Critique report - Skin glue minimizes the failure of ED-inserted PIVCs: A randomized controlled trial
VerifiedAdded on 2023/06/12
|13
|3352
|388
AI Summary
This critique report evaluates a quantitative study on the use of skin glue to minimize the failure of ED-inserted PIVCs. The report includes a PICO table, review of literature, research design, sample, data collection, data analysis, results, conclusion, and relevance to nursing practice.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Critique report
Critical Review- Quantitative Study
On
Skin glue minimizes the failure of ED (emergency department)- inserted PIVCs
(peripheral intravenous catheters): A randomized controlled trial.
1
Critical Review- Quantitative Study
On
Skin glue minimizes the failure of ED (emergency department)- inserted PIVCs
(peripheral intravenous catheters): A randomized controlled trial.
1
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Critique report
Critical Review- Quantitative Study
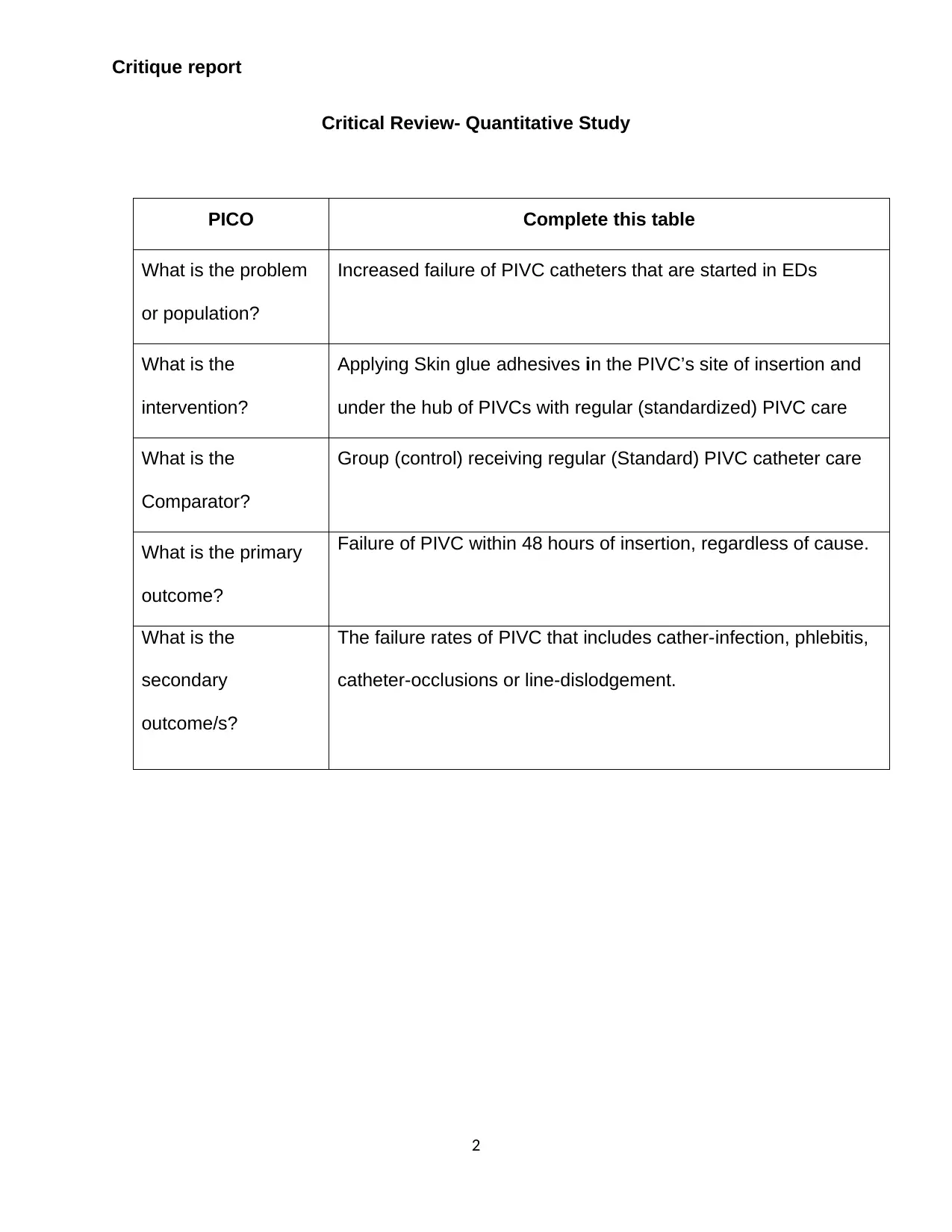
PICO Complete this table
What is the problem
or population?
Increased failure of PIVC catheters that are started in EDs
What is the
intervention?
Applying Skin glue adhesives in the PIVC’s site of insertion and
under the hub of PIVCs with regular (standardized) PIVC care
What is the
Comparator?
Group (control) receiving regular (Standard) PIVC catheter care
What is the primary
outcome?
