(Solved) RCA and FMEA - Assignment
VerifiedAdded on 2020/04/15
|16
|4492
|123
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: RCA and FMEA
RCA AND FMEA
Name of the Student
Name of the University
Author Note
RCA AND FMEA
Name of the Student
Name of the University
Author Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1RCA AND FMEA
Table of Contents
Steps of RCA...................................................................................................................................2
Causes of the scenario.....................................................................................................................3
Process Improvement Plan..............................................................................................................6
Lewin’s change theory.....................................................................................................................7
Purpose of FMEA............................................................................................................................7
FMEA Steps.....................................................................................................................................8
FMEA Table....................................................................................................................................9
Testing of the improvement plan interventions.............................................................................10
Nursing leadership.........................................................................................................................11
Involvement of nurse in RCA and FMEA processes.....................................................................11
Reference List................................................................................................................................12
Table of Contents
Steps of RCA...................................................................................................................................2
Causes of the scenario.....................................................................................................................3
Process Improvement Plan..............................................................................................................6
Lewin’s change theory.....................................................................................................................7
Purpose of FMEA............................................................................................................................7
FMEA Steps.....................................................................................................................................8
FMEA Table....................................................................................................................................9
Testing of the improvement plan interventions.............................................................................10
Nursing leadership.........................................................................................................................11
Involvement of nurse in RCA and FMEA processes.....................................................................11
Reference List................................................................................................................................12
2RCA AND FMEA
Purpose of Root Cause analysis (RCA)
Root cause analysis (RCA) is a problem solving method, which is used for identifying the
root causes of problems and faults associated with a particular process. A factor can be the root
cause if its removal from the process does not prevent the occurrence of the undesirable
outcome. However, if the factor affects the outcomes of an event is not considered to be a root
cause. Root cause is a factor or a part of the process or event, which if corrected can prevent the
occurrence of the problem. RCA focuses on the correction of the root causes in order to solve the
problem and prevent it from recurring in the future. RCA can also be used to predict the
occurrence of adverse events in the future in association with a particular process or method.
RCA identifies the problems, the causes and the necessary prevention measures (Black &
Vernetti, 2015). RCA can be used in various aspects like analysis of healthcare incidents, safety
based situations, change managements or quality control problems, among others. Healthcare
accidents are usually caused as a result of failures on the part of the healthcare officials, work
environments and the underlying failures (Makary & Daniel, 2016).
Steps of RCA
IHI has defined six steps for carrying out an RCA. These steps include:
Step 1: Identify what happened – The RCA team analyzes the process completely and accurately.
In order to understand the problem, the team draws a flow chart of the entire event to identify the
root cause of the undesirable event.
Step 2: Determine what should have happened - The RCA team determines or predicts the
incidents that could have occurred in an ideal situation. They create another flow chart including
the ideal conditions and compares with the flow chart from step 1.
Purpose of Root Cause analysis (RCA)
Root cause analysis (RCA) is a problem solving method, which is used for identifying the
root causes of problems and faults associated with a particular process. A factor can be the root
cause if its removal from the process does not prevent the occurrence of the undesirable
outcome. However, if the factor affects the outcomes of an event is not considered to be a root
cause. Root cause is a factor or a part of the process or event, which if corrected can prevent the
occurrence of the problem. RCA focuses on the correction of the root causes in order to solve the
problem and prevent it from recurring in the future. RCA can also be used to predict the
occurrence of adverse events in the future in association with a particular process or method.
RCA identifies the problems, the causes and the necessary prevention measures (Black &
Vernetti, 2015). RCA can be used in various aspects like analysis of healthcare incidents, safety
based situations, change managements or quality control problems, among others. Healthcare
accidents are usually caused as a result of failures on the part of the healthcare officials, work
environments and the underlying failures (Makary & Daniel, 2016).
Steps of RCA
IHI has defined six steps for carrying out an RCA. These steps include:
Step 1: Identify what happened – The RCA team analyzes the process completely and accurately.
In order to understand the problem, the team draws a flow chart of the entire event to identify the
root cause of the undesirable event.
Step 2: Determine what should have happened - The RCA team determines or predicts the
incidents that could have occurred in an ideal situation. They create another flow chart including
the ideal conditions and compares with the flow chart from step 1.
3RCA AND FMEA
Step 3: Determine causes – In this step, the team determines the factors that are responsible for
the event. The team identifies the most apparent or direct causes and the indirect or contributory
causes. It is necessary for the RCA team to ask “why” at least five times in order to identify the
root cause of the event. A fishbone diagram is used to display the probable causes of an event.
There are various factors that affect the clinical practice and gives rise to medical errors. These
include the characteristics of the patient, members of the healthcare organization, task and team
factors, the working environment, management or organization factors and the institution in
general.
Step 4: Develop causal statements – The causal statement connects the factors with the necessary
outcomes. It provides details about the current condition of the healthcare organization that gave
rise to adverse outcomes with respect to the patient. The causal statement is divided into cause,
effect and outcome.
Step 5: A list of recommended actions are provided in order to prevent such adverse occurrences
in the future. Recommendations can be associated with staff education, instrument
standardization, use of backup systems, preventing mistakes forcibly, updated softwares,
development of new policies, use of checklists and process simplification. The actions to
eliminate the root causes can be classified as strong, intermediate and weak.
Step 6: A summary of the entire event and process is prepared and is shared in the form of a flow
chart to prevent such events in the future (Shaqdan et al., 2014; Www.ihi.org, 2017).
Causes of the scenario
This is the case study of Mr. B, who is a 67 year old patient brought to the emergency
department of the hospital due to severe pain in the hips and legs. His leg appeared swollen, skin
Step 3: Determine causes – In this step, the team determines the factors that are responsible for
the event. The team identifies the most apparent or direct causes and the indirect or contributory
causes. It is necessary for the RCA team to ask “why” at least five times in order to identify the
root cause of the event. A fishbone diagram is used to display the probable causes of an event.
There are various factors that affect the clinical practice and gives rise to medical errors. These
include the characteristics of the patient, members of the healthcare organization, task and team
factors, the working environment, management or organization factors and the institution in
general.
Step 4: Develop causal statements – The causal statement connects the factors with the necessary
outcomes. It provides details about the current condition of the healthcare organization that gave
rise to adverse outcomes with respect to the patient. The causal statement is divided into cause,
effect and outcome.
Step 5: A list of recommended actions are provided in order to prevent such adverse occurrences
in the future. Recommendations can be associated with staff education, instrument
standardization, use of backup systems, preventing mistakes forcibly, updated softwares,
development of new policies, use of checklists and process simplification. The actions to
eliminate the root causes can be classified as strong, intermediate and weak.
Step 6: A summary of the entire event and process is prepared and is shared in the form of a flow
chart to prevent such events in the future (Shaqdan et al., 2014; Www.ihi.org, 2017).
