Prevalence and Causes of Vision Loss in Indigenous and Non-Indigenous Australians
VerifiedAdded on 2022/11/14
|10
|10105
|451
AI Summary
The National Eye Health Survey conducted a nationwide, cross-sectional, population-based survey to determine the prevalence and causes of vision loss in Indigenous and non-Indigenous Australians. The study found that vision loss is more prevalent in Indigenous Australians than in non-Indigenous Australians, with uncorrected refractive error and cataract being the leading causes. Risk factors for vision loss were also identified.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
The Prevalence and Causes of Vision Loss in
Indigenous and Non-Indigenous Australians
The NationalEye Health Survey
Joshua Foreman, BSc (Hons),1,2 Jing Xie, PhD,1 Stuart Keel, PhD,1 Peter van Wijngaarden, FRANZCO,1,2
SukhpalSingh Sandhu, FRANZCO,1,2 Ghee Soon Ang, FRANZCO,1 Jennifer Fan Gaskin, FRANZCO,1
Jonathan Crowston, FRANZCO,1,2 Rupert Bourne, FRCOphth,3 Hugh R. Taylor, AC,4 Mohamed Dirani, PhD1,2
Purpose: To conduct a nationwide survey on the prevalence and causes of vision loss in Indigenous and
non-Indigenous Australians.
Design: Nationwide, cross-sectional, population-based survey.
Participants: Indigenous Australians aged 40 years or older and non-Indigenous Australians aged 50 year
and older.
Methods: Multistage random-clustersampling was used to select3098 non-Indigenous Australians and
1738 Indigenous Australians from 30 sites across 5 remoteness strata (response rate of71.5%).Sociodemo-
graphic and health data were collected using an interviewer-administered questionnaire.Trained examiners
conducted standardized eye examinations,including visualacuity,perimetry,slit-lamp examination, intraocular
pressure,and fundus photography.The prevalence and main causes ofbilateralpresenting vision loss (visual
acuity <6/12 in the better eye)were determined, and risk factors were identified.
Main Outcome Measures: Prevalence and main causes of vision loss.
Results: The overallprevalence of vision loss in Australia was 6.6% (95% confidence interval[CI], 5.4e7.8).
The prevalence ofvision loss was 11.2% (95% CI,9.5e13.1)in Indigenous Australians and 6.5% (95% CI,
5.3e7.9) in non-Indigenous Australians. Vision loss was 2.8 times more prevalent in Indigenous Australians th
in non-Indigenous Australians after age and gender adjustment (17.7%, 95% CI, 14.5 e21.0 vs. 6.4%, 95% CI
5.2e7.6, P < 0.001). In non-Indigenous Australians, the leading causes of vision loss were uncorrected refrac
error (61.3%),cataract (13.2%),and age-related macular degeneration (10.3%).In Indigenous Australians,the
leading causes of vision loss were uncorrected refractive error (60.8%), cataract (20.1%), and diabetic retino
(5.2%). In non-Indigenous Australians, increasing age (odds ratio [OR], 1.72 per decade)and having not had an
eye examination within the pastyear (OR, 1.61)were risk factors forvision loss.Risk factors in Indigenous
Australians included older age (OR,1.61 per decade),remoteness (OR,2.02),gender (OR,0.60 for men),and
diabetes in combination with never having had an eye examination (OR, 14.47).
Conclusions: Vision loss is more prevalentin Indigenous Australians than in non-Indigenous Australians,
highlighting that improvements in eye healthcare in Indigenous communities are required. The leading caus
vision loss were uncorrected refractive errorand cataract,which are readily treatable.Other countries with
Indigenous communities may benefitfrom conducting similarsurveys of Indigenous and non-Indigenous
populations. Ophthalmology 2017;- :1e10 ª 2017 by the American Academy of Ophthalmology
Globally,approximately 223million peopleexperience
vision loss,1 in whom 80% of cases are avoidable through
early detection,prevention,and treatment.2 The feasibility
of reducing the burden of vision loss prompted the World
Health Assemblyto endorse“UniversalEye Health:
A Global Action Plan 2014e2019”(theGlobalAction
Plan)in 2013,which aimed to reduce the prevalence of
avoidable blindnessby 25% before the year2020.3 The
World Health Assembly emphasizedthe need for
population-based survey data on the prevalence and causes
of vision loss to inform resourceallocationfor eye
healthcare services to achieve the objectives of the Glob
Action Plan.3
Less than 20% of countries have conducted nationwide
surveys on the prevalence and causes ofvision loss,and
existing studies vary in terms of methodologicalrigor.2 In
this article,we contend thatthe methodsused in most
surveysto date are limited in theirability to provide a
sufficientlydetailedmap of a nation’seye health,
particularly in countrieswith disadvantaged Indigenous
groups.The definition ofindigeneity iscontentiousand
varies considerably;however, the United Nations
1ª 2017 by the American Academy of Ophthalmology
Published by Elsevier Inc.
http://dx.doi.org/10.1016/j.ophtha.2017.06.001
ISSN 0161-6420/17
Indigenous and Non-Indigenous Australians
The NationalEye Health Survey
Joshua Foreman, BSc (Hons),1,2 Jing Xie, PhD,1 Stuart Keel, PhD,1 Peter van Wijngaarden, FRANZCO,1,2
SukhpalSingh Sandhu, FRANZCO,1,2 Ghee Soon Ang, FRANZCO,1 Jennifer Fan Gaskin, FRANZCO,1
Jonathan Crowston, FRANZCO,1,2 Rupert Bourne, FRCOphth,3 Hugh R. Taylor, AC,4 Mohamed Dirani, PhD1,2
Purpose: To conduct a nationwide survey on the prevalence and causes of vision loss in Indigenous and
non-Indigenous Australians.
Design: Nationwide, cross-sectional, population-based survey.
Participants: Indigenous Australians aged 40 years or older and non-Indigenous Australians aged 50 year
and older.
Methods: Multistage random-clustersampling was used to select3098 non-Indigenous Australians and
1738 Indigenous Australians from 30 sites across 5 remoteness strata (response rate of71.5%).Sociodemo-
graphic and health data were collected using an interviewer-administered questionnaire.Trained examiners
conducted standardized eye examinations,including visualacuity,perimetry,slit-lamp examination, intraocular
pressure,and fundus photography.The prevalence and main causes ofbilateralpresenting vision loss (visual
acuity <6/12 in the better eye)were determined, and risk factors were identified.
Main Outcome Measures: Prevalence and main causes of vision loss.
Results: The overallprevalence of vision loss in Australia was 6.6% (95% confidence interval[CI], 5.4e7.8).
The prevalence ofvision loss was 11.2% (95% CI,9.5e13.1)in Indigenous Australians and 6.5% (95% CI,
5.3e7.9) in non-Indigenous Australians. Vision loss was 2.8 times more prevalent in Indigenous Australians th
in non-Indigenous Australians after age and gender adjustment (17.7%, 95% CI, 14.5 e21.0 vs. 6.4%, 95% CI
5.2e7.6, P < 0.001). In non-Indigenous Australians, the leading causes of vision loss were uncorrected refrac
error (61.3%),cataract (13.2%),and age-related macular degeneration (10.3%).In Indigenous Australians,the
leading causes of vision loss were uncorrected refractive error (60.8%), cataract (20.1%), and diabetic retino
(5.2%). In non-Indigenous Australians, increasing age (odds ratio [OR], 1.72 per decade)and having not had an
eye examination within the pastyear (OR, 1.61)were risk factors forvision loss.Risk factors in Indigenous
Australians included older age (OR,1.61 per decade),remoteness (OR,2.02),gender (OR,0.60 for men),and
diabetes in combination with never having had an eye examination (OR, 14.47).
Conclusions: Vision loss is more prevalentin Indigenous Australians than in non-Indigenous Australians,
highlighting that improvements in eye healthcare in Indigenous communities are required. The leading caus
vision loss were uncorrected refractive errorand cataract,which are readily treatable.Other countries with
Indigenous communities may benefitfrom conducting similarsurveys of Indigenous and non-Indigenous
populations. Ophthalmology 2017;- :1e10 ª 2017 by the American Academy of Ophthalmology
Globally,approximately 223million peopleexperience
vision loss,1 in whom 80% of cases are avoidable through
early detection,prevention,and treatment.2 The feasibility
of reducing the burden of vision loss prompted the World
Health Assemblyto endorse“UniversalEye Health:
A Global Action Plan 2014e2019”(theGlobalAction
Plan)in 2013,which aimed to reduce the prevalence of
avoidable blindnessby 25% before the year2020.3 The
World Health Assembly emphasizedthe need for
population-based survey data on the prevalence and causes
of vision loss to inform resourceallocationfor eye
healthcare services to achieve the objectives of the Glob
Action Plan.3
Less than 20% of countries have conducted nationwide
surveys on the prevalence and causes ofvision loss,and
existing studies vary in terms of methodologicalrigor.2 In
this article,we contend thatthe methodsused in most
surveysto date are limited in theirability to provide a
sufficientlydetailedmap of a nation’seye health,
particularly in countrieswith disadvantaged Indigenous
groups.The definition ofindigeneity iscontentiousand
varies considerably;however, the United Nations
1ª 2017 by the American Academy of Ophthalmology
Published by Elsevier Inc.
http://dx.doi.org/10.1016/j.ophtha.2017.06.001
ISSN 0161-6420/17
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
PermanentForum on IndigenousIssuesloosely defines
Indigenous peoples on the basis ofthe following criteria:
(1) self-identification as Indigenous peoples by individuals
and acceptance as such by their community;(2) historical
continuity and land occupation before invasion and coloni-
zation; (3) strong links to territories including land and water
and related natural resources; (4) distinct social, economic, or
politicalsystems;(5) distinctlanguage,culture,religion,
ceremonies, and beliefs; (6) tendency to form nondominant
groups of society; (7) resolution to maintain and reproduce
ancestral environments and systems as distinct peoples and
communities; and (8) tendency to manage their own affairs
separate from centralized state authorities.4 There are 370
million Indigenouspeoplein 90 countries,and they
consistentlyexperiencesignificantly poorer health
outcomesthan theirnon-Indigenouscounterparts.5,6 This
gap is particularly pronounced in developed nations with
historically colonized Indigenous minorities,including the
United States,Canada,New Zealand,and Australia,where
Indigenous morbidity and mortality rates are higher than in
many developing nations.7 Considering thatvision loss is
more prevalentin disadvantaged communities,8 it follows
thatmany Indigenouspopulationsare likely to havea
higher burden of vision loss. Nationwide studies have been
conducted in regionsof Asia, Africa, and Europe with
Indigenous populations,but none have attempted to collect
samples from Indigenous groups.9e22 By assuming ethnic
homogeneity and neglecting to interrogate Indigenous com-
munities,these surveys may have insufficiently quantified
the burden of vision loss in some of their countries’ most
vulnerable groups.Consequently,they may have under-
estimatedthe prevalenceof vision loss and generated
datathat are insufficientto optimallyinform national
interventions.
With the exceptionof 2 surveys conductedin
Australia,23,24 all surveysinvestigatingIndigenouseye
health have been subnational and focused on isolated tribes
or communities with varying degrees of sampling bias,25e33
and mostdid not makerobustcomparisonswith non-
Indigenousgroups25,27,28,30,33
or collectcomprehensive
ophthalmic data.29,30Nevertheless,the majority ofthese
surveys, in conjunction with other research, have found that
Indigenous communities in Brazil,Ecuador,United States,
and Australia have high rates of vision loss24,34,35
and eye
disease,including trachoma,30,36cataract,25 pterygium,25,37
and diabetic retinopathy.24 Therefore,because Indigenous
peoples constitutemore than 5% of the global
population,7 identifyingthe prevalenceand causesof
vision lossin these groupsin conjunction with general
populationsis critical to inform nationaleye health
programsand to achievethe objectivesof the Global
Action Plan.
Australia requires national prevalence data on vision loss
to fulfill its obligations as a signatory to the Global Action
Plan.State-levelsurveys conducted in the early 1990s in
Victoria,38 New South Wales,39 and South Australia40 have
been thereferencestudiesin Australiauntil now. We
conducted a nationwide study,the NationalEye Health
Survey (NEHS),to determine the prevalence and causes
of vision loss in Australia.This survey has implemented a
novelapproach to stratifying its sampling frame according
to Indigenous status to produce reliable estimates ofthe
prevalence and causes ofvision loss in both Indigenous
and non-Indigenous populations.We presentthe findings
of the NEHS and propose thatourstratified study design
forms the basis for future prevalence studies in all countr
with Indigenous groups.
Methods
Study Design and Participants
The sampling methodology ofthe NEHS has been described in
detail.41 In brief, the targetpopulationwas stratifiedinto
Indigenous Australians and non-Indigenous Australians.In accor-
dance with GlobalAction Plan guidelines,the NEHS recruited
non-IndigenousAustraliansaged 50 yearsor older.3 However,
because Indigenous Australians have earlier onset and more ra
progression ofeye disease and diabetes,42 a youngerage of40
years orolderwas selected.On the basisof the mostreliable
previousestimatesof the prevalenceof vision loss in
Australia,24,43the required sample size was 2794 non-Indigenous
Australiansand 1368 IndigenousAustraliansresidingin 30
geographic areas.
Multistage random-cluster sampling was used to selectpartic-
ipants on the basis of data from the 2011 Australian Census.44 In
stage 1 of sampling,the Australian population was stratified into
5 remoteness strata:Major City,Inner Regional,Outer Regional,
Remote,and Very Remote.Probabilityproportionalto size
sampling was used to select12 MajorCity, 6 InnerRegional,
6 OuterRegional,4 Remote,and 2 Very Remote survey sites,
corresponding to the approximate population distribution in ea
stratum.In the secondstage,a smallerclustercontaining
approximately 100 eligible residents was randomly selected an
nominated asthe enumeration site.Becauseof a numberof
factorsincludinginsufficientpopulationnumbers,inaccurate
Census data,and high absentee rates,a systematic approach was
used to make adjustmentsto some sites,including the use of
backup sitesand sampling from contiguousgeographicareas.
The details of this approach have been published.41 Door-to-door
recruitmentwas conducteduntil approximately100 non-
Indigenousparticipantswere recruitedfrom each cluster.
Although door-to-doorrecruitmentwas used forthe majority of
participants,we consulted Aboriginalelders and localAboriginal
Health Servicesto ensurethatour recruitmentmethodswere
culturallyappropriate.In someinstances,directdoor-to-door
recruitmentwas deemed culturally inappropriate,and telephone
recruitmentfrom formalizedcommunitylists was usedas a
substitute.Householdrecruitment,includingdoor-to-doorand
telephonerecruitment,accountedfor approximately80% of
Indigenous recruitment.Alternative methods ofcontactincluded
concurrent Indigenous health clinics and word of mouth.
The protocol was approved by the Royal Victorian Eye and E
Hospital Human Research Ethics Committee, as well as state-b
Indigenousethicsorganizations.This study wasconducted in
accordance with the tenets of the Declaration of Helsinki.
Procedures
The examination protocolof the NEHS hasbeen described in
detail.45 Participantexaminations were conducted in a totalof 61
testing venues thatincluded community centers,mobile clinics,
town halls, AboriginalCorporations,schools,and medical
clinics,all within 6 km ofeach recruitmentsite.Examinations
were conducted over13 monthsand 7 days,from March 11,
OphthalmologyVolume- , Number- , Month 2017
2
Indigenous peoples on the basis ofthe following criteria:
(1) self-identification as Indigenous peoples by individuals
and acceptance as such by their community;(2) historical
continuity and land occupation before invasion and coloni-
zation; (3) strong links to territories including land and water
and related natural resources; (4) distinct social, economic, or
politicalsystems;(5) distinctlanguage,culture,religion,
ceremonies, and beliefs; (6) tendency to form nondominant
groups of society; (7) resolution to maintain and reproduce
ancestral environments and systems as distinct peoples and
communities; and (8) tendency to manage their own affairs
separate from centralized state authorities.4 There are 370
million Indigenouspeoplein 90 countries,and they
consistentlyexperiencesignificantly poorer health
outcomesthan theirnon-Indigenouscounterparts.5,6 This
gap is particularly pronounced in developed nations with
historically colonized Indigenous minorities,including the
United States,Canada,New Zealand,and Australia,where
Indigenous morbidity and mortality rates are higher than in
many developing nations.7 Considering thatvision loss is
more prevalentin disadvantaged communities,8 it follows
thatmany Indigenouspopulationsare likely to havea
higher burden of vision loss. Nationwide studies have been
conducted in regionsof Asia, Africa, and Europe with
Indigenous populations,but none have attempted to collect
samples from Indigenous groups.9e22 By assuming ethnic
homogeneity and neglecting to interrogate Indigenous com-
munities,these surveys may have insufficiently quantified
the burden of vision loss in some of their countries’ most
vulnerable groups.Consequently,they may have under-
estimatedthe prevalenceof vision loss and generated
datathat are insufficientto optimallyinform national
interventions.
