additional records identified
through other sources
(n = 112 )
Records after duplicates removed
(n = 50,026 )
Records screened
(n = 50,026 )
Records excluded
(n = 49,965 )
Full-text articles
assessed for eligibility
(n =61)
Full-text articles
excluded, with reasons
(n =55) irrelevance to
the research question
Studies included in
qualitative synthesis
(n = 6 )
Studies included in
quantitative synthesis
(meta-analysis)
(n = 6)
3. Full-text available
Exclusion criteria
1. Unsuitable target population
2. Irrelevant information
3. Outdated
Article inclusion flow diagram
Records identified through
database searching
(n = 57,042 )
Scre
eni
ng
Incl
ude
d
Eligi
bility
Ide
ntifi
cati
on
Additional records identified
through other sources
(n = 112 )
Records after duplicates removed
(n = 50,026 )
Records screened
(n = 50,026 )
Records excluded
(n = 49,965 )
Full-text articles
assessed for eligibility
(n =61)
Full-text articles
excluded, with reasons
(n =55) irrelevance to
the research question
Studies included in
qualitative synthesis
(n = 6 )
Studies included in
quantitative synthesis
(meta-analysis)
(n = 6)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
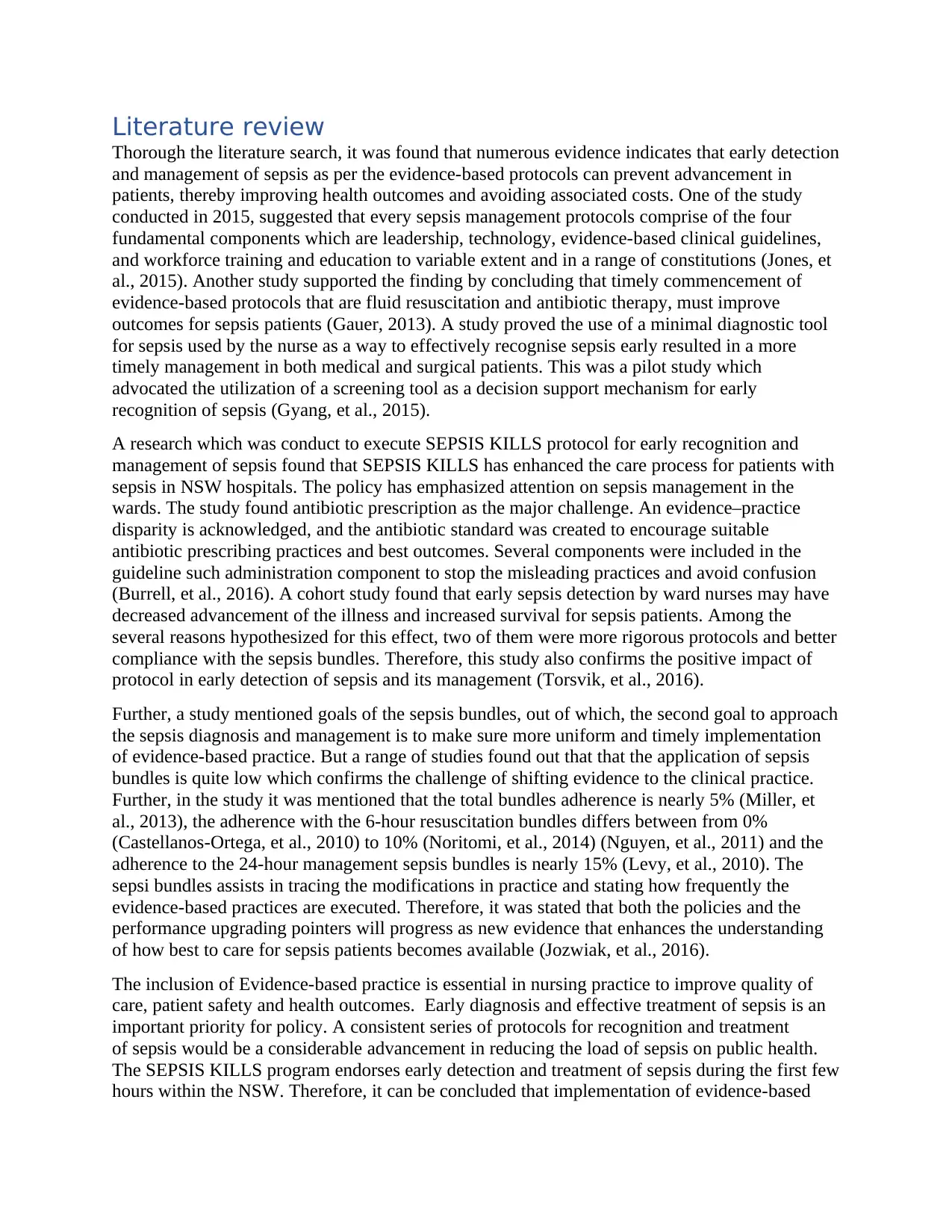
Literature review
Thorough the literature search, it was found that numerous evidence indicates that early detection
and management of sepsis as per the evidence-based protocols can prevent advancement in
patients, thereby improving health outcomes and avoiding associated costs. One of the study
conducted in 2015, suggested that every sepsis management protocols comprise of the four
fundamental components which are leadership, technology, evidence-based clinical guidelines,
and workforce training and education to variable extent and in a range of constitutions (Jones, et
al., 2015). Another study supported the finding by concluding that timely commencement of
evidence-based protocols that are fluid resuscitation and antibiotic therapy, must improve
outcomes for sepsis patients (Gauer, 2013). A study proved the use of a minimal diagnostic tool
for sepsis used by the nurse as a way to effectively recognise sepsis early resulted in a more
timely management in both medical and surgical patients. This was a pilot study which
advocated the utilization of a screening tool as a decision support mechanism for early
recognition of sepsis (Gyang, et al., 2015).
