Hospital Staffing and Health Care–Associated Infections: A Systematic Review of the Literature
VerifiedAdded on 2023/03/20
|10
|8786
|72
AI Summary
This systematic review examines the relationship between hospital staffing and the risk of acquiring health care–associated infections (HAIs). The review found that increased staffing is related to a decreased risk of acquiring HAIs. More rigorous and consistent research designs, definitions, and risk-adjusted HAI data are needed in future studies exploring this area.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Hospital Staffing and Health Care–Associated Infections:
A Systematic Review of the Literature
Brett G. Mitchell, PhD, MAdvPrac; Anne Gardner, PhD; Patricia W. Stone, PhD, RN, FAAN; Lisa Hall, PhD;
Monika Pogorzelska-Maziarz, PhD
Background:Previous literature has linked the level and types of staffing of health facilities to the risk of acquiring a health
care–associated infection (HAI). Investigating this relationship is challenging because of the lack of rigorous study designs
and the use of varying definitions and measures of both staffing and HAIs.
Methods:The objective of this study was to understand and synthesize the most recent research on the relationship of
hospital staffing and HAI risk. A systematic review was undertaken. Electronic databases MEDLINE, PubMed, and the Cu-
mulative Index to Nursing and Allied Health Literature (CINAHL) were searched for studies published between January 1,
2000, and November 30, 2015.
Results:Fifty-four articles were included in the review. The majority of studies examined the relationship between nurse
staffing and HAIs (n = 50, 92.6%) and found nurse staffing variables to be associated with an increase in HAI rates (n = 40,
74.1%). Only 5 studies addressed non-nurse staffing, and those had mixed results. Physician staffing was associated with an
increased HAI risk in 1 of 3 studies. Studies varied in design and methodology, as well as in their use of operational defi-
nitions and measures of staffing and HAIs.
Conclusion:Despite the lack of consistency of the included studies, overall, the results of this systematic review demon-
strate that increased staffing is related to decreased risk of acquiring HAIs. More rigorous and consistent research designs,
definitions, and risk-adjusted HAI data are needed in future studies exploring this area.
Health care–associated infections (HAIs) are a serious
patient safety issue that result in increased morbidity
and mortality as well as excessive health resource utilization.1
Recent estimates from the United States show that on any
given day approximately 1 of every 25 inpatients in acute
care hospitals has at least one HAI.2 In Europe HAIs also
represent a considerable burden, with more than 2.5 million
cases occurring each year,resulting in approximately 2.5
million disability-adjusted life years.3 Given the significant
burden of HAIs with the potential for adverse outcomes in
patients, there is much interest in understanding their trans-
mission, prevention, and control. One particular issue is the
relationship between levels and types of staffing of health fa-
cilities and HAIs. A number of organizational factors that
influence the risk of HAIs have been identified, including
standardized HAI case definitions, adequate data sources, and
complex risk adjustment methods.9 Furthermore, the web
of causation linking staffing and HAI is difficult to under-
stand and may include factors such as the complexity of the
infection process,lack of time to comply with infection
control measures, and job-related burnout.9 Methodologi-
cal issues in studies examining the association between hospital
staffing and adverse outcomes have also been identified. These
include lack of application of standardized definitions of nurse
staffing,different databases,and diverse risk adjustment
methods.10 In addition, the temporal relationship between
staffing and HAI occurrence has recently been noted as a
methodological problem in studies examining hospital staff-
ing and HAI.11 HAIs are by definition infections that occur
48 hours after hospitaladmission.11 Hence,staffing levels
The Joint Commission Journalon Quality and Patient Safety 2018; 44:613–622
A Systematic Review of the Literature
Brett G. Mitchell, PhD, MAdvPrac; Anne Gardner, PhD; Patricia W. Stone, PhD, RN, FAAN; Lisa Hall, PhD;
Monika Pogorzelska-Maziarz, PhD
Background:Previous literature has linked the level and types of staffing of health facilities to the risk of acquiring a health
care–associated infection (HAI). Investigating this relationship is challenging because of the lack of rigorous study designs
and the use of varying definitions and measures of both staffing and HAIs.
Methods:The objective of this study was to understand and synthesize the most recent research on the relationship of
hospital staffing and HAI risk. A systematic review was undertaken. Electronic databases MEDLINE, PubMed, and the Cu-
mulative Index to Nursing and Allied Health Literature (CINAHL) were searched for studies published between January 1,
2000, and November 30, 2015.
Results:Fifty-four articles were included in the review. The majority of studies examined the relationship between nurse
staffing and HAIs (n = 50, 92.6%) and found nurse staffing variables to be associated with an increase in HAI rates (n = 40,
74.1%). Only 5 studies addressed non-nurse staffing, and those had mixed results. Physician staffing was associated with an
increased HAI risk in 1 of 3 studies. Studies varied in design and methodology, as well as in their use of operational defi-
nitions and measures of staffing and HAIs.
Conclusion:Despite the lack of consistency of the included studies, overall, the results of this systematic review demon-
strate that increased staffing is related to decreased risk of acquiring HAIs. More rigorous and consistent research designs,
definitions, and risk-adjusted HAI data are needed in future studies exploring this area.
Health care–associated infections (HAIs) are a serious
patient safety issue that result in increased morbidity
and mortality as well as excessive health resource utilization.1
Recent estimates from the United States show that on any
given day approximately 1 of every 25 inpatients in acute
care hospitals has at least one HAI.2 In Europe HAIs also
represent a considerable burden, with more than 2.5 million
cases occurring each year,resulting in approximately 2.5
million disability-adjusted life years.3 Given the significant
burden of HAIs with the potential for adverse outcomes in
patients, there is much interest in understanding their trans-
mission, prevention, and control. One particular issue is the
relationship between levels and types of staffing of health fa-
cilities and HAIs. A number of organizational factors that
influence the risk of HAIs have been identified, including
standardized HAI case definitions, adequate data sources, and
complex risk adjustment methods.9 Furthermore, the web
of causation linking staffing and HAI is difficult to under-
stand and may include factors such as the complexity of the
infection process,lack of time to comply with infection
control measures, and job-related burnout.9 Methodologi-
cal issues in studies examining the association between hospital
staffing and adverse outcomes have also been identified. These
include lack of application of standardized definitions of nurse
staffing,different databases,and diverse risk adjustment
methods.10 In addition, the temporal relationship between
staffing and HAI occurrence has recently been noted as a
methodological problem in studies examining hospital staff-
ing and HAI.11 HAIs are by definition infections that occur
48 hours after hospitaladmission.11 Hence,staffing levels
The Joint Commission Journalon Quality and Patient Safety 2018; 44:613–622
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
hospital staffing and HAI risk will inform health adminis-
trators,policy makers,and researchers on strategies for
preventing HAIs and thereby improving patient outcomes.
This systematic review therefore aims to examine the asso-
ciation between hospitalstaffing and patients’risk of
developing HAIs in hospital settings.
METHODS
A systematic review of the literature was undertaken to iden-
tify publications that examine the relationships between
hospital staffing and patients’ risk of developing an HAI in
the hospitalsetting. The approach used is consistent with
a previous systematic review of this topic.12Reporting of this
systematic review complied with the preferred reporting items
for systematic reviewsand meta-analyses(PRISMA)
guidelines.14
Protocol and Registration
The protocol for conducting this review was registered prior
to commencement of the review and can be accessed on the
internationalprospective register ofsystematic reviews
(PROSPERO) (registration number: CRD42015032398).
Search Strategy
A systematic search of the literature was conducted accord-
ing to the registered protocol. Electronic databases PubMed
and the Cumulative Index to Nursing and Allied Health Lit-
erature (CINAHL) were searched for studies published
between January 1,2000,and November 30,2015. The
search was performed on December 7,2015.A combina-
tion of Medical Subject Headings (MeSH) and free-text terms
were used,including “infection control,” “staffing,” and
“healthcare associated infection.” For retrieved articles,a
manual search of the reference lists was also performed to
identify any additional studies. Searches were restricted to
studies published in the English language only.
Selection Criteria
The inclusion criteria were all observational studies (cohort,
case control, or cross-sectional) examining the relationship
community-acquired infections, and articles written in lan-
guages other than English.
Definitions
For the purpose of this systematic review, the following defi-
nitions were used:
• Hospital staffing was defined as nurse staffing, medical
staffing, or infection prevention and control staffing.
• Nurse staffing levels were described using one or more
of the following variables:levelof staffing (nurse-to-
patientratio or nursing hours per patient-day or
admission), skill mix, use of float or nonpermanent staff,
absenteeism and/or overtime, workload.
• Health care–associated infectionscomprised blood-
stream infection,pneumonia,urinary tract infection,
wound or surgical site infection, organism-specific in-
fections (for example, Clostridium difficile infection) that
were defined as being health care–associated in the studies
included in the review. The definition of HAI in the
included studies was based on a recognized standard;
that is,a definition agreed on or published by a pro-
fessional association or government agency (for example,
the Centers for Disease Control and Prevention [CDC]),
a definition widely used in the published literature, or
an International Classification of Diseases, Ninth Re-
vision,ClinicalModification (ICD-9-CM) code that
constitutes an HAI (not just any infection).
Study Selection
The titles and abstracts of all articles identified were exam-
ined and assessed for relevance and appropriateness to the
systematic review aim,and those not relevant were ex-
cluded. The fulltexts of potentially relevant articles were
obtained to further assess eligibility based on the inclusion
and exclusion criteria. Articles with data relevant to the sys-
tematic review were included. The electronic database search
and study selection process were performed by trained re-
search assistants. At each stage of the study selection process,
10% of articles retrieved were selected at random and re-
viewed by the study lead author as a cross-check against study
eligibility.Any discrepancies in the application of the in-
clusion or exclusion criteria were resolved by the lead author.
614 Brett G. Mitchell, PhD, MAdvPrac, et al HospitalStaffing and Risk of Infection
trators,policy makers,and researchers on strategies for
preventing HAIs and thereby improving patient outcomes.
This systematic review therefore aims to examine the asso-
ciation between hospitalstaffing and patients’risk of
developing HAIs in hospital settings.
METHODS
A systematic review of the literature was undertaken to iden-
tify publications that examine the relationships between
hospital staffing and patients’ risk of developing an HAI in
the hospitalsetting. The approach used is consistent with
a previous systematic review of this topic.12Reporting of this
systematic review complied with the preferred reporting items
for systematic reviewsand meta-analyses(PRISMA)
guidelines.14
Protocol and Registration
The protocol for conducting this review was registered prior
to commencement of the review and can be accessed on the
internationalprospective register ofsystematic reviews
(PROSPERO) (registration number: CRD42015032398).
Search Strategy
A systematic search of the literature was conducted accord-
ing to the registered protocol. Electronic databases PubMed
and the Cumulative Index to Nursing and Allied Health Lit-
erature (CINAHL) were searched for studies published
between January 1,2000,and November 30,2015. The
search was performed on December 7,2015.A combina-
tion of Medical Subject Headings (MeSH) and free-text terms
were used,including “infection control,” “staffing,” and
“healthcare associated infection.” For retrieved articles,a
manual search of the reference lists was also performed to
identify any additional studies. Searches were restricted to
studies published in the English language only.
Selection Criteria
The inclusion criteria were all observational studies (cohort,
case control, or cross-sectional) examining the relationship
community-acquired infections, and articles written in lan-
guages other than English.
Definitions
For the purpose of this systematic review, the following defi-
nitions were used:
• Hospital staffing was defined as nurse staffing, medical
staffing, or infection prevention and control staffing.
• Nurse staffing levels were described using one or more
of the following variables:levelof staffing (nurse-to-
patientratio or nursing hours per patient-day or
admission), skill mix, use of float or nonpermanent staff,
absenteeism and/or overtime, workload.
