Research Report: Social Engagement & Antipsychotic Use in LTCFs
VerifiedAdded on 2023/06/09
|9
|7533
|133
Report
AI Summary
This research report, published in the Canadian Journal of Nursing Research, investigates the association between social engagement (SE) and the use of antipsychotics in addressing behavioral and psychological symptoms of dementia (BPSD) in newly admitted residents to long-term care facilities (LTCFs). The cross-sectional study utilized administrative data from the Resident Assessment Instrument Minimum Data Set (RAI-MDS) collected between 2008 and 2011 in the Fraser Health region, British Columbia, Canada. The study included 2,639 residents aged 65 or older diagnosed with Alzheimer’s disease or other dementias. Multivariate logistic regression analyses were conducted to predict antipsychotic use based on SE. Results showed that SE was a statistically significant predictor of antipsychotic use when controlling for sociodemographic variables, but this association disappeared when controlling for health variables. The report concludes that the relationship between SE and antipsychotic use is complex and warrants further research. The study highlights the need for alternative approaches to manage BPSD and improve the quality of life for residents in LTCFs.
OriginalResearch Report
Social Engagement and Antipsychotic
Use in Addressing the Behavioral and
Psychological Symptoms of Dementia
in Long-Term Care Facilities
Nasrin Saleh1, Margaret Penning2, Denise Cloutier3,
Anastasia Mallidou1, Kim Nuernberger4, and Deanne Taylor5
Abstract
Objectives: The use of antipsychotics,mainly to address the behavioraland psychologicalsymptoms of dementia (BPSD),
remains a common and frequent practice in long-term care facilities (LTCFs) despite their associated risks.The objective of
this study was to explore the association between socialengagement (SE) and the use ofantipsychotics in addressing the
BPSD in newly admitted residents to LTCFs.
Methods:A cross-sectionalstudy was undertaken using administrative data,primarily the ResidentAssessmentInstrument
Minimum Data Set (Version 2.0) that collected between 2008 and 2011 (Fraser Health region, British Columbia
data analysis conducted on a sample of2,639 newly admitted residents aged 65 or older with a diagnosis ofAlzheimer’s
disease or other dementias as oftheir first fullor first quarterly assessment.Multivariate logistic regression analyses were
undertaken to predict antipsychotic use based on SE.
Results: SE was found to be a statistically significant predictor of antipsychotic use when controlling for sociod
variables (odds ratio (OR) ¼ .86, p < .0001, confidence interval (CI) [0.82, 0.90]). However, the association dis
controlling for health variables (OR ¼ .97,p ¼ .21,CI [0.97,1.0]).
Conclusion: The prediction of antipsychotic use in newly admitted residents to LTCFs by SE is complex. Furthe
warranted for further examination ofthe association ofantipsychotic use in newly admitted residents to LTCFs.
Keywords
long-term care facilities,residentialcare,socialengagement,antipsychotics
Background
Demand on long-term care facilities (LTCFs) in Canada
is increasing due to the rise of life expectancy and the
numberof personswith dementia.In 2011, 5 million
Canadianswere 65 years of age or older, which is
expected to double by the year 2036 (Canadian Nurses
Association,2013).Almost one million Canadians will
be living with dementia by the year 2036 compared to
450,000 in 2012 (Canadian Life and Health Insurance
Association,2012).This is presenting major challenges
to policy makers and the health-care system and requir-
ing a shift of priorities, adapting innovative approaches
to keep older adults healthy and independent.
1Schoolof Nursing,University ofVictoria,British Columbia,Canada
2Department ofSociology and Institute on Aging and Lifelong Health,
University ofVictoria,British Columbia,Canada
3Department ofGeography and Institute on Aging and Lifelong Health,
University ofVictoria,British Columbia,Canada
4British Columbia Trajectories in Care Project,University ofVictoria,
British Columbia,Canada
5Research and Knowledge Translation,Interior Health Authority,Research
Affiliate,Fraser Health Authority,British Columbia,Canada
Corresponding Author:
Nasrin Saleh,Schoolof Nursing,University ofVictoria,2833 Dufferin
Avenue,Victoria,British Columbia,Canada V8R 3L6.
Email:nasrin@uvic.ca
Canadian Journal of Nursing Research
0(0):1–9
! The Author(s) 2017
Reprints and permissions:
sagepub.com/journalsPermissions.nav
DOI: 10.1177/0844562117726253
journals.sagepub.com/home/cjn
Social Engagement and Antipsychotic
Use in Addressing the Behavioral and
Psychological Symptoms of Dementia
in Long-Term Care Facilities
Nasrin Saleh1, Margaret Penning2, Denise Cloutier3,
Anastasia Mallidou1, Kim Nuernberger4, and Deanne Taylor5
Abstract
Objectives: The use of antipsychotics,mainly to address the behavioraland psychologicalsymptoms of dementia (BPSD),
remains a common and frequent practice in long-term care facilities (LTCFs) despite their associated risks.The objective of
this study was to explore the association between socialengagement (SE) and the use ofantipsychotics in addressing the
BPSD in newly admitted residents to LTCFs.
Methods:A cross-sectionalstudy was undertaken using administrative data,primarily the ResidentAssessmentInstrument
Minimum Data Set (Version 2.0) that collected between 2008 and 2011 (Fraser Health region, British Columbia
data analysis conducted on a sample of2,639 newly admitted residents aged 65 or older with a diagnosis ofAlzheimer’s
disease or other dementias as oftheir first fullor first quarterly assessment.Multivariate logistic regression analyses were
undertaken to predict antipsychotic use based on SE.
Results: SE was found to be a statistically significant predictor of antipsychotic use when controlling for sociod
variables (odds ratio (OR) ¼ .86, p < .0001, confidence interval (CI) [0.82, 0.90]). However, the association dis
controlling for health variables (OR ¼ .97,p ¼ .21,CI [0.97,1.0]).
Conclusion: The prediction of antipsychotic use in newly admitted residents to LTCFs by SE is complex. Furthe
warranted for further examination ofthe association ofantipsychotic use in newly admitted residents to LTCFs.
Keywords
long-term care facilities,residentialcare,socialengagement,antipsychotics
Background
Demand on long-term care facilities (LTCFs) in Canada
is increasing due to the rise of life expectancy and the
numberof personswith dementia.In 2011, 5 million
Canadianswere 65 years of age or older, which is
expected to double by the year 2036 (Canadian Nurses
Association,2013).Almost one million Canadians will
be living with dementia by the year 2036 compared to
450,000 in 2012 (Canadian Life and Health Insurance
Association,2012).This is presenting major challenges
to policy makers and the health-care system and requir-
ing a shift of priorities, adapting innovative approaches
to keep older adults healthy and independent.
1Schoolof Nursing,University ofVictoria,British Columbia,Canada
2Department ofSociology and Institute on Aging and Lifelong Health,
University ofVictoria,British Columbia,Canada
3Department ofGeography and Institute on Aging and Lifelong Health,
University ofVictoria,British Columbia,Canada
4British Columbia Trajectories in Care Project,University ofVictoria,
British Columbia,Canada
5Research and Knowledge Translation,Interior Health Authority,Research
Affiliate,Fraser Health Authority,British Columbia,Canada
Corresponding Author:
Nasrin Saleh,Schoolof Nursing,University ofVictoria,2833 Dufferin
Avenue,Victoria,British Columbia,Canada V8R 3L6.
Email:nasrin@uvic.ca
Canadian Journal of Nursing Research
0(0):1–9
! The Author(s) 2017
Reprints and permissions:
sagepub.com/journalsPermissions.nav
DOI: 10.1177/0844562117726253
journals.sagepub.com/home/cjn
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Since the early 1990s,LTCFs have moved from a
medicalmodelfocusing on treatmenttoward a social
modelof care emphasizing a home-like environment.
Moreover, the culturechangemovementin LTCFs,
based on the philosophy of person-centered care, focuses
on well-being and quality of life as defined by the resi-
dent.However,the prevalence ofantipsychotic use in
LTCFs remains high (Fischer, Cohen, Forrest,
Schweizer,& Wasylenki,2011),mainly to address the
behavioraland psychologicalsymptomsof dementia
(BPSD) that include aggression,agitation,restlessness,
wandering,hoarding, sleep disturbances,psychosis,
delusions, hallucinations, and sundowning
(Cohen-Mansfield, Marx, & Rosenthal, 1989).
Recently,British Columbia (BC) Ministry of Health
reviewed antipsychotic use in LTCFs and recommended
its use for the treatment of BPSD under severalcondi-
tions (MoH, 2011).These conditions include weighing
the risks againstthe benefits,using those drugsas a
last resort,obtaining informed consentprior to use,
and following the clinical guidelinesof a low dose,
slow titration, and over a short period with close moni-
toring. Yet, the review illustrated that over half (50.3%)
of the residents were prescribed antipsychotics between
April 2010 and June 2011,an increase of 37% within a
decade(MoH, 2011),with similar increasesreported
across Canadian health authorities. While newly
admitted residents are more likely than other residents
to be prescribed at least one antipsychotic during the first
90 days of admission (Huybrechts,Rothman,Silliman,
Brookhart,& Schneeweiss, 2011), antipsychotic use can
be as twice ashigh in residentswith BPSD (Alanen,
Finne-Soveri,Noro, & Leinonen,2006).Antipsychotic
use in older adults,particularly with dementia,is asso-
ciated with multipleside effects(Perucca & Gilliam,
2012)such as increased risksof mortality,falls, and
hip fractures.Furthermore,antipsychotics may worsen
cognition and increase sedative load (Perucca & Gilliam,
2012) that, in turn, may reduce the level of social engage-
ment (SE).
SE is considered essentialto the psychologicaland
physicalwell-being (Bennett,2002)of older adultsin
LTCFs due to challenges within the setting in keeping
older adults active and stimulated.Scholars have pro-
posed that SE might be an alternative to antipsychotics
use (Mallidou, Oliveira, & Borycki, 2013). Socially enga-
ging residents has positive health outcomes,such as a
protectiveeffecton mortality (Bennett,2002;Kiely,
Simon,Jones,& Morris, 2000),and improved function
and cognition (Chen et al.,2013).SE is also associated
with decreased symptomsof depression (Lou,Chi,
Kwan, & Leung, 2013) and is an indicator of quality of
life, as it relates to positive emotions,sense of purpose,
and life satisfaction.Conversely,lonely older adults
often have low self-rated health and low life satisfaction.
Design and Method
Design and Sample
This is a cross-sectional study using administrative data.
Data from the Resident Assessment Instrument Minimum
Data Set (RAI-MDS, Version 2.0) and the Continuing
Care Information ManagementSystem were collected
between 2008 and 2011 in the FraserHealth region,
BC, Canada (accessiblepopulation).Fraser Health
operates 7,800 residentialcare beds and has systematic-
ally collected RAI-MDS data on residents since 2007.
The RAI-MDS has been rigorously tested for reliability
and validity in Canada and internationally (Hawes et al.,
1995;Lawton etal., 1998;Mor et al., 2003),enabling
comparison between countries and institutions.Trained
clinicians complete the MDS 2.0 upon residentadmis-
sion and ideally every 3 monthsthereafter.It also is
completed ifchangesin health statusare experienced
by residents.In this study,all measureswere drawn
from assessments undertaken 90 days following admis-
sion to LTCFs.
