abrupt exacerbation of COPD
VerifiedAdded on 2022/01/17
|7
|1931
|110
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Student Name
Student Id
Student Id
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Patient scenario
June, a woman who is 75 years old, experienced an abrupt exacerbation of COPD. Last night
was her first hospital admission since she got diagnosed. An individual with COPD may suffer
from a lot severe symptoms than the typical time. This is referred to as an acute exacerbation.
This necessitates medical assistance in a hospital. COPD patients get exacerbations on
averagely 0.85 to 1.3 times per year. Chronic pulmonary obstructive disease (COPD) refers to a
chronic inflammatory pulmonary illness that leads to blocked airflow to and from the lungs.
Indications are trouble breathing, coughing, mucus production (sputum), as well as wheezing. It
is usually a result of long-term exposure to gasses or particulates, and most frequently smoke
from cigarettes. (Miravitlles and Ribera, 2017) The chance of getting a cardiac illness, lung
cancer, and many other diseases is raised for those with COPD.
Understanding of the patient scenario
Chronic bronchitis results from bronchial liner irritation, which carries air from as well as to the
pulmonary bags (alveoli). It is distinguished by daily cough production as well as mucous.
Emphysema refers to a situation in which the alveoli degrade the smoke from cigarettes
and other irritant gasses and particle matter at the base of the (bronchioles of the lungs).
Typically, COPD symptoms do not show until considerable lung problems happen and typically
increase with time, especially in continuing exposure to cigarette smoke. COPD common
symptoms could consist of: a shortage of breath, particularly during strenuous activity, chest
tension, A persistent cough that can result in clear, white, yellow and greenish sputum, frequent
air infections, energy shortage, unintended weight loss and Ankle, foot, or leg inflammation.
Episodes known as recurrences will also probably occur in individuals with COPD who are even
worse than the typical everyday change and last for at least a few days (Perera et al., 2007).
June shows most of these symptoms. She is Expecting copious amounts of green sputum, and her
auscultation shows coarse crackles throughout, which is an indicator of difficulties breathing; she
is also only taking shallow apical breaths and using her accessory muscles at rest. She is
therefore experiencing an exacerbation.
Tobacco smoking remains the principal cause of COPD in industrialised nations. COPD
commonly occurs in persons exposed to gases caused by combustion fuel for cooking as well
June, a woman who is 75 years old, experienced an abrupt exacerbation of COPD. Last night
was her first hospital admission since she got diagnosed. An individual with COPD may suffer
from a lot severe symptoms than the typical time. This is referred to as an acute exacerbation.
This necessitates medical assistance in a hospital. COPD patients get exacerbations on
averagely 0.85 to 1.3 times per year. Chronic pulmonary obstructive disease (COPD) refers to a
chronic inflammatory pulmonary illness that leads to blocked airflow to and from the lungs.
Indications are trouble breathing, coughing, mucus production (sputum), as well as wheezing. It
is usually a result of long-term exposure to gasses or particulates, and most frequently smoke
from cigarettes. (Miravitlles and Ribera, 2017) The chance of getting a cardiac illness, lung
cancer, and many other diseases is raised for those with COPD.
Understanding of the patient scenario
Chronic bronchitis results from bronchial liner irritation, which carries air from as well as to the
pulmonary bags (alveoli). It is distinguished by daily cough production as well as mucous.
Emphysema refers to a situation in which the alveoli degrade the smoke from cigarettes
and other irritant gasses and particle matter at the base of the (bronchioles of the lungs).
Typically, COPD symptoms do not show until considerable lung problems happen and typically
increase with time, especially in continuing exposure to cigarette smoke. COPD common
symptoms could consist of: a shortage of breath, particularly during strenuous activity, chest
tension, A persistent cough that can result in clear, white, yellow and greenish sputum, frequent
air infections, energy shortage, unintended weight loss and Ankle, foot, or leg inflammation.
