HSN211: Glycogen Storage Disease Dietary Handout for Parents
VerifiedAdded on 2022/09/14
|6
|1782
|21
Report
AI Summary
This report provides a comprehensive overview of Glycogen Storage Disease (GSD), focusing on types I, III, IV, and VI, causes, and the impact on liver function. It details the normal liver's role in glucose storage and metabolism, then explains how GSD disrupts this process. The report provides specific dietary recommendations, including the importance of complex carbohydrates, high-protein feedings, and foods to avoid for each GSD type. It emphasizes the need for a balanced diet and the importance of consulting with healthcare professionals for personalized guidance. The report is designed as a handout for parents, ensuring readability and practical application of the information, aiming to support children with GSD through proper nutrition and dietary management.

Title: Glycogen Storage Disease
Name:
Student ID:
Word Count:
1
Name:
Student ID:
Word Count:
1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
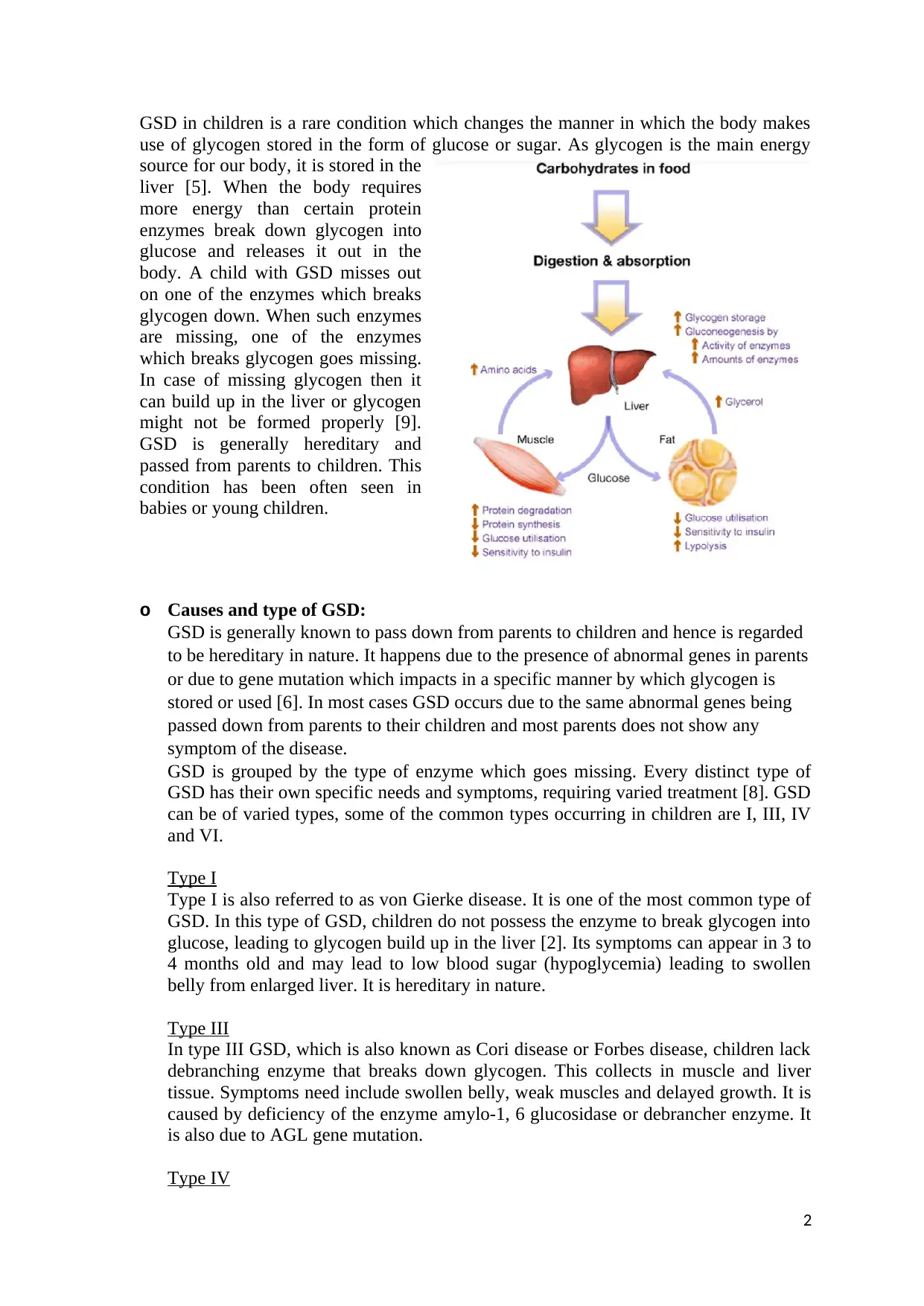
GSD in children is a rare condition which changes the manner in which the body makes
use of glycogen stored in the form of glucose or sugar. As glycogen is the main energy
source for our body, it is stored in the
liver [5]. When the body requires
more energy than certain protein
enzymes break down glycogen into
glucose and releases it out in the
body. A child with GSD misses out
on one of the enzymes which breaks
glycogen down. When such enzymes
are missing, one of the enzymes
which breaks glycogen goes missing.
