2804NRS Case Study: Analyzing Spinal Cord Compression in a 75-Year-Old
VerifiedAdded on 2023/06/13
|3
|1347
|377
Case Study
AI Summary
This assignment presents a detailed case study analysis of Wilma, a 75-year-old woman diagnosed with spinal cord compression due to osteoporotic spinal compression fractures of T5-T6. The analysis includes a concept map outlining the relationships between risk factors (age, gender, menopause, tr...
Decline in calcium and
oestrogen levels
Lowered bone density leading to
osteoporosis
Vertebral bone
fracture
occurrence
Tissue compression
Pathophysiology
Risk Factors
Aetiology
Clinical
manifestations
Diagnostic tests
Treatment
Gender
Age
Reduced bowel
movement
spinal cord
compression on
fractures of T5-T6.
Increased tenderness
on the t5-t6
Urinalysis
assessment
Admission of
verterbroplasty
Urinary Incontinence
Elevated blood pressure
Apoptosis on the nerves and
thoracic borne
Decline sensation on the feet
Paralysis of limbs
Reduced sensory
and motor signal on
lower extremities
Menopause
status
Administration of NSAIDs
X- ray and spine MRI admission
Bone density
medication
Surgical management
Urinary and faecal
incontinence
Burning pain sensation
MRI scan
Key
Trauma
Examination of blood
pressure and medication
application
Fall
Administration of
oral laxatives
Neuro Vascular
Assessments Administration of
Analgesia
Concept map of spinal cord
compression
oestrogen levels
Lowered bone density leading to
osteoporosis
Vertebral bone
fracture
occurrence
Tissue compression
Pathophysiology
Risk Factors
Aetiology
Clinical
manifestations
Diagnostic tests
Treatment
Gender
Age
Reduced bowel
movement
spinal cord
compression on
fractures of T5-T6.
Increased tenderness
on the t5-t6
Urinalysis
assessment
Admission of
verterbroplasty
Urinary Incontinence
Elevated blood pressure
Apoptosis on the nerves and
thoracic borne
Decline sensation on the feet
Paralysis of limbs
Reduced sensory
and motor signal on
