Substance-Induced Psychosis: Case Study, Assessment & Strategies
VerifiedAdded on 2023/06/15
|9
|1872
|183
Case Study
AI Summary
This case study examines a 22-year-old patient, Susan, experiencing substance-induced psychosis due to early and prolonged substance abuse, particularly alcohol and cannabis. Her symptoms include auditory hallucinations, paranoia, and a urinary tract infection exacerbated by alcohol consumption. The study prioritizes managing her hallucinations and paranoia, addressing the risk of cannabis-induced schizophrenia, and treating her UTI. Intervention strategies involve a comprehensive assessment using tools like the Personality Assessment Inventory, therapeutic relationship building, pharmacological interventions (antipsychotics, antidepressants), and health promotion through psychotherapy to address underlying trauma and addiction triggers. The goal is to help Susan overcome her addiction, manage her symptoms, and reintegrate into mainstream society, highlighting the increasing prevalence of substance-induced psychotic disorders among young adults and the importance of tailored care plans for recovery. Desklib offers a wealth of resources, including similar case studies and solved assignments, to aid students in their studies.

Running head: SUBSTANCE INDUCED PSYCHOSIS
Substance induced psychosis
Name of the student:
Name of the university:
Author note:
Substance induced psychosis
Name of the student:
Name of the university:
Author note:
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1SUBSTANCE INDUCED PSYCHOSIS
Table of Contents
Introduction: 2
Aetiology and signs and symptoms: 2
Assessment, Health promotion and intervention strategies: 3
Conclusion: 6
References: 7
Table of Contents
Introduction: 2
Aetiology and signs and symptoms: 2
Assessment, Health promotion and intervention strategies: 3
Conclusion: 6
References: 7
2SUBSTANCE INDUCED PSYCHOSIS
Introduction:
The young and tech savvy generation of present day are leading a life that is ridden with a
myriad of different worries, troubles and challenges. The youngsters of the 21st century have a
life full of hardships, expectations and disappointments as well. However, the impact of the
different stressful elements of life has been affecting the patience and resilience of the youngsters
as well and that is the reason why the majority of the young generation are now straying towards
substance and alcohol abuse (Pierre 2010). This assignment will focus on the psychotic disorder
faced by a patient due to alcohol and substance abuse and recommend intervention strategies
taking the aid of a case study.
Aetiology and signs and symptoms:
The case study represents the case of Susan, the patient under focus in the assignment; a 22-
year-old youngster had been assessed by the nursing practitioner for urinary tract infection
however, the most conspicuous symptoms exhibited by the patient had been her low mood and
depression. On further enquiry, Susan revealed that she had been indulging in substance abuse
from a very early age of ten. On a more elaborative note, the patient also revealed that she had
recently started drinking daily and has been smoking cannabis as well and as a result she had
been suffering auditory hallucination. Elaborating more on her condition, it can be mentioned
that she had been going through addiction for a very long time in her life and being addicted to
substance and alcohol from such a short age has had a significant impact on the psychological
health of the patient. With the recent deterioration of drinking everyday and smoking cannabis
frequently, her auditory hallucination is being further complicated by paranoia and delusions as
well. According to the recent studies, the most important outcome of cannabis addiction is the
Introduction:
The young and tech savvy generation of present day are leading a life that is ridden with a
myriad of different worries, troubles and challenges. The youngsters of the 21st century have a
life full of hardships, expectations and disappointments as well. However, the impact of the
different stressful elements of life has been affecting the patience and resilience of the youngsters
as well and that is the reason why the majority of the young generation are now straying towards
substance and alcohol abuse (Pierre 2010). This assignment will focus on the psychotic disorder
faced by a patient due to alcohol and substance abuse and recommend intervention strategies
taking the aid of a case study.