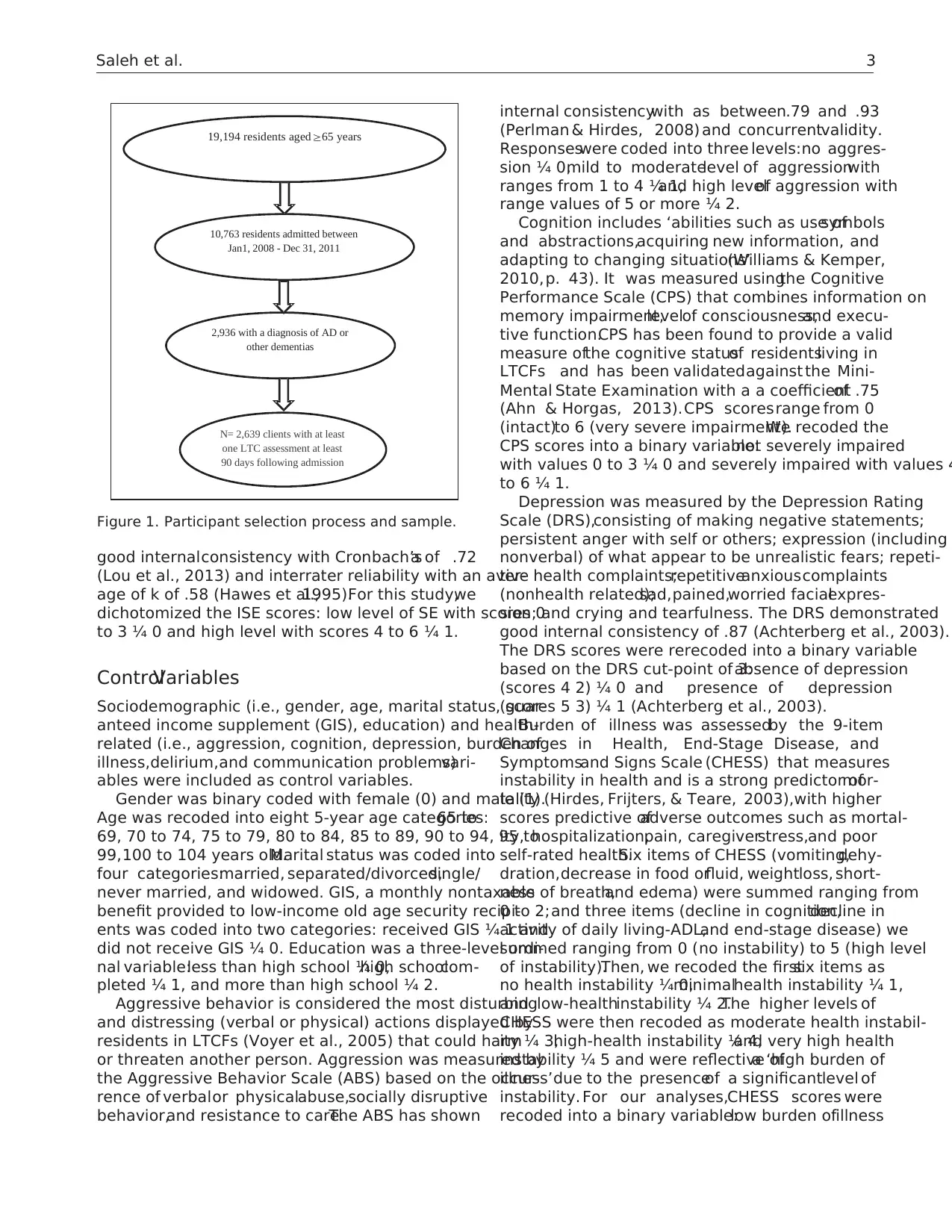
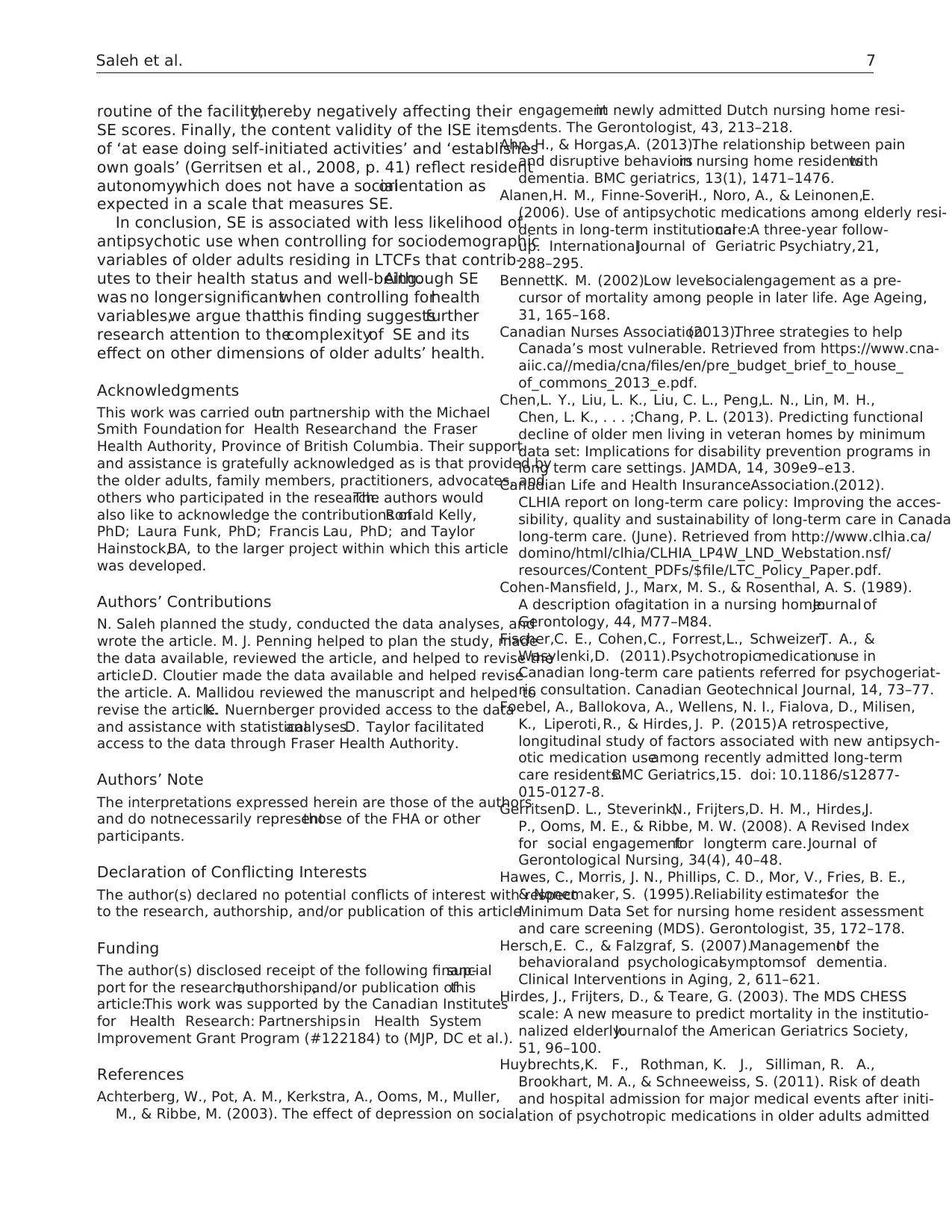
Our initial sample included 10,763 newly admitted
residents(from January 1, 2008, to December31,
2011), aged 65 or older. The final study sample included
2,639 residents who upon admission or in their first full
or quarterly assessment had a diagnosis of dementia and
who had at least one LTC assessment within 90 days of
admission (Figure 1).
Dependent Variable
The dependent variable is antipsychotic use,which was
defined as the use of atypicaland typicalantipsychotic
agent(s).It was coded into a binary variable:did not
receive antipsychotic drugs ¼ 0 and received antipsychotics
(one drug atleastonce,regardless ofthe numbers of
drugs or days the drug is received)in the past7 days
prior to the assessment date ¼ 1.
Independent Variable
The independentvariablewas SE, which within the
contextof LTCFs, was defined as those who have ‘a
high sense of initiative and involvement and can respond
adequately to socialstimuliin the socialenvironment,
participate in socialactivitiesand interactwith other
residents and staff’ (Achterberg et al.,2003, p. 213). SE
was measured using the Index ofSocial Engagement
(ISE), an observationalscale that measures the positive
social behavior of residents. It includes six dichotomous
items reflecting whether the resident is at ease interacting
with others, with planned or structured activities, doing
self-initiatedactivities,establishingtheir own goals,
pursuing involvement in facility life, and accepting invi-
tations into most group activities.The ISE has shown
2 Canadian Journalof Nursing Research 0(0)
medicalmodelfocusing on treatmenttoward a social
modelof care emphasizing a home-like environment.
Moreover, the culturechangemovementin LTCFs,
based on the philosophy of person-centered care, focuses
on well-being and quality of life as defined by the resi-
dent.However,the prevalence ofantipsychotic use in
LTCFs remains high (Fischer, Cohen, Forrest,
Schweizer,& Wasylenki,2011),mainly to address the
behavioraland psychologicalsymptomsof dementia
(BPSD) that include aggression,agitation,restlessness,
wandering,hoarding, sleep disturbances,psychosis,
delusions, hallucinations, and sundowning
(Cohen-Mansfield, Marx, & Rosenthal, 1989).
Recently,British Columbia (BC) Ministry of Health
reviewed antipsychotic use in LTCFs and recommended
its use for the treatment of BPSD under severalcondi-
tions (MoH, 2011).These conditions include weighing
the risks againstthe benefits,using those drugsas a
last resort,obtaining informed consentprior to use,
and following the clinical guidelinesof a low dose,
slow titration, and over a short period with close moni-
toring. Yet, the review illustrated that over half (50.3%)
of the residents were prescribed antipsychotics between
April 2010 and June 2011,an increase of 37% within a
decade(MoH, 2011),with similar increasesreported
across Canadian health authorities. While newly
admitted residents are more likely than other residents
to be prescribed at least one antipsychotic during the first
90 days of admission (Huybrechts,Rothman,Silliman,
Brookhart,& Schneeweiss, 2011), antipsychotic use can
be as twice ashigh in residentswith BPSD (Alanen,
Finne-Soveri,Noro, & Leinonen,2006).Antipsychotic
use in older adults,particularly with dementia,is asso-
ciated with multipleside effects(Perucca & Gilliam,
2012)such as increased risksof mortality,falls, and
hip fractures.Furthermore,antipsychotics may worsen
cognition and increase sedative load (Perucca & Gilliam,
2012) that, in turn, may reduce the level of social engage-
ment (SE).
SE is considered essentialto the psychologicaland
physicalwell-being (Bennett,2002)of older adultsin
LTCFs due to challenges within the setting in keeping
older adults active and stimulated.Scholars have pro-
posed that SE might be an alternative to antipsychotics
use (Mallidou, Oliveira, & Borycki, 2013). Socially enga-
ging residents has positive health outcomes,such as a
protectiveeffecton mortality (Bennett,2002;Kiely,
Simon,Jones,& Morris, 2000),and improved function
and cognition (Chen et al.,2013).SE is also associated
with decreased symptomsof depression (Lou,Chi,
Kwan, & Leung, 2013) and is an indicator of quality of
life, as it relates to positive emotions,sense of purpose,
and life satisfaction.Conversely,lonely older adults
often have low self-rated health and low life satisfaction.
Design and Method
Design and Sample
This is a cross-sectional study using administrative data.
Data from the Resident Assessment Instrument Minimum
Data Set (RAI-MDS, Version 2.0) and the Continuing
Care Information ManagementSystem were collected
between 2008 and 2011 in the FraserHealth region,
BC, Canada (accessiblepopulation).Fraser Health
operates 7,800 residentialcare beds and has systematic-
ally collected RAI-MDS data on residents since 2007.
The RAI-MDS has been rigorously tested for reliability
and validity in Canada and internationally (Hawes et al.,
1995;Lawton etal., 1998;Mor et al., 2003),enabling
comparison between countries and institutions.Trained
clinicians complete the MDS 2.0 upon residentadmis-
sion and ideally every 3 monthsthereafter.It also is
completed ifchangesin health statusare experienced
by residents.In this study,all measureswere drawn
from assessments undertaken 90 days following admis-
sion to LTCFs.
Our initial sample included 10,763 newly admitted
residents(from January 1, 2008, to December31,
2011), aged 65 or older. The final study sample included
2,639 residents who upon admission or in their first full
or quarterly assessment had a diagnosis of dementia and
who had at least one LTC assessment within 90 days of
admission (Figure 1).
