Analyzing SHI's Impact on Egypt's Healthcare System Performance
VerifiedAdded on 2021/11/16
|26
|9220
|80
Report
AI Summary
This report delves into the impact of the Social Health Insurance (SHI) system on the challenges facing the Egyptian health sector and the overall performance of the healthcare system. It begins with a background on the importance of public health and the evolution of health insurance in Egypt, tracing its origins back to 1964 and the subsequent developments, including the launch of the comprehensive health insurance system in 2019. The report highlights the key features of the new law, such as compulsory participation, family doctor files, and reduced patient contributions. It then examines the performance of the Egyptian healthcare system, citing indicators like infant mortality rates, hospital bed availability, and death rates, along with challenges like budget shortages, lack of medicines, and low healthcare worker salaries. The report also discusses the coverage of the SHI program and its funding mechanisms, providing data from various sources to illustrate the changes and challenges within the system. Overall, the report provides a comprehensive overview of the SHI system and its impact on the Egyptian healthcare landscape, providing valuable insights into the current state of the healthcare system and its future prospects.
The Impact of Social Health Insurance (SHI) system on the relationship between
Challenges Facing Egyptian Health Sector and Healthcare System Performance
1. Introduction
1.1 Background
Public health occupies an important place in assessing the state’s commitment to human
rights standards. The state’s health status is assessed according to the number of citizens
who receive appropriate treatment for free under the umbrella of health insurance, the level
of medical services provided and treatment paid for free, as well as the general health level
of citizens. The state is often obligated to cover all the health costs that the citizen needs in
order to receive appropriate care to enable him to enjoy his right to belonging to the country,
as well as the capacity of productivity, which in turn raises the status of in a decent life in a
way that positively affects his patriotism or the state economically.
The health care system in Egypt is characterized by a multiplicity and complexity that brings
together service providers and funders from the public and private sectors. The government
has committed to providing health care to the poor; However, with an inherently pluralistic
system, healthcare providers compete, and clients are free to choose services based on their
needs along with the ability to pay (WHO-EMRO, 2006).
The beginning of social health insurance in Egypt as the main system for providing health
care services goes back to 1964, as many legislations were issued primarily for the workforce
of workers and employees and the work environment and concerned with work injuries and
compensation, and some models for sick care (El-Adawy et al., 1997).
The first health insurance document was issued in the world in Germany in 1883 (Federal
Ministry of Health, 2020). As for the Arab world, the first document written in Arabic to
ensure medical treatment appeared in 1957 in Egypt between “the United Insurance
Company” and Bank of Alexandria, and another document was issued in the same year
between the Egypt Company Insurance and “Asustander Petroleum Services Company” (El-
Adawy et al., 1997).
In recent years, the state has submitted several drafts for a new health insurance law that
has passed two cycles, the first (1997 to 2002) and the second (2006 to 2010) the first phase
has developed a model for health insurance as part of an experimental framework to
separate the service from its delivery units, and family health units have been established,
which are 400 units in three The pilot governorates, which are Alexandria, Menoufia, and
Sohag, and they managed a financial insurance fund for family health. The second phase of
the reform was from 2006 to 2010. Conferences were held to discuss reform plans and start
a new pilot experience, but it failed (Haley and Beg, 2012; WHO-EMRO, 2006).
Challenges Facing Egyptian Health Sector and Healthcare System Performance
1. Introduction
1.1 Background
Public health occupies an important place in assessing the state’s commitment to human
rights standards. The state’s health status is assessed according to the number of citizens
who receive appropriate treatment for free under the umbrella of health insurance, the level
of medical services provided and treatment paid for free, as well as the general health level
of citizens. The state is often obligated to cover all the health costs that the citizen needs in
order to receive appropriate care to enable him to enjoy his right to belonging to the country,
as well as the capacity of productivity, which in turn raises the status of in a decent life in a
way that positively affects his patriotism or the state economically.
The health care system in Egypt is characterized by a multiplicity and complexity that brings
together service providers and funders from the public and private sectors. The government
has committed to providing health care to the poor; However, with an inherently pluralistic
system, healthcare providers compete, and clients are free to choose services based on their
needs along with the ability to pay (WHO-EMRO, 2006).
The beginning of social health insurance in Egypt as the main system for providing health
care services goes back to 1964, as many legislations were issued primarily for the workforce
of workers and employees and the work environment and concerned with work injuries and
compensation, and some models for sick care (El-Adawy et al., 1997).
The first health insurance document was issued in the world in Germany in 1883 (Federal
Ministry of Health, 2020). As for the Arab world, the first document written in Arabic to
ensure medical treatment appeared in 1957 in Egypt between “the United Insurance
Company” and Bank of Alexandria, and another document was issued in the same year
between the Egypt Company Insurance and “Asustander Petroleum Services Company” (El-
Adawy et al., 1997).
In recent years, the state has submitted several drafts for a new health insurance law that
has passed two cycles, the first (1997 to 2002) and the second (2006 to 2010) the first phase
has developed a model for health insurance as part of an experimental framework to
separate the service from its delivery units, and family health units have been established,
which are 400 units in three The pilot governorates, which are Alexandria, Menoufia, and
Sohag, and they managed a financial insurance fund for family health. The second phase of
the reform was from 2006 to 2010. Conferences were held to discuss reform plans and start
a new pilot experience, but it failed (Haley and Beg, 2012; WHO-EMRO, 2006).
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
After the January 25, 2011 revolution, Egypt began dramatic measures to improve the
country's various systems, including the Social health insurance system. Several published
reports identified the challenges facing the health system to achieve the Ministry of Health
and Population's goal of improving the health of all citizens (MOHP, 2015).
Those actions were end by the launching of the comprehensive health insurance system
which includes an integrated package of diagnostic and therapeutic services, and allows the
beneficiary to choose health service providers. It also reduces the personal spending of
citizens on health services, reduces poverty resulting from illness, and this new system
contributes to setting prices. Medical services in a fair manner, and allow patients to access
these services without additional procedures. The new social health insurance system will
be applied in six phases over a period of 15 years (Almasry Alyoum,2019).
In July 2019, President Abdel Fattah El-Sisi launched the actual start signal for the
implementation of the largest national health project in Egypt, the "New Health Insurance
Law", from Port Said Governorate, marking the establishment of the foundations of an
integrated health system that includes one hundred million Egyptians according to the latest
international standards, in a historic event. He has flirted with the aspirations and dreams of
Egyptians over the past long decades.
The health insurance system is a giant project launched by the Egyptian government in order
to improve the medical service and provide it to Egyptians without discrimination, in
implementation of the directives of President Abdel Fattah El-Sisi, as it represents a social
solidarity system, through which high-quality medical services are provided to all groups of
society without discrimination, and the state guarantees treatment in it that is not Those
who are able, through an integrated package of diagnostic and therapeutic services, and
allows the beneficiary the freedom to choose the health service provider. The cost of the new
health insurance bill is between 80 and 120 billion pounds, and it will be applied within 15
years in all governorates, starting from 2019.Participation in the comprehensive health
insurance law is compulsory for all Egyptians, as it brings together all groups of society
under one insurance umbrella, and all forms of health insurance, whether governmental or
private, are canceled, and also the treatment system ends at the expense of the state with its
application in every governorate.
The most important features of the law are that every citizen has a special file with the family
doctor on which his medical history is written, and that he does not treat individuals but is
responsible for treating the entire family, and that the patient’s contributions to patients
’contributions in surgical operations are 5%, with a maximum of 300 pounds, and medicines,
x-rays, and analyzes. 10%. In addition, each health unit provides medical services to 20,000
patients, and private hospitals are contracted after obtaining the accreditation and quality
certificate, after the pricing of the health services that they will purchase from the private
country's various systems, including the Social health insurance system. Several published
reports identified the challenges facing the health system to achieve the Ministry of Health
and Population's goal of improving the health of all citizens (MOHP, 2015).
Those actions were end by the launching of the comprehensive health insurance system
which includes an integrated package of diagnostic and therapeutic services, and allows the
beneficiary to choose health service providers. It also reduces the personal spending of
citizens on health services, reduces poverty resulting from illness, and this new system
contributes to setting prices. Medical services in a fair manner, and allow patients to access
these services without additional procedures. The new social health insurance system will
be applied in six phases over a period of 15 years (Almasry Alyoum,2019).
In July 2019, President Abdel Fattah El-Sisi launched the actual start signal for the
implementation of the largest national health project in Egypt, the "New Health Insurance
Law", from Port Said Governorate, marking the establishment of the foundations of an
integrated health system that includes one hundred million Egyptians according to the latest
international standards, in a historic event. He has flirted with the aspirations and dreams of
Egyptians over the past long decades.