Episodes known as recurrences will also probably occur in individuals with COPD who are even
worse than the typical everyday change and last for at least a few days (Perera et al., 2007).
June shows most of these symptoms. She is Expecting copious amounts of green sputum, and her
auscultation shows coarse crackles throughout, which is an indicator of difficulties breathing; she
is also only taking shallow apical breaths and using her accessory muscles at rest. She is
therefore experiencing an exacerbation.
Tobacco smoking remains the principal cause of COPD in industrialised nations. COPD
commonly occurs in persons exposed to gases caused by combustion fuel for cooking as well
as heating in inadequately aired dwellings in underdeveloped countries. Clinically evident COPD
are produced only by some chronic smokers; however, numerous smokers with extensive
smoking records might have worse lung function (Miravitlles and Ribera, 2017). Many smokers
are experiencing less prevalent lung problems. Until the further assessment is carried out, they
might be misdiagnosed as having COPD.
Physiotherapist impact on COPD patient
Physiotherapists run programmes called pulmonary rehabilitation. The interdisciplinary program
for the treatment of chronic lung disease sufferers, pulmonary rehabilitation, has its main
objective: to improve patients' social and physical conditions. It is tailored individually (Kurzaj
et al., 2013). The pulmonary rehabilitation framework is characterised by physiotherapy (PT),
which enhances exercise endurance, agility, decreases dyspnea, enhances the standard of living
via several physical therapy and respiratory methods.
Through lowering shortness of breath, Lung rehabilitation courses offering means of curing the
condition, then enhancing the patient's capability for everyday tasks, such as bathing or dressing,
enhance the patient's well-being substantially. Improved health results in a better quality of life
as well as less relapse and readmission in hospitals. Physiotherapy shows one breathing method
if one tends to hyperventilate (respire too rapidly) or have trouble emptying the phlegm from the
chest area.
Physiotherapy likewise assists patients in the management of COPD dyspnea. You may employ
posture as well as respiratory workouts, advise one on how to progress and show the patient how
to cope. When an individual suffering from COPD has breathing issues in the hospital,
physiotherapy is essential as it helps him or her clean his or her chest, manages their lung,
and moves (Hilde et al., 2013). Physios can also assist patients with COPD to come back from
the hospital once they are ill and to manage future outbreaks.
A clear focus: exercise training
The main component of pulmonary rehabilitation remains to be exercise training. It decreases
the idleness and deconditioning symptoms, leading to less respiration shortage and enhanced
exercise capacity. Physical restrictions, nevertheless, might restrict the sorts of workouts that
could be employed. Aerobic exercise and strength training in persons with lung disease are
are produced only by some chronic smokers; however, numerous smokers with extensive
smoking records might have worse lung function (Miravitlles and Ribera, 2017). Many smokers
are experiencing less prevalent lung problems. Until the further assessment is carried out, they
might be misdiagnosed as having COPD.
Physiotherapist impact on COPD patient
Physiotherapists run programmes called pulmonary rehabilitation. The interdisciplinary program
for the treatment of chronic lung disease sufferers, pulmonary rehabilitation, has its main
objective: to improve patients' social and physical conditions. It is tailored individually (Kurzaj
et al., 2013). The pulmonary rehabilitation framework is characterised by physiotherapy (PT),
which enhances exercise endurance, agility, decreases dyspnea, enhances the standard of living
via several physical therapy and respiratory methods.
Through lowering shortness of breath, Lung rehabilitation courses offering means of curing the
condition, then enhancing the patient's capability for everyday tasks, such as bathing or dressing,
enhance the patient's well-being substantially. Improved health results in a better quality of life
as well as less relapse and readmission in hospitals. Physiotherapy shows one breathing method
if one tends to hyperventilate (respire too rapidly) or have trouble emptying the phlegm from the
chest area.