Dependent Variable
The dependent variable is antipsychotic use,which was
defined as the use of atypicaland typicalantipsychotic
agent(s).It was coded into a binary variable:did not
receive antipsychotic drugs ¼ 0 and received antipsychotics
(one drug atleastonce,regardless ofthe numbers of
drugs or days the drug is received)in the past7 days
prior to the assessment date ¼ 1.
Independent Variable
The independentvariablewas SE, which within the
contextof LTCFs, was defined as those who have ‘a
high sense of initiative and involvement and can respond
adequately to socialstimuliin the socialenvironment,
participate in socialactivitiesand interactwith other
residents and staff’ (Achterberg et al.,2003, p. 213). SE
was measured using the Index ofSocial Engagement
(ISE), an observationalscale that measures the positive
social behavior of residents. It includes six dichotomous
items reflecting whether the resident is at ease interacting
with others, with planned or structured activities, doing
self-initiatedactivities,establishingtheir own goals,
pursuing involvement in facility life, and accepting invi-
tations into most group activities.The ISE has shown
2 Canadian Journalof Nursing Research 0(0)
good internalconsistency with Cronbach’sa of .72
(Lou et al., 2013) and interrater reliability with an aver-
age of k of .58 (Hawes et al.,1995).For this study,we
dichotomized the ISE scores: low level of SE with scores 0
to 3 ¼ 0 and high level with scores 4 to 6 ¼ 1.
ControlVariables
Sociodemographic (i.e., gender, age, marital status, guar-
anteed income supplement (GIS), education) and health-
related (i.e., aggression, cognition, depression, burden of
illness,delirium,and communication problems)vari-
ables were included as control variables.
Gender was binary coded with female (0) and male (1).
Age was recoded into eight 5-year age categories:65 to
69, 70 to 74, 75 to 79, 80 to 84, 85 to 89, 90 to 94, 95 to
99,100 to 104 years old.Marital status was coded into
four categories:married, separated/divorced,single/
never married, and widowed. GIS, a monthly nontaxable
benefit provided to low-income old age security recipi-
ents was coded into two categories: received GIS ¼ 1 and
did not receive GIS ¼ 0. Education was a three-level ordi-
nal variable:less than high school ¼ 0,high schoolcom-
pleted ¼ 1, and more than high school ¼ 2.
Aggressive behavior is considered the most disturbing
and distressing (verbal or physical) actions displayed by
residents in LTCFs (Voyer et al., 2005) that could harm
or threaten another person. Aggression was measured by
the Aggressive Behavior Scale (ABS) based on the occur-
rence of verbalor physicalabuse,socially disruptive
behavior,and resistance to care.The ABS has shown
internal consistencywith as between.79 and .93
(Perlman & Hirdes, 2008) and concurrentvalidity.
Responseswere coded into three levels:no aggres-
sion ¼ 0,mild to moderatelevel of aggressionwith
ranges from 1 to 4 ¼ 1,and high levelof aggression with
range values of 5 or more ¼ 2.
Cognition includes ‘abilities such as use ofsymbols
and abstractions,acquiring new information, and
adapting to changing situations’(Williams & Kemper,
2010,p. 43). It was measured usingthe Cognitive
Performance Scale (CPS) that combines information on
memory impairment,levelof consciousness,and execu-
tive function.CPS has been found to provide a valid
measure ofthe cognitive statusof residentsliving in
LTCFs and has been validatedagainst the Mini-
Mental State Examination with a a coefficientof .75
(Ahn & Horgas, 2013).CPS scoresrange from 0
(intact)to 6 (very severe impairment).We recoded the
CPS scores into a binary variable:not severely impaired
with values 0 to 3 ¼ 0 and severely impaired with values 4
to 6 ¼ 1.
Depression was measured by the Depression Rating
Scale (DRS),consisting of making negative statements;
persistent anger with self or others; expression (including
nonverbal) of what appear to be unrealistic fears; repeti-
tive health complaints;repetitiveanxiouscomplaints
(nonhealth related);sad,pained,worried facialexpres-
sion; and crying and tearfulness. The DRS demonstrated
good internal consistency of .87 (Achterberg et al., 2003).
The DRS scores were rerecoded into a binary variable
based on the DRS cut-point of 3:absence of depression
(scores 4 2) ¼ 0 and presence of depression
(scores 5 3) ¼ 1 (Achterberg et al., 2003).
Burden of illness was assessedby the 9-item
Changes in Health, End-Stage Disease, and
Symptomsand Signs Scale (CHESS) that measures
instability in health and is a strong predictor ofmor-
tality (Hirdes, Frijters, & Teare, 2003),with higher
scores predictive ofadverse outcomes such as mortal-
ity, hospitalization,pain, caregiverstress,and poor
self-rated health.Six items of CHESS (vomiting,dehy-
dration,decrease in food orfluid, weightloss, short-
ness of breath,and edema) were summed ranging from
0 to 2;and three items (decline in cognition,decline in
activity of daily living-ADL,and end-stage disease) we
summed ranging from 0 (no instability) to 5 (high level
of instability).Then, we recoded the firstsix items as
no health instability ¼ 0,minimalhealth instability ¼ 1,
and low-healthinstability ¼ 2.The higher levels of
CHESS were then recoded as moderate health instabil-
ity ¼ 3,high-health instability ¼ 4,and very high health
instability ¼ 5 and were reflective ofa ‘high burden of
illness’due to the presenceof a significantlevel of
instability. For our analyses,CHESS scores were
recoded into a binary variable:low burden ofillness
19,194 residents aged ≥65 years
10,763 residents admitted between
Jan1, 2008 - Dec 31, 2011
2,936 with a diagnosis of AD or
other dementias
N= 2,639 clients with at least
one LTC assessment at least
90 days following admission
Figure 1. Participant selection process and sample.
Saleh et al. 3
(Lou et al., 2013) and interrater reliability with an aver-
age of k of .58 (Hawes et al.,1995).For this study,we
dichotomized the ISE scores: low level of SE with scores 0
to 3 ¼ 0 and high level with scores 4 to 6 ¼ 1.
ControlVariables
Sociodemographic (i.e., gender, age, marital status, guar-
anteed income supplement (GIS), education) and health-
related (i.e., aggression, cognition, depression, burden of
illness,delirium,and communication problems)vari-
ables were included as control variables.
Gender was binary coded with female (0) and male (1).
Age was recoded into eight 5-year age categories:65 to
69, 70 to 74, 75 to 79, 80 to 84, 85 to 89, 90 to 94, 95 to
99,100 to 104 years old.Marital status was coded into
four categories:married, separated/divorced,single/
never married, and widowed. GIS, a monthly nontaxable
benefit provided to low-income old age security recipi-
ents was coded into two categories: received GIS ¼ 1 and
did not receive GIS ¼ 0. Education was a three-level ordi-
nal variable:less than high school ¼ 0,high schoolcom-
pleted ¼ 1, and more than high school ¼ 2.
Aggressive behavior is considered the most disturbing
and distressing (verbal or physical) actions displayed by
residents in LTCFs (Voyer et al., 2005) that could harm
or threaten another person. Aggression was measured by
the Aggressive Behavior Scale (ABS) based on the occur-
rence of verbalor physicalabuse,socially disruptive
behavior,and resistance to care.The ABS has shown
internal consistencywith as between.79 and .93
(Perlman & Hirdes, 2008) and concurrentvalidity.
Responseswere coded into three levels:no aggres-
sion ¼ 0,mild to moderatelevel of aggressionwith
ranges from 1 to 4 ¼ 1,and high levelof aggression with
range values of 5 or more ¼ 2.
Cognition includes ‘abilities such as use ofsymbols
and abstractions,acquiring new information, and
adapting to changing situations’(Williams & Kemper,
2010,p. 43). It was measured usingthe Cognitive
Performance Scale (CPS) that combines information on
memory impairment,levelof consciousness,and execu-
tive function.CPS has been found to provide a valid
measure ofthe cognitive statusof residentsliving in
LTCFs and has been validatedagainst the Mini-
Mental State Examination with a a coefficientof .75
(Ahn & Horgas, 2013).CPS scoresrange from 0
(intact)to 6 (very severe impairment).We recoded the
CPS scores into a binary variable:not severely impaired
with values 0 to 3 ¼ 0 and severely impaired with values 4
to 6 ¼ 1.
Depression was measured by the Depression Rating
Scale (DRS),consisting of making negative statements;
persistent anger with self or others; expression (including
nonverbal) of what appear to be unrealistic fears; repeti-
tive health complaints;repetitiveanxiouscomplaints
(nonhealth related);sad,pained,worried facialexpres-
sion; and crying and tearfulness. The DRS demonstrated
good internal consistency of .87 (Achterberg et al., 2003).
The DRS scores were rerecoded into a binary variable
based on the DRS cut-point of 3:absence of depression
(scores 4 2) ¼ 0 and presence of depression
(scores 5 3) ¼ 1 (Achterberg et al., 2003).
Burden of illness was assessedby the 9-item
Changes in Health, End-Stage Disease, and
Symptomsand Signs Scale (CHESS) that measures
instability in health and is a strong predictor ofmor-
tality (Hirdes, Frijters, & Teare, 2003),with higher
scores predictive ofadverse outcomes such as mortal-
ity, hospitalization,pain, caregiverstress,and poor
self-rated health.Six items of CHESS (vomiting,dehy-
dration,decrease in food orfluid, weightloss, short-
ness of breath,and edema) were summed ranging from
0 to 2;and three items (decline in cognition,decline in
activity of daily living-ADL,and end-stage disease) we
summed ranging from 0 (no instability) to 5 (high level
of instability).Then, we recoded the firstsix items as
no health instability ¼ 0,minimalhealth instability ¼ 1,
and low-healthinstability ¼ 2.The higher levels of
CHESS were then recoded as moderate health instabil-
ity ¼ 3,high-health instability ¼ 4,and very high health
instability ¼ 5 and were reflective ofa ‘high burden of
illness’due to the presenceof a significantlevel of
instability. For our analyses,CHESS scores were
recoded into a binary variable:low burden ofillness
19,194 residents aged ≥65 years
10,763 residents admitted between
Jan1, 2008 - Dec 31, 2011
2,936 with a diagnosis of AD or
other dementias
N= 2,639 clients with at least
one LTC assessment at least
90 days following admission
Figure 1. Participant selection process and sample.
Saleh et al. 3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

in which we combined the scores of 0 to 2 and recoded
as 0 and high burdenof illnesswhich a combined
scores of3 to 5 that were recoded to 1.
Data were selected thatassessed six delirium symp-
toms: easily distracted, periods of altered perception, dis-
organized speech,periodsof restlessness,periodsof
lethargy,and mental function that varies over the
course of the day. Each symptom was scored as not pre-
sent ¼ 0,present but not of recent onset ¼ 1,and present
that appears different from usuallevelof functioning ¼ 2.
Then,following Voyer and colleagues (2008),we coded
the absence of delirium symptoms as 0) and we combined
the scores of1 and 2 and gave ita score of1, which
indicates positive presence of delirium.
Communication problemsweremeasured by three
items: making oneself understood (1 ¼ sometimes
understood; 2 ¼ rarely or never understood), speech clarity
(1 ¼ unclear speech; 2 ¼ no speech), and ability to under-
stand others (1 ¼ sometimes understand; 2 ¼ rarely or never
understands). The scores were summed into single scores,
ranging from 0 to 3, with a higher score reflecting greater
difficulty communicating with and understanding others.
Data Analysis
Data were analyzed using SAS (9.2). Descriptive analysis
was completed and included cross-tabulation evaluated
with Wald 2. Variablesmeeting minimalsignificance
(p < .25)were included in the multivariateanalysis.
Covariateswere removed from the modelif they are
nonsignificantand not a confounder. Therefore,
models contained only significant covariatesand
confounders. The criterion to establish statistical signifi-
cance for the multivariate analysis was an a of .05.We
conducted logistic regression in a series of three nested
models exploring the effect of SE on antipsychotic use.