Causes of the scenario
This is the case study of Mr. B, who is a 67 year old patient brought to the emergency
department of the hospital due to severe pain in the hips and legs. His leg appeared swollen, skin
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4RCA AND FMEA
discoloration and showing limited range of motion. He had a previous history of glucose
intolerance and prostrate cancer. Moreover, he has high cholesterol and lipid levels. He takes a
cholesterol lowering medication named Atorvastatin and an opiod named Oxycodone for pain
relief (Gierman et al., 2014; Caraceni et al., 2012). After his evaluation, he is given a 5mg IVP
of Diazepam. Then he is given another dose of hydromorphone (an opioid) 2mg IVP. Next, the
doctor gives another dose of 2mg hydromorphone with 5 mg of diazepam. Mr. B was not
provided with supplemental oxygen, while his ECG and respirations were not monitored. Even
after Mr. B suffers from low oxygen saturation, the LPN resets the oxygen saturation alarm and
carries out the automatic blood pressure monitoring. Later Mr. B’s blood pressure falls
drastically and oxygen saturation was also low. Moreover, the patient was not breathing and had
no detectable pulse rate. He was found to suffer from ventricular fibrillation. Various
interventions were carried out like CPR, IV fluids and vassopressors. Mr. B was not able to
breathe on his own and needed a ventilator. His pupils were dialated and fixed and he showed no
signs of movement. He was taken to a tertiary facility, where seven days later he was declared
brain dead. Mr. B’s life support was removed and he died later on.
The causes and the contributing factors that led to the sentinel event, which is the death
of Mr. B includes the dosage of Diazepam. The recommended dosage of Diazepam for elderly
patients with muscle spasms is 2-2.5mg (Www.healthline.com, 2017). Too much use of this drug
can be toxic. However, Dr. T administered an initial dose of 5mg and later on administered
another 5mg dose, which is highly toxic and lethal. The side effects of diazepam includes
slowing of brain activity, drowsiness, fatigue, ataxia, headache, nausea, convulsions, increased
muscle spasms, depression, jaundice, seizures, among others (Www.netdoctor.co.uk, 2017).
Another factor is the use of Diazepam together with Hydromorphone. Hydromorphone is an
discoloration and showing limited range of motion. He had a previous history of glucose
intolerance and prostrate cancer. Moreover, he has high cholesterol and lipid levels. He takes a
cholesterol lowering medication named Atorvastatin and an opiod named Oxycodone for pain
relief (Gierman et al., 2014; Caraceni et al., 2012). After his evaluation, he is given a 5mg IVP
of Diazepam. Then he is given another dose of hydromorphone (an opioid) 2mg IVP. Next, the
doctor gives another dose of 2mg hydromorphone with 5 mg of diazepam. Mr. B was not
provided with supplemental oxygen, while his ECG and respirations were not monitored. Even
after Mr. B suffers from low oxygen saturation, the LPN resets the oxygen saturation alarm and
carries out the automatic blood pressure monitoring. Later Mr. B’s blood pressure falls
drastically and oxygen saturation was also low. Moreover, the patient was not breathing and had
no detectable pulse rate. He was found to suffer from ventricular fibrillation. Various
interventions were carried out like CPR, IV fluids and vassopressors. Mr. B was not able to
breathe on his own and needed a ventilator. His pupils were dialated and fixed and he showed no
signs of movement. He was taken to a tertiary facility, where seven days later he was declared
brain dead. Mr. B’s life support was removed and he died later on.
The causes and the contributing factors that led to the sentinel event, which is the death
of Mr. B includes the dosage of Diazepam. The recommended dosage of Diazepam for elderly
patients with muscle spasms is 2-2.5mg (Www.healthline.com, 2017). Too much use of this drug
can be toxic. However, Dr. T administered an initial dose of 5mg and later on administered
another 5mg dose, which is highly toxic and lethal. The side effects of diazepam includes
slowing of brain activity, drowsiness, fatigue, ataxia, headache, nausea, convulsions, increased
muscle spasms, depression, jaundice, seizures, among others (Www.netdoctor.co.uk, 2017).
Another factor is the use of Diazepam together with Hydromorphone. Hydromorphone is an
5RCA AND FMEA
opioid that is given to the patients suffering from severe pain. The initial IV dose for
hydromorphone is 0.2mg to 1mg. The side effects of Hydromorphone include drowsiness,
dizziness, nausea, vomiting, flushing, itching, heart problems, vision problems, bowel problems,
problems of the nervous system, high or low blood pressure, shortness of breath, among others
(Ahern et al., 2013). Hydromorphone has also been associated with the development of
ventricular fibrillation and can even lead to cardiac arrest (Mann et al., 2012). The FDA has
issued warnings about the use of Diazepam with opioids like hydromorphone. The use of these
drug combinations can lead to drowsiness, coma, slow breathing and even death (Labianca et al.,
2012). If administered together, it is necessary to constantly monitor the patient. Moreover, apart
from using the two drugs together, Dr. T also administered high doses of hydromorphone. He
gave 2 mg initially and then administered another 2 mg of hydromorphone along with Diazepam,
which is lethal. Moreover, another error is that the vital signs of the patient like heart rate (ECG),
respiration rate, and blood pressure were not monitored following opioid administration
(Addison et al., 2015). However, the patient was kept only in an automatic blood pressure
monitor and was not monitored frequently for heart and respiration rate. Moreover, he was not
provided with an external oxygen supply as high doses of Hydromorphone along with Diazepam
can cause shortness of breath (Gelot, Nekhla & Tuch, 2013). Opioid administration in patients
can lead to decrease in insulin secretion and worsening of diabetes (Cryer, 2013). Moreover,
cholesterol leads to heightened effects of opioid on the human body (Zheng et al., 2012). Dr. T
administered the use of high doses of the opioid Hydromorphone, even knowing that Mr. B
suffers from high cholesterol and glucose intolerance. The doctor also administered Diazepam,
when knowing that the patient consumes drugs like Oxycodone and Atorvastatin. Oxycodone is
an opioid that along with Diazepam can lead to coma, respiratory distress and death. This also
opioid that is given to the patients suffering from severe pain. The initial IV dose for
hydromorphone is 0.2mg to 1mg. The side effects of Hydromorphone include drowsiness,
dizziness, nausea, vomiting, flushing, itching, heart problems, vision problems, bowel problems,
problems of the nervous system, high or low blood pressure, shortness of breath, among others
(Ahern et al., 2013). Hydromorphone has also been associated with the development of
ventricular fibrillation and can even lead to cardiac arrest (Mann et al., 2012). The FDA has
issued warnings about the use of Diazepam with opioids like hydromorphone. The use of these
drug combinations can lead to drowsiness, coma, slow breathing and even death (Labianca et al.,
2012). If administered together, it is necessary to constantly monitor the patient. Moreover, apart
from using the two drugs together, Dr. T also administered high doses of hydromorphone. He
gave 2 mg initially and then administered another 2 mg of hydromorphone along with Diazepam,
which is lethal. Moreover, another error is that the vital signs of the patient like heart rate (ECG),
respiration rate, and blood pressure were not monitored following opioid administration
(Addison et al., 2015). However, the patient was kept only in an automatic blood pressure
monitor and was not monitored frequently for heart and respiration rate. Moreover, he was not
provided with an external oxygen supply as high doses of Hydromorphone along with Diazepam
can cause shortness of breath (Gelot, Nekhla & Tuch, 2013). Opioid administration in patients
can lead to decrease in insulin secretion and worsening of diabetes (Cryer, 2013). Moreover,
cholesterol leads to heightened effects of opioid on the human body (Zheng et al., 2012). Dr. T
administered the use of high doses of the opioid Hydromorphone, even knowing that Mr. B
suffers from high cholesterol and glucose intolerance. The doctor also administered Diazepam,
when knowing that the patient consumes drugs like Oxycodone and Atorvastatin. Oxycodone is
an opioid that along with Diazepam can lead to coma, respiratory distress and death. This also
6RCA AND FMEA
resulted in increased amounts of intracellular opioid in Mr B’s body because the doctor also
administered another opioid Hydromorphone at high concentrations. The doctor did not follow
the rules of conscious sedation policy of the hospital. Additionally, there was no one to monitor
the condition of Mr. B. The RN and the LPN had left the room keeping him on an automatic
blood pressure monitor.