Aetiology and signs and symptoms:
The case study represents the case of Susan, the patient under focus in the assignment; a 22-
year-old youngster had been assessed by the nursing practitioner for urinary tract infection
however, the most conspicuous symptoms exhibited by the patient had been her low mood and
depression. On further enquiry, Susan revealed that she had been indulging in substance abuse
from a very early age of ten. On a more elaborative note, the patient also revealed that she had
recently started drinking daily and has been smoking cannabis as well and as a result she had
been suffering auditory hallucination. Elaborating more on her condition, it can be mentioned
that she had been going through addiction for a very long time in her life and being addicted to
substance and alcohol from such a short age has had a significant impact on the psychological
health of the patient. With the recent deterioration of drinking everyday and smoking cannabis
frequently, her auditory hallucination is being further complicated by paranoia and delusions as
well. According to the recent studies, the most important outcome of cannabis addiction is the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3SUBSTANCE INDUCED PSYCHOSIS
onset of schizophrenia. As per the objective data, Susan had been experiencing two key
symptomatic characteristics of substance induced psychosis, auditory hallucination and paranoia
(Shinn, Heckers and Öngür 2013). Along with that, the added impact of alcohol has further
complicated the condition of the patient. Now coming to the urinary tract infection that the
patient had been having, the major cause of the disease is her regular excessive alcohol
consumption. According to the Kingdon et al. (2010), the fluctuation in the intestinal temperature
due to excessive alcohol consumption aids to the growth of opportunistic pathogen in the urinary
tract and the reduction in the hormone vasopressin facilitates excessive urge to urinate and
increases the possibility of the patient catching a UTI.
Assessment, Health promotion and intervention strategies:
The major health care priorities that the patient of the case study represents include
controlling and minimizing the auditory hallucinations that the patient has been suffering with.
Along with that, the healthcare professional will also need to address the paranoia and onset of
cannabis-induced schizophrenia in Susan. Additionally, she will need a care plan for the urinary
tract infection (Hepworth, Ashcroft and Kingdon 2013). Lastly, the patient will require a
thorough health promotional intervention strategy to overcome her addiction to alcohol and
substance abuse so that she can revert to a healthier lifestyle. The first and foremost intervention
strategy will have to focus on assessment of the severity of her substance-induced psychosis. The
healthcare professional will require developing a therapeutic mutually respectful relationship
with the patient, so that she can feel comfortable to share the details of her hallucinations for
better assessment. It has to be understood that the patients had been undergoing a variety of
different health care concerns and hence a comprehensive assessment will be required so that
improved treatment and care planning can be performed. This comprehensive assessment will
onset of schizophrenia. As per the objective data, Susan had been experiencing two key
symptomatic characteristics of substance induced psychosis, auditory hallucination and paranoia
(Shinn, Heckers and Öngür 2013). Along with that, the added impact of alcohol has further
complicated the condition of the patient. Now coming to the urinary tract infection that the
patient had been having, the major cause of the disease is her regular excessive alcohol
consumption. According to the Kingdon et al. (2010), the fluctuation in the intestinal temperature
due to excessive alcohol consumption aids to the growth of opportunistic pathogen in the urinary
tract and the reduction in the hormone vasopressin facilitates excessive urge to urinate and
increases the possibility of the patient catching a UTI.
Assessment, Health promotion and intervention strategies:
The major health care priorities that the patient of the case study represents include
controlling and minimizing the auditory hallucinations that the patient has been suffering with.