We first entered the variable SE followed by the socio-
demographic characteristics,and finally,health-related
variables.
Results
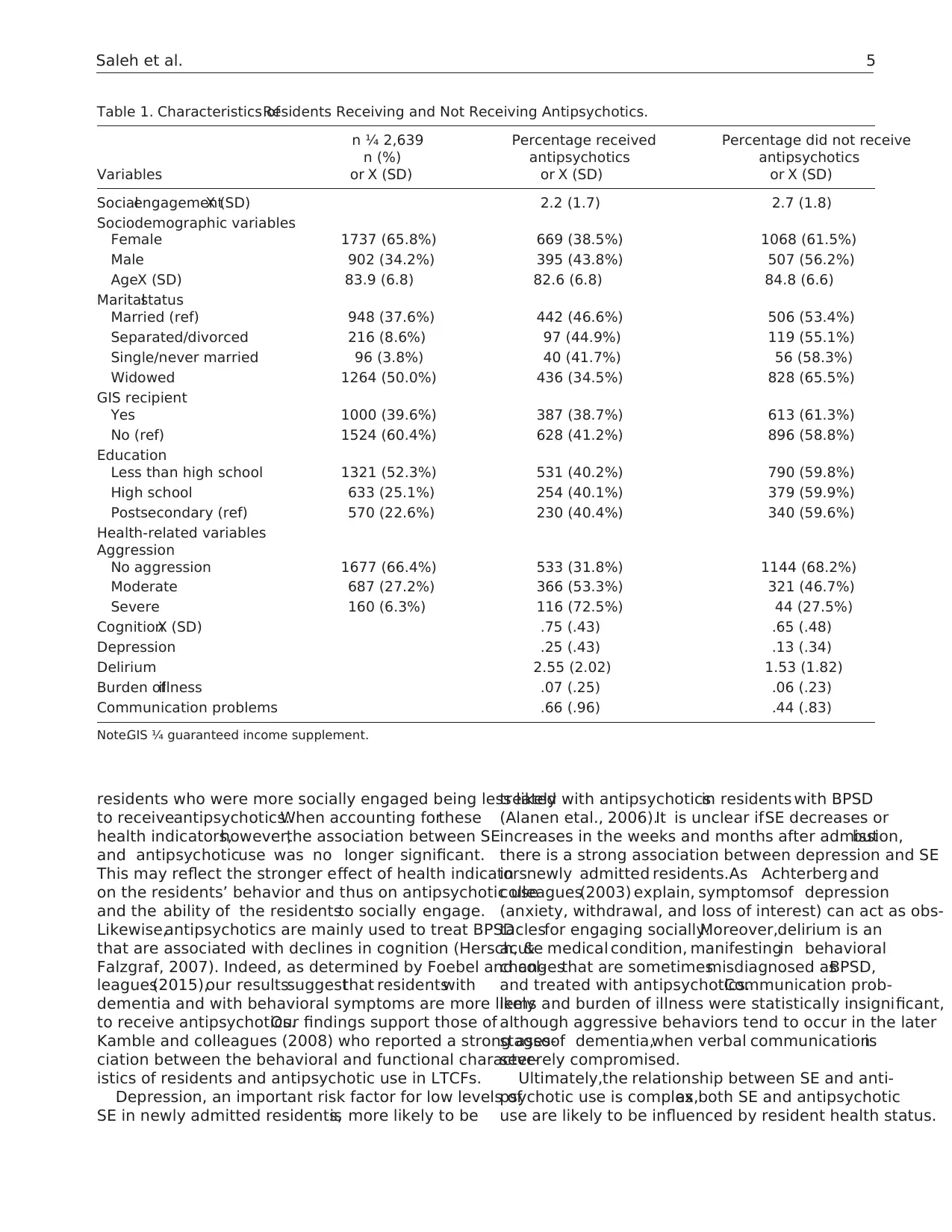
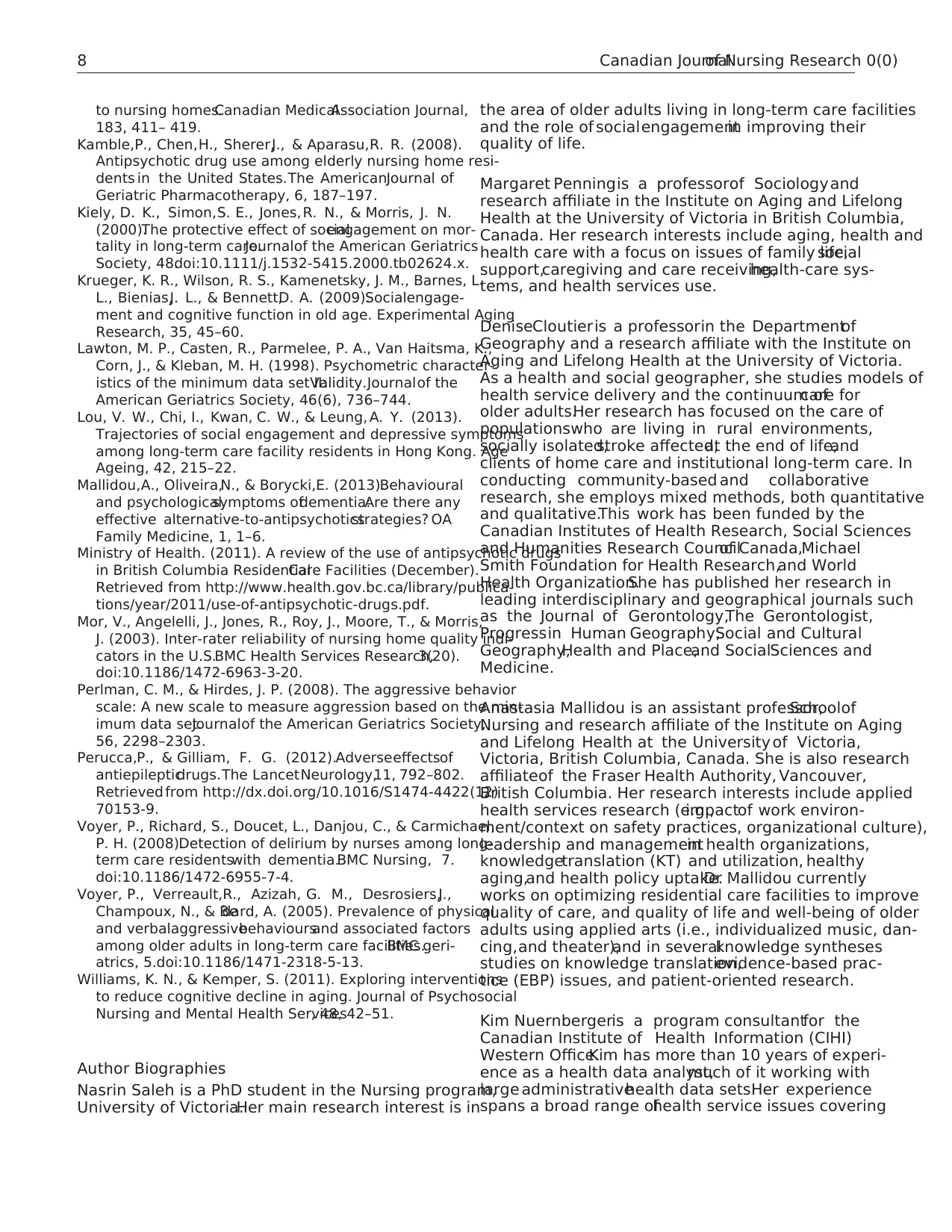
The average age of the study participants was just under
84 years (Table 1).Half of the sample was widowed,
60.4% received GIS,and 52.3% had less than a high
schooleducation.Antipsychoticsreceiverswere males
(43.8%),younger (mean age ¼ 82.6 years),and married
(46.6%),GIS no-recipients(41.2%)and were mildly
aggressive(53.3%) or severelyaggressiveresidents
(72.5%). An interesting finding is that 31.8% of residents
who had no aggressive behavior received antipsychotics,
while 27.5% of participantswith severeaggressive
behaviordid not receive antipsychotics.Furthermore,
residentswho receivedantipsychoticshad a lower
mean level of SE ( X ¼ 2.2,SD ¼ 1.7),experienced
cognitiveissues(.75, SD ¼ .43),depression (X ¼ .25,
SD ¼ .43),delirium (X ¼ 2.55,SD ¼ 2.02),burden of ill-
ness (X ¼ .07,SD ¼ .25),and communication problems
(X ¼ .66, SD ¼ .96).
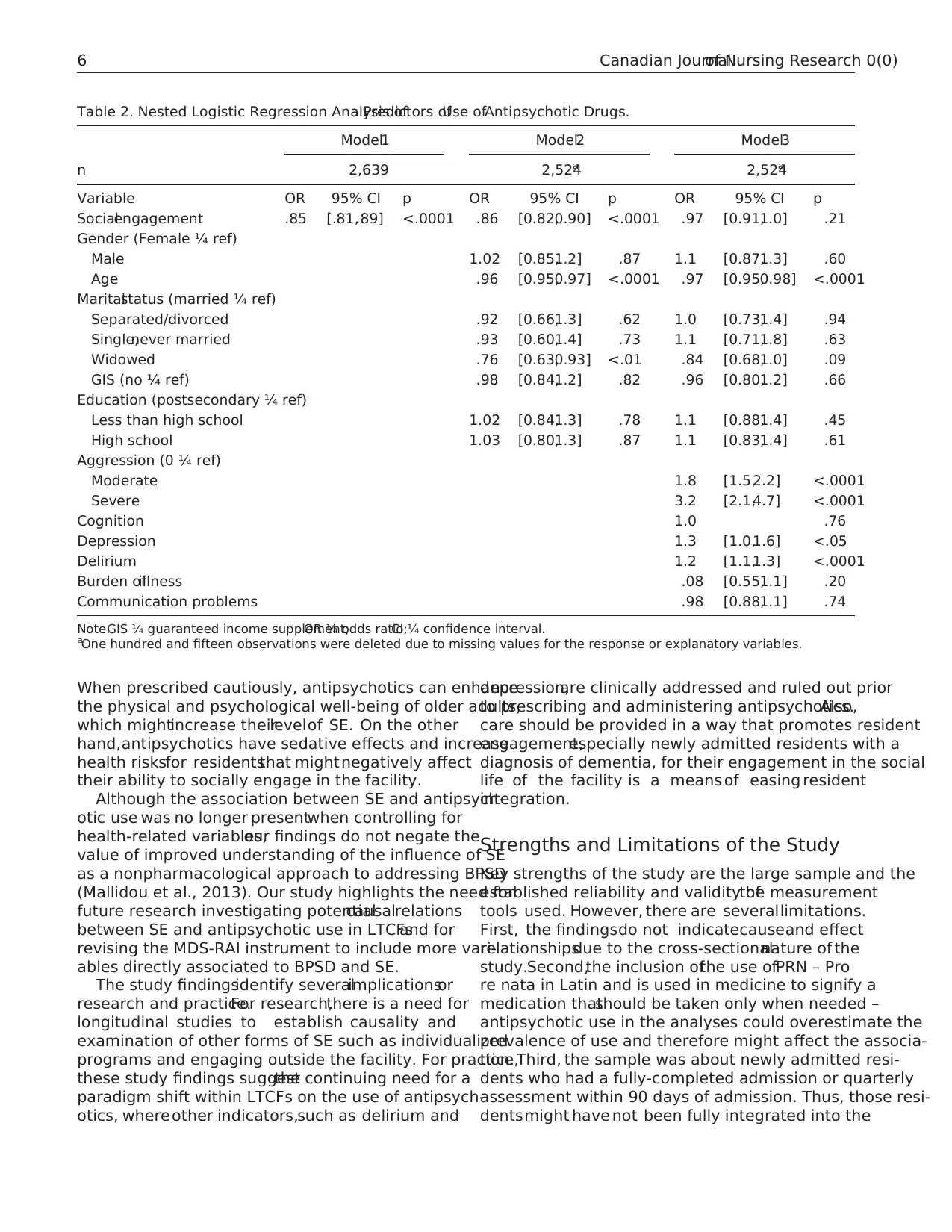
We used logistic regression analyses to predict anti-
psychotic use based on the SE level while we controlled
for sociodemographic-and health-relatedvariables
(Table 2). In both Model 1 and Model 2, a greater
levelof engagementwas associated with a lower level
of antipsychotic use (odds ratio (OR) ¼ .85,p < .0001,
confidenceinterval(CI) [0.81,0.89])and (OR ¼ .86,
p < .0001, CI [0.82, 0.90]), respectively. In addition, find-
ings showed that older age (OR ¼ .96, p < .0001, CI [0.95,
0.97])and widowhood rather than married (OR ¼ .76,
p < .01,CI [0.63,0.93])were associated with lower
likelihood of antipsychotic use.
