Social Engagement and Antipsychotic Use in Addressing the Behavioral and Psychological Symptoms of Dementia in Long-Term Care Facilities
Added on 2023-06-09
9 Pages7533 Words133 Views
Original Research Report
Social Engagement and Antipsychotic
Use in Addressing the Behavioral and
Psychological Symptoms of Dementia
in Long-Term Care Facilities
Nasrin Saleh 1
, Margaret Penning 2 , Denise Cloutier 3
,
Anastasia Mallidou 1 , Kim Nuernberger4 , and Deanne Taylor 5
Abstract
Objectives: The use of antipsychotics, mainly to address the behavioral and psychological symptoms of dementia (BPSD),
remains a common and frequent practice in long-term care facilities (LTCFs) despite their associated risks. The objective of
this study was to explore the association between social engagement (SE) and the use of antipsychotics in addressing the
BPSD in newly admitted residents to LTCFs.
Methods: A cross-sectional study was undertaken using administrative data, primarily the Resident Assessment Instrument
Minimum Data Set (Version 2.0) that collected between 2008 and 2011 (Fraser Health region, British Columbia, Canada). The
data analysis conducted on a sample of 2,639 newly admitted residents aged 65 or older with a diagnosis of Alzheimer’s
disease or other dementias as of their first full or first quarterly assessment. Multivariate logistic regression analyses were
undertaken to predict antipsychotic use based on SE.
Results: SE was found to be a statistically significant predictor of antipsychotic use when controlling for sociodemographic
variables (odds ratio (OR) ¼ .86, p < .0001, confidence interval (CI) [0.82, 0.90]). However, the association disappeared when
controlling for health variables (OR ¼ .97, p ¼ .21, CI [0.97, 1.0]).
Conclusion: The prediction of antipsychotic use in newly admitted residents to LTCFs by SE is complex. Further research is
warranted for further examination of the association of antipsychotic use in newly admitted residents to LTCFs.
Keywords
long-term care facilities, residential care, social engagement, antipsychotics
Background
Demand on long-term care facilities (LTCFs) in Canada
is increasing due to the rise of life expectancy and the
number of persons with dementia. In 2011, 5 million
Canadians were 65 years of age or older, which is
expected to double by the year 2036 (Canadian Nurses
Association, 2013). Almost one million Canadians will
be living with dementia by the year 2036 compared to
450,000 in 2012 (Canadian Life and Health Insurance
Association, 2012). This is presenting major challenges
to policy makers and the health-care system and requir-
ing a shift of priorities, adapting innovative approaches
to keep older adults healthy and independent.
1 School of Nursing, University of Victoria, British Columbia, Canada
2 Department of Sociology and Institute on Aging and Lifelong Health,
University of Victoria, British Columbia, Canada
3 Department of Geography and Institute on Aging and Lifelong Health,
University of Victoria, British Columbia, Canada
4 British Columbia Trajectories in Care Project, University of Victoria,
British Columbia, Canada
5 Research and Knowledge Translation, Interior Health Authority, Research
Affiliate, Fraser Health Authority, British Columbia, Canada
Corresponding Author:
Nasrin Saleh, School of Nursing, University of Victoria, 2833 Dufferin
Avenue, Victoria, British Columbia, Canada V8R 3L6.
Email: nasrin@uvic.ca
Canadian Journal of Nursing Research
0(0): 1–9
! The Author(s) 2017
Reprints and permissions:
sagepub.com/journalsPermissions.nav
DOI: 10.1177/0844562117726253
journals.sagepub.com/home/cjn
Social Engagement and Antipsychotic
Use in Addressing the Behavioral and
Psychological Symptoms of Dementia
in Long-Term Care Facilities
Nasrin Saleh 1
, Margaret Penning 2 , Denise Cloutier 3
,
Anastasia Mallidou 1 , Kim Nuernberger4 , and Deanne Taylor 5
Abstract
Objectives: The use of antipsychotics, mainly to address the behavioral and psychological symptoms of dementia (BPSD),
remains a common and frequent practice in long-term care facilities (LTCFs) despite their associated risks. The objective of
this study was to explore the association between social engagement (SE) and the use of antipsychotics in addressing the
BPSD in newly admitted residents to LTCFs.
