Subchorionic Haematoma: Pathophysiology, Diagnosis, and Treatment
VerifiedAdded on 2023/04/21
|6
|1497
|296
Report
AI Summary
This report delves into the pathophysiology and diagnostic methods for subchorionic haematoma, a common condition characterized by bleeding between the uterine wall and the chorionic membrane during the first trimester of pregnancy. It explores the causes, including poor placentation and disruption of blood vessels, leading to haematoma formation and potential placental detachment. The report details the clinical presentation, including vaginal bleeding and associated symptoms, and emphasizes the role of ultrasound in diagnosis, highlighting sonographic appearances such as hypoechoic lesions. It also discusses potential complications like preterm delivery and placental abruption and touches on the management of subchorionic haematoma, which often involves monitoring and lifestyle adjustments. References to relevant research studies are included.

Running head: SUBCHORIONIC HAEMATOMA
PATHOPHYSIOLOGY AND DIAGNOSIS OF SUBCHORIONIC HAEMATOMA
Name of the Student:
Name of the University:
Author Note:
PATHOPHYSIOLOGY AND DIAGNOSIS OF SUBCHORIONIC HAEMATOMA
Name of the Student:
Name of the University:
Author Note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1PATHOPHYSIOLOGY AND DIAGNOSIS OF SUBCHORIONIC HAEMATOMA
Pathophysiology of Subchorionic Haematoma (1 trimester)
The clotting of the blood between the wall of the uterus and the chorion, the outer
membrane between the uterus and placenta and surrounds the amniotic sac where the embryo
is present, leads to a subchorionic haematoma. The haematoma causes detachment of the
placenta from the chorion membrane, which is the primary cause of vaginal bleeding during
the first trimester. It is one of the most common abnormalities found in women while
performing ultrasonography, which may also result in miscarriage if adequate treatment is not
given on time. The frequency of subchorionic haematoma in the first trimester ranges from 4
to 22 % as diagnosed by ultrasound (Kovalyova 2013).
The exact pathophysiology of the subchorionic haematoma is entirely not clear
currently. However, the underlying cause of the subchorionic haematoma is poor
placentation, which can lead to the disruption of angiogenesis and leads to the generation of
weak blood vessels that can tear of easily. According to Hertzberg and Middleton (2015),
low-pressure bleeding is caused due to the tearing of the peripheral uterus-placental veins.
The blood then forms a haematoma between the chorionic membrane and the wall of the
uterus. The chorionic detachment is usually caused due to endotheliopathy, hormonal,
immune-genetic, autoimmune disorders and so on. According to Kovalyova (2013), few
factors play a critical role in the development of haematoma, which are
Immunological causes (predominance of the Th-1 response),
Maternal coagulation disorders (hereditary and acquired thrombophilia - MTHFR gene
polymorphisms, PAI-1 gene polymorphisms, anti-hCG sensitisation, antiphospholipid
syndrome),
Chronic Disseminated Intravascular Coagulation,
Severe arterial hypertension in the mother,
Bacterial and viral infection,
Chronic endometritis,
Compatibility of spouses on HLA-antigens class II.
The cause of the formation of subchorionic haematoma is believed to be due to the
immunological conflict between the mother and the foetus, associated with the mechanisms
Pathophysiology of Subchorionic Haematoma (1 trimester)
The clotting of the blood between the wall of the uterus and the chorion, the outer
membrane between the uterus and placenta and surrounds the amniotic sac where the embryo
is present, leads to a subchorionic haematoma. The haematoma causes detachment of the
placenta from the chorion membrane, which is the primary cause of vaginal bleeding during
the first trimester. It is one of the most common abnormalities found in women while
performing ultrasonography, which may also result in miscarriage if adequate treatment is not
given on time. The frequency of subchorionic haematoma in the first trimester ranges from 4
to 22 % as diagnosed by ultrasound (Kovalyova 2013).
The exact pathophysiology of the subchorionic haematoma is entirely not clear
currently. However, the underlying cause of the subchorionic haematoma is poor
placentation, which can lead to the disruption of angiogenesis and leads to the generation of
weak blood vessels that can tear of easily. According to Hertzberg and Middleton (2015),
low-pressure bleeding is caused due to the tearing of the peripheral uterus-placental veins.