In Model 3, controlling for both sociodemographic-
and health-related indicators,SE and widowhood were
no longer significantly associated with antipsychotics use
(OR ¼ .97, p ¼ .21, CI [0.91, 1.0]) and (OR ¼ .84, p ¼ .09,
CI [0.68,1.0]),respectively.However,age (OR ¼ .97,
p < .0001, CI [0.95, 0.98]) and several health status indi-
cators remained statisticallysignificant predictors.
Notably, residents with moderate or severe aggressive
behavior were 1.8 times and 3.2 times more likely to
receive antipsychotics (OR ¼ 1.8,p < .0001,CI [1.5,2.2]
and OR ¼ 3.2,p < .0001,CI [2.1, 4.7]), respectively.
Furthermore,residentsdiagnosed with depression or
delirium were 1.3 times (OR ¼ 1.3, p < .05, CI [1.0, 1.6])
or 1.2 times(OR ¼ 1.2,p < .0001,CI [1.1,1.3])more
likely to receive antipsychotics, respectively.
Discussion
The aim of this study wasto explore the association
between SE and antipsychotic use in addressing BPSD
in residentsnewly admitted to LTCFs.Severalnote-
worthy factors were associated with antipsychotic use.
Consistentwith otherstudies,females(65.8% in our
sample)live longer than males and are more likely to
receive LTC services.Also, consistent with the study of
Kamble etal. (2008),the likelihood ofreceiving anti-
psychoticswas lower for femalethan maleresidents
(38.5% vs.43.8%);and as Krueger et al.(2009) found,
the percentageof residentsreceivingantipsychotics
decreased with age (the lowest percentage of those receiv-
ing antipsychotics aged 585). However, gender was not
statistically significant when controlling for other socio-
demographicfactors and health-relatedvariables.
Conversely,age remained statistically significantwhen
controlling for both sociodemographiccharacteristics
and health indicators.
Prior to the introduction of controls for factors such as
aggression,depression,and delirium,SE was found to
have an inverse association with antipsychotic use, with
4 Canadian Journalof Nursing Research 0(0)
as 0 and high burdenof illnesswhich a combined
scores of3 to 5 that were recoded to 1.
Data were selected thatassessed six delirium symp-
toms: easily distracted, periods of altered perception, dis-
organized speech,periodsof restlessness,periodsof
lethargy,and mental function that varies over the
course of the day. Each symptom was scored as not pre-
sent ¼ 0,present but not of recent onset ¼ 1,and present
that appears different from usuallevelof functioning ¼ 2.
Then,following Voyer and colleagues (2008),we coded
the absence of delirium symptoms as 0) and we combined
the scores of1 and 2 and gave ita score of1, which
indicates positive presence of delirium.
Communication problemsweremeasured by three
items: making oneself understood (1 ¼ sometimes
understood; 2 ¼ rarely or never understood), speech clarity
(1 ¼ unclear speech; 2 ¼ no speech), and ability to under-
stand others (1 ¼ sometimes understand; 2 ¼ rarely or never
understands). The scores were summed into single scores,
ranging from 0 to 3, with a higher score reflecting greater
difficulty communicating with and understanding others.
Data Analysis
Data were analyzed using SAS (9.2). Descriptive analysis
was completed and included cross-tabulation evaluated
with Wald 2. Variablesmeeting minimalsignificance
(p < .25)were included in the multivariateanalysis.
Covariateswere removed from the modelif they are
nonsignificantand not a confounder. Therefore,
models contained only significant covariatesand
confounders. The criterion to establish statistical signifi-
cance for the multivariate analysis was an a of .05.We
conducted logistic regression in a series of three nested
models exploring the effect of SE on antipsychotic use.
We first entered the variable SE followed by the socio-
demographic characteristics,and finally,health-related
variables.
Results
The average age of the study participants was just under
84 years (Table 1).Half of the sample was widowed,
60.4% received GIS,and 52.3% had less than a high
schooleducation.Antipsychoticsreceiverswere males
(43.8%),younger (mean age ¼ 82.6 years),and married
(46.6%),GIS no-recipients(41.2%)and were mildly
aggressive(53.3%) or severelyaggressiveresidents
(72.5%). An interesting finding is that 31.8% of residents
who had no aggressive behavior received antipsychotics,
while 27.5% of participantswith severeaggressive
behaviordid not receive antipsychotics.Furthermore,
residentswho receivedantipsychoticshad a lower
mean level of SE ( X ¼ 2.2,SD ¼ 1.7),experienced
cognitiveissues(.75, SD ¼ .43),depression (X ¼ .25,
SD ¼ .43),delirium (X ¼ 2.55,SD ¼ 2.02),burden of ill-
ness (X ¼ .07,SD ¼ .25),and communication problems
(X ¼ .66, SD ¼ .96).
We used logistic regression analyses to predict anti-
psychotic use based on the SE level while we controlled
for sociodemographic-and health-relatedvariables
(Table 2). In both Model 1 and Model 2, a greater
levelof engagementwas associated with a lower level
of antipsychotic use (odds ratio (OR) ¼ .85,p < .0001,
confidenceinterval(CI) [0.81,0.89])and (OR ¼ .86,
p < .0001, CI [0.82, 0.90]), respectively. In addition, find-
ings showed that older age (OR ¼ .96, p < .0001, CI [0.95,
0.97])and widowhood rather than married (OR ¼ .76,
p < .01,CI [0.63,0.93])were associated with lower
likelihood of antipsychotic use.
In Model 3, controlling for both sociodemographic-
and health-related indicators,SE and widowhood were
no longer significantly associated with antipsychotics use
(OR ¼ .97, p ¼ .21, CI [0.91, 1.0]) and (OR ¼ .84, p ¼ .09,
CI [0.68,1.0]),respectively.However,age (OR ¼ .97,
p < .0001, CI [0.95, 0.98]) and several health status indi-
cators remained statisticallysignificant predictors.
Notably, residents with moderate or severe aggressive
behavior were 1.8 times and 3.2 times more likely to
receive antipsychotics (OR ¼ 1.8,p < .0001,CI [1.5,2.2]
and OR ¼ 3.2,p < .0001,CI [2.1, 4.7]), respectively.
Furthermore,residentsdiagnosed with depression or
delirium were 1.3 times (OR ¼ 1.3, p < .05, CI [1.0, 1.6])
or 1.2 times(OR ¼ 1.2,p < .0001,CI [1.1,1.3])more
likely to receive antipsychotics, respectively.
Discussion
The aim of this study wasto explore the association
between SE and antipsychotic use in addressing BPSD
in residentsnewly admitted to LTCFs.Severalnote-
worthy factors were associated with antipsychotic use.
Consistentwith otherstudies,females(65.8% in our
sample)live longer than males and are more likely to
receive LTC services.Also, consistent with the study of
Kamble etal. (2008),the likelihood ofreceiving anti-
psychoticswas lower for femalethan maleresidents
(38.5% vs.43.8%);and as Krueger et al.(2009) found,
the percentageof residentsreceivingantipsychotics
decreased with age (the lowest percentage of those receiv-
ing antipsychotics aged 585). However, gender was not
statistically significant when controlling for other socio-
demographicfactors and health-relatedvariables.
Conversely,age remained statistically significantwhen
controlling for both sociodemographiccharacteristics
and health indicators.
Prior to the introduction of controls for factors such as
aggression,depression,and delirium,SE was found to
have an inverse association with antipsychotic use, with
4 Canadian Journalof Nursing Research 0(0)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
residents who were more socially engaged being less likely
to receiveantipsychotics.When accounting forthese
health indicators,however,the association between SE
and antipsychoticuse was no longer significant.
This may reflect the stronger effect of health indicators
on the residents’ behavior and thus on antipsychotic use
and the ability of the residentsto socially engage.
Likewise,antipsychotics are mainly used to treat BPSD
that are associated with declines in cognition (Hersch, &
Falzgraf, 2007). Indeed, as determined by Foebel and col-
leagues(2015),our resultssuggestthat residentswith
dementia and with behavioral symptoms are more likely
to receive antipsychotics.Our findings support those of
Kamble and colleagues (2008) who reported a strong asso-
ciation between the behavioral and functional character-
istics of residents and antipsychotic use in LTCFs.
Depression, an important risk factor for low levels of
SE in newly admitted residents,is more likely to be
treated with antipsychoticsin residents with BPSD
(Alanen etal., 2006).It is unclear ifSE decreases or
increases in the weeks and months after admission,but
there is a strong association between depression and SE
in newly admitted residents.As Achterberg and
colleagues(2003) explain, symptomsof depression
(anxiety, withdrawal, and loss of interest) can act as obs-
taclesfor engaging socially.Moreover,delirium is an
acute medical condition, manifestingin behavioral
changesthat are sometimesmisdiagnosed asBPSD,
and treated with antipsychotics.Communication prob-
lems and burden of illness were statistically insignificant,
although aggressive behaviors tend to occur in the later
stagesof dementia,when verbal communicationis
severely compromised.
Ultimately,the relationship between SE and anti-
psychotic use is complex,as both SE and antipsychotic
use are likely to be influenced by resident health status.
Table 1. Characteristics ofResidents Receiving and Not Receiving Antipsychotics.
Variables
n ¼ 2,639
n (%)
or X (SD)
Percentage received
antipsychotics
or X (SD)
Percentage did not receive
antipsychotics
or X (SD)
SocialengagementX (SD) 2.2 (1.7) 2.7 (1.8)
Sociodemographic variables
Female 1737 (65.8%) 669 (38.5%) 1068 (61.5%)
Male 902 (34.2%) 395 (43.8%) 507 (56.2%)
AgeX (SD) 83.9 (6.8) 82.6 (6.8) 84.8 (6.6)
Maritalstatus
Married (ref) 948 (37.6%) 442 (46.6%) 506 (53.4%)
Separated/divorced 216 (8.6%) 97 (44.9%) 119 (55.1%)
Single/never married 96 (3.8%) 40 (41.7%) 56 (58.3%)
Widowed 1264 (50.0%) 436 (34.5%) 828 (65.5%)
GIS recipient
Yes 1000 (39.6%) 387 (38.7%) 613 (61.3%)
No (ref) 1524 (60.4%) 628 (41.2%) 896 (58.8%)
Education
Less than high school 1321 (52.3%) 531 (40.2%) 790 (59.8%)
High school 633 (25.1%) 254 (40.1%) 379 (59.9%)
Postsecondary (ref) 570 (22.6%) 230 (40.4%) 340 (59.6%)
Health-related variables
Aggression
No aggression 1677 (66.4%) 533 (31.8%) 1144 (68.2%)
Moderate 687 (27.2%) 366 (53.3%) 321 (46.7%)
Severe 160 (6.3%) 116 (72.5%) 44 (27.5%)
CognitionX (SD) .75 (.43) .65 (.48)
Depression .25 (.43) .13 (.34)
Delirium 2.55 (2.02) 1.53 (1.82)
Burden ofillness .07 (.25) .06 (.23)
Communication problems .66 (.96) .44 (.83)
Note.GIS ¼ guaranteed income supplement.