Methods: A cross-sectional study was undertaken using administrative data, primarily the Resident Assessment Instrument
Minimum Data Set (Version 2.0) that collected between 2008 and 2011 (Fraser Health region, British Columbia, Canada). The
data analysis conducted on a sample of 2,639 newly admitted residents aged 65 or older with a diagnosis of Alzheimer’s
disease or other dementias as of their first full or first quarterly assessment. Multivariate logistic regression analyses were
undertaken to predict antipsychotic use based on SE.
Results: SE was found to be a statistically significant predictor of antipsychotic use when controlling for sociodemographic
variables (odds ratio (OR) ¼ .86, p < .0001, confidence interval (CI) [0.82, 0.90]). However, the association disappeared when
controlling for health variables (OR ¼ .97, p ¼ .21, CI [0.97, 1.0]).
Conclusion: The prediction of antipsychotic use in newly admitted residents to LTCFs by SE is complex. Further research is
warranted for further examination of the association of antipsychotic use in newly admitted residents to LTCFs.
Keywords
long-term care facilities, residential care, social engagement, antipsychotics
Background
Demand on long-term care facilities (LTCFs) in Canada
is increasing due to the rise of life expectancy and the
number of persons with dementia. In 2011, 5 million
Canadians were 65 years of age or older, which is
expected to double by the year 2036 (Canadian Nurses
Association, 2013). Almost one million Canadians will
be living with dementia by the year 2036 compared to
450,000 in 2012 (Canadian Life and Health Insurance
Association, 2012). This is presenting major challenges
to policy makers and the health-care system and requir-
ing a shift of priorities, adapting innovative approaches
to keep older adults healthy and independent.
1 School of Nursing, University of Victoria, British Columbia, Canada
2 Department of Sociology and Institute on Aging and Lifelong Health,
University of Victoria, British Columbia, Canada
3 Department of Geography and Institute on Aging and Lifelong Health,
University of Victoria, British Columbia, Canada
4 British Columbia Trajectories in Care Project, University of Victoria,
British Columbia, Canada
5 Research and Knowledge Translation, Interior Health Authority, Research
Affiliate, Fraser Health Authority, British Columbia, Canada
Corresponding Author:
Nasrin Saleh, School of Nursing, University of Victoria, 2833 Dufferin
Avenue, Victoria, British Columbia, Canada V8R 3L6.
Email: nasrin@uvic.ca
Canadian Journal of Nursing Research
0(0): 1–9
! The Author(s) 2017
Reprints and permissions:
sagepub.com/journalsPermissions.nav
DOI: 10.1177/0844562117726253
journals.sagepub.com/home/cjn
Since the early 1990s, LTCFs have moved from a
medical model focusing on treatment toward a social
model of care emphasizing a home-like environment.
Moreover, the culture change movement in LTCFs,
based on the philosophy of person-centered care, focuses
on well-being and quality of life as defined by the resi-
dent. However, the prevalence of antipsychotic use in
LTCFs remains high (Fischer, Cohen, Forrest,
Schweizer, & Wasylenki, 2011), mainly to address the
behavioral and psychological symptoms of dementia
(BPSD) that include aggression, agitation, restlessness,
wandering, hoarding, sleep disturbances, psychosis,
delusions, hallucinations, and sundowning
(Cohen-Mansfield, Marx, & Rosenthal, 1989).