The health insurance system is a giant project launched by the Egyptian government in order
to improve the medical service and provide it to Egyptians without discrimination, in
implementation of the directives of President Abdel Fattah El-Sisi, as it represents a social
solidarity system, through which high-quality medical services are provided to all groups of
society without discrimination, and the state guarantees treatment in it that is not Those
who are able, through an integrated package of diagnostic and therapeutic services, and
allows the beneficiary the freedom to choose the health service provider. The cost of the new
health insurance bill is between 80 and 120 billion pounds, and it will be applied within 15
years in all governorates, starting from 2019.Participation in the comprehensive health
insurance law is compulsory for all Egyptians, as it brings together all groups of society
under one insurance umbrella, and all forms of health insurance, whether governmental or
private, are canceled, and also the treatment system ends at the expense of the state with its
application in every governorate.
The most important features of the law are that every citizen has a special file with the family
doctor on which his medical history is written, and that he does not treat individuals but is
responsible for treating the entire family, and that the patient’s contributions to patients
’contributions in surgical operations are 5%, with a maximum of 300 pounds, and medicines,
x-rays, and analyzes. 10%. In addition, each health unit provides medical services to 20,000
patients, and private hospitals are contracted after obtaining the accreditation and quality
certificate, after the pricing of the health services that they will purchase from the private
sector is set. The role of the Ministry of Health depends on ambulance services and
preventive medicine after the implementation of the new health insurance law.
Moreover, The Ministry of Health revealed that more than 527,132 of Port Said citizens have
registered in the new system since the start of registration last July through 29 units and a
family health center, in addition to more than 3,234 major surgeries and 611 surgeries that
were performed for the first time in the governorate. And the health insurance system
announced the completion of waiting lists for pediatric heart surgeries in Port Said
Governorate, which are the surgeries that were performed by the hospital’s pediatric heart
surgery team, free of charge.
In October 2019, the Ministry of Health announced the start of the first preparations for
launching the health insurance system in the remaining governorates of the first phase of the
system, including: Ismailia, Suez, South Sinai, Luxor and Aswan.
The door for registration and the family file was opened since the first of October, after the
actual operation began in Port Said. During this period, the system succeeded in registering
486,873 citizens and opening 120,210 family files in each of Ismailia: (207,267 citizens),
Suez (48,344 citizens), Luxor (127088 citizens), Aswan (92,277 citizens) and South Sinai
(11897 citizens). And that is through more than 117 units and family health centers in the
five governorates.
Healthcare System Performance in Egypt
Egyptian Healthcare System is not positioned to deliver high-quality health services to meet
the most pressing needs of its population. Although more than 95% of the population lives
within 5 km of a health facility, facilities are often ill-equipped to respond to the real needs
of the population in their catchment areas, grim conditions at dilapidated state-run facilities,
regular medication stock-outs due to outdated and inefficient supply chains, lack of updated
and enforced clinical guidelines for managing chronic diseases and limited numbers of
specialists have been widely reported. As such, quality of care is often poor, leading to low
utilization and reduced health benefits.
The Egyptian health system faces multiple challenges affecting its performance in improving
and ensuring the health and well-being of the Egyptian people resulted in declined quality of
healthcare services due to serious budget shortage, lack of medicines at medical facilities,
and low salaries of healthcare workers.
Despite MOH in Egypt took many positive steps towards improving the health sector
performance, there are still many negative issues requiring actions to improve the
performance of healthcare system. Rise in non-communicable diseases (NCDs) and a high
birth rate combined with a longer life expectancy is putting additional pressure on the
system and expected to increase healthcare costs.
preventive medicine after the implementation of the new health insurance law.
Moreover, The Ministry of Health revealed that more than 527,132 of Port Said citizens have
registered in the new system since the start of registration last July through 29 units and a
family health center, in addition to more than 3,234 major surgeries and 611 surgeries that
were performed for the first time in the governorate. And the health insurance system
announced the completion of waiting lists for pediatric heart surgeries in Port Said
Governorate, which are the surgeries that were performed by the hospital’s pediatric heart
surgery team, free of charge.
In October 2019, the Ministry of Health announced the start of the first preparations for
launching the health insurance system in the remaining governorates of the first phase of the
system, including: Ismailia, Suez, South Sinai, Luxor and Aswan.
The door for registration and the family file was opened since the first of October, after the
actual operation began in Port Said. During this period, the system succeeded in registering
486,873 citizens and opening 120,210 family files in each of Ismailia: (207,267 citizens),
Suez (48,344 citizens), Luxor (127088 citizens), Aswan (92,277 citizens) and South Sinai
(11897 citizens). And that is through more than 117 units and family health centers in the
five governorates.
Healthcare System Performance in Egypt
Egyptian Healthcare System is not positioned to deliver high-quality health services to meet
the most pressing needs of its population. Although more than 95% of the population lives
within 5 km of a health facility, facilities are often ill-equipped to respond to the real needs
of the population in their catchment areas, grim conditions at dilapidated state-run facilities,
regular medication stock-outs due to outdated and inefficient supply chains, lack of updated
and enforced clinical guidelines for managing chronic diseases and limited numbers of
specialists have been widely reported. As such, quality of care is often poor, leading to low
utilization and reduced health benefits.
The Egyptian health system faces multiple challenges affecting its performance in improving
and ensuring the health and well-being of the Egyptian people resulted in declined quality of
healthcare services due to serious budget shortage, lack of medicines at medical facilities,
and low salaries of healthcare workers.
Despite MOH in Egypt took many positive steps towards improving the health sector
performance, there are still many negative issues requiring actions to improve the
performance of healthcare system. Rise in non-communicable diseases (NCDs) and a high
birth rate combined with a longer life expectancy is putting additional pressure on the
system and expected to increase healthcare costs.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Most healthcare jobs are low paid and provide no incentive for performance. Medical
providers receive life-time licensing with no continuous medical education (CME)
requirements. Dual practice is allowed with no restrictions by law and therefore rampant.
Also, Egypt is one of the lowest healthcare spenders in the Middle East and North Africa
(MENA) region and more than half of the total health expenditure (THE) is out-of-pocket
(OOP). In addition to low health spending, systemic inefficiencies and inequities in health
financing limit the effectiveness of the healthcare system.
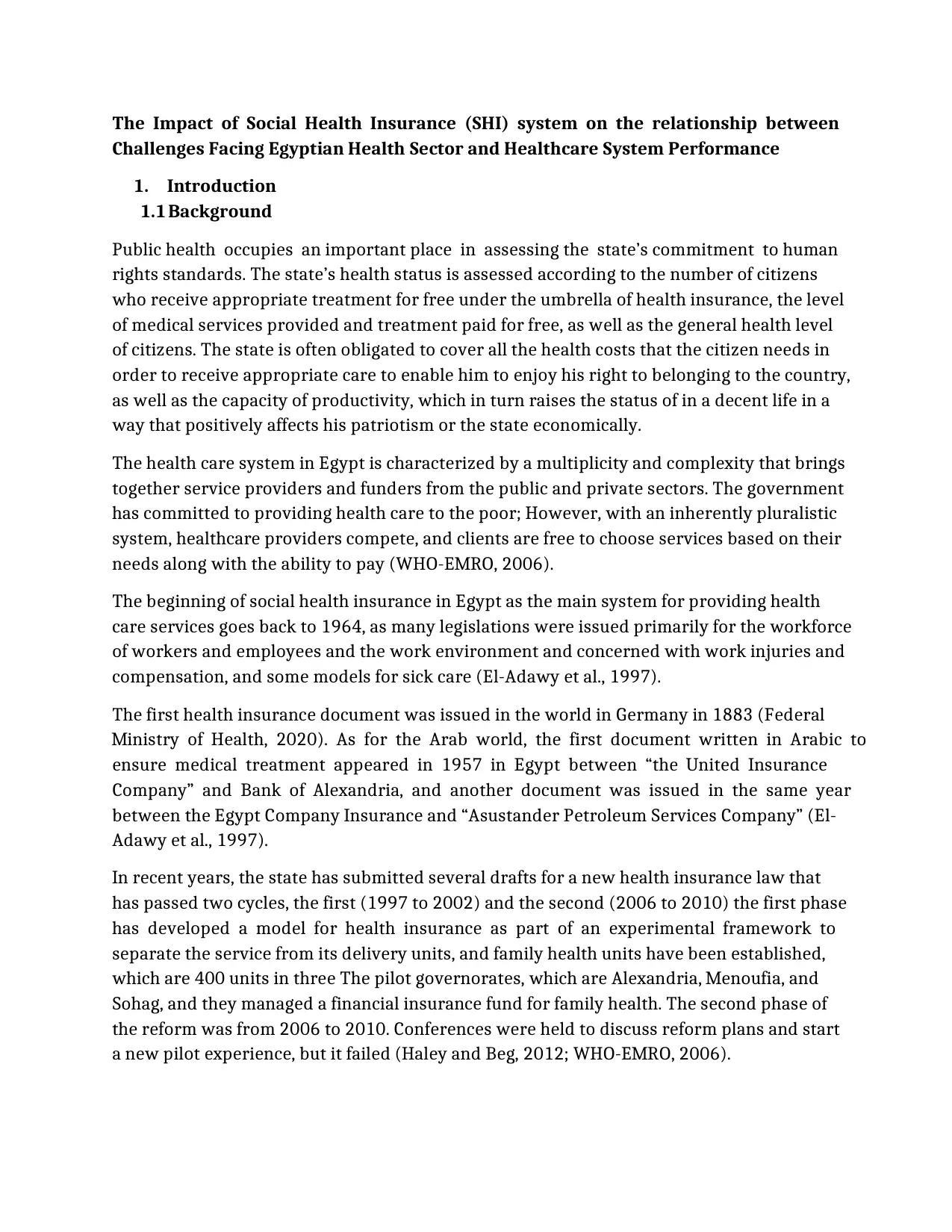
First, it is necessary to mention some important indicators that illustrate the extent of the
deterioration of the health care system performance in Egypt. World Bank data show that
the infant mortality rate was very high in 2009, while it tends to slowly decline until it
reached 17.3 in 2019, which is still high as well. It also shows that Egypt was and still suffers
from a shortage of hospital beds, which include inpatient beds available in the public and
private sectors, public and specialized hospitals, and rehabilitation centers, as shown in
Figure 3 and Figure 4.