With the exceptionof 2 surveys conductedin
Australia,23,24 all surveysinvestigatingIndigenouseye
health have been subnational and focused on isolated tribes
or communities with varying degrees of sampling bias,25e33
and mostdid not makerobustcomparisonswith non-
Indigenousgroups25,27,28,30,33
or collectcomprehensive
ophthalmic data.29,30Nevertheless,the majority ofthese
surveys, in conjunction with other research, have found that
Indigenous communities in Brazil,Ecuador,United States,
and Australia have high rates of vision loss24,34,35
and eye
disease,including trachoma,30,36cataract,25 pterygium,25,37
and diabetic retinopathy.24 Therefore,because Indigenous
peoples constitutemore than 5% of the global
population,7 identifyingthe prevalenceand causesof
vision lossin these groupsin conjunction with general
populationsis critical to inform nationaleye health
programsand to achievethe objectivesof the Global
Action Plan.
Australia requires national prevalence data on vision loss
to fulfill its obligations as a signatory to the Global Action
Plan.State-levelsurveys conducted in the early 1990s in
Victoria,38 New South Wales,39 and South Australia40 have
been thereferencestudiesin Australiauntil now. We
conducted a nationwide study,the NationalEye Health
Survey (NEHS),to determine the prevalence and causes
of vision loss in Australia.This survey has implemented a
novelapproach to stratifying its sampling frame according
to Indigenous status to produce reliable estimates ofthe
prevalence and causes ofvision loss in both Indigenous
and non-Indigenous populations.We presentthe findings
of the NEHS and propose thatourstratified study design
forms the basis for future prevalence studies in all countr
with Indigenous groups.
Methods
Study Design and Participants
The sampling methodology ofthe NEHS has been described in
detail.41 In brief, the targetpopulationwas stratifiedinto
Indigenous Australians and non-Indigenous Australians.In accor-
dance with GlobalAction Plan guidelines,the NEHS recruited
non-IndigenousAustraliansaged 50 yearsor older.3 However,
because Indigenous Australians have earlier onset and more ra
progression ofeye disease and diabetes,42 a youngerage of40
years orolderwas selected.On the basisof the mostreliable
previousestimatesof the prevalenceof vision loss in
Australia,24,43the required sample size was 2794 non-Indigenous
Australiansand 1368 IndigenousAustraliansresidingin 30
geographic areas.
Multistage random-cluster sampling was used to selectpartic-
ipants on the basis of data from the 2011 Australian Census.44 In
stage 1 of sampling,the Australian population was stratified into
5 remoteness strata:Major City,Inner Regional,Outer Regional,
Remote,and Very Remote.Probabilityproportionalto size
sampling was used to select12 MajorCity, 6 InnerRegional,
6 OuterRegional,4 Remote,and 2 Very Remote survey sites,
corresponding to the approximate population distribution in ea
stratum.In the secondstage,a smallerclustercontaining
approximately 100 eligible residents was randomly selected an
nominated asthe enumeration site.Becauseof a numberof
factorsincludinginsufficientpopulationnumbers,inaccurate
Census data,and high absentee rates,a systematic approach was
used to make adjustmentsto some sites,including the use of
backup sitesand sampling from contiguousgeographicareas.
The details of this approach have been published.41 Door-to-door
recruitmentwas conducteduntil approximately100 non-
Indigenousparticipantswere recruitedfrom each cluster.
Although door-to-doorrecruitmentwas used forthe majority of
participants,we consulted Aboriginalelders and localAboriginal
Health Servicesto ensurethatour recruitmentmethodswere
culturallyappropriate.In someinstances,directdoor-to-door
recruitmentwas deemed culturally inappropriate,and telephone
recruitmentfrom formalizedcommunitylists was usedas a
substitute.Householdrecruitment,includingdoor-to-doorand
telephonerecruitment,accountedfor approximately80% of
Indigenous recruitment.Alternative methods ofcontactincluded
concurrent Indigenous health clinics and word of mouth.
The protocol was approved by the Royal Victorian Eye and E
Hospital Human Research Ethics Committee, as well as state-b
Indigenousethicsorganizations.This study wasconducted in
accordance with the tenets of the Declaration of Helsinki.
Procedures
The examination protocolof the NEHS hasbeen described in
detail.45 Participantexaminations were conducted in a totalof 61
testing venues thatincluded community centers,mobile clinics,
town halls, AboriginalCorporations,schools,and medical
clinics,all within 6 km ofeach recruitmentsite.Examinations
were conducted over13 monthsand 7 days,from March 11,
OphthalmologyVolume- , Number- , Month 2017
2
2015,to April 18, 2016.Residentsattended testing centersat
prespecified appointmenttimesand provided written informed
consent.Standardized sociodemographic,stroke,diabetes,and
ocular history data were collectedusing an interviewer-
administered questionnaire.
Standardized eye examinations were conducted by researchers,
including ophthalmologists, optometrists, orthoptists, and research
assistants trained at the Centre for Eye Research Australia (CERA).
Presenting distancevisualacuity wasmeasured foreach eye
separately using a logarithm of the minimum angle of resolution
chart (Brien Holden Vision Institute, New South Wales, Australia)
in well-lit room conditions. Pinhole testing was performed using a
multiple pinhole occluder on participants with visual acuity <6/12
in 1 or both eyes.If visualacuity improved with pinhole testing,
autorefraction wasperformed using aNidek ARK-30 Type-R
handheld autorefractor/keratometer (Nidek Co, Ltd, Tokyo, Japan),
and autorefraction-corrected visual acuity was measured. Binocular
presenting near vision was assessed using a CERA “Tumbling E”
nearvision card (CERA,Melbourne,Australia)held atthe par-
ticipant’s preferred reading distance. The smallest line at which the
direction ofat least3 of the 4 “Tumbling E” optotypeswas
correctly identified was recorded. Visual fields were assessed using
a Frequency Doubling Technology perimeter(ZeissHumphrey
Systems,Oberkochen,Germany,and Welch Allyn,Skaneateles
Falls,NY).
Examination ofthe anteriorsegmentwas performed using a
hand-held slitlamp (KeelerOphthalmic Instruments,Berkshire,
UK) at 10 magnification. BecauseChlamydiatrachomatis
infection is endemic in Indigenous Australians,butnotin non-
Indigenous Australians,grading fortrachomatoustrichiasisand
cornealopacity was performed in Indigenous participants using
only the World Health Organization Trachoma Simplified Grading
System.46 If presenting visualacuity was<6/12 in eithereye,
examiners took an anterior segmentphoto in the affected eye(s)
with a DigitalRetinography System47 camera (CenterVue,SpA,
Padova,Italy).
Two-field,45 colorfundus photographs were taken ofeach
retina, centered on the macula and optic disc, respectively, using a
nonmydriatic Diabetic Retinopathy Screening camera in a dark-
ened room to allow forphysiologic mydriasis.In 663 patients
(13.7%) in whom photograph quality was poor because of small
pupilsize,tropicamide 0.5% was instilled to induce mydriasis if
anterior chambers were deemed wide enough to do so safely using
the method by Van Herick et al,48 and photographs were repeated.
Dilation was not performed when the angle was graded as 1 or 2.
Intraocularpressurewas measured using an iCareTonometer
(iCare,Vantaa,Finland).Participants were provided with verbal
feedback on the health oftheireyes,and those with suspected
pathology were provided with a referralletterto be taken to a
local doctor or optometrist.
Blinded retinal graders at CERA graded all retinal images using
OpenClinica software (OpenClinica LLC and collaborators,Wal-
tham, MA), and pathology was graded according to protocols that
have been described in detail.47,49,50
The main cause of vision loss was determined by 2 independent
ophthalmologists,and disagreements were adjudicated by a third
ophthalmologist.Data pertaining to participants’ age,gender,and
Indigenous status were provided to assist with disease attribution.
Uncorrected refractive errorwas assigned as the main cause of
vision loss when distance visual acuity improved to 6/12 in 1 or
both eyeswith pinhole orautorefraction.For all othercases,
ophthalmologists reviewed questionnaire responses and examina-
tion results to identify the condition mostlikely to accountfor
vision loss. When multiple disorders were identified, the condition
with the most clinically significant influence was determined to be
the primary cause.For cases in which a single primary cause was
notidentifiable,vision loss was attributed to combined mecha-
nisms. Cases of vision loss were deemed “not determinable” if
cause of vision loss was identified.
Definitions
Vision impairmentwas defined asbilateralpresenting distance
visual acuity to 6/60. Blindnesswas definedas bilateral
presenting distance visual acuity <6/60. Vision loss was define
bilateralpresenting distance visualacuity <6/12 and included all
cases ofvision impairmentand blindness.Participants with pre-
senting visual acuity <6/12 in 1 eye but 6/12 in the fellow eye
(unilateral vision loss) were not considered to have vision loss
the purpose of this article.
Statistical Analysis
The crude prevalence ofvision loss was calculated as the per-
centageof participantswith vision loss.Prevalencewas then
weighted to accountfor the sampling rate in each remoteness
stratum becausepopulation sizesvaried between strata.This
involved dividing the target population recruited from each stra
overthe population size in each stratum.This also allowed the
absolute number of Australians with vision loss in each stratum
be estimated.To facilitate comparisons between Indigenous and
non-Indigenous Australians, the weighted prevalence of vision
was adjusted for age and gender. Logistic regression analysis w
used to identify risk factors for vision loss. Factors associated w
vision loss atP < 0.10 in univariable analysis were included in
subsequent multivariable logistic regression analysis. A plot of
residuals compared with estimates was examined to testlinearity
and homoscedasticity. The Box-Tidwell model was used to find
bestpower for modelfit based on maximallikelihood estimates.
Logistic regression Model1 investigated risk factors forIndige-
nous and non-Indigenousparticipantstogether.In Model 2,
Indigenousand non-Indigenousparticipantswere investigated
separately.Analyses were conducted with STATA version 14.2.0
(StataCorp LP,College Station,TX).
Results
Participant Characteristics
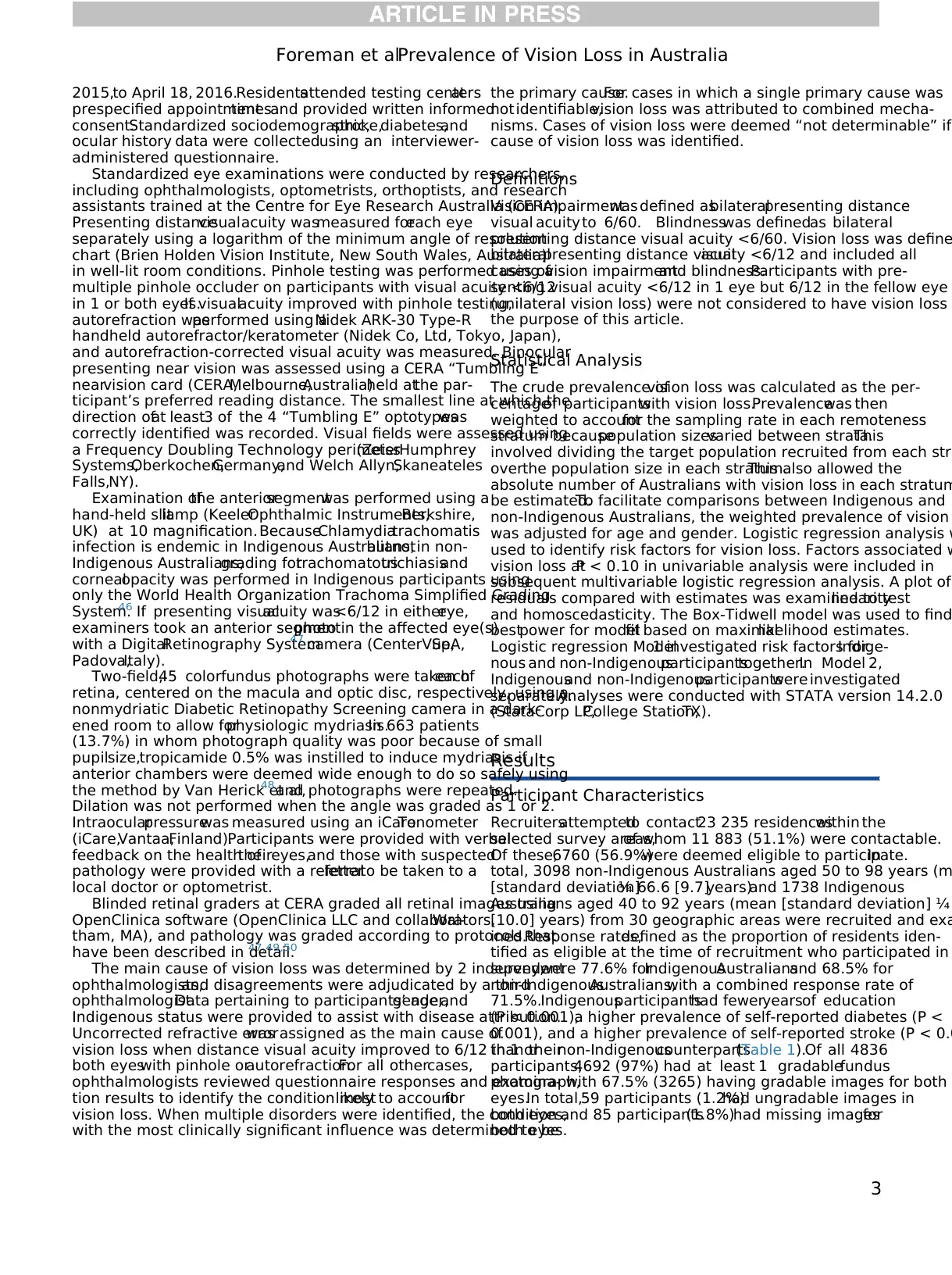
Recruitersattemptedto contact23 235 residenceswithin the
selected survey areas,of whom 11 883 (51.1%) were contactable.
Of these,6760 (56.9%)were deemed eligible to participate.In
total, 3098 non-Indigenous Australians aged 50 to 98 years (m
[standard deviation]¼ 66.6 [9.7]years)and 1738 Indigenous
Australians aged 40 to 92 years (mean [standard deviation] ¼
[10.0] years) from 30 geographic areas were recruited and exa
ined.Response rates,defined as the proportion of residents iden-
tified as eligible at the time of recruitment who participated in
survey,were 77.6% forIndigenousAustraliansand 68.5% for
non-IndigenousAustralians,with a combined response rate of
71.5%.Indigenousparticipantshad feweryearsof education
(P < 0.001),a higher prevalence of self-reported diabetes (P <
0.001), and a higher prevalence of self-reported stroke (P < 0.0
than theirnon-Indigenouscounterparts(Table 1).Of all 4836
participants,4692 (97%) had at least 1 gradablefundus
photograph,with 67.5% (3265) having gradable images for both
eyes.In total,59 participants (1.2%)had ungradable images in
both eyes,and 85 participants(1.8%)had missing imagesfor
both eyes.
Foreman et alPrevalence of Vision Loss in Australia
3
prespecified appointmenttimesand provided written informed
consent.Standardized sociodemographic,stroke,diabetes,and
ocular history data were collectedusing an interviewer-
administered questionnaire.