Recently, British Columbia (BC) Ministry of Health
reviewed antipsychotic use in LTCFs and recommended
its use for the treatment of BPSD under several condi-
tions (MoH, 2011). These conditions include weighing
the risks against the benefits, using those drugs as a
last resort, obtaining informed consent prior to use,
and following the clinical guidelines of a low dose,
slow titration, and over a short period with close moni-
toring. Yet, the review illustrated that over half (50.3%)
of the residents were prescribed antipsychotics between
April 2010 and June 2011, an increase of 37% within a
decade (MoH, 2011), with similar increases reported
across Canadian health authorities. While newly
admitted residents are more likely than other residents
to be prescribed at least one antipsychotic during the first
90 days of admission (Huybrechts, Rothman, Silliman,
Brookhart, & Schneeweiss, 2011), antipsychotic use can
be as twice as high in residents with BPSD (Alanen,
Finne-Soveri, Noro, & Leinonen, 2006). Antipsychotic
use in older adults, particularly with dementia, is asso-
ciated with multiple side effects (Perucca & Gilliam,
2012) such as increased risks of mortality, falls, and
hip fractures. Furthermore, antipsychotics may worsen
cognition and increase sedative load (Perucca & Gilliam,
2012) that, in turn, may reduce the level of social engage-
ment (SE).
SE is considered essential to the psychological and
physical well-being (Bennett, 2002) of older adults in
LTCFs due to challenges within the setting in keeping
older adults active and stimulated. Scholars have pro-
posed that SE might be an alternative to antipsychotics
use (Mallidou, Oliveira, & Borycki, 2013). Socially enga-
ging residents has positive health outcomes, such as a
protective effect on mortality (Bennett, 2002; Kiely,
Simon, Jones, & Morris, 2000), and improved function
and cognition (Chen et al., 2013). SE is also associated
with decreased symptoms of depression (Lou, Chi,
Kwan, & Leung, 2013) and is an indicator of quality of
life, as it relates to positive emotions, sense of purpose,
and life satisfaction. Conversely, lonely older adults
often have low self-rated health and low life satisfaction.
Design and Method
Design and Sample
This is a cross-sectional study using administrative data.
Data from the Resident Assessment Instrument Minimum
Data Set (RAI-MDS, Version 2.0) and the Continuing
Care Information Management System were collected
between 2008 and 2011 in the Fraser Health region,
BC, Canada (accessible population). Fraser Health
operates 7,800 residential care beds and has systematic-
ally collected RAI-MDS data on residents since 2007.
The RAI-MDS has been rigorously tested for reliability
and validity in Canada and internationally (Hawes et al.,
1995; Lawton et al., 1998; Mor et al., 2003), enabling
comparison between countries and institutions. Trained
clinicians complete the MDS 2.0 upon resident admis-
sion and ideally every 3 months thereafter. It also is
completed if changes in health status are experienced
by residents. In this study, all measures were drawn
from assessments undertaken 90 days following admis-
sion to LTCFs.
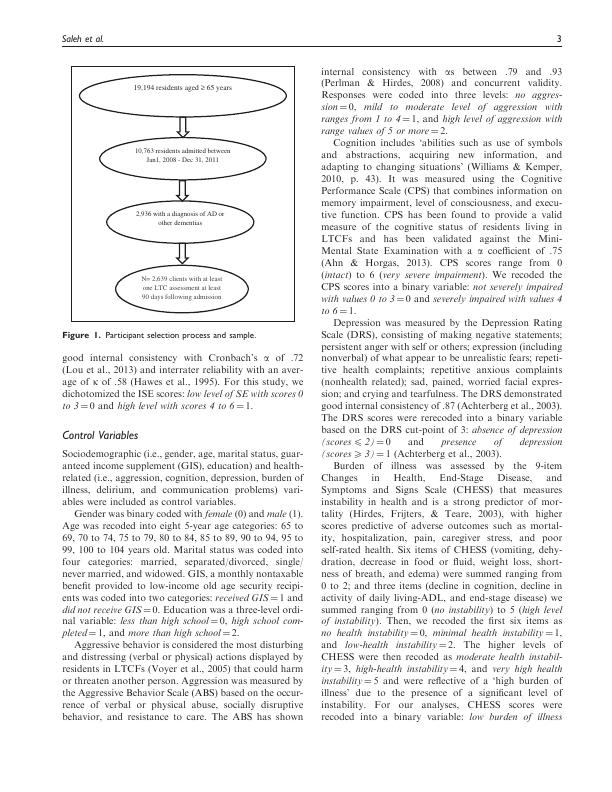
Our initial sample included 10,763 newly admitted
residents (from January 1, 2008, to December 31,
2011), aged 65 or older. The final study sample included
2,639 residents who upon admission or in their first full
or quarterly assessment had a diagnosis of dementia and
who had at least one LTC assessment within 90 days of
admission (Figure 1).