Along with that, the healthcare professional will also need to address the paranoia and onset of
cannabis-induced schizophrenia in Susan. Additionally, she will need a care plan for the urinary
tract infection (Hepworth, Ashcroft and Kingdon 2013). Lastly, the patient will require a
thorough health promotional intervention strategy to overcome her addiction to alcohol and
substance abuse so that she can revert to a healthier lifestyle. The first and foremost intervention
strategy will have to focus on assessment of the severity of her substance-induced psychosis. The
healthcare professional will require developing a therapeutic mutually respectful relationship
with the patient, so that she can feel comfortable to share the details of her hallucinations for
better assessment. It has to be understood that the patients had been undergoing a variety of
different health care concerns and hence a comprehensive assessment will be required so that
improved treatment and care planning can be performed. This comprehensive assessment will
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4SUBSTANCE INDUCED PSYCHOSIS
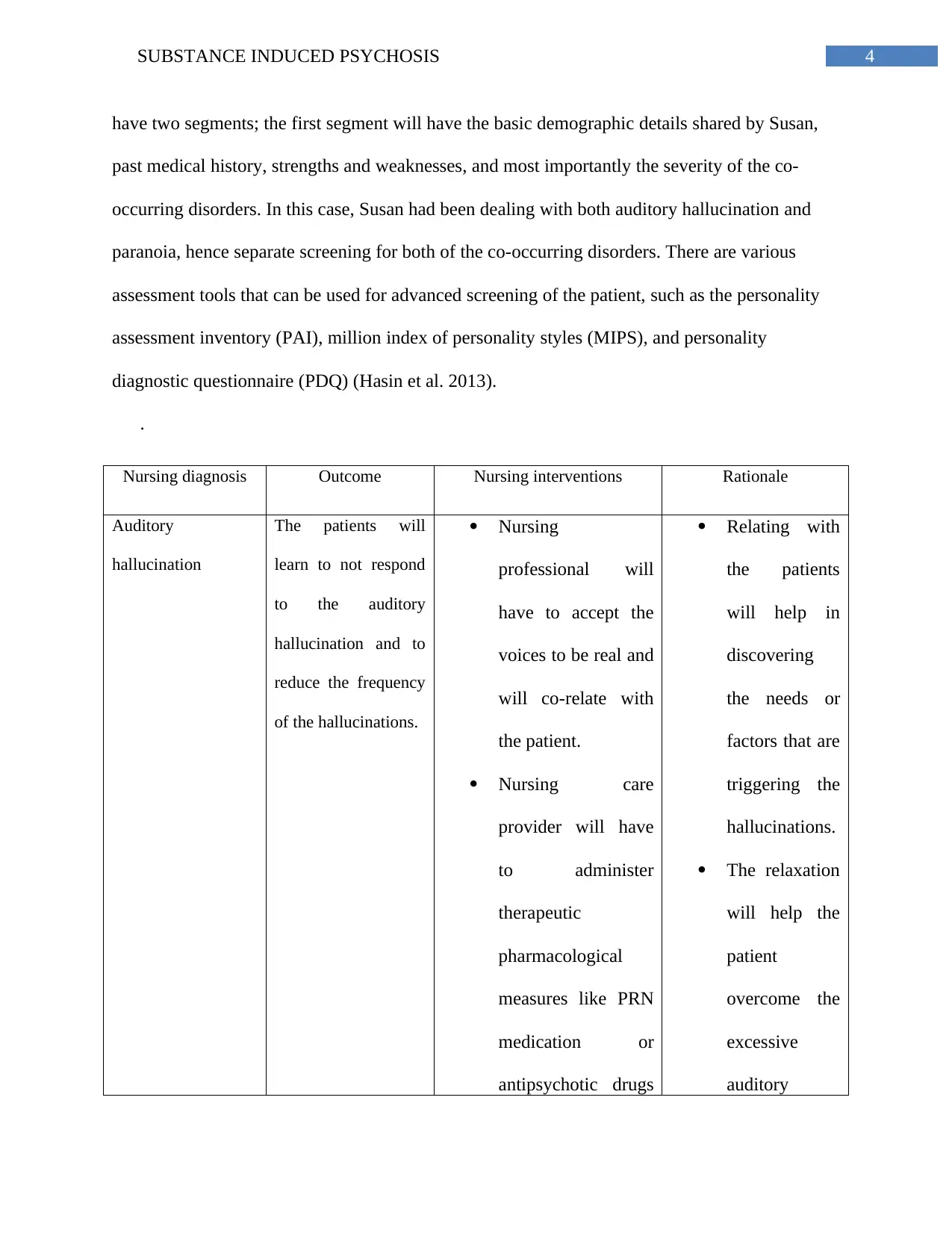
have two segments; the first segment will have the basic demographic details shared by Susan,
past medical history, strengths and weaknesses, and most importantly the severity of the co-
occurring disorders. In this case, Susan had been dealing with both auditory hallucination and
paranoia, hence separate screening for both of the co-occurring disorders. There are various
assessment tools that can be used for advanced screening of the patient, such as the personality
assessment inventory (PAI), million index of personality styles (MIPS), and personality
diagnostic questionnaire (PDQ) (Hasin et al. 2013).