Standardized eye examinations were conducted by researchers,
including ophthalmologists, optometrists, orthoptists, and research
assistants trained at the Centre for Eye Research Australia (CERA).
Presenting distancevisualacuity wasmeasured foreach eye
separately using a logarithm of the minimum angle of resolution
chart (Brien Holden Vision Institute, New South Wales, Australia)
in well-lit room conditions. Pinhole testing was performed using a
multiple pinhole occluder on participants with visual acuity <6/12
in 1 or both eyes.If visualacuity improved with pinhole testing,
autorefraction wasperformed using aNidek ARK-30 Type-R
handheld autorefractor/keratometer (Nidek Co, Ltd, Tokyo, Japan),
and autorefraction-corrected visual acuity was measured. Binocular
presenting near vision was assessed using a CERA “Tumbling E”
nearvision card (CERA,Melbourne,Australia)held atthe par-
ticipant’s preferred reading distance. The smallest line at which the
direction ofat least3 of the 4 “Tumbling E” optotypeswas
correctly identified was recorded. Visual fields were assessed using
a Frequency Doubling Technology perimeter(ZeissHumphrey
Systems,Oberkochen,Germany,and Welch Allyn,Skaneateles
Falls,NY).
Examination ofthe anteriorsegmentwas performed using a
hand-held slitlamp (KeelerOphthalmic Instruments,Berkshire,
UK) at 10 magnification. BecauseChlamydiatrachomatis
infection is endemic in Indigenous Australians,butnotin non-
Indigenous Australians,grading fortrachomatoustrichiasisand
cornealopacity was performed in Indigenous participants using
only the World Health Organization Trachoma Simplified Grading
System.46 If presenting visualacuity was<6/12 in eithereye,
examiners took an anterior segmentphoto in the affected eye(s)
with a DigitalRetinography System47 camera (CenterVue,SpA,
Padova,Italy).
Two-field,45 colorfundus photographs were taken ofeach
retina, centered on the macula and optic disc, respectively, using a
nonmydriatic Diabetic Retinopathy Screening camera in a dark-
ened room to allow forphysiologic mydriasis.In 663 patients
(13.7%) in whom photograph quality was poor because of small
pupilsize,tropicamide 0.5% was instilled to induce mydriasis if
anterior chambers were deemed wide enough to do so safely using
the method by Van Herick et al,48 and photographs were repeated.
Dilation was not performed when the angle was graded as 1 or 2.
Intraocularpressurewas measured using an iCareTonometer
(iCare,Vantaa,Finland).Participants were provided with verbal
feedback on the health oftheireyes,and those with suspected
pathology were provided with a referralletterto be taken to a
local doctor or optometrist.
Blinded retinal graders at CERA graded all retinal images using
OpenClinica software (OpenClinica LLC and collaborators,Wal-
tham, MA), and pathology was graded according to protocols that
have been described in detail.47,49,50
The main cause of vision loss was determined by 2 independent
ophthalmologists,and disagreements were adjudicated by a third
ophthalmologist.Data pertaining to participants’ age,gender,and
Indigenous status were provided to assist with disease attribution.
Uncorrected refractive errorwas assigned as the main cause of
vision loss when distance visual acuity improved to 6/12 in 1 or
both eyeswith pinhole orautorefraction.For all othercases,
ophthalmologists reviewed questionnaire responses and examina-
tion results to identify the condition mostlikely to accountfor
vision loss. When multiple disorders were identified, the condition
with the most clinically significant influence was determined to be
the primary cause.For cases in which a single primary cause was
notidentifiable,vision loss was attributed to combined mecha-
nisms. Cases of vision loss were deemed “not determinable” if
cause of vision loss was identified.
Definitions
Vision impairmentwas defined asbilateralpresenting distance
visual acuity to 6/60. Blindnesswas definedas bilateral
presenting distance visual acuity <6/60. Vision loss was define
bilateralpresenting distance visualacuity <6/12 and included all
cases ofvision impairmentand blindness.Participants with pre-
senting visual acuity <6/12 in 1 eye but 6/12 in the fellow eye
(unilateral vision loss) were not considered to have vision loss
the purpose of this article.
Statistical Analysis
The crude prevalence ofvision loss was calculated as the per-
centageof participantswith vision loss.Prevalencewas then
weighted to accountfor the sampling rate in each remoteness
stratum becausepopulation sizesvaried between strata.This
involved dividing the target population recruited from each stra
overthe population size in each stratum.This also allowed the
absolute number of Australians with vision loss in each stratum
be estimated.To facilitate comparisons between Indigenous and
non-Indigenous Australians, the weighted prevalence of vision
was adjusted for age and gender. Logistic regression analysis w
used to identify risk factors for vision loss. Factors associated w
vision loss atP < 0.10 in univariable analysis were included in
subsequent multivariable logistic regression analysis. A plot of
residuals compared with estimates was examined to testlinearity
and homoscedasticity. The Box-Tidwell model was used to find
bestpower for modelfit based on maximallikelihood estimates.
Logistic regression Model1 investigated risk factors forIndige-
nous and non-Indigenousparticipantstogether.In Model 2,
Indigenousand non-Indigenousparticipantswere investigated
separately.Analyses were conducted with STATA version 14.2.0
(StataCorp LP,College Station,TX).
Results
Participant Characteristics
Recruitersattemptedto contact23 235 residenceswithin the
selected survey areas,of whom 11 883 (51.1%) were contactable.
Of these,6760 (56.9%)were deemed eligible to participate.In
total, 3098 non-Indigenous Australians aged 50 to 98 years (m
[standard deviation]¼ 66.6 [9.7]years)and 1738 Indigenous
Australians aged 40 to 92 years (mean [standard deviation] ¼
[10.0] years) from 30 geographic areas were recruited and exa
ined.Response rates,defined as the proportion of residents iden-
tified as eligible at the time of recruitment who participated in
survey,were 77.6% forIndigenousAustraliansand 68.5% for
non-IndigenousAustralians,with a combined response rate of
71.5%.Indigenousparticipantshad feweryearsof education
(P < 0.001),a higher prevalence of self-reported diabetes (P <
0.001), and a higher prevalence of self-reported stroke (P < 0.0
than theirnon-Indigenouscounterparts(Table 1).Of all 4836
participants,4692 (97%) had at least 1 gradablefundus
photograph,with 67.5% (3265) having gradable images for both
eyes.In total,59 participants (1.2%)had ungradable images in
both eyes,and 85 participants(1.8%)had missing imagesfor
both eyes.
Foreman et alPrevalence of Vision Loss in Australia
3
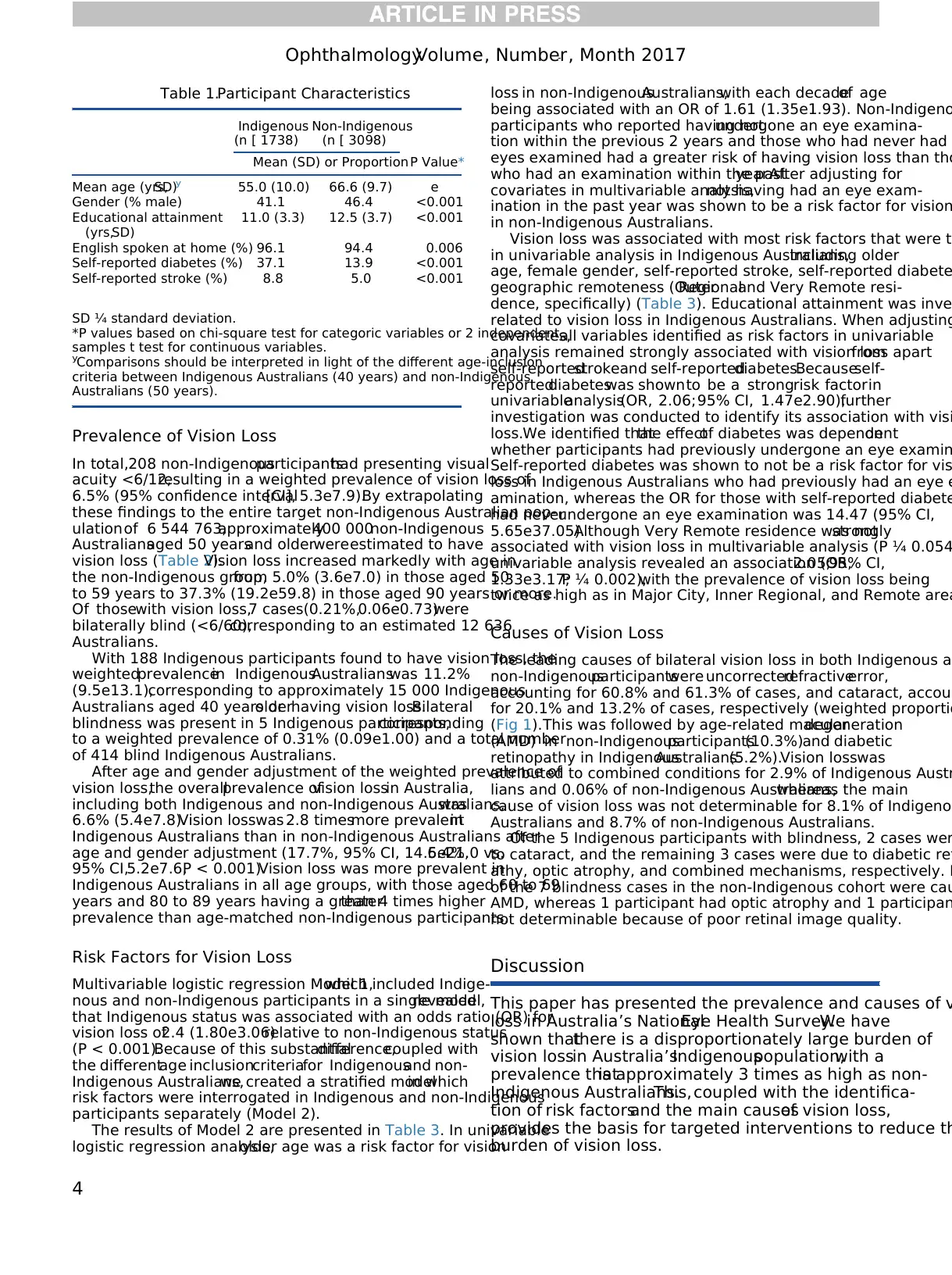
Prevalence of Vision Loss
In total,208 non-Indigenousparticipantshad presenting visual
acuity <6/12,resulting in a weighted prevalence of vision loss of
6.5% (95% confidence interval[CI], 5.3e7.9).By extrapolating
these findings to the entire target non-Indigenous Australian pop-
ulationof 6 544 763,approximately400 000non-Indigenous
Australiansaged 50 yearsand olderwereestimated to have
vision loss (Table 2).Vision loss increased markedly with age in
the non-Indigenous group,from 5.0% (3.6e7.0) in those aged 50
to 59 years to 37.3% (19.2e59.8) in those aged 90 years or more.
Of thosewith vision loss,7 cases(0.21%,0.06e0.73)were
bilaterally blind (<6/60),corresponding to an estimated 12 636
Australians.
With 188 Indigenous participants found to have vision loss, the
weightedprevalencein IndigenousAustralianswas 11.2%
(9.5e13.1),corresponding to approximately 15 000 Indigenous
Australians aged 40 years orolderhaving vision loss.Bilateral
blindness was present in 5 Indigenous participants,corresponding
to a weighted prevalence of 0.31% (0.09e1.00) and a total number
of 414 blind Indigenous Australians.
After age and gender adjustment of the weighted prevalence of
vision loss,the overallprevalence ofvision lossin Australia,
including both Indigenous and non-Indigenous Australians,was
6.6% (5.4e7.8).Vision losswas 2.8 timesmore prevalentin
Indigenous Australians than in non-Indigenous Australians after
age and gender adjustment (17.7%, 95% CI, 14.5e21.0 vs.6.4%,
95% CI,5.2e7.6,P < 0.001).Vision loss was more prevalent in
Indigenous Australians in all age groups, with those aged 60 to 69
years and 80 to 89 years having a greaterthan 4 times higher
prevalence than age-matched non-Indigenous participants.
Risk Factors for Vision Loss
Multivariable logistic regression Model 1,which included Indige-
nous and non-Indigenous participants in a single model,revealed
that Indigenous status was associated with an odds ratio (OR) for
vision loss of2.4 (1.80e3.06)relative to non-Indigenous status
(P < 0.001).Because of this substantialdifference,coupled with
the differentage inclusioncriteriafor Indigenousand non-
Indigenous Australians,we created a stratified modelin which
risk factors were interrogated in Indigenous and non-Indigenous
participants separately (Model 2).
The results of Model 2 are presented in Table 3. In univariable
logistic regression analysis,older age was a risk factor for vision
loss in non-IndigenousAustralians,with each decadeof age
being associated with an OR of 1.61 (1.35e1.93). Non-Indigeno
participants who reported having notundergone an eye examina-
tion within the previous 2 years and those who had never had
eyes examined had a greater risk of having vision loss than tho
who had an examination within the pastyear.After adjusting for
covariates in multivariable analysis,not having had an eye exam-
ination in the past year was shown to be a risk factor for vision
in non-Indigenous Australians.
Vision loss was associated with most risk factors that were te
in univariable analysis in Indigenous Australians,including older
age, female gender, self-reported stroke, self-reported diabete
geographic remoteness (OuterRegionaland Very Remote resi-
dence, specifically) (Table 3). Educational attainment was inve
related to vision loss in Indigenous Australians. When adjusting
covariates,all variables identified as risk factors in univariable
analysis remained strongly associated with vision loss apartfrom
self-reportedstrokeand self-reporteddiabetes.Becauseself-
reporteddiabeteswas shownto be a strongrisk factorin
univariableanalysis(OR, 2.06;95% CI, 1.47e2.90),further
investigation was conducted to identify its association with visi
loss.We identified thatthe effectof diabetes was dependenton
whether participants had previously undergone an eye examin
Self-reported diabetes was shown to not be a risk factor for vis
loss in Indigenous Australians who had previously had an eye e
amination, whereas the OR for those with self-reported diabete
had neverundergone an eye examination was 14.47 (95% CI,
5.65e37.05).Although Very Remote residence was notstrongly
associated with vision loss in multivariable analysis (P ¼ 0.054
univariable analysis revealed an association (OR,2.05;95% CI,
1.33e3.17;P ¼ 0.002),with the prevalence of vision loss being
twice as high as in Major City, Inner Regional, and Remote area
Causes of Vision Loss
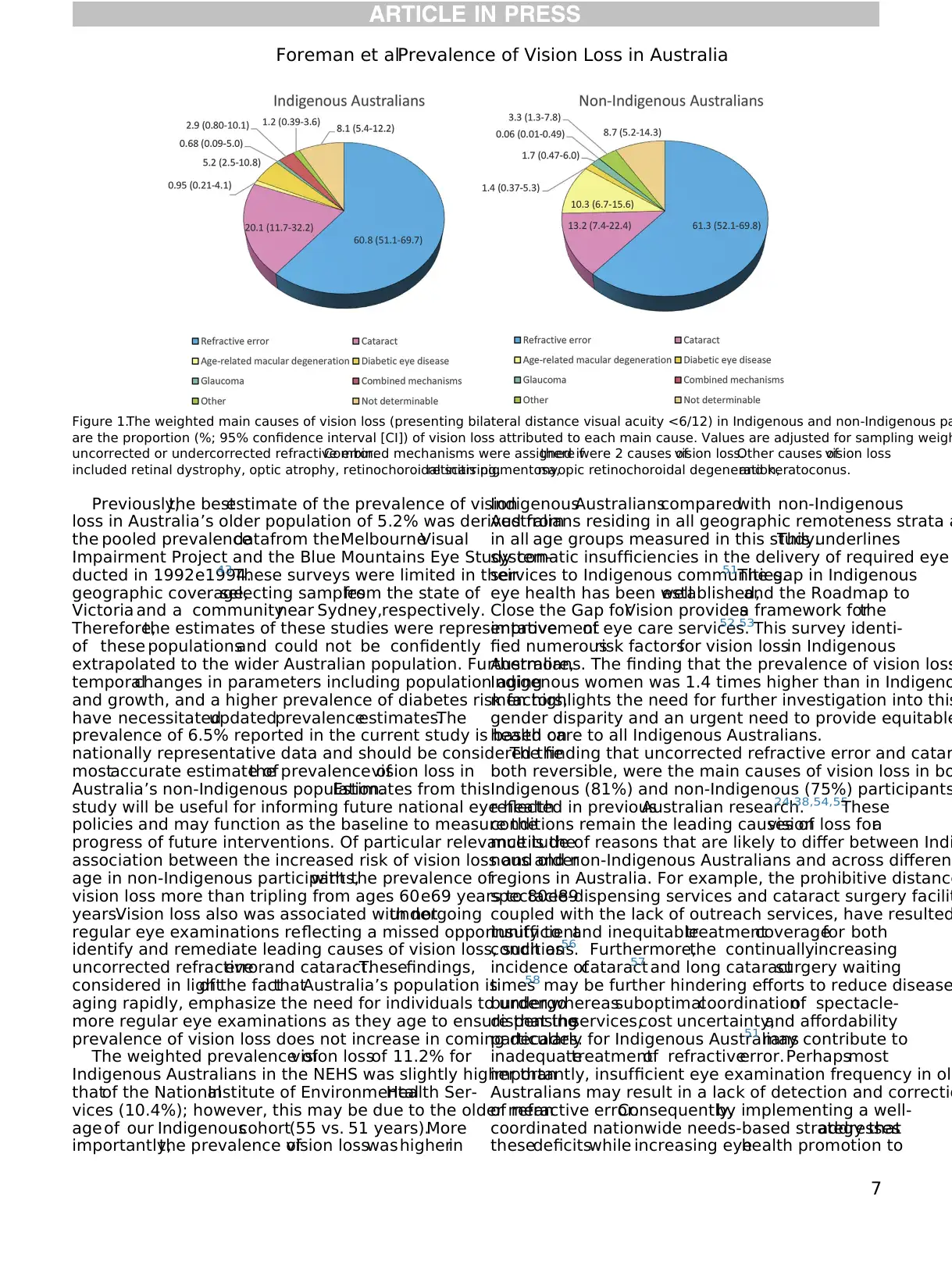
The leading causes of bilateral vision loss in both Indigenous an
non-Indigenousparticipantswere uncorrectedrefractiveerror,
accounting for 60.8% and 61.3% of cases, and cataract, accoun
for 20.1% and 13.2% of cases, respectively (weighted proportio
(Fig 1).This was followed by age-related maculardegeneration
(AMD) in non-Indigenousparticipants(10.3%)and diabetic
retinopathy in IndigenousAustralians(5.2%).Vision losswas
attributed to combined conditions for 2.9% of Indigenous Austr
lians and 0.06% of non-Indigenous Australians,whereas the main
cause of vision loss was not determinable for 8.1% of Indigenou
Australians and 8.7% of non-Indigenous Australians.
