Nursing Practice: Clinical Decision-Making Simulation Report
VerifiedAdded on 2023/04/08
|9
|1430
|149
Report
AI Summary
This report analyzes a clinical simulation scenario involving a 19-year-old male, Mr. Patience, who sustained injuries in a motor vehicle crash. The student utilizes the ADPIE (Assessment, Diagnosis, Planning, Implementation, and Evaluation) nursing process model to assess the patient's condition, diagnose potential issues such as spinal cord injury, neurogenic shock, and hypoxemia, plan appropriate interventions including medication, fluid resuscitation, and oxygen supplementation, implement the care plan, and evaluate the outcomes. The report emphasizes the importance of critical thinking, the role of the healthcare team, and the effectiveness of the ADPIE model in clinical decision-making. Key issues addressed include intense back pain, immobility, shortness of breath, and low blood pressure, with the student providing rationales for each intervention and referencing relevant literature. The paper concludes by highlighting the benefits of the ADPIE model in promoting thorough patient evaluation and improved healthcare provision.

Running head: SIMULATION SCENARIO
Simulation scenario
Name of the student:
Name of the University:
Author’s note
Simulation scenario
Name of the student:
Name of the University:
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1SIMULATION SCENARIO
Introduction:
Decision making in nursing practice is a complex phenomenon that determines the use of
subjective and objective data of patient to identify relevant health problems and use critical
thinking to develop the best plan of care. There are several clinical judgment or decision making
models that help nurses during clinical decision making process. The main purpose of this paper
is to use a clinical decision making model to clinical scenario of Mr. Patience, a 19 year old male
involved in motor vehicle crash (MVC). The paper will analyse how use of different decision
making models helped to interpret patient’s situation and plan appropriate intervention for
patient. It also discusses the responsibility of multi-professional health care team in providing
care to patient.
Primary assessment:
The clinical scenario is about Mr. Patience, who sustained MVC after losing control of
his car and being hit by a tree. He has arrived with a cervical collar and long backboard. His
current symptoms include dizziness, shortness of breath and increased lower back pain. To
systematically identify primary issues for Mr. Patience and critically think aboyt best nursing
response, the ADPIE (assessment, diagnosis, planning, implementation and evaluation) nursing
process model has been used. The main rationale behind the use of ADPIE model is that it
provides a useful framework for critical thinking and problem solving while engaging in care of
a patient.
The first step involved gathering data of patient. The ABCDEFGHI assessment of Mr.
Patience gave the following outcome:
A: No airway obstruction found
Introduction:
Decision making in nursing practice is a complex phenomenon that determines the use of
subjective and objective data of patient to identify relevant health problems and use critical
thinking to develop the best plan of care. There are several clinical judgment or decision making
models that help nurses during clinical decision making process. The main purpose of this paper
is to use a clinical decision making model to clinical scenario of Mr. Patience, a 19 year old male
involved in motor vehicle crash (MVC). The paper will analyse how use of different decision
making models helped to interpret patient’s situation and plan appropriate intervention for
patient. It also discusses the responsibility of multi-professional health care team in providing
care to patient.
Primary assessment:
The clinical scenario is about Mr. Patience, who sustained MVC after losing control of
his car and being hit by a tree. He has arrived with a cervical collar and long backboard. His
current symptoms include dizziness, shortness of breath and increased lower back pain. To
systematically identify primary issues for Mr. Patience and critically think aboyt best nursing
response, the ADPIE (assessment, diagnosis, planning, implementation and evaluation) nursing
process model has been used. The main rationale behind the use of ADPIE model is that it
provides a useful framework for critical thinking and problem solving while engaging in care of
a patient.
The first step involved gathering data of patient. The ABCDEFGHI assessment of Mr.
Patience gave the following outcome:
A: No airway obstruction found
2SIMULATION SCENARIO
B: HR 128, RR 26. Heart rate is found to be high and breathing rate is also slightly above the
normal limit. Shortness of breath is an issue for patient
C: BP is 90/52 indicating that the patient has low blood pressure. HGB value is 80 which
indicates is hyperglycemic
D: The patient is less responsive and immobilized
E: He has a cervical collar and long backboard. A large bore 18-gauge is inserted in his right
forearm. No other cut or bruises found.