.
Nursing diagnosis Outcome Nursing interventions Rationale
Auditory
hallucination
The patients will
learn to not respond
to the auditory
hallucination and to
reduce the frequency
of the hallucinations.
Nursing
professional will
have to accept the
voices to be real and
will co-relate with
the patient.
Nursing care
provider will have
to administer
therapeutic
pharmacological
measures like PRN
medication or
antipsychotic drugs
Relating with
the patients
will help in
discovering
the needs or
factors that are
triggering the
hallucinations.
The relaxation
will help the
patient
overcome the
excessive
auditory
have two segments; the first segment will have the basic demographic details shared by Susan,
past medical history, strengths and weaknesses, and most importantly the severity of the co-
occurring disorders. In this case, Susan had been dealing with both auditory hallucination and
paranoia, hence separate screening for both of the co-occurring disorders. There are various
assessment tools that can be used for advanced screening of the patient, such as the personality
assessment inventory (PAI), million index of personality styles (MIPS), and personality
diagnostic questionnaire (PDQ) (Hasin et al. 2013).
.
Nursing diagnosis Outcome Nursing interventions Rationale
Auditory
hallucination
The patients will
learn to not respond
to the auditory
hallucination and to
reduce the frequency
of the hallucinations.
Nursing
professional will
have to accept the
voices to be real and
will co-relate with
the patient.
Nursing care
provider will have
to administer
therapeutic
pharmacological
measures like PRN
medication or
antipsychotic drugs
Relating with
the patients
will help in
discovering
the needs or
factors that are
triggering the
hallucinations.
The relaxation
will help the