Of the 5 Indigenous participants with blindness, 2 cases wer
to cataract, and the remaining 3 cases were due to diabetic ret
athy, optic atrophy, and combined mechanisms, respectively. F
of the 7 blindness cases in the non-Indigenous cohort were cau
AMD, whereas 1 participant had optic atrophy and 1 participan
not determinable because of poor retinal image quality.
Discussion
This paper has presented the prevalence and causes of v
loss in Australia’s NationalEye Health Survey.We have
shown thatthere is a disproportionately large burden of
vision lossin Australia’sIndigenouspopulation,with a
prevalence thatis approximately 3 times as high as non-
Indigenous Australians.This, coupled with the identifica-
tion of risk factorsand the main causesof vision loss,
provides the basis for targeted interventions to reduce th
burden of vision loss.
Table 1.Participant Characteristics
Indigenous
(n [ 1738)
Non-Indigenous
(n [ 3098)
P Value*Mean (SD) or Proportion
Mean age (yrs,SD)y 55.0 (10.0) 66.6 (9.7) e
Gender (% male) 41.1 46.4 <0.001
Educational attainment
(yrs,SD)
11.0 (3.3) 12.5 (3.7) <0.001
English spoken at home (%) 96.1 94.4 0.006
Self-reported diabetes (%) 37.1 13.9 <0.001
Self-reported stroke (%) 8.8 5.0 <0.001
SD ¼ standard deviation.
*P values based on chi-square test for categoric variables or 2 independent
samples t test for continuous variables.
yComparisons should be interpreted in light of the different age-inclusion
criteria between Indigenous Australians (40 years) and non-Indigenous
Australians (50 years).
OphthalmologyVolume- , Number- , Month 2017
4
In total,208 non-Indigenousparticipantshad presenting visual
acuity <6/12,resulting in a weighted prevalence of vision loss of
6.5% (95% confidence interval[CI], 5.3e7.9).By extrapolating
these findings to the entire target non-Indigenous Australian pop-
ulationof 6 544 763,approximately400 000non-Indigenous
Australiansaged 50 yearsand olderwereestimated to have
vision loss (Table 2).Vision loss increased markedly with age in
the non-Indigenous group,from 5.0% (3.6e7.0) in those aged 50
to 59 years to 37.3% (19.2e59.8) in those aged 90 years or more.
Of thosewith vision loss,7 cases(0.21%,0.06e0.73)were
bilaterally blind (<6/60),corresponding to an estimated 12 636
Australians.
With 188 Indigenous participants found to have vision loss, the
weightedprevalencein IndigenousAustralianswas 11.2%
(9.5e13.1),corresponding to approximately 15 000 Indigenous
Australians aged 40 years orolderhaving vision loss.Bilateral
blindness was present in 5 Indigenous participants,corresponding
to a weighted prevalence of 0.31% (0.09e1.00) and a total number
of 414 blind Indigenous Australians.
After age and gender adjustment of the weighted prevalence of
vision loss,the overallprevalence ofvision lossin Australia,
including both Indigenous and non-Indigenous Australians,was
6.6% (5.4e7.8).Vision losswas 2.8 timesmore prevalentin
Indigenous Australians than in non-Indigenous Australians after
age and gender adjustment (17.7%, 95% CI, 14.5e21.0 vs.6.4%,
95% CI,5.2e7.6,P < 0.001).Vision loss was more prevalent in
Indigenous Australians in all age groups, with those aged 60 to 69
years and 80 to 89 years having a greaterthan 4 times higher
prevalence than age-matched non-Indigenous participants.
Risk Factors for Vision Loss
Multivariable logistic regression Model 1,which included Indige-
nous and non-Indigenous participants in a single model,revealed
that Indigenous status was associated with an odds ratio (OR) for
vision loss of2.4 (1.80e3.06)relative to non-Indigenous status
(P < 0.001).Because of this substantialdifference,coupled with
the differentage inclusioncriteriafor Indigenousand non-
Indigenous Australians,we created a stratified modelin which
risk factors were interrogated in Indigenous and non-Indigenous
participants separately (Model 2).
The results of Model 2 are presented in Table 3. In univariable
logistic regression analysis,older age was a risk factor for vision
loss in non-IndigenousAustralians,with each decadeof age
being associated with an OR of 1.61 (1.35e1.93). Non-Indigeno
participants who reported having notundergone an eye examina-
tion within the previous 2 years and those who had never had
eyes examined had a greater risk of having vision loss than tho
who had an examination within the pastyear.After adjusting for
covariates in multivariable analysis,not having had an eye exam-
ination in the past year was shown to be a risk factor for vision
in non-Indigenous Australians.
Vision loss was associated with most risk factors that were te
in univariable analysis in Indigenous Australians,including older
age, female gender, self-reported stroke, self-reported diabete
geographic remoteness (OuterRegionaland Very Remote resi-
dence, specifically) (Table 3). Educational attainment was inve
related to vision loss in Indigenous Australians. When adjusting
covariates,all variables identified as risk factors in univariable
analysis remained strongly associated with vision loss apartfrom
self-reportedstrokeand self-reporteddiabetes.Becauseself-
reporteddiabeteswas shownto be a strongrisk factorin
univariableanalysis(OR, 2.06;95% CI, 1.47e2.90),further
investigation was conducted to identify its association with visi
loss.We identified thatthe effectof diabetes was dependenton
whether participants had previously undergone an eye examin
Self-reported diabetes was shown to not be a risk factor for vis
loss in Indigenous Australians who had previously had an eye e
amination, whereas the OR for those with self-reported diabete
had neverundergone an eye examination was 14.47 (95% CI,
5.65e37.05).Although Very Remote residence was notstrongly
associated with vision loss in multivariable analysis (P ¼ 0.054
univariable analysis revealed an association (OR,2.05;95% CI,
1.33e3.17;P ¼ 0.002),with the prevalence of vision loss being
twice as high as in Major City, Inner Regional, and Remote area
Causes of Vision Loss
The leading causes of bilateral vision loss in both Indigenous an
non-Indigenousparticipantswere uncorrectedrefractiveerror,
accounting for 60.8% and 61.3% of cases, and cataract, accoun
for 20.1% and 13.2% of cases, respectively (weighted proportio
(Fig 1).This was followed by age-related maculardegeneration
(AMD) in non-Indigenousparticipants(10.3%)and diabetic
retinopathy in IndigenousAustralians(5.2%).Vision losswas
attributed to combined conditions for 2.9% of Indigenous Austr
lians and 0.06% of non-Indigenous Australians,whereas the main
cause of vision loss was not determinable for 8.1% of Indigenou
Australians and 8.7% of non-Indigenous Australians.
Of the 5 Indigenous participants with blindness, 2 cases wer
to cataract, and the remaining 3 cases were due to diabetic ret
athy, optic atrophy, and combined mechanisms, respectively. F
of the 7 blindness cases in the non-Indigenous cohort were cau
AMD, whereas 1 participant had optic atrophy and 1 participan
not determinable because of poor retinal image quality.
Discussion
This paper has presented the prevalence and causes of v
loss in Australia’s NationalEye Health Survey.We have
shown thatthere is a disproportionately large burden of
vision lossin Australia’sIndigenouspopulation,with a
prevalence thatis approximately 3 times as high as non-
Indigenous Australians.This, coupled with the identifica-
tion of risk factorsand the main causesof vision loss,
provides the basis for targeted interventions to reduce th
burden of vision loss.
Table 1.Participant Characteristics
Indigenous
(n [ 1738)
Non-Indigenous
(n [ 3098)
P Value*Mean (SD) or Proportion
Mean age (yrs,SD)y 55.0 (10.0) 66.6 (9.7) e
Gender (% male) 41.1 46.4 <0.001
Educational attainment
(yrs,SD)
11.0 (3.3) 12.5 (3.7) <0.001
English spoken at home (%) 96.1 94.4 0.006
Self-reported diabetes (%) 37.1 13.9 <0.001
Self-reported stroke (%) 8.8 5.0 <0.001
SD ¼ standard deviation.
*P values based on chi-square test for categoric variables or 2 independent
samples t test for continuous variables.
yComparisons should be interpreted in light of the different age-inclusion
criteria between Indigenous Australians (40 years) and non-Indigenous
Australians (50 years).
OphthalmologyVolume- , Number- , Month 2017
4
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
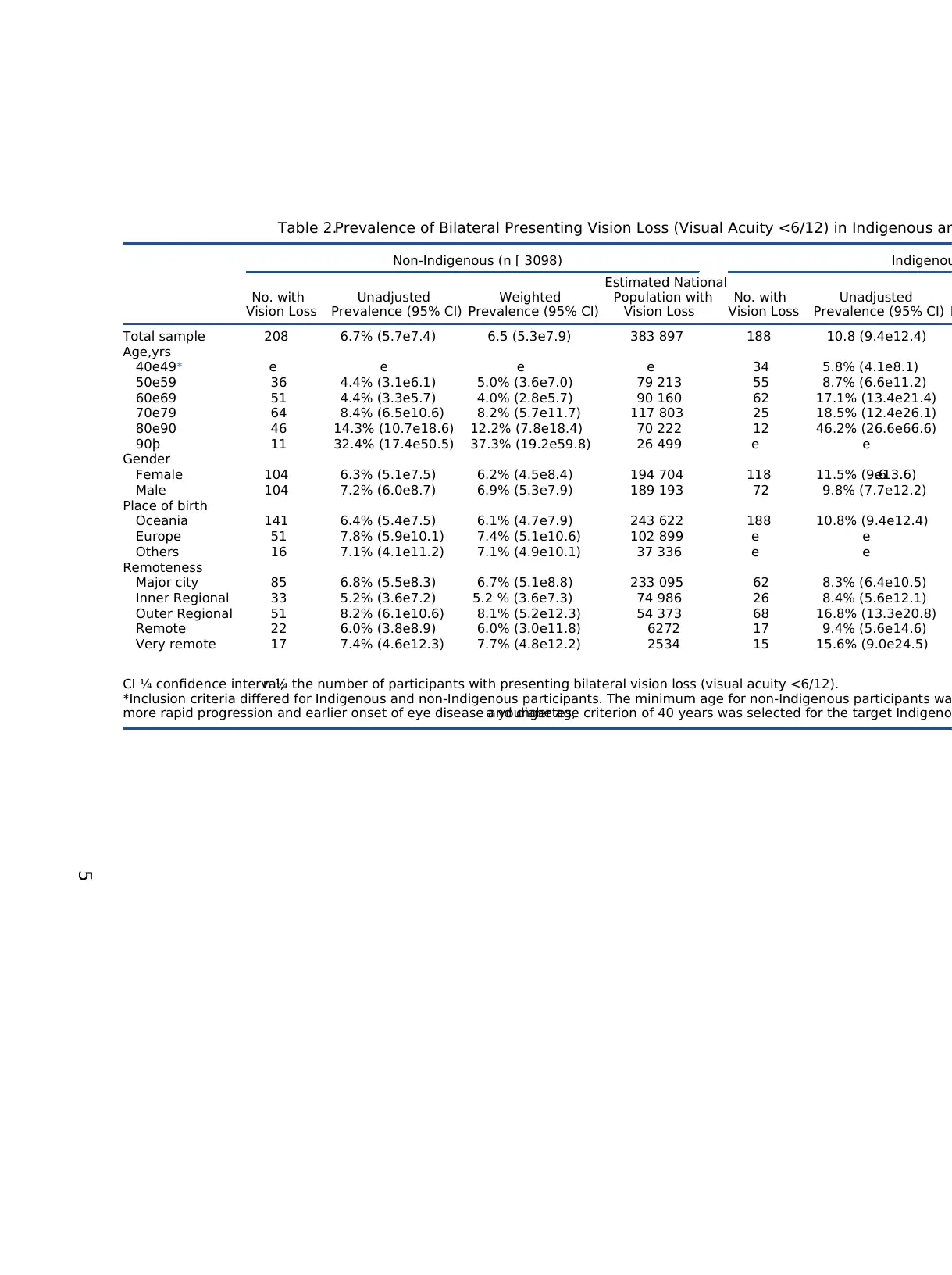
Table 2.Prevalence of Bilateral Presenting Vision Loss (Visual Acuity <6/12) in Indigenous an
Non-Indigenous (n [ 3098) Indigenou
No. with
Vision Loss
Unadjusted
Prevalence (95% CI)
Weighted
Prevalence (95% CI)
Estimated National
Population with
Vision Loss
No. with
Vision Loss
Unadjusted
Prevalence (95% CI) P
Total sample 208 6.7% (5.7e7.4) 6.5 (5.3e7.9) 383 897 188 10.8 (9.4e12.4)
Age,yrs
40e49* e e e e 34 5.8% (4.1e8.1)
50e59 36 4.4% (3.1e6.1) 5.0% (3.6e7.0) 79 213 55 8.7% (6.6e11.2)
60e69 51 4.4% (3.3e5.7) 4.0% (2.8e5.7) 90 160 62 17.1% (13.4e21.4)
70e79 64 8.4% (6.5e10.6) 8.2% (5.7e11.7) 117 803 25 18.5% (12.4e26.1)
80e90 46 14.3% (10.7e18.6) 12.2% (7.8e18.4) 70 222 12 46.2% (26.6e66.6)
90þ 11 32.4% (17.4e50.5) 37.3% (19.2e59.8) 26 499 e e
Gender
Female 104 6.3% (5.1e7.5) 6.2% (4.5e8.4) 194 704 118 11.5% (9.6e13.6)
Male 104 7.2% (6.0e8.7) 6.9% (5.3e7.9) 189 193 72 9.8% (7.7e12.2)
Place of birth
Oceania 141 6.4% (5.4e7.5) 6.1% (4.7e7.9) 243 622 188 10.8% (9.4e12.4)
Europe 51 7.8% (5.9e10.1) 7.4% (5.1e10.6) 102 899 e e
Others 16 7.1% (4.1e11.2) 7.1% (4.9e10.1) 37 336 e e
Remoteness
Major city 85 6.8% (5.5e8.3) 6.7% (5.1e8.8) 233 095 62 8.3% (6.4e10.5)
Inner Regional 33 5.2% (3.6e7.2) 5.2 % (3.6e7.3) 74 986 26 8.4% (5.6e12.1)
Outer Regional 51 8.2% (6.1e10.6) 8.1% (5.2e12.3) 54 373 68 16.8% (13.3e20.8)
Remote 22 6.0% (3.8e8.9) 6.0% (3.0e11.8) 6272 17 9.4% (5.6e14.6)
Very remote 17 7.4% (4.6e12.3) 7.7% (4.8e12.2) 2534 15 15.6% (9.0e24.5)
CI ¼ confidence interval;n ¼ the number of participants with presenting bilateral vision loss (visual acuity <6/12).