Figure 3: Egypt infant mortality rate
Source: By author using WB Data
0
5
10
15
20
25
30
2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
25.1 24.1 23.1 22.2 21.4 20.6 19.9 19.2 18.5 17.9 17.3
infant mortality rate (in deaths per 1000 live births) in
Egypt
providers receive life-time licensing with no continuous medical education (CME)
requirements. Dual practice is allowed with no restrictions by law and therefore rampant.
Also, Egypt is one of the lowest healthcare spenders in the Middle East and North Africa
(MENA) region and more than half of the total health expenditure (THE) is out-of-pocket
(OOP). In addition to low health spending, systemic inefficiencies and inequities in health
financing limit the effectiveness of the healthcare system.
First, it is necessary to mention some important indicators that illustrate the extent of the
deterioration of the health care system performance in Egypt. World Bank data show that
the infant mortality rate was very high in 2009, while it tends to slowly decline until it
reached 17.3 in 2019, which is still high as well. It also shows that Egypt was and still suffers
from a shortage of hospital beds, which include inpatient beds available in the public and
private sectors, public and specialized hospitals, and rehabilitation centers, as shown in
Figure 3 and Figure 4.
Figure 3: Egypt infant mortality rate
Source: By author using WB Data
0
5
10
15
20
25
30
2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019
25.1 24.1 23.1 22.2 21.4 20.6 19.9 19.2 18.5 17.9 17.3
infant mortality rate (in deaths per 1000 live births) in
Egypt
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
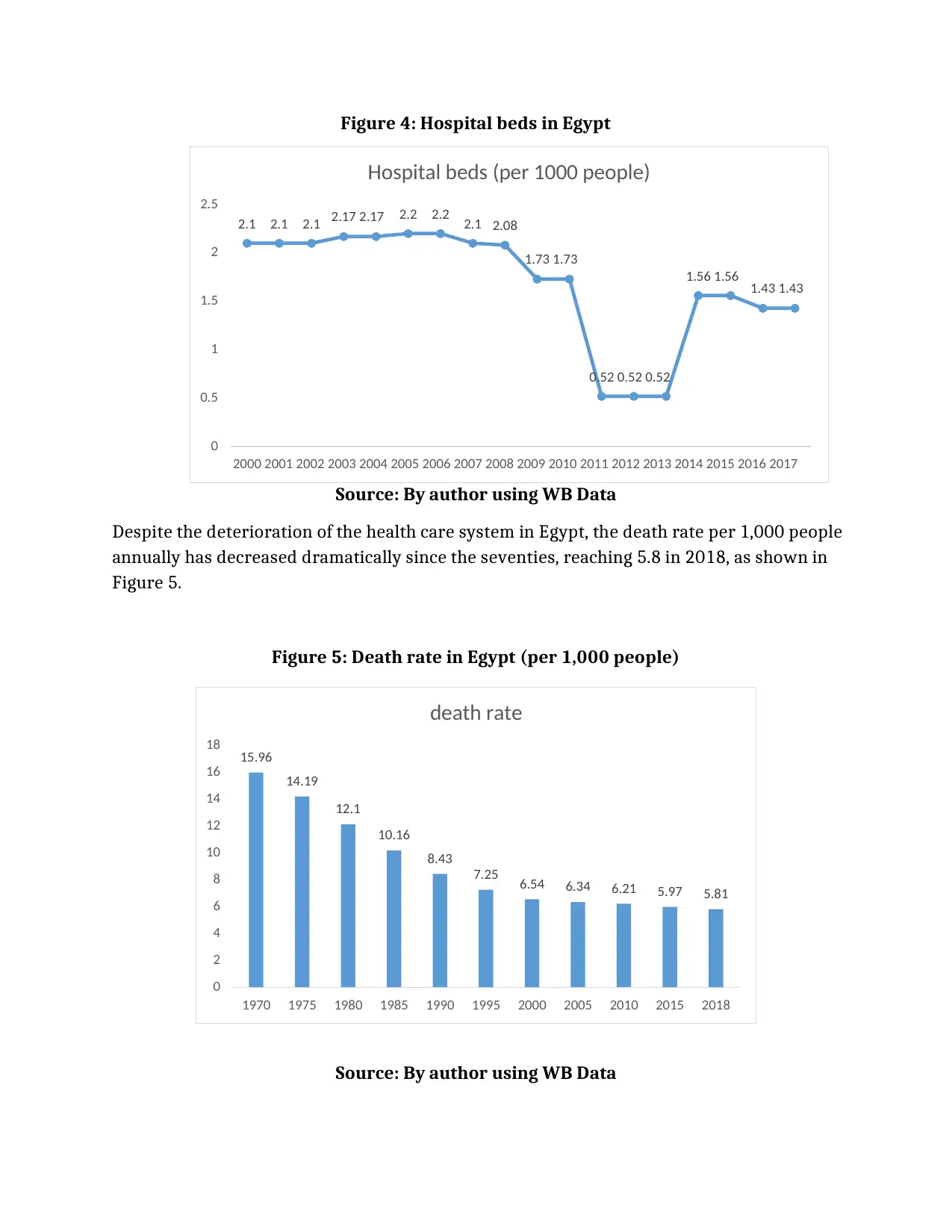
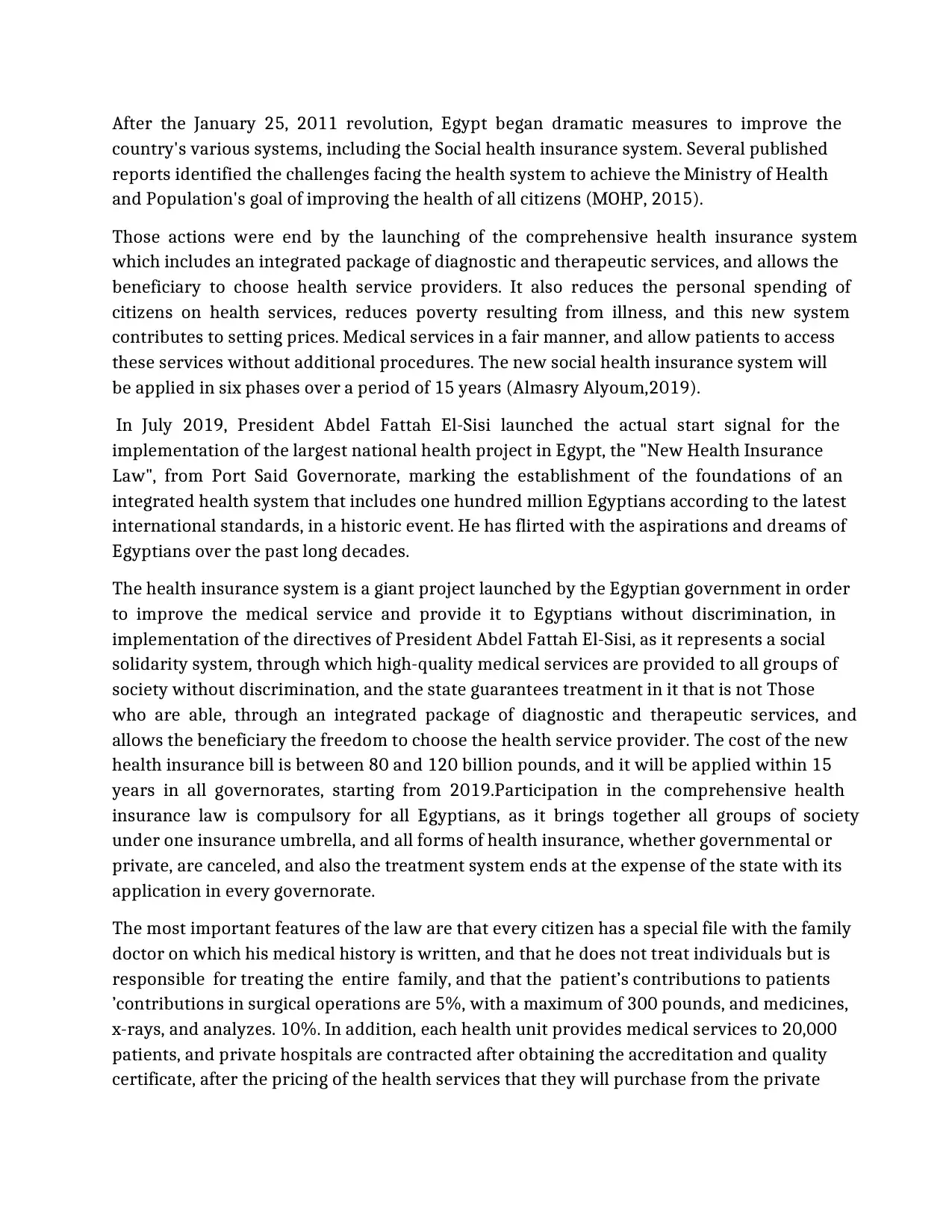
Figure 4: Hospital beds in Egypt
Source: By author using WB Data
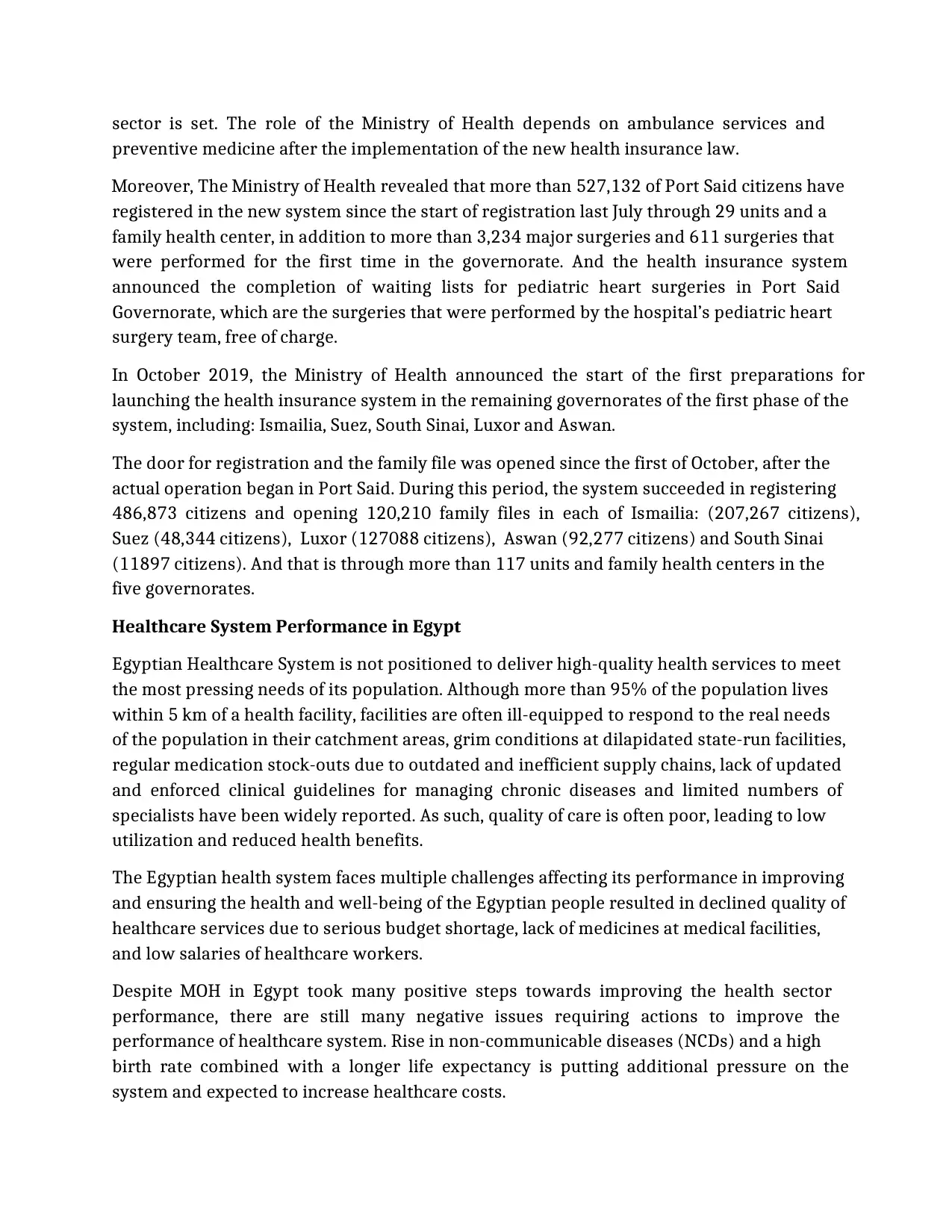
Despite the deterioration of the health care system in Egypt, the death rate per 1,000 people
annually has decreased dramatically since the seventies, reaching 5.8 in 2018, as shown in
Figure 5.
Figure 5: Death rate in Egypt (per 1,000 people)
Source: By author using WB Data
2.1 2.1 2.1 2.17 2.17 2.2 2.2 2.1 2.08
1.73 1.73
0.52 0.52 0.52
1.56 1.56 1.43 1.43
