A Concept Analysis of the Theory-Practice Gap in Nursing Education
VerifiedAdded on 2023/06/05
|24
|7947
|161
Literature Review
AI Summary
This literature review presents a concept analysis of the theory-practice gap in nursing, utilizing Rodgers' evolutionary process to define and clarify the concept. It addresses the widespread use of the phrase 'theory-practice gap' in nursing literature without a consistent definition. The analysis aims to provide a deeper understanding of the concept for consistent application within nurse education. It details the data search, attributes, antecedents, and consequences of the theory-practice gap. The review identifies attributes such as relational problems between university and clinical practice, practice failing to reflect theory, and theory perceived as irrelevant to practice. Antecedents include issues within university and clinical practice relationships. Consequences include the influence on nurses and nursing students and disparity in collaboration between university and clinical practice. A model case is presented to illustrate the concept, contributing to a standardized understanding and relevance within nursing and nurse education. This analysis highlights the persistent gap between theoretical knowledge and practical application, emphasizing the need for collaboration between universities and clinical practice to develop the nursing profession.

See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/329125104
What is a Theory-Practice Gap? An exploration of the concept.
Article in Nurse Education in Practice · November 2018
DOI: 10.1016/j.nepr.2018.10.005
CITATIONS
0
READS
320
1 author:
Some of the authors of this publication are also working on these related projects:
An investigation into the the effects of a theory-practice gap on student nurses' understanding of administering intramuscular injectionsView project
Kathleen Greenway
Oxford Brookes University
7 PUBLICATIONS62CITATIONS
SEE PROFILE
All content following this page was uploaded by Kathleen Greenway on 22 November 2018.
The user has requested enhancement of the downloaded file.
What is a Theory-Practice Gap? An exploration of the concept.
Article in Nurse Education in Practice · November 2018
DOI: 10.1016/j.nepr.2018.10.005
CITATIONS
0
READS
320
1 author:
Some of the authors of this publication are also working on these related projects:
An investigation into the the effects of a theory-practice gap on student nurses' understanding of administering intramuscular injectionsView project
Kathleen Greenway
Oxford Brookes University
7 PUBLICATIONS62CITATIONS
SEE PROFILE
All content following this page was uploaded by Kathleen Greenway on 22 November 2018.
The user has requested enhancement of the downloaded file.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

1
What is a Theory-Practice Gap? An exploration of the concept.
Abstract
In nursing literature, the phrase ‘theory-practice gap’ is widely used without
common definition or description of its underlying concept. This review paper
presents a concept analysis using Rodgers (2000) evolutionary process to
define and clarify the concept of the theory-practice gap as part of a doctoral
study. In so doing it provides a deeper understanding of the concept to enable
its consistent application within nurse education. A theoretical definition is
developed, the data search that was undertaken is described and a
discussion of the attributes, antecedents and consequences is provided. We
conclude by offering, a model case, which is employed to illustrate the
concept.
Introduction
The primary aim of this doctoral research programme using case study
methodology, was to explore the existence of a theory-practice gap, using
student nurses’ experiences of administering intramuscular injections (IMI)
within their clinical placements as the case. The administration of IMIs forms
part of the essential skills clusters for pre-registration nurses (NMC 2010) and
is one of many skills performed by registered nurses, that may appear to an
onlooker to be an easy skill to execute, yet the practice appears to be fraught
with inconsistencies. The practice to administer an IMI by registered nurses is
not evidence based, which results in a variety of techniques being used
without fully rationalise their practice (Walsh and Brophy 2010). This scenario
can leave students unsure of which method they should use as often what
they are taught in university is not being reflected by their mentors in clinical
practice. This results in a theory-practice gap.
The phrase theory-practice gap is commonly used in nursing literature, often
without consistent definition or description, with the gap regularly referred to
What is a Theory-Practice Gap? An exploration of the concept.
Abstract
In nursing literature, the phrase ‘theory-practice gap’ is widely used without
common definition or description of its underlying concept. This review paper
presents a concept analysis using Rodgers (2000) evolutionary process to
define and clarify the concept of the theory-practice gap as part of a doctoral
study. In so doing it provides a deeper understanding of the concept to enable
its consistent application within nurse education. A theoretical definition is
developed, the data search that was undertaken is described and a
discussion of the attributes, antecedents and consequences is provided. We
conclude by offering, a model case, which is employed to illustrate the
concept.
Introduction
The primary aim of this doctoral research programme using case study
methodology, was to explore the existence of a theory-practice gap, using
student nurses’ experiences of administering intramuscular injections (IMI)
within their clinical placements as the case. The administration of IMIs forms
part of the essential skills clusters for pre-registration nurses (NMC 2010) and
is one of many skills performed by registered nurses, that may appear to an
onlooker to be an easy skill to execute, yet the practice appears to be fraught
with inconsistencies. The practice to administer an IMI by registered nurses is
not evidence based, which results in a variety of techniques being used
without fully rationalise their practice (Walsh and Brophy 2010). This scenario
can leave students unsure of which method they should use as often what
they are taught in university is not being reflected by their mentors in clinical
practice. This results in a theory-practice gap.
The phrase theory-practice gap is commonly used in nursing literature, often
without consistent definition or description, with the gap regularly referred to

2
as being ‘bridged’, ‘breached’, ‘avoided’ or ‘negotiated’. A persistent theory-
practice gap is evident in nursing literature (Rolfe, 2002, Maben et al 2006,
Monaghan, 2015) and frequently mentioned in contemporary research, yet
there is little clarity about its virtual or real characteristics; hence there are
omissions and confusion in our common understanding of this phenomenon.