Dependent Variable
The dependent variable is antipsychotic use, which was
defined as the use of atypical and typical antipsychotic
agent(s). It was coded into a binary variable: did not
receive antipsychotic drugs ¼ 0 and received antipsychotics
(one drug at least once, regardless of the numbers of
drugs or days the drug is received) in the past 7 days
prior to the assessment date ¼ 1.
Independent Variable
The independent variable was SE, which within the
context of LTCFs, was defined as those who have ‘a
high sense of initiative and involvement and can respond
adequately to social stimuli in the social environment,
participate in social activities and interact with other
residents and staff’ (Achterberg et al., 2003, p. 213). SE
was measured using the Index of Social Engagement
(ISE), an observational scale that measures the positive
social behavior of residents. It includes six dichotomous
items reflecting whether the resident is at ease interacting
with others, with planned or structured activities, doing
self-initiated activities, establishing their own goals,
pursuing involvement in facility life, and accepting invi-
tations into most group activities. The ISE has shown
2 Canadian Journal of Nursing Research 0(0)
medical model focusing on treatment toward a social
model of care emphasizing a home-like environment.
Moreover, the culture change movement in LTCFs,
based on the philosophy of person-centered care, focuses
on well-being and quality of life as defined by the resi-
dent. However, the prevalence of antipsychotic use in
LTCFs remains high (Fischer, Cohen, Forrest,
Schweizer, & Wasylenki, 2011), mainly to address the
behavioral and psychological symptoms of dementia
(BPSD) that include aggression, agitation, restlessness,
wandering, hoarding, sleep disturbances, psychosis,
delusions, hallucinations, and sundowning
(Cohen-Mansfield, Marx, & Rosenthal, 1989).
Recently, British Columbia (BC) Ministry of Health
reviewed antipsychotic use in LTCFs and recommended
its use for the treatment of BPSD under several condi-
tions (MoH, 2011). These conditions include weighing
the risks against the benefits, using those drugs as a
last resort, obtaining informed consent prior to use,
and following the clinical guidelines of a low dose,
slow titration, and over a short period with close moni-
toring. Yet, the review illustrated that over half (50.3%)
of the residents were prescribed antipsychotics between
April 2010 and June 2011, an increase of 37% within a
decade (MoH, 2011), with similar increases reported
across Canadian health authorities. While newly
admitted residents are more likely than other residents
to be prescribed at least one antipsychotic during the first
90 days of admission (Huybrechts, Rothman, Silliman,
Brookhart, & Schneeweiss, 2011), antipsychotic use can
be as twice as high in residents with BPSD (Alanen,
Finne-Soveri, Noro, & Leinonen, 2006). Antipsychotic
use in older adults, particularly with dementia, is asso-
ciated with multiple side effects (Perucca & Gilliam,
2012) such as increased risks of mortality, falls, and
hip fractures. Furthermore, antipsychotics may worsen
cognition and increase sedative load (Perucca & Gilliam,
2012) that, in turn, may reduce the level of social engage-
ment (SE).
SE is considered essential to the psychological and
physical well-being (Bennett, 2002) of older adults in
LTCFs due to challenges within the setting in keeping
older adults active and stimulated. Scholars have pro-
posed that SE might be an alternative to antipsychotics
use (Mallidou, Oliveira, & Borycki, 2013). Socially enga-
ging residents has positive health outcomes, such as a
protective effect on mortality (Bennett, 2002; Kiely,
Simon, Jones, & Morris, 2000), and improved function
and cognition (Chen et al., 2013). SE is also associated
with decreased symptoms of depression (Lou, Chi,
Kwan, & Leung, 2013) and is an indicator of quality of
life, as it relates to positive emotions, sense of purpose,
and life satisfaction. Conversely, lonely older adults
often have low self-rated health and low life satisfaction.