In case of missing glycogen then it
can build up in the liver or glycogen
might not be formed properly [9].
GSD is generally hereditary and
passed from parents to children. This
condition has been often seen in
babies or young children.
o Causes and type of GSD:
GSD is generally known to pass down from parents to children and hence is regarded
to be hereditary in nature. It happens due to the presence of abnormal genes in parents
or due to gene mutation which impacts in a specific manner by which glycogen is
stored or used [6]. In most cases GSD occurs due to the same abnormal genes being
passed down from parents to their children and most parents does not show any
symptom of the disease.
GSD is grouped by the type of enzyme which goes missing. Every distinct type of
GSD has their own specific needs and symptoms, requiring varied treatment [8]. GSD
can be of varied types, some of the common types occurring in children are I, III, IV
and VI.
Type I
Type I is also referred to as von Gierke disease. It is one of the most common type of
GSD. In this type of GSD, children do not possess the enzyme to break glycogen into
glucose, leading to glycogen build up in the liver [2]. Its symptoms can appear in 3 to
4 months old and may lead to low blood sugar (hypoglycemia) leading to swollen
belly from enlarged liver. It is hereditary in nature.
Type III
In type III GSD, which is also known as Cori disease or Forbes disease, children lack
debranching enzyme that breaks down glycogen. This collects in muscle and liver
tissue. Symptoms need include swollen belly, weak muscles and delayed growth. It is
caused by deficiency of the enzyme amylo-1, 6 glucosidase or debrancher enzyme. It
is also due to AGL gene mutation.
Type IV
2
use of glycogen stored in the form of glucose or sugar. As glycogen is the main energy
source for our body, it is stored in the
liver [5]. When the body requires
more energy than certain protein
enzymes break down glycogen into
glucose and releases it out in the
body. A child with GSD misses out
on one of the enzymes which breaks
glycogen down. When such enzymes
are missing, one of the enzymes
which breaks glycogen goes missing.
In case of missing glycogen then it
can build up in the liver or glycogen
might not be formed properly [9].
GSD is generally hereditary and
passed from parents to children. This
condition has been often seen in
babies or young children.
o Causes and type of GSD:
GSD is generally known to pass down from parents to children and hence is regarded
to be hereditary in nature. It happens due to the presence of abnormal genes in parents
or due to gene mutation which impacts in a specific manner by which glycogen is
stored or used [6]. In most cases GSD occurs due to the same abnormal genes being
passed down from parents to their children and most parents does not show any
symptom of the disease.
GSD is grouped by the type of enzyme which goes missing. Every distinct type of
GSD has their own specific needs and symptoms, requiring varied treatment [8]. GSD
can be of varied types, some of the common types occurring in children are I, III, IV
and VI.
Type I
Type I is also referred to as von Gierke disease. It is one of the most common type of
GSD. In this type of GSD, children do not possess the enzyme to break glycogen into
glucose, leading to glycogen build up in the liver [2]. Its symptoms can appear in 3 to
4 months old and may lead to low blood sugar (hypoglycemia) leading to swollen
belly from enlarged liver. It is hereditary in nature.
Type III
In type III GSD, which is also known as Cori disease or Forbes disease, children lack
debranching enzyme that breaks down glycogen. This collects in muscle and liver
tissue. Symptoms need include swollen belly, weak muscles and delayed growth. It is
caused by deficiency of the enzyme amylo-1, 6 glucosidase or debrancher enzyme. It
is also due to AGL gene mutation.
