HLTH 1037 - Mental Health OSCA Assessment 2: ISBAR Clinical Handover
VerifiedAdded on 2022/08/24
|5
|2836
|19
Practical Assignment
AI Summary
This assignment presents a comprehensive ISBAR (Identify, Situation, Background, Assessment, Recommendation) clinical handover and Mental State Examination (MSE) for a patient presenting with symptoms indicative of a psychotic disorder. The patient, identified as Andy, a male in his late 20s, is experiencing delusions, specifically believing his housemates are associated with MI5 and are attempting to harm him. The situation details his presenting issues including auditory hallucinations, paranoid thoughts, and a decline in appetite due to fear of poisoning. The background reveals no prior psychiatric history, but significant substance use, including daily cannabis use and weekly amphetamine injections. The assessment notes the patient's distressed state, suicidal ideation, and potential risk to others. The recommendations include immediate intervention with antipsychotic medications, cognitive behavioral therapy, and multidisciplinary care involving regular psychiatrist and family doctor check-ins. The MSE details the patient's appearance, behavior, communication, affect, and perceptions, all of which support the diagnosis of a psychotic disorder. The document serves as a clinical handover, providing a clear and concise summary of the patient's condition and the plan of care.
TEMPLATE TO COMPLETE
HLTH 1037 – Mental Health OSCA Assessment 2
Complete the following ISBAR clinical handover as if you were the
Registered Nurse handing this client over to the next shift
ISBAR Clinical Handover
Identify the client:
Identify the client as much as you can. Name, age, gender DOB , MRN no#
The Patient’s name is Andy. He is a male, roughly in the late 20s.
Situation:
Presenting Issue – what is the main reason they have presented today? Current problems
* Recent Significant Events or Stressors – that may have contributed to the current presentation
* Symptoms (Sleep, Concentration, Energy, Appetite, Weight)
* Change in Frequency, Intensity, Duration of Symptoms
* Collateral – Information gained from other resources to support or refute the presentation
Client location ,status under Mental Health Act
The patient is redirected to a psychiatrist by the patient’s family doctor. The patient complains of abnormal
perception about the housemates, how they are associated with MI5 along with the university professor and
how they want to get him out.
The patient states that he has been suffering from stressing vents for the past two months. The patient
informs that he can hear sounds of housemates all the time even when they are not there. Andy states that
thoughts that are not of his own are being put into his mind by the housemates and complains watching
shows like Coronation Street that he would never watch on his own.
Duration of symptoms is 2 months, with no specific details mentioned for intensity of frequency of duration.
The patient is feeling insecure living with his housemates and is facing issue in concentrating. He has
reduced the intake of food due to fear of poisoning, indicative of increased appetite and reduced weight.
The patient states that his housemates have installed some kind of chip in his brain and are inputting
thoughts all the time. The chip is stated as tracking device and patient feels awkward sensation due to the
chip in his head.
The patients mention that he is having too much thoughts in the past couple of months and want to get rid
of them if possible.
The patient is not feeling safe eating food in the house, thinking it might have been poisoned by the
housemates and hence is eating less food.
Under the Mental Health Act 2015, the patient can be confirmed to have mental illness and is suffering from
psychotic disorder.
The mother of the client has requested the client to be redirected to psychiatrist by the doctor and has
presented that the client is facing distressing events.
Background:
Current diagnosis if known
1. Diagnosis if known.
2. How / When / Why did the patient present to Hospital.
3. Relevant history / Physical health.
4. Medications and allergies.
5. Primary carer.
6. Accommodation.
* Current Living Situation / Accommodation
* Significant Relationships
* Developmental History
* Psychiatric History – previous history
* Current Medication – include all medication and herbal supplements
* Drug and Alcohol and Gambling History
* Family History – especially psychiatric history
HLTH 1037 – Mental Health OSCA Assessment 2
Complete the following ISBAR clinical handover as if you were the
Registered Nurse handing this client over to the next shift
ISBAR Clinical Handover
Identify the client:
Identify the client as much as you can. Name, age, gender DOB , MRN no#
The Patient’s name is Andy. He is a male, roughly in the late 20s.