Design and Method
Design and Sample
This is a cross-sectional study using administrative data.
Data from the Resident Assessment Instrument Minimum
Data Set (RAI-MDS, Version 2.0) and the Continuing
Care Information Management System were collected
between 2008 and 2011 in the Fraser Health region,
BC, Canada (accessible population). Fraser Health
operates 7,800 residential care beds and has systematic-
ally collected RAI-MDS data on residents since 2007.
The RAI-MDS has been rigorously tested for reliability
and validity in Canada and internationally (Hawes et al.,
1995; Lawton et al., 1998; Mor et al., 2003), enabling
comparison between countries and institutions. Trained
clinicians complete the MDS 2.0 upon resident admis-
sion and ideally every 3 months thereafter. It also is
completed if changes in health status are experienced
by residents. In this study, all measures were drawn
from assessments undertaken 90 days following admis-
sion to LTCFs.
Our initial sample included 10,763 newly admitted
residents (from January 1, 2008, to December 31,
2011), aged 65 or older. The final study sample included
2,639 residents who upon admission or in their first full
or quarterly assessment had a diagnosis of dementia and
who had at least one LTC assessment within 90 days of
admission (Figure 1).
Dependent Variable
The dependent variable is antipsychotic use, which was
defined as the use of atypical and typical antipsychotic
agent(s). It was coded into a binary variable: did not
receive antipsychotic drugs ¼ 0 and received antipsychotics
(one drug at least once, regardless of the numbers of
drugs or days the drug is received) in the past 7 days
prior to the assessment date ¼ 1.
Independent Variable
The independent variable was SE, which within the
context of LTCFs, was defined as those who have ‘a
high sense of initiative and involvement and can respond
adequately to social stimuli in the social environment,
participate in social activities and interact with other
residents and staff’ (Achterberg et al., 2003, p. 213). SE
was measured using the Index of Social Engagement
(ISE), an observational scale that measures the positive
social behavior of residents. It includes six dichotomous
items reflecting whether the resident is at ease interacting
with others, with planned or structured activities, doing
self-initiated activities, establishing their own goals,
pursuing involvement in facility life, and accepting invi-
tations into most group activities. The ISE has shown
2 Canadian Journal of Nursing Research 0(0)

good internal consistency with Cronbach’s a of .72
(Lou et al., 2013) and interrater reliability with an aver-
age of k of .58 (Hawes et al., 1995). For this study, we
dichotomized the ISE scores: low level of SE with scores 0
to 3 ¼ 0 and high level with scores 4 to 6 ¼ 1.
Control Variables
Sociodemographic (i.e., gender, age, marital status, guar-
anteed income supplement (GIS), education) and health-
related (i.e., aggression, cognition, depression, burden of
illness, delirium, and communication problems) vari-
ables were included as control variables.
Gender was binary coded with female (0) and male (1).
Age was recoded into eight 5-year age categories: 65 to
69, 70 to 74, 75 to 79, 80 to 84, 85 to 89, 90 to 94, 95 to
99, 100 to 104 years old. Marital status was coded into
four categories: married, separated/divorced, single/
never married, and widowed. GIS, a monthly nontaxable
benefit provided to low-income old age security recipi-
ents was coded into two categories: received GIS ¼ 1 and
did not receive GIS ¼ 0. Education was a three-level ordi-
nal variable: less than high school ¼ 0, high school com-
pleted ¼ 1, and more than high school ¼ 2.
Aggressive behavior is considered the most disturbing
and distressing (verbal or physical) actions displayed by
residents in LTCFs (Voyer et al., 2005) that could harm
or threaten another person. Aggression was measured by
the Aggressive Behavior Scale (ABS) based on the occur-
rence of verbal or physical abuse, socially disruptive
behavior, and resistance to care. The ABS has shown
internal consistency with as between .79 and .93
(Perlman & Hirdes, 2008) and concurrent validity.
