Comprehensive Report: Total Hip Replacement (THR) in Medical Science
VerifiedAdded on 2020/07/22
|31
|14473
|325
Report
AI Summary
This report provides a comprehensive overview of Total Hip Replacement (THR), a crucial medical procedure involving the replacement of damaged hip joints with prosthetic components. It begins with an introduction to THR, its applications in addressing conditions like osteoarthritis and rheumatoid arthritis, and its positive impact on patients' quality of life. The report then delves into the anatomy of the hip joint, differentiating between cemented and cementless arthroplasties and highlighting the growing prevalence of THR surgeries globally. It discusses the biomechanical reasons behind implant failures, including adverse remodeling, excessive stress, and micro-motion. The report also explores the significance of femoral implant design, anatomical planes, and human gait cycles. Additionally, it details the structure of the femur and the phases of the human gait cycle. The document provides a detailed analysis of THR, offering valuable insights into this significant medical procedure, and is available on Desklib, a platform offering study resources such as past papers and assignment solutions.
Medical Science and bone
Replacement
Replacement
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Introduction
Total Hip Replacement (THR) or Arthroplasty is the medical procedure wherein
damaged cartilage and bone in the body is replaced with the prosthetic components. It is one of
the successful surgical procedures in the field of orthopaedic surgery. Patients who are suffering
health issues due to osteoarthritis, congenital deformities, avascular neurosis, rheumatoid
arthritis and post-traumatic disorder can get over rid of pain through hip joints restoration. THR
not only helps to reduce pain but also helps patients in better sleeping which helps in improving
their quality of life.
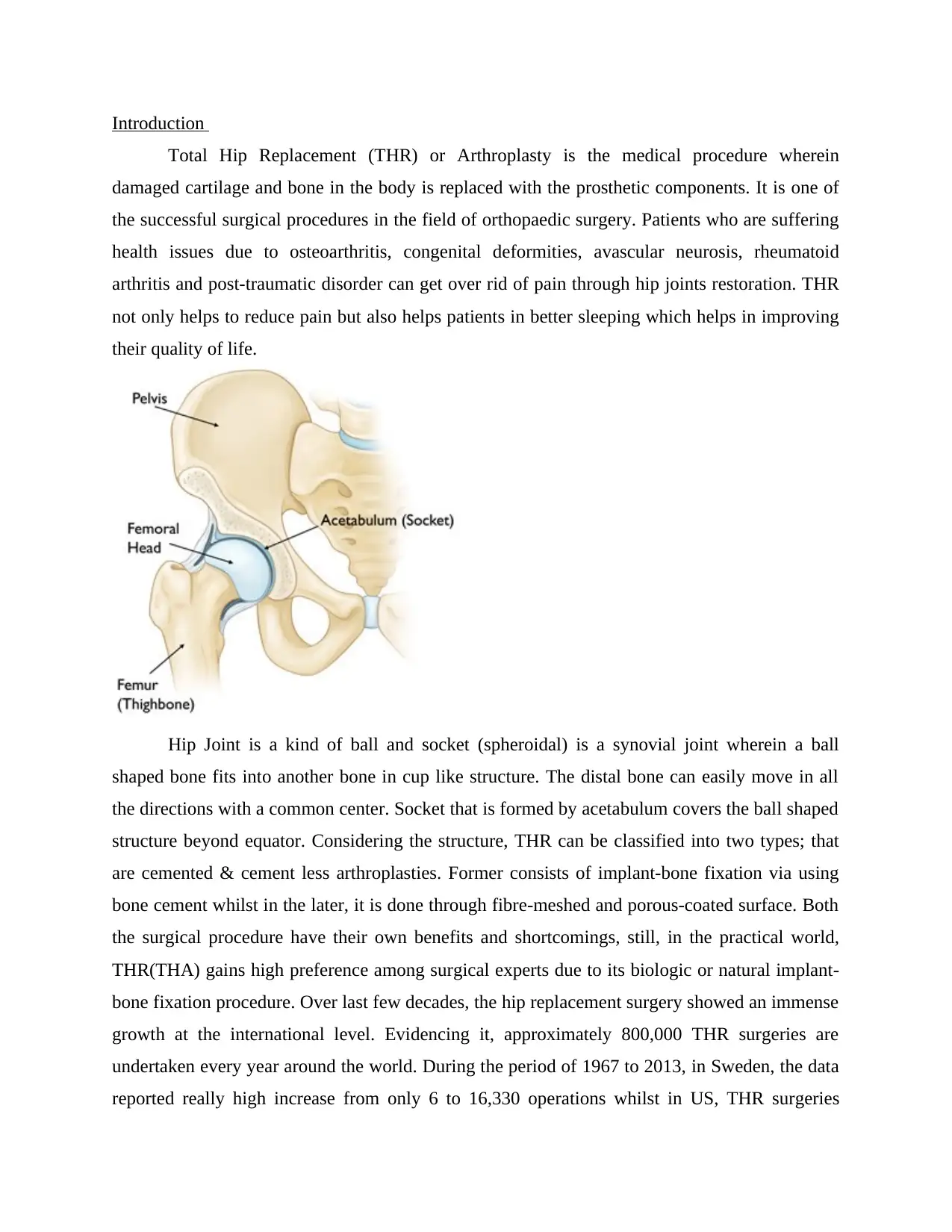
Hip Joint is a kind of ball and socket (spheroidal) is a synovial joint wherein a ball
shaped bone fits into another bone in cup like structure. The distal bone can easily move in all
the directions with a common center. Socket that is formed by acetabulum covers the ball shaped
structure beyond equator. Considering the structure, THR can be classified into two types; that
are cemented & cement less arthroplasties. Former consists of implant-bone fixation via using
bone cement whilst in the later, it is done through fibre-meshed and porous-coated surface. Both
the surgical procedure have their own benefits and shortcomings, still, in the practical world,
THR(THA) gains high preference among surgical experts due to its biologic or natural implant-
bone fixation procedure. Over last few decades, the hip replacement surgery showed an immense
growth at the international level. Evidencing it, approximately 800,000 THR surgeries are
undertaken every year around the world. During the period of 1967 to 2013, in Sweden, the data
reported really high increase from only 6 to 16,330 operations whilst in US, THR surgeries
Total Hip Replacement (THR) or Arthroplasty is the medical procedure wherein
damaged cartilage and bone in the body is replaced with the prosthetic components. It is one of
the successful surgical procedures in the field of orthopaedic surgery. Patients who are suffering
health issues due to osteoarthritis, congenital deformities, avascular neurosis, rheumatoid
arthritis and post-traumatic disorder can get over rid of pain through hip joints restoration. THR
not only helps to reduce pain but also helps patients in better sleeping which helps in improving
their quality of life.