F: Review of his vital signs suggest high heart rate, low blood pressure and low body
temperature
G: He has intense back pain indicated by score of 10/10
H: The review of patient history suggests that he has a history of Type 1 Diabetes.
The advantage of assessment is that it gives an overview of abnormalities in the patient
data. This helped to identify potential problem for patient.
Diagnosis: The following can be interpreted based on patient’s data and assessment records:
Interpretation#1: The first priority concern for patient is intense back pain and immobility due to
C-spine fracture.
Rationale: This has been identified as the primary concern because Mr. Patience’s back pain
score is 10/10 and he has come immobilized with a cervical collar and long backboard. This is
indicative of the fact that he has sustained C-spine fracture. This type of fracture results in loss of
all motor and sensory function below the level of injury. Zonfrillo et al. (2014) suggest that
B: HR 128, RR 26. Heart rate is found to be high and breathing rate is also slightly above the
normal limit. Shortness of breath is an issue for patient
C: BP is 90/52 indicating that the patient has low blood pressure. HGB value is 80 which
indicates is hyperglycemic
D: The patient is less responsive and immobilized
E: He has a cervical collar and long backboard. A large bore 18-gauge is inserted in his right
forearm. No other cut or bruises found.
F: Review of his vital signs suggest high heart rate, low blood pressure and low body
temperature
G: He has intense back pain indicated by score of 10/10
H: The review of patient history suggests that he has a history of Type 1 Diabetes.
The advantage of assessment is that it gives an overview of abnormalities in the patient
data. This helped to identify potential problem for patient.
Diagnosis: The following can be interpreted based on patient’s data and assessment records:
Interpretation#1: The first priority concern for patient is intense back pain and immobility due to
C-spine fracture.
Rationale: This has been identified as the primary concern because Mr. Patience’s back pain
score is 10/10 and he has come immobilized with a cervical collar and long backboard. This is
indicative of the fact that he has sustained C-spine fracture. This type of fracture results in loss of
all motor and sensory function below the level of injury. Zonfrillo et al. (2014) suggest that
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3SIMULATION SCENARIO
motor vehicle crash is the common mechanism of spinal injury and the same cause was
identified for Mr. Patience too.
Interpretation#2: The patient is at risk of neurogenic shock evidenced by hypotension and low
body temperature.
Rationale: Mr. Patience blood pressure was found to be very low and skin assessment revealed
that his body was cool to touch. He is also very slow to response. Neurogenic shock or reduced
blood pressure is common in patient after spinal cord injury because of trauma to the spinal cord
and stimulation of the sympathetic nervous system (Partida et al., 2018).
Interpretation#3: Mr. Patience is at risk of hypoxemia because of c-spine fracture and bleeding
Rationale: Risk of hypoxemia has been interpreted because of shortness of breath, oxygen 93%
and temperature of 35.9. This indicates that the patient might require supplemental oxygen.
Planning: In response to the anticipated problem for patient, the anticipated plan of care or
nursing response are as follows:
Response#1: To reduce the problem of intense pain and immobility, it is planned to provide
medications like muscle relaxant and employ relaxation technique to alleviate pain and anxiety
for patient.
Rationale: Muscle relaxant like Dantrolene and analgesics are effective in relieving muscle
spasm and pain due to spasticity. Furthermore, comfort measures like cold packs and deep
breathing exercise works to promote sense of control and coping abilities in Mr. Patience. Jeon et
al. (2014) gives evidence regarding the efficacy of Dantrolene in treating spasticity after spinal
cord injury. Busch et al. (2012) gives the evidence that deep breathing technique is often
motor vehicle crash is the common mechanism of spinal injury and the same cause was
identified for Mr. Patience too.
Interpretation#2: The patient is at risk of neurogenic shock evidenced by hypotension and low
body temperature.
Rationale: Mr. Patience blood pressure was found to be very low and skin assessment revealed
that his body was cool to touch. He is also very slow to response. Neurogenic shock or reduced
blood pressure is common in patient after spinal cord injury because of trauma to the spinal cord
and stimulation of the sympathetic nervous system (Partida et al., 2018).
Interpretation#3: Mr. Patience is at risk of hypoxemia because of c-spine fracture and bleeding
Rationale: Risk of hypoxemia has been interpreted because of shortness of breath, oxygen 93%
and temperature of 35.9. This indicates that the patient might require supplemental oxygen.
