Integrated Health and Social Care: Supporting Individual's Journey
VerifiedAdded on 2024/05/14
|35
|7712
|123
Report
AI Summary
This report provides a comprehensive overview of integrated health and social care, emphasizing the importance of multidisciplinary approaches in supporting individuals' journeys. It identifies various local resources and provisions, such as NHS, PCTs, CQC, and NICE, that contribute to integrated care. The report also addresses unmet needs related to poverty, mental health, and maternity care, highlighting the disparities and challenges individuals face in accessing necessary services. Furthermore, it contrasts healthcare and social care providers, emphasizing the benefits of interagency collaboration for holistic patient care. The case of Lucy, a 75-year-old with Alzheimer's and other health conditions, illustrates the complexities of managing patients with multiple needs and the importance of coordinated support from healthcare practitioners and social care providers. The report underscores the significance of integrated care in addressing both physical and social well-being to enhance the quality of life for individuals.
Supporting the Individual Journey through Integrated
Health and Social Care
Contents
INTRODUCTION...........................................................................................................................................2
LO1..............................................................................................................................................................3
P1................................................................................................................................................................4
P2................................................................................................................................................................6
M1...............................................................................................................................................................8
LO 2...........................................................................................................................................................10
P3..............................................................................................................................................................10
P4..............................................................................................................................................................12
M2.............................................................................................................................................................14
LO 3...........................................................................................................................................................16
P5..............................................................................................................................................................16
P6..............................................................................................................................................................18
M3.............................................................................................................................................................20
LO 4...........................................................................................................................................................22
P7..............................................................................................................................................................22
P8..............................................................................................................................................................25
CONCLUSION–......................................................................................................................................27
REFERENCES..............................................................................................................................................29
Health and Social Care
Contents
INTRODUCTION...........................................................................................................................................2
LO1..............................................................................................................................................................3
P1................................................................................................................................................................4
P2................................................................................................................................................................6
M1...............................................................................................................................................................8
LO 2...........................................................................................................................................................10
P3..............................................................................................................................................................10
P4..............................................................................................................................................................12
M2.............................................................................................................................................................14
LO 3...........................................................................................................................................................16
P5..............................................................................................................................................................16
P6..............................................................................................................................................................18
M3.............................................................................................................................................................20
LO 4...........................................................................................................................................................22
P7..............................................................................................................................................................22
P8..............................................................................................................................................................25
CONCLUSION–......................................................................................................................................27
REFERENCES..............................................................................................................................................29
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

INTRODUCTION
Integrated health care is defined as comprehensive care which consists of innovative
and new organizational arrangements that focuses on the integrated form of care that is
care from the various sections of the organization and health and social care sectors
linked together and coordinated to provide care to an individual.
Integrated health care is defined as comprehensive care which consists of innovative
and new organizational arrangements that focuses on the integrated form of care that is
care from the various sections of the organization and health and social care sectors
linked together and coordinated to provide care to an individual.
LO1
Multidisciplinary care is care which includes a range of professionals with their different-
different discipline, experience in particular discipline, knowledge, and skills to give an
inclusive and complete healthcare treatment to an individual at their best possible
outcome depends on the individuals need which are physical and psychological. The
health care and support services available for an individual in London requiring
multidisciplinary are Multidisciplinary team coordinator, General physicians, Clinical
nurse, Surgeons, Physiotherapist, Histopathologist, Radiologist and Dentists.
Multidisciplinary team coordinator
A team coordinator is a person who coordinates between all the sections of
health and social care with the people and staffs related to it and manage to work
together, which results in fulfilment of the requirement of patients and get the
desired outcome.
General physicians
A general physician in a multidisciplinary team will diagnose and handle the
normal sickness and illness and gives basic treatment to people.
Clinical nurse
A clinical nurse supports all the treatments, procedures and diagnosis of a
patient to provide care, advise, support and information to the doctor as well as
to the patient.
Multidisciplinary care is care which includes a range of professionals with their different-
different discipline, experience in particular discipline, knowledge, and skills to give an
inclusive and complete healthcare treatment to an individual at their best possible
outcome depends on the individuals need which are physical and psychological. The
health care and support services available for an individual in London requiring
multidisciplinary are Multidisciplinary team coordinator, General physicians, Clinical
nurse, Surgeons, Physiotherapist, Histopathologist, Radiologist and Dentists.