0
0.5
1
1.5
2
2.5
2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017
Hospital beds (per 1000 people)
15.96
14.19
12.1
10.16
8.43
7.25 6.54 6.34 6.21 5.97 5.81
0
2
4
6
8
10
12
14
16
18
1970 1975 1980 1985 1990 1995 2000 2005 2010 2015 2018
death rate
Source: By author using WB Data
Despite the deterioration of the health care system in Egypt, the death rate per 1,000 people
annually has decreased dramatically since the seventies, reaching 5.8 in 2018, as shown in
Figure 5.
Figure 5: Death rate in Egypt (per 1,000 people)
Source: By author using WB Data
2.1 2.1 2.1 2.17 2.17 2.2 2.2 2.1 2.08
1.73 1.73
0.52 0.52 0.52
1.56 1.56 1.43 1.43
0
0.5
1
1.5
2
2.5
2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017
Hospital beds (per 1000 people)
15.96
14.19
12.1
10.16
8.43
7.25 6.54 6.34 6.21 5.97 5.81
0
2
4
6
8
10
12
14
16
18
1970 1975 1980 1985 1990 1995 2000 2005 2010 2015 2018
death rate
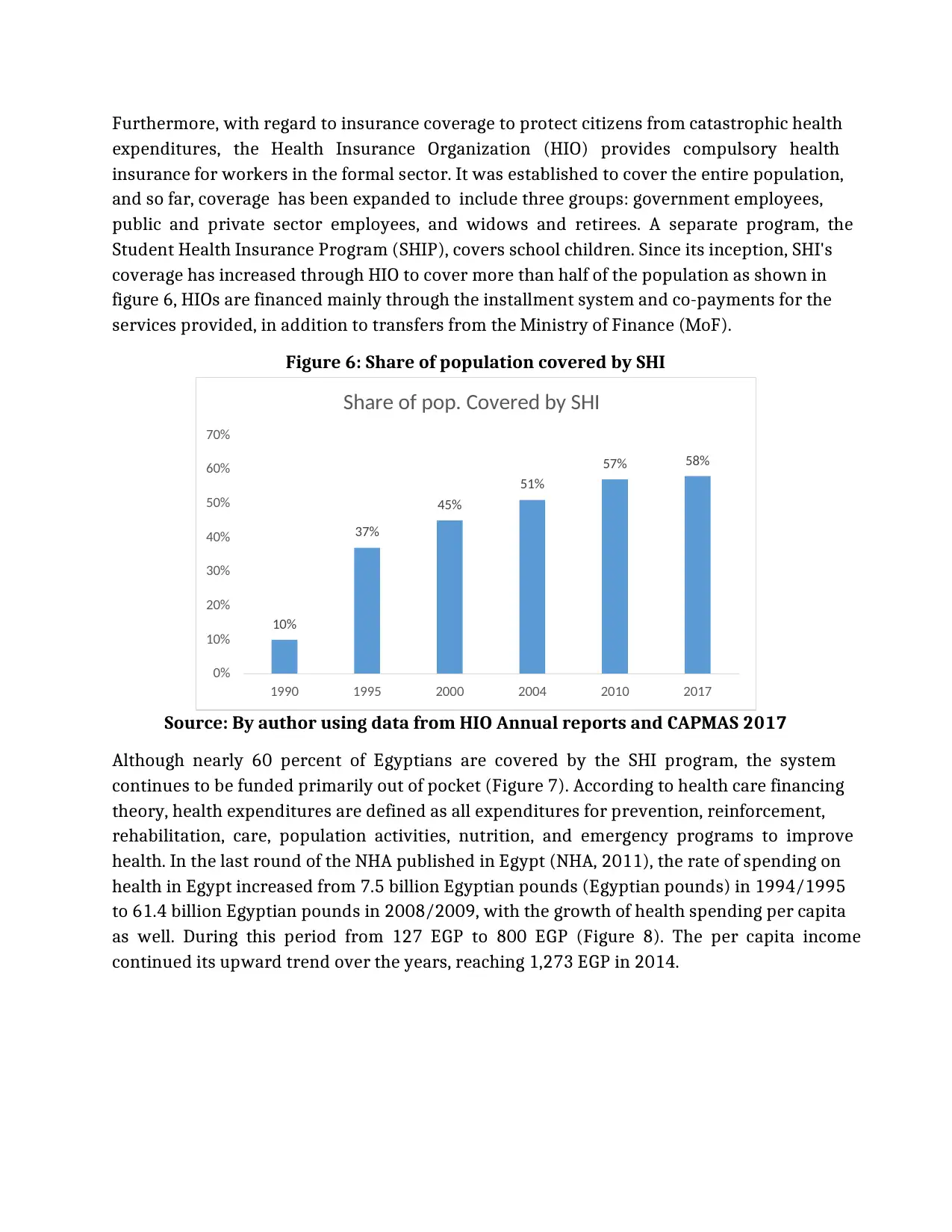
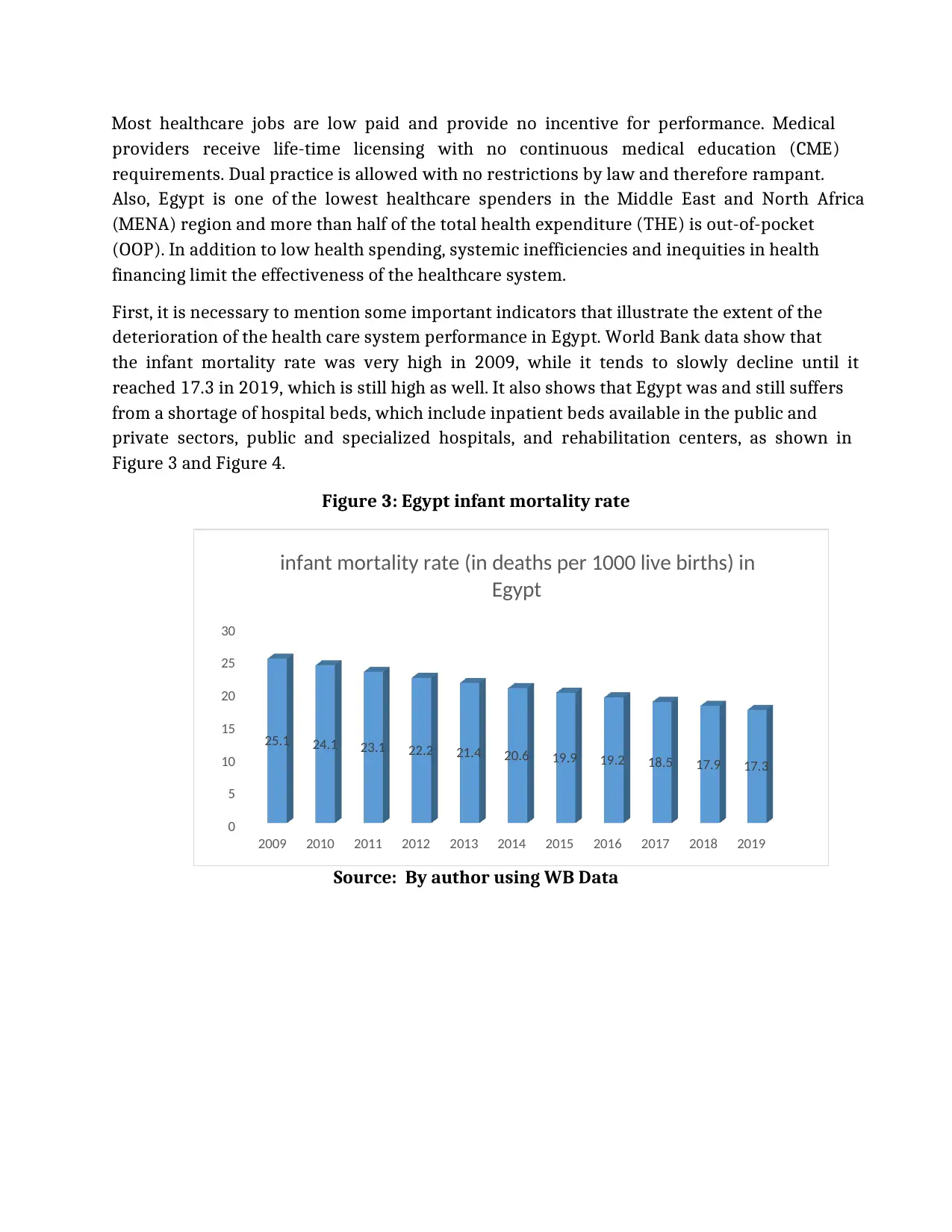
Furthermore, with regard to insurance coverage to protect citizens from catastrophic health
expenditures, the Health Insurance Organization (HIO) provides compulsory health
insurance for workers in the formal sector. It was established to cover the entire population,
and so far, coverage has been expanded to include three groups: government employees,
public and private sector employees, and widows and retirees. A separate program, the
Student Health Insurance Program (SHIP), covers school children. Since its inception, SHI's
coverage has increased through HIO to cover more than half of the population as shown in
figure 6, HIOs are financed mainly through the installment system and co-payments for the
services provided, in addition to transfers from the Ministry of Finance (MoF).
Figure 6: Share of population covered by SHI
Source: By author using data from HIO Annual reports and CAPMAS 2017
Although nearly 60 percent of Egyptians are covered by the SHI program, the system
continues to be funded primarily out of pocket (Figure 7). According to health care financing
theory, health expenditures are defined as all expenditures for prevention, reinforcement,