lower extremities
Menopause
status
Administration of NSAIDs
X- ray and spine MRI admission
Bone density
medication
Surgical management
Urinary and faecal
incontinence
Burning pain sensation
MRI scan
Key
Trauma
Examination of blood
pressure and medication
application
Fall
Administration of
oral laxatives
Neuro Vascular
Assessments Administration of
Analgesia
Concept map of spinal cord
compression
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
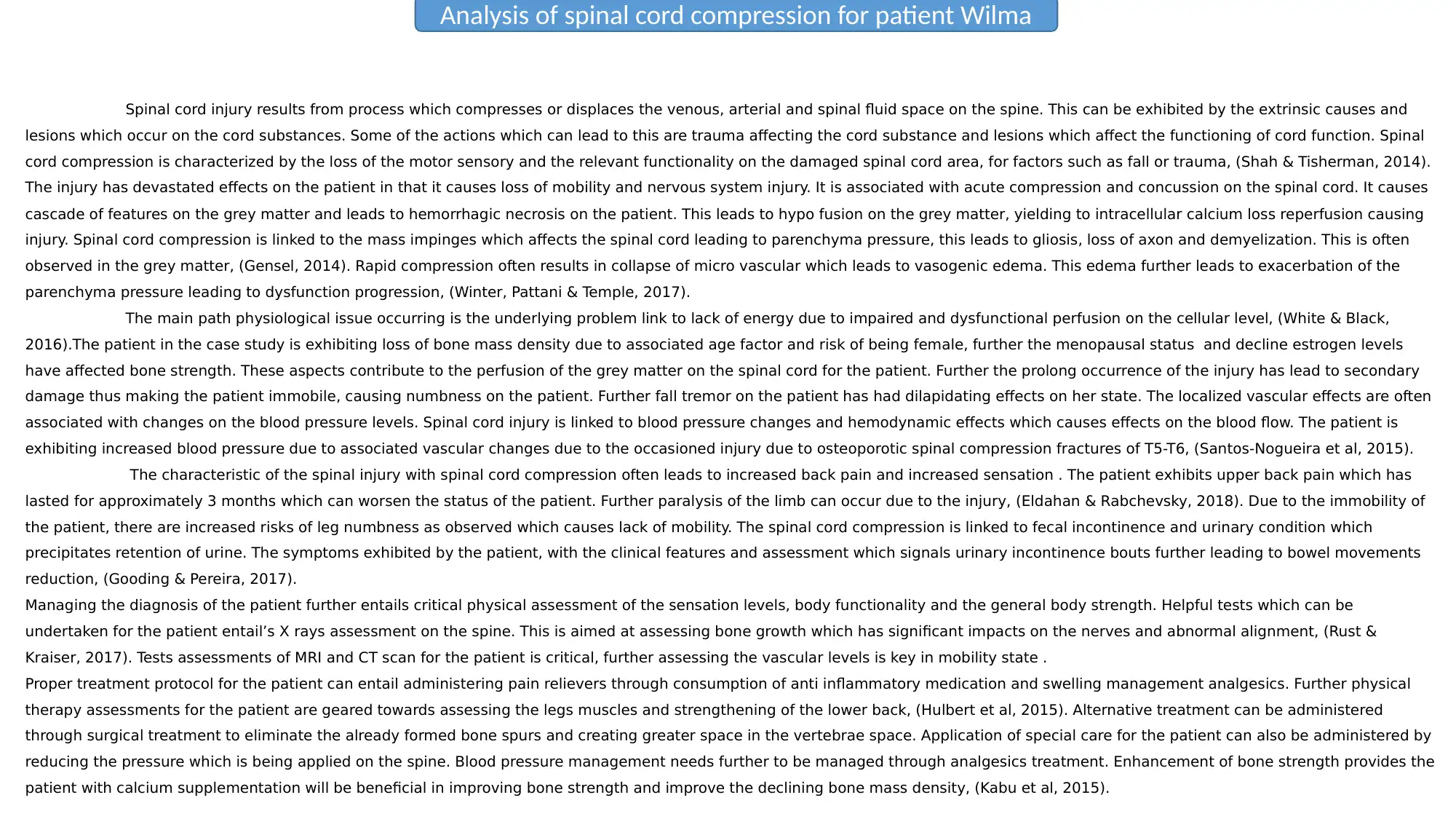
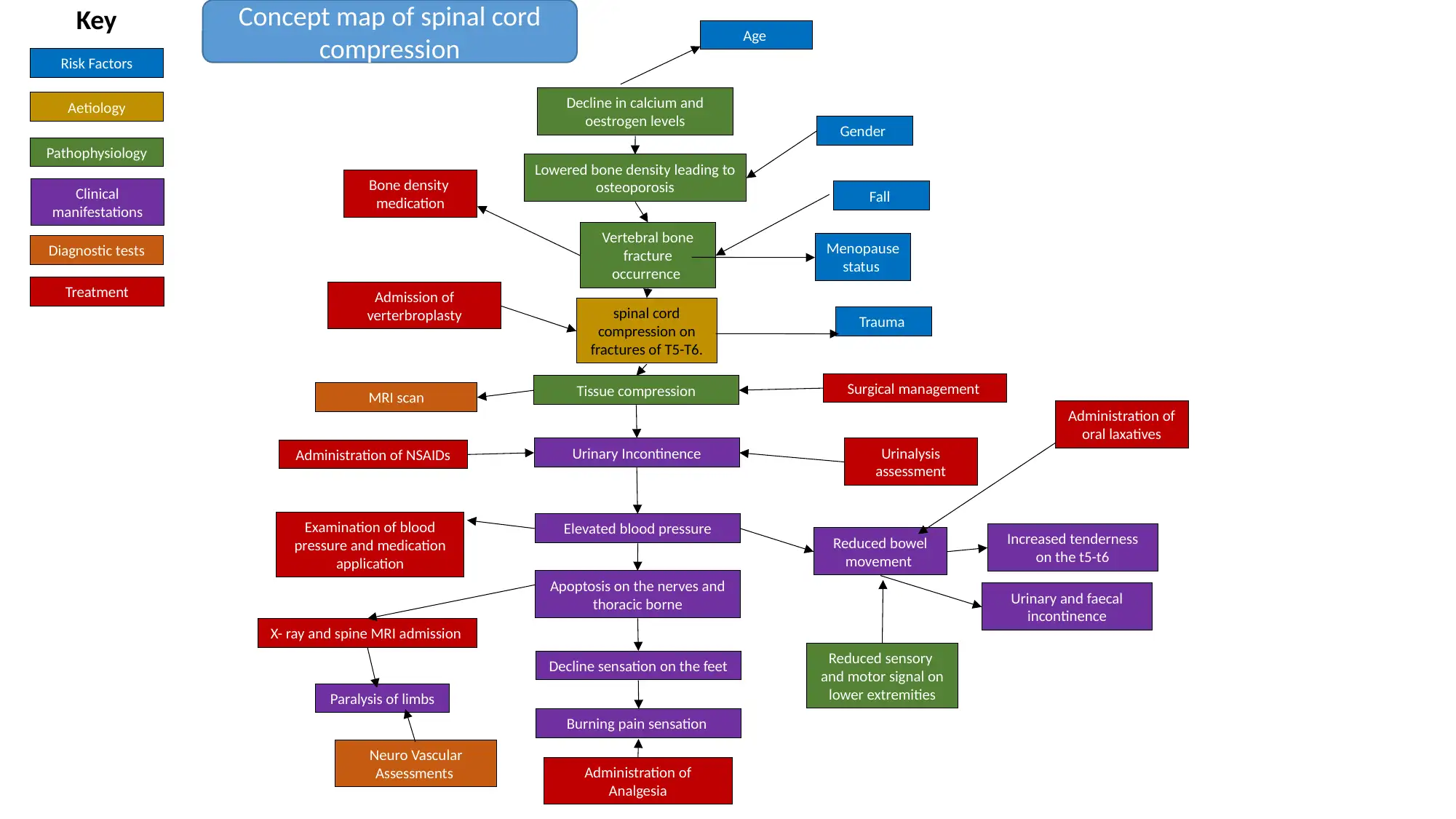
Spinal cord injury results from process which compresses or displaces the venous, arterial and spinal fluid space on the spine. This can be exhibited by the extrinsic causes and
lesions which occur on the cord substances. Some of the actions which can lead to this are trauma affecting the cord substance and lesions which affect the functioning of cord function. Spinal
cord compression is characterized by the loss of the motor sensory and the relevant functionality on the damaged spinal cord area, for factors such as fall or trauma, (Shah & Tisherman, 2014).
The injury has devastated effects on the patient in that it causes loss of mobility and nervous system injury. It is associated with acute compression and concussion on the spinal cord. It causes
cascade of features on the grey matter and leads to hemorrhagic necrosis on the patient. This leads to hypo fusion on the grey matter, yielding to intracellular calcium loss reperfusion causing
injury. Spinal cord compression is linked to the mass impinges which affects the spinal cord leading to parenchyma pressure, this leads to gliosis, loss of axon and demyelization. This is often
observed in the grey matter, (Gensel, 2014). Rapid compression often results in collapse of micro vascular which leads to vasogenic edema. This edema further leads to exacerbation of the
parenchyma pressure leading to dysfunction progression, (Winter, Pattani & Temple, 2017).