Multidisciplinary team coordinator
A team coordinator is a person who coordinates between all the sections of
health and social care with the people and staffs related to it and manage to work
together, which results in fulfilment of the requirement of patients and get the
desired outcome.
General physicians
A general physician in a multidisciplinary team will diagnose and handle the
normal sickness and illness and gives basic treatment to people.
Clinical nurse
A clinical nurse supports all the treatments, procedures and diagnosis of a
patient to provide care, advise, support and information to the doctor as well as
to the patient.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
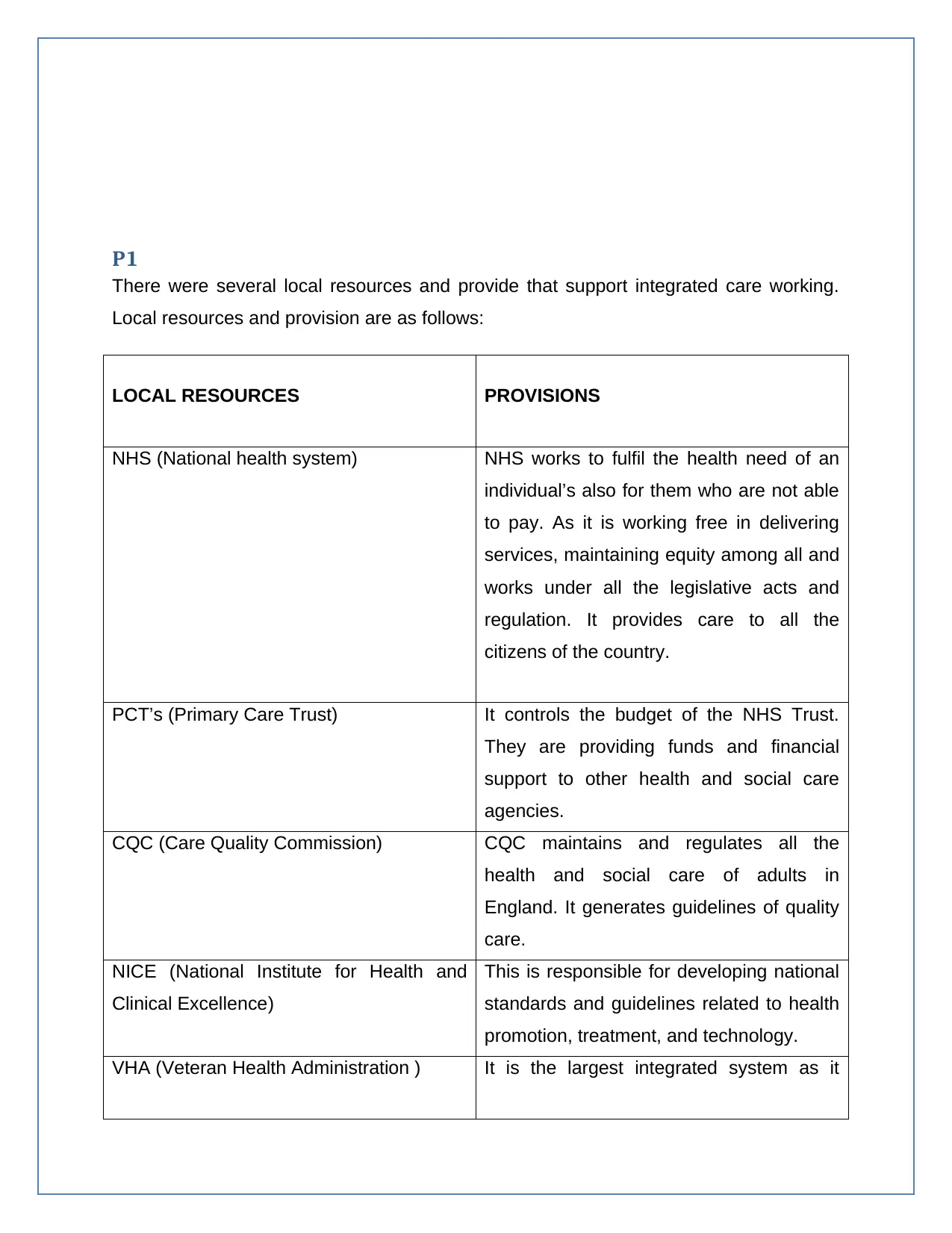
P1
There were several local resources and provide that support integrated care working.