rehabilitation, care, population activities, nutrition, and emergency programs to improve
health. In the last round of the NHA published in Egypt (NHA, 2011), the rate of spending on
health in Egypt increased from 7.5 billion Egyptian pounds (Egyptian pounds) in 1994/1995
to 61.4 billion Egyptian pounds in 2008/2009, with the growth of health spending per capita
as well. During this period from 127 EGP to 800 EGP (Figure 8). The per capita income
continued its upward trend over the years, reaching 1,273 EGP in 2014.
10%
37%
45%
51%
57% 58%
0%
10%
20%
30%
40%
50%
60%
70%
1990 1995 2000 2004 2010 2017
Share of pop. Covered by SHI
expenditures, the Health Insurance Organization (HIO) provides compulsory health
insurance for workers in the formal sector. It was established to cover the entire population,
and so far, coverage has been expanded to include three groups: government employees,
public and private sector employees, and widows and retirees. A separate program, the
Student Health Insurance Program (SHIP), covers school children. Since its inception, SHI's
coverage has increased through HIO to cover more than half of the population as shown in
figure 6, HIOs are financed mainly through the installment system and co-payments for the
services provided, in addition to transfers from the Ministry of Finance (MoF).
Figure 6: Share of population covered by SHI
Source: By author using data from HIO Annual reports and CAPMAS 2017
Although nearly 60 percent of Egyptians are covered by the SHI program, the system
continues to be funded primarily out of pocket (Figure 7). According to health care financing
theory, health expenditures are defined as all expenditures for prevention, reinforcement,
rehabilitation, care, population activities, nutrition, and emergency programs to improve
health. In the last round of the NHA published in Egypt (NHA, 2011), the rate of spending on
health in Egypt increased from 7.5 billion Egyptian pounds (Egyptian pounds) in 1994/1995
to 61.4 billion Egyptian pounds in 2008/2009, with the growth of health spending per capita
as well. During this period from 127 EGP to 800 EGP (Figure 8). The per capita income
continued its upward trend over the years, reaching 1,273 EGP in 2014.