Failure of PIVC within 48 hours of insertion, regardless of cause.
What is the
secondary
outcome/s?
The failure rates of PIVC that includes cather-infection, phlebitis,
catheter-occlusions or line-dislodgement.
2
Critical Review- Quantitative Study
PICO Complete this table
What is the problem
or population?
Increased failure of PIVC catheters that are started in EDs
What is the
intervention?
Applying Skin glue adhesives in the PIVC’s site of insertion and
under the hub of PIVCs with regular (standardized) PIVC care
What is the
Comparator?
Group (control) receiving regular (Standard) PIVC catheter care
What is the primary
outcome?
Failure of PIVC within 48 hours of insertion, regardless of cause.
What is the
secondary
outcome/s?
The failure rates of PIVC that includes cather-infection, phlebitis,
catheter-occlusions or line-dislodgement.
2
Critique report
Introduction
A critical review is a systematic way of logically evaluating a study to identify its
strengths as well as weaknesses along with its applicability in clinical practice (Boswell,
2017). A quantitative study can be critiqued by using many models as CASP,
CONSORT, Polit critiquing-tools and Crombie models (University of South Australia, n.
d.). CONSORT (Consolidated standards for randomized-trials) guidelines are explicitly
developed for critiquing RCT that includes a checklist (22 items) and flow-chart to track
the study-participants from the trial through eligibility-assessment (Polit, 2016).
Annals are an international peer-reviewed emergency journal that was published
by the American college’s ED physicians in United States. It is the largest circulating
journal with impact- factor: 5.008, five year’s impact factor: 5.041 and Science citation-
index journal-rank: 1.942 with over 33,000 subscribers. It publishes articles, facts,
reports, and opinions related to emergency medicine that includes pediatric, toxicology,
injuries with prevention in other specialties which suggest that Annals are the highly
regarded journal (ACEP, 2016). The above informations prove that Annals will definitely
help me to provide evidence-based care to ED patients.
The authors Bugden, Scott, Clark and Johnstone are the emergency experts of
Caboolture-Hospital; author Mihala from the Applied Health-related Economics’ centre,
Griffith University while Bugden, Fraser and Rickard is from the NHMRC’s Centre for
Nursing-Research and also the members of Critical-care research group. Author’s
current position helps me to utilize the study’s findings undoubtedly in my clinical area
and prevent PIVC failure.
3
Introduction
A critical review is a systematic way of logically evaluating a study to identify its
strengths as well as weaknesses along with its applicability in clinical practice (Boswell,
2017). A quantitative study can be critiqued by using many models as CASP,
CONSORT, Polit critiquing-tools and Crombie models (University of South Australia, n.
d.). CONSORT (Consolidated standards for randomized-trials) guidelines are explicitly
developed for critiquing RCT that includes a checklist (22 items) and flow-chart to track
the study-participants from the trial through eligibility-assessment (Polit, 2016).
Annals are an international peer-reviewed emergency journal that was published
by the American college’s ED physicians in United States. It is the largest circulating
journal with impact- factor: 5.008, five year’s impact factor: 5.041 and Science citation-
index journal-rank: 1.942 with over 33,000 subscribers. It publishes articles, facts,
reports, and opinions related to emergency medicine that includes pediatric, toxicology,
injuries with prevention in other specialties which suggest that Annals are the highly
regarded journal (ACEP, 2016). The above informations prove that Annals will definitely
help me to provide evidence-based care to ED patients.
The authors Bugden, Scott, Clark and Johnstone are the emergency experts of
Caboolture-Hospital; author Mihala from the Applied Health-related Economics’ centre,
Griffith University while Bugden, Fraser and Rickard is from the NHMRC’s Centre for
Nursing-Research and also the members of Critical-care research group. Author’s
current position helps me to utilize the study’s findings undoubtedly in my clinical area
and prevent PIVC failure.
3
Critique report
Title, Abstract & Review of Literature
They have stated a clear title that stimulates a prompt perception of the study’s
fundamental nature and is also consistent with the text (Melnyk, 2014). They have given
a clear and acceptable objective as ‘to investigate whether the effect of Skin glue
application and regular care can reduce the ED-inserted PIVC failure rate. An abstract
should provoke clear insight into the study’s complexity and its applicability into the
particular healthcare practice setting (Iverson, 2014). The study’s abstract includes an
accurate-objective, focused-hypothesis, appropriate study-methods, results and
conclusions. They have cited current, appropriate, relevant as well as comprehensive
literatures. Bugden (2016) has discussed what is already known about the topic;
identified knowledge inconsistencies, mentioned the study’s significance and has also
situated this study within the best-available knowledge, as given by Polit (2016).
Research Design
Bugden (2016) has used RCT which is a true-experimental quantitative design in
which the investigator manipulates (Skin-glue application & regular measure), controls
the independent variable (regular-care group) and randomly assigns samples to both
control and experimental group (LoBiondo-Wood, 2014). RCT is considered as a gold
standard for providing reliable evidences in-regard to cause and effect relationship
(Polit, 2016). They have clearly stated their research question as ‘Whether the Skin-glue
applications to secure the PIVCs can prevent PIVC’s failure than usual securing
method?’, that matches the study’s purpose.