Type IV
2
In type IV GSD also referred to as Anderson disease, children develop abnormal
glycogen. This triggers body’s infection-fighting system creating scarring of the liver,
muscles and the heart. It is caused due to mutation in the GBE1 gene. This gene
normally carries instruction for making glycogen branching enzyme.
Type VI
It is caused due to storage disease caused by deficiency in liver glycogen
phosphorylase and other components associated with phosphorylase cascade system.
This is also referred to as “Hers’ disease”
o Normal liver function
Normal liver function is to
filter out blood coming
from the digestive tract
before it passes on to the
rest of the body. The liver
is also responsible for
detoxification of chemicals
and metabolizing drugs. It
secrets bile that ends up in
the intestine. The liver also
makes crucial proteins that
is important for clotting of
the blood and other
functions [3]. In normal
situation, the liver serves as
a store for glucose to be
used throughout the body, especially for the central nervous system. The human body
is said to consume approximately 60% of the blood glucose in fasting, in sedentary
individuals. Thus, the liver storing glycogen, act as a reservoir for energy for normal
human body [7].
o Liver function changes caused by GSD:
The body’s cells requires a steady supply of fuel/ energy for conducting various
functions, which comes from sugar in the body by breaking down of glucose. Glucose
in turn comes from the various food that we eat [10]. Our body uses as much glucose
from the food eaten and stores the rest in the liver for later usage. Prior to being stored
in the liver, the body combines simple glucose units into new and complex sugars
called glycogen. Glycogen is stored in the liver and muscle cells. When the body
requires extra fuel, then it triggers a mechanism to turn back glucose stored in the
liver to form glycogen. Presence of special protein in the liver referred to as enzymes
breaks down glycogen. When a child is born with the enzyme being missing for this
process then it might not work right.
3
glycogen. This triggers body’s infection-fighting system creating scarring of the liver,
muscles and the heart. It is caused due to mutation in the GBE1 gene. This gene
normally carries instruction for making glycogen branching enzyme.
Type VI
It is caused due to storage disease caused by deficiency in liver glycogen
phosphorylase and other components associated with phosphorylase cascade system.
This is also referred to as “Hers’ disease”
o Normal liver function
Normal liver function is to
filter out blood coming
from the digestive tract
before it passes on to the
rest of the body. The liver
is also responsible for
detoxification of chemicals
and metabolizing drugs. It
secrets bile that ends up in
the intestine. The liver also
makes crucial proteins that
is important for clotting of
the blood and other
functions [3]. In normal
situation, the liver serves as
a store for glucose to be
used throughout the body, especially for the central nervous system. The human body
is said to consume approximately 60% of the blood glucose in fasting, in sedentary
individuals. Thus, the liver storing glycogen, act as a reservoir for energy for normal
human body [7].
o Liver function changes caused by GSD:
The body’s cells requires a steady supply of fuel/ energy for conducting various
functions, which comes from sugar in the body by breaking down of glucose. Glucose
in turn comes from the various food that we eat [10]. Our body uses as much glucose
from the food eaten and stores the rest in the liver for later usage. Prior to being stored
in the liver, the body combines simple glucose units into new and complex sugars
called glycogen. Glycogen is stored in the liver and muscle cells. When the body
requires extra fuel, then it triggers a mechanism to turn back glucose stored in the
liver to form glycogen. Presence of special protein in the liver referred to as enzymes
breaks down glycogen. When a child is born with the enzyme being missing for this
process then it might not work right.
3
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Type I
In this case, the body is unable to store or break down glucose as it should have. This
might lead to very low blood glucose levels during fasting periods. The liver
eventually gets enlarged.
Type III
It is an inborn error in metabolism due to gene mutation. In this case the liver keeps
storing glycogen for future use.
Type IV
In this case, the body is unable to store or break down glucose as it should have. This
might lead to very low blood glucose levels during fasting periods [1]. In case of
GSD, the liver might be storing excess of glycogen hampering it functionality.
Type VI
This causes liver enlargement (hepatomegaly). People with type VI are able to store
glycogen but not release it normally.
o Dietary recommendations for treating of GSD
Children diagnosed with GSD then dietary recommendations includes feeding
complex carbohydrates with each meal for maintaining blood sugar levels. Complex
carbohydrate includes puffed rice cereals, rice, wheat, barley and other carbohydrates.