patient
overcome the
excessive
auditory
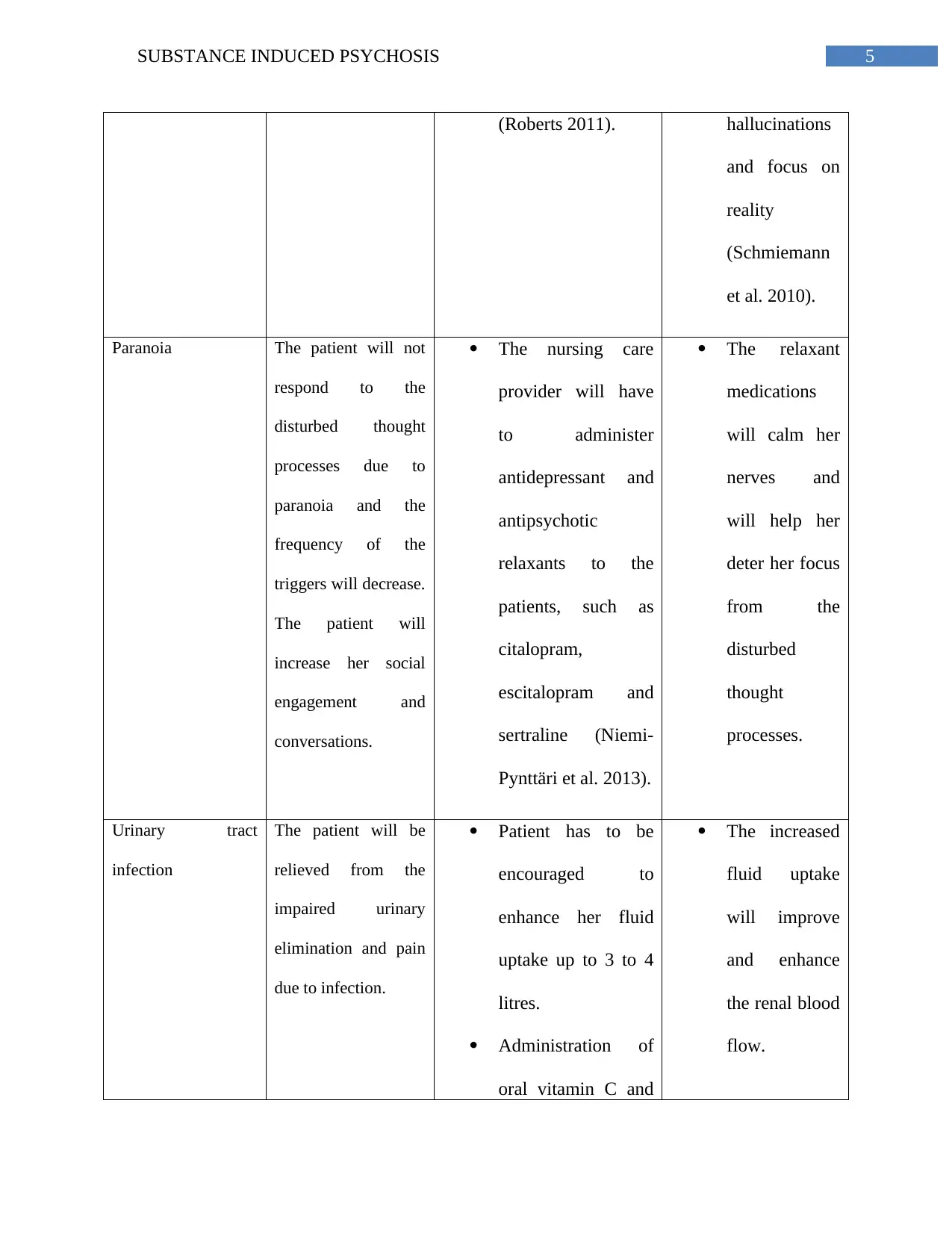
5SUBSTANCE INDUCED PSYCHOSIS
(Roberts 2011). hallucinations
and focus on
reality
(Schmiemann
et al. 2010).
Paranoia The patient will not
respond to the
disturbed thought
processes due to
paranoia and the
frequency of the
triggers will decrease.
The patient will
increase her social
engagement and
conversations.
The nursing care
provider will have
to administer
antidepressant and
antipsychotic
relaxants to the
patients, such as
citalopram,
escitalopram and
sertraline (Niemi-
Pynttäri et al. 2013).
The relaxant
medications
will calm her
nerves and
will help her
deter her focus
from the
disturbed
thought
processes.
Urinary tract
infection
The patient will be
relieved from the
impaired urinary
elimination and pain
due to infection.
Patient has to be
encouraged to
enhance her fluid
uptake up to 3 to 4
litres.
Administration of
oral vitamin C and
The increased
fluid uptake
will improve
and enhance
the renal blood
flow.
(Roberts 2011). hallucinations
and focus on
reality
(Schmiemann
et al. 2010).
Paranoia The patient will not
respond to the
disturbed thought
processes due to
paranoia and the
frequency of the
triggers will decrease.
The patient will
increase her social
engagement and
conversations.
The nursing care
provider will have
to administer
antidepressant and
antipsychotic
relaxants to the
patients, such as
citalopram,
escitalopram and
sertraline (Niemi-
Pynttäri et al. 2013).
The relaxant
medications
will calm her
nerves and
will help her
deter her focus
from the
disturbed
thought
processes.
Urinary tract
infection
The patient will be
relieved from the
impaired urinary
elimination and pain
due to infection.
Patient has to be
encouraged to
enhance her fluid
uptake up to 3 to 4
litres.