Saleh et al. 5
to receiveantipsychotics.When accounting forthese
health indicators,however,the association between SE
and antipsychoticuse was no longer significant.
This may reflect the stronger effect of health indicators
on the residents’ behavior and thus on antipsychotic use
and the ability of the residentsto socially engage.
Likewise,antipsychotics are mainly used to treat BPSD
that are associated with declines in cognition (Hersch, &
Falzgraf, 2007). Indeed, as determined by Foebel and col-
leagues(2015),our resultssuggestthat residentswith
dementia and with behavioral symptoms are more likely
to receive antipsychotics.Our findings support those of
Kamble and colleagues (2008) who reported a strong asso-
ciation between the behavioral and functional character-
istics of residents and antipsychotic use in LTCFs.
Depression, an important risk factor for low levels of
SE in newly admitted residents,is more likely to be
treated with antipsychoticsin residents with BPSD
(Alanen etal., 2006).It is unclear ifSE decreases or
increases in the weeks and months after admission,but
there is a strong association between depression and SE
in newly admitted residents.As Achterberg and
colleagues(2003) explain, symptomsof depression
(anxiety, withdrawal, and loss of interest) can act as obs-
taclesfor engaging socially.Moreover,delirium is an
acute medical condition, manifestingin behavioral
changesthat are sometimesmisdiagnosed asBPSD,
and treated with antipsychotics.Communication prob-
lems and burden of illness were statistically insignificant,
although aggressive behaviors tend to occur in the later
stagesof dementia,when verbal communicationis
severely compromised.
Ultimately,the relationship between SE and anti-
psychotic use is complex,as both SE and antipsychotic
use are likely to be influenced by resident health status.
Table 1. Characteristics ofResidents Receiving and Not Receiving Antipsychotics.
Variables
n ¼ 2,639
n (%)
or X (SD)
Percentage received
antipsychotics
or X (SD)
Percentage did not receive
antipsychotics
or X (SD)
SocialengagementX (SD) 2.2 (1.7) 2.7 (1.8)
Sociodemographic variables
Female 1737 (65.8%) 669 (38.5%) 1068 (61.5%)
Male 902 (34.2%) 395 (43.8%) 507 (56.2%)
AgeX (SD) 83.9 (6.8) 82.6 (6.8) 84.8 (6.6)
Maritalstatus
Married (ref) 948 (37.6%) 442 (46.6%) 506 (53.4%)
Separated/divorced 216 (8.6%) 97 (44.9%) 119 (55.1%)
Single/never married 96 (3.8%) 40 (41.7%) 56 (58.3%)
Widowed 1264 (50.0%) 436 (34.5%) 828 (65.5%)
GIS recipient
Yes 1000 (39.6%) 387 (38.7%) 613 (61.3%)
No (ref) 1524 (60.4%) 628 (41.2%) 896 (58.8%)
Education
Less than high school 1321 (52.3%) 531 (40.2%) 790 (59.8%)
High school 633 (25.1%) 254 (40.1%) 379 (59.9%)
Postsecondary (ref) 570 (22.6%) 230 (40.4%) 340 (59.6%)
Health-related variables
Aggression
No aggression 1677 (66.4%) 533 (31.8%) 1144 (68.2%)
Moderate 687 (27.2%) 366 (53.3%) 321 (46.7%)
Severe 160 (6.3%) 116 (72.5%) 44 (27.5%)
CognitionX (SD) .75 (.43) .65 (.48)
Depression .25 (.43) .13 (.34)
Delirium 2.55 (2.02) 1.53 (1.82)
Burden ofillness .07 (.25) .06 (.23)
Communication problems .66 (.96) .44 (.83)
Note.GIS ¼ guaranteed income supplement.
Saleh et al. 5
When prescribed cautiously, antipsychotics can enhance
the physical and psychological well-being of older adults,
which mightincrease theirlevelof SE. On the other
hand,antipsychotics have sedative effects and increase
health risksfor residentsthat mightnegatively affect
their ability to socially engage in the facility.
Although the association between SE and antipsych-
otic use was no longer presentwhen controlling for
health-related variables,our findings do not negate the
value of improved understanding of the influence of SE
as a nonpharmacological approach to addressing BPSD
(Mallidou et al., 2013). Our study highlights the need for
future research investigating potentialcausalrelations
between SE and antipsychotic use in LTCFsand for
revising the MDS-RAI instrument to include more vari-
ables directly associated to BPSD and SE.
The study findingsidentify severalimplicationsor
research and practice.For research,there is a need for
longitudinal studies to establish causality and
examination of other forms of SE such as individualized
programs and engaging outside the facility. For practice,
these study findings suggestthe continuing need for a
paradigm shift within LTCFs on the use of antipsych-
otics, where other indicators,such as delirium and
depression,are clinically addressed and ruled out prior
to prescribing and administering antipsychotics.Also,
care should be provided in a way that promotes resident
engagement,especially newly admitted residents with a
diagnosis of dementia, for their engagement in the social
life of the facility is a means of easing resident
integration.
Strengths and Limitations of the Study
Key strengths of the study are the large sample and the
established reliability and validity ofthe measurement
tools used. However, there are severallimitations.
First, the findingsdo not indicatecauseand effect
relationshipsdue to the cross-sectionalnature of the
study.Second,the inclusion ofthe use ofPRN – Pro
re nata in Latin and is used in medicine to signify a
medication thatshould be taken only when needed –
antipsychotic use in the analyses could overestimate the
prevalence of use and therefore might affect the associa-
tion. Third, the sample was about newly admitted resi-
dents who had a fully-completed admission or quarterly
assessment within 90 days of admission. Thus, those resi-
dentsmight have not been fully integrated into the
Table 2. Nested Logistic Regression Analysis ofPredictors ofUse ofAntipsychotic Drugs.
Model1 Model2 Model3
n 2,639 2,524a 2,524a
Variable OR 95% CI p OR 95% CI p OR 95% CI p
Socialengagement .85 [.81,.89] <.0001 .86 [0.82,0.90] <.0001 .97 [0.91,1.0] .21
Gender (Female ¼ ref)
Male 1.02 [0.85,1.2] .87 1.1 [0.87,1.3] .60
Age .96 [0.95,0.97] <.0001 .97 [0.95,0.98] <.0001
Maritalstatus (married ¼ ref)
Separated/divorced .92 [0.66,1.3] .62 1.0 [0.73,1.4] .94
Single,never married .93 [0.60,1.4] .73 1.1 [0.71,1.8] .63
Widowed .76 [0.63,0.93] <.01 .84 [0.68,1.0] .09
GIS (no ¼ ref) .98 [0.84,1.2] .82 .96 [0.80,1.2] .66
Education (postsecondary ¼ ref)
Less than high school 1.02 [0.84,1.3] .78 1.1 [0.88,1.4] .45
High school 1.03 [0.80,1.3] .87 1.1 [0.83,1.4] .61
Aggression (0 ¼ ref)
Moderate 1.8 [1.5,2.2] <.0001
Severe 3.2 [2.1,4.7] <.0001
Cognition 1.0 .76
Depression 1.3 [1.0,1.6] <.05
Delirium 1.2 [1.1,1.3] <.0001
Burden ofillness .08 [0.55,1.1] .20
Communication problems .98 [0.88,1.1] .74
Note.GIS ¼ guaranteed income supplement;OR ¼ odds ratio;CI ¼ confidence interval.
aOne hundred and fifteen observations were deleted due to missing values for the response or explanatory variables.
6 Canadian Journalof Nursing Research 0(0)
the physical and psychological well-being of older adults,
which mightincrease theirlevelof SE. On the other
hand,antipsychotics have sedative effects and increase
health risksfor residentsthat mightnegatively affect
their ability to socially engage in the facility.
Although the association between SE and antipsych-
otic use was no longer presentwhen controlling for
health-related variables,our findings do not negate the
value of improved understanding of the influence of SE
as a nonpharmacological approach to addressing BPSD
(Mallidou et al., 2013). Our study highlights the need for
future research investigating potentialcausalrelations
between SE and antipsychotic use in LTCFsand for
revising the MDS-RAI instrument to include more vari-
ables directly associated to BPSD and SE.
The study findingsidentify severalimplicationsor
research and practice.For research,there is a need for
longitudinal studies to establish causality and
examination of other forms of SE such as individualized
programs and engaging outside the facility. For practice,
these study findings suggestthe continuing need for a
paradigm shift within LTCFs on the use of antipsych-
otics, where other indicators,such as delirium and
depression,are clinically addressed and ruled out prior
to prescribing and administering antipsychotics.Also,
care should be provided in a way that promotes resident
engagement,especially newly admitted residents with a
diagnosis of dementia, for their engagement in the social
life of the facility is a means of easing resident
integration.
Strengths and Limitations of the Study
Key strengths of the study are the large sample and the
established reliability and validity ofthe measurement
tools used. However, there are severallimitations.
First, the findingsdo not indicatecauseand effect
relationshipsdue to the cross-sectionalnature of the
study.Second,the inclusion ofthe use ofPRN – Pro
re nata in Latin and is used in medicine to signify a
medication thatshould be taken only when needed –
antipsychotic use in the analyses could overestimate the
prevalence of use and therefore might affect the associa-
tion. Third, the sample was about newly admitted resi-
dents who had a fully-completed admission or quarterly
assessment within 90 days of admission. Thus, those resi-
dentsmight have not been fully integrated into the
Table 2. Nested Logistic Regression Analysis ofPredictors ofUse ofAntipsychotic Drugs.
Model1 Model2 Model3
n 2,639 2,524a 2,524a
Variable OR 95% CI p OR 95% CI p OR 95% CI p
Socialengagement .85 [.81,.89] <.0001 .86 [0.82,0.90] <.0001 .97 [0.91,1.0] .21
Gender (Female ¼ ref)
Male 1.02 [0.85,1.2] .87 1.1 [0.87,1.3] .60
Age .96 [0.95,0.97] <.0001 .97 [0.95,0.98] <.0001
Maritalstatus (married ¼ ref)
Separated/divorced .92 [0.66,1.3] .62 1.0 [0.73,1.4] .94
Single,never married .93 [0.60,1.4] .73 1.1 [0.71,1.8] .63
Widowed .76 [0.63,0.93] <.01 .84 [0.68,1.0] .09
GIS (no ¼ ref) .98 [0.84,1.2] .82 .96 [0.80,1.2] .66
Education (postsecondary ¼ ref)
Less than high school 1.02 [0.84,1.3] .78 1.1 [0.88,1.4] .45
High school 1.03 [0.80,1.3] .87 1.1 [0.83,1.4] .61
Aggression (0 ¼ ref)
Moderate 1.8 [1.5,2.2] <.0001
Severe 3.2 [2.1,4.7] <.0001
Cognition 1.0 .76
Depression 1.3 [1.0,1.6] <.05
Delirium 1.2 [1.1,1.3] <.0001
Burden ofillness .08 [0.55,1.1] .20
Communication problems .98 [0.88,1.1] .74
Note.GIS ¼ guaranteed income supplement;OR ¼ odds ratio;CI ¼ confidence interval.
aOne hundred and fifteen observations were deleted due to missing values for the response or explanatory variables.
6 Canadian Journalof Nursing Research 0(0)
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
routine of the facility,thereby negatively affecting their
SE scores. Finally, the content validity of the ISE items
of ‘at ease doing self-initiated activities’ and ‘establishes
own goals’ (Gerritsen et al., 2008, p. 41) reflect resident
autonomy,which does not have a socialorientation as
expected in a scale that measures SE.
In conclusion, SE is associated with less likelihood of
antipsychotic use when controlling for sociodemographic
variables of older adults residing in LTCFs that contrib-
utes to their health status and well-being.Although SE
was no longersignificantwhen controlling forhealth
variables,we argue thatthis finding suggestsfurther
research attention to thecomplexityof SE and its
effect on other dimensions of older adults’ health.