According to Limm (2013), about 80% of the hospital-admitted patients are
inserted with PIVCs with more specifically in emergencies. Majority of PIVCs are found
4
Title, Abstract & Review of Literature
They have stated a clear title that stimulates a prompt perception of the study’s
fundamental nature and is also consistent with the text (Melnyk, 2014). They have given
a clear and acceptable objective as ‘to investigate whether the effect of Skin glue
application and regular care can reduce the ED-inserted PIVC failure rate. An abstract
should provoke clear insight into the study’s complexity and its applicability into the
particular healthcare practice setting (Iverson, 2014). The study’s abstract includes an
accurate-objective, focused-hypothesis, appropriate study-methods, results and
conclusions. They have cited current, appropriate, relevant as well as comprehensive
literatures. Bugden (2016) has discussed what is already known about the topic;
identified knowledge inconsistencies, mentioned the study’s significance and has also
situated this study within the best-available knowledge, as given by Polit (2016).
Research Design
Bugden (2016) has used RCT which is a true-experimental quantitative design in
which the investigator manipulates (Skin-glue application & regular measure), controls
the independent variable (regular-care group) and randomly assigns samples to both
control and experimental group (LoBiondo-Wood, 2014). RCT is considered as a gold
standard for providing reliable evidences in-regard to cause and effect relationship
(Polit, 2016). They have clearly stated their research question as ‘Whether the Skin-glue
applications to secure the PIVCs can prevent PIVC’s failure than usual securing
method?’, that matches the study’s purpose.
According to Limm (2013), about 80% of the hospital-admitted patients are
inserted with PIVCs with more specifically in emergencies. Majority of PIVCs are found
4
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Critique report
to prematurely fail because of site-infections, catheter’s dislodgement or others (Marsh,
2015). Such type of failure appears to occur because of improper device fixations in the
patient’s skin. Bugden (2016) suggests that no previous studies have been conducted
to identify the best securing measures for PIVCs. Hence, their experiment in using the
cyanoacrylate skin-glue with regular securement in improving the device fixations is
highly crucial.
Hypothesis is defined as the expected relationship between variables (Polit,
2016). They have given a concise and testable scientific hypothesis as ‘the application
of skin-glue can minimize the failure of PIVCs within 48 hrs’, to draw the relationship
between independent (Skin-glue application) and dependent variable (PIVC-failure).
They conducted single-sited, two-arm, non-blinded, RCT-trial among 360 subjects
having 380 catheter insertions. They randomized the subjects with the help of
Randomizer’s-software for clinical trial to both the experimental (Skin-glue securing &
regular securement as per guidelines of Queensland, 2015) and control subjects
(regular care) in 1:1 ratio. The experimental subjects received skin-glue adhesive in the
insertion-site as well as PIVC’s hub to enhance its securement.
Sample
Grove (2015) stated that the process of selecting target population and study-
participants by using appropriate sampling frame is highly crucial. They are interested to
propose their study among the ED-patients with catheter-insertions; admitted in
Caboolture Hospital. Their setting of Caboolture Hospital is a community hospital (50km
from North of Brisbane) with 52,000 ED-presentations every year. Samples are the
aggregate of the entire population. They recruited subjects using random sampling by
5
to prematurely fail because of site-infections, catheter’s dislodgement or others (Marsh,
2015). Such type of failure appears to occur because of improper device fixations in the
patient’s skin. Bugden (2016) suggests that no previous studies have been conducted
to identify the best securing measures for PIVCs. Hence, their experiment in using the
cyanoacrylate skin-glue with regular securement in improving the device fixations is
highly crucial.
Hypothesis is defined as the expected relationship between variables (Polit,
2016). They have given a concise and testable scientific hypothesis as ‘the application
of skin-glue can minimize the failure of PIVCs within 48 hrs’, to draw the relationship
between independent (Skin-glue application) and dependent variable (PIVC-failure).
They conducted single-sited, two-arm, non-blinded, RCT-trial among 360 subjects
having 380 catheter insertions. They randomized the subjects with the help of
Randomizer’s-software for clinical trial to both the experimental (Skin-glue securing &
regular securement as per guidelines of Queensland, 2015) and control subjects
(regular care) in 1:1 ratio. The experimental subjects received skin-glue adhesive in the
insertion-site as well as PIVC’s hub to enhance its securement.
Sample
Grove (2015) stated that the process of selecting target population and study-
participants by using appropriate sampling frame is highly crucial. They are interested to
propose their study among the ED-patients with catheter-insertions; admitted in
Caboolture Hospital. Their setting of Caboolture Hospital is a community hospital (50km
from North of Brisbane) with 52,000 ED-presentations every year. Samples are the
aggregate of the entire population. They recruited subjects using random sampling by
5
Critique report
allotting 174 ED-patients having PIVCs to both groups in which all the members of
population will get equal chance of being selected (Iverson, 2014).