Situation:
Presenting Issue – what is the main reason they have presented today? Current problems
* Recent Significant Events or Stressors – that may have contributed to the current presentation
* Symptoms (Sleep, Concentration, Energy, Appetite, Weight)
* Change in Frequency, Intensity, Duration of Symptoms
* Collateral – Information gained from other resources to support or refute the presentation
Client location ,status under Mental Health Act
The patient is redirected to a psychiatrist by the patient’s family doctor. The patient complains of abnormal
perception about the housemates, how they are associated with MI5 along with the university professor and
how they want to get him out.
The patient states that he has been suffering from stressing vents for the past two months. The patient
informs that he can hear sounds of housemates all the time even when they are not there. Andy states that
thoughts that are not of his own are being put into his mind by the housemates and complains watching
shows like Coronation Street that he would never watch on his own.
Duration of symptoms is 2 months, with no specific details mentioned for intensity of frequency of duration.
The patient is feeling insecure living with his housemates and is facing issue in concentrating. He has
reduced the intake of food due to fear of poisoning, indicative of increased appetite and reduced weight.
The patient states that his housemates have installed some kind of chip in his brain and are inputting
thoughts all the time. The chip is stated as tracking device and patient feels awkward sensation due to the
chip in his head.
The patients mention that he is having too much thoughts in the past couple of months and want to get rid
of them if possible.
The patient is not feeling safe eating food in the house, thinking it might have been poisoned by the
housemates and hence is eating less food.
Under the Mental Health Act 2015, the patient can be confirmed to have mental illness and is suffering from
psychotic disorder.
The mother of the client has requested the client to be redirected to psychiatrist by the doctor and has
presented that the client is facing distressing events.
Background:
Current diagnosis if known
1. Diagnosis if known.
2. How / When / Why did the patient present to Hospital.
3. Relevant history / Physical health.
4. Medications and allergies.
5. Primary carer.
6. Accommodation.
* Current Living Situation / Accommodation
* Significant Relationships
* Developmental History
* Psychiatric History – previous history
* Current Medication – include all medication and herbal supplements
* Drug and Alcohol and Gambling History
* Family History – especially psychiatric history
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
* Previous Treatment / Medication
* Relevant Health / Medical Problems
* Domestic Violence
* Psychosocial
* Allergies – food as well as medication allergies
The patient is currently living with his two housemates in a different place, isolated from his family.
The patient feels comfortable in living with his mother, but does not want to do so as he thinks his
housemates might harm her.
No previous history of mental illness has been mentioned by the patient.
The patient has not been prescribed any medication.
The patient describes himself as general fit with no issues in physical health.
The patient does not drink much alcohol. The patient, however, smokes weed every day in high doses.
The patient states that he smokes 10 bags of weed every day approximately.
The patient admits injecting Amphetamines on weekly basis along with friends.
No psychiatric history of the family is presented.
The patient has no complains of domestic violence but fears that his housemates might harm him.
The patient’s psychosocial status is unhealthy with emotional and cognitive dysfunctionality. The patient
feels that he will be safe with his families, but fears that his housemates might harm them too. Moreover, he
believes that the housemates work for the MI5 and want to get him out. The client has thought of committing
suicide by overdosing on pills. The client keeps weapons such as knife and baseball bat with the intention of
harming the housemates. These are evident that the client is facing cognitive dysfunctionality.
Assessment:
In mental health settings clinicians would complete a Mental State Assessment in this section along with
noting the following points
* What are the current clinical signs
* Are they distressed, suicidal or at risk of harming others? For example threatening someone
* Are they engaged with the treatment plan? For example are they compliant with medication?
* What risks to self or others have been identified?