As a consequence of this lack of consensus a conceptual analysis of the term
was deemed necessary. Walker and Avant (2005) suggest several reasons
for completing a concept analysis, ranging from developing operational
definitions, to clarifying the meaning of an existing concept, to adding to
existing theory. The process for undertaking a concept analysis has been
linked with philosophical inquiry, which in turn uses intellectual analysis to
clarify meaning; moreover in this instance it was crucial as Duncan et al
(2007) argue to embody a shared meaning within a professional discipline to
enable effective communication.
Background
Scully (2011) indicates that despite the differing interpretations of the nature
of the theory-practice gap, there is widespread agreement that it represents
the separation of the practical dimension of nursing from that of theoretical
knowledge (Rolfe 1998, 2002). During the process of completing this concept
analysis it was possible, in the absence of any other given definition, to create
and emergent definition of the theory-practice gap as:
‘The gap between the theoretical knowledge and the practical
application of nursing, most often expressed as a negative entity,
with adverse consequences.’
A definition is important as the theory-practice gap is not tangible; it
represents a metaphorical void which is felt or experienced, yet is not easily
measurable or quantifiable. Consequently, analysis of the components of the
theory-practice gap was expected to produce a classification, a
standardisation of the concept, and an adoption of the common meaning and
relevance to nursing and nurse education.
as being ‘bridged’, ‘breached’, ‘avoided’ or ‘negotiated’. A persistent theory-
practice gap is evident in nursing literature (Rolfe, 2002, Maben et al 2006,
Monaghan, 2015) and frequently mentioned in contemporary research, yet
there is little clarity about its virtual or real characteristics; hence there are
omissions and confusion in our common understanding of this phenomenon.
As a consequence of this lack of consensus a conceptual analysis of the term
was deemed necessary. Walker and Avant (2005) suggest several reasons
for completing a concept analysis, ranging from developing operational
definitions, to clarifying the meaning of an existing concept, to adding to
existing theory. The process for undertaking a concept analysis has been
linked with philosophical inquiry, which in turn uses intellectual analysis to
clarify meaning; moreover in this instance it was crucial as Duncan et al
(2007) argue to embody a shared meaning within a professional discipline to
enable effective communication.
Background
Scully (2011) indicates that despite the differing interpretations of the nature
of the theory-practice gap, there is widespread agreement that it represents
the separation of the practical dimension of nursing from that of theoretical
knowledge (Rolfe 1998, 2002). During the process of completing this concept
analysis it was possible, in the absence of any other given definition, to create
and emergent definition of the theory-practice gap as:
‘The gap between the theoretical knowledge and the practical
application of nursing, most often expressed as a negative entity,
with adverse consequences.’
A definition is important as the theory-practice gap is not tangible; it
represents a metaphorical void which is felt or experienced, yet is not easily
measurable or quantifiable. Consequently, analysis of the components of the
theory-practice gap was expected to produce a classification, a
standardisation of the concept, and an adoption of the common meaning and
relevance to nursing and nurse education.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

3
The theory-practice gap has persisted in nursing and continues to have
negative connotations, although its continued presence may facilitate dynamic
change within the profession (Haigh 2008), highlighting the separation
between theoretical or evidence-based knowledge and practical elements of
nursing (Scully 2011). This gap between theory (what should happen), and
what occurs (what actually happens) in the clinical environment is not new.
Yet it is not only the practical skills of new graduate nurses that are
questioned (Voldbjerg et al 2016), it is also the potential lack of proficiency
among nurses in both their clinical skills and critical thinking abilities. Thus the
theory-practice gap remains a continuing problem for nursing, felt both by
experienced and newly qualified and student nurses (Scully 2011). Despite
the more frequently articulated negative associations of the theory-practice
gap, the concept is not always regarded as being resolutely negative. Ousey
has coherently argued, in a debate with Gallagher (Ousey and Gallagher
2007), that the presence of the theory-practice gap can encourage students
and staff to question and thus to avoid complacency in their practice.
Monaghan (2015) suggests as the theory-practice gap begins during pre-
registration education, effecting clinical skills capabilities of student nurses,
collaboration between universities and practice is essential for the
development of the nursing profession.
Method:
Risjord (2009), provides a comprehensive critique of the epistemological
foundations of concept analysis and deems that it can be seen as an arbitrary
and vacuous exercise when it is performed in an unsupported and unjustified
fashion. A concept analysis therefore needs to be undertaken using a
theoretical framework, essential for providing operational definitions.
Traditionally a concept analysis within nursing has used Wilson’s (1963)
method, although many authors have subsequently modified and adapted
Wilson’s framework. Currently, the two most used frameworks within nursing
are those of Walker and Avant (2005) and Rodgers (2000). Walker and
The theory-practice gap has persisted in nursing and continues to have
negative connotations, although its continued presence may facilitate dynamic
change within the profession (Haigh 2008), highlighting the separation
between theoretical or evidence-based knowledge and practical elements of
nursing (Scully 2011). This gap between theory (what should happen), and
what occurs (what actually happens) in the clinical environment is not new.
Yet it is not only the practical skills of new graduate nurses that are
questioned (Voldbjerg et al 2016), it is also the potential lack of proficiency
among nurses in both their clinical skills and critical thinking abilities. Thus the
theory-practice gap remains a continuing problem for nursing, felt both by
experienced and newly qualified and student nurses (Scully 2011). Despite
the more frequently articulated negative associations of the theory-practice
gap, the concept is not always regarded as being resolutely negative. Ousey
has coherently argued, in a debate with Gallagher (Ousey and Gallagher
2007), that the presence of the theory-practice gap can encourage students
and staff to question and thus to avoid complacency in their practice.
Monaghan (2015) suggests as the theory-practice gap begins during pre-
registration education, effecting clinical skills capabilities of student nurses,
collaboration between universities and practice is essential for the
development of the nursing profession.
