NRSG355: Prioritization and Delegation in Nursing Practice Assignment
VerifiedAdded on 2022/11/10
|13
|3783
|72
Homework Assignment
AI Summary
This assignment solution addresses a scenario-based nursing assessment for NRSG355, covering prioritization and delegation of tasks, collaborative and therapeutic practices, provision and coordination of care, and time management. The solution prioritizes patient needs, detailing rationales for actions and delegations, supported by references. It includes responses to a series of critical incidents, such as a patient collapse, medication errors, and staff shortages, and analyzes the roles of a multidisciplinary team. The assessment also provides a case study analysis focusing on a patient with intellectual impairment and physical injuries, highlighting the need for coordinated care from doctors, nurses, therapists, and social workers. Further, it delves into patient assessment, the use of tools like CURB-65, and the importance of hygiene and vital sign monitoring. The final section focuses on staff allocation, emphasizing the need to assign staff to tasks within their scope of practice to ensure efficient and safe patient care.
NRSG355 2018 |
TEMPLATE: NRSG355 WRITTEN ASSESSMENT
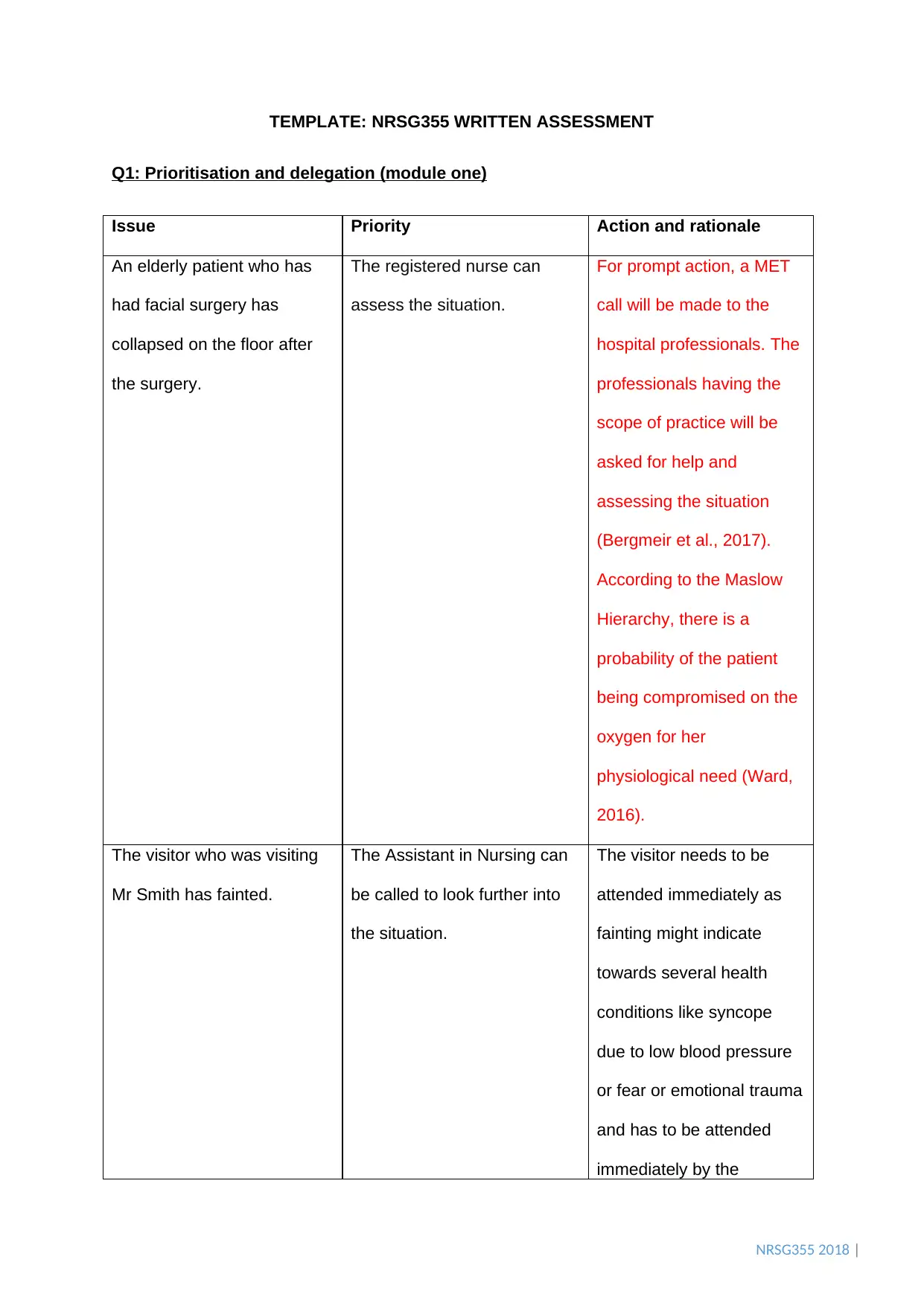
Q1: Prioritisation and delegation (module one)
Issue Priority Action and rationale
An elderly patient who has
had facial surgery has
collapsed on the floor after
the surgery.
The registered nurse can
assess the situation.
For prompt action, a MET
call will be made to the
hospital professionals. The
professionals having the
scope of practice will be
asked for help and
assessing the situation
(Bergmeir et al., 2017).
According to the Maslow
Hierarchy, there is a
probability of the patient
being compromised on the
oxygen for her
physiological need (Ward,
2016).
The visitor who was visiting
Mr Smith has fainted.
The Assistant in Nursing can
be called to look further into
the situation.
The visitor needs to be
attended immediately as
fainting might indicate
towards several health
conditions like syncope
due to low blood pressure
or fear or emotional trauma
and has to be attended
immediately by the
TEMPLATE: NRSG355 WRITTEN ASSESSMENT
Q1: Prioritisation and delegation (module one)
Issue Priority Action and rationale
An elderly patient who has
had facial surgery has
collapsed on the floor after
the surgery.
The registered nurse can
assess the situation.