Process Improvement Plan
The patient suffers from high levels of cholesterol and glucose intolerance. As a result,
high doses of opioid administration should be avoided. The process improvement plan should
include a conscious sedation step. Diazepam should be given at an initial dose of 2-2.5 mg and
doses can be increased, depending on the patient response and tolerance to the medication. Next,
an opioid should not be used in association with Diazepam. However, if used the dose of the
opioid should be low. If Hydromorphone is given, then the dose should be 0.2-1mg. It is
necessary to decrease the dose of Diazepam before decreasing the dose of an opioid. Moreover,
the vital signs of the patient should be monitored like heart rate (ECG), respiration rate, blood
pressure, among others. Supplemental oxygen should also be provided. Optimal conscious
sedation steps should be followed according to the hospital guidelines (Karamnov et al., 2017).
The level of sedation should be assessed based on a sedation scale. Emergency medications and
equipments like defibrillators should be available. Presence of reversal agents like Naloxone and
Flumazenil (Lameijer et al., 2014). The patient should be provided with the summary of the
procedure and necessary consent is to be taken. The RN should provide treatments for side
effects of sedation and carry out constant assessment and patient monitoring. A one to one RN to
patient ratio is to be maintained. The RN has the responsibility to provide full time attention to
the patient and carry out continuous monitoring. A qualified professional is to be present at all
resulted in increased amounts of intracellular opioid in Mr B’s body because the doctor also
administered another opioid Hydromorphone at high concentrations. The doctor did not follow
the rules of conscious sedation policy of the hospital. Additionally, there was no one to monitor
the condition of Mr. B. The RN and the LPN had left the room keeping him on an automatic
blood pressure monitor.
Process Improvement Plan
The patient suffers from high levels of cholesterol and glucose intolerance. As a result,
high doses of opioid administration should be avoided. The process improvement plan should
include a conscious sedation step. Diazepam should be given at an initial dose of 2-2.5 mg and
doses can be increased, depending on the patient response and tolerance to the medication. Next,
an opioid should not be used in association with Diazepam. However, if used the dose of the
opioid should be low. If Hydromorphone is given, then the dose should be 0.2-1mg. It is
necessary to decrease the dose of Diazepam before decreasing the dose of an opioid. Moreover,
the vital signs of the patient should be monitored like heart rate (ECG), respiration rate, blood
pressure, among others. Supplemental oxygen should also be provided. Optimal conscious
sedation steps should be followed according to the hospital guidelines (Karamnov et al., 2017).
The level of sedation should be assessed based on a sedation scale. Emergency medications and
equipments like defibrillators should be available. Presence of reversal agents like Naloxone and
Flumazenil (Lameijer et al., 2014). The patient should be provided with the summary of the
procedure and necessary consent is to be taken. The RN should provide treatments for side
effects of sedation and carry out constant assessment and patient monitoring. A one to one RN to
patient ratio is to be maintained. The RN has the responsibility to provide full time attention to
the patient and carry out continuous monitoring. A qualified professional is to be present at all
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7RCA AND FMEA
times to handle any complications associated with sedation. All vital signs of a patient are to be
monitored before discharge (Balas et al., 2012).
Lewin’s change theory
The Kurt Lewin change theory is a 3 step model that provides an approach to change.
The approaches are of high level and allow the manager or the organizational head to implement
changes based on a particular framework. The changes should be sensitive and seamless. The
Kurt Lewin change theory or model proposes the following steps to carry out a change. These
are making a radical change, minimizing the organization’s structure disruption and ensuring that
the changes are permanently adopted by the members of the organization (Shirey, 2013). The
Kurt Lewin change theory can be implemented in the improvement plan as it will bring about
changes in the way the healthcare organization was running. It will enable the healthcare workers
to analyze their daily activities and carry out practices that will that are efficient and effective. It
is necessary to educate the staff about the necessary practices according to the organizational
guidelines. Moreover, the staff should be empowered to carry out practices keeping in mind the
consequences of such practices on the health of the patient. Lastly, the healthcare staff should
adopt the necessary changes in the guidelines and follow it all times (Mitchell, 2013).
Purpose of FMEA
The general purpose of a failure modes and effect analysis (FMEA) process is to identify
the probable failures in association with a program design or healthcare approach. Failure modes
refer to the different ways by which the program may fail. Failures are the problems or the errors
that can affect an individual like a patient participating in a medical plan or care program. Effect
analysis on the other hand can be defined as the events or the outcomes resulting from such
times to handle any complications associated with sedation. All vital signs of a patient are to be
monitored before discharge (Balas et al., 2012).
Lewin’s change theory
The Kurt Lewin change theory is a 3 step model that provides an approach to change.
The approaches are of high level and allow the manager or the organizational head to implement
changes based on a particular framework. The changes should be sensitive and seamless. The
Kurt Lewin change theory or model proposes the following steps to carry out a change. These
are making a radical change, minimizing the organization’s structure disruption and ensuring that
the changes are permanently adopted by the members of the organization (Shirey, 2013). The
Kurt Lewin change theory can be implemented in the improvement plan as it will bring about
changes in the way the healthcare organization was running. It will enable the healthcare workers
to analyze their daily activities and carry out practices that will that are efficient and effective. It
is necessary to educate the staff about the necessary practices according to the organizational
guidelines. Moreover, the staff should be empowered to carry out practices keeping in mind the
consequences of such practices on the health of the patient. Lastly, the healthcare staff should
adopt the necessary changes in the guidelines and follow it all times (Mitchell, 2013).
Purpose of FMEA
The general purpose of a failure modes and effect analysis (FMEA) process is to identify
the probable failures in association with a program design or healthcare approach. Failure modes
refer to the different ways by which the program may fail. Failures are the problems or the errors
that can affect an individual like a patient participating in a medical plan or care program. Effect
analysis on the other hand can be defined as the events or the outcomes resulting from such
8RCA AND FMEA
failures. The importance of the failures is based on the seriousness of the outcomes, the
frequency and the possibility of their detection. The purpose of the FMEA is to eliminate the
failures, beginning from the highest and moving to the lowest priority ones. FMEA creates a
documentation of the problems, the current knowledge base and the necessary actions in order to
prevent such outcomes in the future and also to carry out continuous improvements in the field.
FMEA can also be used to prevent problems and failures. It is used throughout the process in
order to prevent adverse outcomes in a timely manner (Liu, Liu & Liu, 2013; Ford et al., 2014).