Method:
Risjord (2009), provides a comprehensive critique of the epistemological
foundations of concept analysis and deems that it can be seen as an arbitrary
and vacuous exercise when it is performed in an unsupported and unjustified
fashion. A concept analysis therefore needs to be undertaken using a
theoretical framework, essential for providing operational definitions.
Traditionally a concept analysis within nursing has used Wilson’s (1963)
method, although many authors have subsequently modified and adapted
Wilson’s framework. Currently, the two most used frameworks within nursing
are those of Walker and Avant (2005) and Rodgers (2000). Walker and
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

4
Avants’ framework omits the issue of contextualisation which is central within
Rodgers’ (2000) evolutionary framework. Rodgers’ framework emphasises the
dynamic way concepts and theories change over time, or considers when
different contexts are reviewed at the same point in time; thus when the
context of use alters, so must the meaning, focussing on the current
application of the concept and its interconnectedness with other factors. The
theory-practice gap might not only exist in nursing (it might also exist in other
professions such as medicine or teaching, for example) thus the contextual
features and application of Rodgers model, together with its emphasis on
temporal and heuristic elements, was reasoned to provide the most
appropriate framework for this conceptual analysis. The presentation of this
concept analysis will follow the steps as described below in Rodgers’ model.
Steps in Rodgers’ (2000) model
Rodgers (2000) advocates no preconceived descriptions of a concept should
be allowed; instead stating a concept must come from searching the literature
using a systematic technique. Although Rodgers’ model has evolved from
Wilson’s (1963) original 11-step model, it has been refined into an 8-step
process as shown in table 1:
Rodgers' Evolutionary Model
• 1. Identify the concept of interest
• 2. Identify surrogate terms
• 3. Choose the setting and the sample
• 4. Identify the attributes
• 5. Identify the references, antecedents and consequences
• 6. Identify related concepts
• 7. Identify a model case
• 8. Identify implications for further research and development of the concept
Avants’ framework omits the issue of contextualisation which is central within
Rodgers’ (2000) evolutionary framework. Rodgers’ framework emphasises the
dynamic way concepts and theories change over time, or considers when
different contexts are reviewed at the same point in time; thus when the
context of use alters, so must the meaning, focussing on the current
application of the concept and its interconnectedness with other factors. The
theory-practice gap might not only exist in nursing (it might also exist in other
professions such as medicine or teaching, for example) thus the contextual
features and application of Rodgers model, together with its emphasis on
temporal and heuristic elements, was reasoned to provide the most
appropriate framework for this conceptual analysis. The presentation of this
concept analysis will follow the steps as described below in Rodgers’ model.
Steps in Rodgers’ (2000) model
Rodgers (2000) advocates no preconceived descriptions of a concept should
be allowed; instead stating a concept must come from searching the literature
using a systematic technique. Although Rodgers’ model has evolved from
Wilson’s (1963) original 11-step model, it has been refined into an 8-step
process as shown in table 1:
Rodgers' Evolutionary Model
• 1. Identify the concept of interest
• 2. Identify surrogate terms
• 3. Choose the setting and the sample
• 4. Identify the attributes
• 5. Identify the references, antecedents and consequences
• 6. Identify related concepts
• 7. Identify a model case
• 8. Identify implications for further research and development of the concept

5
Concept of interest
Within nursing there is perceived to be a gap between theory and practice
which is persistent and mostly has negative connotations; yet whilst there is
the awareness that it can be felt or experienced, it is not easily measured or
quantifiable. Therefore the theory-practice gap required describing, defining
and exploring; in achieving this it becomes valid for the advancement of the
understanding of the concept within nursing, in both education and practice
(Duncan et al 2007).
Surrogate terms
Rodgers (2000) refers to surrogate terms as being similar or related; those
that can be identified as synonymous to the term theory-practice gap. This
was difficult to quantify as the only other synonym identified was the
‘education-practice gap’ - succinct terms to encompass the void or gulf
between theory and practice were not found. Substitute words such as
‘schism’, ‘gulf’ or ‘dichotomy’, instead of gap, were infrequently used. However
these did not offer a complete, surrogate term, rather they were merely
descriptive, alternative semantics.