Acknowledgments
This work was carried outin partnership with the Michael
Smith Foundation for Health Researchand the Fraser
Health Authority, Province of British Columbia. Their support
and assistance is gratefully acknowledged as is that provided by
the older adults, family members, practitioners, advocates, and
others who participated in the research.The authors would
also like to acknowledge the contributions ofRonald Kelly,
PhD; Laura Funk, PhD; Francis Lau, PhD; and Taylor
Hainstock,BA, to the larger project within which this article
was developed.
Authors’ Contributions
N. Saleh planned the study, conducted the data analyses, and
wrote the article. M. J. Penning helped to plan the study, made
the data available, reviewed the article, and helped to revise the
article.D. Cloutier made the data available and helped revise
the article. A. Mallidou reviewed the manuscript and helped to
revise the article.K. Nuernberger provided access to the data
and assistance with statisticalanalyses.D. Taylor facilitated
access to the data through Fraser Health Authority.
Authors’ Note
The interpretations expressed herein are those of the authors
and do notnecessarily representthose of the FHA or other
participants.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect
to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financialsup-
port for the research,authorship,and/or publication ofthis
article:This work was supported by the Canadian Institutes
for Health Research: Partnershipsin Health System
Improvement Grant Program (#122184) to (MJP, DC et al.).
References
Achterberg, W., Pot, A. M., Kerkstra, A., Ooms, M., Muller,
M., & Ribbe, M. (2003). The effect of depression on social
engagementin newly admitted Dutch nursing home resi-
dents. The Gerontologist, 43, 213–218.
Ahn, H., & Horgas,A. (2013).The relationship between pain
and disruptive behaviorsin nursing home residentswith
dementia. BMC geriatrics, 13(1), 1471–1476.
Alanen,H. M., Finne-Soveri,H., Noro, A., & Leinonen,E.
(2006). Use of antipsychotic medications among elderly resi-
dents in long-term institutionalcare:A three-year follow-
up. InternationalJournal of Geriatric Psychiatry,21,
288–295.
Bennett,K. M. (2002).Low levelsocialengagement as a pre-
cursor of mortality among people in later life. Age Ageing,
31, 165–168.
Canadian Nurses Association.(2013).Three strategies to help
Canada’s most vulnerable. Retrieved from https://www.cna-
aiic.ca//media/cna/files/en/pre_budget_brief_to_house_
of_commons_2013_e.pdf.
Chen,L. Y., Liu, L. K., Liu, C. L., Peng,L. N., Lin, M. H.,
Chen, L. K., . . . ;Chang, P. L. (2013). Predicting functional
decline of older men living in veteran homes by minimum
data set: Implications for disability prevention programs in
long term care settings. JAMDA, 14, 309e9–e13.
Canadian Life and Health InsuranceAssociation.(2012).
CLHIA report on long-term care policy: Improving the acces-
sibility, quality and sustainability of long-term care in Canada
long-term care. (June). Retrieved from http://www.clhia.ca/
domino/html/clhia/CLHIA_LP4W_LND_Webstation.nsf/
resources/Content_PDFs/$file/LTC_Policy_Paper.pdf.
Cohen-Mansfield, J., Marx, M. S., & Rosenthal, A. S. (1989).
A description ofagitation in a nursing home.Journal of
Gerontology, 44, M77–M84.
Fischer,C. E., Cohen,C., Forrest,L., Schweizer,T. A., &
Wasylenki,D. (2011).Psychotropicmedicationuse in
Canadian long-term care patients referred for psychogeriat-
ric consultation. Canadian Geotechnical Journal, 14, 73–77.
Foebel, A., Ballokova, A., Wellens, N. I., Fialova, D., Milisen,
K., Liperoti,R., & Hirdes, J. P. (2015).A retrospective,
longitudinal study of factors associated with new antipsych-
otic medication useamong recently admitted long-term
care residents.BMC Geriatrics,15. doi: 10.1186/s12877-
015-0127-8.
Gerritsen,D. L., Steverink,N., Frijters,D. H. M., Hirdes,J.
P., Ooms, M. E., & Ribbe, M. W. (2008). A Revised Index
for social engagementfor longterm care.Journal of
Gerontological Nursing, 34(4), 40–48.
Hawes, C., Morris, J. N., Phillips, C. D., Mor, V., Fries, B. E.,
& Nonemaker, S. (1995).Reliability estimatesfor the
Minimum Data Set for nursing home resident assessment
and care screening (MDS). Gerontologist, 35, 172–178.
Hersch,E. C., & Falzgraf, S. (2007).Managementof the
behavioraland psychologicalsymptomsof dementia.
Clinical Interventions in Aging, 2, 611–621.
Hirdes, J., Frijters, D., & Teare, G. (2003). The MDS CHESS
scale: A new measure to predict mortality in the institutio-
nalized elderly.Journalof the American Geriatrics Society,
51, 96–100.
Huybrechts,K. F., Rothman, K. J., Silliman, R. A.,
Brookhart, M. A., & Schneeweiss, S. (2011). Risk of death
and hospital admission for major medical events after initi-
ation of psychotropic medications in older adults admitted
Saleh et al. 7
SE scores. Finally, the content validity of the ISE items
of ‘at ease doing self-initiated activities’ and ‘establishes
own goals’ (Gerritsen et al., 2008, p. 41) reflect resident
autonomy,which does not have a socialorientation as
expected in a scale that measures SE.
In conclusion, SE is associated with less likelihood of
antipsychotic use when controlling for sociodemographic
variables of older adults residing in LTCFs that contrib-
utes to their health status and well-being.Although SE
was no longersignificantwhen controlling forhealth
variables,we argue thatthis finding suggestsfurther
research attention to thecomplexityof SE and its
effect on other dimensions of older adults’ health.
Acknowledgments
This work was carried outin partnership with the Michael
Smith Foundation for Health Researchand the Fraser
Health Authority, Province of British Columbia. Their support
and assistance is gratefully acknowledged as is that provided by
the older adults, family members, practitioners, advocates, and
others who participated in the research.The authors would
also like to acknowledge the contributions ofRonald Kelly,
PhD; Laura Funk, PhD; Francis Lau, PhD; and Taylor
Hainstock,BA, to the larger project within which this article
was developed.
Authors’ Contributions
N. Saleh planned the study, conducted the data analyses, and
wrote the article. M. J. Penning helped to plan the study, made
the data available, reviewed the article, and helped to revise the
article.D. Cloutier made the data available and helped revise
the article. A. Mallidou reviewed the manuscript and helped to
revise the article.K. Nuernberger provided access to the data
and assistance with statisticalanalyses.D. Taylor facilitated
access to the data through Fraser Health Authority.
Authors’ Note
The interpretations expressed herein are those of the authors
and do notnecessarily representthose of the FHA or other
participants.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect
to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financialsup-
port for the research,authorship,and/or publication ofthis
article:This work was supported by the Canadian Institutes
for Health Research: Partnershipsin Health System
Improvement Grant Program (#122184) to (MJP, DC et al.).
References
Achterberg, W., Pot, A. M., Kerkstra, A., Ooms, M., Muller,
M., & Ribbe, M. (2003). The effect of depression on social
engagementin newly admitted Dutch nursing home resi-
dents. The Gerontologist, 43, 213–218.
Ahn, H., & Horgas,A. (2013).The relationship between pain
and disruptive behaviorsin nursing home residentswith
dementia. BMC geriatrics, 13(1), 1471–1476.
Alanen,H. M., Finne-Soveri,H., Noro, A., & Leinonen,E.
(2006). Use of antipsychotic medications among elderly resi-
dents in long-term institutionalcare:A three-year follow-
up. InternationalJournal of Geriatric Psychiatry,21,
288–295.
Bennett,K. M. (2002).Low levelsocialengagement as a pre-
cursor of mortality among people in later life. Age Ageing,
31, 165–168.
Canadian Nurses Association.(2013).Three strategies to help
Canada’s most vulnerable. Retrieved from https://www.cna-
aiic.ca//media/cna/files/en/pre_budget_brief_to_house_
of_commons_2013_e.pdf.
Chen,L. Y., Liu, L. K., Liu, C. L., Peng,L. N., Lin, M. H.,
Chen, L. K., . . . ;Chang, P. L. (2013). Predicting functional
decline of older men living in veteran homes by minimum
data set: Implications for disability prevention programs in
long term care settings. JAMDA, 14, 309e9–e13.
Canadian Life and Health InsuranceAssociation.(2012).
CLHIA report on long-term care policy: Improving the acces-
sibility, quality and sustainability of long-term care in Canada
long-term care. (June). Retrieved from http://www.clhia.ca/
domino/html/clhia/CLHIA_LP4W_LND_Webstation.nsf/
resources/Content_PDFs/$file/LTC_Policy_Paper.pdf.
Cohen-Mansfield, J., Marx, M. S., & Rosenthal, A. S. (1989).
A description ofagitation in a nursing home.Journal of
Gerontology, 44, M77–M84.
Fischer,C. E., Cohen,C., Forrest,L., Schweizer,T. A., &
Wasylenki,D. (2011).Psychotropicmedicationuse in
Canadian long-term care patients referred for psychogeriat-
ric consultation. Canadian Geotechnical Journal, 14, 73–77.
Foebel, A., Ballokova, A., Wellens, N. I., Fialova, D., Milisen,
K., Liperoti,R., & Hirdes, J. P. (2015).A retrospective,
longitudinal study of factors associated with new antipsych-
otic medication useamong recently admitted long-term
care residents.BMC Geriatrics,15. doi: 10.1186/s12877-
015-0127-8.
Gerritsen,D. L., Steverink,N., Frijters,D. H. M., Hirdes,J.
P., Ooms, M. E., & Ribbe, M. W. (2008). A Revised Index
for social engagementfor longterm care.Journal of
Gerontological Nursing, 34(4), 40–48.
Hawes, C., Morris, J. N., Phillips, C. D., Mor, V., Fries, B. E.,
& Nonemaker, S. (1995).Reliability estimatesfor the
Minimum Data Set for nursing home resident assessment
and care screening (MDS). Gerontologist, 35, 172–178.
Hersch,E. C., & Falzgraf, S. (2007).Managementof the
behavioraland psychologicalsymptomsof dementia.
Clinical Interventions in Aging, 2, 611–621.
Hirdes, J., Frijters, D., & Teare, G. (2003). The MDS CHESS
scale: A new measure to predict mortality in the institutio-
nalized elderly.Journalof the American Geriatrics Society,
51, 96–100.
Huybrechts,K. F., Rothman, K. J., Silliman, R. A.,
Brookhart, M. A., & Schneeweiss, S. (2011). Risk of death
and hospital admission for major medical events after initi-
ation of psychotropic medications in older adults admitted
Saleh et al. 7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
to nursing homes.Canadian MedicalAssociation Journal,
183, 411– 419.
Kamble,P., Chen,H., Sherer,J., & Aparasu,R. R. (2008).
Antipsychotic drug use among elderly nursing home resi-
dents in the United States.The AmericanJournal of
Geriatric Pharmacotherapy, 6, 187–197.
Kiely, D. K., Simon,S. E., Jones, R. N., & Morris, J. N.
(2000).The protective effect of socialengagement on mor-
tality in long-term care.Journalof the American Geriatrics
Society, 48.doi:10.1111/j.1532-5415.2000.tb02624.x.
Krueger, K. R., Wilson, R. S., Kamenetsky, J. M., Barnes, L.
L., Bienias,J. L., & Bennett,D. A. (2009).Socialengage-
ment and cognitive function in old age. Experimental Aging
Research, 35, 45–60.
Lawton, M. P., Casten, R., Parmelee, P. A., Van Haitsma, K.,
Corn, J., & Kleban, M. H. (1998). Psychometric character-
istics of the minimum data set II:Validity.Journalof the
American Geriatrics Society, 46(6), 736–744.
Lou, V. W., Chi, I., Kwan, C. W., & Leung, A. Y. (2013).
Trajectories of social engagement and depressive symptoms
among long-term care facility residents in Hong Kong. Age
Ageing, 42, 215–22.