FMEA Steps
There are seven steps to perform an FMEA. These steps include:
Step 1: It is necessary to choose a process that can be problematic. After choosing the
problematic process that gave rise to the adverse outcome, analysis of the process is carried out.
Step 2: Determination of project charter, team facilitator and members. The team
members carry out the analysis of the process.
Step 3: The process steps are described thoroughly for everyone in the team in order to to
identify the necessary steps that will be subjected to analysis. Flow charts can be used to list all
the steps of the process and identifying the steps that require thorough analysis.
Step 4: The teams lists the failure modes or problems that can occur in the different steps
of the process and then all the possible causes in association with the respective failures are
outlined.
Step 5: For the different failure modes, the team determines the “likelihood of
occurrence” of such failures. Thus, the frequency of the failure is determined. It is given a rating
failures. The importance of the failures is based on the seriousness of the outcomes, the
frequency and the possibility of their detection. The purpose of the FMEA is to eliminate the
failures, beginning from the highest and moving to the lowest priority ones. FMEA creates a
documentation of the problems, the current knowledge base and the necessary actions in order to
prevent such outcomes in the future and also to carry out continuous improvements in the field.
FMEA can also be used to prevent problems and failures. It is used throughout the process in
order to prevent adverse outcomes in a timely manner (Liu, Liu & Liu, 2013; Ford et al., 2014).
FMEA Steps
There are seven steps to perform an FMEA. These steps include:
Step 1: It is necessary to choose a process that can be problematic. After choosing the
problematic process that gave rise to the adverse outcome, analysis of the process is carried out.
Step 2: Determination of project charter, team facilitator and members. The team
members carry out the analysis of the process.
Step 3: The process steps are described thoroughly for everyone in the team in order to to
identify the necessary steps that will be subjected to analysis. Flow charts can be used to list all
the steps of the process and identifying the steps that require thorough analysis.
Step 4: The teams lists the failure modes or problems that can occur in the different steps
of the process and then all the possible causes in association with the respective failures are
outlined.
Step 5: For the different failure modes, the team determines the “likelihood of
occurrence” of such failures. Thus, the frequency of the failure is determined. It is given a rating
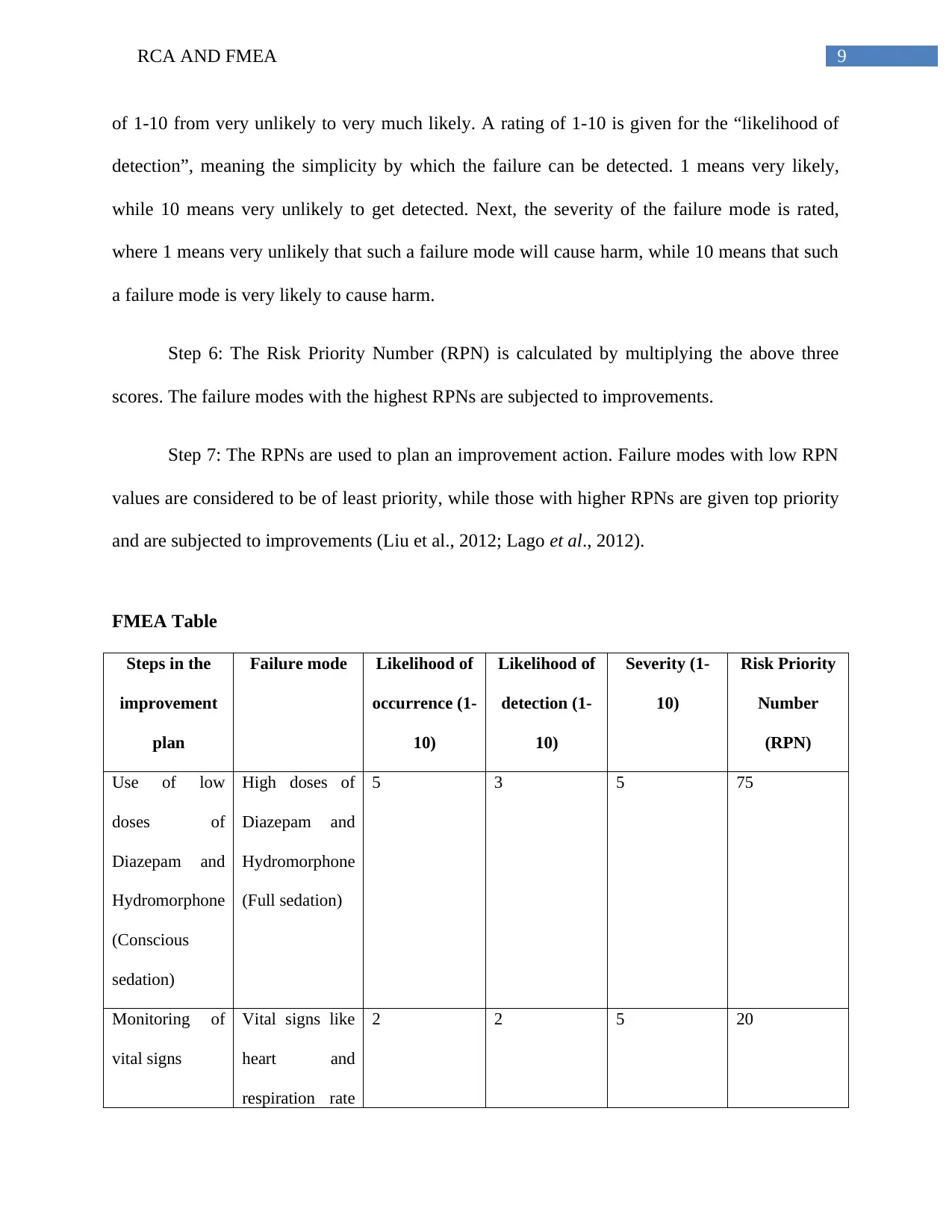
9RCA AND FMEA
of 1-10 from very unlikely to very much likely. A rating of 1-10 is given for the “likelihood of
detection”, meaning the simplicity by which the failure can be detected. 1 means very likely,
while 10 means very unlikely to get detected. Next, the severity of the failure mode is rated,
where 1 means very unlikely that such a failure mode will cause harm, while 10 means that such
a failure mode is very likely to cause harm.
Step 6: The Risk Priority Number (RPN) is calculated by multiplying the above three
scores. The failure modes with the highest RPNs are subjected to improvements.
Step 7: The RPNs are used to plan an improvement action. Failure modes with low RPN
values are considered to be of least priority, while those with higher RPNs are given top priority
and are subjected to improvements (Liu et al., 2012; Lago et al., 2012).
FMEA Table
Steps in the
improvement
plan
Failure mode Likelihood of
occurrence (1-
10)
Likelihood of
detection (1-
10)
Severity (1-
10)
Risk Priority
Number
(RPN)
Use of low
doses of
Diazepam and
Hydromorphone
(Conscious
sedation)
High doses of
Diazepam and
Hydromorphone
(Full sedation)
5 3 5 75
Monitoring of
vital signs
Vital signs like
heart and
respiration rate
2 2 5 20
of 1-10 from very unlikely to very much likely. A rating of 1-10 is given for the “likelihood of
detection”, meaning the simplicity by which the failure can be detected. 1 means very likely,
while 10 means very unlikely to get detected. Next, the severity of the failure mode is rated,
where 1 means very unlikely that such a failure mode will cause harm, while 10 means that such
a failure mode is very likely to cause harm.