A research which was conduct to execute SEPSIS KILLS protocol for early recognition and
management of sepsis found that SEPSIS KILLS has enhanced the care process for patients with
sepsis in NSW hospitals. The policy has emphasized attention on sepsis management in the
wards. The study found antibiotic prescription as the major challenge. An evidence–practice
disparity is acknowledged, and the antibiotic standard was created to encourage suitable
antibiotic prescribing practices and best outcomes. Several components were included in the
guideline such administration component to stop the misleading practices and avoid confusion
(Burrell, et al., 2016). A cohort study found that early sepsis detection by ward nurses may have
decreased advancement of the illness and increased survival for sepsis patients. Among the
several reasons hypothesized for this effect, two of them were more rigorous protocols and better
compliance with the sepsis bundles. Therefore, this study also confirms the positive impact of
protocol in early detection of sepsis and its management (Torsvik, et al., 2016).
Further, a study mentioned goals of the sepsis bundles, out of which, the second goal to approach
the sepsis diagnosis and management is to make sure more uniform and timely implementation
of evidence-based practice. But a range of studies found out that that the application of sepsis
bundles is quite low which confirms the challenge of shifting evidence to the clinical practice.
Further, in the study it was mentioned that the total bundles adherence is nearly 5% (Miller, et
al., 2013), the adherence with the 6-hour resuscitation bundles differs between from 0%
(Castellanos-Ortega, et al., 2010) to 10% (Noritomi, et al., 2014) (Nguyen, et al., 2011) and the
adherence to the 24-hour management sepsis bundles is nearly 15% (Levy, et al., 2010). The
sepsi bundles assists in tracing the modifications in practice and stating how frequently the
evidence-based practices are executed. Therefore, it was stated that both the policies and the
performance upgrading pointers will progress as new evidence that enhances the understanding
of how best to care for sepsis patients becomes available (Jozwiak, et al., 2016).
The inclusion of Evidence-based practice is essential in nursing practice to improve quality of
care, patient safety and health outcomes. Early diagnosis and effective treatment of sepsis is an
important priority for policy. A consistent series of protocols for recognition and treatment
of sepsis would be a considerable advancement in reducing the load of sepsis on public health.
The SEPSIS KILLS program endorses early detection and treatment of sepsis during the first few
hours within the NSW. Therefore, it can be concluded that implementation of evidence-based
Thorough the literature search, it was found that numerous evidence indicates that early detection
and management of sepsis as per the evidence-based protocols can prevent advancement in
patients, thereby improving health outcomes and avoiding associated costs. One of the study
conducted in 2015, suggested that every sepsis management protocols comprise of the four
fundamental components which are leadership, technology, evidence-based clinical guidelines,
and workforce training and education to variable extent and in a range of constitutions (Jones, et
al., 2015). Another study supported the finding by concluding that timely commencement of
evidence-based protocols that are fluid resuscitation and antibiotic therapy, must improve
outcomes for sepsis patients (Gauer, 2013). A study proved the use of a minimal diagnostic tool
for sepsis used by the nurse as a way to effectively recognise sepsis early resulted in a more
timely management in both medical and surgical patients. This was a pilot study which
advocated the utilization of a screening tool as a decision support mechanism for early
recognition of sepsis (Gyang, et al., 2015).
A research which was conduct to execute SEPSIS KILLS protocol for early recognition and
management of sepsis found that SEPSIS KILLS has enhanced the care process for patients with
sepsis in NSW hospitals. The policy has emphasized attention on sepsis management in the
wards. The study found antibiotic prescription as the major challenge. An evidence–practice
disparity is acknowledged, and the antibiotic standard was created to encourage suitable
antibiotic prescribing practices and best outcomes. Several components were included in the
guideline such administration component to stop the misleading practices and avoid confusion
(Burrell, et al., 2016). A cohort study found that early sepsis detection by ward nurses may have
decreased advancement of the illness and increased survival for sepsis patients. Among the
several reasons hypothesized for this effect, two of them were more rigorous protocols and better
compliance with the sepsis bundles. Therefore, this study also confirms the positive impact of
protocol in early detection of sepsis and its management (Torsvik, et al., 2016).