• Health care–associated infectionscomprised blood-
stream infection,pneumonia,urinary tract infection,
wound or surgical site infection, organism-specific in-
fections (for example, Clostridium difficile infection) that
were defined as being health care–associated in the studies
included in the review. The definition of HAI in the
included studies was based on a recognized standard;
that is,a definition agreed on or published by a pro-
fessional association or government agency (for example,
the Centers for Disease Control and Prevention [CDC]),
a definition widely used in the published literature, or
an International Classification of Diseases, Ninth Re-
vision,ClinicalModification (ICD-9-CM) code that
constitutes an HAI (not just any infection).
Study Selection
The titles and abstracts of all articles identified were exam-
ined and assessed for relevance and appropriateness to the
systematic review aim,and those not relevant were ex-
cluded. The fulltexts of potentially relevant articles were
obtained to further assess eligibility based on the inclusion
and exclusion criteria. Articles with data relevant to the sys-
tematic review were included. The electronic database search
and study selection process were performed by trained re-
search assistants. At each stage of the study selection process,
10% of articles retrieved were selected at random and re-
viewed by the study lead author as a cross-check against study
eligibility.Any discrepancies in the application of the in-
clusion or exclusion criteria were resolved by the lead author.
614 Brett G. Mitchell, PhD, MAdvPrac, et al HospitalStaffing and Risk of Infection
incidence or prevalence data. Data extracted were crossed-
checked by a different research assistant.
Risk of Bias
An assessment of study quality and risk of bias in the ar-
ticles included in the review was conducted using the
Newcastle–Ottawa Scale.15,16
The content validity and inter-
rater reliability of this tool has been established.16One reviewer
undertook this assessment independently, with a random 10%
of articles reviewed by a second reviewer. No discrepancies
were identified.
Data Analysis
Extracted data from included studies were synthesized and
summarized in evidence tables.Summary tables include
studies that examined nurse staffing and single site–specific
HAI, nurse staffing and multiple types of HAI, nurse staff-
ing and organism-specific HAI, nurse staffing and unspecified
HAI, and non-nurse staffing and HAI.Given the hetero-
geneity of the studies included in the systematic review,
pooling of data in a meta-analysis was not feasible.
RESULTS
Overview
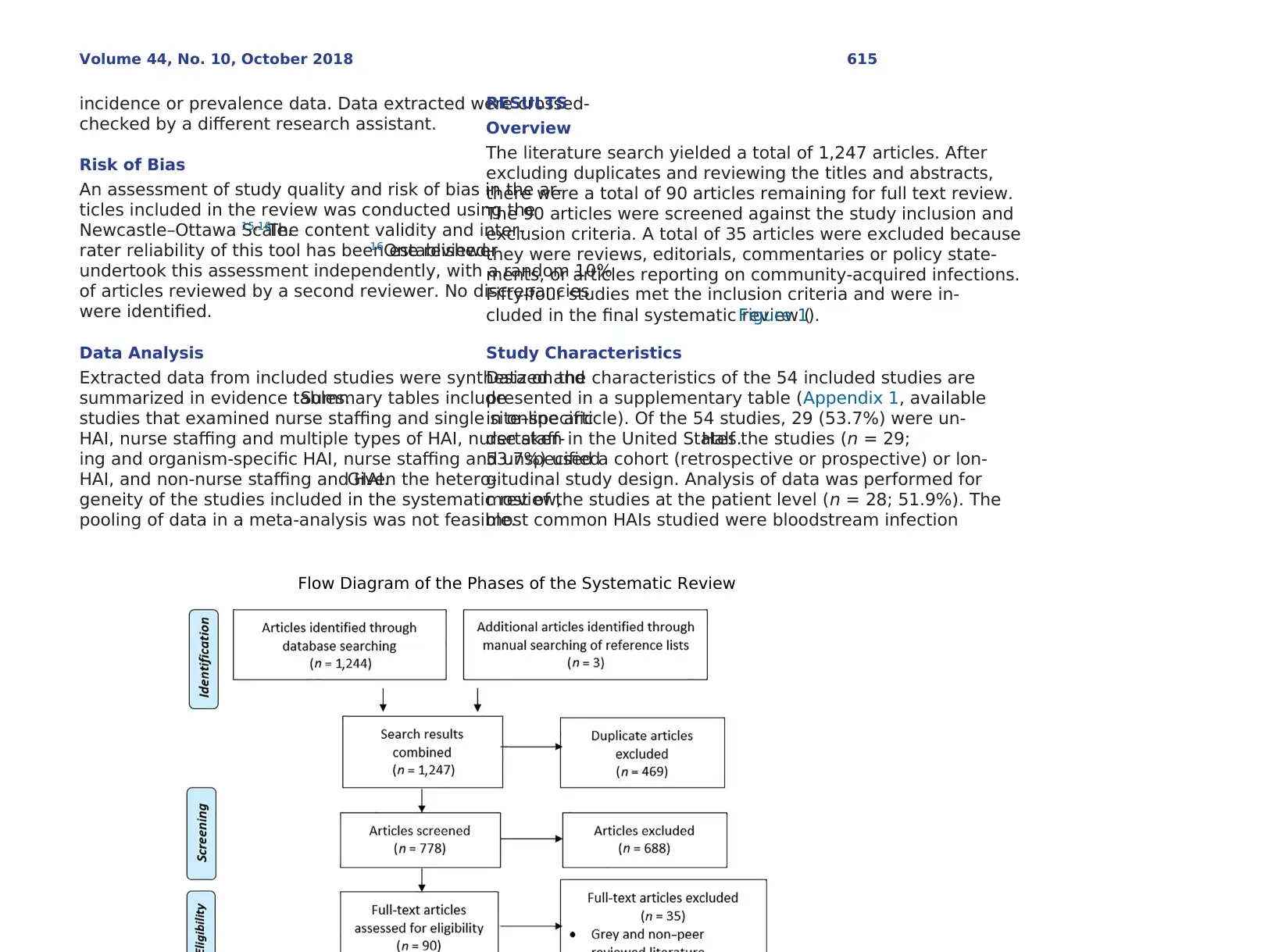
The literature search yielded a total of 1,247 articles. After
excluding duplicates and reviewing the titles and abstracts,
there were a total of 90 articles remaining for full text review.
The 90 articles were screened against the study inclusion and
exclusion criteria. A total of 35 articles were excluded because
they were reviews, editorials, commentaries or policy state-
ments, or articles reporting on community-acquired infections.
Fifty-four studies met the inclusion criteria and were in-
cluded in the final systematic review (Figure 1).
Study Characteristics
Data on the characteristics of the 54 included studies are
presented in a supplementary table (Appendix 1, available
in online article). Of the 54 studies, 29 (53.7%) were un-
dertaken in the United States.Half the studies (n = 29;
53.7%) used a cohort (retrospective or prospective) or lon-
gitudinal study design. Analysis of data was performed for
most of the studies at the patient level (n = 28; 51.9%). The
most common HAIs studied were bloodstream infection
Flow Diagram of the Phases of the Systematic Review
Volume 44, No. 10, October 2018 615
checked by a different research assistant.
Risk of Bias
An assessment of study quality and risk of bias in the ar-
ticles included in the review was conducted using the
Newcastle–Ottawa Scale.15,16
The content validity and inter-
rater reliability of this tool has been established.16One reviewer
undertook this assessment independently, with a random 10%
of articles reviewed by a second reviewer. No discrepancies
were identified.
Data Analysis
Extracted data from included studies were synthesized and
summarized in evidence tables.Summary tables include
studies that examined nurse staffing and single site–specific
HAI, nurse staffing and multiple types of HAI, nurse staff-
ing and organism-specific HAI, nurse staffing and unspecified
HAI, and non-nurse staffing and HAI.Given the hetero-
geneity of the studies included in the systematic review,
pooling of data in a meta-analysis was not feasible.
RESULTS
Overview
The literature search yielded a total of 1,247 articles. After
excluding duplicates and reviewing the titles and abstracts,
there were a total of 90 articles remaining for full text review.
The 90 articles were screened against the study inclusion and
exclusion criteria. A total of 35 articles were excluded because
they were reviews, editorials, commentaries or policy state-
ments, or articles reporting on community-acquired infections.
Fifty-four studies met the inclusion criteria and were in-
cluded in the final systematic review (Figure 1).
Study Characteristics
Data on the characteristics of the 54 included studies are
presented in a supplementary table (Appendix 1, available
in online article). Of the 54 studies, 29 (53.7%) were un-
dertaken in the United States.Half the studies (n = 29;
53.7%) used a cohort (retrospective or prospective) or lon-
gitudinal study design. Analysis of data was performed for
most of the studies at the patient level (n = 28; 51.9%). The
most common HAIs studied were bloodstream infection
Flow Diagram of the Phases of the Systematic Review
Volume 44, No. 10, October 2018 615
(BSI) (n = 30; 55.6%), pneumonia (n = 24; 44.4%), urinary
tract infection (UTI) (n = 21;38.9%),and wound infec-
tion (n = 8; 14.8%). The most frequent type of hospital staff
examined were nurses (n = 50; 92.6%). Of these, the ma-
jority (n = 40; 74.1%) found a significant association between
the nurse staffing variable(s) studied and HAI risk.The
number of stars awarded to studies as part of the risk of bias
assessment ranged from three to nine, with the full assess-
ment presented in a supplementary table (Appendix 2,
available in online article). Twenty-one of the 54 articles re-
ceived five or more stars. Studies were of moderate quality,
however,as many of the included studies did not control
for potential confounders (comparability). All studies were
included in the review, regardless of the risk of bias assess-
ment.As no meta-analysis was performed and there was
considerable heterogeneity in the study methods, no further
subanalysis of results based on the risk of bias assessment
was undertaken.