The main path physiological issue occurring is the underlying problem link to lack of energy due to impaired and dysfunctional perfusion on the cellular level, (White & Black,
2016).The patient in the case study is exhibiting loss of bone mass density due to associated age factor and risk of being female, further the menopausal status and decline estrogen levels
have affected bone strength. These aspects contribute to the perfusion of the grey matter on the spinal cord for the patient. Further the prolong occurrence of the injury has lead to secondary
damage thus making the patient immobile, causing numbness on the patient. Further fall tremor on the patient has had dilapidating effects on her state. The localized vascular effects are often
associated with changes on the blood pressure levels. Spinal cord injury is linked to blood pressure changes and hemodynamic effects which causes effects on the blood flow. The patient is
exhibiting increased blood pressure due to associated vascular changes due to the occasioned injury due to osteoporotic spinal compression fractures of T5-T6, (Santos-Nogueira et al, 2015).
The characteristic of the spinal injury with spinal cord compression often leads to increased back pain and increased sensation . The patient exhibits upper back pain which has
lasted for approximately 3 months which can worsen the status of the patient. Further paralysis of the limb can occur due to the injury, (Eldahan & Rabchevsky, 2018). Due to the immobility of
the patient, there are increased risks of leg numbness as observed which causes lack of mobility. The spinal cord compression is linked to fecal incontinence and urinary condition which
precipitates retention of urine. The symptoms exhibited by the patient, with the clinical features and assessment which signals urinary incontinence bouts further leading to bowel movements
reduction, (Gooding & Pereira, 2017).