Ethical guidelines are the standards that govern the degree to which the
experiment follows the moral & legal obligations in-order to protect the individual’s
privacy (LoBiondo-Wood, 2014). They obtained written consent from their subjects to
protect the patient from harm. They got ethical approval from the ethics committee of
Caboolture Hospital and have also got registered in the clinical-trials registry of Australia
& New Zealand.
Data collection
Quantitative data-collection involves collection of information in a numeric form
(Gerrish, 2015). They collected demographic and study-cofounder data at the time of
patient’s recruitment using self-developed questionnaires including categories of age,
gender, medication intake, PIVC details with time from PIVCs insertion to intervention &
follow up. They have analyzed their primary outcome of PIVC-failure within 48 hours by
directly observing the hospitalized-patients or telephoning the discharged-patients and
secondary outcomes of investigating the individual aspects of PIVC-failure (infection,
occlusion, vein-phlebitis and dislodgement) through observation (direct), reviewing
patient’s chart and questionnaire method. Data was collected by 1 of 3 nurses
experienced in EDs for 16 hours/ day in one week by above methods.
According to Grove (2015), the researchers should give rationale with
advantages and disadvantages of selecting particular tool as compared with other tool
and their literature search should have mentioned about the selection of specific tool.
Bugden (2016) has not explained about the advantage of selecting their tool but has
6
allotting 174 ED-patients having PIVCs to both groups in which all the members of
population will get equal chance of being selected (Iverson, 2014).
Ethical guidelines are the standards that govern the degree to which the
experiment follows the moral & legal obligations in-order to protect the individual’s
privacy (LoBiondo-Wood, 2014). They obtained written consent from their subjects to
protect the patient from harm. They got ethical approval from the ethics committee of
Caboolture Hospital and have also got registered in the clinical-trials registry of Australia
& New Zealand.
Data collection
Quantitative data-collection involves collection of information in a numeric form
(Gerrish, 2015). They collected demographic and study-cofounder data at the time of
patient’s recruitment using self-developed questionnaires including categories of age,
gender, medication intake, PIVC details with time from PIVCs insertion to intervention &
follow up. They have analyzed their primary outcome of PIVC-failure within 48 hours by
directly observing the hospitalized-patients or telephoning the discharged-patients and
secondary outcomes of investigating the individual aspects of PIVC-failure (infection,
occlusion, vein-phlebitis and dislodgement) through observation (direct), reviewing
patient’s chart and questionnaire method. Data was collected by 1 of 3 nurses
experienced in EDs for 16 hours/ day in one week by above methods.
According to Grove (2015), the researchers should give rationale with
advantages and disadvantages of selecting particular tool as compared with other tool
and their literature search should have mentioned about the selection of specific tool.
Bugden (2016) has not explained about the advantage of selecting their tool but has
6
Critique report
commented on their tool reference from Rickard (2012). They have given their
measurement variables but their measurement method was missing. The reliability
(degree of accuracy) and validity (degree to which the tool measures) has to be
determined in pilot study which was not found in this study.
Bias is an influence that can produce error in the study results (Grove, 2015). No
evidence of sample imbalances as they have adopted random-sampling approach to
give equal chance to all subjects to be selected for both groups with minimal sample
losses (Polit, 2016). Blinding involves preventing the subjects from knowing the details
of participants, investigation and researchers to avoid bias (LoBiondo-Wood, 2014).
They have not blinded the subjects because of their intervention’s nature having subtitle
skin glue color as well as appearance on the patient’s limb. Research nurses were also
not-masked as they are the one who allocates subjects to intervention group.
Data Analysis
They have performed quantitative-analysis by manipulating the numerical-data
using statistical methods to evaluate the magnitude of the relationships between
variables (Polit, 2016). They determined the sample’s size by assuming a single
PIVC/patient and hypothesizing PIVC failure-rates of 11% in control and 4% in
treatment groups (80% power). Even-though the subject loss to follow-up was low
(2.8%/device, 0.83%/patient) with similar occurrence in both groups, they have
excluded the subjects with incomplete data. They performed descriptive analysis to
describe and synthesis data through averages and percentages and inferential analysis
to draw conclusions at CI95% (confidence intervals) and statistical significance at p<.05.
They performed per-patient analysis in multiple PIVC patients.
7
commented on their tool reference from Rickard (2012). They have given their
measurement variables but their measurement method was missing. The reliability
(degree of accuracy) and validity (degree to which the tool measures) has to be
determined in pilot study which was not found in this study.
Bias is an influence that can produce error in the study results (Grove, 2015). No
evidence of sample imbalances as they have adopted random-sampling approach to
give equal chance to all subjects to be selected for both groups with minimal sample
losses (Polit, 2016). Blinding involves preventing the subjects from knowing the details
of participants, investigation and researchers to avoid bias (LoBiondo-Wood, 2014).