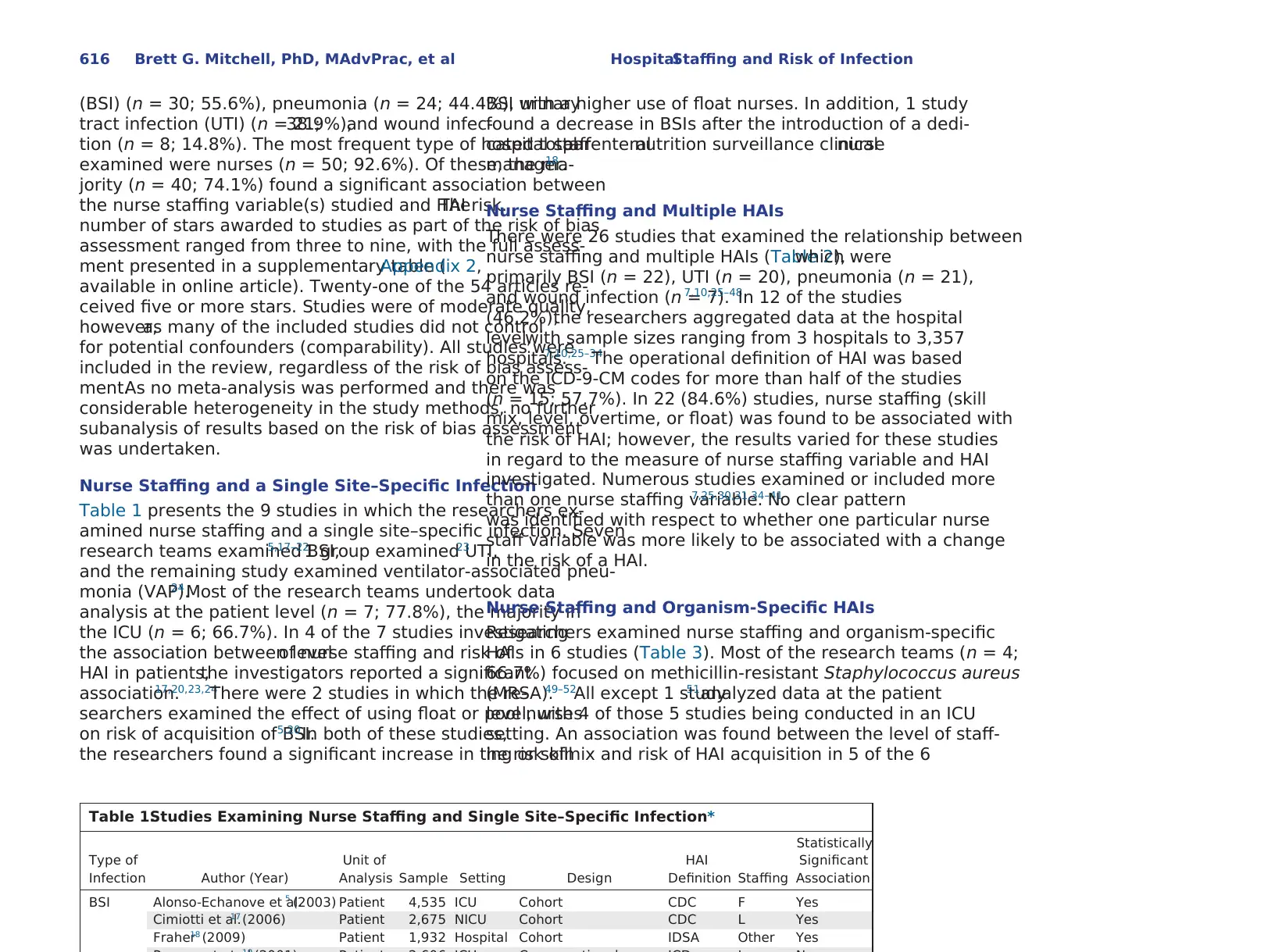
Nurse Staffing and a Single Site–Specific Infection
Table 1 presents the 9 studies in which the researchers ex-
amined nurse staffing and a single site–specific infection. Seven
research teams examined BSI,5,17–22
1 group examined UTI,23
and the remaining study examined ventilator-associated pneu-
monia (VAP).24 Most of the research teams undertook data
analysis at the patient level (n = 7; 77.8%), the majority in
the ICU (n = 6; 66.7%). In 4 of the 7 studies investigating
the association between levelof nurse staffing and risk of
HAI in patients,the investigators reported a significant
association.17,20,23,24
There were 2 studies in which the re-
searchers examined the effect of using float or pool nurses
on risk of acquisition of BSI.5,20 In both of these studies,
the researchers found a significant increase in the risk of
BSI with a higher use of float nurses. In addition, 1 study
found a decrease in BSIs after the introduction of a dedi-
cated totalparenteralnutrition surveillance clinicalnurse
manager.18
Nurse Staffing and Multiple HAIs
There were 26 studies that examined the relationship between
nurse staffing and multiple HAIs (Table 2),which were
primarily BSI (n = 22), UTI (n = 20), pneumonia (n = 21),
and wound infection (n = 7).7,10,25–48
In 12 of the studies
(46.2%),the researchers aggregated data at the hospital
level,with sample sizes ranging from 3 hospitals to 3,357
hospitals.7,10,25–34
The operational definition of HAI was based
on the ICD-9-CM codes for more than half of the studies
(n = 15; 57.7%). In 22 (84.6%) studies, nurse staffing (skill
mix, level, overtime, or float) was found to be associated with
the risk of HAI; however, the results varied for these studies
in regard to the measure of nurse staffing variable and HAI
investigated. Numerous studies examined or included more
than one nurse staffing variable.7,25,30,31,34–41
No clear pattern
was identified with respect to whether one particular nurse
staff variable was more likely to be associated with a change
in the risk of a HAI.
Nurse Staffing and Organism-Specific HAIs
Researchers examined nurse staffing and organism-specific
HAIs in 6 studies (Table 3). Most of the research teams (n = 4;
66.7%) focused on methicillin-resistant Staphylococcus aureus
(MRSA).49–52
All except 1 study51analyzed data at the patient
level, with 4 of those 5 studies being conducted in an ICU
setting. An association was found between the level of staff-
ing or skillmix and risk of HAI acquisition in 5 of the 6
Table 1.Studies Examining Nurse Staffing and Single Site–Specific Infection*
Type of
Infection Author (Year)
Unit of
Analysis Sample Setting Design
HAI
Definition Staffing
Statistically
Significant
Association
BSI Alonso-Echanove et al.5 (2003) Patient 4,535 ICU Cohort CDC F Yes
Cimiotti et al.17 (2006) Patient 2,675 NICU Cohort CDC L Yes
Fraher18 (2009) Patient 1,932 Hospital Cohort IDSA Other Yes
616 Brett G. Mitchell, PhD, MAdvPrac, et al HospitalStaffing and Risk of Infection
tract infection (UTI) (n = 21;38.9%),and wound infec-
tion (n = 8; 14.8%). The most frequent type of hospital staff
examined were nurses (n = 50; 92.6%). Of these, the ma-
jority (n = 40; 74.1%) found a significant association between
the nurse staffing variable(s) studied and HAI risk.The
number of stars awarded to studies as part of the risk of bias
assessment ranged from three to nine, with the full assess-
ment presented in a supplementary table (Appendix 2,
available in online article). Twenty-one of the 54 articles re-
ceived five or more stars. Studies were of moderate quality,
however,as many of the included studies did not control
for potential confounders (comparability). All studies were
included in the review, regardless of the risk of bias assess-
ment.As no meta-analysis was performed and there was
considerable heterogeneity in the study methods, no further
subanalysis of results based on the risk of bias assessment
was undertaken.
Nurse Staffing and a Single Site–Specific Infection
Table 1 presents the 9 studies in which the researchers ex-
amined nurse staffing and a single site–specific infection. Seven
research teams examined BSI,5,17–22
1 group examined UTI,23
and the remaining study examined ventilator-associated pneu-
monia (VAP).24 Most of the research teams undertook data
analysis at the patient level (n = 7; 77.8%), the majority in
the ICU (n = 6; 66.7%). In 4 of the 7 studies investigating
the association between levelof nurse staffing and risk of
HAI in patients,the investigators reported a significant
association.17,20,23,24
There were 2 studies in which the re-
searchers examined the effect of using float or pool nurses
on risk of acquisition of BSI.5,20 In both of these studies,
the researchers found a significant increase in the risk of
BSI with a higher use of float nurses. In addition, 1 study
found a decrease in BSIs after the introduction of a dedi-
cated totalparenteralnutrition surveillance clinicalnurse
manager.18
Nurse Staffing and Multiple HAIs
There were 26 studies that examined the relationship between
nurse staffing and multiple HAIs (Table 2),which were
primarily BSI (n = 22), UTI (n = 20), pneumonia (n = 21),
and wound infection (n = 7).7,10,25–48
In 12 of the studies
(46.2%),the researchers aggregated data at the hospital
level,with sample sizes ranging from 3 hospitals to 3,357
hospitals.7,10,25–34
The operational definition of HAI was based
on the ICD-9-CM codes for more than half of the studies
(n = 15; 57.7%). In 22 (84.6%) studies, nurse staffing (skill
mix, level, overtime, or float) was found to be associated with
the risk of HAI; however, the results varied for these studies
in regard to the measure of nurse staffing variable and HAI
investigated. Numerous studies examined or included more
than one nurse staffing variable.7,25,30,31,34–41
No clear pattern
was identified with respect to whether one particular nurse
staff variable was more likely to be associated with a change
in the risk of a HAI.
Nurse Staffing and Organism-Specific HAIs
Researchers examined nurse staffing and organism-specific
HAIs in 6 studies (Table 3). Most of the research teams (n = 4;
66.7%) focused on methicillin-resistant Staphylococcus aureus
(MRSA).49–52
All except 1 study51analyzed data at the patient
level, with 4 of those 5 studies being conducted in an ICU
setting. An association was found between the level of staff-
ing or skillmix and risk of HAI acquisition in 5 of the 6
Table 1.Studies Examining Nurse Staffing and Single Site–Specific Infection*
Type of
Infection Author (Year)
Unit of
Analysis Sample Setting Design
HAI
Definition Staffing
Statistically
Significant
Association
BSI Alonso-Echanove et al.5 (2003) Patient 4,535 ICU Cohort CDC F Yes
Cimiotti et al.17 (2006) Patient 2,675 NICU Cohort CDC L Yes
Fraher18 (2009) Patient 1,932 Hospital Cohort IDSA Other Yes
616 Brett G. Mitchell, PhD, MAdvPrac, et al HospitalStaffing and Risk of Infection
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
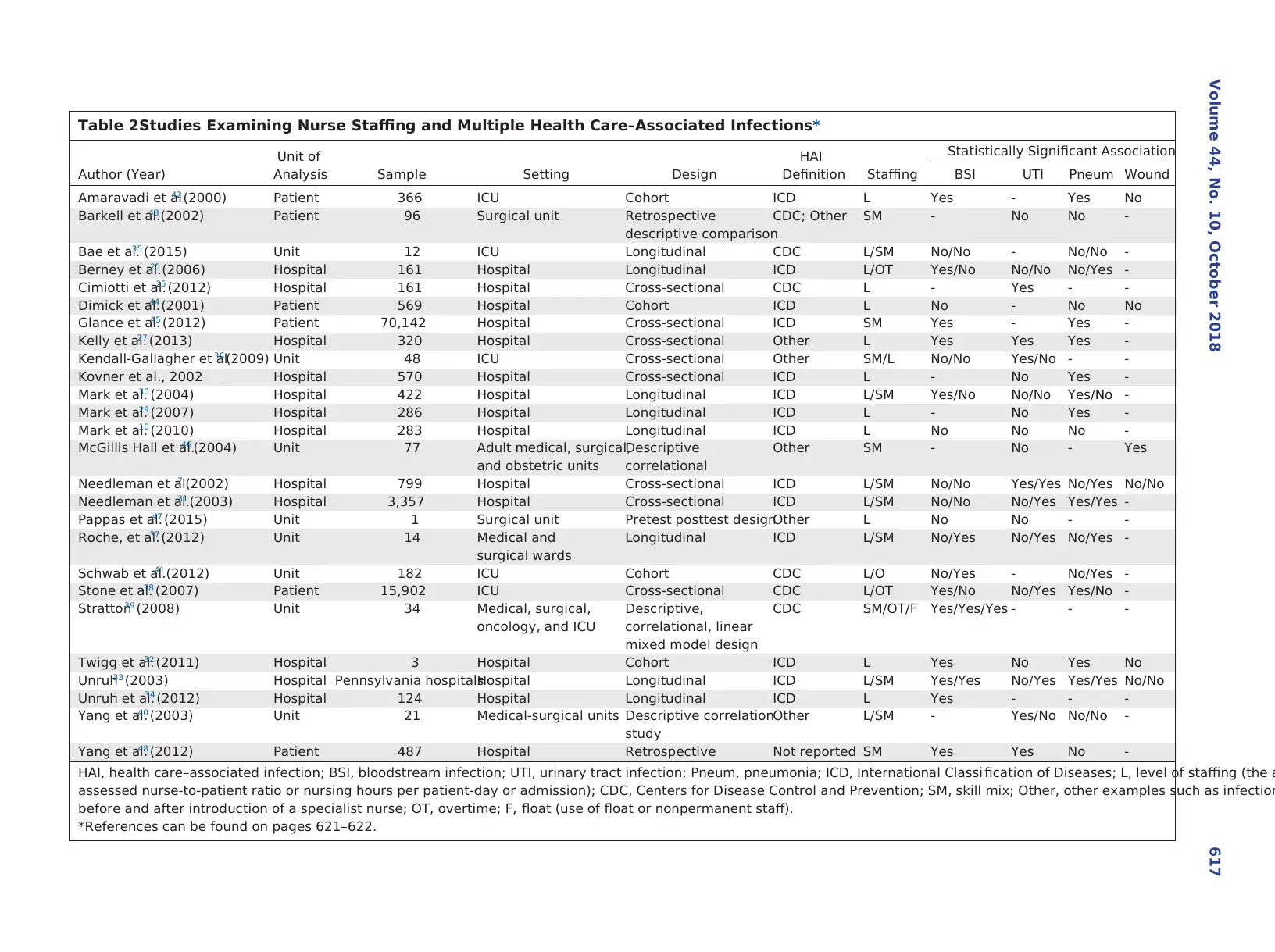