For prompt action, a MET
call will be made to the
hospital professionals. The
professionals having the
scope of practice will be
asked for help and
assessing the situation
(Bergmeir et al., 2017).
According to the Maslow
Hierarchy, there is a
probability of the patient
being compromised on the
oxygen for her
physiological need (Ward,
2016).
The visitor who was visiting
Mr Smith has fainted.
The Assistant in Nursing can
be called to look further into
the situation.
The visitor needs to be
attended immediately as
fainting might indicate
towards several health
conditions like syncope
due to low blood pressure
or fear or emotional trauma
and has to be attended
immediately by the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NRSG355 2018 |
assistant (Kumaraswami et
al., 2018). The hospital
policy regarding a situation
of a non-hospitalized
individual fainting should
be assessed by a nursing
assistant to check the vital
parameters (Nett et al.,
2018). The AIN has scope
in their practice to code for
blue which revolves around
respiratory or cardiac
arrest (Jackson & Grugan,
2015).
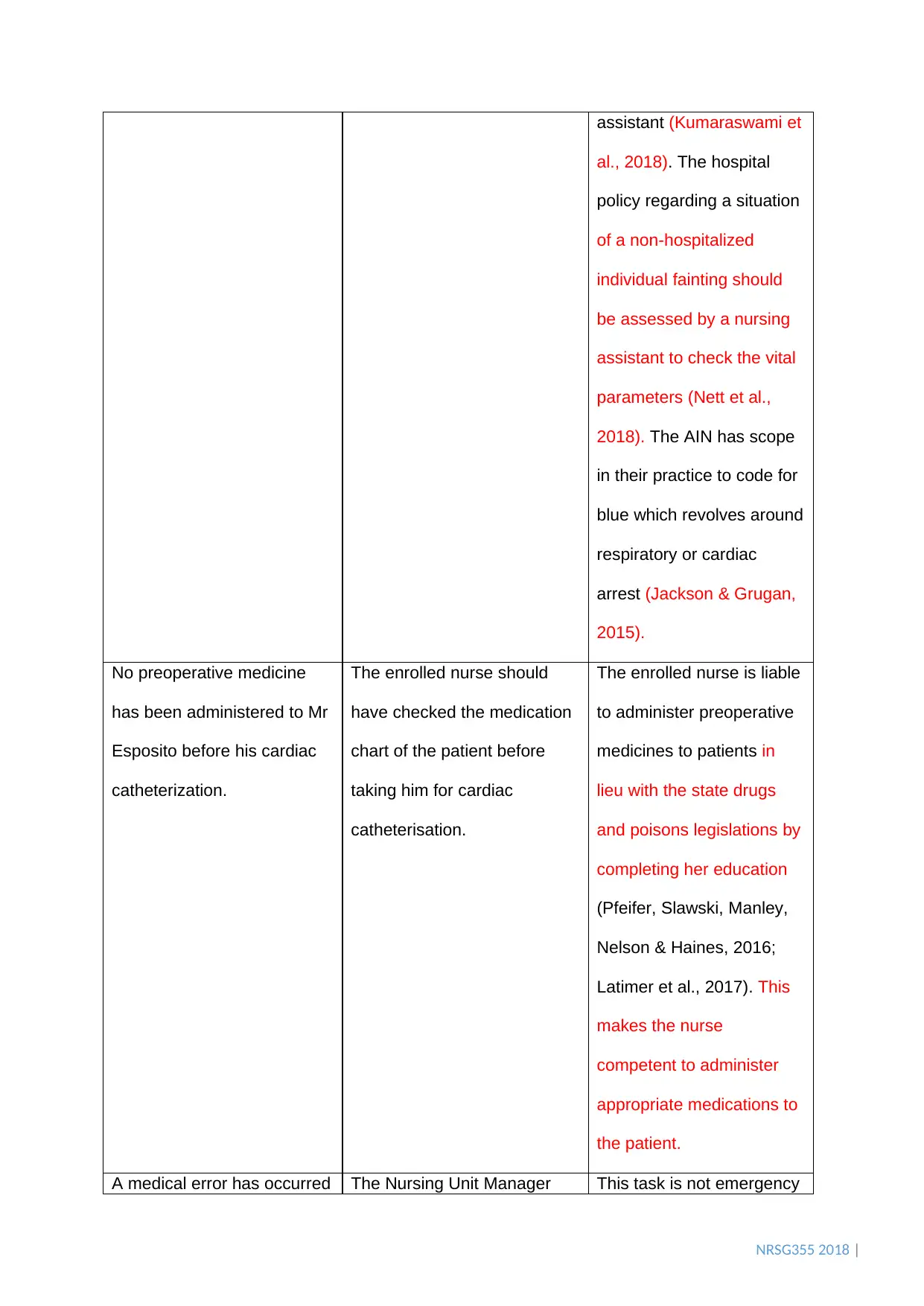
No preoperative medicine
has been administered to Mr
Esposito before his cardiac
catheterization.
The enrolled nurse should
have checked the medication
chart of the patient before
taking him for cardiac
catheterisation.
The enrolled nurse is liable
to administer preoperative
medicines to patients in
lieu with the state drugs
and poisons legislations by
completing her education
(Pfeifer, Slawski, Manley,
Nelson & Haines, 2016;
Latimer et al., 2017). This
makes the nurse
competent to administer
appropriate medications to
the patient.
A medical error has occurred The Nursing Unit Manager This task is not emergency
assistant (Kumaraswami et
al., 2018). The hospital
policy regarding a situation
of a non-hospitalized
individual fainting should
be assessed by a nursing
assistant to check the vital
parameters (Nett et al.,
2018). The AIN has scope
in their practice to code for
blue which revolves around
respiratory or cardiac
arrest (Jackson & Grugan,
2015).
No preoperative medicine
has been administered to Mr
Esposito before his cardiac
catheterization.
The enrolled nurse should
have checked the medication
chart of the patient before
taking him for cardiac
catheterisation.
The enrolled nurse is liable
to administer preoperative
medicines to patients in
lieu with the state drugs
and poisons legislations by
completing her education
(Pfeifer, Slawski, Manley,
Nelson & Haines, 2016;
Latimer et al., 2017). This
makes the nurse
competent to administer
appropriate medications to
the patient.