Local resources and provision are as follows:
LOCAL RESOURCES PROVISIONS
NHS (National health system) NHS works to fulfil the health need of an
individual’s also for them who are not able
to pay. As it is working free in delivering
services, maintaining equity among all and
works under all the legislative acts and
regulation. It provides care to all the
citizens of the country.
PCT’s (Primary Care Trust) It controls the budget of the NHS Trust.
They are providing funds and financial
support to other health and social care
agencies.
CQC (Care Quality Commission) CQC maintains and regulates all the
health and social care of adults in
England. It generates guidelines of quality
care.
NICE (National Institute for Health and
Clinical Excellence)
This is responsible for developing national
standards and guidelines related to health
promotion, treatment, and technology.
VHA (Veteran Health Administration ) It is the largest integrated system as it
There were several local resources and provide that support integrated care working.
Local resources and provision are as follows:
LOCAL RESOURCES PROVISIONS
NHS (National health system) NHS works to fulfil the health need of an
individual’s also for them who are not able
to pay. As it is working free in delivering
services, maintaining equity among all and
works under all the legislative acts and
regulation. It provides care to all the
citizens of the country.
PCT’s (Primary Care Trust) It controls the budget of the NHS Trust.
They are providing funds and financial
support to other health and social care
agencies.
CQC (Care Quality Commission) CQC maintains and regulates all the
health and social care of adults in
England. It generates guidelines of quality
care.
NICE (National Institute for Health and
Clinical Excellence)
This is responsible for developing national
standards and guidelines related to health
promotion, treatment, and technology.
VHA (Veteran Health Administration ) It is the largest integrated system as it
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

provides care to veterans only.
LINks (Local Involvement Networks ) It supports patient and people by taking
and understanding their feedbacks.
PALS ( Patient Advice Liaison Service ) It also provides support to patients by
listening to advises and feedbacks about
the care service.
Ambulance service NHS trust This service provides ambulance in case
of emergency as well as also provides
transport facilities for patients.
Child care services It deals with child health and development.
It also helps parents and family to
understand and advice about children. It
protects children and also the decision
making in case of child custody referrals.
LINks (Local Involvement Networks ) It supports patient and people by taking
and understanding their feedbacks.
PALS ( Patient Advice Liaison Service ) It also provides support to patients by
listening to advises and feedbacks about
the care service.
Ambulance service NHS trust This service provides ambulance in case
of emergency as well as also provides
transport facilities for patients.
Child care services It deals with child health and development.
It also helps parents and family to
understand and advice about children. It
protects children and also the decision
making in case of child custody referrals.
P2
An unmet need is described as the needs of the individual under certain age group want
or felt needed in health care but does not receive it, because of some factors such as
long waiting lists, lack of financial support, knowledge and information and
transportation problems. As unmet need also includes the unsatisfactory method of
diagnosis treatment, delay in treatment or poor quality work. For the needs to be
fulfilled, people need to express them to the authorities and if the needs expressed and
not met then they are referred to unmet needs. In England, the unmet needs of people
are described below (Lewis et al, 2003).
Poverty
There are many people whose demands are not met as they live in a low
socioeconomic culture where not many facilities are available. In terms of food, clothing,
lifestyle, children and adults suffer due to low pay and unmet needs (Hood, 2017). It
was observed that 330,000 houses were required in Great Britain with a safe and clean
environment and surrounding to solve issues like homelessness and crowding. 2017
polls of UK on poverty suggest 14 million people suffering from poverty o corresponding
to 1 in every 5 people is suffering. Off these 14 million people, 8.1 million are adults, 4.1
million are children and 1.9 million are aged people (Statistics on poverty England,
2018).
Mental health
Work satisfaction and mental needs are very much necessary for the government for
the accurate functioning of the economy. It is required to focus on the polls that suggest
depression and anxiety in 1 of every 6 people in England which suggest that people
require sound mental health which eventually will help the working of government. The
polls in 2018 also suggest that people living in deprived areas are likely to not recover
after psychological therapy which is because of their lifestyle and their everyday
struggle and unmet needs. For every person to be mentally sound, housing, positive
An unmet need is described as the needs of the individual under certain age group want
or felt needed in health care but does not receive it, because of some factors such as
long waiting lists, lack of financial support, knowledge and information and
transportation problems. As unmet need also includes the unsatisfactory method of
diagnosis treatment, delay in treatment or poor quality work. For the needs to be
fulfilled, people need to express them to the authorities and if the needs expressed and
not met then they are referred to unmet needs. In England, the unmet needs of people
are described below (Lewis et al, 2003).