*Inclusion criteria differed for Indigenous and non-Indigenous participants. The minimum age for non-Indigenous participants wa
more rapid progression and earlier onset of eye disease and diabetes,a younger age criterion of 40 years was selected for the target Indigeno
5
Non-Indigenous (n [ 3098) Indigenou
No. with
Vision Loss
Unadjusted
Prevalence (95% CI)
Weighted
Prevalence (95% CI)
Estimated National
Population with
Vision Loss
No. with
Vision Loss
Unadjusted
Prevalence (95% CI) P
Total sample 208 6.7% (5.7e7.4) 6.5 (5.3e7.9) 383 897 188 10.8 (9.4e12.4)
Age,yrs
40e49* e e e e 34 5.8% (4.1e8.1)
50e59 36 4.4% (3.1e6.1) 5.0% (3.6e7.0) 79 213 55 8.7% (6.6e11.2)
60e69 51 4.4% (3.3e5.7) 4.0% (2.8e5.7) 90 160 62 17.1% (13.4e21.4)
70e79 64 8.4% (6.5e10.6) 8.2% (5.7e11.7) 117 803 25 18.5% (12.4e26.1)
80e90 46 14.3% (10.7e18.6) 12.2% (7.8e18.4) 70 222 12 46.2% (26.6e66.6)
90þ 11 32.4% (17.4e50.5) 37.3% (19.2e59.8) 26 499 e e
Gender
Female 104 6.3% (5.1e7.5) 6.2% (4.5e8.4) 194 704 118 11.5% (9.6e13.6)
Male 104 7.2% (6.0e8.7) 6.9% (5.3e7.9) 189 193 72 9.8% (7.7e12.2)
Place of birth
Oceania 141 6.4% (5.4e7.5) 6.1% (4.7e7.9) 243 622 188 10.8% (9.4e12.4)
Europe 51 7.8% (5.9e10.1) 7.4% (5.1e10.6) 102 899 e e
Others 16 7.1% (4.1e11.2) 7.1% (4.9e10.1) 37 336 e e
Remoteness
Major city 85 6.8% (5.5e8.3) 6.7% (5.1e8.8) 233 095 62 8.3% (6.4e10.5)
Inner Regional 33 5.2% (3.6e7.2) 5.2 % (3.6e7.3) 74 986 26 8.4% (5.6e12.1)
Outer Regional 51 8.2% (6.1e10.6) 8.1% (5.2e12.3) 54 373 68 16.8% (13.3e20.8)
Remote 22 6.0% (3.8e8.9) 6.0% (3.0e11.8) 6272 17 9.4% (5.6e14.6)
Very remote 17 7.4% (4.6e12.3) 7.7% (4.8e12.2) 2534 15 15.6% (9.0e24.5)
CI ¼ confidence interval;n ¼ the number of participants with presenting bilateral vision loss (visual acuity <6/12).
*Inclusion criteria differed for Indigenous and non-Indigenous participants. The minimum age for non-Indigenous participants wa
more rapid progression and earlier onset of eye disease and diabetes,a younger age criterion of 40 years was selected for the target Indigeno
5
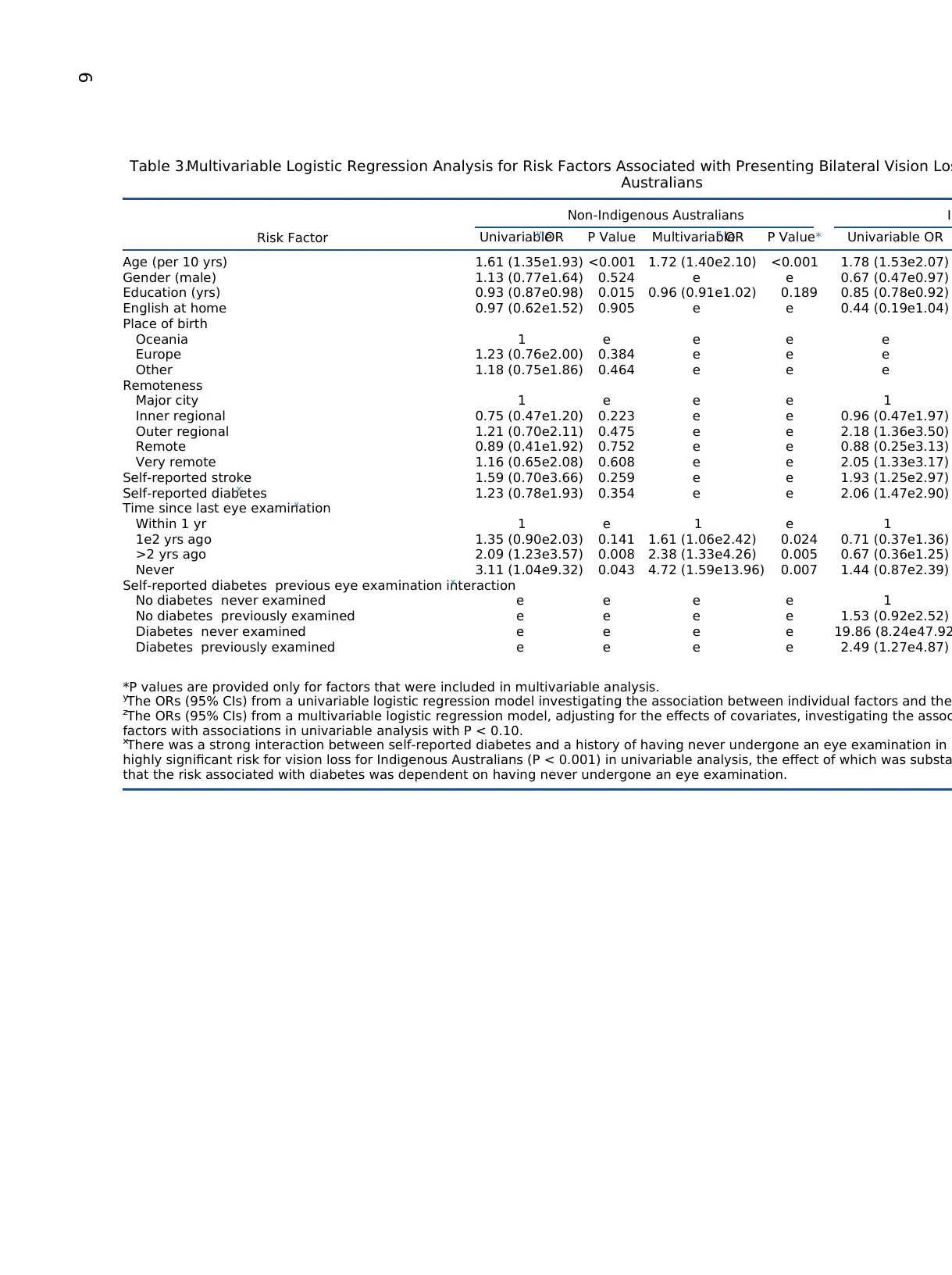
Table 3.Multivariable Logistic Regression Analysis for Risk Factors Associated with Presenting Bilateral Vision Los
Australians
Risk Factor
Non-Indigenous Australians In
Univariabley OR P Value Multivariablez OR P Value* Univariable OR
Age (per 10 yrs) 1.61 (1.35e1.93) <0.001 1.72 (1.40e2.10) <0.001 1.78 (1.53e2.07)
Gender (male) 1.13 (0.77e1.64) 0.524 e e 0.67 (0.47e0.97)
Education (yrs) 0.93 (0.87e0.98) 0.015 0.96 (0.91e1.02) 0.189 0.85 (0.78e0.92)
English at home 0.97 (0.62e1.52) 0.905 e e 0.44 (0.19e1.04)
Place of birth
Oceania 1 e e e e
Europe 1.23 (0.76e2.00) 0.384 e e e
Other 1.18 (0.75e1.86) 0.464 e e e
Remoteness
Major city 1 e e e 1
Inner regional 0.75 (0.47e1.20) 0.223 e e 0.96 (0.47e1.97)
Outer regional 1.21 (0.70e2.11) 0.475 e e 2.18 (1.36e3.50)
Remote 0.89 (0.41e1.92) 0.752 e e 0.88 (0.25e3.13)
Very remote 1.16 (0.65e2.08) 0.608 e e 2.05 (1.33e3.17)
Self-reported stroke 1.59 (0.70e3.66) 0.259 e e 1.93 (1.25e2.97)
Self-reported diabetesx 1.23 (0.78e1.93) 0.354 e e 2.06 (1.47e2.90)
Time since last eye examinationx
Within 1 yr 1 e 1 e 1
1e2 yrs ago 1.35 (0.90e2.03) 0.141 1.61 (1.06e2.42) 0.024 0.71 (0.37e1.36)
>2 yrs ago 2.09 (1.23e3.57) 0.008 2.38 (1.33e4.26) 0.005 0.67 (0.36e1.25)
Never 3.11 (1.04e9.32) 0.043 4.72 (1.59e13.96) 0.007 1.44 (0.87e2.39)
Self-reported diabetes previous eye examination interactionx
No diabetes never examined e e e e 1
No diabetes previously examined e e e e 1.53 (0.92e2.52)
Diabetes never examined e e e e 19.86 (8.24e47.92
Diabetes previously examined e e e e 2.49 (1.27e4.87)
*P values are provided only for factors that were included in multivariable analysis.
yThe ORs (95% CIs) from a univariable logistic regression model investigating the association between individual factors and the
zThe ORs (95% CIs) from a multivariable logistic regression model, adjusting for the effects of covariates, investigating the assoc
factors with associations in univariable analysis with P < 0.10.
xThere was a strong interaction between self-reported diabetes and a history of having never undergone an eye examination in I
highly significant risk for vision loss for Indigenous Australians (P < 0.001) in univariable analysis, the effect of which was substa
that the risk associated with diabetes was dependent on having never undergone an eye examination.
6
Australians
Risk Factor
Non-Indigenous Australians In
Univariabley OR P Value Multivariablez OR P Value* Univariable OR
Age (per 10 yrs) 1.61 (1.35e1.93) <0.001 1.72 (1.40e2.10) <0.001 1.78 (1.53e2.07)
Gender (male) 1.13 (0.77e1.64) 0.524 e e 0.67 (0.47e0.97)
Education (yrs) 0.93 (0.87e0.98) 0.015 0.96 (0.91e1.02) 0.189 0.85 (0.78e0.92)
English at home 0.97 (0.62e1.52) 0.905 e e 0.44 (0.19e1.04)
Place of birth
Oceania 1 e e e e
Europe 1.23 (0.76e2.00) 0.384 e e e
Other 1.18 (0.75e1.86) 0.464 e e e
Remoteness
Major city 1 e e e 1
Inner regional 0.75 (0.47e1.20) 0.223 e e 0.96 (0.47e1.97)
Outer regional 1.21 (0.70e2.11) 0.475 e e 2.18 (1.36e3.50)
Remote 0.89 (0.41e1.92) 0.752 e e 0.88 (0.25e3.13)
Very remote 1.16 (0.65e2.08) 0.608 e e 2.05 (1.33e3.17)
Self-reported stroke 1.59 (0.70e3.66) 0.259 e e 1.93 (1.25e2.97)
Self-reported diabetesx 1.23 (0.78e1.93) 0.354 e e 2.06 (1.47e2.90)
Time since last eye examinationx
Within 1 yr 1 e 1 e 1
1e2 yrs ago 1.35 (0.90e2.03) 0.141 1.61 (1.06e2.42) 0.024 0.71 (0.37e1.36)
>2 yrs ago 2.09 (1.23e3.57) 0.008 2.38 (1.33e4.26) 0.005 0.67 (0.36e1.25)
Never 3.11 (1.04e9.32) 0.043 4.72 (1.59e13.96) 0.007 1.44 (0.87e2.39)
Self-reported diabetes previous eye examination interactionx
No diabetes never examined e e e e 1
No diabetes previously examined e e e e 1.53 (0.92e2.52)
Diabetes never examined e e e e 19.86 (8.24e47.92
Diabetes previously examined e e e e 2.49 (1.27e4.87)
*P values are provided only for factors that were included in multivariable analysis.
yThe ORs (95% CIs) from a univariable logistic regression model investigating the association between individual factors and the
zThe ORs (95% CIs) from a multivariable logistic regression model, adjusting for the effects of covariates, investigating the assoc
factors with associations in univariable analysis with P < 0.10.
xThere was a strong interaction between self-reported diabetes and a history of having never undergone an eye examination in I
highly significant risk for vision loss for Indigenous Australians (P < 0.001) in univariable analysis, the effect of which was substa
that the risk associated with diabetes was dependent on having never undergone an eye examination.
6
Previously,the bestestimate of the prevalence of vision
loss in Australia’s older population of 5.2% was derived from
the pooled prevalencedatafrom theMelbourneVisual
Impairment Project and the Blue Mountains Eye Study con-
ducted in 1992e1994.43 These surveys were limited in their
geographic coverage,selecting samplesfrom the state of
Victoria and a communitynear Sydney,respectively.
Therefore,the estimates of these studies were representative
of these populationsand could not be confidently
extrapolated to the wider Australian population. Furthermore,
temporalchanges in parameters including population aging
and growth, and a higher prevalence of diabetes risk factors,
have necessitatedupdatedprevalenceestimates.The
prevalence of 6.5% reported in the current study is based on
nationally representative data and should be considered the
mostaccurate estimate ofthe prevalence ofvision loss in
Australia’s non-Indigenous population.Estimates from this
study will be useful for informing future national eye health
policies and may function as the baseline to measure the
progress of future interventions. Of particular relevance is the
association between the increased risk of vision loss and older
age in non-Indigenous participants,with the prevalence of
vision loss more than tripling from ages 60e69 years to 80e89
years.Vision loss also was associated with notundergoing
regular eye examinations reflecting a missed opportunity to
identify and remediate leading causes of vision loss, such as
uncorrected refractiveerrorand cataract.Thesefindings,
considered in lightof the factthatAustralia’s population is
aging rapidly, emphasize the need for individuals to undergo
more regular eye examinations as they age to ensure that the
prevalence of vision loss does not increase in coming decades.
The weighted prevalence ofvision lossof 11.2% for
Indigenous Australians in the NEHS was slightly higher than
thatof the NationalInstitute of EnvironmentalHealth Ser-
vices (10.4%); however, this may be due to the older mean
age of our Indigenouscohort(55 vs. 51 years).More
importantly,the prevalence ofvision losswashigherin
IndigenousAustralianscomparedwith non-Indigenous
Australians residing in all geographic remoteness strata a
in all age groups measured in this study.This underlines
systematic insufficiencies in the delivery of required eye
services to Indigenous communities.51The gap in Indigenous
eye health has been wellestablished,and the Roadmap to
Close the Gap forVision providesa framework forthe
improvementof eye care services.52,53This survey identi-
fied numerousrisk factorsfor vision lossin Indigenous
Australians. The finding that the prevalence of vision loss
Indigenous women was 1.4 times higher than in Indigeno
men highlights the need for further investigation into this
gender disparity and an urgent need to provide equitable
health care to all Indigenous Australians.