Managing the diagnosis of the patient further entails critical physical assessment of the sensation levels, body functionality and the general body strength. Helpful tests which can be
undertaken for the patient entail’s X rays assessment on the spine. This is aimed at assessing bone growth which has significant impacts on the nerves and abnormal alignment, (Rust &
Kraiser, 2017). Tests assessments of MRI and CT scan for the patient is critical, further assessing the vascular levels is key in mobility state .
Proper treatment protocol for the patient can entail administering pain relievers through consumption of anti inflammatory medication and swelling management analgesics. Further physical
therapy assessments for the patient are geared towards assessing the legs muscles and strengthening of the lower back, (Hulbert et al, 2015). Alternative treatment can be administered
through surgical treatment to eliminate the already formed bone spurs and creating greater space in the vertebrae space. Application of special care for the patient can also be administered by
reducing the pressure which is being applied on the spine. Blood pressure management needs further to be managed through analgesics treatment. Enhancement of bone strength provides the
patient with calcium supplementation will be beneficial in improving bone strength and improve the declining bone mass density, (Kabu et al, 2015).
Analysis of spinal cord compression for patient Wilma
lesions which occur on the cord substances. Some of the actions which can lead to this are trauma affecting the cord substance and lesions which affect the functioning of cord function. Spinal
cord compression is characterized by the loss of the motor sensory and the relevant functionality on the damaged spinal cord area, for factors such as fall or trauma, (Shah & Tisherman, 2014).
The injury has devastated effects on the patient in that it causes loss of mobility and nervous system injury. It is associated with acute compression and concussion on the spinal cord. It causes
cascade of features on the grey matter and leads to hemorrhagic necrosis on the patient. This leads to hypo fusion on the grey matter, yielding to intracellular calcium loss reperfusion causing
injury. Spinal cord compression is linked to the mass impinges which affects the spinal cord leading to parenchyma pressure, this leads to gliosis, loss of axon and demyelization. This is often
observed in the grey matter, (Gensel, 2014). Rapid compression often results in collapse of micro vascular which leads to vasogenic edema. This edema further leads to exacerbation of the
parenchyma pressure leading to dysfunction progression, (Winter, Pattani & Temple, 2017).
The main path physiological issue occurring is the underlying problem link to lack of energy due to impaired and dysfunctional perfusion on the cellular level, (White & Black,
2016).The patient in the case study is exhibiting loss of bone mass density due to associated age factor and risk of being female, further the menopausal status and decline estrogen levels
have affected bone strength. These aspects contribute to the perfusion of the grey matter on the spinal cord for the patient. Further the prolong occurrence of the injury has lead to secondary
damage thus making the patient immobile, causing numbness on the patient. Further fall tremor on the patient has had dilapidating effects on her state. The localized vascular effects are often
associated with changes on the blood pressure levels. Spinal cord injury is linked to blood pressure changes and hemodynamic effects which causes effects on the blood flow. The patient is
exhibiting increased blood pressure due to associated vascular changes due to the occasioned injury due to osteoporotic spinal compression fractures of T5-T6, (Santos-Nogueira et al, 2015).
The characteristic of the spinal injury with spinal cord compression often leads to increased back pain and increased sensation . The patient exhibits upper back pain which has
lasted for approximately 3 months which can worsen the status of the patient. Further paralysis of the limb can occur due to the injury, (Eldahan & Rabchevsky, 2018). Due to the immobility of
the patient, there are increased risks of leg numbness as observed which causes lack of mobility. The spinal cord compression is linked to fecal incontinence and urinary condition which
precipitates retention of urine. The symptoms exhibited by the patient, with the clinical features and assessment which signals urinary incontinence bouts further leading to bowel movements
reduction, (Gooding & Pereira, 2017).
Managing the diagnosis of the patient further entails critical physical assessment of the sensation levels, body functionality and the general body strength. Helpful tests which can be
undertaken for the patient entail’s X rays assessment on the spine. This is aimed at assessing bone growth which has significant impacts on the nerves and abnormal alignment, (Rust &
Kraiser, 2017). Tests assessments of MRI and CT scan for the patient is critical, further assessing the vascular levels is key in mobility state .