The blood then forms a haematoma between the chorionic membrane and the wall of the
uterus. The chorionic detachment is usually caused due to endotheliopathy, hormonal,
immune-genetic, autoimmune disorders and so on. According to Kovalyova (2013), few
factors play a critical role in the development of haematoma, which are
Immunological causes (predominance of the Th-1 response),
Maternal coagulation disorders (hereditary and acquired thrombophilia - MTHFR gene
polymorphisms, PAI-1 gene polymorphisms, anti-hCG sensitisation, antiphospholipid
syndrome),
Chronic Disseminated Intravascular Coagulation,
Severe arterial hypertension in the mother,
Bacterial and viral infection,
Chronic endometritis,
Compatibility of spouses on HLA-antigens class II.
The cause of the formation of subchorionic haematoma is believed to be due to the
immunological conflict between the mother and the foetus, associated with the mechanisms
2PATHOPHYSIOLOGY AND DIAGNOSIS OF SUBCHORIONIC HAEMATOMA
of the modification of the immune system that is mediated by progesterone. This hypothesis
is proved by a study where it is found that subchorionic haematoma is more common in
pregnancies that use medical procedures such as the induction of ovulation and in-vitro
fertilisation, which uses the transfer of the embryo that is frozen-thawed (Asato et al. 2014).
The characteristic symptom of subchorionic haematoma is vaginal bleeding, which
can be in the form of either spotting or heavy bleeding. It can be accompanied by severe
abdominal pain, cramping and dizziness (Costantino, Guaraldi and Costantino 2016).
However, the cause of vaginal bleeding is the subchorionic haematoma can only be detected
by ultrasound. The size of the haematoma is identified by evaluating how much the chorionic
membrane has been elevated from the wall of the uterus.
The subchorionic haematoma causes bleeding, which does not usually cause any
problems. However, research on subchorionic haematoma whether can cause pregnancy
complications, such as preterm delivery or pregnancy loss, varies. For example, a review
of 2012 found possible links between the subchorionic haematoma and a higher risk of giving
birth prematurely and pregnancy loss. However, a study of 2013 found that subchorionic
haematoma did not increase the risk of pregnancy loss.
Another possible complication is placental abruption, which is a severe complication
that happens when the placenta detaches from the womb lining. The principal sign of