Table 2.Studies Examining Nurse Staffing and Multiple Health Care–Associated Infections*
Author (Year)
Unit of
Analysis Sample Setting Design
HAI
Definition Staffing
Statistically Significant Association
BSI UTI Pneum Wound
Amaravadi et al.42 (2000) Patient 366 ICU Cohort ICD L Yes - Yes No
Barkell et al.43 (2002) Patient 96 Surgical unit Retrospective
descriptive comparison
CDC; Other SM - No No -
Bae et al.35 (2015) Unit 12 ICU Longitudinal CDC L/SM No/No - No/No -
Berney et al.25 (2006) Hospital 161 Hospital Longitudinal ICD L/OT Yes/No No/No No/Yes -
Cimiotti et al.25 (2012) Hospital 161 Hospital Cross-sectional CDC L - Yes - -
Dimick et al.44 (2001) Patient 569 Hospital Cohort ICD L No - No No
Glance et al.45 (2012) Patient 70,142 Hospital Cross-sectional ICD SM Yes - Yes -
Kelly et al.27 (2013) Hospital 320 Hospital Cross-sectional Other L Yes Yes Yes -
Kendall-Gallagher et al.36 (2009) Unit 48 ICU Cross-sectional Other SM/L No/No Yes/No - -
Kovner et al., 2002 Hospital 570 Hospital Cross-sectional ICD L - No Yes -
Mark et al.30 (2004) Hospital 422 Hospital Longitudinal ICD L/SM Yes/No No/No Yes/No -
Mark et al.29 (2007) Hospital 286 Hospital Longitudinal ICD L - No Yes -
Mark et al.10 (2010) Hospital 283 Hospital Longitudinal ICD L No No No -
McGillis Hall et al.46 (2004) Unit 77 Adult medical, surgical,
and obstetric units
Descriptive
correlational
Other SM - No - Yes
Needleman et al.7 (2002) Hospital 799 Hospital Cross-sectional ICD L/SM No/No Yes/Yes No/Yes No/No
Needleman et al.31 (2003) Hospital 3,357 Hospital Cross-sectional ICD L/SM No/No No/Yes Yes/Yes -
Pappas et al.47 (2015) Unit 1 Surgical unit Pretest posttest designOther L No No - -
Roche, et al.37 (2012) Unit 14 Medical and
surgical wards
Longitudinal ICD L/SM No/Yes No/Yes No/Yes -
Schwab et al.41 (2012) Unit 182 ICU Cohort CDC L/O No/Yes - No/Yes -
Stone et al.38 (2007) Patient 15,902 ICU Cross-sectional CDC L/OT Yes/No No/Yes Yes/No -
Stratton39 (2008) Unit 34 Medical, surgical,
oncology, and ICU
Descriptive,
correlational, linear
mixed model design
CDC SM/OT/F Yes/Yes/Yes - - -
Twigg et al.32 (2011) Hospital 3 Hospital Cohort ICD L Yes No Yes No
Unruh33 (2003) Hospital Pennsylvania hospitalsHospital Longitudinal ICD L/SM Yes/Yes No/Yes Yes/Yes No/No
Unruh et al.34 (2012) Hospital 124 Hospital Longitudinal ICD L Yes - - -
Yang et al.40 (2003) Unit 21 Medical-surgical units Descriptive correlation
study
Other L/SM - Yes/No No/No -
Yang et al.48 (2012) Patient 487 Hospital Retrospective Not reported SM Yes Yes No -
HAI, health care–associated infection; BSI, bloodstream infection; UTI, urinary tract infection; Pneum, pneumonia; ICD, International Classi fication of Diseases; L, level of staffing (the a
assessed nurse-to-patient ratio or nursing hours per patient-day or admission); CDC, Centers for Disease Control and Prevention; SM, skill mix; Other, other examples such as infection
before and after introduction of a specialist nurse; OT, overtime; F, float (use of float or nonpermanent staff).
*References can be found on pages 621–622.
Volume 44, No. 10, October 2018 617
Author (Year)
Unit of
Analysis Sample Setting Design
HAI
Definition Staffing
Statistically Significant Association
BSI UTI Pneum Wound
Amaravadi et al.42 (2000) Patient 366 ICU Cohort ICD L Yes - Yes No
Barkell et al.43 (2002) Patient 96 Surgical unit Retrospective
descriptive comparison
CDC; Other SM - No No -
Bae et al.35 (2015) Unit 12 ICU Longitudinal CDC L/SM No/No - No/No -
Berney et al.25 (2006) Hospital 161 Hospital Longitudinal ICD L/OT Yes/No No/No No/Yes -
Cimiotti et al.25 (2012) Hospital 161 Hospital Cross-sectional CDC L - Yes - -
Dimick et al.44 (2001) Patient 569 Hospital Cohort ICD L No - No No
Glance et al.45 (2012) Patient 70,142 Hospital Cross-sectional ICD SM Yes - Yes -
Kelly et al.27 (2013) Hospital 320 Hospital Cross-sectional Other L Yes Yes Yes -
Kendall-Gallagher et al.36 (2009) Unit 48 ICU Cross-sectional Other SM/L No/No Yes/No - -
Kovner et al., 2002 Hospital 570 Hospital Cross-sectional ICD L - No Yes -
Mark et al.30 (2004) Hospital 422 Hospital Longitudinal ICD L/SM Yes/No No/No Yes/No -
Mark et al.29 (2007) Hospital 286 Hospital Longitudinal ICD L - No Yes -
Mark et al.10 (2010) Hospital 283 Hospital Longitudinal ICD L No No No -
McGillis Hall et al.46 (2004) Unit 77 Adult medical, surgical,
and obstetric units
Descriptive
correlational
Other SM - No - Yes
Needleman et al.7 (2002) Hospital 799 Hospital Cross-sectional ICD L/SM No/No Yes/Yes No/Yes No/No
Needleman et al.31 (2003) Hospital 3,357 Hospital Cross-sectional ICD L/SM No/No No/Yes Yes/Yes -
Pappas et al.47 (2015) Unit 1 Surgical unit Pretest posttest designOther L No No - -
Roche, et al.37 (2012) Unit 14 Medical and
surgical wards
Longitudinal ICD L/SM No/Yes No/Yes No/Yes -
Schwab et al.41 (2012) Unit 182 ICU Cohort CDC L/O No/Yes - No/Yes -
Stone et al.38 (2007) Patient 15,902 ICU Cross-sectional CDC L/OT Yes/No No/Yes Yes/No -
Stratton39 (2008) Unit 34 Medical, surgical,
oncology, and ICU
Descriptive,
correlational, linear
mixed model design
CDC SM/OT/F Yes/Yes/Yes - - -
Twigg et al.32 (2011) Hospital 3 Hospital Cohort ICD L Yes No Yes No
Unruh33 (2003) Hospital Pennsylvania hospitalsHospital Longitudinal ICD L/SM Yes/Yes No/Yes Yes/Yes No/No
Unruh et al.34 (2012) Hospital 124 Hospital Longitudinal ICD L Yes - - -
Yang et al.40 (2003) Unit 21 Medical-surgical units Descriptive correlation
study
Other L/SM - Yes/No No/No -
Yang et al.48 (2012) Patient 487 Hospital Retrospective Not reported SM Yes Yes No -
HAI, health care–associated infection; BSI, bloodstream infection; UTI, urinary tract infection; Pneum, pneumonia; ICD, International Classi fication of Diseases; L, level of staffing (the a
assessed nurse-to-patient ratio or nursing hours per patient-day or admission); CDC, Centers for Disease Control and Prevention; SM, skill mix; Other, other examples such as infection
before and after introduction of a specialist nurse; OT, overtime; F, float (use of float or nonpermanent staff).
*References can be found on pages 621–622.
Volume 44, No. 10, October 2018 617
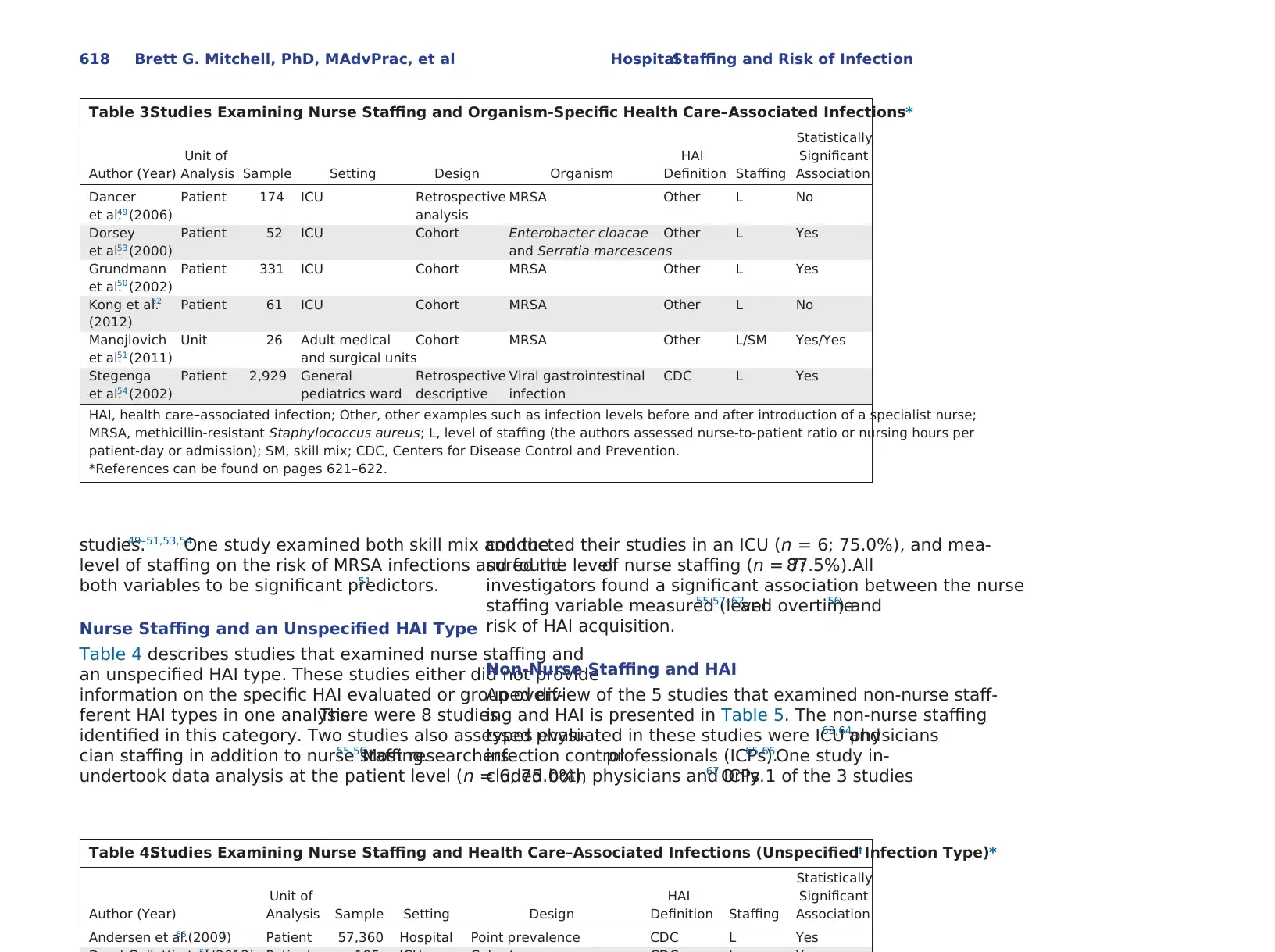
studies.49–51,53,54
One study examined both skill mix and the
level of staffing on the risk of MRSA infections and found
both variables to be significant predictors.51
Nurse Staffing and an Unspecified HAI Type
Table 4 describes studies that examined nurse staffing and
an unspecified HAI type. These studies either did not provide
information on the specific HAI evaluated or grouped dif-
ferent HAI types in one analysis.There were 8 studies
identified in this category. Two studies also assessed physi-
cian staffing in addition to nurse staffing.55,56
Most researchers
undertook data analysis at the patient level (n = 6; 75.0%),
conducted their studies in an ICU (n = 6; 75.0%), and mea-
sured the levelof nurse staffing (n = 7;87.5%).All
investigators found a significant association between the nurse
staffing variable measured (level55,57–62
and overtime56
) and
risk of HAI acquisition.