Proper treatment protocol for the patient can entail administering pain relievers through consumption of anti inflammatory medication and swelling management analgesics. Further physical
therapy assessments for the patient are geared towards assessing the legs muscles and strengthening of the lower back, (Hulbert et al, 2015). Alternative treatment can be administered
through surgical treatment to eliminate the already formed bone spurs and creating greater space in the vertebrae space. Application of special care for the patient can also be administered by
reducing the pressure which is being applied on the spine. Blood pressure management needs further to be managed through analgesics treatment. Enhancement of bone strength provides the
patient with calcium supplementation will be beneficial in improving bone strength and improve the declining bone mass density, (Kabu et al, 2015).
Analysis of spinal cord compression for patient Wilma
Eldahan, K. C., & Rabchevsky, A. G. (2018). Autonomic dysreflexia after spinal cord injury: Systemic
pathophysiology and methods of management. Autonomic Neuroscience: Basic and Clinical, 209, 59-
70.
Gensel, J. C. (2014). Spinal cord injury. Neuroinflammation and CNS disorders, 339-361.
Gooding, M., & Pereira, L. (2017). Spinal cord injury. Maternal-Fetal Evidence Based Guidelines.
Hurlbert, R. J., Hadley, M. N., Walters, B. C., Aarabi, B., Dhall, S. S., Gelb, D. E., ... & Theodore, N. (2015).
Pharmacological therapy for acute spinal cord injury. Neurosurgery, 76(suppl_1), S71-S83.
Kabu, S., Gao, Y., Kwon, B. K., & Labhasetwar, V. (2015). Drug delivery, cell-based therapies, and tissue
engineering approaches for spinal cord injury. Journal of Controlled Release, 219, 141-154.
Rust, R., & Kaiser, J. (2017). Insights into the dual role of inflammation after spinal cord injury. Journal of
Neuroscience, 37(18), 4658-4660.
Santos-Nogueira, E., López-Serrano, C., Hernández, J., Lago, N., Astudillo, A. M., Balsinde, J., ... & López-
Vales, R. (2015). Activation of lysophosphatidic acid receptor type 1 contributes to pathophysiology of
spinal cord injury. Journal of Neuroscience, 35(28), 10224-10235.
Shah, R. R., & Tisherman, S. A. (2014). Spinal cord injury. In Imaging the ICU Patient (pp. 377-380). Springer,
London.
White, N. H., & Black, N. H. (2016). Spinal cord injury (SCI) facts and figures at a glance. National spinal cord
injury statistical center, facts and figures at a glance.
Winter, B., Pattani, H., & Temple, E. (2017). Spinal cord injury. Anaesthesia & Intensive Care Medicine, 18(8),
404-409.
Reference list
pathophysiology and methods of management. Autonomic Neuroscience: Basic and Clinical, 209, 59-
70.
Gensel, J. C. (2014). Spinal cord injury. Neuroinflammation and CNS disorders, 339-361.
Gooding, M., & Pereira, L. (2017). Spinal cord injury. Maternal-Fetal Evidence Based Guidelines.
Hurlbert, R. J., Hadley, M. N., Walters, B. C., Aarabi, B., Dhall, S. S., Gelb, D. E., ... & Theodore, N. (2015).
Pharmacological therapy for acute spinal cord injury. Neurosurgery, 76(suppl_1), S71-S83.
Kabu, S., Gao, Y., Kwon, B. K., & Labhasetwar, V. (2015). Drug delivery, cell-based therapies, and tissue
engineering approaches for spinal cord injury. Journal of Controlled Release, 219, 141-154.
Rust, R., & Kaiser, J. (2017). Insights into the dual role of inflammation after spinal cord injury. Journal of
Neuroscience, 37(18), 4658-4660.
Santos-Nogueira, E., López-Serrano, C., Hernández, J., Lago, N., Astudillo, A. M., Balsinde, J., ... & López-
Vales, R. (2015). Activation of lysophosphatidic acid receptor type 1 contributes to pathophysiology of
spinal cord injury. Journal of Neuroscience, 35(28), 10224-10235.
Shah, R. R., & Tisherman, S. A. (2014). Spinal cord injury. In Imaging the ICU Patient (pp. 377-380). Springer,
London.
White, N. H., & Black, N. H. (2016). Spinal cord injury (SCI) facts and figures at a glance. National spinal cord
injury statistical center, facts and figures at a glance.
Winter, B., Pattani, H., & Temple, E. (2017). Spinal cord injury. Anaesthesia & Intensive Care Medicine, 18(8),
404-409.
Reference list
You're viewing a preview
Unlock full access by subscribing today!
1 out of 3
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