placental abruption is vaginal bleeding, but a pregnant woman may also feel discomfort and
tenderness, and a pain in the belly or back that comes on suddenly and does not go away.
Sonographic appearances of Subchorionic Haematoma (1 trimester)
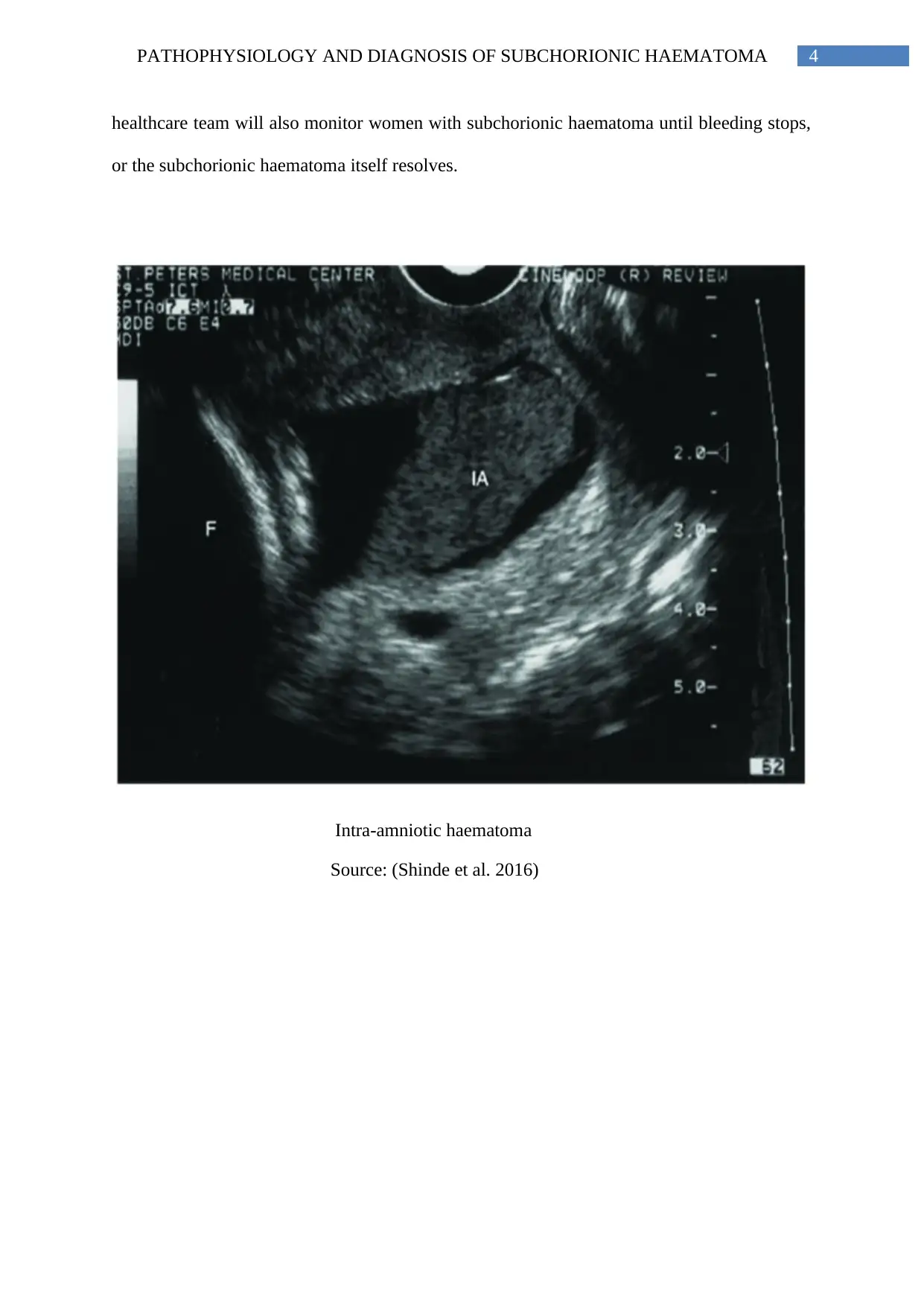
The woman who experiences vaginal bleeding during pregnancy should speak to a
doctor. To diagnose the cause of the bleeding, the doctor will usually perform a physical
examination and may order blood tests. The doctor may also suggest an ultrasonography
examination. The high-frequency sound waves are used in an ultrasonographic examination
to generate a black and white image of the foetus and placenta on a screen. If a person is
experiencing subchorionic bleeding, the areas of blood inside the uterus will show up on this
sonographic picture.
of the modification of the immune system that is mediated by progesterone. This hypothesis
is proved by a study where it is found that subchorionic haematoma is more common in
pregnancies that use medical procedures such as the induction of ovulation and in-vitro
fertilisation, which uses the transfer of the embryo that is frozen-thawed (Asato et al. 2014).
The characteristic symptom of subchorionic haematoma is vaginal bleeding, which
can be in the form of either spotting or heavy bleeding. It can be accompanied by severe
abdominal pain, cramping and dizziness (Costantino, Guaraldi and Costantino 2016).
However, the cause of vaginal bleeding is the subchorionic haematoma can only be detected
by ultrasound. The size of the haematoma is identified by evaluating how much the chorionic
membrane has been elevated from the wall of the uterus.
The subchorionic haematoma causes bleeding, which does not usually cause any
problems. However, research on subchorionic haematoma whether can cause pregnancy
complications, such as preterm delivery or pregnancy loss, varies. For example, a review
of 2012 found possible links between the subchorionic haematoma and a higher risk of giving
birth prematurely and pregnancy loss. However, a study of 2013 found that subchorionic
haematoma did not increase the risk of pregnancy loss.
Another possible complication is placental abruption, which is a severe complication
that happens when the placenta detaches from the womb lining. The principal sign of
placental abruption is vaginal bleeding, but a pregnant woman may also feel discomfort and
tenderness, and a pain in the belly or back that comes on suddenly and does not go away.