Hip Joint is a kind of ball and socket (spheroidal) is a synovial joint wherein a ball
shaped bone fits into another bone in cup like structure. The distal bone can easily move in all
the directions with a common center. Socket that is formed by acetabulum covers the ball shaped
structure beyond equator. Considering the structure, THR can be classified into two types; that
are cemented & cement less arthroplasties. Former consists of implant-bone fixation via using
bone cement whilst in the later, it is done through fibre-meshed and porous-coated surface. Both
the surgical procedure have their own benefits and shortcomings, still, in the practical world,
THR(THA) gains high preference among surgical experts due to its biologic or natural implant-
bone fixation procedure. Over last few decades, the hip replacement surgery showed an immense
growth at the international level. Evidencing it, approximately 800,000 THR surgeries are
undertaken every year around the world. During the period of 1967 to 2013, in Sweden, the data
reported really high increase from only 6 to 16,330 operations whilst in US, THR surgeries
exceeded 285,000 surgeries per year however, total fractures reported by the end of year 2040 is
forecasted to go beyond 500,000. Australia reported 46.50% in the hip joint surgeries from 2003
and also projected the rate will go up in the forthcoming period. On the other side, in England &
Wales, National Joint Registry stated 620,400 THR between the period of 2003 to 2013, whereas
osteoarthritis reported 93% case. In this, the cement-less THR surgery reported increase from
16.8% to 42.5% with the decline in cemented THR from 60.5% to 33.2%. In India, National
Institute of Arthritis reported 470,000 incidence rate per year. Out of these, 65% of the reported
surgeries have been undertaken through cement-less. The surgical procedure reported a good
progress and success in the past few decades at a failure estimation of 10%. The failed cases is
founded in the first revision surgery which requires revision surgery after 10 years taking into
account patient health conditions & implant used. Although, there are multiple of reasons behind
such failure, still, most of the cases reported bio mechanical reasons for the same. Implant
indulged adverse remodeling & excessive implant interface stress, which in turn, leads to
progressive interface debonding that have been discovered as two most important bio mechanical
reasons for failure that compromised cement fewer prostheses' durability. Besides this, lack of
stability due to excessive micro-motion has a strong influence over the cement-less arthroplasties
which compromises biological attachment that took place between femur and implant.
The mechanism's cumulative or individual effect may result in gross aseptic loosening of the
implant or in cases of extreme scenario, femur fracture.
Keeping aside key aspects, including surgical procedure and patient conditions, the femoral
implant 's design or geometry is also known to be effective on these mechanisms (Huiskes and
Boeklagen, 1988; Viceconti et al., 2001).
Although a wide variety of cement-less femoral implants have a commercial availability in the
market (Fig. 1.1), for maximum of those the outcomes of design remain to be unexplored,
primarily due to a lack in the clinical data. The mechanical designs of hip implant, thus, can be
assessed preclinically and search for the optimal geometry may be conducted for the
minimization of the effects of all the failure in the mechanisms.
The solutions of the design of a prosthesis may be either structural or functional, or both.
However, investigations of the prosthesis have been centralised mostly on the structural aspects.