10%
37%
45%
51%
57% 58%
0%
10%
20%
30%
40%
50%
60%
70%
1990 1995 2000 2004 2010 2017
Share of pop. Covered by SHI
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
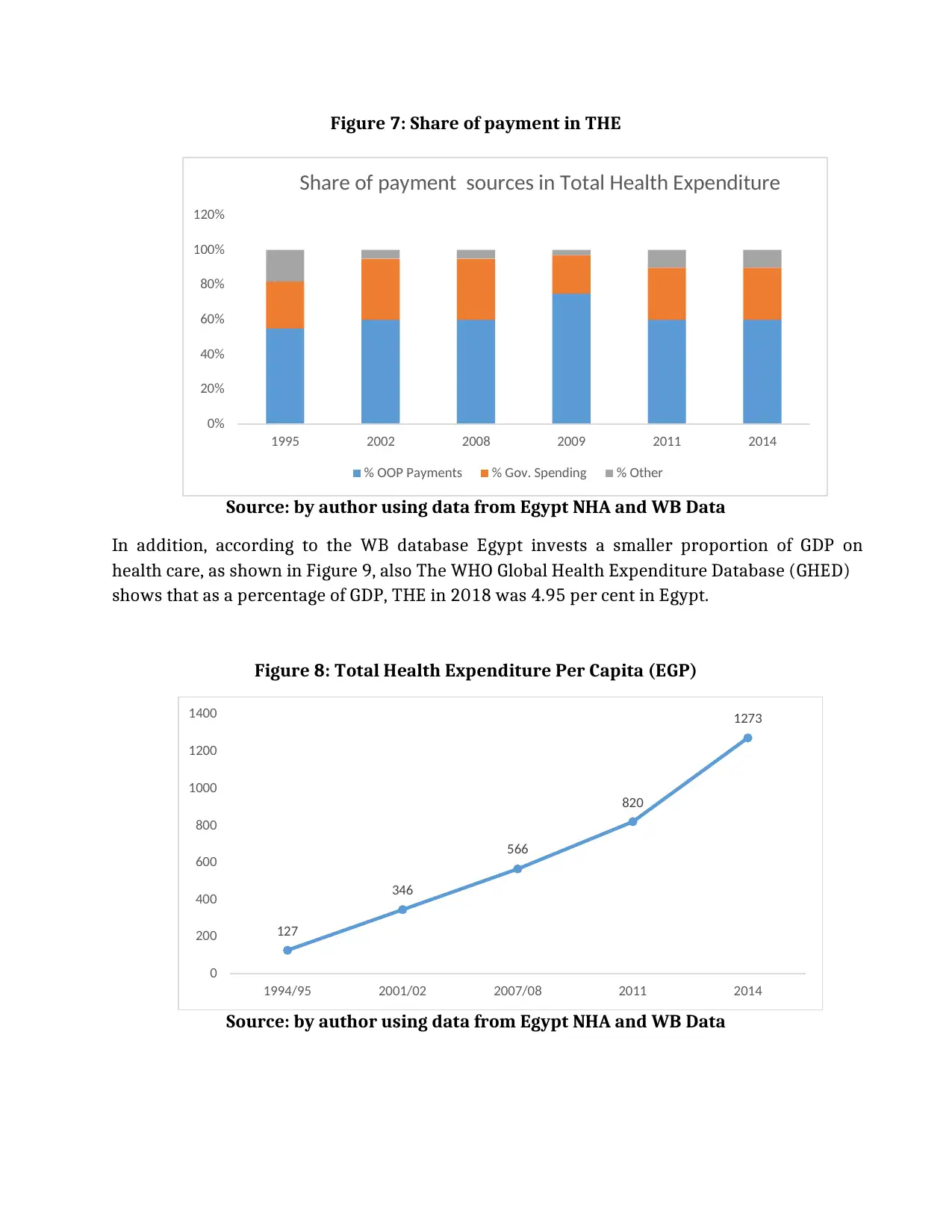
Figure 7: Share of payment in THE
Source: by author using data from Egypt NHA and WB Data
In addition, according to the WB database Egypt invests a smaller proportion of GDP on
health care, as shown in Figure 9, also The WHO Global Health Expenditure Database (GHED)
shows that as a percentage of GDP, THE in 2018 was 4.95 per cent in Egypt.
Figure 8: Total Health Expenditure Per Capita (EGP)
Source: by author using data from Egypt NHA and WB Data
0%
20%
40%
60%
80%
100%
120%
1995 2002 2008 2009 2011 2014
Share of payment sources in Total Health Expenditure
% OOP Payments % Gov. Spending % Other
127
346
566
820
1273
0
200
400
600
800
1000
1200
1400
1994/95 2001/02 2007/08 2011 2014
Source: by author using data from Egypt NHA and WB Data
In addition, according to the WB database Egypt invests a smaller proportion of GDP on
health care, as shown in Figure 9, also The WHO Global Health Expenditure Database (GHED)
shows that as a percentage of GDP, THE in 2018 was 4.95 per cent in Egypt.
Figure 8: Total Health Expenditure Per Capita (EGP)
Source: by author using data from Egypt NHA and WB Data
0%
20%
40%
60%
80%
100%
120%
1995 2002 2008 2009 2011 2014
Share of payment sources in Total Health Expenditure
% OOP Payments % Gov. Spending % Other
127
346
566
820
1273
0
200
400
600
800
1000
1200
1400
1994/95 2001/02 2007/08 2011 2014
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
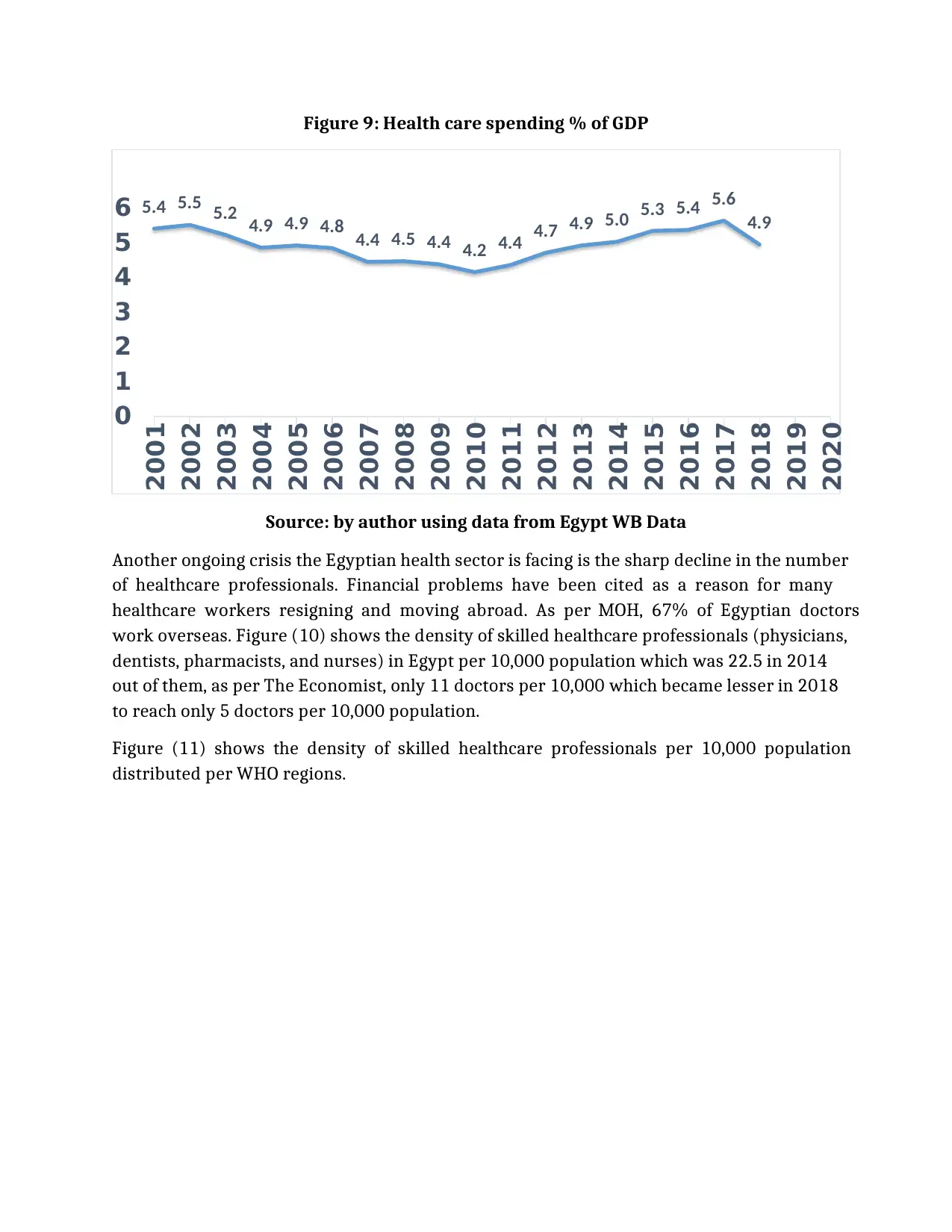
Figure 9: Health care spending % of GDP
Source: by author using data from Egypt WB Data
Another ongoing crisis the Egyptian health sector is facing is the sharp decline in the number
of healthcare professionals. Financial problems have been cited as a reason for many
healthcare workers resigning and moving abroad. As per MOH, 67% of Egyptian doctors
work overseas. Figure (10) shows the density of skilled healthcare professionals (physicians,
dentists, pharmacists, and nurses) in Egypt per 10,000 population which was 22.5 in 2014
out of them, as per The Economist, only 11 doctors per 10,000 which became lesser in 2018
to reach only 5 doctors per 10,000 population.