Non-Nurse Staffing and HAI
An overview of the 5 studies that examined non-nurse staff-
ing and HAI is presented in Table 5. The non-nurse staffing
types evaluated in these studies were ICU physicians63,64
and
infection controlprofessionals (ICPs).65,66One study in-
cluded both physicians and ICPs.67 Only 1 of the 3 studies
Table 3.Studies Examining Nurse Staffing and Organism-Specific Health Care–Associated Infections*
Author (Year)
Unit of
Analysis Sample Setting Design Organism
HAI
Definition Staffing
Statistically
Significant
Association
Dancer
et al.49 (2006)
Patient 174 ICU Retrospective
analysis
MRSA Other L No
Dorsey
et al.53 (2000)
Patient 52 ICU Cohort Enterobacter cloacae
and Serratia marcescens
Other L Yes
Grundmann
et al.50 (2002)
Patient 331 ICU Cohort MRSA Other L Yes
Kong et al.52
(2012)
Patient 61 ICU Cohort MRSA Other L No
Manojlovich
et al.51 (2011)
Unit 26 Adult medical
and surgical units
Cohort MRSA Other L/SM Yes/Yes
Stegenga
et al.54 (2002)
Patient 2,929 General
pediatrics ward
Retrospective
descriptive
Viral gastrointestinal
infection
CDC L Yes
HAI, health care–associated infection; Other, other examples such as infection levels before and after introduction of a specialist nurse;
MRSA, methicillin-resistant Staphylococcus aureus; L, level of staffing (the authors assessed nurse-to-patient ratio or nursing hours per
patient-day or admission); SM, skill mix; CDC, Centers for Disease Control and Prevention.
*References can be found on pages 621–622.
Table 4.Studies Examining Nurse Staffing and Health Care–Associated Infections (Unspecified Infection Type)*†
Author (Year)
Unit of
Analysis Sample Setting Design
HAI
Definition Staffing
Statistically
Significant
Association
Andersen et al.55 (2009)‡ Patient 57,360 Hospital Point prevalence CDC L Yes
618 Brett G. Mitchell, PhD, MAdvPrac, et al HospitalStaffing and Risk of Infection
One study examined both skill mix and the
level of staffing on the risk of MRSA infections and found
both variables to be significant predictors.51
Nurse Staffing and an Unspecified HAI Type
Table 4 describes studies that examined nurse staffing and
an unspecified HAI type. These studies either did not provide
information on the specific HAI evaluated or grouped dif-
ferent HAI types in one analysis.There were 8 studies
identified in this category. Two studies also assessed physi-
cian staffing in addition to nurse staffing.55,56
Most researchers
undertook data analysis at the patient level (n = 6; 75.0%),
conducted their studies in an ICU (n = 6; 75.0%), and mea-
sured the levelof nurse staffing (n = 7;87.5%).All
investigators found a significant association between the nurse
staffing variable measured (level55,57–62
and overtime56
) and
risk of HAI acquisition.
Non-Nurse Staffing and HAI
An overview of the 5 studies that examined non-nurse staff-
ing and HAI is presented in Table 5. The non-nurse staffing
types evaluated in these studies were ICU physicians63,64
and
infection controlprofessionals (ICPs).65,66One study in-
cluded both physicians and ICPs.67 Only 1 of the 3 studies
Table 3.Studies Examining Nurse Staffing and Organism-Specific Health Care–Associated Infections*
Author (Year)
Unit of
Analysis Sample Setting Design Organism
HAI
Definition Staffing
Statistically
Significant
Association
Dancer
et al.49 (2006)
Patient 174 ICU Retrospective
analysis
MRSA Other L No
Dorsey
et al.53 (2000)
Patient 52 ICU Cohort Enterobacter cloacae
and Serratia marcescens
Other L Yes
Grundmann
et al.50 (2002)
Patient 331 ICU Cohort MRSA Other L Yes
Kong et al.52
(2012)
Patient 61 ICU Cohort MRSA Other L No
Manojlovich
et al.51 (2011)
Unit 26 Adult medical
and surgical units
Cohort MRSA Other L/SM Yes/Yes
Stegenga
et al.54 (2002)
Patient 2,929 General
pediatrics ward
Retrospective
descriptive
Viral gastrointestinal
infection
CDC L Yes
HAI, health care–associated infection; Other, other examples such as infection levels before and after introduction of a specialist nurse;
MRSA, methicillin-resistant Staphylococcus aureus; L, level of staffing (the authors assessed nurse-to-patient ratio or nursing hours per
patient-day or admission); SM, skill mix; CDC, Centers for Disease Control and Prevention.
*References can be found on pages 621–622.
Table 4.Studies Examining Nurse Staffing and Health Care–Associated Infections (Unspecified Infection Type)*†
Author (Year)
Unit of
Analysis Sample Setting Design
HAI
Definition Staffing
Statistically
Significant
Association
Andersen et al.55 (2009)‡ Patient 57,360 Hospital Point prevalence CDC L Yes
618 Brett G. Mitchell, PhD, MAdvPrac, et al HospitalStaffing and Risk of Infection
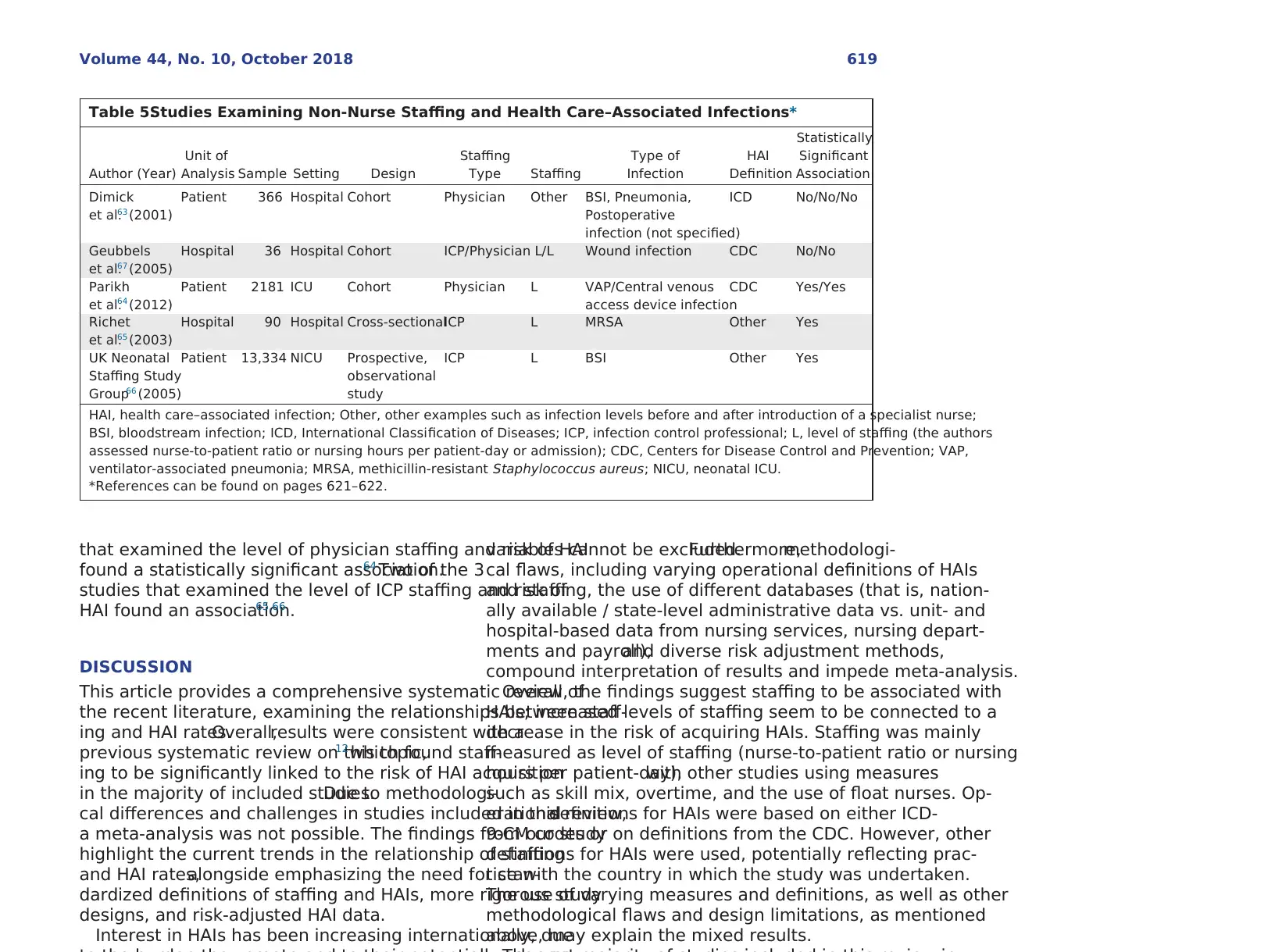
that examined the level of physician staffing and risk of HAI
found a statistically significant association.64 Two of the 3
studies that examined the level of ICP staffing and risk of
HAI found an association.65,66
DISCUSSION
This article provides a comprehensive systematic review of
the recent literature, examining the relationships between staff-
ing and HAI rates.Overall,results were consistent with a
previous systematic review on this topic,12which found staff-
ing to be significantly linked to the risk of HAI acquisition
in the majority of included studies.Due to methodologi-
cal differences and challenges in studies included in this review,
a meta-analysis was not possible. The findings from our study
highlight the current trends in the relationship of staffing
and HAI rates,alongside emphasizing the need for stan-
dardized definitions of staffing and HAIs, more rigorous study
designs, and risk-adjusted HAI data.
Interest in HAIs has been increasing internationally, due
variables cannot be excluded.Furthermore,methodologi-
cal flaws, including varying operational definitions of HAIs
and staffing, the use of different databases (that is, nation-
ally available / state-level administrative data vs. unit- and
hospital-based data from nursing services, nursing depart-
ments and payroll),and diverse risk adjustment methods,
compound interpretation of results and impede meta-analysis.