They have not blinded the subjects because of their intervention’s nature having subtitle
skin glue color as well as appearance on the patient’s limb. Research nurses were also
not-masked as they are the one who allocates subjects to intervention group.
Data Analysis
They have performed quantitative-analysis by manipulating the numerical-data
using statistical methods to evaluate the magnitude of the relationships between
variables (Polit, 2016). They determined the sample’s size by assuming a single
PIVC/patient and hypothesizing PIVC failure-rates of 11% in control and 4% in
treatment groups (80% power). Even-though the subject loss to follow-up was low
(2.8%/device, 0.83%/patient) with similar occurrence in both groups, they have
excluded the subjects with incomplete data. They performed descriptive analysis to
describe and synthesis data through averages and percentages and inferential analysis
to draw conclusions at CI95% (confidence intervals) and statistical significance at p<.05.
They performed per-patient analysis in multiple PIVC patients.
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Critique report
Results
The primary outcome of PIVC failure-rate at 48 hrs was noted to be lowered in
skin-glue (17%) than regular-care (27%) patients (CI95%:–18% to –2%; p=.02), less
than 5% possibility (p<.05) of being caused by chance and hence was statistically
significant, thus hypothesis was accepted, similar to Edwards (2014). The secondary
outcome of dislodgement was lowered in skin-glue (7.0%) than regular-care (14%)
patients (CI95%:–13% to 0%, p=0.04) at p<.05 suggesting statistically-significant, thus
hypothesis accepted.
Phlebitis-rate (CI95%:–5% to 3%) and occlusions (CI95%:–8% to 4%) were
reduced in skin-glue as compared to regular-care patients but not statistically-
significant, thus hypothesis was rejected in-regard to these failure-modes. Infection was
absent in both groups. In-case of per-patient analysis of standard Vs skin-glue group,
primary failure-rate: 52 Vs 31; secondary failure-rate: dislodgement: 25 Vs 12, infection:
0 Vs 0, phlebitis: 9 Vs 5 & occlusion: 20 Vs 14 indicates that skin-glue usage with
regular-care could minimize PIVC’s failure. They haven’t given permission to replicate
their study yet they have mentioned of conducting cost-benefit analysis in the future.
They have given implications as adding skin-glue adhesives enables PIVC stabilization
and serves as simplest and rapid measure to be carried-out in emergencies.
Conclusion
In conclusion, the major findings of the study based on their original objectives
should be discussed in-regard to whether the analyzed-data supports/negates the
study-hypothesis (Grove, 2015). They have given that the application of a single drop of
skin glue in the insertion site and hub of PIVC plus standard PIVC care as suggested by
8
Results
The primary outcome of PIVC failure-rate at 48 hrs was noted to be lowered in
skin-glue (17%) than regular-care (27%) patients (CI95%:–18% to –2%; p=.02), less
than 5% possibility (p<.05) of being caused by chance and hence was statistically
significant, thus hypothesis was accepted, similar to Edwards (2014). The secondary
outcome of dislodgement was lowered in skin-glue (7.0%) than regular-care (14%)
patients (CI95%:–13% to 0%, p=0.04) at p<.05 suggesting statistically-significant, thus
hypothesis accepted.
Phlebitis-rate (CI95%:–5% to 3%) and occlusions (CI95%:–8% to 4%) were
reduced in skin-glue as compared to regular-care patients but not statistically-
significant, thus hypothesis was rejected in-regard to these failure-modes. Infection was
absent in both groups. In-case of per-patient analysis of standard Vs skin-glue group,
primary failure-rate: 52 Vs 31; secondary failure-rate: dislodgement: 25 Vs 12, infection:
0 Vs 0, phlebitis: 9 Vs 5 & occlusion: 20 Vs 14 indicates that skin-glue usage with
regular-care could minimize PIVC’s failure. They haven’t given permission to replicate
their study yet they have mentioned of conducting cost-benefit analysis in the future.
They have given implications as adding skin-glue adhesives enables PIVC stabilization
and serves as simplest and rapid measure to be carried-out in emergencies.
Conclusion
In conclusion, the major findings of the study based on their original objectives
should be discussed in-regard to whether the analyzed-data supports/negates the
study-hypothesis (Grove, 2015). They have given that the application of a single drop of
skin glue in the insertion site and hub of PIVC plus standard PIVC care as suggested by
8
Critique report
Queensland’s Department of Health (2015) can control the failure of PIVCs in adults
being admitted in hospital emergencies. The reduction of the failure of PIVC can help
the patients by enhancing comfort and reducing the number of admissions in hospital.
According to Budgen (2016), the application of skin-glue (cyanoacrylate) can make the
PIVC lines to become harder and so unintentional PIVC removal as well as site-
infection is minimized (HospiMedica, 2016). They also suggested that using skin- glue
in catheter site can in-directly prevent interruptions to medication therapies, thereby
preventing patient’s anxiety and discomfort of reinserting PIVCs.