* Any changes to the patients status
1. A summary of the patients current condition or situation.
2. Clinical signs supporting the diagnosis.
3. Any signs of distress / Suicidal risk or harm to others.
4. Any planned diagnostic tests / Procedures Results from tests.
5. Is the patient / Carer engaged with the treatment plan.
6. What risks to self or others have been identified.
The patient is suffering from psychotic disorder. Clinical symptoms of the patient observed are
suspiciousness, difficult in concentrating, withdrawal from family, delusion, suicidal actions and thoughts.
The patient is severely distressed and is have had suicidal thoughts in the past. The patient thought of
committing suicide by overdose of pills.
The patient is at increased risk of harming others, especially the two housemates. The patient has kept a
baseball bat and knife in the room with the thought of harming the two housemates as they have been
disturbing him a lot recently.
The patient currently has not been prescribed any medication plans.
The patient has not voluntarily went for meetings with health care professional. After the meeting with
psychiatrist the patient seems to be more relaxed and open ups critical detail that will guide healthcare
professionals to adopt suitable intervention.
Recommendations:
Plan – what is the plan? immediate and short term, and possible long term plans
* Relevant Health / Medical Problems
* Domestic Violence
* Psychosocial
* Allergies – food as well as medication allergies
The patient is currently living with his two housemates in a different place, isolated from his family.
The patient feels comfortable in living with his mother, but does not want to do so as he thinks his
housemates might harm her.
No previous history of mental illness has been mentioned by the patient.
The patient has not been prescribed any medication.
The patient describes himself as general fit with no issues in physical health.
The patient does not drink much alcohol. The patient, however, smokes weed every day in high doses.
The patient states that he smokes 10 bags of weed every day approximately.
The patient admits injecting Amphetamines on weekly basis along with friends.
No psychiatric history of the family is presented.
The patient has no complains of domestic violence but fears that his housemates might harm him.
The patient’s psychosocial status is unhealthy with emotional and cognitive dysfunctionality. The patient
feels that he will be safe with his families, but fears that his housemates might harm them too. Moreover, he
believes that the housemates work for the MI5 and want to get him out. The client has thought of committing
suicide by overdosing on pills. The client keeps weapons such as knife and baseball bat with the intention of
harming the housemates. These are evident that the client is facing cognitive dysfunctionality.
Assessment:
In mental health settings clinicians would complete a Mental State Assessment in this section along with
noting the following points
* What are the current clinical signs
* Are they distressed, suicidal or at risk of harming others? For example threatening someone
* Are they engaged with the treatment plan? For example are they compliant with medication?
* What risks to self or others have been identified?
* Any changes to the patients status
1. A summary of the patients current condition or situation.
2. Clinical signs supporting the diagnosis.
3. Any signs of distress / Suicidal risk or harm to others.
4. Any planned diagnostic tests / Procedures Results from tests.
5. Is the patient / Carer engaged with the treatment plan.
6. What risks to self or others have been identified.
The patient is suffering from psychotic disorder. Clinical symptoms of the patient observed are
suspiciousness, difficult in concentrating, withdrawal from family, delusion, suicidal actions and thoughts.
The patient is severely distressed and is have had suicidal thoughts in the past. The patient thought of
committing suicide by overdose of pills.
The patient is at increased risk of harming others, especially the two housemates. The patient has kept a
baseball bat and knife in the room with the thought of harming the two housemates as they have been
disturbing him a lot recently.
The patient currently has not been prescribed any medication plans.
The patient has not voluntarily went for meetings with health care professional. After the meeting with
psychiatrist the patient seems to be more relaxed and open ups critical detail that will guide healthcare
professionals to adopt suitable intervention.
Recommendations:
Plan – what is the plan? immediate and short term, and possible long term plans
* What are the specific recommendations for treatment?
* Relevant multidisciplinary considerations
* Recommendations for ongoing care
* Timeframe for care
Adequate diagnosis of the patient reveals requirement of immediate intervention with medications and
therapies.
For immediate short term intervention, antipsychotic medications can be prescribed to the patient to reduce
symptoms of delusions. Short term intervention is critical for the patient to refrain him from having suicidal
thoughts.