A medical error has occurred The Nursing Unit Manager This task is not emergency
NRSG355 2018 |
which need to be discussed
at the earliest by the surgical
consultant.
must ensure a priority
discussion with the surgical
consultant about the medical
error.
task Strict action will be
taken against the individual
who is responsible for
conducting a medical error
and placing the life of the
patient in grave danger
(Richter, McAlearney &
Pennell, 2015). This is
because medical error can
cause adverse drug
reactions and can even
react with other drugs
causing anaphylactic
reaction.
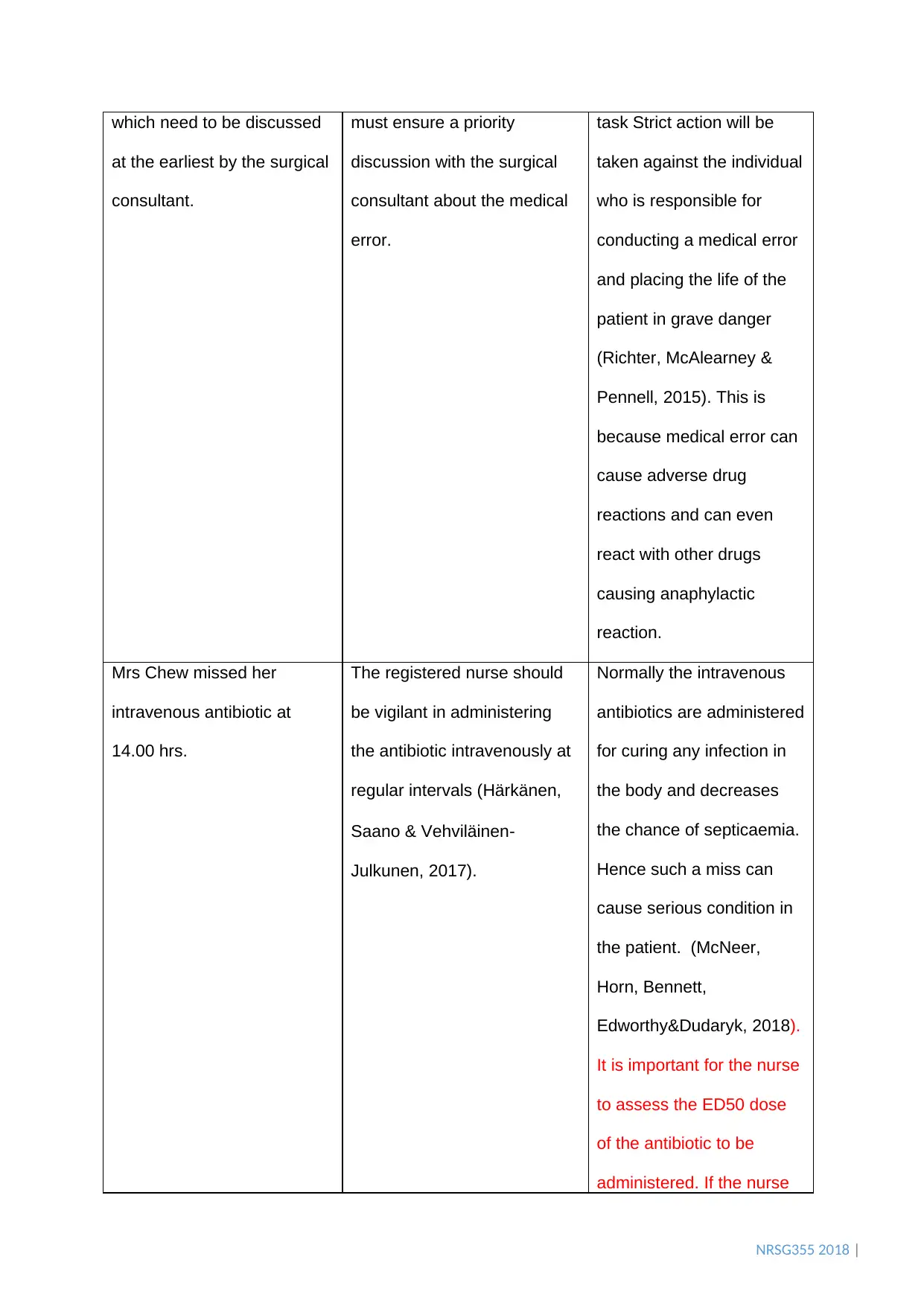
Mrs Chew missed her
intravenous antibiotic at
14.00 hrs.
The registered nurse should
be vigilant in administering
the antibiotic intravenously at
regular intervals (Härkänen,
Saano & Vehviläinen‐
Julkunen, 2017).
Normally the intravenous
antibiotics are administered
for curing any infection in
the body and decreases
the chance of septicaemia.
Hence such a miss can
cause serious condition in
the patient. (McNeer,
Horn, Bennett,
Edworthy&Dudaryk, 2018).
It is important for the nurse
to assess the ED50 dose
of the antibiotic to be
administered. If the nurse
which need to be discussed
at the earliest by the surgical
consultant.
must ensure a priority
discussion with the surgical
consultant about the medical
error.
task Strict action will be
taken against the individual
who is responsible for
conducting a medical error
and placing the life of the
patient in grave danger
(Richter, McAlearney &
Pennell, 2015). This is
because medical error can
cause adverse drug
reactions and can even
react with other drugs
causing anaphylactic
reaction.
Mrs Chew missed her
intravenous antibiotic at
14.00 hrs.
The registered nurse should
be vigilant in administering
the antibiotic intravenously at
regular intervals (Härkänen,
Saano & Vehviläinen‐
Julkunen, 2017).
Normally the intravenous
antibiotics are administered
for curing any infection in
the body and decreases
the chance of septicaemia.
Hence such a miss can
cause serious condition in
the patient. (McNeer,
Horn, Bennett,
Edworthy&Dudaryk, 2018).