Mallidou,A., Oliveira,N., & Borycki,E. (2013).Behavioural
and psychologicalsymptoms ofdementia:Are there any
effective alternative-to-antipsychoticsstrategies? OA
Family Medicine, 1, 1–6.
Ministry of Health. (2011). A review of the use of antipsychotic drugs
in British Columbia ResidentialCare Facilities (December).
Retrieved from http://www.health.gov.bc.ca/library/publica-
tions/year/2011/use-of-antipsychotic-drugs.pdf.
Mor, V., Angelelli, J., Jones, R., Roy, J., Moore, T., & Morris,
J. (2003). Inter-rater reliability of nursing home quality indi-
cators in the U.S.BMC Health Services Research,3(20).
doi:10.1186/1472-6963-3-20.
Perlman, C. M., & Hirdes, J. P. (2008). The aggressive behavior
scale: A new scale to measure aggression based on the min-
imum data set.Journalof the American Geriatrics Society,
56, 2298–2303.
Perucca,P., & Gilliam, F. G. (2012).Adverseeffectsof
antiepilepticdrugs.The LancetNeurology,11, 792–802.
Retrieved from http://dx.doi.org/10.1016/S1474-4422(12)
70153-9.
Voyer, P., Richard, S., Doucet, L., Danjou, C., & Carmichael,
P. H. (2008).Detection of delirium by nurses among long-
term care residentswith dementia.BMC Nursing, 7.
doi:10.1186/1472-6955-7-4.
Voyer, P., Verreault,R., Azizah, G. M., Desrosiers,J.,
Champoux, N., & Be´dard, A. (2005). Prevalence of physical
and verbalaggressivebehavioursand associated factors
among older adults in long-term care facilities.BMC geri-
atrics, 5.doi:10.1186/1471-2318-5-13.
Williams, K. N., & Kemper, S. (2011). Exploring interventions
to reduce cognitive decline in aging. Journal of Psychosocial
Nursing and Mental Health Services, 48, 42–51.
Author Biographies
Nasrin Saleh is a PhD student in the Nursing program,
University of Victoria.Her main research interest is in
the area of older adults living in long-term care facilities
and the role of socialengagementin improving their
quality of life.
Margaret Penningis a professorof Sociology and
research affiliate in the Institute on Aging and Lifelong
Health at the University of Victoria in British Columbia,
Canada. Her research interests include aging, health and
health care with a focus on issues of family life,social
support,caregiving and care receiving,health-care sys-
tems, and health services use.
DeniseCloutieris a professorin the Departmentof
Geography and a research affiliate with the Institute on
Aging and Lifelong Health at the University of Victoria.
As a health and social geographer, she studies models of
health service delivery and the continuum ofcare for
older adults.Her research has focused on the care of
populationswho are living in rural environments,
socially isolated,stroke affected,at the end of life,and
clients of home care and institutional long-term care. In
conducting community-based and collaborative
research, she employs mixed methods, both quantitative
and qualitative.This work has been funded by the
Canadian Institutes of Health Research, Social Sciences
and Humanities Research Councilof Canada,Michael
Smith Foundation for Health Research,and World
Health Organization.She has published her research in
leading interdisciplinary and geographical journals such
as the Journal of Gerontology,The Gerontologist,
Progressin Human Geography,Social and Cultural
Geography,Health and Place,and SocialSciences and
Medicine.
Anastasia Mallidou is an assistant professor,Schoolof
Nursing and research affiliate of the Institute on Aging
and Lifelong Health at the University of Victoria,
Victoria, British Columbia, Canada. She is also research
affiliateof the Fraser Health Authority, Vancouver,
British Columbia. Her research interests include applied
health services research (e.g.,impactof work environ-
ment/context on safety practices, organizational culture),
leadership and managementin health organizations,
knowledgetranslation (KT) and utilization, healthy
aging,and health policy uptake.Dr Mallidou currently
works on optimizing residential care facilities to improve
quality of care, and quality of life and well-being of older
adults using applied arts (i.e., individualized music, dan-
cing,and theater),and in severalknowledge syntheses
studies on knowledge translation,evidence-based prac-
tice (EBP) issues, and patient-oriented research.
Kim Nuernbergeris a program consultantfor the
Canadian Institute of Health Information (CIHI)
Western Office.Kim has more than 10 years of experi-
ence as a health data analyst,much of it working with
large administrativehealth data sets.Her experience
spans a broad range ofhealth service issues covering
8 Canadian Journalof Nursing Research 0(0)
183, 411– 419.
Kamble,P., Chen,H., Sherer,J., & Aparasu,R. R. (2008).
Antipsychotic drug use among elderly nursing home resi-
dents in the United States.The AmericanJournal of
Geriatric Pharmacotherapy, 6, 187–197.
Kiely, D. K., Simon,S. E., Jones, R. N., & Morris, J. N.
(2000).The protective effect of socialengagement on mor-
tality in long-term care.Journalof the American Geriatrics
Society, 48.doi:10.1111/j.1532-5415.2000.tb02624.x.
Krueger, K. R., Wilson, R. S., Kamenetsky, J. M., Barnes, L.
L., Bienias,J. L., & Bennett,D. A. (2009).Socialengage-
ment and cognitive function in old age. Experimental Aging
Research, 35, 45–60.
Lawton, M. P., Casten, R., Parmelee, P. A., Van Haitsma, K.,
Corn, J., & Kleban, M. H. (1998). Psychometric character-
istics of the minimum data set II:Validity.Journalof the
American Geriatrics Society, 46(6), 736–744.
Lou, V. W., Chi, I., Kwan, C. W., & Leung, A. Y. (2013).
Trajectories of social engagement and depressive symptoms
among long-term care facility residents in Hong Kong. Age
Ageing, 42, 215–22.
Mallidou,A., Oliveira,N., & Borycki,E. (2013).Behavioural
and psychologicalsymptoms ofdementia:Are there any
effective alternative-to-antipsychoticsstrategies? OA
Family Medicine, 1, 1–6.
Ministry of Health. (2011). A review of the use of antipsychotic drugs
in British Columbia ResidentialCare Facilities (December).
Retrieved from http://www.health.gov.bc.ca/library/publica-
tions/year/2011/use-of-antipsychotic-drugs.pdf.
Mor, V., Angelelli, J., Jones, R., Roy, J., Moore, T., & Morris,
J. (2003). Inter-rater reliability of nursing home quality indi-
cators in the U.S.BMC Health Services Research,3(20).
doi:10.1186/1472-6963-3-20.
Perlman, C. M., & Hirdes, J. P. (2008). The aggressive behavior
scale: A new scale to measure aggression based on the min-
imum data set.Journalof the American Geriatrics Society,
56, 2298–2303.
Perucca,P., & Gilliam, F. G. (2012).Adverseeffectsof
antiepilepticdrugs.The LancetNeurology,11, 792–802.
Retrieved from http://dx.doi.org/10.1016/S1474-4422(12)
70153-9.
Voyer, P., Richard, S., Doucet, L., Danjou, C., & Carmichael,
P. H. (2008).Detection of delirium by nurses among long-
term care residentswith dementia.BMC Nursing, 7.
doi:10.1186/1472-6955-7-4.
Voyer, P., Verreault,R., Azizah, G. M., Desrosiers,J.,
Champoux, N., & Be´dard, A. (2005). Prevalence of physical
and verbalaggressivebehavioursand associated factors
among older adults in long-term care facilities.BMC geri-
atrics, 5.doi:10.1186/1471-2318-5-13.
Williams, K. N., & Kemper, S. (2011). Exploring interventions
to reduce cognitive decline in aging. Journal of Psychosocial
Nursing and Mental Health Services, 48, 42–51.
Author Biographies
Nasrin Saleh is a PhD student in the Nursing program,
University of Victoria.Her main research interest is in
the area of older adults living in long-term care facilities
and the role of socialengagementin improving their
quality of life.
Margaret Penningis a professorof Sociology and
research affiliate in the Institute on Aging and Lifelong
Health at the University of Victoria in British Columbia,
Canada. Her research interests include aging, health and
health care with a focus on issues of family life,social
support,caregiving and care receiving,health-care sys-
tems, and health services use.
DeniseCloutieris a professorin the Departmentof
Geography and a research affiliate with the Institute on
Aging and Lifelong Health at the University of Victoria.
As a health and social geographer, she studies models of
health service delivery and the continuum ofcare for
older adults.Her research has focused on the care of
populationswho are living in rural environments,
socially isolated,stroke affected,at the end of life,and
clients of home care and institutional long-term care. In
conducting community-based and collaborative
research, she employs mixed methods, both quantitative
and qualitative.This work has been funded by the
Canadian Institutes of Health Research, Social Sciences
and Humanities Research Councilof Canada,Michael
Smith Foundation for Health Research,and World
Health Organization.She has published her research in
leading interdisciplinary and geographical journals such
as the Journal of Gerontology,The Gerontologist,
Progressin Human Geography,Social and Cultural
Geography,Health and Place,and SocialSciences and
Medicine.
Anastasia Mallidou is an assistant professor,Schoolof
Nursing and research affiliate of the Institute on Aging
and Lifelong Health at the University of Victoria,
Victoria, British Columbia, Canada. She is also research
affiliateof the Fraser Health Authority, Vancouver,
British Columbia. Her research interests include applied
health services research (e.g.,impactof work environ-
ment/context on safety practices, organizational culture),
leadership and managementin health organizations,
knowledgetranslation (KT) and utilization, healthy
aging,and health policy uptake.Dr Mallidou currently
works on optimizing residential care facilities to improve
quality of care, and quality of life and well-being of older
adults using applied arts (i.e., individualized music, dan-
cing,and theater),and in severalknowledge syntheses
studies on knowledge translation,evidence-based prac-
tice (EBP) issues, and patient-oriented research.
Kim Nuernbergeris a program consultantfor the
Canadian Institute of Health Information (CIHI)
Western Office.Kim has more than 10 years of experi-
ence as a health data analyst,much of it working with
large administrativehealth data sets.Her experience
spans a broad range ofhealth service issues covering
8 Canadian Journalof Nursing Research 0(0)

the life course and representing everything from contra-
ception to the provision and delivery ofappropriate
long-term careservices.Most recently,she has been
involved in a collaborative project involving researchers
based at the University of Victoria and the Fraser Health
Authority examining patternsand predictorsof long-
term care use through administrative and clinicaldata.
This project has involved extensive use of SAS and other
statisticalsoftware to link anonymized data setsand
employ a wide variety of statistical techniques.
Dee Taylor is the director of the Research Department at
Interior Health.She is involved with local,provincial,
national,and internationalcollaborative research pro-
jects consistingof academics,policy makers,health
authority leaders,healthcare administrators,and care
teams from multiple jurisdictions.Dee has a Masters,
Disability and Community Studies, a PhD, Community
Health Science,and is a postdoctoralfellow with the
Centre on Aging in Halifax,Nova Scotia,Mount St.
Vincent University. Her research interests center on resi-
dentiallong-term care,the quality ofcare and life for
residents, and policies, workplace culture, and relational
practices within healthcare settings.
Saleh et al. 9
ception to the provision and delivery ofappropriate
long-term careservices.Most recently,she has been
involved in a collaborative project involving researchers
based at the University of Victoria and the Fraser Health
Authority examining patternsand predictorsof long-
term care use through administrative and clinicaldata.
This project has involved extensive use of SAS and other
statisticalsoftware to link anonymized data setsand
employ a wide variety of statistical techniques.
Dee Taylor is the director of the Research Department at
Interior Health.She is involved with local,provincial,
national,and internationalcollaborative research pro-
jects consistingof academics,policy makers,health
authority leaders,healthcare administrators,and care
teams from multiple jurisdictions.Dee has a Masters,
Disability and Community Studies, a PhD, Community
Health Science,and is a postdoctoralfellow with the
Centre on Aging in Halifax,Nova Scotia,Mount St.
Vincent University. Her research interests center on resi-
dentiallong-term care,the quality ofcare and life for
residents, and policies, workplace culture, and relational
practices within healthcare settings.
Saleh et al. 9
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