Choosing the setting and sample
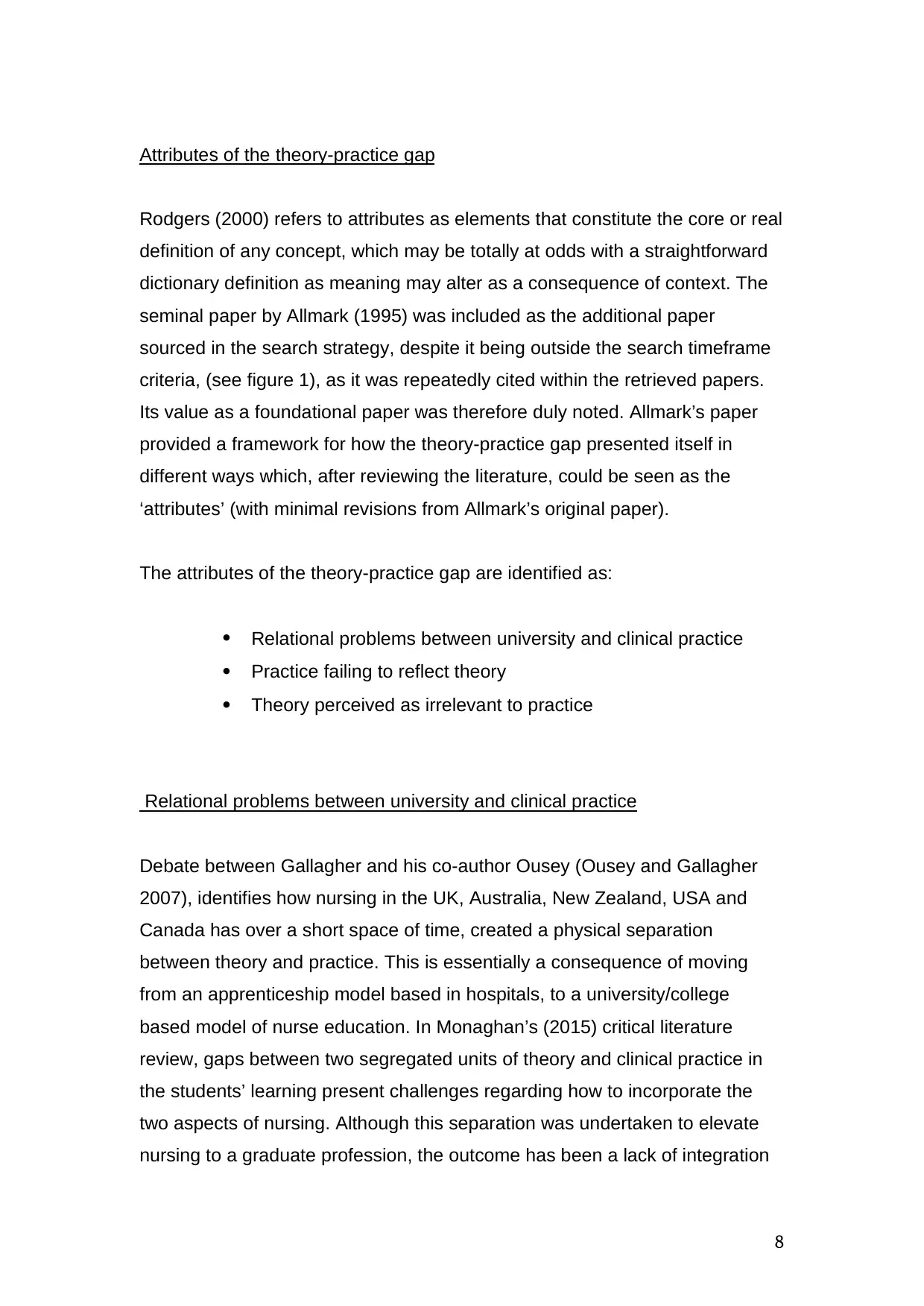
The keywords for the literature search were derived from the term ‘theory-
practice gap’ and its surrogate term ‘education-practice gap’ using the
CINAHL, BNI, BEI and MEDLINE databases. Limits for English language, for
peer reviewed journals and with a publication date ranging from 2005-2016
were applied. The results were as indicated in Figure 1
Concept of interest
Within nursing there is perceived to be a gap between theory and practice
which is persistent and mostly has negative connotations; yet whilst there is
the awareness that it can be felt or experienced, it is not easily measured or
quantifiable. Therefore the theory-practice gap required describing, defining
and exploring; in achieving this it becomes valid for the advancement of the
understanding of the concept within nursing, in both education and practice
(Duncan et al 2007).
Surrogate terms
Rodgers (2000) refers to surrogate terms as being similar or related; those
that can be identified as synonymous to the term theory-practice gap. This
was difficult to quantify as the only other synonym identified was the
‘education-practice gap’ - succinct terms to encompass the void or gulf
between theory and practice were not found. Substitute words such as
‘schism’, ‘gulf’ or ‘dichotomy’, instead of gap, were infrequently used. However
these did not offer a complete, surrogate term, rather they were merely
descriptive, alternative semantics.
Choosing the setting and sample
The keywords for the literature search were derived from the term ‘theory-
practice gap’ and its surrogate term ‘education-practice gap’ using the
CINAHL, BNI, BEI and MEDLINE databases. Limits for English language, for
peer reviewed journals and with a publication date ranging from 2005-2016
were applied. The results were as indicated in Figure 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

6
* 88 papers were identified as being duplicates on multiple databases and an
excel spreadsheet was created to list and compare the occurrences of each
paper within the databases searched.
Figure 1 - PRISMA style diagram representing the audit trail of the search
strategy using the Rogerian process.
Records identified through
database searching
(n = 512)
Additional records identified
through snowball sampling
(n = 1)
88 duplicates
removed*
Records screened
(n = 425)
Records excluded
(n = 301)
Full-text articles assessed
for eligibility
(n = 124)
Full-text articles
excluded, with reasons
(n = 0)
Studies included in
concept analysis 20%
representative sample
(n = 26)
* 88 papers were identified as being duplicates on multiple databases and an
excel spreadsheet was created to list and compare the occurrences of each
paper within the databases searched.
Figure 1 - PRISMA style diagram representing the audit trail of the search
strategy using the Rogerian process.
Records identified through
database searching
(n = 512)
Additional records identified
through snowball sampling
(n = 1)
88 duplicates
removed*
Records screened
(n = 425)
Records excluded
(n = 301)
Full-text articles assessed
for eligibility
(n = 124)
Full-text articles
excluded, with reasons
(n = 0)
Studies included in
concept analysis 20%
representative sample
(n = 26)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
After removal of the duplicates, and the preliminary screening of the abstracts,
a total of 124 papers remained for detailed screening. The papers excluded
by this process mostly referred to ‘bridging’ or ‘overcoming’ the theory-
practice gap, without recourse to defining the term or providing any insight
into the nature of the concept. In accordance with Rodgers’ process of
sampling, 20% of the total results (n=26) were retrieved commencing with a
random starting point to select the literature for inclusion in the analysis. This
was then used as the representative sample to complete the concept
analysis. Whilst the majority of the papers retrieved were research studies,
using Rogerian sampling it is also accepted practice to include any other
cognitive conception of the concept under scrutiny. As concepts are cognitive
conceptions, Tofthagen and Fagerstrøm (2010) concur that data sources can
include professional literature, interviews, or other forms of verbalised
language; several papers which included debates, expressions of personal
experiences or editorial opinions were therefore included in this concept
analysis, though these represent the minority.