Analysing the symptoms of the patient, cognitive behavioural therapy as long term intervention is
recommended. The patient will continue multiple sessions with the counsellor with the aim of changing
thinking system and behaviour. Such long-term intervention is critical to help the patient change their
thinking system, which would help to cure delusion and eliminate its consequences.
Along with cognitive behavioural therapy, the general physicians and psychiatrist are required to keep in
touch with the patient to address any multidisciplinary issue. Scheduled meetings with psychiatrist will help
at keeping a check on the patient’s mental health on regular basis and the family doctor can examine
patient’s vital signs to track any changes.
The family doctor of the patient should recommend medication to address the distress of the patient. Weekly
schedules with the psychiatrist should be made.
The timeframe for long term intervention of cognitive behavioural therapy should be continued for two weeks
and eight sessions to increase the efficacy of the intervention.
Mental State Examination
Appearance:
General Appearance
Note the physical characteristics of the Client their apparent age
Any distinguishing marks or tattoos
Peculiarities of dress use of cosmetics and jewellery
Any vocation indicators
The patient is appeared preoccupied with his own set of thoughts and is confused.
Apparent signs of distress along with distraction is visible with the patient.
The patient is of mid or late 20s.
No peculiarities in the dress use is observed and the patient is decently dressed.
The patient is well-groomed and is co-operating well with the psychiatrist.
No sign of aggression, or hostility is observed in the patient.
No significant movement of hands or legs have been observed and the patient is sitting still with reduced
motor activity.
Behaviour:
Status Posture Gait Gestures Tics Grimaces Tremors Mannerisms
Activity Overactive Underactive Purposeful or Disorganised Stereotypical Graceful Echopraxia Apraxia
Any signs of psychomotor retardation
Facial expression Alert Tense Worried Happy Sad Happy Dreamy Frightened Pained Angry Sneering
Ecstatic Laughing Smiling or Suspicious
* Relevant multidisciplinary considerations
* Recommendations for ongoing care
* Timeframe for care
Adequate diagnosis of the patient reveals requirement of immediate intervention with medications and
therapies.
For immediate short term intervention, antipsychotic medications can be prescribed to the patient to reduce
symptoms of delusions. Short term intervention is critical for the patient to refrain him from having suicidal
thoughts.
Analysing the symptoms of the patient, cognitive behavioural therapy as long term intervention is
recommended. The patient will continue multiple sessions with the counsellor with the aim of changing
thinking system and behaviour. Such long-term intervention is critical to help the patient change their
thinking system, which would help to cure delusion and eliminate its consequences.
Along with cognitive behavioural therapy, the general physicians and psychiatrist are required to keep in
touch with the patient to address any multidisciplinary issue. Scheduled meetings with psychiatrist will help
at keeping a check on the patient’s mental health on regular basis and the family doctor can examine
patient’s vital signs to track any changes.
The family doctor of the patient should recommend medication to address the distress of the patient. Weekly
schedules with the psychiatrist should be made.
The timeframe for long term intervention of cognitive behavioural therapy should be continued for two weeks
and eight sessions to increase the efficacy of the intervention.
Mental State Examination
Appearance:
General Appearance
Note the physical characteristics of the Client their apparent age
Any distinguishing marks or tattoos
Peculiarities of dress use of cosmetics and jewellery
Any vocation indicators
The patient is appeared preoccupied with his own set of thoughts and is confused.
Apparent signs of distress along with distraction is visible with the patient.
The patient is of mid or late 20s.
No peculiarities in the dress use is observed and the patient is decently dressed.
The patient is well-groomed and is co-operating well with the psychiatrist.
No sign of aggression, or hostility is observed in the patient.
No significant movement of hands or legs have been observed and the patient is sitting still with reduced
motor activity.
Behaviour:
Status Posture Gait Gestures Tics Grimaces Tremors Mannerisms
Activity Overactive Underactive Purposeful or Disorganised Stereotypical Graceful Echopraxia Apraxia
Any signs of psychomotor retardation
Facial expression Alert Tense Worried Happy Sad Happy Dreamy Frightened Pained Angry Sneering
Ecstatic Laughing Smiling or Suspicious
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Indifferent Frank Friendly Dramatic Evasive Resentful Sullen Irritable Afraid
Seductive Exhibitionistic Impulsive Embarrassed
The patient is not sitting straight and is moving constantly in distress with the head looking down.