Administration of
oral vitamin C and
The increased
fluid uptake
will improve
and enhance
the renal blood
flow.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6SUBSTANCE INDUCED PSYCHOSIS
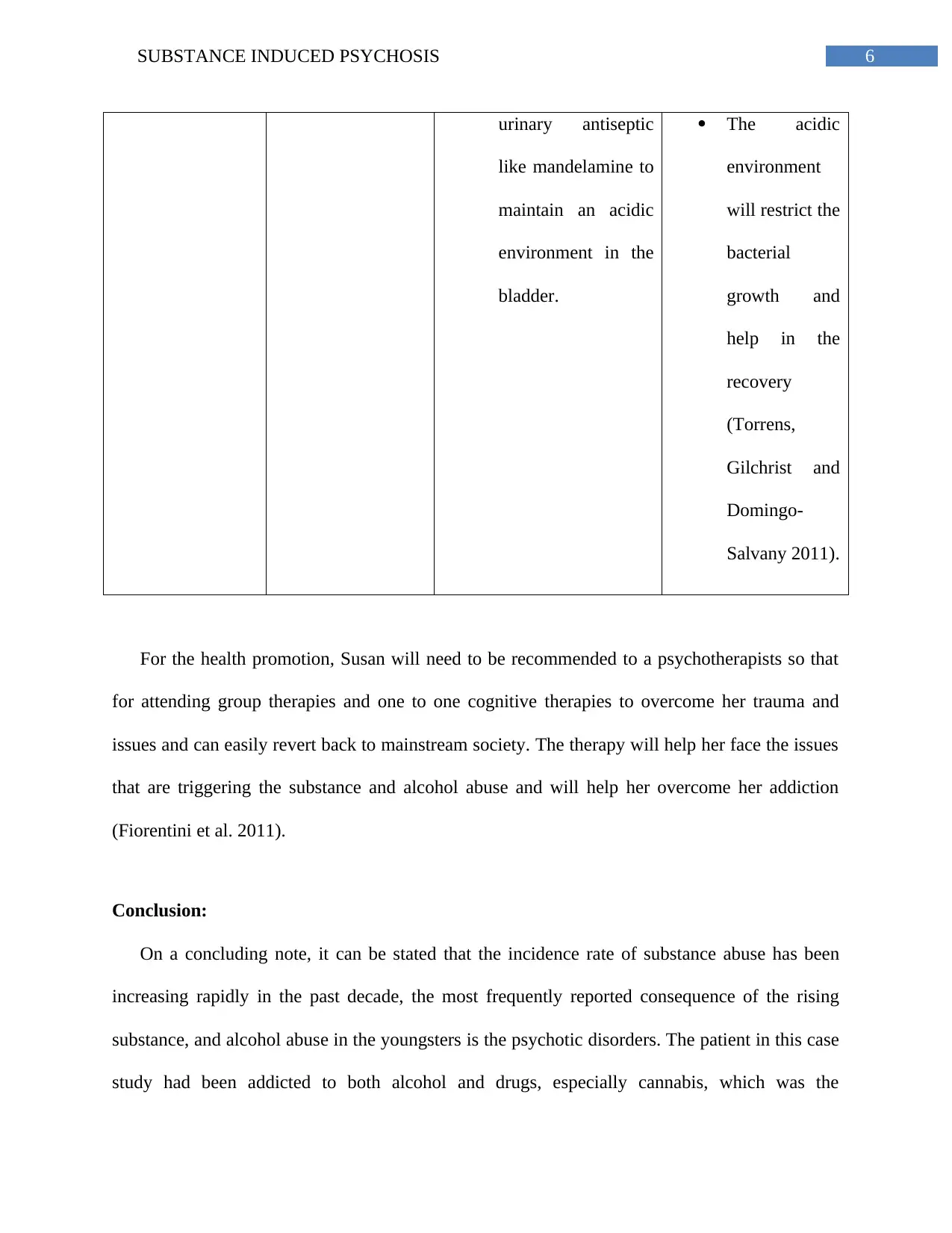
urinary antiseptic
like mandelamine to
maintain an acidic
environment in the
bladder.