Responses were coded into three levels: no aggres-
sion ¼ 0, mild to moderate level of aggression with
ranges from 1 to 4 ¼ 1, and high level of aggression with
range values of 5 or more ¼ 2.
Cognition includes ‘abilities such as use of symbols
and abstractions, acquiring new information, and
adapting to changing situations’ (Williams & Kemper,
2010, p. 43). It was measured using the Cognitive
Performance Scale (CPS) that combines information on
memory impairment, level of consciousness, and execu-
tive function. CPS has been found to provide a valid
measure of the cognitive status of residents living in
LTCFs and has been validated against the Mini-
Mental State Examination with a a coefficient of .75
(Ahn & Horgas, 2013). CPS scores range from 0
(intact) to 6 (very severe impairment). We recoded the
CPS scores into a binary variable: not severely impaired
with values 0 to 3 ¼ 0 and severely impaired with values 4
to 6 ¼ 1.
Depression was measured by the Depression Rating
Scale (DRS), consisting of making negative statements;
persistent anger with self or others; expression (including
nonverbal) of what appear to be unrealistic fears; repeti-
tive health complaints; repetitive anxious complaints
(nonhealth related); sad, pained, worried facial expres-
sion; and crying and tearfulness. The DRS demonstrated
good internal consistency of .87 (Achterberg et al., 2003).
The DRS scores were rerecoded into a binary variable
based on the DRS cut-point of 3: absence of depression
(scores 4 2) ¼ 0 and presence of depression
(scores 5 3) ¼ 1 (Achterberg et al., 2003).
Burden of illness was assessed by the 9-item
Changes in Health, End-Stage Disease, and
Symptoms and Signs Scale (CHESS) that measures
instability in health and is a strong predictor of mor-
tality (Hirdes, Frijters, & Teare, 2003), with higher
scores predictive of adverse outcomes such as mortal-
ity, hospitalization, pain, caregiver stress, and poor
self-rated health. Six items of CHESS (vomiting, dehy-
dration, decrease in food or fluid, weight loss, short-
ness of breath, and edema) were summed ranging from
0 to 2; and three items (decline in cognition, decline in
activity of daily living-ADL, and end-stage disease) we
summed ranging from 0 (no instability) to 5 (high level
of instability). Then, we recoded the first six items as
no health instability ¼ 0, minimal health instability ¼ 1,
and low-health instability ¼ 2. The higher levels of
CHESS were then recoded as moderate health instabil-
ity ¼ 3, high-health instability ¼ 4, and very high health
instability ¼ 5 and were reflective of a ‘high burden of
illness’ due to the presence of a significant level of
instability. For our analyses, CHESS scores were
recoded into a binary variable: low burden of illness
19,194 residents aged ≥ 65 years
10,763 residents admitted between
Jan1, 2008 - Dec 31, 2011
2,936 with a diagnosis of AD or
other dementias
N= 2,639 clients with at least
one LTC assessment at least
90 days following admission
Figure 1. Participant selection process and sample.
Saleh et al. 3
(Lou et al., 2013) and interrater reliability with an aver-
age of k of .58 (Hawes et al., 1995). For this study, we
dichotomized the ISE scores: low level of SE with scores 0
to 3 ¼ 0 and high level with scores 4 to 6 ¼ 1.
Control Variables
Sociodemographic (i.e., gender, age, marital status, guar-
anteed income supplement (GIS), education) and health-
related (i.e., aggression, cognition, depression, burden of
illness, delirium, and communication problems) vari-
ables were included as control variables.
Gender was binary coded with female (0) and male (1).
Age was recoded into eight 5-year age categories: 65 to
69, 70 to 74, 75 to 79, 80 to 84, 85 to 89, 90 to 94, 95 to
99, 100 to 104 years old. Marital status was coded into
four categories: married, separated/divorced, single/
never married, and widowed. GIS, a monthly nontaxable
benefit provided to low-income old age security recipi-
ents was coded into two categories: received GIS ¼ 1 and
did not receive GIS ¼ 0. Education was a three-level ordi-
nal variable: less than high school ¼ 0, high school com-
pleted ¼ 1, and more than high school ¼ 2.