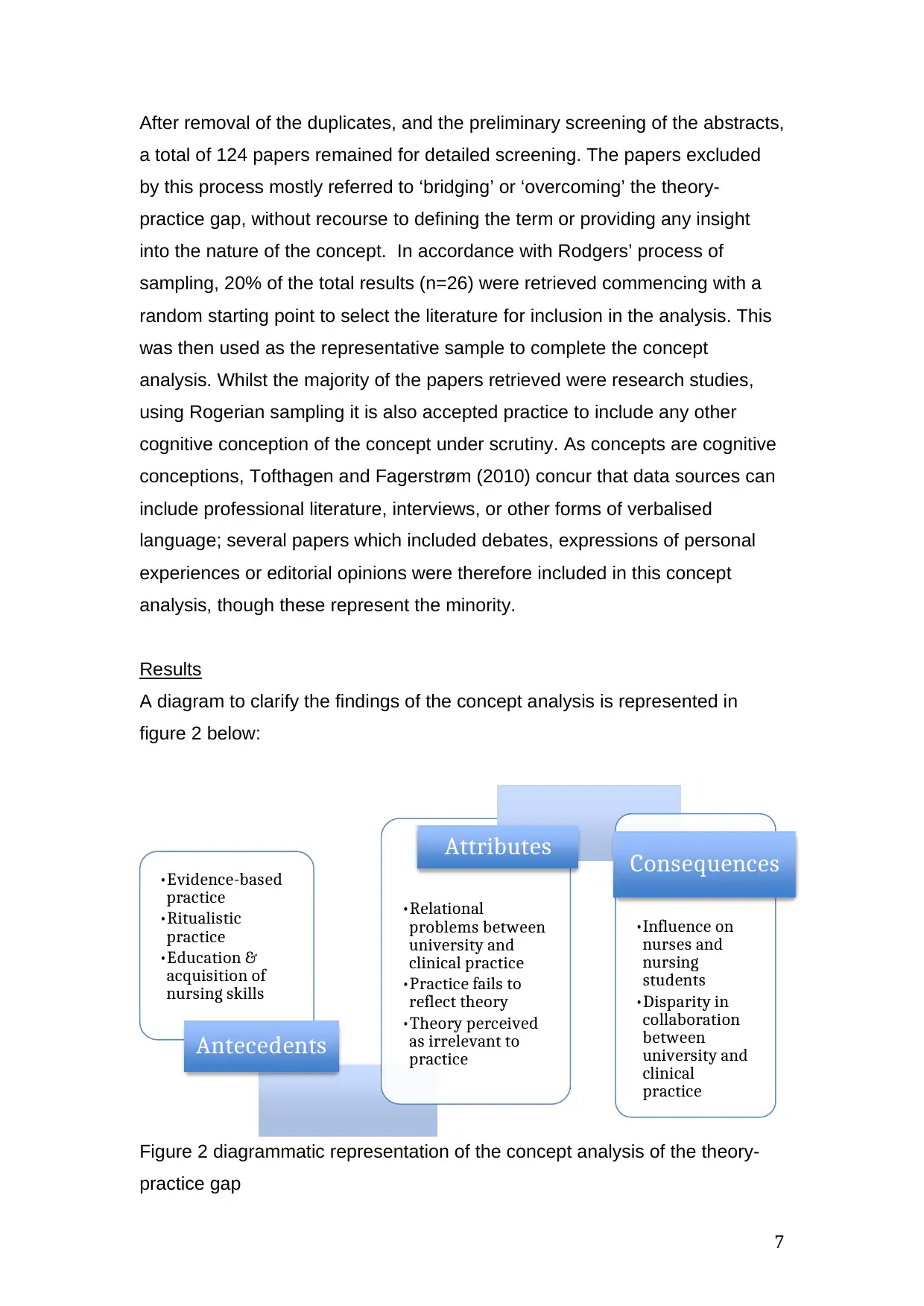
Results
A diagram to clarify the findings of the concept analysis is represented in
figure 2 below:
Figure 2 diagrammatic representation of the concept analysis of the theory-
practice gap
•Evidence-based
practice
•Ritualistic
practice
•Education &
acquisition of
nursing skills
Antecedents
•Relational
problems between
university and
clinical practice
•Practice fails to
reflect theory
•Theory perceived
as irrelevant to
practice
Attributes
•Influence on
nurses and
nursing
students
•Disparity in
collaboration
between
university and
clinical
practice
Consequences
After removal of the duplicates, and the preliminary screening of the abstracts,
a total of 124 papers remained for detailed screening. The papers excluded
by this process mostly referred to ‘bridging’ or ‘overcoming’ the theory-
practice gap, without recourse to defining the term or providing any insight
into the nature of the concept. In accordance with Rodgers’ process of
sampling, 20% of the total results (n=26) were retrieved commencing with a
random starting point to select the literature for inclusion in the analysis. This
was then used as the representative sample to complete the concept
analysis. Whilst the majority of the papers retrieved were research studies,
using Rogerian sampling it is also accepted practice to include any other
cognitive conception of the concept under scrutiny. As concepts are cognitive
conceptions, Tofthagen and Fagerstrøm (2010) concur that data sources can
include professional literature, interviews, or other forms of verbalised
language; several papers which included debates, expressions of personal
experiences or editorial opinions were therefore included in this concept
analysis, though these represent the minority.