The finding that uncorrected refractive error and catar
both reversible, were the main causes of vision loss in bo
Indigenous (81%) and non-Indigenous (75%) participants
reflected in previousAustralian research.24,38,54,55
These
conditions remain the leading causes ofvision loss fora
multitude of reasons that are likely to differ between Indi
nous and non-Indigenous Australians and across different
regions in Australia. For example, the prohibitive distance
spectacle-dispensing services and cataract surgery facilit
coupled with the lack of outreach services, have resulted
insufficientand inequitabletreatmentcoveragefor both
conditions.56 Furthermore,the continuallyincreasing
incidence ofcataract57 and long cataractsurgery waiting
times58 may be further hindering efforts to reduce disease
burden,whereassuboptimalcoordinationof spectacle-
dispensingservices,cost uncertainty,and affordability
particularly for Indigenous Australians51 may contribute to
inadequatetreatmentof refractiveerror.Perhapsmost
importantly, insufficient eye examination frequency in old
Australians may result in a lack of detection and correctio
of refractive error.Consequently,by implementing a well-
coordinated nationwide needs-based strategy thataddresses
thesedeficitswhile increasing eyehealth promotion to
Figure 1.The weighted main causes of vision loss (presenting bilateral distance visual acuity <6/12) in Indigenous and non-Indigenous pa
are the proportion (%; 95% confidence interval [CI]) of vision loss attributed to each main cause. Values are adjusted for sampling weigh
uncorrected or undercorrected refractive error.Combined mechanisms were assigned ifthere were 2 causes ofvision loss.Other causes ofvision loss
included retinal dystrophy, optic atrophy, retinochoroidal scarring,retinitis pigmentosa,myopic retinochoroidal degeneration,and keratoconus.
Foreman et alPrevalence of Vision Loss in Australia
7
loss in Australia’s older population of 5.2% was derived from
the pooled prevalencedatafrom theMelbourneVisual
Impairment Project and the Blue Mountains Eye Study con-
ducted in 1992e1994.43 These surveys were limited in their
geographic coverage,selecting samplesfrom the state of
Victoria and a communitynear Sydney,respectively.
Therefore,the estimates of these studies were representative
of these populationsand could not be confidently
extrapolated to the wider Australian population. Furthermore,
temporalchanges in parameters including population aging
and growth, and a higher prevalence of diabetes risk factors,
have necessitatedupdatedprevalenceestimates.The
prevalence of 6.5% reported in the current study is based on
nationally representative data and should be considered the
mostaccurate estimate ofthe prevalence ofvision loss in
Australia’s non-Indigenous population.Estimates from this
study will be useful for informing future national eye health
policies and may function as the baseline to measure the
progress of future interventions. Of particular relevance is the
association between the increased risk of vision loss and older
age in non-Indigenous participants,with the prevalence of
vision loss more than tripling from ages 60e69 years to 80e89
years.Vision loss also was associated with notundergoing
regular eye examinations reflecting a missed opportunity to
identify and remediate leading causes of vision loss, such as
uncorrected refractiveerrorand cataract.Thesefindings,
considered in lightof the factthatAustralia’s population is
aging rapidly, emphasize the need for individuals to undergo
more regular eye examinations as they age to ensure that the
prevalence of vision loss does not increase in coming decades.
The weighted prevalence ofvision lossof 11.2% for
Indigenous Australians in the NEHS was slightly higher than
thatof the NationalInstitute of EnvironmentalHealth Ser-
vices (10.4%); however, this may be due to the older mean
age of our Indigenouscohort(55 vs. 51 years).More
importantly,the prevalence ofvision losswashigherin
IndigenousAustralianscomparedwith non-Indigenous
Australians residing in all geographic remoteness strata a
in all age groups measured in this study.This underlines
systematic insufficiencies in the delivery of required eye
services to Indigenous communities.51The gap in Indigenous
eye health has been wellestablished,and the Roadmap to
Close the Gap forVision providesa framework forthe
improvementof eye care services.52,53This survey identi-
fied numerousrisk factorsfor vision lossin Indigenous
Australians. The finding that the prevalence of vision loss
Indigenous women was 1.4 times higher than in Indigeno
men highlights the need for further investigation into this
gender disparity and an urgent need to provide equitable
health care to all Indigenous Australians.
The finding that uncorrected refractive error and catar
both reversible, were the main causes of vision loss in bo
Indigenous (81%) and non-Indigenous (75%) participants
reflected in previousAustralian research.24,38,54,55
These
conditions remain the leading causes ofvision loss fora
multitude of reasons that are likely to differ between Indi
nous and non-Indigenous Australians and across different
regions in Australia. For example, the prohibitive distance
spectacle-dispensing services and cataract surgery facilit
coupled with the lack of outreach services, have resulted
insufficientand inequitabletreatmentcoveragefor both
conditions.56 Furthermore,the continuallyincreasing
incidence ofcataract57 and long cataractsurgery waiting
times58 may be further hindering efforts to reduce disease
burden,whereassuboptimalcoordinationof spectacle-
dispensingservices,cost uncertainty,and affordability
particularly for Indigenous Australians51 may contribute to
inadequatetreatmentof refractiveerror.Perhapsmost
importantly, insufficient eye examination frequency in old
Australians may result in a lack of detection and correctio
of refractive error.Consequently,by implementing a well-
coordinated nationwide needs-based strategy thataddresses
thesedeficitswhile increasing eyehealth promotion to
Figure 1.The weighted main causes of vision loss (presenting bilateral distance visual acuity <6/12) in Indigenous and non-Indigenous pa
are the proportion (%; 95% confidence interval [CI]) of vision loss attributed to each main cause. Values are adjusted for sampling weigh
uncorrected or undercorrected refractive error.Combined mechanisms were assigned ifthere were 2 causes ofvision loss.Other causes ofvision loss
included retinal dystrophy, optic atrophy, retinochoroidal scarring,retinitis pigmentosa,myopic retinochoroidal degeneration,and keratoconus.
Foreman et alPrevalence of Vision Loss in Australia
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

improve service use, Australia would successfully supersede
its commitment to the Global Action Plan.
Diabetic retinopathy contributed to 5.2% of vision loss in
Indigenous participants, but less than 1.5% of vision loss in
non-Indigenous participants.This reflects the substantially
higherprevalence ofself-reported diabetes in Indigenous
participants (37.1% vs. 13.9%) and the higher prevalence of
advanced vision-threatening diabetic retinopathy in Indige-
nous Australians that has been attributed to insufficient use
of early detection and treatmentservices.59 Implementing
strategiesto targetrisk factorsfor diabeticretinopathy,
including glycemic,lipid, and blood pressure controlin
Indigenouscommunities,while also enhancing screening
services (supported by the strong association with vision
loss in those who had diabetes and had never had an eye
examination [OR,14.47])may contribute to reducing the
burden of vision loss in Indigenous Australians.52
As the leading cause of blindness (71%) and one of the
leading causes of vision impairmentin Australia and other
high income countries, the burden of AMD as a public health
concern is likely to increase with the aging of the popula-
tion.60 Because the vision loss induced by AMD is largely
irreversible,early detection,treatment,and education on
prevention are critical in slowing disease progression.
Many nationaleye health surveyshaveused Rapid
Assessmentof Avoidable Blindness,Rapid Assessmentof
CataractSurgicalServicesor similarmethodologies.61,62
The strengthsof thesestudy designsare theirrelative
inexpensivenessand thatthey usemultistagesampling
frames,while permitting rapid identification ofobvious
ocular disease.However,their practicalutility is hindered
by a number of weaknesses, including simplified ophthalmic
examinations(often consistingof only slit-lampand
ophthalmoscopy,thereby limiting disease attribution)and
rigid nonstratified sampling methods that do not account for
heterogeneous populations.
Population-based eyesurveysthathaveimplemented
some levelof stratification,howevercrude,have consis-
tently revealed geographic14,15,18
or ethnic34,63,64
variations.
Therefore,it is likely thatnonstratified surveys may not
adequately identify regions and ethnic groups most in need
of improvements in eye healthcare services.Through our
stratifiedsamplingmethodology,in which we have
collectedlarge samplesof both Indigenousand non-
Indigenousparticipantsfrom all levels of geographic
remoteness,we have shown thatthe Indigenous people of
Australia, particularly those living in nonmetropolitan areas,
have a substantially higher risk for vision loss.These find-
ings will strengthen national programs aiming to reduce the
burden of vision loss by assisting policymakers and health
providers to allocate limited resources to communities most
in need.52 On the basis of our findings,future population-
based surveys may benefitfrom using similar stratification
methods to identify and investigate Indigenous groups in
countries with defined Indigenous populations.
Study Limitations
A limitation of this study resulted from Australia’s unique
geographic and population structures, including its unusually
low population density.65A systematic protocol was used to
reducethe risk of bias when selecting new population
clusters imposed by prohibitively low population densitie
high absentee rates, and erroneous census data. Noneth
the completeelimination ofboth nonresponsebias and
selection bias could not be achieved because nonrespond
and absentees may have differed from responders in way
relevantto study outcomes.An additionallimitation is that
the sample size was calculated to detectthe prevalence of
vision loss in general,and the study was notpowered to
achieve precision in the estimates ofthe causes ofvision
loss, the prevalence of vision loss by age, or the presuma
much lowerprevalence ofblindness.Future studies may
benefit from having larger samples,but the benefit must be
weighed against the financial and logistic consequences.
In light of the aim to reduce the prevalence of avoidab
vision loss by 25% before the year 2020 under the Globa
Action Plan,there is an urgentneed for more countries to
conductwell-designed nationaleye health surveys to iden-
tify at-risk populations to guide domestic strategies in the
fight against vision loss. In Australia, uncorrected refracti
error and cataract, both reversible, remain the leading ca
of vision loss, highlighting that avoidable vision loss can b
largely addressed by implementing needs-based nationw
strategiesthatimprove ratesof spectacle correction and
cataract surgery.Diabetic retinopathy and AMD contribute
significantly to the burden of vision loss in Australia,and
early detection and treatment are well known to reduce t
burden ofvision lossfrom these conditions.Indigenous
Australians have a high burden of vision loss, and proper
stratifiedsurveysin other countrieswith Indigenous
inhabitants,or indeed other marginalizedpopulation
subgroups,may reflectthese findings in those populations,
thereby informing targeted interventions to reduce vision
loss in those countries.
Acknowledgments.The CERA and Vision 2020 Australia
recognize the contributions ofall of the NEHS projectsteering
committee members (Professor Hugh Taylor,Dr. Peter van Wijn-
gaarden,JenniferGersbeck,Dr. Jason Agostino,Anna Morse,
Sharon Bentley,Robyn Weinberg,Christine Black,Genevieve
Quilty,Louis Young,and Rhonda Stilling)and the core CERA
research team who assisted with the survey field work (PeiYing
Lee,Rosamond Gilden,Larissa Andersen,Benny Phanthakesone,
Celestina Pham, Alison Schokman, Megan Jackson, Hiba Wehbe
John Komser,and Cayley Bush).The authors also acknowledge
the overwhelmingsupportfrom all collaboratingIndigenous
organizations thatassisted with the implementation of the survey
and the Indigenous health workers and volunteers in each surv
site who contributed to the field work.
References
1. Stevens GA, White RA, Flaxman SR, et al. Global prevalence
of vision impairmentand blindness:magnitude and temporal
trends,1990-2010.Ophthalmology.2013;120:2377-2384.
2. PascoliniD, MariottiSP. Globalestimates of visualimpair-
ment: 2010.Br J Ophthalmol.2012;96:614-618.
3. World Health Organization.UniversalEye Health: A Global
Action Plan 2014-2019.Geneva,Switzerland:World Health
Organization; 2013.
OphthalmologyVolume- , Number- , Month 2017
8
its commitment to the Global Action Plan.
Diabetic retinopathy contributed to 5.2% of vision loss in
Indigenous participants, but less than 1.5% of vision loss in
non-Indigenous participants.This reflects the substantially
higherprevalence ofself-reported diabetes in Indigenous
participants (37.1% vs. 13.9%) and the higher prevalence of
advanced vision-threatening diabetic retinopathy in Indige-
nous Australians that has been attributed to insufficient use
of early detection and treatmentservices.59 Implementing
strategiesto targetrisk factorsfor diabeticretinopathy,
including glycemic,lipid, and blood pressure controlin
Indigenouscommunities,while also enhancing screening
services (supported by the strong association with vision
loss in those who had diabetes and had never had an eye
examination [OR,14.47])may contribute to reducing the
burden of vision loss in Indigenous Australians.52
As the leading cause of blindness (71%) and one of the
leading causes of vision impairmentin Australia and other
high income countries, the burden of AMD as a public health
concern is likely to increase with the aging of the popula-
tion.60 Because the vision loss induced by AMD is largely
irreversible,early detection,treatment,and education on
prevention are critical in slowing disease progression.
Many nationaleye health surveyshaveused Rapid
Assessmentof Avoidable Blindness,Rapid Assessmentof
CataractSurgicalServicesor similarmethodologies.61,62
The strengthsof thesestudy designsare theirrelative
inexpensivenessand thatthey usemultistagesampling
frames,while permitting rapid identification ofobvious
ocular disease.However,their practicalutility is hindered
by a number of weaknesses, including simplified ophthalmic
examinations(often consistingof only slit-lampand
ophthalmoscopy,thereby limiting disease attribution)and
rigid nonstratified sampling methods that do not account for
heterogeneous populations.
Population-based eyesurveysthathaveimplemented
some levelof stratification,howevercrude,have consis-
tently revealed geographic14,15,18
or ethnic34,63,64
variations.
Therefore,it is likely thatnonstratified surveys may not
adequately identify regions and ethnic groups most in need
of improvements in eye healthcare services.Through our
stratifiedsamplingmethodology,in which we have
collectedlarge samplesof both Indigenousand non-
Indigenousparticipantsfrom all levels of geographic
remoteness,we have shown thatthe Indigenous people of
Australia, particularly those living in nonmetropolitan areas,
have a substantially higher risk for vision loss.These find-
ings will strengthen national programs aiming to reduce the
burden of vision loss by assisting policymakers and health
providers to allocate limited resources to communities most
in need.52 On the basis of our findings,future population-
based surveys may benefitfrom using similar stratification
methods to identify and investigate Indigenous groups in
countries with defined Indigenous populations.
Study Limitations
A limitation of this study resulted from Australia’s unique
geographic and population structures, including its unusually
low population density.65A systematic protocol was used to
reducethe risk of bias when selecting new population
clusters imposed by prohibitively low population densitie
high absentee rates, and erroneous census data. Noneth
the completeelimination ofboth nonresponsebias and
selection bias could not be achieved because nonrespond
and absentees may have differed from responders in way
relevantto study outcomes.An additionallimitation is that
the sample size was calculated to detectthe prevalence of
vision loss in general,and the study was notpowered to
achieve precision in the estimates ofthe causes ofvision
loss, the prevalence of vision loss by age, or the presuma
much lowerprevalence ofblindness.Future studies may
benefit from having larger samples,but the benefit must be
weighed against the financial and logistic consequences.
In light of the aim to reduce the prevalence of avoidab
vision loss by 25% before the year 2020 under the Globa
Action Plan,there is an urgentneed for more countries to
conductwell-designed nationaleye health surveys to iden-
tify at-risk populations to guide domestic strategies in the
fight against vision loss. In Australia, uncorrected refracti
error and cataract, both reversible, remain the leading ca
of vision loss, highlighting that avoidable vision loss can b
largely addressed by implementing needs-based nationw
strategiesthatimprove ratesof spectacle correction and
cataract surgery.Diabetic retinopathy and AMD contribute
significantly to the burden of vision loss in Australia,and
early detection and treatment are well known to reduce t
burden ofvision lossfrom these conditions.Indigenous
Australians have a high burden of vision loss, and proper
stratifiedsurveysin other countrieswith Indigenous
inhabitants,or indeed other marginalizedpopulation
subgroups,may reflectthese findings in those populations,
thereby informing targeted interventions to reduce vision
loss in those countries.