It is important for the nurse
to assess the ED50 dose
of the antibiotic to be
administered. If the nurse
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NRSG355 2018 |
can administer it within the
timeframe, then a next
dose can be administered
(Patel et al., 2019).
The toilet for the staff is
overflowing with waste
rapidly pouring out.
The ward clerk is contacted to
clean the toilet to be used by
their staff members.
The waste pouring out can
generate a risk of fall for
the staff and patient
(Watson, 2017). Thus,
overflowing can be stopped
by calling a plumber who
can repair the critical areas
(Watson, 2017).
Q2: Collaborative and Therapeutic practice(module two)
(a)The Multidisciplinary team
i. For an efficient delivery of healthcare service to the patients, there exist certain factors
that help in determining which medical professionals are required depending on the
situation of the patient (Schepman, Hansen, De Putter, Batenburg & De Bakker,
2015).Cultural competency, decision-making abilities and communication skills are some
of the factors that are critically assessed in individuals who desire to be part of the
medical team (Brown, Bekker, Davison, Koffman & Schell, 2016). In addition to this,
leadership with a great coordination among the team members by communicating
efficiently with the patient and the team members ensure a better care to the patient with
a positive health outcome (Brown, Bekker, Davison, Koffman & Schell, 2016).
ii. A healthcare multidisciplinary team involves a lot of individuals who belong to different
occupations (Barr & Dowding, 2019). They come together as a team and provide the
patient with the holistic care (Barr & Dowding, 2019). But, for the team to work efficiently,
can administer it within the
timeframe, then a next
dose can be administered
(Patel et al., 2019).
The toilet for the staff is
overflowing with waste
rapidly pouring out.
The ward clerk is contacted to
clean the toilet to be used by
their staff members.
The waste pouring out can
generate a risk of fall for
the staff and patient
(Watson, 2017). Thus,
overflowing can be stopped
by calling a plumber who
can repair the critical areas
(Watson, 2017).
Q2: Collaborative and Therapeutic practice(module two)
(a)The Multidisciplinary team
i. For an efficient delivery of healthcare service to the patients, there exist certain factors
that help in determining which medical professionals are required depending on the
situation of the patient (Schepman, Hansen, De Putter, Batenburg & De Bakker,
2015).Cultural competency, decision-making abilities and communication skills are some
of the factors that are critically assessed in individuals who desire to be part of the
medical team (Brown, Bekker, Davison, Koffman & Schell, 2016). In addition to this,
leadership with a great coordination among the team members by communicating
efficiently with the patient and the team members ensure a better care to the patient with
a positive health outcome (Brown, Bekker, Davison, Koffman & Schell, 2016).
ii. A healthcare multidisciplinary team involves a lot of individuals who belong to different
occupations (Barr & Dowding, 2019). They come together as a team and provide the
patient with the holistic care (Barr & Dowding, 2019). But, for the team to work efficiently,
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NRSG355 2018 |
a leader is an integral part to keep the team together in harmony and deliver the work
(Barr & Dowding, 2019). For a healthcare team, there is no appropriate leader (Fox &
Reeves, 2015). A patient-centred care requires a professional who belongs to the same
profession as the illness suffered by the patient such that better health outcome is
achieved (Fox & Reeves, 2015). Different scenarios with patients require different
professionals who meet the needs of the patient effectively (Fox & Reeves, 2015).
iii. Each and every member of the healthcare multidisciplinary team plays a great role in
ensuring proper functioning of the team (Lawton et al., 2017). The patient who is brought
to obtain treatment is also a part of the healthcare team (Lawton et al., 2017). They are
the most important member as they are an integral part for whom the team is being
constructed (Lawton et al., 2017). It is for them that their needs are evaluated and a
treatment plan is deduced to reduce their suffering (Lawton et al., 2017). Involvement of
the patients in their care is important as they feel informed and have a more empathetic
feel towards their medical condition (Lawton et al., 2017).
(b) Case study name: Robert Hughes Case Study
i. The key issues that are observed in the Robert Hughes Case Study are the inability of
the patient to handle the outbursts towards the staff members while being intellectually
impaired. Proper rehabilitation to the patient is a major concern to control the erratic
behaviours of Robert. The mother is unable to take care of her son due to age and
deteriorating health of her son. Robert was a part of a bicycle accident two months ago
which resulted in his fractures of tibia/fibula and radius. The patient is frequently irritated
by the surrounding environment because of pain associated with the fracture.
Impairment can also cause irritability in the patient which may lead to unruly behaviour
with the staff and family members.
ii. For the management of the patient, a multidisciplinary approach is required to result in a
positive outcome for Robert. Doctors, nurses, physiotherapist, dieticians, occupational
therapist and social workers are typically the members which are involved in providing
a leader is an integral part to keep the team together in harmony and deliver the work
(Barr & Dowding, 2019). For a healthcare team, there is no appropriate leader (Fox &
Reeves, 2015). A patient-centred care requires a professional who belongs to the same
profession as the illness suffered by the patient such that better health outcome is
achieved (Fox & Reeves, 2015). Different scenarios with patients require different
professionals who meet the needs of the patient effectively (Fox & Reeves, 2015).
iii. Each and every member of the healthcare multidisciplinary team plays a great role in
ensuring proper functioning of the team (Lawton et al., 2017). The patient who is brought
to obtain treatment is also a part of the healthcare team (Lawton et al., 2017). They are
the most important member as they are an integral part for whom the team is being
constructed (Lawton et al., 2017). It is for them that their needs are evaluated and a
treatment plan is deduced to reduce their suffering (Lawton et al., 2017). Involvement of
the patients in their care is important as they feel informed and have a more empathetic
feel towards their medical condition (Lawton et al., 2017).
(b) Case study name: Robert Hughes Case Study
i. The key issues that are observed in the Robert Hughes Case Study are the inability of
the patient to handle the outbursts towards the staff members while being intellectually
impaired. Proper rehabilitation to the patient is a major concern to control the erratic
behaviours of Robert. The mother is unable to take care of her son due to age and
deteriorating health of her son. Robert was a part of a bicycle accident two months ago
which resulted in his fractures of tibia/fibula and radius. The patient is frequently irritated
by the surrounding environment because of pain associated with the fracture.