Step 6: The Risk Priority Number (RPN) is calculated by multiplying the above three
scores. The failure modes with the highest RPNs are subjected to improvements.
Step 7: The RPNs are used to plan an improvement action. Failure modes with low RPN
values are considered to be of least priority, while those with higher RPNs are given top priority
and are subjected to improvements (Liu et al., 2012; Lago et al., 2012).
FMEA Table
Steps in the
improvement
plan
Failure mode Likelihood of
occurrence (1-
10)
Likelihood of
detection (1-
10)
Severity (1-
10)
Risk Priority
Number
(RPN)
Use of low
doses of
Diazepam and
Hydromorphone
(Conscious
sedation)
High doses of
Diazepam and
Hydromorphone
(Full sedation)
5 3 5 75
Monitoring of
vital signs
Vital signs like
heart and
respiration rate
2 2 5 20
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
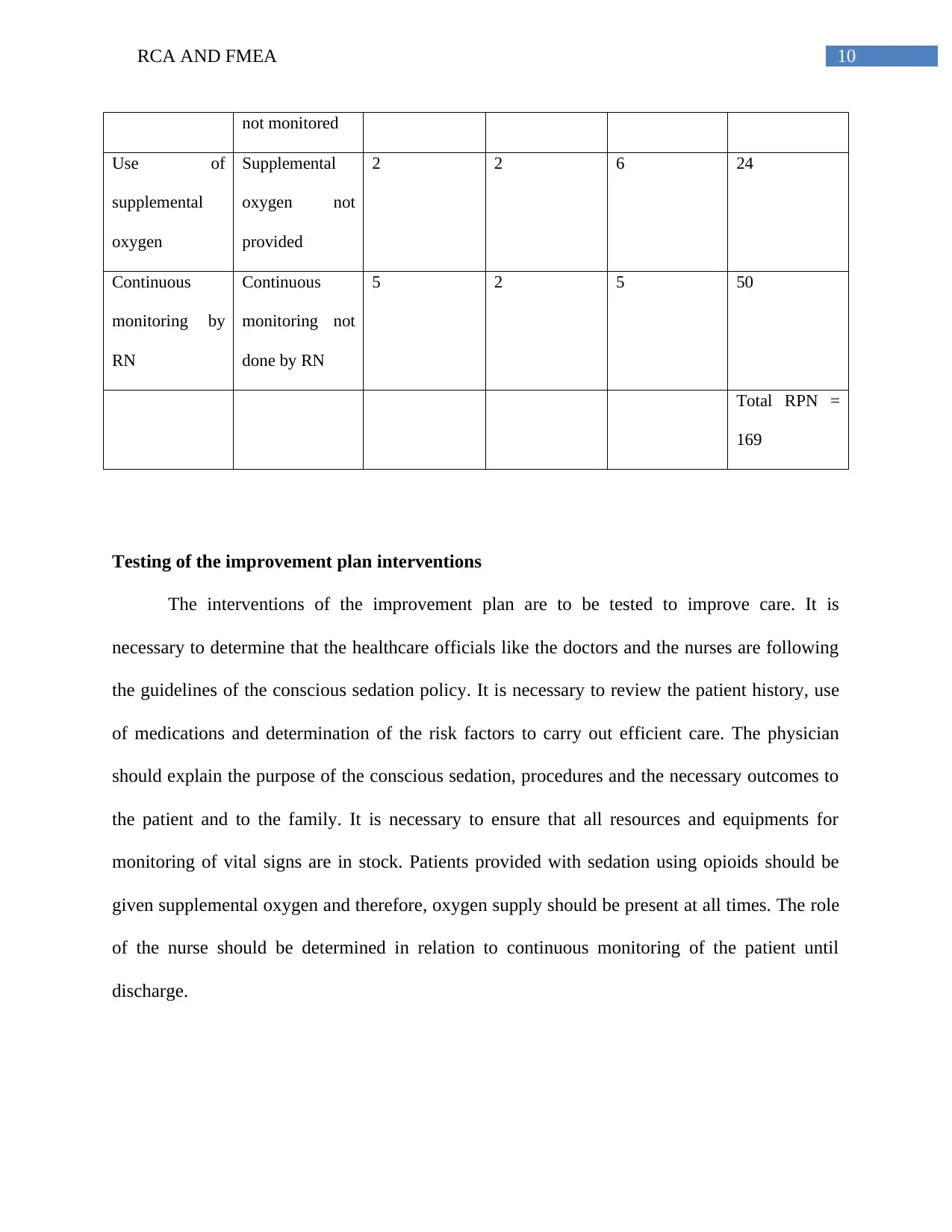
10RCA AND FMEA
not monitored
Use of
supplemental
oxygen
Supplemental
oxygen not
provided
2 2 6 24
Continuous
monitoring by
RN
Continuous
monitoring not
done by RN
5 2 5 50
Total RPN =
169
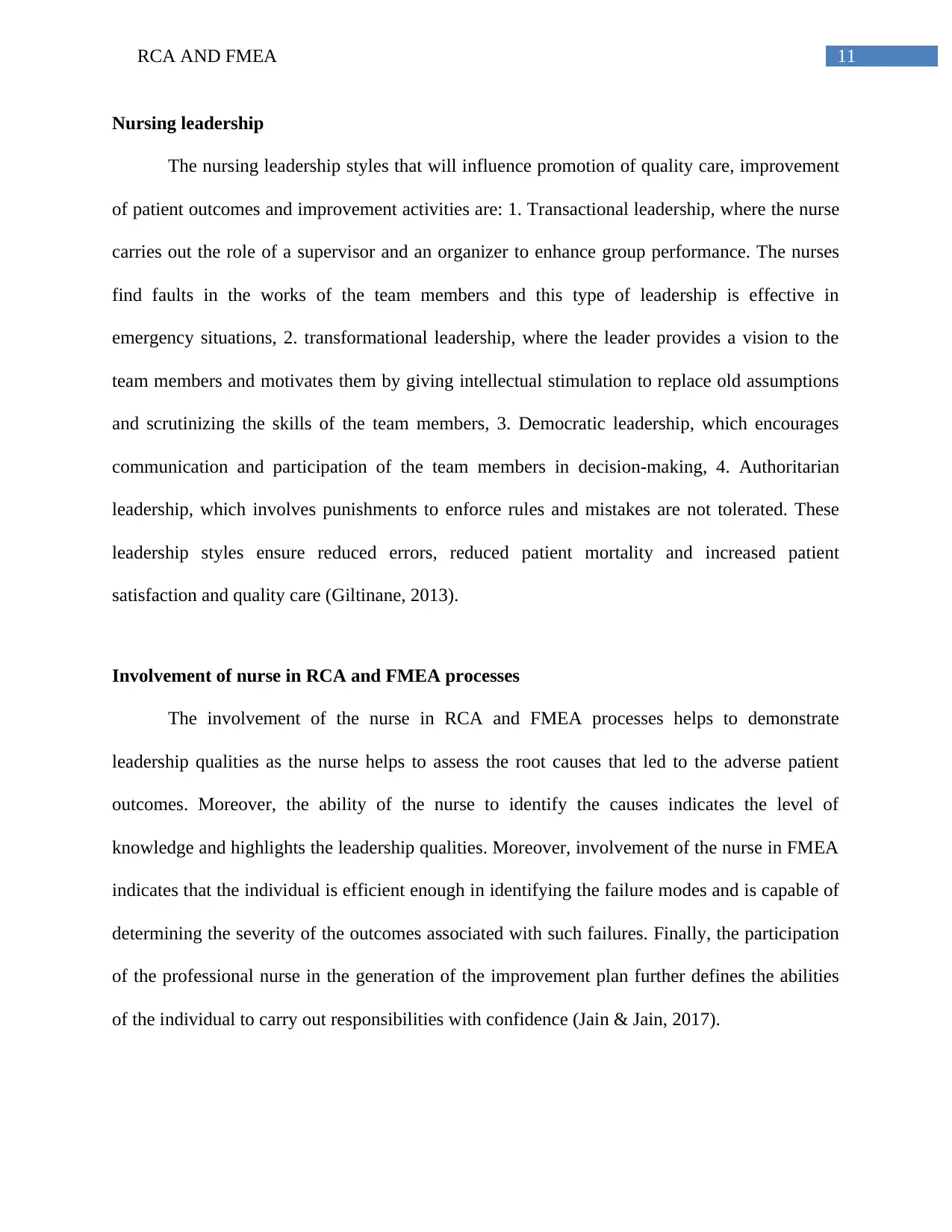
Testing of the improvement plan interventions
The interventions of the improvement plan are to be tested to improve care. It is
necessary to determine that the healthcare officials like the doctors and the nurses are following
the guidelines of the conscious sedation policy. It is necessary to review the patient history, use
of medications and determination of the risk factors to carry out efficient care. The physician
should explain the purpose of the conscious sedation, procedures and the necessary outcomes to
the patient and to the family. It is necessary to ensure that all resources and equipments for
monitoring of vital signs are in stock. Patients provided with sedation using opioids should be
given supplemental oxygen and therefore, oxygen supply should be present at all times. The role
of the nurse should be determined in relation to continuous monitoring of the patient until
discharge.
not monitored
Use of
supplemental
oxygen
Supplemental