Poverty
There are many people whose demands are not met as they live in a low
socioeconomic culture where not many facilities are available. In terms of food, clothing,
lifestyle, children and adults suffer due to low pay and unmet needs (Hood, 2017). It
was observed that 330,000 houses were required in Great Britain with a safe and clean
environment and surrounding to solve issues like homelessness and crowding. 2017
polls of UK on poverty suggest 14 million people suffering from poverty o corresponding
to 1 in every 5 people is suffering. Off these 14 million people, 8.1 million are adults, 4.1
million are children and 1.9 million are aged people (Statistics on poverty England,
2018).
Mental health
Work satisfaction and mental needs are very much necessary for the government for
the accurate functioning of the economy. It is required to focus on the polls that suggest
depression and anxiety in 1 of every 6 people in England which suggest that people
require sound mental health which eventually will help the working of government. The
polls in 2018 also suggest that people living in deprived areas are likely to not recover
after psychological therapy which is because of their lifestyle and their everyday
struggle and unmet needs. For every person to be mentally sound, housing, positive
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
working environment, governmental support is necessary to prevent stressful situations
regarding living conditions. Also, it is the need of every mental patient receiving
psychological therapy to get through the therapy quickly without any delays but it is
observed that people in Waltham wait for 16 days while in Leicester it is 167 days
(Mental health foundation, 2017).
Maternity and infant care
Women in their pregnancy and infants require immediate care and support from health
care facilities. There are many needs of maternity mother regarding her health, infant
health, immediate check-ups, and regular routine check-ups etc. reports of NHS in 2018
suggested a decline in deliveries in hospitals by 1.6% from 2017-2018. This suggests
women being more comfortable with at home delivery because of delays in
appointments and poor quality work. They find themselves comfortable in a home
environment rather n hospitals. It is a growing concern as at home deliveries can be
lethal and thus serious actions need to be taken (NHS, 2018).
The above categories suggest unmet needs of people which lead to lethal events or
results both for the individual as well as the government.
regarding living conditions. Also, it is the need of every mental patient receiving
psychological therapy to get through the therapy quickly without any delays but it is
observed that people in Waltham wait for 16 days while in Leicester it is 167 days
(Mental health foundation, 2017).
Maternity and infant care
Women in their pregnancy and infants require immediate care and support from health
care facilities. There are many needs of maternity mother regarding her health, infant
health, immediate check-ups, and regular routine check-ups etc. reports of NHS in 2018
suggested a decline in deliveries in hospitals by 1.6% from 2017-2018. This suggests
women being more comfortable with at home delivery because of delays in
appointments and poor quality work. They find themselves comfortable in a home
environment rather n hospitals. It is a growing concern as at home deliveries can be
lethal and thus serious actions need to be taken (NHS, 2018).
The above categories suggest unmet needs of people which lead to lethal events or
results both for the individual as well as the government.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
M1
Healthcare providers are very different from social care providers but if they work
together it can be effective and helpful for the people. Healthcare providers are focused
on providing the health needs of people that are concerned with the diagnosis,
treatment, and prevention of diseases. This sector involves nurses, doctors, and
professionals who help to keep the individual healthy and sound and thus it is required
for them to work effectively to manage the health of every patient. Every patient in
health centres has different needs which are to be fulfilled by healthcare providers for
quick recovery of patients. Health care providers help patients by curing or treating the
disease and the nurses provide necessary support to help people with a certain
disease. Also, emotional attachment of health care providers is not good for their
profession as it can affect them and their work in delivering services. For healthcare
workers, any mistake or error can be lethal to the patient and can risk their life (Naylor
et al, 2010).
Social care providers on the other hand focus on the living conditions of people, support
the vulnerable population, care, and support for homeless people, assisting people in
their daily chores, helping people live independently, helping mentally challenged to
lead life normally and support them to be of importance to themselves and the country.
Healthcare providers are very different from social care providers but if they work
together it can be effective and helpful for the people. Healthcare providers are focused
on providing the health needs of people that are concerned with the diagnosis,
treatment, and prevention of diseases. This sector involves nurses, doctors, and
professionals who help to keep the individual healthy and sound and thus it is required
for them to work effectively to manage the health of every patient. Every patient in
health centres has different needs which are to be fulfilled by healthcare providers for
quick recovery of patients. Health care providers help patients by curing or treating the
disease and the nurses provide necessary support to help people with a certain
disease. Also, emotional attachment of health care providers is not good for their
profession as it can affect them and their work in delivering services. For healthcare
workers, any mistake or error can be lethal to the patient and can risk their life (Naylor
et al, 2010).