No signs of psychomotor retardation is observed in the patient, as the patient is effectively using hand
gestures to support his speech and responses.
The patient touches forehead and face often to show concern with troubled thoughts.
The patient is confused and has not voluntarily agreed for meeting with the psychiatrist. It is evident with
few responses of ‘I don’t know’ and the patient is looking all around the room confusingly.
The patient is underactive.
The patient is looking in all directions of the room and is distracted during the conduct of the meeting.
The patient is afraid, suspicious and irritated with the housemates.
The patient feels embarrassed while admitting the use of drugs, speed and weed.
Conversation/Communication/Speech:
Is the Clients conversation Soft Loud Stuttering or Hesitant
Is there evidence of an Accent Enunciation or is the Client Mute or evidence of Echolalia
Is there any indication that the conversation speech is Pressured
What is the flow like Even or Uneven
Does the Clients conversation contain references to Disordered Thought or Psychotic thinking.
Is there any evidence of Thought Blocking or Ideas of Reference
The client is soft spoken and the flow of conversation is even between the client and psychiatrist.
No signs of though blocking is observed with the patient as he smoothly addresses every question of the
psychiatrist.
The perception of housemates working for MI5, and they want to hurt him, provides a clear image of the
delusion the client is having, that can be referenced to psychotic thinking of the patient.
No evidence of accent enunciation has been observed with the client and he is speaking smoothly with no
unusual change in the speech volume, intensity or accent.
The patient answers all the question spontaneously showing no signs that the speech is pressured.
Affect/Mood:
Affect = The feeling state inferred by the assessor on the basis of the patients statements appearance and behaviour Is there indication of
Shallowness or Flattening of Affect Is there an indication of Inappropriate Affect or Dissociation between Affect and thought content Note Lability or
Fluctuating Affect
Other descriptors include Aloof Apathetic Complacent Composed Dull Elated Grandiose Recalcitrant Sarcastic Tense Worried Restricted Blunted
Euthymic
Mood = This is the patients subjective statement about their feeling state
The patient is tensed and afraid of the housemates that he is currently living with. The patient feels shallow
and thinks that no one believes him and point out his problem as consequence of smoking weed and taking
drugs.
The patient shows restriction in answering few questions but answers them clearly afterwards.
The patient is worried while sharing personal wrong habits such as smoking weed, pills, and injecting speed
with the psychiatrist, and does not want his mother to know about all this.
The patient wants to live with his parents where he feels safe, but thinks it is better for the parents to not get
involved in his problems. This creates a dilemma in the client and he feels more insecure and alone in his
problem.
Perceptions:
Illusions = Please note any misperceptions of External Stimuli
Hallucinations = False sensory impression without any external basis
Note any Visual Auditory Olfactory Gustatory or Tactile hallucinations
Note any apparent distractibility or possible responses to hallucinations
The patient is distracted as he is looking everywhere in the room during the meeting with psychiatrist.
Patient is having false impression of his housemates and even his parents. The patient is having delusion
that his housemates are associated with MI5 and want to get him out or hurt him. The client also states that
he once thought that his parents might be involved too.
Seductive Exhibitionistic Impulsive Embarrassed
The patient is not sitting straight and is moving constantly in distress with the head looking down.
No signs of psychomotor retardation is observed in the patient, as the patient is effectively using hand
gestures to support his speech and responses.
The patient touches forehead and face often to show concern with troubled thoughts.
The patient is confused and has not voluntarily agreed for meeting with the psychiatrist. It is evident with
few responses of ‘I don’t know’ and the patient is looking all around the room confusingly.
The patient is underactive.
The patient is looking in all directions of the room and is distracted during the conduct of the meeting.
The patient is afraid, suspicious and irritated with the housemates.