Impairment can also cause irritability in the patient which may lead to unruly behaviour
with the staff and family members.
ii. For the management of the patient, a multidisciplinary approach is required to result in a
positive outcome for Robert. Doctors, nurses, physiotherapist, dieticians, occupational
therapist and social workers are typically the members which are involved in providing
NRSG355 2018 |
the patient with the best care (Reeves, Pelone, Harrison, Goldman & Zwarenstein,
2017). In the case of Robert, each and every member will play a critical role for the
betterment and recovery of the patient (Reeves, Pelone, Harrison, Goldman &
Zwarenstein, 2017). The doctor will evaluate the medical condition of the patient and
administer medications to improve the health. The nurse will provide holistic care with
emotional and mental support for their wellbeing (Rosano et al., 2016). The
physiotherapist and dietician will incorporate proper diet as well as massages to relieve
the patient from the pain (Reeves, Pelone, Harrison, Goldman & Zwarenstein, 2017).
The occupational therapist will ensure delivery of the treatment to make the patient ready
to conduct daily activities. The social worker can ensure proper wellbeing of the mother
as because she is unable to help her son from this medical condition (Ambrose-Miller &
Ashcroft, 2016).
Q3: Provision and coordination of care (module three
i. The registered nurse obtained the handover report from the emergency department
nurse. It mentioned about that a patient aged 93 years had been brought to the hospital
after complaining of abdominal pains. The first question that a nursing professional must
ask in these situations would be about the onset of the abdominal pains (Festic &
Scanlon, 2015). Moreover, the family history needs to be asked to understand the history
of illnesses. It is possible that his family members have been suffering from abdominal
pain which had further deteriorated to an infection (Kikutani et al., 2015). In addition to
this, the kind of social life will ascertain the mental and social wellbeing of the patient
(Kikutani et al., 2015). Further symptoms like shortness of breath, tightness in the chest
and pain will be asked to understand the intensity of the pain and the breathing pattern
experienced by the patient (Kikutani et al., 2015). It will be mandatory to ask whether he
suffers from any form of infection before medications are administered to him as
otherwise, an allergic reaction can occur (Kerr et al., 2016). In addition to this, any form
the patient with the best care (Reeves, Pelone, Harrison, Goldman & Zwarenstein,
2017). In the case of Robert, each and every member will play a critical role for the
betterment and recovery of the patient (Reeves, Pelone, Harrison, Goldman &
Zwarenstein, 2017). The doctor will evaluate the medical condition of the patient and
administer medications to improve the health. The nurse will provide holistic care with
emotional and mental support for their wellbeing (Rosano et al., 2016). The
physiotherapist and dietician will incorporate proper diet as well as massages to relieve
the patient from the pain (Reeves, Pelone, Harrison, Goldman & Zwarenstein, 2017).
The occupational therapist will ensure delivery of the treatment to make the patient ready
to conduct daily activities. The social worker can ensure proper wellbeing of the mother
as because she is unable to help her son from this medical condition (Ambrose-Miller &
Ashcroft, 2016).
Q3: Provision and coordination of care (module three
i. The registered nurse obtained the handover report from the emergency department
nurse. It mentioned about that a patient aged 93 years had been brought to the hospital
after complaining of abdominal pains. The first question that a nursing professional must
ask in these situations would be about the onset of the abdominal pains (Festic &
Scanlon, 2015). Moreover, the family history needs to be asked to understand the history
of illnesses. It is possible that his family members have been suffering from abdominal
pain which had further deteriorated to an infection (Kikutani et al., 2015). In addition to
this, the kind of social life will ascertain the mental and social wellbeing of the patient
(Kikutani et al., 2015). Further symptoms like shortness of breath, tightness in the chest
and pain will be asked to understand the intensity of the pain and the breathing pattern
experienced by the patient (Kikutani et al., 2015). It will be mandatory to ask whether he
suffers from any form of infection before medications are administered to him as
otherwise, an allergic reaction can occur (Kerr et al., 2016). In addition to this, any form
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NRSG355 2018 |
of changes in the vitals are to be asked by the nurse like blood sugar as it may change
due to IV fluid dextrose (Nair et al., 2016). Hygiene is important thus, IV should be
ensured to be clean (Kerr et al., 2016).
ii. For assessments, the nursing professional needs to conduct a test of the vital signs of
the patient like respiratory rate, oxygen saturation rate, heart rate, pulse rate and blood
pressure in addition to a head-to-toe assessment (Festic & Scanlon, 2015). As
assessment tool, CURB-65 is used on patients who are sick and need to be admitted to
the intensive care unit in the hospital (Chen, Wang & Guo 2016). It is an assessment tool
appropriate for people who are above the age of 65 and who have community-acquired
pneumonia (Chen, Wang & Guo 2016). It is perceived that higher the score of the test,
higher is the likeliness of the patient suffering from a life-threatening illness (Kikutani et
al., 2015). Sputum sample and arterial blood gas evaluation can help further in deducing
the extensive prevalence of pneumonia in the body of the patient. Sputum samples are
mainly conducted on patients to analyse the presence of bacterial pneumonia. The most
common forms of bacteria that are detected in the test results are Staphylococcus
aureus and Streptococcus pneumonia (Kikutani et al., 2015). Moreover, the abdominal
pain should be managed with proper management interventions from the nurses
(Gardner, Jaffe & Nelson, 2015). The mobility of the person should be assessed carefully
to understand the degree of disability affecting the walking of the patient (Festic &
Scanlon, 2015). Moreover, full blood counts of the individual need to be evaluated to
understand the number of white blood cells in the blood. It has been observed that
higher the number of white blood cells, higher will be the likeliness of sustaining an
infection (Honda et al., 2016).