Relevance to nursing practice
Nursing professionals should constantly contemplate research articles to develop
solutions and/or outcomes for patient care; that forms the highest available evidence to
continuously validate and promote nursing-care (Grove, 2015). According to PoIit
(2016), evidence based practice is the conscientious use of current- best evidence to
make clinical judgment about client care. Nurses who are the basic care providers
should provide quality evidence care to all the patients based on the ethical principles
(ACSQHC, 2013).
Nursing care rendered to the patients should maximize benefit to the patients
and minimize harms based on the principle of beneficence and should not cause any
harm and/or discomforts to them (maleficience) that includes physical harms (injuries),
psychological harm (anxiety, stress), social (no societal support) as well as economical
harm (loss of income). The care should be rendered by respecting their dignity and
justice (Polit, 2016). Hence, much emphasis has to be given to practice evidence-
based care and to protect patient’s lives.
9
Queensland’s Department of Health (2015) can control the failure of PIVCs in adults
being admitted in hospital emergencies. The reduction of the failure of PIVC can help
the patients by enhancing comfort and reducing the number of admissions in hospital.
According to Budgen (2016), the application of skin-glue (cyanoacrylate) can make the
PIVC lines to become harder and so unintentional PIVC removal as well as site-
infection is minimized (HospiMedica, 2016). They also suggested that using skin- glue
in catheter site can in-directly prevent interruptions to medication therapies, thereby
preventing patient’s anxiety and discomfort of reinserting PIVCs.
Relevance to nursing practice
Nursing professionals should constantly contemplate research articles to develop
solutions and/or outcomes for patient care; that forms the highest available evidence to
continuously validate and promote nursing-care (Grove, 2015). According to PoIit
(2016), evidence based practice is the conscientious use of current- best evidence to
make clinical judgment about client care. Nurses who are the basic care providers
should provide quality evidence care to all the patients based on the ethical principles
(ACSQHC, 2013).
Nursing care rendered to the patients should maximize benefit to the patients
and minimize harms based on the principle of beneficence and should not cause any
harm and/or discomforts to them (maleficience) that includes physical harms (injuries),
psychological harm (anxiety, stress), social (no societal support) as well as economical
harm (loss of income). The care should be rendered by respecting their dignity and
justice (Polit, 2016). Hence, much emphasis has to be given to practice evidence-
based care and to protect patient’s lives.
9
Critique report
Douglas (2012) given that a nursing professional should strive to prevent illness,
promote health and protect health, which implies protecting patient from harms. Nurses
should propose appropriate research studies to develop more evidences to protect our
profession. As nurses are the front-line care givers in ED of any hospitals, they should
render life- saving measures to the patients in which PIVC catheter insertion is
commonly needed to initiate management process and should be expertise in protect it
from its premature failure and PIVC dislodgement, infections at the catheter insertion
site and PIVC occlusions because of blood clot or phlebitis (Rebelem, 2016).
PIVC’s failure can cause disruption of therapies to patients as hydration,
antibiotic and/or analgesic therapies causing deterioration in patient’s heath severely as
well as interrupting the treatment modalities and cause systemic sepsis (Stuart, 2013).
This indirectly burdens the clients and their families by rising the cost, causing anxiety,
stress and discomfort of re-inserting the PIVCs repeatedly (Aymes, 2016). Therefore,
nurses should increase expertise to secure PIVC line safely in-order to protect the
values of patient.
PIVC also increases the healthcare cost of a Nation by increasing the time of
staffs in client’s care, extending length of hospital’s stay and increasing adverse event’s
management. According to Wallis (2014), at-least a minor reduction in the IV-device
failure can cause greater improvements in client-care, healthcare outcomes and
healthcare costs. Hence, nurses should use skin glue adhesives to secure PIVCs with
patient’s skin to promote patient’s values, minimize healthcare cost and enhance patient
treatment.
10
Douglas (2012) given that a nursing professional should strive to prevent illness,
promote health and protect health, which implies protecting patient from harms. Nurses
should propose appropriate research studies to develop more evidences to protect our
profession. As nurses are the front-line care givers in ED of any hospitals, they should
render life- saving measures to the patients in which PIVC catheter insertion is
commonly needed to initiate management process and should be expertise in protect it
from its premature failure and PIVC dislodgement, infections at the catheter insertion
site and PIVC occlusions because of blood clot or phlebitis (Rebelem, 2016).
PIVC’s failure can cause disruption of therapies to patients as hydration,
antibiotic and/or analgesic therapies causing deterioration in patient’s heath severely as
well as interrupting the treatment modalities and cause systemic sepsis (Stuart, 2013).
This indirectly burdens the clients and their families by rising the cost, causing anxiety,
stress and discomfort of re-inserting the PIVCs repeatedly (Aymes, 2016). Therefore,
nurses should increase expertise to secure PIVC line safely in-order to protect the
values of patient.