Planning: In response to the anticipated problem for patient, the anticipated plan of care or
nursing response are as follows:
Response#1: To reduce the problem of intense pain and immobility, it is planned to provide
medications like muscle relaxant and employ relaxation technique to alleviate pain and anxiety
for patient.
Rationale: Muscle relaxant like Dantrolene and analgesics are effective in relieving muscle
spasm and pain due to spasticity. Furthermore, comfort measures like cold packs and deep
breathing exercise works to promote sense of control and coping abilities in Mr. Patience. Jeon et
al. (2014) gives evidence regarding the efficacy of Dantrolene in treating spasticity after spinal
cord injury. Busch et al. (2012) gives the evidence that deep breathing technique is often
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4SIMULATION SCENARIO
integrated in many multimodal treatment approaches because of its effect on pain perception and
autonomic activity.
Response#2: It is planned to provide intravenous fluid resuscitation to patient to overcome
neurogenic shock.
Rationale: The main rationale behind giving the nursing intervention of intravenous fluid
resuscitation is that it is appropriate for compensation of the vasogenic dilation that occur post
injury in patient. Fluid replacement with crystalloid results in vasodilation and management of
initial neurogenic shock. This can be followed by administration of drugs like dopamine to treat
hypotension (Boyd & Keene, 2017).
Response#3: Mr. Patience needs to be provided supplementation oxygen because of symptom of
respiratory distress evidenced by symptom of shortness of breath and oxygen rate of 93%.
Rationale: This intervention is necessary because spinal cord injuries often lead to respiratory
impairment because of hypoventilation and mucus plugging (Galeiras Vázquez et al., 2013).
Hence, supplemental oxygen can address and control respiratory complication in patient.
Implementation: To successfully implement the above nursing care plan, it is planned to
collaborate with nurses, physicians, dieticians and therapist to address various needs of patients.
For example role of dietician and nurse is necessary to understand medication and nutritional
needs for client in the event of increased pain and discomfort. They will also play a role in
implementing fluid resuscitation and supplement oxygen therapy. Furthermore, therapist and
physician will play a role in position changes and promote mobility for Mr. Patience.
Evaluation: By using the ADPIE model to identify and interpret patient problem, I was able to
identify concerns and consequence of the issues for patient. By systematically following the five
integrated in many multimodal treatment approaches because of its effect on pain perception and
autonomic activity.
Response#2: It is planned to provide intravenous fluid resuscitation to patient to overcome
neurogenic shock.
Rationale: The main rationale behind giving the nursing intervention of intravenous fluid
resuscitation is that it is appropriate for compensation of the vasogenic dilation that occur post
injury in patient. Fluid replacement with crystalloid results in vasodilation and management of
initial neurogenic shock. This can be followed by administration of drugs like dopamine to treat
hypotension (Boyd & Keene, 2017).
Response#3: Mr. Patience needs to be provided supplementation oxygen because of symptom of
respiratory distress evidenced by symptom of shortness of breath and oxygen rate of 93%.
Rationale: This intervention is necessary because spinal cord injuries often lead to respiratory
impairment because of hypoventilation and mucus plugging (Galeiras Vázquez et al., 2013).
Hence, supplemental oxygen can address and control respiratory complication in patient.
Implementation: To successfully implement the above nursing care plan, it is planned to
collaborate with nurses, physicians, dieticians and therapist to address various needs of patients.
For example role of dietician and nurse is necessary to understand medication and nutritional
needs for client in the event of increased pain and discomfort. They will also play a role in
implementing fluid resuscitation and supplement oxygen therapy. Furthermore, therapist and
physician will play a role in position changes and promote mobility for Mr. Patience.
Evaluation: By using the ADPIE model to identify and interpret patient problem, I was able to
identify concerns and consequence of the issues for patient. By systematically following the five
5SIMULATION SCENARIO
steps of the model, I was able to take appropriate clinical judgment for the decision as well as
identify the steps needed to debrief other health care team about the physical health needs of Mr.
Patience.
Conclusion: To conclude, by the experience of deciding nursing response and care priorities for
Mr. patience, it can be said that the ADPIE is an effective model for promoting critical thinking
and increasing the benefits of health care provision. It encourages thorough evaluation of
patient’s outcome.
steps of the model, I was able to take appropriate clinical judgment for the decision as well as
identify the steps needed to debrief other health care team about the physical health needs of Mr.