Results
A diagram to clarify the findings of the concept analysis is represented in
figure 2 below:
Figure 2 diagrammatic representation of the concept analysis of the theory-
practice gap
•Evidence-based
practice
•Ritualistic
practice
•Education &
acquisition of
nursing skills
Antecedents
•Relational
problems between
university and
clinical practice
•Practice fails to
reflect theory
•Theory perceived
as irrelevant to
practice
Attributes
•Influence on
nurses and
nursing
students
•Disparity in
collaboration
between
university and
clinical
practice
Consequences
8
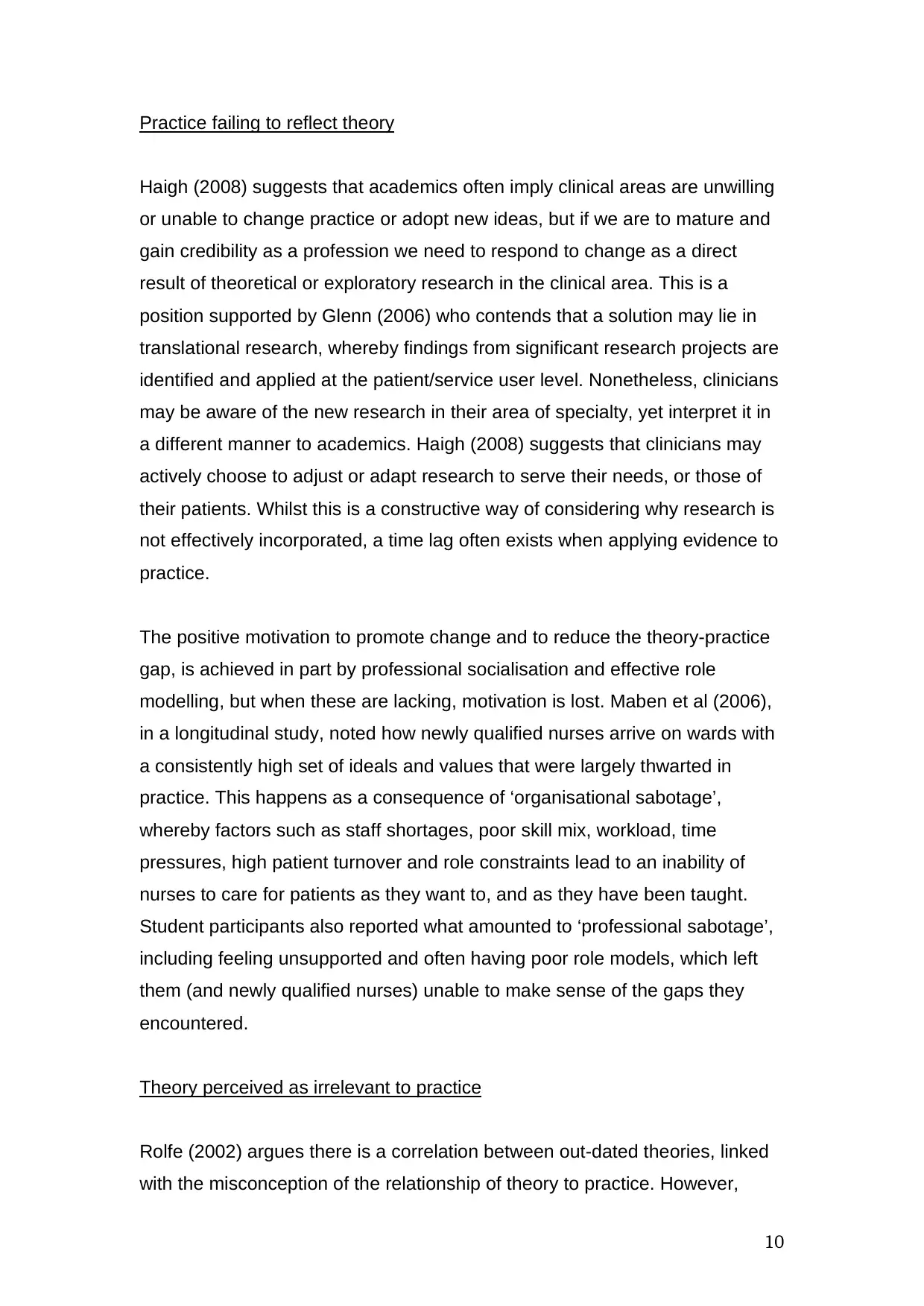
Attributes of the theory-practice gap
Rodgers (2000) refers to attributes as elements that constitute the core or real
definition of any concept, which may be totally at odds with a straightforward
dictionary definition as meaning may alter as a consequence of context. The
seminal paper by Allmark (1995) was included as the additional paper
sourced in the search strategy, despite it being outside the search timeframe
criteria, (see figure 1), as it was repeatedly cited within the retrieved papers.
Its value as a foundational paper was therefore duly noted. Allmark’s paper
provided a framework for how the theory-practice gap presented itself in
different ways which, after reviewing the literature, could be seen as the
‘attributes’ (with minimal revisions from Allmark’s original paper).
The attributes of the theory-practice gap are identified as:
Relational problems between university and clinical practice
Practice failing to reflect theory
Theory perceived as irrelevant to practice
Relational problems between university and clinical practice
Debate between Gallagher and his co-author Ousey (Ousey and Gallagher
2007), identifies how nursing in the UK, Australia, New Zealand, USA and
Canada has over a short space of time, created a physical separation
between theory and practice. This is essentially a consequence of moving
from an apprenticeship model based in hospitals, to a university/college
based model of nurse education. In Monaghan’s (2015) critical literature
review, gaps between two segregated units of theory and clinical practice in
the students’ learning present challenges regarding how to incorporate the
two aspects of nursing. Although this separation was undertaken to elevate
nursing to a graduate profession, the outcome has been a lack of integration
Attributes of the theory-practice gap
Rodgers (2000) refers to attributes as elements that constitute the core or real
definition of any concept, which may be totally at odds with a straightforward
dictionary definition as meaning may alter as a consequence of context. The
seminal paper by Allmark (1995) was included as the additional paper
sourced in the search strategy, despite it being outside the search timeframe
criteria, (see figure 1), as it was repeatedly cited within the retrieved papers.