PIVC also increases the healthcare cost of a Nation by increasing the time of
staffs in client’s care, extending length of hospital’s stay and increasing adverse event’s
management. According to Wallis (2014), at-least a minor reduction in the IV-device
failure can cause greater improvements in client-care, healthcare outcomes and
healthcare costs. Hence, nurses should use skin glue adhesives to secure PIVCs with
patient’s skin to promote patient’s values, minimize healthcare cost and enhance patient
treatment.
10
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Critique report
Reference
ACEP- (American college of Emergency- Physicians). (2016). Annals of Emergency
Medicine. Retrieved from https://www.acep.org/annals
ACSQHC (Australian Commission on Safety and Quality in HealthCare). (2013).
Literature Review: Medication Safety in Australia. ACSQHC, Sydney.
Aymes, S. (2016). Skin Glue Reduces IV Failure Rate in the Emergency Department.
Retrieved from http://www.acepnow.com/skin-glue-reduces-iv-failure-rate-in-the-
emergency-department/
Boswell, C & Cannon. . (2017). Introduction to nursing research- Incorporating evidence
based practice Retrieved from https://books.google.co.in/books?
id=nsQwCwAAQBAJ&pg=
PA312&dq=Polit+tools+in+research&hl=en&sa=X&ved=0ahUKEwj6xdOJmpHbA
hUBKJQKHYLMBKQQ6AEIXzAJ#v=onepage&q=Polit%20tools%20in
%20research&f=fal
Bugden, S., Shean, K., Scott, M., Mihala, G., Clark, S., Johnstone, C., … Rickard, C.
(2016). Skin glue reduces the failure rate of emergency department-inserted
peripheral intravenous catheters: A randomized controlled trial. Annals of
Emergency Medicine, 68,
196–201.http://dx.doi.org/10.1016/j.annemergmed.2015.11.026
Douglas, C. (2012). Potter and Perry’s Fundamentals of Nursing- Australian version. (4th
edition). Elsevier: St. Louis, Missouri
Edwards, M. (2014). A pilot trial of bordered polyurethane dressings, tissue adhesive
and sutureless devices compared with standard polyurethane dressings for
securing short term arterial catheters. Crit Care Resusc,16, 175-183.
11
Reference
ACEP- (American college of Emergency- Physicians). (2016). Annals of Emergency
Medicine. Retrieved from https://www.acep.org/annals
ACSQHC (Australian Commission on Safety and Quality in HealthCare). (2013).
Literature Review: Medication Safety in Australia. ACSQHC, Sydney.
Aymes, S. (2016). Skin Glue Reduces IV Failure Rate in the Emergency Department.
Retrieved from http://www.acepnow.com/skin-glue-reduces-iv-failure-rate-in-the-
emergency-department/
Boswell, C & Cannon. . (2017). Introduction to nursing research- Incorporating evidence
based practice Retrieved from https://books.google.co.in/books?
id=nsQwCwAAQBAJ&pg=
PA312&dq=Polit+tools+in+research&hl=en&sa=X&ved=0ahUKEwj6xdOJmpHbA
hUBKJQKHYLMBKQQ6AEIXzAJ#v=onepage&q=Polit%20tools%20in
%20research&f=fal
Bugden, S., Shean, K., Scott, M., Mihala, G., Clark, S., Johnstone, C., … Rickard, C.
(2016). Skin glue reduces the failure rate of emergency department-inserted
peripheral intravenous catheters: A randomized controlled trial. Annals of
Emergency Medicine, 68,
196–201.http://dx.doi.org/10.1016/j.annemergmed.2015.11.026
Douglas, C. (2012). Potter and Perry’s Fundamentals of Nursing- Australian version. (4th
edition). Elsevier: St. Louis, Missouri
Edwards, M. (2014). A pilot trial of bordered polyurethane dressings, tissue adhesive
and sutureless devices compared with standard polyurethane dressings for
securing short term arterial catheters. Crit Care Resusc,16, 175-183.
11
Critique report
Gerrish, K., & Lathlean, J. (2015). The research process in nursing (7th ed.). Malden,
MA: John Wiley & Sons.
Grove, S. K., Grey, J. R., & Burns, N. (2015). Understanding nursing research: Building
an evidence-based practice (6th ed.). London, United Kingdom: Elsevier
HospiMedica. (2016). IV Drip Failure Reduced by Skin Glue Application. Retrieved from
https://www.hospimedica.com/critical-care/articles/294767305/iv-drip-failure-
reduced-by-skin-glue-application.html
Iverson, K.M. (2014). Women veterans’ preferences for intimate partner violence
screening and response procedures within the Veterans Health Administration.
Research in Nursing and Health, 37, 302-311
Limm, E. (2013). Half of all peripheral intravenous lines in an Australian tertiary
emergency department are unused: pain with no gain?: Ann Emerg Med. 62:521-
525.
LoBiondo-Wood, G & Haber, J. (2014). Nursing Research: Methods and Critical
Appraisal for Evidence-Based. Retrieved from https://books.google.co.in/books?
isbn=0323100864
Marsh. (2015). Securement methods for peripheral venous catheters to prevent failure:
a randomized controlled pilot trial: J Vasc Access.16:237-244.