Q4: Time management and delegation (module four)
For the scope of this activity, it is required to allocate staff to the patients. However, it
is important to delegate each staff upon their scope of practice. Task allocation model for
of changes in the vitals are to be asked by the nurse like blood sugar as it may change
due to IV fluid dextrose (Nair et al., 2016). Hygiene is important thus, IV should be
ensured to be clean (Kerr et al., 2016).
ii. For assessments, the nursing professional needs to conduct a test of the vital signs of
the patient like respiratory rate, oxygen saturation rate, heart rate, pulse rate and blood
pressure in addition to a head-to-toe assessment (Festic & Scanlon, 2015). As
assessment tool, CURB-65 is used on patients who are sick and need to be admitted to
the intensive care unit in the hospital (Chen, Wang & Guo 2016). It is an assessment tool
appropriate for people who are above the age of 65 and who have community-acquired
pneumonia (Chen, Wang & Guo 2016). It is perceived that higher the score of the test,
higher is the likeliness of the patient suffering from a life-threatening illness (Kikutani et
al., 2015). Sputum sample and arterial blood gas evaluation can help further in deducing
the extensive prevalence of pneumonia in the body of the patient. Sputum samples are
mainly conducted on patients to analyse the presence of bacterial pneumonia. The most
common forms of bacteria that are detected in the test results are Staphylococcus
aureus and Streptococcus pneumonia (Kikutani et al., 2015). Moreover, the abdominal
pain should be managed with proper management interventions from the nurses
(Gardner, Jaffe & Nelson, 2015). The mobility of the person should be assessed carefully
to understand the degree of disability affecting the walking of the patient (Festic &
Scanlon, 2015). Moreover, full blood counts of the individual need to be evaluated to
understand the number of white blood cells in the blood. It has been observed that
higher the number of white blood cells, higher will be the likeliness of sustaining an
infection (Honda et al., 2016).
Q4: Time management and delegation (module four)
For the scope of this activity, it is required to allocate staff to the patients. However, it
is important to delegate each staff upon their scope of practice. Task allocation model for
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NRSG355 2018 |
delegation is thought to be the most efficient method to allocate the professionals with their
tasks (Edwards et al., 2015). There are two registered nurses – myself and another nurse
who is also acting as a Nurse Unit Manager. In addition to this, one enrolled nurse and three
nursing assistants are present. By allocating the staff to their best of practices will ensure a
safe environment for the patients (Edwards et al., 2015). It would be viable to allocate the
NUM/RN to the six patients with an AIN assigned with her. This would help in equal
distribution of the workload with an efficient delivery of care (Edwards et al., 2015). The
enrolled nurse can be assigned to the eight patients with an AIN as a help. AIN’s are
required in a healthcare team as they help the enrolled as well as registered nurses with a
number of tasks. The AIN requires to be working under continuous supervision of the
registered nurse while doing bed making, repositioning and showering the patient. They
require a basic understanding of medical terminologies to provide optimum care (Nursing and
Midwifery Board of Australia, 2016). It is not liable to work beyond their scope of practice while
respecting the dignity, privacy and culture of the patient.
Enrolled nurses are part of the healthcare inter professional team to be aware of the
treatment plans of the patient. It is under their practice to be able to conduct appropriate
tests with the help of the policy in the hospital to assess the situation of the patient (Nursing
and Midwifery Board of Australia, 2016). They are liable to tabulate and document information
about the patient while respecting the cultural diversity to show evidence of the care
provided.
It is the responsibility of the registered nurse to ensure proper functioning of the staff
towards the patients that have been allocated towards them. Building of trust with the patient
will help in effective communication of the treatment and better understanding of the needs
(Nursing and Midwifery Board of Australia, 2016). It is under their framework to promote
wellbeing of the patient by adhering to the guidelines stipulated by the hospital.
delegation is thought to be the most efficient method to allocate the professionals with their
tasks (Edwards et al., 2015). There are two registered nurses – myself and another nurse
who is also acting as a Nurse Unit Manager. In addition to this, one enrolled nurse and three
nursing assistants are present. By allocating the staff to their best of practices will ensure a
safe environment for the patients (Edwards et al., 2015). It would be viable to allocate the
NUM/RN to the six patients with an AIN assigned with her. This would help in equal
distribution of the workload with an efficient delivery of care (Edwards et al., 2015). The
enrolled nurse can be assigned to the eight patients with an AIN as a help. AIN’s are
required in a healthcare team as they help the enrolled as well as registered nurses with a
number of tasks. The AIN requires to be working under continuous supervision of the
registered nurse while doing bed making, repositioning and showering the patient. They
require a basic understanding of medical terminologies to provide optimum care (Nursing and
Midwifery Board of Australia, 2016). It is not liable to work beyond their scope of practice while
respecting the dignity, privacy and culture of the patient.
Enrolled nurses are part of the healthcare inter professional team to be aware of the
treatment plans of the patient. It is under their practice to be able to conduct appropriate
tests with the help of the policy in the hospital to assess the situation of the patient (Nursing
and Midwifery Board of Australia, 2016). They are liable to tabulate and document information
about the patient while respecting the cultural diversity to show evidence of the care
provided.
It is the responsibility of the registered nurse to ensure proper functioning of the staff
towards the patients that have been allocated towards them. Building of trust with the patient
will help in effective communication of the treatment and better understanding of the needs
(Nursing and Midwifery Board of Australia, 2016). It is under their framework to promote
wellbeing of the patient by adhering to the guidelines stipulated by the hospital.

NRSG355 2018 |
Reference List (APA style)
Ambrose-Miller, W., & Ashcroft, R. (2016). Challenges faced by social workers as members
of interprofessional collaborative health care teams. Health & social work, 41(2), 101-
109.
Reference List (APA style)
Ambrose-Miller, W., & Ashcroft, R. (2016). Challenges faced by social workers as members
of interprofessional collaborative health care teams. Health & social work, 41(2), 101-
109.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
NRSG355 2018 |
Barr, J., & Dowding, L. (2019). Leadership in health care. Sage Publications Limited.
Bergmeir, C., Bilgrami, I., Bain, C., Webb, G. I., Orosz, J., & Pilcher, D. (2017). Designing a
more efficient, effective and safe Medical Emergency Team (MET) service using data
analysis. PloS one, 12(12), e0188688.