The acidic
environment
will restrict the
bacterial
growth and
help in the
recovery
(Torrens,
Gilchrist and
Domingo-
Salvany 2011).
For the health promotion, Susan will need to be recommended to a psychotherapists so that
for attending group therapies and one to one cognitive therapies to overcome her trauma and
issues and can easily revert back to mainstream society. The therapy will help her face the issues
that are triggering the substance and alcohol abuse and will help her overcome her addiction
(Fiorentini et al. 2011).
Conclusion:
On a concluding note, it can be stated that the incidence rate of substance abuse has been
increasing rapidly in the past decade, the most frequently reported consequence of the rising
substance, and alcohol abuse in the youngsters is the psychotic disorders. The patient in this case
study had been addicted to both alcohol and drugs, especially cannabis, which was the
urinary antiseptic
like mandelamine to
maintain an acidic
environment in the
bladder.
The acidic
environment
will restrict the
bacterial
growth and
help in the
recovery
(Torrens,
Gilchrist and
Domingo-
Salvany 2011).
For the health promotion, Susan will need to be recommended to a psychotherapists so that
for attending group therapies and one to one cognitive therapies to overcome her trauma and
issues and can easily revert back to mainstream society. The therapy will help her face the issues
that are triggering the substance and alcohol abuse and will help her overcome her addiction
(Fiorentini et al. 2011).
Conclusion:
On a concluding note, it can be stated that the incidence rate of substance abuse has been
increasing rapidly in the past decade, the most frequently reported consequence of the rising
substance, and alcohol abuse in the youngsters is the psychotic disorders. The patient in this case
study had been addicted to both alcohol and drugs, especially cannabis, which was the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7SUBSTANCE INDUCED PSYCHOSIS
contributing factor behind the psychotic disorders she had been suffering through. Her paranoia
and auditory hallucinations were affecting her career and her social life and without proper
attention or medical care, her conditions could easily escalate to cannabis induced schizophrenia.
However, with the care plan and health promotional strategy out together for her, she will be able
to gain recovery easily.
References:
Fiorentini, A., Sara Volonteri, L., Dragogna, F., Rovera, C., Maffini, M., Carlo Mauri, M. and A
Altamura, C., 2011. Substance-induced psychoses: a critical review of the literature. Current
drug abuse reviews, 4(4), pp.228-240.
Hasin, D.S., O’Brien, C.P., Auriacombe, M., Borges, G., Bucholz, K., Budney, A., Compton,
W.M., Crowley, T., Ling, W., Petry, N.M. and Schuckit, M., 2013. DSM-5 criteria for substance
use disorders: recommendations and rationale. American Journal of Psychiatry, 170(8), pp.834-
851.
Hepworth, C.R., Ashcroft, K. and Kingdon, D., 2013. Auditory hallucinations: a comparison of
beliefs about voices in individuals with schizophrenia and borderline personality
disorder. Clinical psychology & psychotherapy, 20(3), pp.239-245.
Kingdon, D.G., Ashcroft, K., Bhandari, B., Gleeson, S., Warikoo, N., Symons, M., Taylor, L.,
Lucas, E., Mahendra, R., Ghosh, S. and Mason, A., 2010. Schizophrenia and borderline
personality disorder: similarities and differences in the experience of auditory hallucinations,
paranoia, and childhood trauma. The Journal of nervous and mental disease, 198(6), pp.399-403.
contributing factor behind the psychotic disorders she had been suffering through. Her paranoia
and auditory hallucinations were affecting her career and her social life and without proper
attention or medical care, her conditions could easily escalate to cannabis induced schizophrenia.
However, with the care plan and health promotional strategy out together for her, she will be able
to gain recovery easily.
References:
Fiorentini, A., Sara Volonteri, L., Dragogna, F., Rovera, C., Maffini, M., Carlo Mauri, M. and A
Altamura, C., 2011. Substance-induced psychoses: a critical review of the literature. Current
drug abuse reviews, 4(4), pp.228-240.