Melnyk, B.M et al. (2014). The establishment of EBP competencies for practicing RNs
and advanced practice nurses in real world clinical settings: Proficiencies to
improve health care quality, reliability, patient outcomes and cost: worldview on
Evidence based practice. 11 (1). 5-15. doi.10.1111./WBN.12021
12
Gerrish, K., & Lathlean, J. (2015). The research process in nursing (7th ed.). Malden,
MA: John Wiley & Sons.
Grove, S. K., Grey, J. R., & Burns, N. (2015). Understanding nursing research: Building
an evidence-based practice (6th ed.). London, United Kingdom: Elsevier
HospiMedica. (2016). IV Drip Failure Reduced by Skin Glue Application. Retrieved from
https://www.hospimedica.com/critical-care/articles/294767305/iv-drip-failure-
reduced-by-skin-glue-application.html
Iverson, K.M. (2014). Women veterans’ preferences for intimate partner violence
screening and response procedures within the Veterans Health Administration.
Research in Nursing and Health, 37, 302-311
Limm, E. (2013). Half of all peripheral intravenous lines in an Australian tertiary
emergency department are unused: pain with no gain?: Ann Emerg Med. 62:521-
525.
LoBiondo-Wood, G & Haber, J. (2014). Nursing Research: Methods and Critical
Appraisal for Evidence-Based. Retrieved from https://books.google.co.in/books?
isbn=0323100864
Marsh. (2015). Securement methods for peripheral venous catheters to prevent failure:
a randomized controlled pilot trial: J Vasc Access.16:237-244.
Melnyk, B.M et al. (2014). The establishment of EBP competencies for practicing RNs
and advanced practice nurses in real world clinical settings: Proficiencies to
improve health care quality, reliability, patient outcomes and cost: worldview on
Evidence based practice. 11 (1). 5-15. doi.10.1111./WBN.12021
12
Critique report
Polit, D.F & Beck, C.T. (2016). Nursing Research: Generating and assessing evidence
for nursing practice. Lippincott Williams & Wilkins: New Delhi.
Queensland- Department of Health. (2015). Centre for Healthcare Related Infection
Surveillance and Prevention, Australia: PIVC guideline. Retrieved from
https://www.health.qld.gov.au/publications/clinical-practice/guidelines-
procedures/diseases-infection/governance/icare-pivc-guideline.pdf.
Rebelem. (2016). Should We Use Skin Glue to Secure Peripheral IVs: R.E.B.E.L. E.M.
Retrieved from http://rebelem.com/should-we-use-skin-glue-to-secure-peripheral-
ivs/
Rickard, C.M. (2012). Routine versus clinically indicated replacement of peripheral
intravenous catheters: a randomized controlled equivalence trial: Lancet.
380:1066-1074
Stuart, R.L et al. (2013). Peripheral intravenous catheter–associated Staphylococcus
aureus bacteraemia: more than 5 years of prospective data from two tertiary
health services: Med J Aust. 198:551-553.
University of South Australia. (n. d.). Critical Appraisal Tools. Retrieved from
http://www.unisa.edu.au/Research/Sansom-Institute-for-Health-Research/
Research/Allied-Health-Evidence/Resources/CAT/#Randomised
Wallis, M.C. (2014). Risk factors for peripheral intravenous catheter failure: a
multivariate analysis of data from a randomized controlled trial: Infect Control
Hosp Epidemiol.35: 63-68.
13
Polit, D.F & Beck, C.T. (2016). Nursing Research: Generating and assessing evidence
for nursing practice. Lippincott Williams & Wilkins: New Delhi.
Queensland- Department of Health. (2015). Centre for Healthcare Related Infection
Surveillance and Prevention, Australia: PIVC guideline. Retrieved from
https://www.health.qld.gov.au/publications/clinical-practice/guidelines-
procedures/diseases-infection/governance/icare-pivc-guideline.pdf.
Rebelem. (2016). Should We Use Skin Glue to Secure Peripheral IVs: R.E.B.E.L. E.M.
Retrieved from http://rebelem.com/should-we-use-skin-glue-to-secure-peripheral-
ivs/
Rickard, C.M. (2012). Routine versus clinically indicated replacement of peripheral
intravenous catheters: a randomized controlled equivalence trial: Lancet.
380:1066-1074
Stuart, R.L et al. (2013). Peripheral intravenous catheter–associated Staphylococcus
aureus bacteraemia: more than 5 years of prospective data from two tertiary
health services: Med J Aust. 198:551-553.
University of South Australia. (n. d.). Critical Appraisal Tools. Retrieved from
http://www.unisa.edu.au/Research/Sansom-Institute-for-Health-Research/
Research/Allied-Health-Evidence/Resources/CAT/#Randomised
Wallis, M.C. (2014). Risk factors for peripheral intravenous catheter failure: a
multivariate analysis of data from a randomized controlled trial: Infect Control
Hosp Epidemiol.35: 63-68.
13
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