Figure (11) shows the density of skilled healthcare professionals per 10,000 population
distributed per WHO regions.
5.4 5.5 5.2 4.9 4.9 4.8 4.4 4.5 4.4 4.2 4.4 4.7 4.9 5.0 5.3 5.4 5.6
4.9
0
1
2
3
4
5
6
2001
2002
2003
2004
2005
2006
2007
2008
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
2019
2020
Source: by author using data from Egypt WB Data
Another ongoing crisis the Egyptian health sector is facing is the sharp decline in the number
of healthcare professionals. Financial problems have been cited as a reason for many
healthcare workers resigning and moving abroad. As per MOH, 67% of Egyptian doctors
work overseas. Figure (10) shows the density of skilled healthcare professionals (physicians,
dentists, pharmacists, and nurses) in Egypt per 10,000 population which was 22.5 in 2014
out of them, as per The Economist, only 11 doctors per 10,000 which became lesser in 2018
to reach only 5 doctors per 10,000 population.
Figure (11) shows the density of skilled healthcare professionals per 10,000 population
distributed per WHO regions.
5.4 5.5 5.2 4.9 4.9 4.8 4.4 4.5 4.4 4.2 4.4 4.7 4.9 5.0 5.3 5.4 5.6
4.9
0
1
2
3
4
5
6
2001
2002
2003
2004
2005
2006
2007
2008
2009
2010
2011
2012
2013
2014
2015
2016
2017
2018
2019
2020
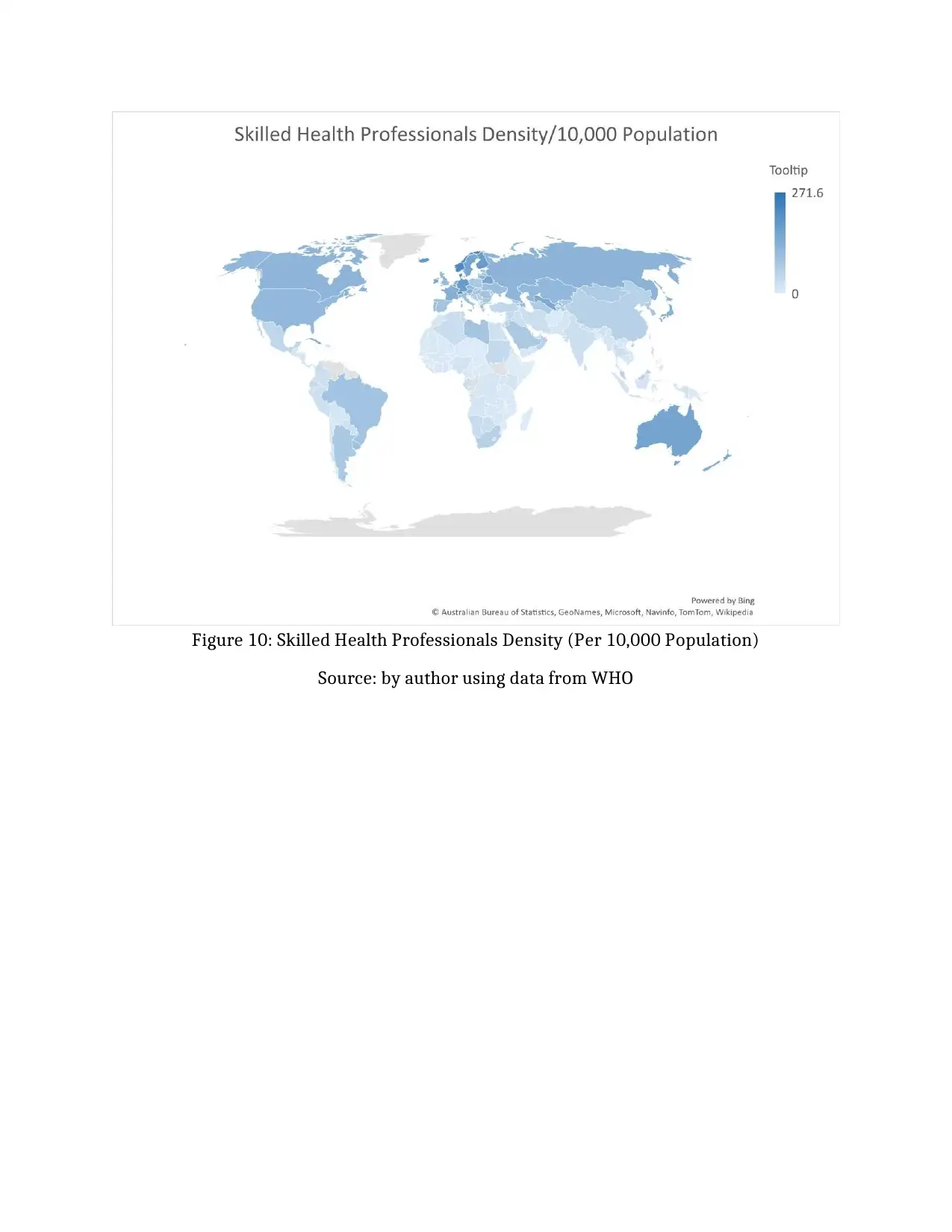
Figure 10: Skilled Health Professionals Density (Per 10,000 Population)
Source: by author using data from WHO
Source: by author using data from WHO
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
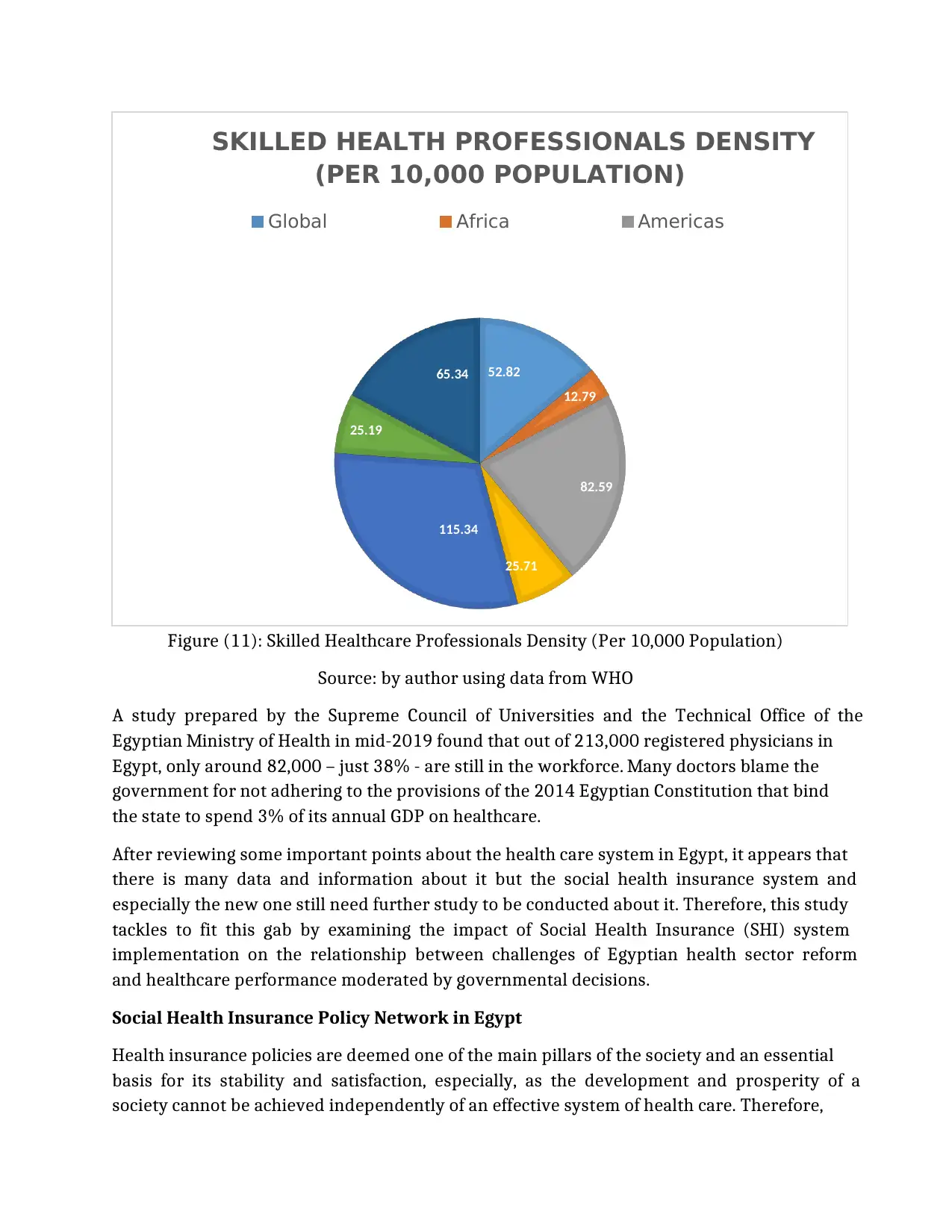
Figure (11): Skilled Healthcare Professionals Density (Per 10,000 Population)
Source: by author using data from WHO
A study prepared by the Supreme Council of Universities and the Technical Office of the
Egyptian Ministry of Health in mid-2019 found that out of 213,000 registered physicians in
Egypt, only around 82,000 – just 38% - are still in the workforce. Many doctors blame the
government for not adhering to the provisions of the 2014 Egyptian Constitution that bind
the state to spend 3% of its annual GDP on healthcare.