Aggressive behavior is considered the most disturbing
and distressing (verbal or physical) actions displayed by
residents in LTCFs (Voyer et al., 2005) that could harm
or threaten another person. Aggression was measured by
the Aggressive Behavior Scale (ABS) based on the occur-
rence of verbal or physical abuse, socially disruptive
behavior, and resistance to care. The ABS has shown
internal consistency with as between .79 and .93
(Perlman & Hirdes, 2008) and concurrent validity.
Responses were coded into three levels: no aggres-
sion ¼ 0, mild to moderate level of aggression with
ranges from 1 to 4 ¼ 1, and high level of aggression with
range values of 5 or more ¼ 2.
Cognition includes ‘abilities such as use of symbols
and abstractions, acquiring new information, and
adapting to changing situations’ (Williams & Kemper,
2010, p. 43). It was measured using the Cognitive
Performance Scale (CPS) that combines information on
memory impairment, level of consciousness, and execu-
tive function. CPS has been found to provide a valid
measure of the cognitive status of residents living in
LTCFs and has been validated against the Mini-
Mental State Examination with a a coefficient of .75
(Ahn & Horgas, 2013). CPS scores range from 0
(intact) to 6 (very severe impairment). We recoded the
CPS scores into a binary variable: not severely impaired
with values 0 to 3 ¼ 0 and severely impaired with values 4
to 6 ¼ 1.
Depression was measured by the Depression Rating
Scale (DRS), consisting of making negative statements;
persistent anger with self or others; expression (including
nonverbal) of what appear to be unrealistic fears; repeti-
tive health complaints; repetitive anxious complaints
(nonhealth related); sad, pained, worried facial expres-
sion; and crying and tearfulness. The DRS demonstrated
good internal consistency of .87 (Achterberg et al., 2003).
The DRS scores were rerecoded into a binary variable
based on the DRS cut-point of 3: absence of depression
(scores 4 2) ¼ 0 and presence of depression
(scores 5 3) ¼ 1 (Achterberg et al., 2003).
Burden of illness was assessed by the 9-item
Changes in Health, End-Stage Disease, and
Symptoms and Signs Scale (CHESS) that measures
instability in health and is a strong predictor of mor-
tality (Hirdes, Frijters, & Teare, 2003), with higher
scores predictive of adverse outcomes such as mortal-
ity, hospitalization, pain, caregiver stress, and poor
self-rated health. Six items of CHESS (vomiting, dehy-
dration, decrease in food or fluid, weight loss, short-
ness of breath, and edema) were summed ranging from
0 to 2; and three items (decline in cognition, decline in
activity of daily living-ADL, and end-stage disease) we
summed ranging from 0 (no instability) to 5 (high level
of instability). Then, we recoded the first six items as
no health instability ¼ 0, minimal health instability ¼ 1,
and low-health instability ¼ 2. The higher levels of
CHESS were then recoded as moderate health instabil-
ity ¼ 3, high-health instability ¼ 4, and very high health
instability ¼ 5 and were reflective of a ‘high burden of
illness’ due to the presence of a significant level of
instability. For our analyses, CHESS scores were
recoded into a binary variable: low burden of illness
19,194 residents aged ≥ 65 years
10,763 residents admitted between
Jan1, 2008 - Dec 31, 2011
2,936 with a diagnosis of AD or
other dementias
N= 2,639 clients with at least
one LTC assessment at least
90 days following admission
Figure 1. Participant selection process and sample.
Saleh et al. 3
End of preview
Want to access all the pages? Upload your documents or become a member.
Related Documents
Social Engagement and Antipsychotic Use in Addressing the Behavioral and Psychological Symptoms of Dementia in Long-Term Care Facilitieslg...
|5
|850
|468