Acknowledgments.The CERA and Vision 2020 Australia
recognize the contributions ofall of the NEHS projectsteering
committee members (Professor Hugh Taylor,Dr. Peter van Wijn-
gaarden,JenniferGersbeck,Dr. Jason Agostino,Anna Morse,
Sharon Bentley,Robyn Weinberg,Christine Black,Genevieve
Quilty,Louis Young,and Rhonda Stilling)and the core CERA
research team who assisted with the survey field work (PeiYing
Lee,Rosamond Gilden,Larissa Andersen,Benny Phanthakesone,
Celestina Pham, Alison Schokman, Megan Jackson, Hiba Wehbe
John Komser,and Cayley Bush).The authors also acknowledge
the overwhelmingsupportfrom all collaboratingIndigenous
organizations thatassisted with the implementation of the survey
and the Indigenous health workers and volunteers in each surv
site who contributed to the field work.
References
1. Stevens GA, White RA, Flaxman SR, et al. Global prevalence
of vision impairmentand blindness:magnitude and temporal
trends,1990-2010.Ophthalmology.2013;120:2377-2384.
2. PascoliniD, MariottiSP. Globalestimates of visualimpair-
ment: 2010.Br J Ophthalmol.2012;96:614-618.
3. World Health Organization.UniversalEye Health: A Global
Action Plan 2014-2019.Geneva,Switzerland:World Health
Organization; 2013.
OphthalmologyVolume- , Number- , Month 2017
8
4. UN PermanentForum on Indigenous Issues.Who are indig-
enous peoples? Available at:http://www.un.org/en/ga/search/
view_doc.asp?symbol¼E/2016/43&referer¼http://www.un.
org/en/documents/index.html&Lang¼E.Accessed October
31,2016.
5. United Nations. State of the World’s Indigenous Peoples. New
York: United Nations Departmentof Economic and Social
Affairs,Division for SocialPolicy and Development,Secre-
tariat of the Permanent Forum on Indigenous Issues; 2009.
6. Anderson I,Robson B,Connolly M,et al. Indigenous and
tribalpeoples’health (The Lancet-Lowitja Institute Global
Collaboration): a population study. Lancet. 2016;388:131-157.
7. Gracey M, King M. Indigenous health part 1: determinants and
disease patterns.Lancet.2009;374:65-75.
8. Ulldemolins AR,Lansingh VC,Valencia LG,et al. Social
inequalities in blindness and visualimpairment:a review of
social determinants.Indian J Ophthalmol.2012;60:368-375.
9. Bourne RR,Dineen B,Modasser AliS, et al. The National
Blindness and Low Vision Prevalence Survey of Bangladesh:
research design,eye examination methodology and results of
the pilot study.Ophthalmic Epidemiol.2002;9:119-132.
10. Lepcha NT, Chettri CK, Getshen K, et al. Rapid assessment of
avoidableblindnessin Bhutan.OphthalmicEpidemiol.
2013;20:212-219.
11. Schemann JF,Inocencio F,de Lourdes Monteiro M,et al.
Blindness and low vision in Cape Verde Islands:results of a
national eye survey. Ophthalmic Epidemiol. 2006;13:219-226.
12. Laitinen A,Koskinen S,Harkanen T,et al. A nationwide
population-based survey on visual acuity, near vision, and self-
reported visualfunction in the adultpopulation in Finland.
Ophthalmology.2005;112:2227-2237.
13. Nicolosi A, Marighi PE, Rizzardi P, et al. Prevalence and causes
of visual impairment in Italy. Int J Epidemiol. 1994;23:359-364.
14. Rabiu MM,Jenf M,FituriS, etal. Prevalence and causes of
visualimpairmentand blindness,cataractsurgicalcoverage
and outcomes of cataractsurgery in Libya.Ophthalmic Epi-
demiol.2013;20:26-32.
15. Zatic T,Bendelic E,Paduca A,et al. Rapid assessmentof
avoidable blindness and diabetic retinopathy in Republic of
Moldova.Br J Ophthalmol.2015;99:832-836.
16. Baasanhu J,Johnson GJ,BurendeiG, Minassian DC.Preva-
lenceand causesof blindnessand visualimpairmentin
Mongolia:a survey of populations aged 40 years and older.
Bull World Health Organ.1994;72:771-776.
17. Kyari F, GudlavalletiMV, Sivsubramaniam S,et al. Preva-
lenceof blindnessand visualimpairmentin Nigeria:the
NationalBlindnessand Visual ImpairmentStudy.Invest
Ophthalmol Vis Sci.2009;50:2033-2039.
18. Dineen B,Bourne RR,Jadoon Z,etal. Causes of blindness
and visualimpairmentin Pakistan.The Pakistan national
blindnessand visualimpairmentsurvey.Br J Ophthalmol.
2007;91:1005-1010.
19. Duerksen R,Limburg H, Carron JE, FosterA. Cataract
blindnessin Paraguayeresultsof a national survey.
Ophthalmic Epidemiol.2003;10:349-357.
20. Cubillan LDP,Olivar-Santos EO.Third nationalsurvey on
blindness.Philipp J Ophthalmol.2005;30:100-114.
21. IsipraditS, SirimaharajM, Charukamnoetkanok P,etal.The
first rapid assessmentof avoidableblindness(RAAB) in
Thailand.PLoS One.2014;9:e114245.
22. Faal H, Minassian DC, Dolin PJ, et al. Evaluation of a national
eye care programme: re-survey after 10 years. Br J Ophthalmol.
2000;84:948-951.
23. Taylor HR.Prevalence and causes of blindness in Australian
aborigines.Med J Aust.1980;1:71-76.
24. Taylor HR,Xie J, Fox S,et al.The prevalence and causes of
vision loss in Indigenous Australians: the National Indigenou
Eye Health Survey.Med J Aust.2010;192:312-318.
25. Paula JS,Thorn F,Cruz AA. Prevalence ofpterygium and
cataractin indigenous populations ofthe Brazilian Amazon
rain forest.Eye (Lond).2006;20:533-536.
26. Thorn F,Cruz AA, Machado AJ,Carvalho RA.Refractive
status of indigenous people in the northwestern Amazon re
gion of Brazil.Optom Vis Sci.2005;82:267-272.
27. Lee ET, Russell D, Morris T, et al. Visual impairment and eye
abnormalitiesin OklahomaIndians. Arch Ophthalmol.
2005;123:1699-1704.
28. MansbergerSL, Romero FC,Smith NH,et al. Causesof
visualimpairmentand common eye problems in Northwest
American Indians and Alaska Natives.Am J Public Health.
2005;95:881-886.
29. Jimenez JR,Bermudez J,Rubino M, et al. Prevalence of
myopia in an adult population of two different ethnic group
the Ecuadorian Amazon. Jpn J Ophthalmol. 2004;48:163-165
30. Alves AP,Medina NH,Cruz AA. Trachoma and ethnic di-
versity in the UpperRio Negro Basin ofAmazonas State,
Brazil.Ophthalmic Epidemiol.2002;9:29-34.
31. Arkell SM, Lightman DA, Sommer A, et al. The prevalence o
glaucoma among Eskimos ofnorthwestAlaska.Arch Oph-
thalmol.1987;105:482-485.
32. PaulaJS, MedinaNH, Cruz AA. Trachomaamongthe
Yanomami Indians. Braz J Med Biol Res. 2002;35:1153-1157
33. Landers J,Henderson T,Craig J. CentralAustralian Ocular
Health Study: design and baseline description of participant
Clin Exp Ophthalmol.2010;38:375-380.
34. ZainalM, Ismail SM, Ropilah AR, et al. Prevalenceof
blindnessand low vision in Malaysian population:results
from the NationalEye Survey1996.Br J Ophthalmol.
2002;86:951-956.
35. Landers J, Henderson T, Craig J. The prevalence and causes
visualimpairmentin indigenousAustralianswithin central
Australia:the CentralAustralian OcularHealth Study.Br J
Ophthalmol.2010;94:1140-1144.
36. Landers J, Henderson T,Craig J.Prevalence and associations
of blinding trachoma in indigenous Australians within centra
Australia:the CentralAustralian OcularHealth Study.Clin
Exp Ophthalmol.2010;38:398-404.
37. Landers J,Henderson T,Craig J.Prevalence of pterygium in
indigenous Australians within centralAustralia:the Central
AustralianOcular Health Study. Clin Exp Ophthalmol.
2011;39:604-606.
38. VanNewkirk MR,Weih L,McCarty CA,Taylor HR.Cause-
specific prevalence of bilateralvisual impairmentin Victoria,
Australia:the Visual ImpairmentProject.Ophthalmology.
2001;108:960-967.
39. Wang JJ, Foran S,MitchellP. Age-specific prevalence and
causes ofbilateraland unilateralvisualimpairmentin older
Australians:the Blue MountainsEye Study. Clin Exp
Ophthalmol.2000;28:268-273.
40. Newland HS, Hiller JE, Casson RJ, Obermeder S. Prevalence
and causes ofblindness in the South Australian population
aged 50 and over.Ophthalmic Epidemiol.1996;3:97-107.
41. Foreman J, Keel S, Dunn R, et al. Sampling methodology an
site selection in the NationalEye Health Survey (NEHS):an
Australian population-based prevalence study.Clin Exp Oph-
thalmol.2017;45:336-347.
42. Australian Institute ofHealth and Welfare.Vision Problems
Among Older Australians.Bulletin No.27.AIHW Cat.No.
AUS 60. Canberra: Australian Institute of Health and Welfar
2005.
Foreman et alPrevalence of Vision Loss in Australia
9
enous peoples? Available at:http://www.un.org/en/ga/search/
view_doc.asp?symbol¼E/2016/43&referer¼http://www.un.
org/en/documents/index.html&Lang¼E.Accessed October
31,2016.
5. United Nations. State of the World’s Indigenous Peoples. New
York: United Nations Departmentof Economic and Social
Affairs,Division for SocialPolicy and Development,Secre-
tariat of the Permanent Forum on Indigenous Issues; 2009.
6. Anderson I,Robson B,Connolly M,et al. Indigenous and
tribalpeoples’health (The Lancet-Lowitja Institute Global
Collaboration): a population study. Lancet. 2016;388:131-157.
7. Gracey M, King M. Indigenous health part 1: determinants and
disease patterns.Lancet.2009;374:65-75.
8. Ulldemolins AR,Lansingh VC,Valencia LG,et al. Social
inequalities in blindness and visualimpairment:a review of
social determinants.Indian J Ophthalmol.2012;60:368-375.
9. Bourne RR,Dineen B,Modasser AliS, et al. The National
Blindness and Low Vision Prevalence Survey of Bangladesh:
research design,eye examination methodology and results of
the pilot study.Ophthalmic Epidemiol.2002;9:119-132.
10. Lepcha NT, Chettri CK, Getshen K, et al. Rapid assessment of
avoidableblindnessin Bhutan.OphthalmicEpidemiol.
2013;20:212-219.
11. Schemann JF,Inocencio F,de Lourdes Monteiro M,et al.
Blindness and low vision in Cape Verde Islands:results of a
national eye survey. Ophthalmic Epidemiol. 2006;13:219-226.
12. Laitinen A,Koskinen S,Harkanen T,et al. A nationwide
population-based survey on visual acuity, near vision, and self-
reported visualfunction in the adultpopulation in Finland.
Ophthalmology.2005;112:2227-2237.
13. Nicolosi A, Marighi PE, Rizzardi P, et al. Prevalence and causes
of visual impairment in Italy. Int J Epidemiol. 1994;23:359-364.
14. Rabiu MM,Jenf M,FituriS, etal. Prevalence and causes of
visualimpairmentand blindness,cataractsurgicalcoverage
and outcomes of cataractsurgery in Libya.Ophthalmic Epi-
demiol.2013;20:26-32.
15. Zatic T,Bendelic E,Paduca A,et al. Rapid assessmentof
avoidable blindness and diabetic retinopathy in Republic of
Moldova.Br J Ophthalmol.2015;99:832-836.
16. Baasanhu J,Johnson GJ,BurendeiG, Minassian DC.Preva-
lenceand causesof blindnessand visualimpairmentin
Mongolia:a survey of populations aged 40 years and older.
Bull World Health Organ.1994;72:771-776.
17. Kyari F, GudlavalletiMV, Sivsubramaniam S,et al. Preva-
lenceof blindnessand visualimpairmentin Nigeria:the
NationalBlindnessand Visual ImpairmentStudy.Invest
Ophthalmol Vis Sci.2009;50:2033-2039.
18. Dineen B,Bourne RR,Jadoon Z,etal. Causes of blindness
and visualimpairmentin Pakistan.The Pakistan national
blindnessand visualimpairmentsurvey.Br J Ophthalmol.
2007;91:1005-1010.
19. Duerksen R,Limburg H, Carron JE, FosterA. Cataract
blindnessin Paraguayeresultsof a national survey.
Ophthalmic Epidemiol.2003;10:349-357.
20. Cubillan LDP,Olivar-Santos EO.Third nationalsurvey on
blindness.Philipp J Ophthalmol.2005;30:100-114.
21. IsipraditS, SirimaharajM, Charukamnoetkanok P,etal.The
first rapid assessmentof avoidableblindness(RAAB) in
Thailand.PLoS One.2014;9:e114245.
22. Faal H, Minassian DC, Dolin PJ, et al. Evaluation of a national
eye care programme: re-survey after 10 years. Br J Ophthalmol.
2000;84:948-951.
23. Taylor HR.Prevalence and causes of blindness in Australian
aborigines.Med J Aust.1980;1:71-76.
24. Taylor HR,Xie J, Fox S,et al.The prevalence and causes of
vision loss in Indigenous Australians: the National Indigenou
Eye Health Survey.Med J Aust.2010;192:312-318.
25. Paula JS,Thorn F,Cruz AA. Prevalence ofpterygium and
cataractin indigenous populations ofthe Brazilian Amazon
rain forest.Eye (Lond).2006;20:533-536.
26. Thorn F,Cruz AA, Machado AJ,Carvalho RA.Refractive
status of indigenous people in the northwestern Amazon re
gion of Brazil.Optom Vis Sci.2005;82:267-272.
27. Lee ET, Russell D, Morris T, et al. Visual impairment and eye
abnormalitiesin OklahomaIndians. Arch Ophthalmol.
2005;123:1699-1704.
28. MansbergerSL, Romero FC,Smith NH,et al. Causesof
visualimpairmentand common eye problems in Northwest
American Indians and Alaska Natives.Am J Public Health.
2005;95:881-886.
29. Jimenez JR,Bermudez J,Rubino M, et al. Prevalence of
myopia in an adult population of two different ethnic group
the Ecuadorian Amazon. Jpn J Ophthalmol. 2004;48:163-165
30. Alves AP,Medina NH,Cruz AA. Trachoma and ethnic di-
versity in the UpperRio Negro Basin ofAmazonas State,
Brazil.Ophthalmic Epidemiol.2002;9:29-34.
31. Arkell SM, Lightman DA, Sommer A, et al. The prevalence o
glaucoma among Eskimos ofnorthwestAlaska.Arch Oph-
thalmol.1987;105:482-485.
32. PaulaJS, MedinaNH, Cruz AA. Trachomaamongthe
Yanomami Indians. Braz J Med Biol Res. 2002;35:1153-1157
33. Landers J,Henderson T,Craig J. CentralAustralian Ocular
Health Study: design and baseline description of participant
Clin Exp Ophthalmol.2010;38:375-380.
34. ZainalM, Ismail SM, Ropilah AR, et al. Prevalenceof
blindnessand low vision in Malaysian population:results
from the NationalEye Survey1996.Br J Ophthalmol.
2002;86:951-956.