Social care providers on the other hand focus on the living conditions of people, support
the vulnerable population, care, and support for homeless people, assisting people in
their daily chores, helping people live independently, helping mentally challenged to
lead life normally and support them to be of importance to themselves and the country.
Social care providers focus not just focus on the physical health of people but provide
social wellbeing as well which is very important for a person. Social wellbeing of a
person is important for a person's mental and physical health. Social care providers help
patients with their overall health and daily work, there is no precision or limit and they
support them for easy independent living. Any error or mistake by the provider is not
lethal to the person and can be managed and social care providers often are attached
to their patients emotionally which helps them connect with them and in turn care and
support them (Andrews et al, 2013).
The collaboration of both healthcare providers and social providers is beneficial for the
patients as they receive both physical health and social wellbeing. Thus it is required for
hospitals to work in collaboration with social services such that people who require
social care and assistance can attain both the services easily and it will be effective for
the patient as well (Hurlburt et al, 2014).
There is much interagency collaboration that can take place for making it easy and
convenient for people. The collaboration of health, housing, and social care will help
people in physical and their mental health. Every agency has its own rules and
regulations and their own way of working and thus working in collaboration with multiple
agencies can be a difficult task (Aarons et al, 2014).
Interagency collaboration is very convenient and helpful for people as they don't have to
run to other services and start the process from the beginning and can easily get
guidance on different available services at one place and receive the benefit. For the
agencies to work in collaboration effectively, it is required for them to understand the
working of every sector and make rules and regulations in their collaboration to help
them avoid issues. Routine conferences and required changes should be made to
facilitate the needs of patients and benefit and health of patient should be the priority of
every agency working together (Schmied et al, 2010).
As for health and social care, working in collaboration will always help both the agencies
as they are similar in function and thus it is easy to merge and help patients receive the
benefit of both the services.
social wellbeing as well which is very important for a person. Social wellbeing of a
person is important for a person's mental and physical health. Social care providers help
patients with their overall health and daily work, there is no precision or limit and they
support them for easy independent living. Any error or mistake by the provider is not
lethal to the person and can be managed and social care providers often are attached
to their patients emotionally which helps them connect with them and in turn care and
support them (Andrews et al, 2013).
The collaboration of both healthcare providers and social providers is beneficial for the
patients as they receive both physical health and social wellbeing. Thus it is required for
hospitals to work in collaboration with social services such that people who require
social care and assistance can attain both the services easily and it will be effective for
the patient as well (Hurlburt et al, 2014).
There is much interagency collaboration that can take place for making it easy and
convenient for people. The collaboration of health, housing, and social care will help
people in physical and their mental health. Every agency has its own rules and
regulations and their own way of working and thus working in collaboration with multiple
agencies can be a difficult task (Aarons et al, 2014).
Interagency collaboration is very convenient and helpful for people as they don't have to
run to other services and start the process from the beginning and can easily get
guidance on different available services at one place and receive the benefit. For the
agencies to work in collaboration effectively, it is required for them to understand the
working of every sector and make rules and regulations in their collaboration to help
them avoid issues. Routine conferences and required changes should be made to
facilitate the needs of patients and benefit and health of patient should be the priority of
every agency working together (Schmied et al, 2010).
As for health and social care, working in collaboration will always help both the agencies
as they are similar in function and thus it is easy to merge and help patients receive the
benefit of both the services.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
LO 2
P3
Lucy is a 75-year-old living alone with her grandchildren and children settled in another
city. She has Alzheimer’s and stays at service home in the UK and is keen on painting,
she loves to live her life independently but her condition led her to the social service
centre. She has asthma and needs to visit her doctor often for check-ups. She also has
a heart condition and takes regular medication for high blood pressure. She had a
severe asthmatic attack and almost lost her life till she was saved by doctors at the
hospital but it is suggested by doctors that she is supported and cared for and that she
will under observation for some days (Oliver, 2012).