Brown, E. A., Bekker, H. L., Davison, S. N., Koffman, J., & Schell, J. O. (2016). Supportive
care: Communication strategies to improve cultural competence in shared decision
making. Clinical Journal of the American Society of Nephrology, 11(10), 1902-1908.
Chen, Y. X., Wang, J. Y., & Guo, S. B. (2016). Use of CRB-65 and quick Sepsis-related
Organ Failure Assessment to predict site of care and mortality in pneumonia patients in
the emergency department: a retrospective study. Critical Care, 20(1), 167.
Edwards, S. T., Rubenstein, L. V., Meredith, L. S., Hackbarth, N. S., Stockdale, S. E.,
Cordasco, K. M., ... & Yano, E. M. (2015, September). Who is responsible for what
tasks within primary care: perceived task allocation among primary care providers
and interdisciplinary team members. In Healthcare (Vol. 3, No. 3, pp. 142-149).
Elsevier.
Festic, E., & Scanlon, P. D. (2015). Incident pneumonia and mortality in patients with chronic
obstructive pulmonary disease. A double effect of inhaled corticosteroids?.American
journal of respiratory and critical care medicine, 191(2), 141-148.
Fox, A., & Reeves, S. (2015). Interprofessional collaborative patient-centred care: a critical
exploration of two related discourses. Journal of Interprofessional Care, 29(2), 113-
118.
Gardner, C. S., Jaffe, T. A., & Nelson, R. C. (2015). Impact of CT in elderly patients
presenting to the emergency department with acute abdominal pain. Abdominal
imaging, 40(7), 2877-2882.
Härkänen, M., Saano, S., & Vehviläinen‐Julkunen, K. (2017). Using incident reports to inform
the prevention of medication administration errors. Journal of clinical nursing, 26(21-
22), 3486-3499.
Barr, J., & Dowding, L. (2019). Leadership in health care. Sage Publications Limited.
Bergmeir, C., Bilgrami, I., Bain, C., Webb, G. I., Orosz, J., & Pilcher, D. (2017). Designing a
more efficient, effective and safe Medical Emergency Team (MET) service using data
analysis. PloS one, 12(12), e0188688.
Brown, E. A., Bekker, H. L., Davison, S. N., Koffman, J., & Schell, J. O. (2016). Supportive
care: Communication strategies to improve cultural competence in shared decision
making. Clinical Journal of the American Society of Nephrology, 11(10), 1902-1908.
Chen, Y. X., Wang, J. Y., & Guo, S. B. (2016). Use of CRB-65 and quick Sepsis-related
Organ Failure Assessment to predict site of care and mortality in pneumonia patients in
the emergency department: a retrospective study. Critical Care, 20(1), 167.
Edwards, S. T., Rubenstein, L. V., Meredith, L. S., Hackbarth, N. S., Stockdale, S. E.,
Cordasco, K. M., ... & Yano, E. M. (2015, September). Who is responsible for what
tasks within primary care: perceived task allocation among primary care providers
and interdisciplinary team members. In Healthcare (Vol. 3, No. 3, pp. 142-149).
Elsevier.
Festic, E., & Scanlon, P. D. (2015). Incident pneumonia and mortality in patients with chronic
obstructive pulmonary disease. A double effect of inhaled corticosteroids?.American
journal of respiratory and critical care medicine, 191(2), 141-148.
Fox, A., & Reeves, S. (2015). Interprofessional collaborative patient-centred care: a critical
exploration of two related discourses. Journal of Interprofessional Care, 29(2), 113-
118.
Gardner, C. S., Jaffe, T. A., & Nelson, R. C. (2015). Impact of CT in elderly patients
presenting to the emergency department with acute abdominal pain. Abdominal
imaging, 40(7), 2877-2882.
Härkänen, M., Saano, S., & Vehviläinen‐Julkunen, K. (2017). Using incident reports to inform
the prevention of medication administration errors. Journal of clinical nursing, 26(21-
22), 3486-3499.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
NRSG355 2018 |
Honda, T., Uehara, T., Matsumoto, G., Arai, S., & Sugano, M. (2016). Neutrophil left shift
and white blood cell count as markers of bacterial infection. Clinica chimica
acta, 457, 46-53.
Jackson, J. E., & Grugan, A. S. (2015). Code blue: Do you know what to
do?. Nursing2019, 45(5), 34-39.
Kerr, D., Klim, S., Kelly, A. M., & McCann, T. (2016). Impact of a modified nursing handover
model for improving nursing care and documentation in the emergency department:
A pre‐and post‐implementation study. International journal of nursing practice, 22(1),
89-97.
Kikutani, T., Tamura, F., Tashiro, H., Yoshida, M., Konishi, K., & Hamada, R. (2015).
Relationship between oral bacteria count and pneumonia onset in elderly nursing
home residents. Geriatrics & gerontology international, 15(4), 417-421.
Latimer, S., Hewitt, J., Stanbrough, R., & McAndrew, R. (2017). Reducing medication errors:
Teaching strategies that increase nursing students' awareness of medication errors
and their prevention.
Lawton, R., O'Hara, J. K., Sheard, L., Armitage, G., Cocks, K., Buckley, H., ...& Watt, I.
(2017). Can patient involvement improve patient safety? A cluster randomised control
trial of the Patient Reporting and Action for a Safe Environment (PRASE)
intervention. BMJ Qual Saf, 26(8), 622-631.
McNeer, R. R., Horn, D. B., Bennett, C. L., Edworthy, J. R., & Dudaryk, R. (2018). Auditory
icon alarms are more accurately and quickly identified than current standard melodic
alarms in a simulated clinical setting. Anesthesiology: The Journal of the American
Society of Anesthesiologists, 129(1), 58-66.
Nair, B. G., Grunzweig, K., Peterson, G. N., Horibe, M., Neradilek, M. B., Newman, S. F., ...
& Dellinger, E. P. (2016). Intraoperative blood glucose management: impact of a real-
time decision support system on adherence to institutional protocol. Journal of clinical
monitoring and computing, 30(3), 301-312.
Honda, T., Uehara, T., Matsumoto, G., Arai, S., & Sugano, M. (2016). Neutrophil left shift
and white blood cell count as markers of bacterial infection. Clinica chimica
acta, 457, 46-53.