Its value as a foundational paper was therefore duly noted. Allmark’s paper
provided a framework for how the theory-practice gap presented itself in
different ways which, after reviewing the literature, could be seen as the
‘attributes’ (with minimal revisions from Allmark’s original paper).
The attributes of the theory-practice gap are identified as:
Relational problems between university and clinical practice
Practice failing to reflect theory
Theory perceived as irrelevant to practice
Relational problems between university and clinical practice
Debate between Gallagher and his co-author Ousey (Ousey and Gallagher
2007), identifies how nursing in the UK, Australia, New Zealand, USA and
Canada has over a short space of time, created a physical separation
between theory and practice. This is essentially a consequence of moving
from an apprenticeship model based in hospitals, to a university/college
based model of nurse education. In Monaghan’s (2015) critical literature
review, gaps between two segregated units of theory and clinical practice in
the students’ learning present challenges regarding how to incorporate the
two aspects of nursing. Although this separation was undertaken to elevate
nursing to a graduate profession, the outcome has been a lack of integration
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

9
between university and clinical staff in planning the students’ clinical
education. The role of the Lecturer-Practitioner (LP) was created in the 1990s
in the UK with the specific aim of bridging the theory-practice gap. Hancock et
al (2007), in an evaluation study, explored the experiences of LPs and found
that as well as supporting students in practice and providing academic
teaching, their role included the development of clinical skills for newly
qualified nurses. Their joint appointment promoted their clinical credibility and
encouraged stronger links between practice and education. However, Barrett
(2007), in his critical review, states limitations of the LP role resulting in split
loyalties, heavy workloads, unclear career structures and limited effectiveness
of the post holder.
The introduction of joint clinical chairs in nursing, whereby a professorial
position is created as a collaborative appointment between a university and
the healthcare provider, has also been heralded as another means of bridging
the theory-practice gap. Such strategic and operational posts, specifically
designed to straddle the realms of academia and clinical practice, appear
ideally placed to cultivate research and develop clinical practice. Nonetheless,
Darbyshire’s (2010) critical editorial, laments how constant capricious change
within the organisations regarding focus and priorities, fosters the impossibility
of filling these positions - a problem further compounded by a lack of suitable
applicants. This is particularly unfortunate given that Evans (2009), in his
review of mental health nurse training, argues that mutual collaboration
requires a top down leadership approach supporting the two institutions in
developing a joint strategy for student learning.
Hence the roles of LPs and joint chairs were created with the aim of
increasing collaboration between the parties, as well as targeting, influencing
and cascading issues for research or practice. It is apparent that the full
potential of these roles may not yet have been reached.
between university and clinical staff in planning the students’ clinical
education. The role of the Lecturer-Practitioner (LP) was created in the 1990s
in the UK with the specific aim of bridging the theory-practice gap. Hancock et
al (2007), in an evaluation study, explored the experiences of LPs and found
that as well as supporting students in practice and providing academic
teaching, their role included the development of clinical skills for newly
qualified nurses. Their joint appointment promoted their clinical credibility and
encouraged stronger links between practice and education. However, Barrett
(2007), in his critical review, states limitations of the LP role resulting in split
loyalties, heavy workloads, unclear career structures and limited effectiveness
of the post holder.
The introduction of joint clinical chairs in nursing, whereby a professorial
position is created as a collaborative appointment between a university and
the healthcare provider, has also been heralded as another means of bridging
the theory-practice gap. Such strategic and operational posts, specifically
designed to straddle the realms of academia and clinical practice, appear
ideally placed to cultivate research and develop clinical practice. Nonetheless,
Darbyshire’s (2010) critical editorial, laments how constant capricious change
within the organisations regarding focus and priorities, fosters the impossibility
of filling these positions - a problem further compounded by a lack of suitable
applicants. This is particularly unfortunate given that Evans (2009), in his
review of mental health nurse training, argues that mutual collaboration
requires a top down leadership approach supporting the two institutions in
developing a joint strategy for student learning.
Hence the roles of LPs and joint chairs were created with the aim of
increasing collaboration between the parties, as well as targeting, influencing
and cascading issues for research or practice. It is apparent that the full
potential of these roles may not yet have been reached.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10
Practice failing to reflect theory
Haigh (2008) suggests that academics often imply clinical areas are unwilling
or unable to change practice or adopt new ideas, but if we are to mature and
gain credibility as a profession we need to respond to change as a direct
result of theoretical or exploratory research in the clinical area. This is a
position supported by Glenn (2006) who contends that a solution may lie in
translational research, whereby findings from significant research projects are
identified and applied at the patient/service user level. Nonetheless, clinicians
may be aware of the new research in their area of specialty, yet interpret it in
a different manner to academics. Haigh (2008) suggests that clinicians may
actively choose to adjust or adapt research to serve their needs, or those of
their patients. Whilst this is a constructive way of considering why research is
not effectively incorporated, a time lag often exists when applying evidence to
practice.
The positive motivation to promote change and to reduce the theory-practice
gap, is achieved in part by professional socialisation and effective role
modelling, but when these are lacking, motivation is lost. Maben et al (2006),
in a longitudinal study, noted how newly qualified nurses arrive on wards with
a consistently high set of ideals and values that were largely thwarted in
practice. This happens as a consequence of ‘organisational sabotage’,
whereby factors such as staff shortages, poor skill mix, workload, time
pressures, high patient turnover and role constraints lead to an inability of
nurses to care for patients as they want to, and as they have been taught.