The patient feels embarrassed while admitting the use of drugs, speed and weed.
Conversation/Communication/Speech:
Is the Clients conversation Soft Loud Stuttering or Hesitant
Is there evidence of an Accent Enunciation or is the Client Mute or evidence of Echolalia
Is there any indication that the conversation speech is Pressured
What is the flow like Even or Uneven
Does the Clients conversation contain references to Disordered Thought or Psychotic thinking.
Is there any evidence of Thought Blocking or Ideas of Reference
The client is soft spoken and the flow of conversation is even between the client and psychiatrist.
No signs of though blocking is observed with the patient as he smoothly addresses every question of the
psychiatrist.
The perception of housemates working for MI5, and they want to hurt him, provides a clear image of the
delusion the client is having, that can be referenced to psychotic thinking of the patient.
No evidence of accent enunciation has been observed with the client and he is speaking smoothly with no
unusual change in the speech volume, intensity or accent.
The patient answers all the question spontaneously showing no signs that the speech is pressured.
Affect/Mood:
Affect = The feeling state inferred by the assessor on the basis of the patients statements appearance and behaviour Is there indication of
Shallowness or Flattening of Affect Is there an indication of Inappropriate Affect or Dissociation between Affect and thought content Note Lability or
Fluctuating Affect
Other descriptors include Aloof Apathetic Complacent Composed Dull Elated Grandiose Recalcitrant Sarcastic Tense Worried Restricted Blunted
Euthymic
Mood = This is the patients subjective statement about their feeling state
The patient is tensed and afraid of the housemates that he is currently living with. The patient feels shallow
and thinks that no one believes him and point out his problem as consequence of smoking weed and taking
drugs.
The patient shows restriction in answering few questions but answers them clearly afterwards.
The patient is worried while sharing personal wrong habits such as smoking weed, pills, and injecting speed
with the psychiatrist, and does not want his mother to know about all this.
The patient wants to live with his parents where he feels safe, but thinks it is better for the parents to not get
involved in his problems. This creates a dilemma in the client and he feels more insecure and alone in his
problem.
Perceptions:
Illusions = Please note any misperceptions of External Stimuli
Hallucinations = False sensory impression without any external basis
Note any Visual Auditory Olfactory Gustatory or Tactile hallucinations