Sonographic appearances of Subchorionic Haematoma (1 trimester)
The woman who experiences vaginal bleeding during pregnancy should speak to a
doctor. To diagnose the cause of the bleeding, the doctor will usually perform a physical
examination and may order blood tests. The doctor may also suggest an ultrasonography
examination. The high-frequency sound waves are used in an ultrasonographic examination
to generate a black and white image of the foetus and placenta on a screen. If a person is
experiencing subchorionic bleeding, the areas of blood inside the uterus will show up on this
sonographic picture.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3PATHOPHYSIOLOGY AND DIAGNOSIS OF SUBCHORIONIC HAEMATOMA
The subchorionic haematoma is diagnosed only by ultrasound. The sonographic
evidence of subchorionic haematoma is evaluated clinically and sonographically. Clinical
evaluation includes several characteristics such as the age of the mother, gravidity, parity, age
of the embryo, the presence of pain, the presence and amount of bleeding, and outcomes of
pregnancy (Ananth and Kinzler 2014). The sonographic evaluation includes the relative and
complete size of the haematoma, the echogenicity and location of the haematoma in
connection with the placenta, the appearance of marginal placental abruption, and
progression in the follow-up examinations.
The characteristic of the sonographic finding is the hypo-echoic lesion, which is
crescent-shaped present in between the wall of the uterus and the chorionic membrane. The
crescent-shaped lesion formed due to the clotting of the blood results in the elevation of the
chorionic membrane from the uterine wall. The haematoma initially appears to be hyper-
echoic but becomes hypo-echoic with time, and this can be due to chorio-amniotic separation
and twin gestational sac (Palatnik and Grobman 2015). The difference in the echo texture is
also dependent on the time elapsed since bleeding. In most of the cases of subchorionic
haematoma, there is an extension of the haematoma towards the margin of the placenta. A
subchorionic haematoma is small if it is less than 20 % of the amniotic sac and is large if it is
greater than 55 to 65 % of the sac, the quantification of the haematoma is done in this
manner. The haematoma in most cases extends to the margin of the placenta (Arleo and
Troiano 2015).
In most cases, subchorionic haematoma does not require treatment. Most doctors will
recommend the woman to put a limit on some activities, such as sexual intercourse, to stand
for long hours and to lift any heavy objects, to drink plenty water and eat regular small meals
to avoid cramps and get an adequate amount of rest. A doctor and other members of the
The subchorionic haematoma is diagnosed only by ultrasound. The sonographic
evidence of subchorionic haematoma is evaluated clinically and sonographically. Clinical
evaluation includes several characteristics such as the age of the mother, gravidity, parity, age
of the embryo, the presence of pain, the presence and amount of bleeding, and outcomes of
pregnancy (Ananth and Kinzler 2014). The sonographic evaluation includes the relative and
complete size of the haematoma, the echogenicity and location of the haematoma in
connection with the placenta, the appearance of marginal placental abruption, and
progression in the follow-up examinations.
The characteristic of the sonographic finding is the hypo-echoic lesion, which is
crescent-shaped present in between the wall of the uterus and the chorionic membrane. The
crescent-shaped lesion formed due to the clotting of the blood results in the elevation of the
chorionic membrane from the uterine wall. The haematoma initially appears to be hyper-
echoic but becomes hypo-echoic with time, and this can be due to chorio-amniotic separation
and twin gestational sac (Palatnik and Grobman 2015). The difference in the echo texture is
also dependent on the time elapsed since bleeding. In most of the cases of subchorionic
haematoma, there is an extension of the haematoma towards the margin of the placenta. A
subchorionic haematoma is small if it is less than 20 % of the amniotic sac and is large if it is
greater than 55 to 65 % of the sac, the quantification of the haematoma is done in this
manner. The haematoma in most cases extends to the margin of the placenta (Arleo and
Troiano 2015).
In most cases, subchorionic haematoma does not require treatment. Most doctors will
recommend the woman to put a limit on some activities, such as sexual intercourse, to stand
for long hours and to lift any heavy objects, to drink plenty water and eat regular small meals
to avoid cramps and get an adequate amount of rest. A doctor and other members of the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4PATHOPHYSIOLOGY AND DIAGNOSIS OF SUBCHORIONIC HAEMATOMA
healthcare team will also monitor women with subchorionic haematoma until bleeding stops,
or the subchorionic haematoma itself resolves.