Lucy's Alzheimer's along with these health conditions have made her more dependent
on others for her daily work. Managing Lucy is difficult as she forgets about her
conditions and being at the hospital and it becomes difficult to manage her. With her
multiple problems, her needs increase as well. Patient like Lucy require 24/7 care and
support, she needs doctors and nurses to monitor her physical health routinely along
with social care providers to help her and assist her in daily work, she also requires the
support of psychologist and counselling sessions to help her deal with Alzheimer's and
other health condition easily. She requires care providers to be by her side always to
help her with daily work and also to manage her asthma problems (Baillie, 2012).
To support Lucy health care practitioners arranged a wheelchair for her while social
care providers helped her by having a volunteer 24/7 with her to move her around and
help in her daily work. To facilitate with her Alzheimer's regular visit of her psychologist
was made to ensure she was calm and at ease and social providers made the effort to
have normal conversations with her regarding her paintings. To distract her mind,
Healthcare providers along with social care providers set up canvas and paints to help
her be engaged in painting. This will maintain her blood pressure and relax her heart at
the same tie she will not wonder about being in the hospital. Even after being shifted to
the social service centre, Lucy was visited regularly by doctors to check her medical
health and ensure everything is well (Clegg et al, 2013).
P3
Lucy is a 75-year-old living alone with her grandchildren and children settled in another
city. She has Alzheimer’s and stays at service home in the UK and is keen on painting,
she loves to live her life independently but her condition led her to the social service
centre. She has asthma and needs to visit her doctor often for check-ups. She also has
a heart condition and takes regular medication for high blood pressure. She had a
severe asthmatic attack and almost lost her life till she was saved by doctors at the
hospital but it is suggested by doctors that she is supported and cared for and that she
will under observation for some days (Oliver, 2012).
Lucy's Alzheimer's along with these health conditions have made her more dependent
on others for her daily work. Managing Lucy is difficult as she forgets about her
conditions and being at the hospital and it becomes difficult to manage her. With her
multiple problems, her needs increase as well. Patient like Lucy require 24/7 care and
support, she needs doctors and nurses to monitor her physical health routinely along
with social care providers to help her and assist her in daily work, she also requires the
support of psychologist and counselling sessions to help her deal with Alzheimer's and
other health condition easily. She requires care providers to be by her side always to
help her with daily work and also to manage her asthma problems (Baillie, 2012).
To support Lucy health care practitioners arranged a wheelchair for her while social
care providers helped her by having a volunteer 24/7 with her to move her around and
help in her daily work. To facilitate with her Alzheimer's regular visit of her psychologist
was made to ensure she was calm and at ease and social providers made the effort to
have normal conversations with her regarding her paintings. To distract her mind,
Healthcare providers along with social care providers set up canvas and paints to help
her be engaged in painting. This will maintain her blood pressure and relax her heart at
the same tie she will not wonder about being in the hospital. Even after being shifted to
the social service centre, Lucy was visited regularly by doctors to check her medical
health and ensure everything is well (Clegg et al, 2013).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

With all the help and support, there were times when she missed her children and
grandchildren and to keep her happy and ensure her health, her children visited her
every 3rd week to ensure she was healthy. She always was delighted to see her
grandchildren even when she did not recognise them at times. Fulfilling her
requirements and ensuring her health, helped her to be better and improved both her
physical and mental health (Zautra, 2010).
grandchildren and to keep her happy and ensure her health, her children visited her
every 3rd week to ensure she was healthy. She always was delighted to see her
grandchildren even when she did not recognise them at times. Fulfilling her
requirements and ensuring her health, helped her to be better and improved both her
physical and mental health (Zautra, 2010).

P4
The patient centred approach is important to be adapted to facilitate patients in health
and social care centres. Patient centred approach means caring and supporting patients
by considering their choices and need. It is the responsibility of health professionals to
keep patient requirement and choices as the centre of care and treatment and focus on
providing and benefitting patients. Social care providers as well need to work according
to the choices of the patient and prioritise their health and care when treating them.
When care is provided in the best interest of patients, it leads to faster and better
recovery thus helping both patients and care providers (Epstein, 2011).
The patient centred approach is important to be adapted to facilitate patients in health
and social care centres. Patient centred approach means caring and supporting patients
by considering their choices and need. It is the responsibility of health professionals to
keep patient requirement and choices as the centre of care and treatment and focus on
providing and benefitting patients. Social care providers as well need to work according
to the choices of the patient and prioritise their health and care when treating them.
When care is provided in the best interest of patients, it leads to faster and better
recovery thus helping both patients and care providers (Epstein, 2011).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 35
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