Physiotherapy likewise assists patients in the management of COPD dyspnea. You may employ
posture as well as respiratory workouts, advise one on how to progress and show the patient how
to cope. When an individual suffering from COPD has breathing issues in the hospital,
physiotherapy is essential as it helps him or her clean his or her chest, manages their lung,
and moves (Hilde et al., 2013). Physios can also assist patients with COPD to come back from
the hospital once they are ill and to manage future outbreaks.
A clear focus: exercise training
The main component of pulmonary rehabilitation remains to be exercise training. It decreases
the idleness and deconditioning symptoms, leading to less respiration shortage and enhanced
exercise capacity. Physical restrictions, nevertheless, might restrict the sorts of workouts that
could be employed. Aerobic exercise and strength training in persons with lung disease are
both important elements of exercise. The workout centrepiece is the training of the legs. Since
walking is required for most everyday tasks, numerous rehabilitation programmes have it as
their preferred exercise method (often on a treadmill) (Hilde et al., 2013). Several folks
might want to practice on a stationary bicycle. The choice of a pleasant and satisfactory
workout increases the individual's desire to accept and be part over the long run.
Arms exercises also help patients with chronic lung illnesses who suffer difficulty breathing or
other problems in their usual everyday tasks, like hair washing. This is because chronic
respiratory illness can result in muscle loss, and part of the muscles of the shoulders is required
to breathe and move the hands. This training is essential. Arms exercises may strain these
muscles fast.
The rationale for exercise training for COPD patient
Various research papers have shown that benefits in exercise training include decreases of
inflammatory markers, like IL-8, and a rise in muscular activities, like peroxisomes with a
proliferator-activated 1-α receptor as well as irisin coactivator (McCarthy et al., 2015). Lastly,
training remains to be an economical operation and decreases the sum of hospitals
Various training methods were suggested for optimisation of exercise tolerance and
maximisation of training benefits in COPD patients. However, the most efficient methods of
practice still are unknown. Recommendations include resistance training 2-3 times a week
accompanied by moderate level muscular endurance 3-5 times per week (Horton et al., 2018).
Further rigorous training ideas like rapid escalation of physical activity are less recognised.
Workout training at high impact results in improving exercise as well as lowering inflammatory
action. High-intensity therapy is popular for enhancing the aerobic muscle process, which
permits high-stress toleration without restricting breathlessness.
The planned management approaches
Various training regimens have been helpful for COPD patients who can finish their training
opportunities. For individuals with moderate COPD, high-intensity exercising is possible bi-
weekly over 3-6 months and outcomes in a much better exercise intensity, muscular strength,
and life quality.
walking is required for most everyday tasks, numerous rehabilitation programmes have it as
their preferred exercise method (often on a treadmill) (Hilde et al., 2013). Several folks
might want to practice on a stationary bicycle. The choice of a pleasant and satisfactory
workout increases the individual's desire to accept and be part over the long run.
Arms exercises also help patients with chronic lung illnesses who suffer difficulty breathing or
other problems in their usual everyday tasks, like hair washing. This is because chronic
respiratory illness can result in muscle loss, and part of the muscles of the shoulders is required
to breathe and move the hands. This training is essential. Arms exercises may strain these
muscles fast.
The rationale for exercise training for COPD patient
Various research papers have shown that benefits in exercise training include decreases of
inflammatory markers, like IL-8, and a rise in muscular activities, like peroxisomes with a
proliferator-activated 1-α receptor as well as irisin coactivator (McCarthy et al., 2015). Lastly,
training remains to be an economical operation and decreases the sum of hospitals
Various training methods were suggested for optimisation of exercise tolerance and
maximisation of training benefits in COPD patients. However, the most efficient methods of
practice still are unknown. Recommendations include resistance training 2-3 times a week
accompanied by moderate level muscular endurance 3-5 times per week (Horton et al., 2018).
Further rigorous training ideas like rapid escalation of physical activity are less recognised.