Patience.
Conclusion: To conclude, by the experience of deciding nursing response and care priorities for
Mr. patience, it can be said that the ADPIE is an effective model for promoting critical thinking
and increasing the benefits of health care provision. It encourages thorough evaluation of
patient’s outcome.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6SIMULATION SCENARIO
References:
Boyd, M., & Keene, D. D. (2017). Management of shock in trauma. Anaesthesia & Intensive
Care Medicine, 18(8), 386-389.
Busch, V., Magerl, W., Kern, U., Haas, J., Hajak, G. and Eichhammer, P., 2012. The effect of
deep and slow breathing on pain perception, autonomic activity, and mood processing—
an experimental study. Pain Medicine, 13(2), pp.215-228.
Galeiras Vázquez, R., Rascado Sedes, P., Mourelo Fariña, M., Montoto Marqués, A. and Ferreiro
Velasco, M.E., 2013. Respiratory management in the patient with spinal cord
injury. BioMed research international, 2013.
Jeon, J., Song, S., Kim, M. C., Kim, K. M., & Lee, S. (2014). The effect of long-term oral
dantrolene on the neuromuscular action of rocuronium: a case report. Korean journal of
anesthesiology, 66(2), 153.
Partida, E., Mironets, E., Hou, S., & Tom, V. J. (2016). Cardiovascular dysfunction following
spinal cord injury. Neural regeneration research, 11(2), 189.
Zonfrillo, M. R., Locey, C. M., Scarfone, S. R., & Arbogast, K. B. (2014). Motor vehicle crash–
related injury causation scenarios for spinal injuries in restrained children and
adolescents. Traffic injury prevention, 15(sup1), S49-S55.
References:
Boyd, M., & Keene, D. D. (2017). Management of shock in trauma. Anaesthesia & Intensive
Care Medicine, 18(8), 386-389.
Busch, V., Magerl, W., Kern, U., Haas, J., Hajak, G. and Eichhammer, P., 2012. The effect of
deep and slow breathing on pain perception, autonomic activity, and mood processing—
an experimental study. Pain Medicine, 13(2), pp.215-228.
Galeiras Vázquez, R., Rascado Sedes, P., Mourelo Fariña, M., Montoto Marqués, A. and Ferreiro
Velasco, M.E., 2013. Respiratory management in the patient with spinal cord
injury. BioMed research international, 2013.
Jeon, J., Song, S., Kim, M. C., Kim, K. M., & Lee, S. (2014). The effect of long-term oral