oxygen not
provided
2 2 6 24
Continuous
monitoring by
RN
Continuous
monitoring not
done by RN
5 2 5 50
Total RPN =
169
Testing of the improvement plan interventions
The interventions of the improvement plan are to be tested to improve care. It is
necessary to determine that the healthcare officials like the doctors and the nurses are following
the guidelines of the conscious sedation policy. It is necessary to review the patient history, use
of medications and determination of the risk factors to carry out efficient care. The physician
should explain the purpose of the conscious sedation, procedures and the necessary outcomes to
the patient and to the family. It is necessary to ensure that all resources and equipments for
monitoring of vital signs are in stock. Patients provided with sedation using opioids should be
given supplemental oxygen and therefore, oxygen supply should be present at all times. The role
of the nurse should be determined in relation to continuous monitoring of the patient until
discharge.
11RCA AND FMEA
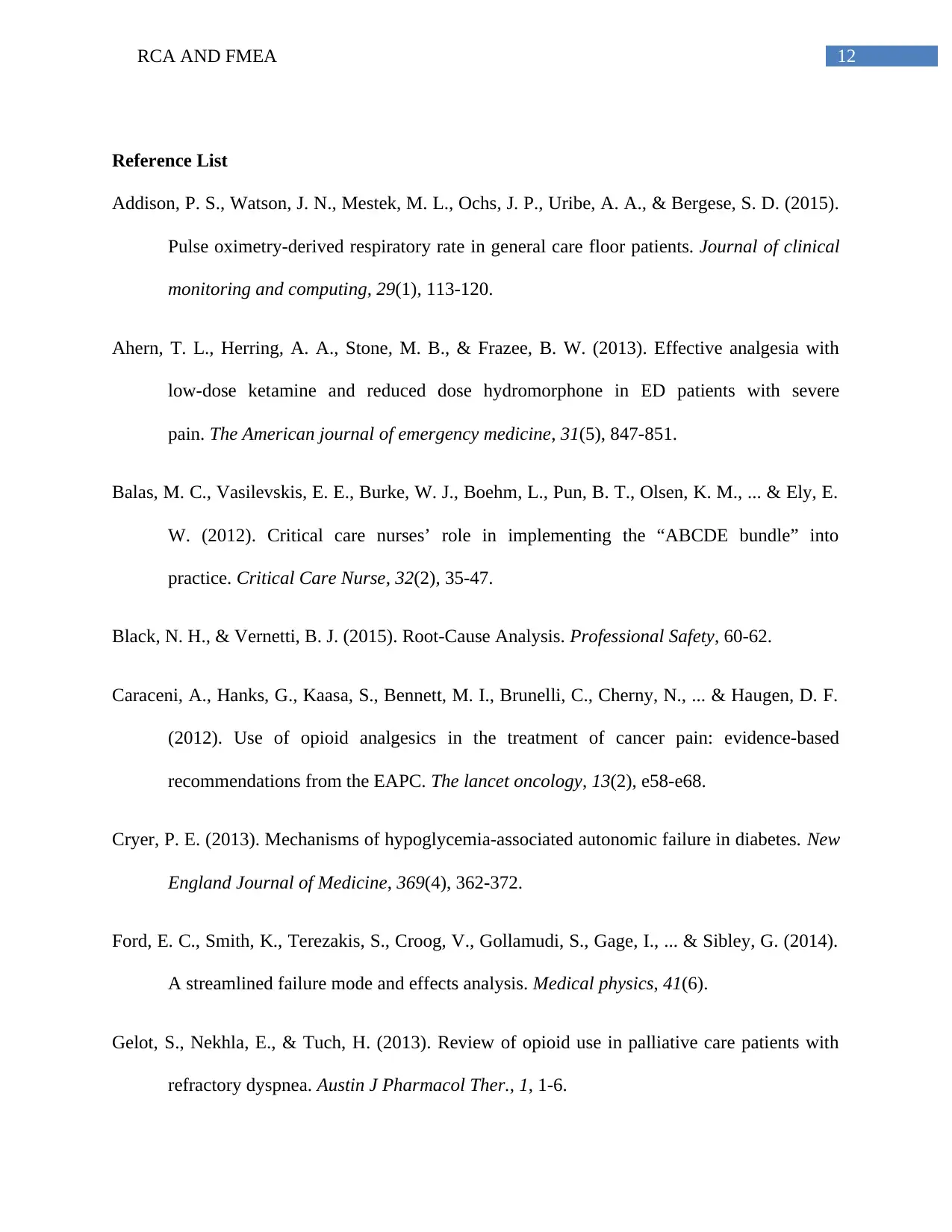
Nursing leadership
The nursing leadership styles that will influence promotion of quality care, improvement
of patient outcomes and improvement activities are: 1. Transactional leadership, where the nurse
carries out the role of a supervisor and an organizer to enhance group performance. The nurses
find faults in the works of the team members and this type of leadership is effective in
emergency situations, 2. transformational leadership, where the leader provides a vision to the
team members and motivates them by giving intellectual stimulation to replace old assumptions
and scrutinizing the skills of the team members, 3. Democratic leadership, which encourages
communication and participation of the team members in decision-making, 4. Authoritarian
leadership, which involves punishments to enforce rules and mistakes are not tolerated. These
leadership styles ensure reduced errors, reduced patient mortality and increased patient
satisfaction and quality care (Giltinane, 2013).