Workout training at high impact results in improving exercise as well as lowering inflammatory
action. High-intensity therapy is popular for enhancing the aerobic muscle process, which
permits high-stress toleration without restricting breathlessness.
The planned management approaches
Various training regimens have been helpful for COPD patients who can finish their training
opportunities. For individuals with moderate COPD, high-intensity exercising is possible bi-
weekly over 3-6 months and outcomes in a much better exercise intensity, muscular strength,
and life quality.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Justification of the management approach
The foundation of efficient therapy of COPD is characterised as pulmonary rehabilitation.
Powerful, standardised evidence is provided to illustrate that Patients with COPD, after
finalisation, have enhanced their capacity to exercise concerning greater 6-minute walking
distance (6MWD), maximum oxygen absorption (V-O2peak) along with better patient centres
like life quality as well as dyspnea (McCarthy et al., 2015).
The intensity of exercise is a parameter frequently manipulated by doctors to optimise the results
of rehabilitation programs that are physical as well as patient-focused. Exercise intensity
remains typically an essential therapeutic issue when considering patient safety. Increased
intensity workout will lead to increased heat production and need for myocardial oxygen, plus it
might not be suitable for people with significantly existing comorbid diseases (Leddy et al.,
2019).
The concept of training remains a gradual overburden, leading to continuous development in
capability by increasing demands on the body. The training dosage may be largely adjusted by
changing the intensity and length of the workout, increasing as well as reducing the weekly
workout regularity. The duration as well as a method of training (walk, biking, sprinting and
swimming), as well as the people's starting training ability, also contribute to many other aspects.
For practice, the air, cardiovascular, and skeletal muscle units have to be linked to provide air to
the training muscle and eliminate metabolic raw material for the production. These processes are
overcharged with repeated workouts as well as physiologic adaptive responses, resulting in a
central adaptation in which an enhancement in cardiovascular efficiency occurs through an
increased cardiovascular level as well as the adjustment of the peripheral nervous system when
the intensity of the exercise and oxidative capability of the skeletal muscles spike. These
adjustments increase the supply and use of oxygen both at maximum as well as at low intensities
in the exercise tissue.
The foundation of efficient therapy of COPD is characterised as pulmonary rehabilitation.
Powerful, standardised evidence is provided to illustrate that Patients with COPD, after
finalisation, have enhanced their capacity to exercise concerning greater 6-minute walking
distance (6MWD), maximum oxygen absorption (V-O2peak) along with better patient centres
like life quality as well as dyspnea (McCarthy et al., 2015).
The intensity of exercise is a parameter frequently manipulated by doctors to optimise the results
of rehabilitation programs that are physical as well as patient-focused. Exercise intensity
remains typically an essential therapeutic issue when considering patient safety. Increased
intensity workout will lead to increased heat production and need for myocardial oxygen, plus it
might not be suitable for people with significantly existing comorbid diseases (Leddy et al.,
2019).
The concept of training remains a gradual overburden, leading to continuous development in
capability by increasing demands on the body. The training dosage may be largely adjusted by
changing the intensity and length of the workout, increasing as well as reducing the weekly
workout regularity. The duration as well as a method of training (walk, biking, sprinting and
swimming), as well as the people's starting training ability, also contribute to many other aspects.
For practice, the air, cardiovascular, and skeletal muscle units have to be linked to provide air to
the training muscle and eliminate metabolic raw material for the production. These processes are
overcharged with repeated workouts as well as physiologic adaptive responses, resulting in a
central adaptation in which an enhancement in cardiovascular efficiency occurs through an
increased cardiovascular level as well as the adjustment of the peripheral nervous system when
the intensity of the exercise and oxidative capability of the skeletal muscles spike. These
adjustments increase the supply and use of oxygen both at maximum as well as at low intensities
in the exercise tissue.