Student participants also reported what amounted to ‘professional sabotage’,
including feeling unsupported and often having poor role models, which left
them (and newly qualified nurses) unable to make sense of the gaps they
encountered.
Theory perceived as irrelevant to practice
Rolfe (2002) argues there is a correlation between out-dated theories, linked
with the misconception of the relationship of theory to practice. However,
Practice failing to reflect theory
Haigh (2008) suggests that academics often imply clinical areas are unwilling
or unable to change practice or adopt new ideas, but if we are to mature and
gain credibility as a profession we need to respond to change as a direct
result of theoretical or exploratory research in the clinical area. This is a
position supported by Glenn (2006) who contends that a solution may lie in
translational research, whereby findings from significant research projects are
identified and applied at the patient/service user level. Nonetheless, clinicians
may be aware of the new research in their area of specialty, yet interpret it in
a different manner to academics. Haigh (2008) suggests that clinicians may
actively choose to adjust or adapt research to serve their needs, or those of
their patients. Whilst this is a constructive way of considering why research is
not effectively incorporated, a time lag often exists when applying evidence to
practice.
The positive motivation to promote change and to reduce the theory-practice
gap, is achieved in part by professional socialisation and effective role
modelling, but when these are lacking, motivation is lost. Maben et al (2006),
in a longitudinal study, noted how newly qualified nurses arrive on wards with
a consistently high set of ideals and values that were largely thwarted in
practice. This happens as a consequence of ‘organisational sabotage’,
whereby factors such as staff shortages, poor skill mix, workload, time
pressures, high patient turnover and role constraints lead to an inability of
nurses to care for patients as they want to, and as they have been taught.
Student participants also reported what amounted to ‘professional sabotage’,
including feeling unsupported and often having poor role models, which left
them (and newly qualified nurses) unable to make sense of the gaps they
encountered.
Theory perceived as irrelevant to practice
Rolfe (2002) argues there is a correlation between out-dated theories, linked
with the misconception of the relationship of theory to practice. However,

11
other authors (Maben et al 2006, Ousey and Gallagher 2007) suggest the
fault lies with the lack of socialisation of the theories into the clinical setting
and the failure to integrate research into the clinical practice environment.
Haigh (2008) suggests this aspect of the theory-practice gap should be
embraced, not despised. The dynamic and evolving nature of nursing implies
old theories will become irrelevant whilst new theories and skills being
developed, will require testing and evaluation. When new skills or theories are
accepted, or well evaluated, there is a need to cascade into the global nursing
network. It is therefore inevitable that a gap is experienced until such time as
the transfer of knowledge or skills is complete.
Additionally, as nurse education is split between clinical practice and the
university, there is a need to prioritise applying theory in context specific and
workable ways. The use of human patient simulators (HPS) within a simulated
based education (SBE) to provide a more realistic yet controlled classroom
environment has been advocated as a way of making skills learning more
representative of the contextual realities of everyday clinical practice. The
claim university lecturers are out of touch with reality, not clinically credible
and that the theories they espouse do not reflect practice, opposes the
previous position. Ousey and Gallagher (2010) refute this statement in their
debate regarding the clinical credibility of nurse educators. They argue
maintaining such credibility is not of paramount importance, stating that this is
an unrealistic expectation of lecturers given their pressure of work and
requirement to display competence so to remain on the professional register.
Ousey and Gallagher (2010) find this debate to be an unnecessary
distraction, arguing that emphasis should be on partnership between
academia and clinical practice, whilst the issue of clinical credibility should
instead be focused on the mentor in practice. Myall et al (2008) have declared
effective mentorship to be pivotal to students’ clinical learning experiences;
this is of particular importance as mentors provide the summative assessment
of a student’s clinical practice. Therefore, the need for a competent, clinically
credible, research aware and reflective mentor is extremely desirable. Indeed,
this is increasingly regarded as essential for the effective professional
other authors (Maben et al 2006, Ousey and Gallagher 2007) suggest the
fault lies with the lack of socialisation of the theories into the clinical setting
and the failure to integrate research into the clinical practice environment.
Haigh (2008) suggests this aspect of the theory-practice gap should be
embraced, not despised. The dynamic and evolving nature of nursing implies
old theories will become irrelevant whilst new theories and skills being
developed, will require testing and evaluation. When new skills or theories are
accepted, or well evaluated, there is a need to cascade into the global nursing
network. It is therefore inevitable that a gap is experienced until such time as
the transfer of knowledge or skills is complete.
Additionally, as nurse education is split between clinical practice and the
university, there is a need to prioritise applying theory in context specific and
workable ways. The use of human patient simulators (HPS) within a simulated
based education (SBE) to provide a more realistic yet controlled classroom
environment has been advocated as a way of making skills learning more
representative of the contextual realities of everyday clinical practice. The
claim university lecturers are out of touch with reality, not clinically credible
and that the theories they espouse do not reflect practice, opposes the
previous position. Ousey and Gallagher (2010) refute this statement in their
debate regarding the clinical credibility of nurse educators. They argue
maintaining such credibility is not of paramount importance, stating that this is
an unrealistic expectation of lecturers given their pressure of work and
requirement to display competence so to remain on the professional register.
Ousey and Gallagher (2010) find this debate to be an unnecessary
distraction, arguing that emphasis should be on partnership between
academia and clinical practice, whilst the issue of clinical credibility should
instead be focused on the mentor in practice. Myall et al (2008) have declared
effective mentorship to be pivotal to students’ clinical learning experiences;
this is of particular importance as mentors provide the summative assessment
of a student’s clinical practice. Therefore, the need for a competent, clinically
credible, research aware and reflective mentor is extremely desirable. Indeed,
this is increasingly regarded as essential for the effective professional
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 24
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.