Note any apparent distractibility or possible responses to hallucinations
The patient is distracted as he is looking everywhere in the room during the meeting with psychiatrist.
Patient is having false impression of his housemates and even his parents. The patient is having delusion
that his housemates are associated with MI5 and want to get him out or hurt him. The client also states that
he once thought that his parents might be involved too.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
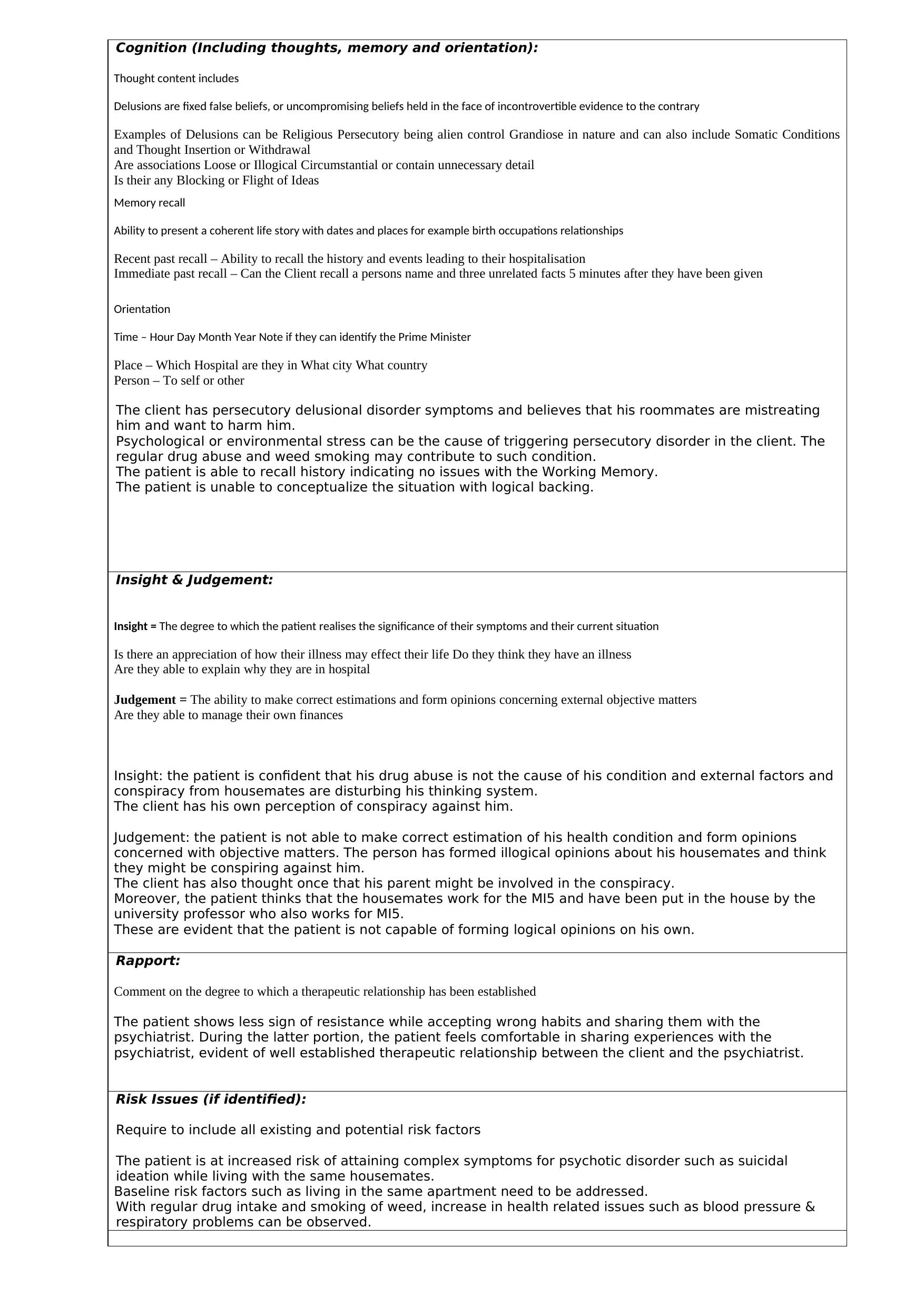
Cognition (Including thoughts, memory and orientation):
Thought content includes
Delusions are fixed false beliefs, or uncompromising beliefs held in the face of incontrovertible evidence to the contrary
Examples of Delusions can be Religious Persecutory being alien control Grandiose in nature and can also include Somatic Conditions
and Thought Insertion or Withdrawal
Are associations Loose or Illogical Circumstantial or contain unnecessary detail
Is their any Blocking or Flight of Ideas
Memory recall
Ability to present a coherent life story with dates and places for example birth occupations relationships
Recent past recall – Ability to recall the history and events leading to their hospitalisation
Immediate past recall – Can the Client recall a persons name and three unrelated facts 5 minutes after they have been given
Orientation
Time – Hour Day Month Year Note if they can identify the Prime Minister
Place – Which Hospital are they in What city What country
Person – To self or other
The client has persecutory delusional disorder symptoms and believes that his roommates are mistreating
him and want to harm him.
Psychological or environmental stress can be the cause of triggering persecutory disorder in the client. The
regular drug abuse and weed smoking may contribute to such condition.
The patient is able to recall history indicating no issues with the Working Memory.
The patient is unable to conceptualize the situation with logical backing.
Insight & Judgement:
Insight = The degree to which the patient realises the significance of their symptoms and their current situation
Is there an appreciation of how their illness may effect their life Do they think they have an illness
Are they able to explain why they are in hospital
Judgement = The ability to make correct estimations and form opinions concerning external objective matters
Are they able to manage their own finances
Insight: the patient is confident that his drug abuse is not the cause of his condition and external factors and
conspiracy from housemates are disturbing his thinking system.