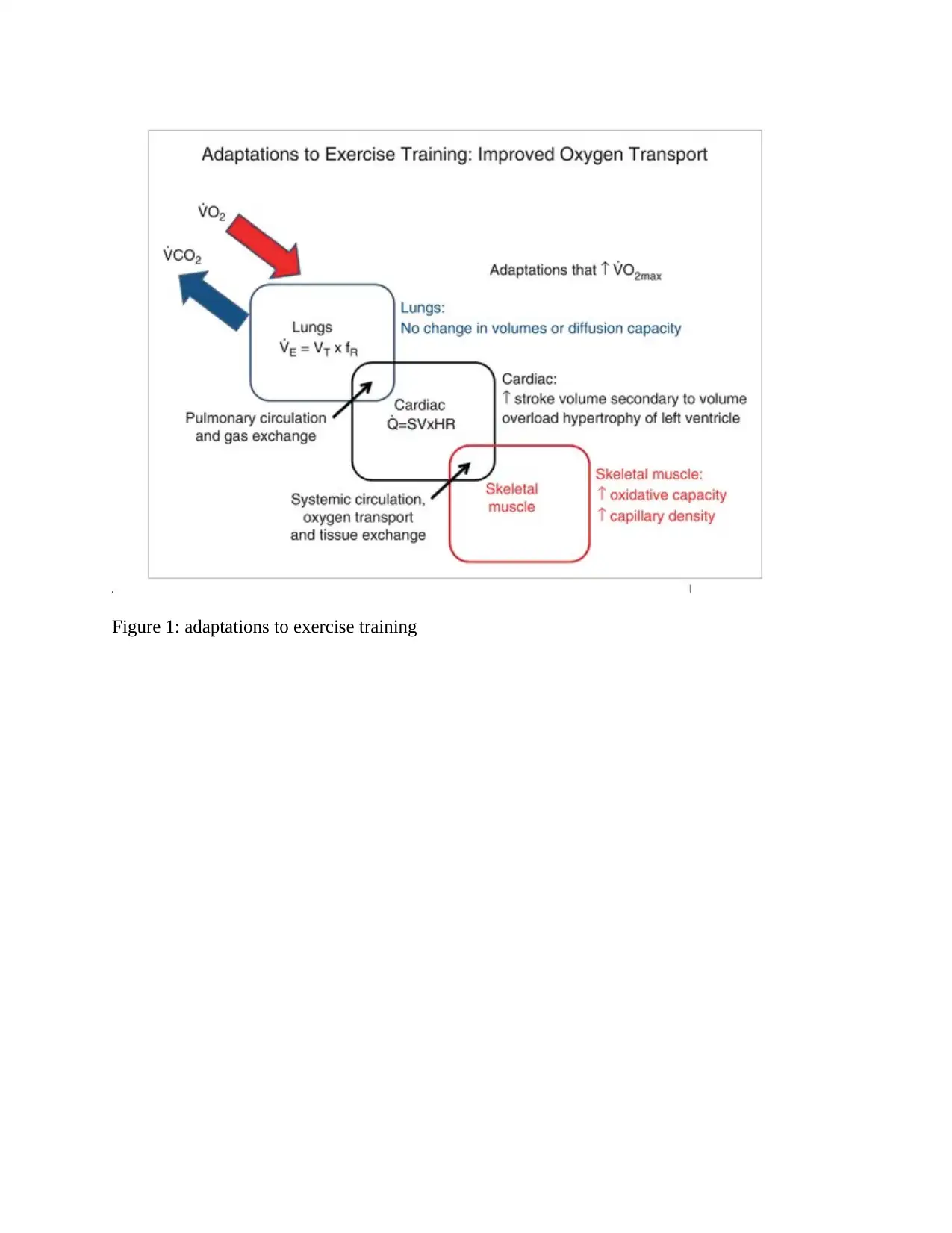
Figure 1: adaptations to exercise training
References
HILDE, J. M., SKJØRTEN, I., HANSTEEN, V., MELSOM, M. N., HISDAL, J.,
HUMERFELT, S. & STEINE, K. 2013. Haemodynamic responses to exercise in patients
with COPD. European Respiratory Journal, 41, 1031-1041.