Involvement of nurse in RCA and FMEA processes
The involvement of the nurse in RCA and FMEA processes helps to demonstrate
leadership qualities as the nurse helps to assess the root causes that led to the adverse patient
outcomes. Moreover, the ability of the nurse to identify the causes indicates the level of
knowledge and highlights the leadership qualities. Moreover, involvement of the nurse in FMEA
indicates that the individual is efficient enough in identifying the failure modes and is capable of
determining the severity of the outcomes associated with such failures. Finally, the participation
of the professional nurse in the generation of the improvement plan further defines the abilities
of the individual to carry out responsibilities with confidence (Jain & Jain, 2017).
Nursing leadership
The nursing leadership styles that will influence promotion of quality care, improvement
of patient outcomes and improvement activities are: 1. Transactional leadership, where the nurse
carries out the role of a supervisor and an organizer to enhance group performance. The nurses
find faults in the works of the team members and this type of leadership is effective in
emergency situations, 2. transformational leadership, where the leader provides a vision to the
team members and motivates them by giving intellectual stimulation to replace old assumptions
and scrutinizing the skills of the team members, 3. Democratic leadership, which encourages
communication and participation of the team members in decision-making, 4. Authoritarian
leadership, which involves punishments to enforce rules and mistakes are not tolerated. These
leadership styles ensure reduced errors, reduced patient mortality and increased patient
satisfaction and quality care (Giltinane, 2013).
Involvement of nurse in RCA and FMEA processes
The involvement of the nurse in RCA and FMEA processes helps to demonstrate
leadership qualities as the nurse helps to assess the root causes that led to the adverse patient
outcomes. Moreover, the ability of the nurse to identify the causes indicates the level of
knowledge and highlights the leadership qualities. Moreover, involvement of the nurse in FMEA
indicates that the individual is efficient enough in identifying the failure modes and is capable of
determining the severity of the outcomes associated with such failures. Finally, the participation
of the professional nurse in the generation of the improvement plan further defines the abilities
of the individual to carry out responsibilities with confidence (Jain & Jain, 2017).
12RCA AND FMEA
Reference List
Addison, P. S., Watson, J. N., Mestek, M. L., Ochs, J. P., Uribe, A. A., & Bergese, S. D. (2015).
Pulse oximetry-derived respiratory rate in general care floor patients. Journal of clinical
monitoring and computing, 29(1), 113-120.
Ahern, T. L., Herring, A. A., Stone, M. B., & Frazee, B. W. (2013). Effective analgesia with
low-dose ketamine and reduced dose hydromorphone in ED patients with severe
pain. The American journal of emergency medicine, 31(5), 847-851.
Balas, M. C., Vasilevskis, E. E., Burke, W. J., Boehm, L., Pun, B. T., Olsen, K. M., ... & Ely, E.
W. (2012). Critical care nurses’ role in implementing the “ABCDE bundle” into
practice. Critical Care Nurse, 32(2), 35-47.
Black, N. H., & Vernetti, B. J. (2015). Root-Cause Analysis. Professional Safety, 60-62.
Caraceni, A., Hanks, G., Kaasa, S., Bennett, M. I., Brunelli, C., Cherny, N., ... & Haugen, D. F.
(2012). Use of opioid analgesics in the treatment of cancer pain: evidence-based
recommendations from the EAPC. The lancet oncology, 13(2), e58-e68.
Cryer, P. E. (2013). Mechanisms of hypoglycemia-associated autonomic failure in diabetes. New
England Journal of Medicine, 369(4), 362-372.
Ford, E. C., Smith, K., Terezakis, S., Croog, V., Gollamudi, S., Gage, I., ... & Sibley, G. (2014).
A streamlined failure mode and effects analysis. Medical physics, 41(6).
Gelot, S., Nekhla, E., & Tuch, H. (2013). Review of opioid use in palliative care patients with
refractory dyspnea. Austin J Pharmacol Ther., 1, 1-6.
Reference List
Addison, P. S., Watson, J. N., Mestek, M. L., Ochs, J. P., Uribe, A. A., & Bergese, S. D. (2015).
Pulse oximetry-derived respiratory rate in general care floor patients. Journal of clinical
monitoring and computing, 29(1), 113-120.
Ahern, T. L., Herring, A. A., Stone, M. B., & Frazee, B. W. (2013). Effective analgesia with
low-dose ketamine and reduced dose hydromorphone in ED patients with severe
pain. The American journal of emergency medicine, 31(5), 847-851.
Balas, M. C., Vasilevskis, E. E., Burke, W. J., Boehm, L., Pun, B. T., Olsen, K. M., ... & Ely, E.
W. (2012). Critical care nurses’ role in implementing the “ABCDE bundle” into
practice. Critical Care Nurse, 32(2), 35-47.
Black, N. H., & Vernetti, B. J. (2015). Root-Cause Analysis. Professional Safety, 60-62.
Caraceni, A., Hanks, G., Kaasa, S., Bennett, M. I., Brunelli, C., Cherny, N., ... & Haugen, D. F.
(2012). Use of opioid analgesics in the treatment of cancer pain: evidence-based
recommendations from the EAPC. The lancet oncology, 13(2), e58-e68.
Cryer, P. E. (2013). Mechanisms of hypoglycemia-associated autonomic failure in diabetes. New
England Journal of Medicine, 369(4), 362-372.
Ford, E. C., Smith, K., Terezakis, S., Croog, V., Gollamudi, S., Gage, I., ... & Sibley, G. (2014).
A streamlined failure mode and effects analysis. Medical physics, 41(6).
Gelot, S., Nekhla, E., & Tuch, H. (2013). Review of opioid use in palliative care patients with
refractory dyspnea. Austin J Pharmacol Ther., 1, 1-6.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13RCA AND FMEA
Gierman, L. M., Kühnast, S., Koudijs, A., Pieterman, E. J., Kloppenburg, M., van Osch, G. J. V.
M., ... & Zuurmond, A. M. (2014). Osteoarthritis development is induced by increased
dietary cholesterol and can be inhibited by atorvastatin in APOE* 3Leiden. CETP mice—
a translational model for atherosclerosis. Annals of the rheumatic diseases, 73(5), 921-
927.
Giltinane, C. L. (2013). Leadership styles and theories. Nursing Standard (through
2013), 27(41), 35.
Jain, K., & Jain, K. (2017). Use of failure mode effect analysis (FMEA) to improve medication
management process. International Journal of Health Care Quality Assurance, 30(2),
175-186.
Karamnov, S., Sarkisian, N., Grammer, R., Gross, W. L., & Urman, R. D. (2017). Analysis of
adverse events associated with adult moderate procedural sedation outside the operating
room. Journal of patient safety, 13(3), 111-121.
Labianca, R., Sarzi-Puttini, P., Zuccaro, S. M., Cherubino, P., Vellucci, R., & Fornasari, D.