Intra-amniotic haematoma
Source: (Shinde et al. 2016)
healthcare team will also monitor women with subchorionic haematoma until bleeding stops,
or the subchorionic haematoma itself resolves.
Intra-amniotic haematoma
Source: (Shinde et al. 2016)
5PATHOPHYSIOLOGY AND DIAGNOSIS OF SUBCHORIONIC HAEMATOMA
References
Ananth, C. and Kinzler, W. 2014. Placental abruption: Clinical features and
diagnosis. Secondary placental abruption: clinical features and diagnosis..
Arleo, E. and Troiano, R. 2015. Chorionic Bump on First-Trimester Sonography. Journal of
Ultrasound in Medicine, 34(1), pp.137-142.
Asato, K., Mekaru, K., Heshiki, C., Sugiyama, H., Kinjyo, T., Masamoto, H. and Aoki, Y.
2014. Subchorionic hematoma occurs more frequently in in vitro fertilization
pregnancy. European Journal of Obstetrics & Gynecology and Reproductive Biology, 181,
pp.41-44.
Costantino, M., Guaraldi, C. and Costantino, D., 2016. Resolution of subchorionic hematoma
and symptoms of threatened miscarriage using vaginal alpha lipoic acid or progesterone:
clinical evidences. Eur Rev Med Pharmacol Sci, 20(8), pp.1656-1663.
Hertzberg, B.S. and Middleton, W.D., 2015. Ultrasound: The Requisites E-Book. Elsevier
Health Sciences.
Kovalyova, J.V., 2013. Subchorionic hematoma. Causes, pathogenesis, diagnostic and
treatment management. Journal of obstetrics and women's diseases, 62(4), pp.37-47.
Palatnik, A. and Grobman, W. 2015. The relationship between first-trimester subchorionic
hematoma, cervical length, and preterm birth. American Journal of Obstetrics and
Gynecology, 213(3), pp.403.e1-403.e4.
Shinde, G.R., VaSwani, B.P., Patange, R.P., Laddad, M.M. and Bhosale, R.B., 2016.
Diagnostic performance of ultrasonography for detection of abruption and its clinical
correlation and maternal and foetal outcome. Journal of clinical and diagnostic research:
JCDR, 10(8), p.QC04.
References
Ananth, C. and Kinzler, W. 2014. Placental abruption: Clinical features and
diagnosis. Secondary placental abruption: clinical features and diagnosis..
Arleo, E. and Troiano, R. 2015. Chorionic Bump on First-Trimester Sonography. Journal of
Ultrasound in Medicine, 34(1), pp.137-142.
Asato, K., Mekaru, K., Heshiki, C., Sugiyama, H., Kinjyo, T., Masamoto, H. and Aoki, Y.
2014. Subchorionic hematoma occurs more frequently in in vitro fertilization
pregnancy. European Journal of Obstetrics & Gynecology and Reproductive Biology, 181,
pp.41-44.
Costantino, M., Guaraldi, C. and Costantino, D., 2016. Resolution of subchorionic hematoma
and symptoms of threatened miscarriage using vaginal alpha lipoic acid or progesterone:
clinical evidences. Eur Rev Med Pharmacol Sci, 20(8), pp.1656-1663.
Hertzberg, B.S. and Middleton, W.D., 2015. Ultrasound: The Requisites E-Book. Elsevier
Health Sciences.
Kovalyova, J.V., 2013. Subchorionic hematoma. Causes, pathogenesis, diagnostic and
treatment management. Journal of obstetrics and women's diseases, 62(4), pp.37-47.
Palatnik, A. and Grobman, W. 2015. The relationship between first-trimester subchorionic
hematoma, cervical length, and preterm birth. American Journal of Obstetrics and
Gynecology, 213(3), pp.403.e1-403.e4.
Shinde, G.R., VaSwani, B.P., Patange, R.P., Laddad, M.M. and Bhosale, R.B., 2016.
Diagnostic performance of ultrasonography for detection of abruption and its clinical
correlation and maternal and foetal outcome. Journal of clinical and diagnostic research:
JCDR, 10(8), p.QC04.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.