Overall, the findings suggest staffing to be associated with
HAIs; increased levels of staffing seem to be connected to a
decrease in the risk of acquiring HAIs. Staffing was mainly
measured as level of staffing (nurse-to-patient ratio or nursing
hours per patient-day),with other studies using measures
such as skill mix, overtime, and the use of float nurses. Op-
erationaldefinitions for HAIs were based on either ICD-
9-CM codes or on definitions from the CDC. However, other
definitions for HAIs were used, potentially reflecting prac-
tice with the country in which the study was undertaken.
The use of varying measures and definitions, as well as other
methodological flaws and design limitations, as mentioned
above, may explain the mixed results.
Table 5.Studies Examining Non-Nurse Staffing and Health Care–Associated Infections*
Author (Year)
Unit of
Analysis Sample Setting Design
Staffing
Type Staffing
Type of
Infection
HAI
Definition
Statistically
Significant
Association
Dimick
et al.63 (2001)
Patient 366 Hospital Cohort Physician Other BSI, Pneumonia,
Postoperative
infection (not specified)
ICD No/No/No
Geubbels
et al.67 (2005)
Hospital 36 Hospital Cohort ICP/Physician L/L Wound infection CDC No/No
Parikh
et al.64 (2012)
Patient 2181 ICU Cohort Physician L VAP/Central venous
access device infection
CDC Yes/Yes
Richet
et al.65 (2003)
Hospital 90 Hospital Cross-sectionalICP L MRSA Other Yes
UK Neonatal
Staffing Study
Group66 (2005)
Patient 13,334 NICU Prospective,
observational
study
ICP L BSI Other Yes
HAI, health care–associated infection; Other, other examples such as infection levels before and after introduction of a specialist nurse;
BSI, bloodstream infection; ICD, International Classification of Diseases; ICP, infection control professional; L, level of staffing (the authors
assessed nurse-to-patient ratio or nursing hours per patient-day or admission); CDC, Centers for Disease Control and Prevention; VAP,
ventilator-associated pneumonia; MRSA, methicillin-resistant Staphylococcus aureus; NICU, neonatal ICU.
*References can be found on pages 621–622.
Volume 44, No. 10, October 2018 619
found a statistically significant association.64 Two of the 3
studies that examined the level of ICP staffing and risk of
HAI found an association.65,66
DISCUSSION
This article provides a comprehensive systematic review of
the recent literature, examining the relationships between staff-
ing and HAI rates.Overall,results were consistent with a
previous systematic review on this topic,12which found staff-
ing to be significantly linked to the risk of HAI acquisition
in the majority of included studies.Due to methodologi-
cal differences and challenges in studies included in this review,
a meta-analysis was not possible. The findings from our study
highlight the current trends in the relationship of staffing
and HAI rates,alongside emphasizing the need for stan-
dardized definitions of staffing and HAIs, more rigorous study
designs, and risk-adjusted HAI data.
Interest in HAIs has been increasing internationally, due
variables cannot be excluded.Furthermore,methodologi-
cal flaws, including varying operational definitions of HAIs
and staffing, the use of different databases (that is, nation-
ally available / state-level administrative data vs. unit- and
hospital-based data from nursing services, nursing depart-
ments and payroll),and diverse risk adjustment methods,
compound interpretation of results and impede meta-analysis.
Overall, the findings suggest staffing to be associated with
HAIs; increased levels of staffing seem to be connected to a
decrease in the risk of acquiring HAIs. Staffing was mainly
measured as level of staffing (nurse-to-patient ratio or nursing
hours per patient-day),with other studies using measures
such as skill mix, overtime, and the use of float nurses. Op-
erationaldefinitions for HAIs were based on either ICD-
9-CM codes or on definitions from the CDC. However, other
definitions for HAIs were used, potentially reflecting prac-
tice with the country in which the study was undertaken.
The use of varying measures and definitions, as well as other
methodological flaws and design limitations, as mentioned
above, may explain the mixed results.
Table 5.Studies Examining Non-Nurse Staffing and Health Care–Associated Infections*
Author (Year)
Unit of
Analysis Sample Setting Design
Staffing
Type Staffing
Type of
Infection
HAI
Definition
Statistically
Significant
Association
Dimick
et al.63 (2001)
Patient 366 Hospital Cohort Physician Other BSI, Pneumonia,
Postoperative
infection (not specified)
ICD No/No/No
Geubbels
et al.67 (2005)
Hospital 36 Hospital Cohort ICP/Physician L/L Wound infection CDC No/No
Parikh
et al.64 (2012)
Patient 2181 ICU Cohort Physician L VAP/Central venous
access device infection
CDC Yes/Yes
Richet
et al.65 (2003)
Hospital 90 Hospital Cross-sectionalICP L MRSA Other Yes
UK Neonatal
Staffing Study
Group66 (2005)
Patient 13,334 NICU Prospective,
observational
study
ICP L BSI Other Yes
HAI, health care–associated infection; Other, other examples such as infection levels before and after introduction of a specialist nurse;
BSI, bloodstream infection; ICD, International Classification of Diseases; ICP, infection control professional; L, level of staffing (the authors
assessed nurse-to-patient ratio or nursing hours per patient-day or admission); CDC, Centers for Disease Control and Prevention; VAP,
ventilator-associated pneumonia; MRSA, methicillin-resistant Staphylococcus aureus; NICU, neonatal ICU.
*References can be found on pages 621–622.
Volume 44, No. 10, October 2018 619
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
are consistent with a previous review that also did not iden-
tify a statistically significant link between physician staffing
and HAIs.12 If these results are to be taken at face value, one
explanation may be that nurses constitute the largest pro-
portion of the health care workforce and have considerable
patient contact,11 thus providing an opportunity for in-
creased risk of organism transmission. As such, nurses have
the unique opportunity to directly reduce HAIs through rec-
ognizing and applying evidence-based procedures to prevent
HAIs among patients and protecting the health of the staff.4
In studies that examine the association between nurse staff-
ing and the risk of HAIs, a differentiation between permanent
nurse staffing and nonpermanent (temporary or float) staff-
ing is often made. Consistent with previous findings,12 the
majority of studies in our review suggested that the use of
permanent nurse staff was connected to a decrease in risk
of HAI acquisition.Conversely,the use of nonpermanent
nurse staff was linked to an increase in HAI risk. However,
evidence on the effects of using nonpermanent staff is scarce,
with our study identifying only three studies exploring this
association.5,20,39
To explain this result, it is plausible that non-
permanent nurse staff are less familiar with ward routine and
infection prevention strategies, may lack specific training, and
may not have the same levelof communication with co-
workers due to the inability to form established relationships.12
The importance of clear, interdisciplinary communication
and collaboration among health care professionals has been
highlighted by severalstudies,68–70with poor communica-
tion being named as one of the most common causes for
medical errors (that is, HAIs).68,69
Our review identified a lack of studies exploring the re-
lationship of specialized staff, including ICPs. The CDC’s
Study on the Efficacy ofNosocomialInfection Control
(SENIC), which suggested an adequate staffing ratio of ICPs
to patients,was published more than four decades ago.71
Given the high interest in HAIs and the number of studies
examining staffing and HAIs published in the last decade,
this scarceness of evidence is problematic; however, the chal-
lenges in undertaking a study such as the SENIC Project
cannot be understated. Only three studies included in our
review examined associations between ICPs and HAIs, and
only one study examined the effect of a specialist nurse on
care as the “problem of many hands.”72 Practicalapplica-
tions of this problem have been demonstrated through the
introduction of checklists to improve different groups of health
care professionals’ compliance with infection prevention.73
Future research is needed to establish a body of evidence to
support the tentative link between specialized nurse staff-
ing and ICPs and HAI rates.
Our review has limitations. Non–peer reviewed literature,
reviews, editorials, and commentaries or policy statements
and articles were excluded to maintain rigour and consistency
of the study. Publications in a language other than English
were also excluded. As such, evidence from such research was
not included.Further,no meta-analysis,and therefore as-
sessment of publication bias,was undertaken due to the
methodological limitations of the included studies. A further
challenge in exploring this topic is understanding a hospital’s
investment areas such as infrastructure,personnel,and
activities aimed at promoting quality. These are potential con-
founders that are not easily controlled or quantified,as
evidenced by the risk of bias assessment. With the trend of
shorter lengths of stay,patients have increased acuity and
may need a higher level of care; however, in this review we
were not able to examine staffing ratios adjusted for patient
acuity.74
CONCLUSION
Despite the data being observational, there is a growing and
updated evidence base demonstrating the relationship between
staffing characteristics and HAIs. The findings support ad-
vocacy for effective use of staffing resources and will inform
health care managers and professional organizations on future
changes to hospital staffing, as they relate to infection pre-
vention. Considerable variability in the study design, methods,
and definitions used to examine staffing and the risk of HAIs
exist in the literature. This highlights the need to move to
uniform operational definitions of staffing and HAIs in future
studies that explore this area.
Funding.This project was supported by an externalcompetitive grant
(Covidien)and scholarship awarded by Avondale College of Higher Ed-
ucation. Funders played no role in any element of this research.
Conflicts of Interest. One of the authors [P.W.S.]was a lead author on
620 Brett G. Mitchell, PhD, MAdvPrac, et al HospitalStaffing and Risk of Infection
tify a statistically significant link between physician staffing
and HAIs.12 If these results are to be taken at face value, one
explanation may be that nurses constitute the largest pro-
portion of the health care workforce and have considerable
patient contact,11 thus providing an opportunity for in-
creased risk of organism transmission. As such, nurses have
the unique opportunity to directly reduce HAIs through rec-
ognizing and applying evidence-based procedures to prevent
HAIs among patients and protecting the health of the staff.4
In studies that examine the association between nurse staff-
ing and the risk of HAIs, a differentiation between permanent
nurse staffing and nonpermanent (temporary or float) staff-
ing is often made. Consistent with previous findings,12 the
majority of studies in our review suggested that the use of
permanent nurse staff was connected to a decrease in risk
of HAI acquisition.Conversely,the use of nonpermanent
nurse staff was linked to an increase in HAI risk. However,
evidence on the effects of using nonpermanent staff is scarce,
with our study identifying only three studies exploring this
association.5,20,39
To explain this result, it is plausible that non-
permanent nurse staff are less familiar with ward routine and
infection prevention strategies, may lack specific training, and
may not have the same levelof communication with co-
workers due to the inability to form established relationships.12
The importance of clear, interdisciplinary communication
and collaboration among health care professionals has been
highlighted by severalstudies,68–70with poor communica-
tion being named as one of the most common causes for
medical errors (that is, HAIs).68,69
Our review identified a lack of studies exploring the re-
lationship of specialized staff, including ICPs. The CDC’s
Study on the Efficacy ofNosocomialInfection Control
(SENIC), which suggested an adequate staffing ratio of ICPs
to patients,was published more than four decades ago.71
Given the high interest in HAIs and the number of studies
examining staffing and HAIs published in the last decade,
this scarceness of evidence is problematic; however, the chal-
lenges in undertaking a study such as the SENIC Project
cannot be understated. Only three studies included in our
review examined associations between ICPs and HAIs, and
only one study examined the effect of a specialist nurse on
care as the “problem of many hands.”72 Practicalapplica-
tions of this problem have been demonstrated through the
introduction of checklists to improve different groups of health
care professionals’ compliance with infection prevention.73
Future research is needed to establish a body of evidence to
support the tentative link between specialized nurse staff-
ing and ICPs and HAI rates.