The client has his own perception of conspiracy against him.
Judgement: the patient is not able to make correct estimation of his health condition and form opinions
concerned with objective matters. The person has formed illogical opinions about his housemates and think
they might be conspiring against him.
The client has also thought once that his parent might be involved in the conspiracy.
Moreover, the patient thinks that the housemates work for the MI5 and have been put in the house by the
university professor who also works for MI5.
These are evident that the patient is not capable of forming logical opinions on his own.
Rapport:
Comment on the degree to which a therapeutic relationship has been established
The patient shows less sign of resistance while accepting wrong habits and sharing them with the
psychiatrist. During the latter portion, the patient feels comfortable in sharing experiences with the
psychiatrist, evident of well established therapeutic relationship between the client and the psychiatrist.
Risk Issues (if identified):
Require to include all existing and potential risk factors
The patient is at increased risk of attaining complex symptoms for psychotic disorder such as suicidal
ideation while living with the same housemates.
Baseline risk factors such as living in the same apartment need to be addressed.
With regular drug intake and smoking of weed, increase in health related issues such as blood pressure &
respiratory problems can be observed.
Thought content includes
Delusions are fixed false beliefs, or uncompromising beliefs held in the face of incontrovertible evidence to the contrary
Examples of Delusions can be Religious Persecutory being alien control Grandiose in nature and can also include Somatic Conditions
and Thought Insertion or Withdrawal
Are associations Loose or Illogical Circumstantial or contain unnecessary detail
Is their any Blocking or Flight of Ideas
Memory recall
Ability to present a coherent life story with dates and places for example birth occupations relationships
Recent past recall – Ability to recall the history and events leading to their hospitalisation
Immediate past recall – Can the Client recall a persons name and three unrelated facts 5 minutes after they have been given
Orientation
Time – Hour Day Month Year Note if they can identify the Prime Minister
Place – Which Hospital are they in What city What country
Person – To self or other
The client has persecutory delusional disorder symptoms and believes that his roommates are mistreating
him and want to harm him.
Psychological or environmental stress can be the cause of triggering persecutory disorder in the client. The
regular drug abuse and weed smoking may contribute to such condition.
The patient is able to recall history indicating no issues with the Working Memory.
The patient is unable to conceptualize the situation with logical backing.
Insight & Judgement:
Insight = The degree to which the patient realises the significance of their symptoms and their current situation
Is there an appreciation of how their illness may effect their life Do they think they have an illness
Are they able to explain why they are in hospital
Judgement = The ability to make correct estimations and form opinions concerning external objective matters
Are they able to manage their own finances
Insight: the patient is confident that his drug abuse is not the cause of his condition and external factors and
conspiracy from housemates are disturbing his thinking system.
The client has his own perception of conspiracy against him.
Judgement: the patient is not able to make correct estimation of his health condition and form opinions
concerned with objective matters. The person has formed illogical opinions about his housemates and think
they might be conspiring against him.
The client has also thought once that his parent might be involved in the conspiracy.
Moreover, the patient thinks that the housemates work for the MI5 and have been put in the house by the
university professor who also works for MI5.
These are evident that the patient is not capable of forming logical opinions on his own.
Rapport:
Comment on the degree to which a therapeutic relationship has been established
The patient shows less sign of resistance while accepting wrong habits and sharing them with the
psychiatrist. During the latter portion, the patient feels comfortable in sharing experiences with the
psychiatrist, evident of well established therapeutic relationship between the client and the psychiatrist.
Risk Issues (if identified):
Require to include all existing and potential risk factors
The patient is at increased risk of attaining complex symptoms for psychotic disorder such as suicidal
ideation while living with the same housemates.
Baseline risk factors such as living in the same apartment need to be addressed.
With regular drug intake and smoking of weed, increase in health related issues such as blood pressure &
respiratory problems can be observed.
1 out of 5
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