Hasin, D.S., O’Brien, C.P., Auriacombe, M., Borges, G., Bucholz, K., Budney, A., Compton,
W.M., Crowley, T., Ling, W., Petry, N.M. and Schuckit, M., 2013. DSM-5 criteria for substance
use disorders: recommendations and rationale. American Journal of Psychiatry, 170(8), pp.834-
851.
Hepworth, C.R., Ashcroft, K. and Kingdon, D., 2013. Auditory hallucinations: a comparison of
beliefs about voices in individuals with schizophrenia and borderline personality
disorder. Clinical psychology & psychotherapy, 20(3), pp.239-245.
Kingdon, D.G., Ashcroft, K., Bhandari, B., Gleeson, S., Warikoo, N., Symons, M., Taylor, L.,
Lucas, E., Mahendra, R., Ghosh, S. and Mason, A., 2010. Schizophrenia and borderline
personality disorder: similarities and differences in the experience of auditory hallucinations,
paranoia, and childhood trauma. The Journal of nervous and mental disease, 198(6), pp.399-403.
8SUBSTANCE INDUCED PSYCHOSIS
Niemi-Pynttäri, J.A., Sund, R., Putkonen, H., Vorma, H., Wahlbeck, K. and Pirkola, S.P., 2013.
Substance-induced psychoses converting into schizophrenia: a register-based study of 18,478
Finnish inpatient cases. The Journal of clinical psychiatry, 74(1), pp.e94-9.
Pierre, J.M., 2010. Hallucinations in nonpsychotic disorders: toward a differential diagnosis of
“hearing voices”. Harvard review of psychiatry, 18(1), pp.22-35.
Roberts, K.B., 2011. Urinary tract infection: clinical practice guideline for the diagnosis and
management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics, 128(3),
pp.595-610.
Schmiemann, G., Kniehl, E., Gebhardt, K., Matejczyk, M.M. and Hummers-Pradier, E., 2010.
The diagnosis of urinary tract infection: a systematic review. Deutsches Ärzteblatt
International, 107(21), p.361.
Shinn, A.K., Heckers, S. and Öngür, D., 2013. The special treatment of first rank auditory
hallucinations and bizarre delusions in the diagnosis of schizophrenia. Schizophrenia
research, 146(1), pp.17-21.
Torrens, M., Gilchrist, G. and Domingo-Salvany, A., 2011. Psychiatric comorbidity in illicit
drug users: substance-induced versus independent disorders. Drug & Alcohol
Dependence, 113(2), pp.147-156.
Niemi-Pynttäri, J.A., Sund, R., Putkonen, H., Vorma, H., Wahlbeck, K. and Pirkola, S.P., 2013.
Substance-induced psychoses converting into schizophrenia: a register-based study of 18,478
Finnish inpatient cases. The Journal of clinical psychiatry, 74(1), pp.e94-9.
Pierre, J.M., 2010. Hallucinations in nonpsychotic disorders: toward a differential diagnosis of
“hearing voices”. Harvard review of psychiatry, 18(1), pp.22-35.
Roberts, K.B., 2011. Urinary tract infection: clinical practice guideline for the diagnosis and
management of the initial UTI in febrile infants and children 2 to 24 months. Pediatrics, 128(3),
pp.595-610.
Schmiemann, G., Kniehl, E., Gebhardt, K., Matejczyk, M.M. and Hummers-Pradier, E., 2010.
The diagnosis of urinary tract infection: a systematic review. Deutsches Ärzteblatt
International, 107(21), p.361.
Shinn, A.K., Heckers, S. and Öngür, D., 2013. The special treatment of first rank auditory
hallucinations and bizarre delusions in the diagnosis of schizophrenia. Schizophrenia
research, 146(1), pp.17-21.
Torrens, M., Gilchrist, G. and Domingo-Salvany, A., 2011. Psychiatric comorbidity in illicit
drug users: substance-induced versus independent disorders. Drug & Alcohol
Dependence, 113(2), pp.147-156.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