Our review has limitations. Non–peer reviewed literature,
reviews, editorials, and commentaries or policy statements
and articles were excluded to maintain rigour and consistency
of the study. Publications in a language other than English
were also excluded. As such, evidence from such research was
not included.Further,no meta-analysis,and therefore as-
sessment of publication bias,was undertaken due to the
methodological limitations of the included studies. A further
challenge in exploring this topic is understanding a hospital’s
investment areas such as infrastructure,personnel,and
activities aimed at promoting quality. These are potential con-
founders that are not easily controlled or quantified,as
evidenced by the risk of bias assessment. With the trend of
shorter lengths of stay,patients have increased acuity and
may need a higher level of care; however, in this review we
were not able to examine staffing ratios adjusted for patient
acuity.74
CONCLUSION
Despite the data being observational, there is a growing and
updated evidence base demonstrating the relationship between
staffing characteristics and HAIs. The findings support ad-
vocacy for effective use of staffing resources and will inform
health care managers and professional organizations on future
changes to hospital staffing, as they relate to infection pre-
vention. Considerable variability in the study design, methods,
and definitions used to examine staffing and the risk of HAIs
exist in the literature. This highlights the need to move to
uniform operational definitions of staffing and HAIs in future
studies that explore this area.
Funding.This project was supported by an externalcompetitive grant
(Covidien)and scholarship awarded by Avondale College of Higher Ed-
ucation. Funders played no role in any element of this research.
Conflicts of Interest. One of the authors [P.W.S.]was a lead author on
620 Brett G. Mitchell, PhD, MAdvPrac, et al HospitalStaffing and Risk of Infection
ONLINE-ONLY CONTENT
See the online version of this article for Appendix 1 Char-
acteristics of Studies Included in the Systematic Review.
Appendix 2 Risk of Bias Assessment in the Studies in the
Systematic Review.
REFERENCES
1. Allegranzi B, et al. Burden of endemic health-care-associated
infection in developing countries:systematic review and
meta-analysis. Lancet. 2011 Jan 15;377:228–241.
2. Magill SS, et al. Multistate point-prevalence survey of health
care–associated infections.N Engl J Med. 2014 Mar
27;370:1198–1208.
3. Cassini A, et al. Burden of six healthcare-associated infections
on European population health: estimating incidence-based
disability-adjusted life years through a population
prevalence-based modelling study.PLoS Med. 2016 Oct
18;13:e1002150.
4. Collins AS. Preventing health care–associated infections. In:
Hughes RG, editor. Patient Safety and Quality: An Evidence-
Based Handbook for Nurses.Rockville,MD: Agency for
Healthcare Research and Quality,2008 Accessed Apr 26,
2018. https://www.ncbi.nlm.nih.gov/books/NBK2683/.
5. Alonso-Echanove J, et al. Effect of nurse staffing and
antimicrobial-impregnated central venous catheters on the
risk for bloodstream infections in intensive care units. Infect
Control Hosp Epidemiol. 2003;24:916–925.
6. Jackson M, et al. Nurse staffing and health care–associated
infections: proceedings from a working group meeting. Am
J Infect Control. 2002;30:199–206.
7. Needleman J, et al. Nurse-staffing levels and the quality of
care in hospitals. N Engl J Med. 2002 May 30;346:1715–1722.
8. Aiken LH,et al.Educationallevels of hospitalnurses and
surgical patient mortality. JAMA. 2003 Sep 24;290:1617–1623.
9. Hugonnet S, et al. Nursing resources: a major determinant
of nosocomial infection? Curr Opin Infect Dis. 2004;17:329–
333.
10. Mark BA, Harless DW.Nurse staffing and post-surgical
complications using the present on admission indicator. Res
Nurs Health. 2010;33:35–47.
11. Shang J, Stone P, Larson E. Studies on nurse staffing and
health care–associated infection: methodologic challenges
and potential solutions. Am J Infect Control. 2015;43:581–588.
12. Stone PW, et al. Hospital staffing and health care–associated
infections: a systematic review of the literature. Clin Infect
Dis. 2008 Oct 1;47:937–944.
13. Dettenkofer M, et al. Infection control—a European research
18. Fraher MH,et al.Cost-effectiveness of employing a total
parenteral nutrition surveillance nurse for the prevention of
catheter-related bloodstream infections.J Hosp Infect.
2009;73:129–134.
19. Pronovost PJ, et al. Intensive care unit nurse staffing and the
risk for complications after abdominal aortic surgery. Eff Clin
Pract. 2001;4:199–206.
20. Robert J, et al. The influence ofthe composition ofthe
nursing staff on primary bloodstream infection rates in a
surgical intensive care unit. Infect Control Hosp Epidemiol.
2000;21:12–17.
21. Tucker J, UK Neonatal Staffing Study Group. Patient volume,
staffing, and workload in relation to risk-adjusted outcomes
in a random stratified sample of UK neonatal intensive care
units: a prospective evaluation. Lancet. 2002 Jan 12;359:99–
107.
22. Whitman GR, et al. The impact of staffing on patient
outcomes across specialty units. J Nurs Adm. 2002;32:633–
639.
23. Sujijantararat R, Booth RZ, Davis LL. Nosocomial urinary tract
infection: nursing-sensitive quality indicator in a Thai hospital.
J Nurs Care Qual. 2005;20:134–139.
24. Hugonnet S, Uçkay I, Pittet D. Staffing level: a determinant
of late-onset ventilator-associated pneumonia.Crit Care.
2007;11(4):R80.
25. Berney B,Needleman J. Impact ofnursing overtime on
nurse-sensitive patient outcomes in New York hospitals,
1995–2000. Policy Polit Nurs Pract. 2006;7:87–100.
26. Cimiotti JP, et al. Nurse staffing, burnout, and health care–
associated infection. Am J Infect Control. 2012;40:486–490.
Erratum in: Am J Infect Control. 2012;40:680.
27. Kelly D, et al. The critical care work environment and nurse-
reported health care–associated infections. Am J Crit Care.
2013;22:482–488.
28. Kovner C,et al. Nurse staffing and postsurgicaladverse
events: an analysis of administrative data from a sample of
U.S. hospitals,1990–1996.Health Serv Res.2002;37:611–
629.
29. Mark BA, Harless DW,Berman WF.Nurse staffing and
adverse events in hospitalized children.Policy Polit Nurs
Pract. 2007;8:83–92.
30. Mark BA, et al. A longitudinal examination ofhospital
registered nurse staffing and quality of care. Health Serv Res.
2004;39:279–300. Erratum in: Health Serv Res. 2004;39:1629.
31. Needleman J, et al. Measuring hospital quality: can Medicare
data substitute for all-payer data? Health Serv Res.
2003;38:1487–1508.
32. Twigg D, et al. The impact of the nursing hours per patient
day (NHPPD) staffing method on patient outcomes:
a retrospective analysis of patient and staffing data. Int J Nurs
Volume 44, No. 10, October 2018 621
See the online version of this article for Appendix 1 Char-
acteristics of Studies Included in the Systematic Review.
Appendix 2 Risk of Bias Assessment in the Studies in the
Systematic Review.
REFERENCES
1. Allegranzi B, et al. Burden of endemic health-care-associated
infection in developing countries:systematic review and
meta-analysis. Lancet. 2011 Jan 15;377:228–241.
2. Magill SS, et al. Multistate point-prevalence survey of health
care–associated infections.N Engl J Med. 2014 Mar
27;370:1198–1208.
3. Cassini A, et al. Burden of six healthcare-associated infections
on European population health: estimating incidence-based
disability-adjusted life years through a population
prevalence-based modelling study.PLoS Med. 2016 Oct
18;13:e1002150.
4. Collins AS. Preventing health care–associated infections. In:
Hughes RG, editor. Patient Safety and Quality: An Evidence-
Based Handbook for Nurses.Rockville,MD: Agency for
Healthcare Research and Quality,2008 Accessed Apr 26,
2018. https://www.ncbi.nlm.nih.gov/books/NBK2683/.
5. Alonso-Echanove J, et al. Effect of nurse staffing and
antimicrobial-impregnated central venous catheters on the
risk for bloodstream infections in intensive care units. Infect
Control Hosp Epidemiol. 2003;24:916–925.
6. Jackson M, et al. Nurse staffing and health care–associated
infections: proceedings from a working group meeting. Am
J Infect Control. 2002;30:199–206.
7. Needleman J, et al. Nurse-staffing levels and the quality of
care in hospitals. N Engl J Med. 2002 May 30;346:1715–1722.
8. Aiken LH,et al.Educationallevels of hospitalnurses and
surgical patient mortality. JAMA. 2003 Sep 24;290:1617–1623.
9. Hugonnet S, et al. Nursing resources: a major determinant
of nosocomial infection? Curr Opin Infect Dis. 2004;17:329–
333.
10. Mark BA, Harless DW.Nurse staffing and post-surgical
complications using the present on admission indicator. Res
Nurs Health. 2010;33:35–47.
11. Shang J, Stone P, Larson E. Studies on nurse staffing and
health care–associated infection: methodologic challenges
and potential solutions. Am J Infect Control. 2015;43:581–588.
12. Stone PW, et al. Hospital staffing and health care–associated
infections: a systematic review of the literature. Clin Infect
Dis. 2008 Oct 1;47:937–944.
13. Dettenkofer M, et al. Infection control—a European research
18. Fraher MH,et al.Cost-effectiveness of employing a total
parenteral nutrition surveillance nurse for the prevention of
catheter-related bloodstream infections.J Hosp Infect.
2009;73:129–134.
19. Pronovost PJ, et al. Intensive care unit nurse staffing and the
risk for complications after abdominal aortic surgery. Eff Clin
Pract. 2001;4:199–206.
20. Robert J, et al. The influence ofthe composition ofthe
nursing staff on primary bloodstream infection rates in a
surgical intensive care unit. Infect Control Hosp Epidemiol.
2000;21:12–17.
21. Tucker J, UK Neonatal Staffing Study Group. Patient volume,
staffing, and workload in relation to risk-adjusted outcomes
in a random stratified sample of UK neonatal intensive care
units: a prospective evaluation. Lancet. 2002 Jan 12;359:99–
107.
22. Whitman GR, et al. The impact of staffing on patient
outcomes across specialty units. J Nurs Adm. 2002;32:633–
639.
23. Sujijantararat R, Booth RZ, Davis LL. Nosocomial urinary tract
infection: nursing-sensitive quality indicator in a Thai hospital.
J Nurs Care Qual. 2005;20:134–139.
24. Hugonnet S, Uçkay I, Pittet D. Staffing level: a determinant
of late-onset ventilator-associated pneumonia.Crit Care.
2007;11(4):R80.
25. Berney B,Needleman J. Impact ofnursing overtime on
nurse-sensitive patient outcomes in New York hospitals,
1995–2000. Policy Polit Nurs Pract. 2006;7:87–100.
26. Cimiotti JP, et al. Nurse staffing, burnout, and health care–
associated infection. Am J Infect Control. 2012;40:486–490.
Erratum in: Am J Infect Control. 2012;40:680.
27. Kelly D, et al. The critical care work environment and nurse-
reported health care–associated infections. Am J Crit Care.
2013;22:482–488.
28. Kovner C,et al. Nurse staffing and postsurgicaladverse
events: an analysis of administrative data from a sample of
U.S. hospitals,1990–1996.Health Serv Res.2002;37:611–
629.
29. Mark BA, Harless DW,Berman WF.Nurse staffing and
adverse events in hospitalized children.Policy Polit Nurs
Pract. 2007;8:83–92.
30. Mark BA, et al. A longitudinal examination ofhospital
registered nurse staffing and quality of care. Health Serv Res.
2004;39:279–300. Erratum in: Health Serv Res. 2004;39:1629.