Jackson, J. E., & Grugan, A. S. (2015). Code blue: Do you know what to
do?. Nursing2019, 45(5), 34-39.
Kerr, D., Klim, S., Kelly, A. M., & McCann, T. (2016). Impact of a modified nursing handover
model for improving nursing care and documentation in the emergency department:
A pre‐and post‐implementation study. International journal of nursing practice, 22(1),
89-97.
Kikutani, T., Tamura, F., Tashiro, H., Yoshida, M., Konishi, K., & Hamada, R. (2015).
Relationship between oral bacteria count and pneumonia onset in elderly nursing
home residents. Geriatrics & gerontology international, 15(4), 417-421.
Latimer, S., Hewitt, J., Stanbrough, R., & McAndrew, R. (2017). Reducing medication errors:
Teaching strategies that increase nursing students' awareness of medication errors
and their prevention.
Lawton, R., O'Hara, J. K., Sheard, L., Armitage, G., Cocks, K., Buckley, H., ...& Watt, I.
(2017). Can patient involvement improve patient safety? A cluster randomised control
trial of the Patient Reporting and Action for a Safe Environment (PRASE)
intervention. BMJ Qual Saf, 26(8), 622-631.
McNeer, R. R., Horn, D. B., Bennett, C. L., Edworthy, J. R., & Dudaryk, R. (2018). Auditory
icon alarms are more accurately and quickly identified than current standard melodic
alarms in a simulated clinical setting. Anesthesiology: The Journal of the American
Society of Anesthesiologists, 129(1), 58-66.
Nair, B. G., Grunzweig, K., Peterson, G. N., Horibe, M., Neradilek, M. B., Newman, S. F., ...
& Dellinger, E. P. (2016). Intraoperative blood glucose management: impact of a real-
time decision support system on adherence to institutional protocol. Journal of clinical
monitoring and computing, 30(3), 301-312.
NRSG355 2018 |
Nursing and Midwifery Board of Australia. (2016). Enrolled nurse standards for practice.
Retrieved from http://www.nurdingmidwiferyboard.gov.au/Codes-Guidelines-
Statements/ Professional-standards.aspx
Nursing and Midwifery Board of Australia. (2016). Registered nurse standards for practice.
Retrieved from http://www.nurdingmidwiferyboard.gov.au/Codes-Guidelines-
Statements/ Professional-standards.aspx
Patel, C. N., Swartz, M. D., Tomasek, J. S., Vincent, L. E., Hallum, W. E., & Holcomb, J. B.
(2019). The effects of missed doses of antibiotics on hospitalized patient
outcomes. Journal of Surgical Research, 233, 276-283.
Pfeifer, K., Slawski, B., Manley, A. M., Nelson, V., & Haines, M. (2016). Improving
preoperative medication compliance with standardized instructions. Minerva
anestesiologica, 82(1), 44-49.
Reeves, S., Pelone, F., Harrison, R., Goldman, J., & Zwarenstein, M. (2017).
Interprofessional collaboration to improve professional practice and healthcare
outcomes. Cochrane Database of Systematic Reviews, (6).
Richter, J. P., McAlearney, A. S., & Pennell, M. L. (2015). Evaluating the effect of safety
culture on error reporting: a comparison of managerial and staff
perspectives. American Journal of Medical Quality, 30(6), 550-558.
Rosano, C., Perera, S., Inzitari, M., Newman, A. B., Longstreth, W. T., & Studenski, S.
(2016). Digit symbol substitution test and future clinical and subclinical disorders of
cognition, mobility and mood in older adults. Age and ageing, 45(5), 688-695.
Schepman, S., Hansen, J., De Putter, I. D., Batenburg, R. S., & De Bakker, D. H. (2015).
The common characteristics and outcomes of multidisciplinary collaboration in
primary health care: a systematic literature review. International journal of integrated
care, 15.
Ward, T. D. (2016). Think Like a Nurse: A Critical Thinking Initiative. ABNF Journal, 27(3).
Nursing and Midwifery Board of Australia. (2016). Enrolled nurse standards for practice.
Retrieved from http://www.nurdingmidwiferyboard.gov.au/Codes-Guidelines-
Statements/ Professional-standards.aspx
Nursing and Midwifery Board of Australia. (2016). Registered nurse standards for practice.
Retrieved from http://www.nurdingmidwiferyboard.gov.au/Codes-Guidelines-
Statements/ Professional-standards.aspx
Patel, C. N., Swartz, M. D., Tomasek, J. S., Vincent, L. E., Hallum, W. E., & Holcomb, J. B.
(2019). The effects of missed doses of antibiotics on hospitalized patient
outcomes. Journal of Surgical Research, 233, 276-283.
Pfeifer, K., Slawski, B., Manley, A. M., Nelson, V., & Haines, M. (2016). Improving
preoperative medication compliance with standardized instructions. Minerva
anestesiologica, 82(1), 44-49.
Reeves, S., Pelone, F., Harrison, R., Goldman, J., & Zwarenstein, M. (2017).
Interprofessional collaboration to improve professional practice and healthcare
outcomes. Cochrane Database of Systematic Reviews, (6).
Richter, J. P., McAlearney, A. S., & Pennell, M. L. (2015). Evaluating the effect of safety
culture on error reporting: a comparison of managerial and staff
perspectives. American Journal of Medical Quality, 30(6), 550-558.
Rosano, C., Perera, S., Inzitari, M., Newman, A. B., Longstreth, W. T., & Studenski, S.
(2016). Digit symbol substitution test and future clinical and subclinical disorders of
cognition, mobility and mood in older adults. Age and ageing, 45(5), 688-695.
Schepman, S., Hansen, J., De Putter, I. D., Batenburg, R. S., & De Bakker, D. H. (2015).
The common characteristics and outcomes of multidisciplinary collaboration in
primary health care: a systematic literature review. International journal of integrated
care, 15.
Ward, T. D. (2016). Think Like a Nurse: A Critical Thinking Initiative. ABNF Journal, 27(3).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