Further, a study mentioned goals of the sepsis bundles, out of which, the second goal to approach
the sepsis diagnosis and management is to make sure more uniform and timely implementation
of evidence-based practice. But a range of studies found out that that the application of sepsis
bundles is quite low which confirms the challenge of shifting evidence to the clinical practice.
Further, in the study it was mentioned that the total bundles adherence is nearly 5% (Miller, et
al., 2013), the adherence with the 6-hour resuscitation bundles differs between from 0%
(Castellanos-Ortega, et al., 2010) to 10% (Noritomi, et al., 2014) (Nguyen, et al., 2011) and the
adherence to the 24-hour management sepsis bundles is nearly 15% (Levy, et al., 2010). The
sepsi bundles assists in tracing the modifications in practice and stating how frequently the
evidence-based practices are executed. Therefore, it was stated that both the policies and the
performance upgrading pointers will progress as new evidence that enhances the understanding
of how best to care for sepsis patients becomes available (Jozwiak, et al., 2016).
The inclusion of Evidence-based practice is essential in nursing practice to improve quality of
care, patient safety and health outcomes. Early diagnosis and effective treatment of sepsis is an
important priority for policy. A consistent series of protocols for recognition and treatment
of sepsis would be a considerable advancement in reducing the load of sepsis on public health.
The SEPSIS KILLS program endorses early detection and treatment of sepsis during the first few
hours within the NSW. Therefore, it can be concluded that implementation of evidence-based
practice by using protocols such as SEPSIS KILLS can assist in early recognition of sepsis in
patients which would eventually help in their suitable treatment. However, the barriers to
implementation of EBP in nursing practice should be identified and efforts should be made to
remove them.
References
Aslam, S. & Emmanuel, P., 2010. Formulating a researchable question: A critical step for
facilitating good clinical research. Indian J Sex Transm Dis AIDS, 31(1), pp. 47-50.
Burrell, A. R. et al., 2016. SEPSIS KILLS: early intervention saves lives. MJA, 204(2).
Castellanos-Ortega, Suberviola & García-Astudillo, 2010. Impact of the Surviving Sepsis
Campaign protocols on hospital length of stay and mortality in septic shock patients: results of a
three-year follow-up quasi-experimental study. Crit Care Med, Volume 38, pp. 1036-43.
Clinical Excellence Commission Patient Safety Team, 2012. Recognition and Management of
Sepsis, s.l.: Clinical Excellence Commission.
Gauer, 2013. Early recognition and management of sepsis in adults: the first six hours. Am Fam
Physician, 88(1), pp. 44-53.
Gyang, E., Shieh, L., Forsey, L. & Maggio, P., 2015. A Nurse-Driven Screening Tool for the
Early Identification of Sepsis in an Intermediate Care Unit Setting. J Hosp Med, 10(2), pp. 97-
103.
Jones, S. L., Ashton, C. M., Kiehne, L. & Gigliotti, E., 2015. Reductions in Sepsis Mortality and
Costs After Design and Implementation of a Nurse-Based Early Recognition and Response
Program. Jt Comm J Qual Patient Saf, 41(11), p. 483–491.
Jozwiak, M., Monnet, X. & Teboul, J.-L., 2016. Implementing sepsis bundles. Ann Transl Med,
4(17).
Kaukonen, Bailey & Suzuki, 2014. Mortality related to severe sepsis and septic shock among
critically ill patients in Australia and New Zealand, 2000-2012. JAMA, 311(13), p. 1308–1316.
Levy, Dellinger & Townsend, 2010. The Surviving Sepsis Campaign: results of an international
guideline-based performance improvement program targeting severe sepsis. Intensive Care
Med , Volume 36, pp. 222-31.
Majid, S., Foo, S., Luyt, B. & Zhang, X., 2011. Adopting evidence-based practice in clinical
decision making: nurses' perceptions, knowledge, and barriers. J Med Libr Assoc, 99(3).
McPherson, Griffiths & Williams, 2013. Sepsis-associated mortality in England: an analysis of
multiple cause of death data from 2001 to 2010. BMJ Open, 3(8).
Miller, Dong & Nelson, 2013. Multicenter implementation of a severe sepsis and septic shock
treatment bundle. Am J Respir Crit Care Med, Volume 188, pp. 77-82.
patients which would eventually help in their suitable treatment. However, the barriers to
implementation of EBP in nursing practice should be identified and efforts should be made to
remove them.