Complex carbohydrates containing sugars needs to be avoided.
Type I
Frequent high-protein feedings in a day and meals as indicated above.
Type III
Frequent high-protein feedings in a day. High protein snack at night.
Type IV
Frequent high-protein feedings in daytime. Sugars that are allowed to be taken by
children diagnosed with GSD includes glucose, dextrose, dextrin, corn syrup, maltose,
stevia, barley syrup and so on. There should be distribution of monosaturated,
saturated and polysaturated fats [4]. Cholesterol intake should be limited to less than
300 mg/day. Beverages containing fructose, sucrose or lactose should be completely
avoided. Snacking ideas should also be free from any sweetened products.
Type VI
4
In this case, the body is unable to store or break down glucose as it should have. This
might lead to very low blood glucose levels during fasting periods. The liver
eventually gets enlarged.
Type III
It is an inborn error in metabolism due to gene mutation. In this case the liver keeps
storing glycogen for future use.
Type IV
In this case, the body is unable to store or break down glucose as it should have. This
might lead to very low blood glucose levels during fasting periods [1]. In case of
GSD, the liver might be storing excess of glycogen hampering it functionality.
Type VI
This causes liver enlargement (hepatomegaly). People with type VI are able to store
glycogen but not release it normally.
o Dietary recommendations for treating of GSD
Children diagnosed with GSD then dietary recommendations includes feeding
complex carbohydrates with each meal for maintaining blood sugar levels. Complex
carbohydrate includes puffed rice cereals, rice, wheat, barley and other carbohydrates.
Complex carbohydrates containing sugars needs to be avoided.
Type I
Frequent high-protein feedings in a day and meals as indicated above.
Type III
Frequent high-protein feedings in a day. High protein snack at night.
Type IV
Frequent high-protein feedings in daytime. Sugars that are allowed to be taken by
children diagnosed with GSD includes glucose, dextrose, dextrin, corn syrup, maltose,
stevia, barley syrup and so on. There should be distribution of monosaturated,
saturated and polysaturated fats [4]. Cholesterol intake should be limited to less than
300 mg/day. Beverages containing fructose, sucrose or lactose should be completely
avoided. Snacking ideas should also be free from any sweetened products.
Type VI
4
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Frequent high-protein feedings in daytime. Fruits contains fructose and should be
avoided and if consumed needs to be taken in very small amounts. Vegetables are low
in sugars and calories and needs to be included in every meal of children with Type I
GSD. Milk and diary products should be taken as much as possible. Milk intake
should be limited to 2 oz or less per day. Meats should be consumed with meals as
they are low in sugar content. However, meat cooked in sweet sauce should be
avoided. Also the meat should be cooked in low-fat method. Intake of dietary fats
should be limited to 20 -30% of total calorie intake.
5
avoided and if consumed needs to be taken in very small amounts. Vegetables are low
in sugars and calories and needs to be included in every meal of children with Type I
GSD. Milk and diary products should be taken as much as possible. Milk intake
should be limited to 2 oz or less per day. Meats should be consumed with meals as
they are low in sugar content. However, meat cooked in sweet sauce should be
avoided. Also the meat should be cooked in low-fat method. Intake of dietary fats
should be limited to 20 -30% of total calorie intake.
5
References
[1] Bali DS, Chen YT, Austin S, Goldstein JL. Glycogen storage disease type I.
InGeneReviews®[Internet] 2016 Aug 25. University of Washington, Seattle.
[2] Brown LM, Corrado MM, van der Ende RM, Derks TG, Chen MA, Siegel S, Hoyt K,
Correia CE, Lumpkin C, Flanagan TB, Carreras CT. Evaluation of glycogen storage disease
as a cause of ketotic hypoglycemia in children. Journal of Inherited Metabolic Disease:
Official Journal of the Society for the Study of Inborn Errors of Metabolism. 2015
May;38(3):489-93.
[3] Cho JH, Kim GY, Pan CJ, Anduaga J, Choi EJ, Mansfield BC, Chou JY. Downregulation
of SIRT1 signaling underlies hepatic autophagy impairment in glycogen storage disease type
Ia. PLoS genetics. 2017 May 30;13(5):e1006819.