HORTON, E. J., MITCHELL, K. E., JOHNSON-WARRINGTON, V., APPS, L. D., SEWELL,
L., MORGAN, M., TAYLOR, R. S. & SINGH, S. J. 2018. Comparison of a structured
home-based rehabilitation programme with conventional supervised pulmonary
rehabilitation: a randomised non-inferiority trial. Thorax, 73, 29-36.
KURZAJ, M., WIERZEJSKI, W., DOR, A., STAWSKA, J. & ROŻEK, K. 2013. The impact of
specialised physiotherapy methods on BODE index in COPD patients during
hospitalisation. Advances in Clinical and Experimental Medicine, 22, 721-730.
LEDDY, J. J., HAIDER, M. N., ELLIS, M. J., MANNIX, R., DARLING, S. R., FREITAS, M.
S., SUFFOLETTO, H. N., LEITER, J., CORDINGLEY, D. M. & WILLER, B. 2019.
Early subthreshold aerobic exercise for sport-related concussion: a randomised clinical
trial. JAMA pediatrics, 173, 319-325.
MCCARTHY, B., CASEY, D., DEVANE, D., MURPHY, K., MURPHY, E. & LACASSE, Y.
2015. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane
database of systematic reviews.
MIRAVITLLES, M. & RIBERA, A. 2017. Understanding the impact of symptoms on the burden
of COPD. Respiratory research, 18, 1-11.
PERERA, W. R., HURST, J. R., WILKINSON, T. M., SAPSFORD, R. J., MÜLLEROVA, H.,
DONALDSON, G. C. & WEDZICHA, J. A. 2007. Inflammatory changes, recovery and
recurrence at COPD exacerbation. European Respiratory Journal, 29, 527-534.
HILDE, J. M., SKJØRTEN, I., HANSTEEN, V., MELSOM, M. N., HISDAL, J.,
HUMERFELT, S. & STEINE, K. 2013. Haemodynamic responses to exercise in patients
with COPD. European Respiratory Journal, 41, 1031-1041.
HORTON, E. J., MITCHELL, K. E., JOHNSON-WARRINGTON, V., APPS, L. D., SEWELL,
L., MORGAN, M., TAYLOR, R. S. & SINGH, S. J. 2018. Comparison of a structured
home-based rehabilitation programme with conventional supervised pulmonary
rehabilitation: a randomised non-inferiority trial. Thorax, 73, 29-36.
KURZAJ, M., WIERZEJSKI, W., DOR, A., STAWSKA, J. & ROŻEK, K. 2013. The impact of
specialised physiotherapy methods on BODE index in COPD patients during
hospitalisation. Advances in Clinical and Experimental Medicine, 22, 721-730.
LEDDY, J. J., HAIDER, M. N., ELLIS, M. J., MANNIX, R., DARLING, S. R., FREITAS, M.
S., SUFFOLETTO, H. N., LEITER, J., CORDINGLEY, D. M. & WILLER, B. 2019.
Early subthreshold aerobic exercise for sport-related concussion: a randomised clinical
trial. JAMA pediatrics, 173, 319-325.
MCCARTHY, B., CASEY, D., DEVANE, D., MURPHY, K., MURPHY, E. & LACASSE, Y.
2015. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane
database of systematic reviews.
MIRAVITLLES, M. & RIBERA, A. 2017. Understanding the impact of symptoms on the burden
of COPD. Respiratory research, 18, 1-11.
PERERA, W. R., HURST, J. R., WILKINSON, T. M., SAPSFORD, R. J., MÜLLEROVA, H.,
DONALDSON, G. C. & WEDZICHA, J. A. 2007. Inflammatory changes, recovery and
recurrence at COPD exacerbation. European Respiratory Journal, 29, 527-534.
1 out of 7
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