31. Needleman J, et al. Measuring hospital quality: can Medicare
data substitute for all-payer data? Health Serv Res.
2003;38:1487–1508.
32. Twigg D, et al. The impact of the nursing hours per patient
day (NHPPD) staffing method on patient outcomes:
a retrospective analysis of patient and staffing data. Int J Nurs
Volume 44, No. 10, October 2018 621
38. Stone PW, et al. Nurse working conditions and patient safety
outcomes. Med Care. 2007;45:571–578.
39. Stratton KM.Pediatric nurse staffing and quality ofcare
in the hospitalsetting.J Nurs Care Qual. 2008;23:105–
114.
40. Yang KP. Relationships between nurse staffing and patient
outcomes. J Nurs Res. 2003;11:149–158.
41. Schwab F, et al. Understaffing, overcrowding, inappropriate
nurse:ventilated patient ratio and nosocomialinfections:
which parameter is the best reflection of deficits? J Hosp
Infect. 2012;80:133–139.
42. Amaravadi RK, et al. ICU nurse-to-patient ratio is associated
with complications and resource use after esophagectomy.
Intensive Care Med. 2000;26:1857–1862.
43. Barkell NP, Killinger KA, Schultz SD. The relationship between
nurse staffing models and patient outcomes: a descriptive
study. Outcomes Manag. 2002;6:27–33.
44. Dimick JB, et al. Effect of nurse-to-patient ratio in the
intensive care unit on pulmonary complications and resource
use after hepatectomy. Am J Crit Care. 2001;10:376–382.
45. Glance LG, et al. The association between nurse staffing and
hospital outcomes in injured patients. BMC Health Serv Res.
2012 Aug 9;12:247.
46. McGillis HallL, Doran D,Pink GH.Nurse staffing models,
nursing hours,and patient safety outcomes.J Nurs Adm.
2004;34:41–45.
47. Pappas S,et al.Risk-adjusted staffing to improve patient
value. Nurs Econ. 2015;33:73–78, 87.
48. Yang PH,et al. The impact ofdifferent nursing skillmix
models on patient outcomes in a respiratory care center.
Worldviews Evid Based Nurs. 2012;9:227–233.
49. Dancer SJ, et al. MRSA acquisition in an intensive care unit.
Am J Infect Control. 2006;34:10–17.
50. Grundmann H,et al. Risk factors for the transmission of
methicillin-resistant Staphylococcus aureus in an adult
intensive care unit: fitting a model to the data. J Infect Dis.
2002 Feb 15;185:481–488.
51. Manojlovich M, et al. Nurse dose: linking staffing variables
to adverse patient outcomes. Nurs Res. 2011;60:214–
220.
52. Kong F, et al. Do staffing and workload levels influence the
risk of new acquisitions of meticillin-resistant Staphylococcus
aureus in a well-resourced intensive care unit? J Hosp Infect.
2012;80:331–339.
53. Dorsey G, et al. A heterogeneous outbreak of Enterobacter
cloacae and Serratia marcescens infections in a surgical
intensive care unit. Infect Control Hosp Epidemiol.
2000;21:465–469.
54. Stegenga J, Bell E, Matlow A. The role of nurse understaffing
in nosocomial viral gastrointestinal infections on a general
57. Daud-GallottiRM, et al.Nursing workload as a risk factor
for healthcare associated infections in ICU:a prospective
study. PLoS ONE. 2012;7:e52342.
58. Halwani M, et al. Cross-transmission of nosocomial
pathogens in an adult intensive care unit: incidence and risk
factors. J Hosp Infect. 2006;63:39–46.
59. Maillet JM, et al. Comparison of intensive-care-unit-acquired
infections and their outcomes among patients over and
under 80 years of age. J Hosp Infect. 2014;87:152–158.
60. Rogowski JA, et al. Nurse staffing and NICU infection rates.
JAMA Pediatr. 2013;167:444–450.
61. Hugonnet S, Chevrolet JC, Pittet D. The effect of workload
on infection risk in critically illpatients.Crit Care Med.
2007;35:76–81.
62. Hugonnet S, Villaveces A, Pittet D. Nurse staffing level and
nosocomialinfections:empiricalevaluation ofthe case-
crossover and case-time-control designs. Am J Epidemiol.
2007 Jun 1;165:1321–1327.
63. Dimick JB, et al. Intensive care unit physician staffing is
associated with decreased length of stay, hospital cost, and
complications after esophagealresection.Crit Care Med.
2001;29:753–758.
64. Parikh A, et al. Quality improvement and cost savings after
implementation of the Leapfrog intensive care unit physician
staffing standard at a community teaching hospital. Crit Care
Med. 2012;40:2754–2759.
65. Richet HM, et al. Are there regional variations in the
diagnosis,surveillance,and controlof methicillin-resistant
Staphylococcus aureus? Infect ControlHosp Epidemiol.
2003;24:334–341.
66. UK NeonatalStaffing Study Group.Relationship between
probable nosocomialbacteraemia and organisationaland
structuralfactors in UK neonatalintensive care units. Qual
Saf Health Care. 2005;14:264–269.
67. Geubbels EL, et al. Hospital-related determinants for
surgical-site infection following hip arthroplasty.Infect
Control Hosp Epidemiol. 2005;26:435–441.
68. Tschannen D, et al. Implications of nurse-physician relations:
report of a successful intervention. Nurs Econ. 2011;29:127–
135.
69. Siegele P. Enhancing outcomes in a surgical intensive care
unit by implementing daily goals tools.Crit Care Nurse.
2009;29:58–69.
70. Lancaster G,et al. Interdisciplinary communication and
collaboration among physicians,nurses,and unlicensed
assistive personnel. J Nurs Scholarsh. 2015;47:275–284.
71. Haley RW, et al. The SENIC Project. Study on the efficacy
of nosocomialinfection control(SENIC Project).Summary
of study design. Am J Epidemiol. 1980;111:472–485.
72. Dixon-Woods M, Pronovost PJ. Patient safety and the
622 Brett G. Mitchell, PhD, MAdvPrac, et al HospitalStaffing and Risk of Infection
outcomes. Med Care. 2007;45:571–578.
39. Stratton KM.Pediatric nurse staffing and quality ofcare
in the hospitalsetting.J Nurs Care Qual. 2008;23:105–
114.
40. Yang KP. Relationships between nurse staffing and patient
outcomes. J Nurs Res. 2003;11:149–158.
41. Schwab F, et al. Understaffing, overcrowding, inappropriate
nurse:ventilated patient ratio and nosocomialinfections:
which parameter is the best reflection of deficits? J Hosp
Infect. 2012;80:133–139.
42. Amaravadi RK, et al. ICU nurse-to-patient ratio is associated
with complications and resource use after esophagectomy.
Intensive Care Med. 2000;26:1857–1862.
43. Barkell NP, Killinger KA, Schultz SD. The relationship between
nurse staffing models and patient outcomes: a descriptive
study. Outcomes Manag. 2002;6:27–33.
44. Dimick JB, et al. Effect of nurse-to-patient ratio in the
intensive care unit on pulmonary complications and resource
use after hepatectomy. Am J Crit Care. 2001;10:376–382.
45. Glance LG, et al. The association between nurse staffing and
hospital outcomes in injured patients. BMC Health Serv Res.
2012 Aug 9;12:247.
46. McGillis HallL, Doran D,Pink GH.Nurse staffing models,
nursing hours,and patient safety outcomes.J Nurs Adm.
2004;34:41–45.
47. Pappas S,et al.Risk-adjusted staffing to improve patient
value. Nurs Econ. 2015;33:73–78, 87.
48. Yang PH,et al. The impact ofdifferent nursing skillmix
models on patient outcomes in a respiratory care center.
Worldviews Evid Based Nurs. 2012;9:227–233.
49. Dancer SJ, et al. MRSA acquisition in an intensive care unit.
Am J Infect Control. 2006;34:10–17.
50. Grundmann H,et al. Risk factors for the transmission of
methicillin-resistant Staphylococcus aureus in an adult
intensive care unit: fitting a model to the data. J Infect Dis.
2002 Feb 15;185:481–488.
51. Manojlovich M, et al. Nurse dose: linking staffing variables
to adverse patient outcomes. Nurs Res. 2011;60:214–
220.
52. Kong F, et al. Do staffing and workload levels influence the
risk of new acquisitions of meticillin-resistant Staphylococcus
aureus in a well-resourced intensive care unit? J Hosp Infect.
2012;80:331–339.
53. Dorsey G, et al. A heterogeneous outbreak of Enterobacter
cloacae and Serratia marcescens infections in a surgical
intensive care unit. Infect Control Hosp Epidemiol.
2000;21:465–469.
54. Stegenga J, Bell E, Matlow A. The role of nurse understaffing
in nosocomial viral gastrointestinal infections on a general
57. Daud-GallottiRM, et al.Nursing workload as a risk factor
for healthcare associated infections in ICU:a prospective
study. PLoS ONE. 2012;7:e52342.
58. Halwani M, et al. Cross-transmission of nosocomial
pathogens in an adult intensive care unit: incidence and risk
factors. J Hosp Infect. 2006;63:39–46.
59. Maillet JM, et al. Comparison of intensive-care-unit-acquired
infections and their outcomes among patients over and
under 80 years of age. J Hosp Infect. 2014;87:152–158.
60. Rogowski JA, et al. Nurse staffing and NICU infection rates.
JAMA Pediatr. 2013;167:444–450.
61. Hugonnet S, Chevrolet JC, Pittet D. The effect of workload
on infection risk in critically illpatients.Crit Care Med.
2007;35:76–81.
62. Hugonnet S, Villaveces A, Pittet D. Nurse staffing level and
nosocomialinfections:empiricalevaluation ofthe case-
crossover and case-time-control designs. Am J Epidemiol.
2007 Jun 1;165:1321–1327.
63. Dimick JB, et al. Intensive care unit physician staffing is
associated with decreased length of stay, hospital cost, and
complications after esophagealresection.Crit Care Med.
2001;29:753–758.
64. Parikh A, et al. Quality improvement and cost savings after
implementation of the Leapfrog intensive care unit physician
staffing standard at a community teaching hospital. Crit Care
Med. 2012;40:2754–2759.
65. Richet HM, et al. Are there regional variations in the
diagnosis,surveillance,and controlof methicillin-resistant
Staphylococcus aureus? Infect ControlHosp Epidemiol.
2003;24:334–341.
66. UK NeonatalStaffing Study Group.Relationship between
probable nosocomialbacteraemia and organisationaland
structuralfactors in UK neonatalintensive care units. Qual
Saf Health Care. 2005;14:264–269.
67. Geubbels EL, et al. Hospital-related determinants for
surgical-site infection following hip arthroplasty.Infect
Control Hosp Epidemiol. 2005;26:435–441.
68. Tschannen D, et al. Implications of nurse-physician relations:
report of a successful intervention. Nurs Econ. 2011;29:127–
135.
69. Siegele P. Enhancing outcomes in a surgical intensive care
unit by implementing daily goals tools.Crit Care Nurse.
2009;29:58–69.
70. Lancaster G,et al. Interdisciplinary communication and
collaboration among physicians,nurses,and unlicensed
assistive personnel. J Nurs Scholarsh. 2015;47:275–284.
71. Haley RW, et al. The SENIC Project. Study on the efficacy
of nosocomialinfection control(SENIC Project).Summary
of study design. Am J Epidemiol. 1980;111:472–485.
72. Dixon-Woods M, Pronovost PJ. Patient safety and the
622 Brett G. Mitchell, PhD, MAdvPrac, et al HospitalStaffing and Risk of Infection
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