After reviewing some important points about the health care system in Egypt, it appears that
there is many data and information about it but the social health insurance system and
especially the new one still need further study to be conducted about it. Therefore, this study
tackles to fit this gab by examining the impact of Social Health Insurance (SHI) system
implementation on the relationship between challenges of Egyptian health sector reform
and healthcare performance moderated by governmental decisions.
Social Health Insurance Policy Network in Egypt
Health insurance policies are deemed one of the main pillars of the society and an essential
basis for its stability and satisfaction, especially, as the development and prosperity of a
society cannot be achieved independently of an effective system of health care. Therefore,
52.82
12.79
82.59
25.71
115.34
25.19
65.34
SKILLED HEALTH PROFESSIONALS DENSITY
(PER 10,000 POPULATION)
Global Africa Americas
Source: by author using data from WHO
A study prepared by the Supreme Council of Universities and the Technical Office of the
Egyptian Ministry of Health in mid-2019 found that out of 213,000 registered physicians in
Egypt, only around 82,000 – just 38% - are still in the workforce. Many doctors blame the
government for not adhering to the provisions of the 2014 Egyptian Constitution that bind
the state to spend 3% of its annual GDP on healthcare.
After reviewing some important points about the health care system in Egypt, it appears that
there is many data and information about it but the social health insurance system and
especially the new one still need further study to be conducted about it. Therefore, this study
tackles to fit this gab by examining the impact of Social Health Insurance (SHI) system
implementation on the relationship between challenges of Egyptian health sector reform
and healthcare performance moderated by governmental decisions.
Social Health Insurance Policy Network in Egypt
Health insurance policies are deemed one of the main pillars of the society and an essential
basis for its stability and satisfaction, especially, as the development and prosperity of a
society cannot be achieved independently of an effective system of health care. Therefore,
52.82
12.79
82.59
25.71
115.34
25.19
65.34
SKILLED HEALTH PROFESSIONALS DENSITY
(PER 10,000 POPULATION)
Global Africa Americas
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
these policies received considerable attention from both the state and those who are
concerned with health issues.
Since the mid-1990s and after the deterioration of health services, there have been frequent
attempts to reform the health system in Egypt, especially with the support of donor entities
and the emergence of a number of new actors such as international organizations, the private
sector and civil society organizations working in the health sector.
The mutual influence enabled these actors – by working together within a network of social
health insurance policies – to have a prominent role in the policymaking process. Although
Law No. 2 of 2018 on comprehensive health insurance has been enacted and put into effect,
scant studies examined the lawmaking and the impact of policy networks on its
development. The available studies, however, focused on health insurance policies with
regard to public satisfaction, outsourcing, funding, restructuring, etc. To fill this gap in
research, this study attempts to investigate the impact of policy networks on the making of
comprehensive health insurance law in Egypt.
1.2 Research problem
The key role of the new SHI is to provide medical services of high quality for all segments of
society without discrimination. Aims to reduce poverty and disease and focuses on the
provision of full medical protection for all members of the family in exchange for payment of
contributions. The current SHI system can get more advantages from the accumulation of
previous reforms of improving health system in Egypt, increasing surveillance, and reducing
communicable disease incidence (WHO 2010).
However, due to Egypt's lower middle-income status, the overall health of its population is
relatively poor compared to other lower middle-income countries. Moreover, despite some
improvements, the burden of non-communicable diseases has increased, adding to the
pressure on the health system in Egypt, which has undoubtedly led to the clarity of the
importance of having a system to achieve universal health care (Roberts et al. 2013).
A question that remains of paramount importance in a majority of the world’s countries is
how the health systems can provide sufficient healthy protection from epidemics and
diseases to all of the population without any burden of costs of healthcare and also without
discrimination between them (Ileana et al., 2020).
Therefore, the study will shed the light on how assessing the new social health insurance
program through four main pillars:
1. Pros and cons of implementing the new social health insurance program.
2. The concerns facing the implementation process.
3. The primary results of implementing the new social health insurance program.
concerned with health issues.
Since the mid-1990s and after the deterioration of health services, there have been frequent
attempts to reform the health system in Egypt, especially with the support of donor entities
and the emergence of a number of new actors such as international organizations, the private
sector and civil society organizations working in the health sector.
The mutual influence enabled these actors – by working together within a network of social
health insurance policies – to have a prominent role in the policymaking process. Although
Law No. 2 of 2018 on comprehensive health insurance has been enacted and put into effect,
scant studies examined the lawmaking and the impact of policy networks on its
development. The available studies, however, focused on health insurance policies with
regard to public satisfaction, outsourcing, funding, restructuring, etc. To fill this gap in
research, this study attempts to investigate the impact of policy networks on the making of
comprehensive health insurance law in Egypt.
1.2 Research problem
The key role of the new SHI is to provide medical services of high quality for all segments of
society without discrimination. Aims to reduce poverty and disease and focuses on the
provision of full medical protection for all members of the family in exchange for payment of
contributions. The current SHI system can get more advantages from the accumulation of
previous reforms of improving health system in Egypt, increasing surveillance, and reducing
communicable disease incidence (WHO 2010).
However, due to Egypt's lower middle-income status, the overall health of its population is
relatively poor compared to other lower middle-income countries. Moreover, despite some
improvements, the burden of non-communicable diseases has increased, adding to the
pressure on the health system in Egypt, which has undoubtedly led to the clarity of the
importance of having a system to achieve universal health care (Roberts et al. 2013).
A question that remains of paramount importance in a majority of the world’s countries is
how the health systems can provide sufficient healthy protection from epidemics and
diseases to all of the population without any burden of costs of healthcare and also without
discrimination between them (Ileana et al., 2020).
Therefore, the study will shed the light on how assessing the new social health insurance
program through four main pillars:
1. Pros and cons of implementing the new social health insurance program.
2. The concerns facing the implementation process.
3. The primary results of implementing the new social health insurance program.
4. Emergence and evolution of the concept of social health insurance policy network in
Egypt and its impact on the stages of health insurance policymaking.
Research Questions
This work aims to address the following research problem:
I. What is the current situation concerning healthcare system in Egypt?
II. What are the basic features of social health insurance and how it will
contribute in solving the problem?
III. What are the main challenges and opportunities associated with the
implementation of the new social health insurance system in Egypt?
IV. What are the main processes of implementing a high-quality universal SHI in
developing countries?
V. How did the policy network affect the stages of health insurance
policymaking in Egypt?
VI. What are the most important recommendations through which we can
benefit from these networks in the development of the health sector?
Research aims and Objectives
The main objective of this study is to evaluate the impact of the implementation of Social
Health Insurance (SHI) system on the relationship between challenges of Egyptian health
sector reform and healthcare performance moderated by governmental decisions.
This paper includes a description about the characteristics of the new Egyptian social health
insurance system, the pillars underpinning it and the main obstacles which hamper its
implementation and how to overcome it to achieve a better progress towards sustainable
development for Egypt and the developing countries as well. This document will also
present, in addition to the SWOT analysis for the Egyptian social health insurance system,
detailed instructions for measuring its performance and an annex including its different
initiatives.
Egypt and its impact on the stages of health insurance policymaking.
Research Questions
This work aims to address the following research problem:
I. What is the current situation concerning healthcare system in Egypt?
II. What are the basic features of social health insurance and how it will
contribute in solving the problem?
III. What are the main challenges and opportunities associated with the
implementation of the new social health insurance system in Egypt?
IV. What are the main processes of implementing a high-quality universal SHI in
developing countries?
V. How did the policy network affect the stages of health insurance
policymaking in Egypt?
VI. What are the most important recommendations through which we can
benefit from these networks in the development of the health sector?
Research aims and Objectives
The main objective of this study is to evaluate the impact of the implementation of Social
Health Insurance (SHI) system on the relationship between challenges of Egyptian health
sector reform and healthcare performance moderated by governmental decisions.
This paper includes a description about the characteristics of the new Egyptian social health
insurance system, the pillars underpinning it and the main obstacles which hamper its
implementation and how to overcome it to achieve a better progress towards sustainable
development for Egypt and the developing countries as well. This document will also
present, in addition to the SWOT analysis for the Egyptian social health insurance system,
detailed instructions for measuring its performance and an annex including its different
initiatives.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 26
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