[4] Chou JY, Jun HS, Mansfield BC. Type I glycogen storage diseases: disorders of the
glucose-6-phosphatase/glucose-6-phosphate transporter complexes. Journal of inherited
metabolic disease. 2015 May 1;38(3):511-9.
[5] Dagli A, Sentner CP, Weinstein DA. Glycogen storage disease type III.
InGeneReviews®[Internet] 2016 Dec 29. University of Washington, Seattle.
[6] Derks TG, Smit GP. Dietary management in glycogen storage disease type III: what is the
evidence?. Journal of inherited metabolic disease. 2015 May 1;38(3):545-50.
[7] Derks TG, van Rijn M. Lipids in hepatic glycogen storage diseases: pathophysiology,
monitoring of dietary management and future directions. Journal of inherited metabolic
disease. 2015 May 1;38(3):537-43.
[8] Magoulas PL, El-Hattab AW. Glycogen storage disease type IV.
InGeneReviews®[Internet] 2019 Aug 1. University of Washington, Seattle.
[9] Preisler N, Laforêt P, Madsen KL, Prahm KP, Hedermann G, Vissing CR, Galbo H,
Vissing J. Skeletal muscle metabolism is impaired during exercise in glycogen storage
disease type III. Neurology. 2015 Apr 28;84(17):1767-71.
[10] Sentner CP, Hoogeveen IJ, Weinstein DA, Santer R, Murphy E, McKiernan PJ,
Steuerwald U, Beauchamp NJ, Taybert J, Laforêt P, Petit FM. Glycogen storage disease type
III: diagnosis, genotype, management, clinical course and outcome. Journal of inherited
metabolic disease. 2016 Sep 1;39(5):697-704.
6
[1] Bali DS, Chen YT, Austin S, Goldstein JL. Glycogen storage disease type I.
InGeneReviews®[Internet] 2016 Aug 25. University of Washington, Seattle.
[2] Brown LM, Corrado MM, van der Ende RM, Derks TG, Chen MA, Siegel S, Hoyt K,
Correia CE, Lumpkin C, Flanagan TB, Carreras CT. Evaluation of glycogen storage disease
as a cause of ketotic hypoglycemia in children. Journal of Inherited Metabolic Disease:
Official Journal of the Society for the Study of Inborn Errors of Metabolism. 2015
May;38(3):489-93.
[3] Cho JH, Kim GY, Pan CJ, Anduaga J, Choi EJ, Mansfield BC, Chou JY. Downregulation
of SIRT1 signaling underlies hepatic autophagy impairment in glycogen storage disease type
Ia. PLoS genetics. 2017 May 30;13(5):e1006819.
[4] Chou JY, Jun HS, Mansfield BC. Type I glycogen storage diseases: disorders of the
glucose-6-phosphatase/glucose-6-phosphate transporter complexes. Journal of inherited
metabolic disease. 2015 May 1;38(3):511-9.
[5] Dagli A, Sentner CP, Weinstein DA. Glycogen storage disease type III.
InGeneReviews®[Internet] 2016 Dec 29. University of Washington, Seattle.
[6] Derks TG, Smit GP. Dietary management in glycogen storage disease type III: what is the
evidence?. Journal of inherited metabolic disease. 2015 May 1;38(3):545-50.
[7] Derks TG, van Rijn M. Lipids in hepatic glycogen storage diseases: pathophysiology,
monitoring of dietary management and future directions. Journal of inherited metabolic
disease. 2015 May 1;38(3):537-43.
[8] Magoulas PL, El-Hattab AW. Glycogen storage disease type IV.
InGeneReviews®[Internet] 2019 Aug 1. University of Washington, Seattle.
[9] Preisler N, Laforêt P, Madsen KL, Prahm KP, Hedermann G, Vissing CR, Galbo H,
Vissing J. Skeletal muscle metabolism is impaired during exercise in glycogen storage
disease type III. Neurology. 2015 Apr 28;84(17):1767-71.
[10] Sentner CP, Hoogeveen IJ, Weinstein DA, Santer R, Murphy E, McKiernan PJ,
Steuerwald U, Beauchamp NJ, Taybert J, Laforêt P, Petit FM. Glycogen storage disease type
III: diagnosis, genotype, management, clinical course and outcome. Journal of inherited
metabolic disease. 2016 Sep 1;39(5):697-704.
6
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 6
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