References
Aslam, S. & Emmanuel, P., 2010. Formulating a researchable question: A critical step for
facilitating good clinical research. Indian J Sex Transm Dis AIDS, 31(1), pp. 47-50.
Burrell, A. R. et al., 2016. SEPSIS KILLS: early intervention saves lives. MJA, 204(2).
Castellanos-Ortega, Suberviola & García-Astudillo, 2010. Impact of the Surviving Sepsis
Campaign protocols on hospital length of stay and mortality in septic shock patients: results of a
three-year follow-up quasi-experimental study. Crit Care Med, Volume 38, pp. 1036-43.
Clinical Excellence Commission Patient Safety Team, 2012. Recognition and Management of
Sepsis, s.l.: Clinical Excellence Commission.
Gauer, 2013. Early recognition and management of sepsis in adults: the first six hours. Am Fam
Physician, 88(1), pp. 44-53.
Gyang, E., Shieh, L., Forsey, L. & Maggio, P., 2015. A Nurse-Driven Screening Tool for the
Early Identification of Sepsis in an Intermediate Care Unit Setting. J Hosp Med, 10(2), pp. 97-
103.
Jones, S. L., Ashton, C. M., Kiehne, L. & Gigliotti, E., 2015. Reductions in Sepsis Mortality and
Costs After Design and Implementation of a Nurse-Based Early Recognition and Response
Program. Jt Comm J Qual Patient Saf, 41(11), p. 483–491.
Jozwiak, M., Monnet, X. & Teboul, J.-L., 2016. Implementing sepsis bundles. Ann Transl Med,
4(17).
Kaukonen, Bailey & Suzuki, 2014. Mortality related to severe sepsis and septic shock among
critically ill patients in Australia and New Zealand, 2000-2012. JAMA, 311(13), p. 1308–1316.
Levy, Dellinger & Townsend, 2010. The Surviving Sepsis Campaign: results of an international
guideline-based performance improvement program targeting severe sepsis. Intensive Care
Med , Volume 36, pp. 222-31.
Majid, S., Foo, S., Luyt, B. & Zhang, X., 2011. Adopting evidence-based practice in clinical
decision making: nurses' perceptions, knowledge, and barriers. J Med Libr Assoc, 99(3).
McPherson, Griffiths & Williams, 2013. Sepsis-associated mortality in England: an analysis of
multiple cause of death data from 2001 to 2010. BMJ Open, 3(8).
Miller, Dong & Nelson, 2013. Multicenter implementation of a severe sepsis and septic shock
treatment bundle. Am J Respir Crit Care Med, Volume 188, pp. 77-82.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Nguyen, Kuan & Batech, 2011. Outcome effectiveness of the severe sepsis resuscitation bundle
with addition of lactate clearance as a bundle item: a multi-national evaluation. Crit Care,
Volume 15.
Noritomi, Ranzani & Monteiro, 2014. Implementation of a multifaceted sepsis education
program in an emerging country setting: clinical outcomes and cost-effectiveness in a long-term
follow-up study. Intensive Care Med, Volume 40, pp. 182-91.
The George Institute for Global Health and the Australian Sepsis Network, 2017. Stopping
Sepsis: A National Action Plan, s.l.: The George Institute for Global Health and the Australian
Sepsis Network.
Torsvik, M. et al., 2016. Early identification of sepsis in hospital inpatients by ward nurses
increases 30-day survival. Crit Care, 20(244).
Wylie-Cheer, B. & Goodson, H., 2016. Sepsis Care and Treatment in New Zealand and
Australia. [Online]
Available at: https://www.jems.com/articles/print/volume-41/issue-9/special-focus-septic-alert/
sepsis-care-and-treatment-in-new-zealand-and-australia.html
[Accessed 22 September 2018].
with addition of lactate clearance as a bundle item: a multi-national evaluation. Crit Care,
Volume 15.
Noritomi, Ranzani & Monteiro, 2014. Implementation of a multifaceted sepsis education
program in an emerging country setting: clinical outcomes and cost-effectiveness in a long-term
follow-up study. Intensive Care Med, Volume 40, pp. 182-91.
The George Institute for Global Health and the Australian Sepsis Network, 2017. Stopping
Sepsis: A National Action Plan, s.l.: The George Institute for Global Health and the Australian
Sepsis Network.
Torsvik, M. et al., 2016. Early identification of sepsis in hospital inpatients by ward nurses
increases 30-day survival. Crit Care, 20(244).
Wylie-Cheer, B. & Goodson, H., 2016. Sepsis Care and Treatment in New Zealand and
Australia. [Online]
Available at: https://www.jems.com/articles/print/volume-41/issue-9/special-focus-septic-alert/
sepsis-care-and-treatment-in-new-zealand-and-australia.html
[Accessed 22 September 2018].
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