dantrolene on the neuromuscular action of rocuronium: a case report. Korean journal of
anesthesiology, 66(2), 153.
Partida, E., Mironets, E., Hou, S., & Tom, V. J. (2016). Cardiovascular dysfunction following
spinal cord injury. Neural regeneration research, 11(2), 189.
Zonfrillo, M. R., Locey, C. M., Scarfone, S. R., & Arbogast, K. B. (2014). Motor vehicle crash–
related injury causation scenarios for spinal injuries in restrained children and
adolescents. Traffic injury prevention, 15(sup1), S49-S55.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

7SIMULATION SCENARIO
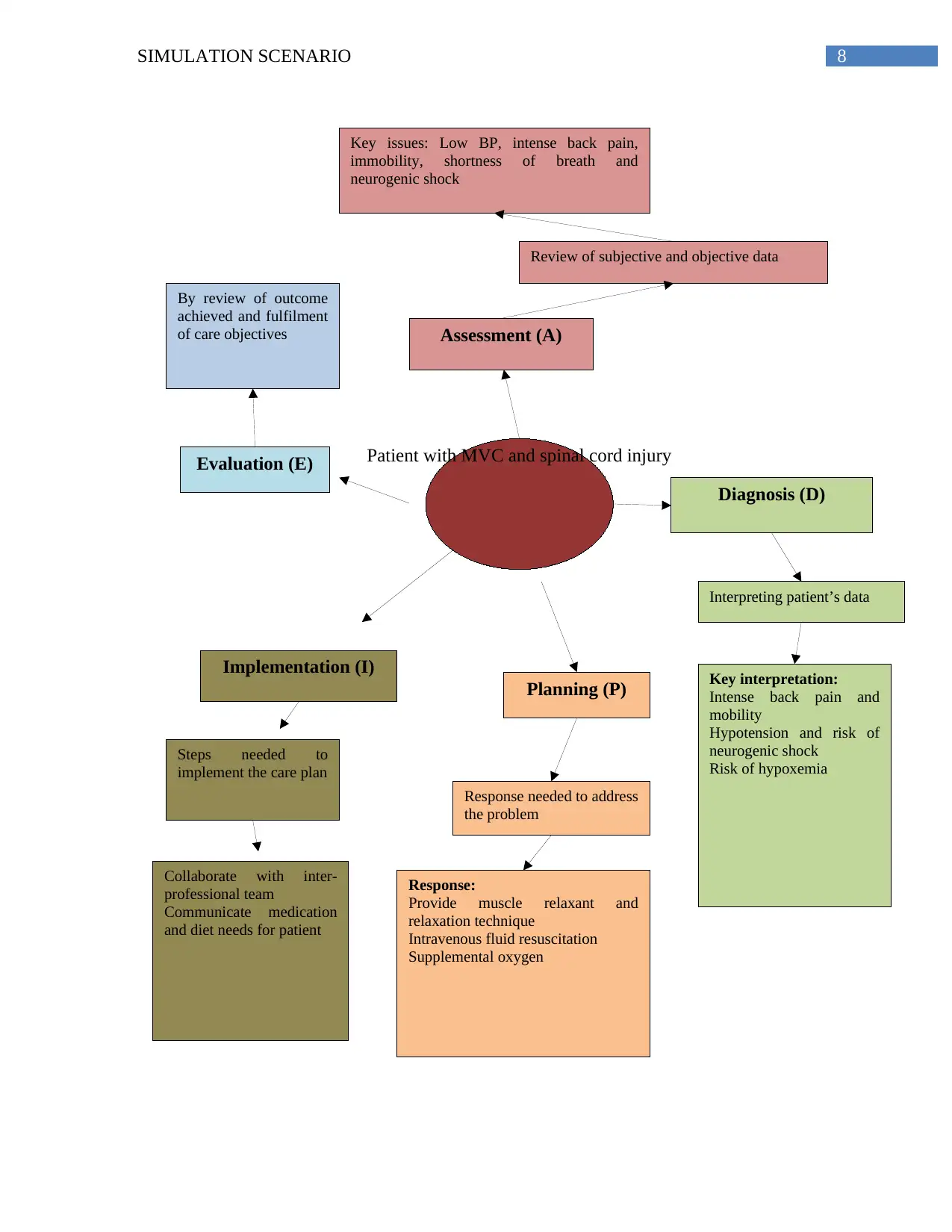
Appendix:
1. Mind map for clinical decision making:
Appendix:
1. Mind map for clinical decision making:
8SIMULATION SCENARIO
Patient with MVC and spinal cord injury
Assessment (A)
Diagnosis (D)
Planning (P)
Implementation (I)
Evaluation (E)
Review of subjective and objective data
Key issues: Low BP, intense back pain,
immobility, shortness of breath and
neurogenic shock
Interpreting patient’s data
Key interpretation:
Intense back pain and
mobility
Hypotension and risk of
neurogenic shock
Risk of hypoxemia
Response needed to address
the problem
Response:
Provide muscle relaxant and
relaxation technique
Intravenous fluid resuscitation
Supplemental oxygen
Steps needed to
implement the care plan
Collaborate with inter-
professional team
Communicate medication
and diet needs for patient
By review of outcome
achieved and fulfilment
of care objectives
Patient with MVC and spinal cord injury
Assessment (A)
Diagnosis (D)
Planning (P)
Implementation (I)
Evaluation (E)
Review of subjective and objective data
Key issues: Low BP, intense back pain,
immobility, shortness of breath and
neurogenic shock
Interpreting patient’s data
Key interpretation:
Intense back pain and
mobility
Hypotension and risk of
neurogenic shock
Risk of hypoxemia
Response needed to address
the problem
Response:
Provide muscle relaxant and
relaxation technique
Intravenous fluid resuscitation
Supplemental oxygen
Steps needed to
implement the care plan
Collaborate with inter-
professional team
Communicate medication
and diet needs for patient
By review of outcome
achieved and fulfilment
of care objectives
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