(2012). Adverse effects associated with non-opioid and opioid treatment in patients with
chronic pain. Clinical drug investigation, 32(suppl_1 Chronic), 53.
Lago, P., Bizzarri, G., Scalzotto, F., Parpaiola, A., Amigoni, A., Putoto, G., & Perilongo, G.
(2012). Use of FMEA analysis to reduce risk of errors in prescribing and administering
drugs in paediatric wards: a quality improvement report. BMJ open, 2(6), e001249.
Gierman, L. M., Kühnast, S., Koudijs, A., Pieterman, E. J., Kloppenburg, M., van Osch, G. J. V.
M., ... & Zuurmond, A. M. (2014). Osteoarthritis development is induced by increased
dietary cholesterol and can be inhibited by atorvastatin in APOE* 3Leiden. CETP mice—
a translational model for atherosclerosis. Annals of the rheumatic diseases, 73(5), 921-
927.
Giltinane, C. L. (2013). Leadership styles and theories. Nursing Standard (through
2013), 27(41), 35.
Jain, K., & Jain, K. (2017). Use of failure mode effect analysis (FMEA) to improve medication
management process. International Journal of Health Care Quality Assurance, 30(2),
175-186.
Karamnov, S., Sarkisian, N., Grammer, R., Gross, W. L., & Urman, R. D. (2017). Analysis of
adverse events associated with adult moderate procedural sedation outside the operating
room. Journal of patient safety, 13(3), 111-121.
Labianca, R., Sarzi-Puttini, P., Zuccaro, S. M., Cherubino, P., Vellucci, R., & Fornasari, D.
(2012). Adverse effects associated with non-opioid and opioid treatment in patients with
chronic pain. Clinical drug investigation, 32(suppl_1 Chronic), 53.
Lago, P., Bizzarri, G., Scalzotto, F., Parpaiola, A., Amigoni, A., Putoto, G., & Perilongo, G.
(2012). Use of FMEA analysis to reduce risk of errors in prescribing and administering
drugs in paediatric wards: a quality improvement report. BMJ open, 2(6), e001249.
14RCA AND FMEA
Lameijer, H., Azizi, N., Ligtenberg, J. J., & Ter Maaten, J. C. (2014). Ventricular tachycardia
after naloxone administration: A drug related complication? Case report and literature
review. Drug safety-case reports, 1(1), 2.
Liu, H. C., Liu, L., & Liu, N. (2013). Risk evaluation approaches in failure mode and effects
analysis: A literature review. Expert systems with applications, 40(2), 828-838.
Liu, H. C., Liu, L., Liu, N., & Mao, L. X. (2012). Risk evaluation in failure mode and effects
analysis with extended VIKOR method under fuzzy environment. Expert Systems with
Applications, 39(17), 12926-12934.
Makary, M. A., & Daniel, M. (2016). Medical error-the third leading cause of death in the
US. BMJ: British Medical Journal (Online), 353.
Mann, E., Böhmdorfer, B., Frühwald, T., Roller-Wirnsberger, R. E., Dovjak, P., Dückelmann-
Hofer, C., ... & Iglseder, B. (2012). Potentially inappropriate medication in geriatric
patients: the Austrian consensus panel list. Wiener klinische Wochenschrift, 124(5), 160-
169.
Mitchell, G. (2013). Selecting the best theory to implement planned change. Nursing
Management-UK, 20(1).
Shaqdan, K., Aran, S., Besheli, L. D., & Abujudeh, H. (2014). Root-cause analysis and health
failure mode and effect analysis: two leading techniques in health care quality
assessment. Journal of the American College of Radiology, 11(6), 572-579.
Shirey, M. R. (2013). Lewin’s theory of planned change as a strategic resource. Journal of
Nursing Administration, 43(2), 69-72.
Lameijer, H., Azizi, N., Ligtenberg, J. J., & Ter Maaten, J. C. (2014). Ventricular tachycardia
after naloxone administration: A drug related complication? Case report and literature
review. Drug safety-case reports, 1(1), 2.
Liu, H. C., Liu, L., & Liu, N. (2013). Risk evaluation approaches in failure mode and effects
analysis: A literature review. Expert systems with applications, 40(2), 828-838.
Liu, H. C., Liu, L., Liu, N., & Mao, L. X. (2012). Risk evaluation in failure mode and effects
analysis with extended VIKOR method under fuzzy environment. Expert Systems with
Applications, 39(17), 12926-12934.
Makary, M. A., & Daniel, M. (2016). Medical error-the third leading cause of death in the
US. BMJ: British Medical Journal (Online), 353.
Mann, E., Böhmdorfer, B., Frühwald, T., Roller-Wirnsberger, R. E., Dovjak, P., Dückelmann-
Hofer, C., ... & Iglseder, B. (2012). Potentially inappropriate medication in geriatric
patients: the Austrian consensus panel list. Wiener klinische Wochenschrift, 124(5), 160-
169.
Mitchell, G. (2013). Selecting the best theory to implement planned change. Nursing
Management-UK, 20(1).
Shaqdan, K., Aran, S., Besheli, L. D., & Abujudeh, H. (2014). Root-cause analysis and health
failure mode and effect analysis: two leading techniques in health care quality
assessment. Journal of the American College of Radiology, 11(6), 572-579.
Shirey, M. R. (2013). Lewin’s theory of planned change as a strategic resource. Journal of
Nursing Administration, 43(2), 69-72.
15RCA AND FMEA
Www.healthline.com. (2017). Diazepam, Oral Tablet. Healthline. Retrieved 23 November 2017,
from https://www.healthline.com/health/diazepam-oral-tablet#side-effects4
Www.ihi.org. (2017). Search: root cause analysis tool. Ihi.org. Retrieved 23 November 2017,
from http://www.ihi.org/sites/search/Pages/results.aspx?k=root+cause+analysis+tool
Www.netdoctor.co.uk. (2017). Diazepam. Netdoctor. Retrieved 23 November 2017, from
http://www.netdoctor.co.uk/medicines/depression/a6560/diazepam/
Zheng, H., Zou, H., Liu, X., Chu, J., Zhou, Y., Loh, H. H., & Law, P. Y. (2012). Cholesterol
level influences opioid signaling in cell models and analgesia in mice and
humans. Journal of lipid research, 53(6), 1153-1162.
Www.healthline.com. (2017). Diazepam, Oral Tablet. Healthline. Retrieved 23 November 2017,
from https://www.healthline.com/health/diazepam-oral-tablet#side-effects4
Www.ihi.org. (2017). Search: root cause analysis tool. Ihi.org. Retrieved 23 November 2017,
from http://www.ihi.org/sites/search/Pages/results.aspx?k=root+cause+analysis+tool
Www.netdoctor.co.uk. (2017). Diazepam. Netdoctor. Retrieved 23 November 2017, from
http://www.netdoctor.co.uk/medicines/depression/a6560/diazepam/
Zheng, H., Zou, H., Liu, X., Chu, J., Zhou, Y., Loh, H. H., & Law, P. Y. (2012). Cholesterol
level influences opioid signaling in cell models and analgesia in mice and
humans. Journal of lipid research, 53(6), 1153-1162.
1 out of 16
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