35. Landers J, Henderson T, Craig J. The prevalence and causes
visualimpairmentin indigenousAustralianswithin central
Australia:the CentralAustralian OcularHealth Study.Br J
Ophthalmol.2010;94:1140-1144.
36. Landers J, Henderson T,Craig J.Prevalence and associations
of blinding trachoma in indigenous Australians within centra
Australia:the CentralAustralian OcularHealth Study.Clin
Exp Ophthalmol.2010;38:398-404.
37. Landers J,Henderson T,Craig J.Prevalence of pterygium in
indigenous Australians within centralAustralia:the Central
AustralianOcular Health Study. Clin Exp Ophthalmol.
2011;39:604-606.
38. VanNewkirk MR,Weih L,McCarty CA,Taylor HR.Cause-
specific prevalence of bilateralvisual impairmentin Victoria,
Australia:the Visual ImpairmentProject.Ophthalmology.
2001;108:960-967.
39. Wang JJ, Foran S,MitchellP. Age-specific prevalence and
causes ofbilateraland unilateralvisualimpairmentin older
Australians:the Blue MountainsEye Study. Clin Exp
Ophthalmol.2000;28:268-273.
40. Newland HS, Hiller JE, Casson RJ, Obermeder S. Prevalence
and causes ofblindness in the South Australian population
aged 50 and over.Ophthalmic Epidemiol.1996;3:97-107.
41. Foreman J, Keel S, Dunn R, et al. Sampling methodology an
site selection in the NationalEye Health Survey (NEHS):an
Australian population-based prevalence study.Clin Exp Oph-
thalmol.2017;45:336-347.
42. Australian Institute ofHealth and Welfare.Vision Problems
Among Older Australians.Bulletin No.27.AIHW Cat.No.
AUS 60. Canberra: Australian Institute of Health and Welfar
2005.
Foreman et alPrevalence of Vision Loss in Australia
9
43. Taylor HR, Keeffe JE, Vu HT, et al. Vision loss in Australia.
Med J Aust.2005;182:565-568.
44. Australian Bureau ofStatistics.Australian StatisticalGeog-
raphy Standard (ASGS).Canberra,Australia:Australian Bu-
reau of Statistics; 2014.
45. Foreman J, Keel S, van Wijngaarden P, et al. Recruitment and
testingprotocolin the NationalEye HealthSurvey:a
population-based eyestudy in Australia.OphthalmicEpi-
demiol.2017:1-11.
46. WHO simplified trachoma grading system.Community Eye
Health.2004;17:68.
47. Diabetic Retinopathy Screening.Design,Methods,and Base-
line Results: A Modification of the Airlie House Classification
of DiabeticRetinopathy(DRS Report#7). Investigative
Ophthalmology & Visual Science: Diabetic Retinopathy Study
Research Group.1981; v.21.
48. Van Herick W, Shaffer RN, Schwartz A. Estimation of width
of angle of anterior chamber. Incidence and significance of the
narrow angle.Am J Ophthalmol.1969;68:626-629.
49. Ferris F,Wilkinson C,Bird A,et al.Clinical classification of
age-related macular degeneration.Ophthalmology.2013;120:
844-851.
50. Mukesh B, McCarty C, Rait J,Taylor H. Five-year incidence
of open-angleglaucoma.Ophthalmology.2002;109:1047-
1051.
51. Anjou MD,Boudville AI,Taylor HR.Correcting Indigenous
Australians’refractive errorand presbyopia.Clin Exp Oph-
thalmol.2013;41:320-328.
52. Taylor HR,Boudville AI,Anjou MD.The roadmap to close
the gap for vision.Med J Aust.2012;197:613-615.
53. KelaherM, Ferdinand A,TaylorH. Accessto eye health
services among indigenous Australians: an area level analysis.
BMC Ophthalmol.2012;12:51.
54. Attebo K,Mitchell P,Smith W.Visual acuity and the causes
of visualloss in Australia.The Blue Mountains Eye Study.
Ophthalmology.1996;103:357-364.
55. Landers J,Henderson T,Abhary S,Craig J.Prevalence and
associations of diabetic retinopathy in indigenous Australian
within central Australia: the Central Australian Ocular Healt
Study.Clin Exp Ophthalmol.2010;38:393-397.
56. Kiely PM, Chakman J.Optometricpracticein Australian
Standard GeographicalClassificationeRemotenessAreasin
Australia,2010.Clin Exp Optom.2011;94:468-477.
57. Rochtchina E,Mukesh BN,Wang JJ,etal. Projected preva-
lence of age-related cataract and cataractsurgery in Australia
for the years 2001 and 2021: pooled data from two populat
based surveys.Clin Exp Ophthalmol.2003;31:233-236.
58. Australian Institute of Health and Welfare.Admitted Patient
Care 2013e14: Australian Hospital Statistics. Health Service
Series No. 60 Cat No. HSE 156. Canberra: Australian Institut
of Health and Welfare; 2015.
59. Turner AW, Xie J, Arnold AL, et al. Eye health service access
and utilization in the National Indigenous Eye Health Survey
Clin Exp Ophthalmol.2011;39:598-603.
60. Jonas JB,Bourne RR,White RA,et al. Visualimpairment
and blindness due to maculardiseases globally:a system-
atic review and meta-analysis.Am J Ophthalmol.2014;158:
808-815.
61. Kuper H, Polack S, Limburg H. Rapid assessment of avoidab
blindness.Community Eye Health.2006;19:68-69.
62. World Health Organization.Rapid Assessmentof Cataract
SurgicalServices.Geneva,Switzerland:World Health Orga-
nization; 2001.
63. Ramke J,Brian G,Maher L,etal. Prevalence and causes of
blindnessand low vision among adultsin Fiji. Clin Exp
Ophthalmol.2012;40:490-496.
64. Varma R,Ying-LaiM, Klein R,etal.Prevalence and risk in-
dicators of visual impairment and blindness in Latinos: the L
Angeles Latino Eye Study. Ophthalmology. 2004;111:1132-
65. United Nations Departmentof Economic and SocialAffairs
Population Division.World Population Prospects: The 2015
Revision.New York: United Nations; 2015.
Footnotes and Financial Disclosures
Originally received: February 13,2017.
Final revision: May 31,2017.
Accepted: June 1,2017.
Available online:--- . Manuscript no. 2017-360.
1 Centre forEye Research Australia,The RoyalVictorian Eye & Ear
Hospital, Melbourne, Australia.
2 Ophthalmology,Departmentof Surgery,University of Melbourne,Mel-
bourne, Australia.
3 Vision & Eye Research Unit,Postgraduate MedicalInstitute,Anglia
Ruskin University,Cambridge,United Kingdom.
4 Indigenous Eye Health Unit, Melbourne School of Population and Global
Health,The University of Melbourne,Melbourne,Australia.
Financial Disclosure(s):
The author(s)have made the following disclosure(s):J.F., J.X., S.K.,
P.vW., S.S.S., G.S.A., J.F.G., J.C., and M.D.: Grants and travel support e
Commonwealth Governmentof Australia,Cranbourne Foundation,and
Novartis.
The NEHS was funded by the Departmentof Health ofthe Australian
Governmentand received financialcontributions from Novartis Australia
and in-kind supportfrom ourindustry and sectorpartners:OpticalPre-
scription Spectacle Makers,Carl Zeiss,Designsfor Vision, the Royal
Flying Doctor Service, Optometry Australia,and the Brien Holden Vision
Institute. The authors acknowledge Optical Prescription Spectacle Makers,
who donated sunglasses valued at$130 foreach study participant.The
CERA receivesOperationalInfrastructureSupportfrom theVictorian
Government. The Principal Investigator (M.D.) is supported by a Nationa
Health and MedicalResearch CouncilCareerDevelopmentFellowship
(#1090466).A PhD student(J.F.) is supported by an Australian Post-
graduateAward scholarship.Funded byThe AustralianGovernment
Department of Health, Canberra, Australia, Novartis, Australia, and Pegg
and Leslie Cranbourne Foundation. The funding organizations had no ro
in the design or conduct of this research.
Author Contributions:
Conception and design: Taylor,Dirani,Foreman,Keel,van Wijngaarden,
Crowston
Data collection: Dirani,Foreman, Keel, Sandhu, Ang, Fan Gaskin
Analysis and interpretation: Dirani, Foreman, Xie, Keel, Sandhu, Ang, Fa
Gaskin, Crowston
Obtained funding: Dirani
Overallresponsibility:Bourne,Taylor,Dirani,Foreman,Xie, Keel, van
Wijngaarden,Sandhu, Ang,Fan Gaskin,Crowston
Abbreviations and Acronyms:
AMD ¼ age-related maculardegeneration;CERA ¼ Centre for Eye
Research Australia;CI ¼ confidence interval;NEHS ¼ NationalEye
Health Survey; OR ¼ odds ratio.
Correspondence:
Joshua Foreman, BSc (Hons), Centre for Eye Research Australia, Level 1
32 Gisborne Street,EastMelbourne,Victoria,Australia 3002.E-mail:
foreman.j@unimelb.edu.au.
OphthalmologyVolume- , Number- , Month 2017
10
Med J Aust.2005;182:565-568.
44. Australian Bureau ofStatistics.Australian StatisticalGeog-
raphy Standard (ASGS).Canberra,Australia:Australian Bu-
reau of Statistics; 2014.
45. Foreman J, Keel S, van Wijngaarden P, et al. Recruitment and
testingprotocolin the NationalEye HealthSurvey:a
population-based eyestudy in Australia.OphthalmicEpi-
demiol.2017:1-11.
46. WHO simplified trachoma grading system.Community Eye
Health.2004;17:68.
47. Diabetic Retinopathy Screening.Design,Methods,and Base-
line Results: A Modification of the Airlie House Classification
of DiabeticRetinopathy(DRS Report#7). Investigative
Ophthalmology & Visual Science: Diabetic Retinopathy Study
Research Group.1981; v.21.
48. Van Herick W, Shaffer RN, Schwartz A. Estimation of width
of angle of anterior chamber. Incidence and significance of the
narrow angle.Am J Ophthalmol.1969;68:626-629.
49. Ferris F,Wilkinson C,Bird A,et al.Clinical classification of
age-related macular degeneration.Ophthalmology.2013;120:
844-851.
50. Mukesh B, McCarty C, Rait J,Taylor H. Five-year incidence
of open-angleglaucoma.Ophthalmology.2002;109:1047-
1051.
51. Anjou MD,Boudville AI,Taylor HR.Correcting Indigenous
Australians’refractive errorand presbyopia.Clin Exp Oph-
thalmol.2013;41:320-328.
52. Taylor HR,Boudville AI,Anjou MD.The roadmap to close
the gap for vision.Med J Aust.2012;197:613-615.
53. KelaherM, Ferdinand A,TaylorH. Accessto eye health
services among indigenous Australians: an area level analysis.
BMC Ophthalmol.2012;12:51.
54. Attebo K,Mitchell P,Smith W.Visual acuity and the causes
of visualloss in Australia.The Blue Mountains Eye Study.
Ophthalmology.1996;103:357-364.
55. Landers J,Henderson T,Abhary S,Craig J.Prevalence and
associations of diabetic retinopathy in indigenous Australian
within central Australia: the Central Australian Ocular Healt
Study.Clin Exp Ophthalmol.2010;38:393-397.
56. Kiely PM, Chakman J.Optometricpracticein Australian
Standard GeographicalClassificationeRemotenessAreasin
Australia,2010.Clin Exp Optom.2011;94:468-477.
57. Rochtchina E,Mukesh BN,Wang JJ,etal. Projected preva-
lence of age-related cataract and cataractsurgery in Australia
for the years 2001 and 2021: pooled data from two populat
based surveys.Clin Exp Ophthalmol.2003;31:233-236.
58. Australian Institute of Health and Welfare.Admitted Patient
Care 2013e14: Australian Hospital Statistics. Health Service
Series No. 60 Cat No. HSE 156. Canberra: Australian Institut
of Health and Welfare; 2015.
59. Turner AW, Xie J, Arnold AL, et al. Eye health service access
and utilization in the National Indigenous Eye Health Survey
Clin Exp Ophthalmol.2011;39:598-603.
60. Jonas JB,Bourne RR,White RA,et al. Visualimpairment
and blindness due to maculardiseases globally:a system-
atic review and meta-analysis.Am J Ophthalmol.2014;158:
808-815.
61. Kuper H, Polack S, Limburg H. Rapid assessment of avoidab
blindness.Community Eye Health.2006;19:68-69.
62. World Health Organization.Rapid Assessmentof Cataract
SurgicalServices.Geneva,Switzerland:World Health Orga-
nization; 2001.
63. Ramke J,Brian G,Maher L,etal. Prevalence and causes of
blindnessand low vision among adultsin Fiji. Clin Exp
Ophthalmol.2012;40:490-496.
64. Varma R,Ying-LaiM, Klein R,etal.Prevalence and risk in-
dicators of visual impairment and blindness in Latinos: the L
Angeles Latino Eye Study. Ophthalmology. 2004;111:1132-
65. United Nations Departmentof Economic and SocialAffairs
Population Division.World Population Prospects: The 2015
Revision.New York: United Nations; 2015.
Footnotes and Financial Disclosures
Originally received: February 13,2017.
Final revision: May 31,2017.
Accepted: June 1,2017.
Available online:--- . Manuscript no. 2017-360.
1 Centre forEye Research Australia,The RoyalVictorian Eye & Ear
Hospital, Melbourne, Australia.
2 Ophthalmology,Departmentof Surgery,University of Melbourne,Mel-
bourne, Australia.
3 Vision & Eye Research Unit,Postgraduate MedicalInstitute,Anglia
Ruskin University,Cambridge,United Kingdom.
4 Indigenous Eye Health Unit, Melbourne School of Population and Global
Health,The University of Melbourne,Melbourne,Australia.
Financial Disclosure(s):
The author(s)have made the following disclosure(s):J.F., J.X., S.K.,
P.vW., S.S.S., G.S.A., J.F.G., J.C., and M.D.: Grants and travel support e
Commonwealth Governmentof Australia,Cranbourne Foundation,and
Novartis.
The NEHS was funded by the Departmentof Health ofthe Australian
Governmentand received financialcontributions from Novartis Australia
and in-kind supportfrom ourindustry and sectorpartners:OpticalPre-
scription Spectacle Makers,Carl Zeiss,Designsfor Vision, the Royal
Flying Doctor Service, Optometry Australia,and the Brien Holden Vision
Institute. The authors acknowledge Optical Prescription Spectacle Makers,
who donated sunglasses valued at$130 foreach study participant.The
CERA receivesOperationalInfrastructureSupportfrom theVictorian
Government. The Principal Investigator (M.D.) is supported by a Nationa
Health and MedicalResearch CouncilCareerDevelopmentFellowship
(#1090466).A PhD student(J.F.) is supported by an Australian Post-
graduateAward scholarship.Funded byThe AustralianGovernment
Department of Health, Canberra, Australia, Novartis, Australia, and Pegg
and Leslie Cranbourne Foundation. The funding organizations had no ro
in the design or conduct of this research.
Author Contributions:
Conception and design: Taylor,Dirani,Foreman,Keel,van Wijngaarden,
Crowston
Data collection: Dirani,Foreman, Keel, Sandhu, Ang, Fan Gaskin
Analysis and interpretation: Dirani, Foreman, Xie, Keel, Sandhu, Ang, Fa
Gaskin, Crowston
Obtained funding: Dirani
Overallresponsibility:Bourne,Taylor,Dirani,Foreman,Xie, Keel, van
Wijngaarden,Sandhu, Ang,Fan Gaskin,Crowston
Abbreviations and Acronyms:
AMD ¼ age-related maculardegeneration;CERA ¼ Centre for Eye
Research Australia;CI ¼ confidence interval;NEHS ¼ NationalEye
Health Survey; OR ¼ odds ratio.
Correspondence:
Joshua Foreman, BSc (Hons), Centre for Eye Research Australia, Level 1
32 Gisborne Street,EastMelbourne,Victoria,Australia 3002.E-mail:
foreman.j@unimelb.edu.au.
OphthalmologyVolume- , Number- , Month 2017
10
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.