Considering the various structural aspects of hip prosthesis, its is determined that geometry of
the femoral implant plays a critical role in the outcome of design. Although the gross appearance
of a femoral stem has changed hardly since it was mentioned for the first time (Gluck, 1891), the
overall shape being non-primitive hence offers a lot of scope for a complex study by profile
alteration of stem transverse sections along the stem-length by usage of the state-of-the-art solid
modeling process and finite element (FE) analysis software.
forecasted to go beyond 500,000. Australia reported 46.50% in the hip joint surgeries from 2003
and also projected the rate will go up in the forthcoming period. On the other side, in England &
Wales, National Joint Registry stated 620,400 THR between the period of 2003 to 2013, whereas
osteoarthritis reported 93% case. In this, the cement-less THR surgery reported increase from
16.8% to 42.5% with the decline in cemented THR from 60.5% to 33.2%. In India, National
Institute of Arthritis reported 470,000 incidence rate per year. Out of these, 65% of the reported
surgeries have been undertaken through cement-less. The surgical procedure reported a good
progress and success in the past few decades at a failure estimation of 10%. The failed cases is
founded in the first revision surgery which requires revision surgery after 10 years taking into
account patient health conditions & implant used. Although, there are multiple of reasons behind
such failure, still, most of the cases reported bio mechanical reasons for the same. Implant
indulged adverse remodeling & excessive implant interface stress, which in turn, leads to
progressive interface debonding that have been discovered as two most important bio mechanical
reasons for failure that compromised cement fewer prostheses' durability. Besides this, lack of
stability due to excessive micro-motion has a strong influence over the cement-less arthroplasties
which compromises biological attachment that took place between femur and implant.
The mechanism's cumulative or individual effect may result in gross aseptic loosening of the
implant or in cases of extreme scenario, femur fracture.
Keeping aside key aspects, including surgical procedure and patient conditions, the femoral
implant 's design or geometry is also known to be effective on these mechanisms (Huiskes and
Boeklagen, 1988; Viceconti et al., 2001).
Although a wide variety of cement-less femoral implants have a commercial availability in the
market (Fig. 1.1), for maximum of those the outcomes of design remain to be unexplored,
primarily due to a lack in the clinical data. The mechanical designs of hip implant, thus, can be
assessed preclinically and search for the optimal geometry may be conducted for the
minimization of the effects of all the failure in the mechanisms.
The solutions of the design of a prosthesis may be either structural or functional, or both.
However, investigations of the prosthesis have been centralised mostly on the structural aspects.
Considering the various structural aspects of hip prosthesis, its is determined that geometry of
the femoral implant plays a critical role in the outcome of design. Although the gross appearance
of a femoral stem has changed hardly since it was mentioned for the first time (Gluck, 1891), the
overall shape being non-primitive hence offers a lot of scope for a complex study by profile
alteration of stem transverse sections along the stem-length by usage of the state-of-the-art solid
modeling process and finite element (FE) analysis software.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Moreover, with the arrival of the technically advanced high-performance computers, large
number of stem shapes may be assessed in a relatively small period, and one which is most
suited may be selected on basis of its predicted outcomes of design. Therefore, a combination of
suitable design optimization strategy with a solid modeling and FE analysis may result in a more
improved prosthesis design.
Optimization of shape (or geometry) is said to be a particular stage in structural optimization,
which deals with the search of the design domain with optimal configuration of it. (Fraternali et
al., 2011). In optimization of shape, introduction of design variables is done to control the
geometry of the structure and an FE model is required for methodology that changes during
optimization process. The growth in interest of optimization of shapes reflects a realization made
by the effectiveness of changes in shape for improvement in the structural performance. By
employing shape optimization as a design tool, evaluation of stem geometries can be done based
on bio-mechanical cost functions, framed on failure principles taken as a base. Therefore, a
suitable cost function must be formed, representing the effects on global level of these failure
mechanisms. It is necessary in order to search for optimal designs of the cement-less femoral
implant that would enhance prosthesis durability. However, for a priori and understanding the
failures associated with THA practically, a study on the hip joint's bio-mechanics is required.
1.2.1 Anatomical planes and directions
Hip joint bio-mechanics may form a basic understanding of the human anatomy. Typical
orientations of the human body of different anatomical planes are presented in the Fig. 1.2a. The
transverse (axial or horizontal) plane which is noted to be parallel to the ground, apart the
superior (top) from the inferior (bottom) part of the human body. The coronal (frontal) plane,
with perpendicular anatomy towards the ground, separates the anterior (front) from the posterior
(back).
The sagittal (median) plane is noted to be perpendicular to the transverse and coronal plane, and
it separates the left part of the body from the right part. The medial and lateral directions refers to
the direction towards and away from the mid-line of the body respectively (Fig. 1.2b). The
direction towards the front and the back side of the body are termed as The ‘anterior’ and
‘posterior’ directions respectively. The term ‘proximal’ describes the direction which is towards
the limbs origin, while the part which is away from the origin of the limbs is known as the
‘distal’.
This clinical definition done is based on their proximity with their respect to the head. The
‘superior’ and ‘inferior’ directions point towards the top and the bottom parts of the body,
respectively.
Fig. 1.2:
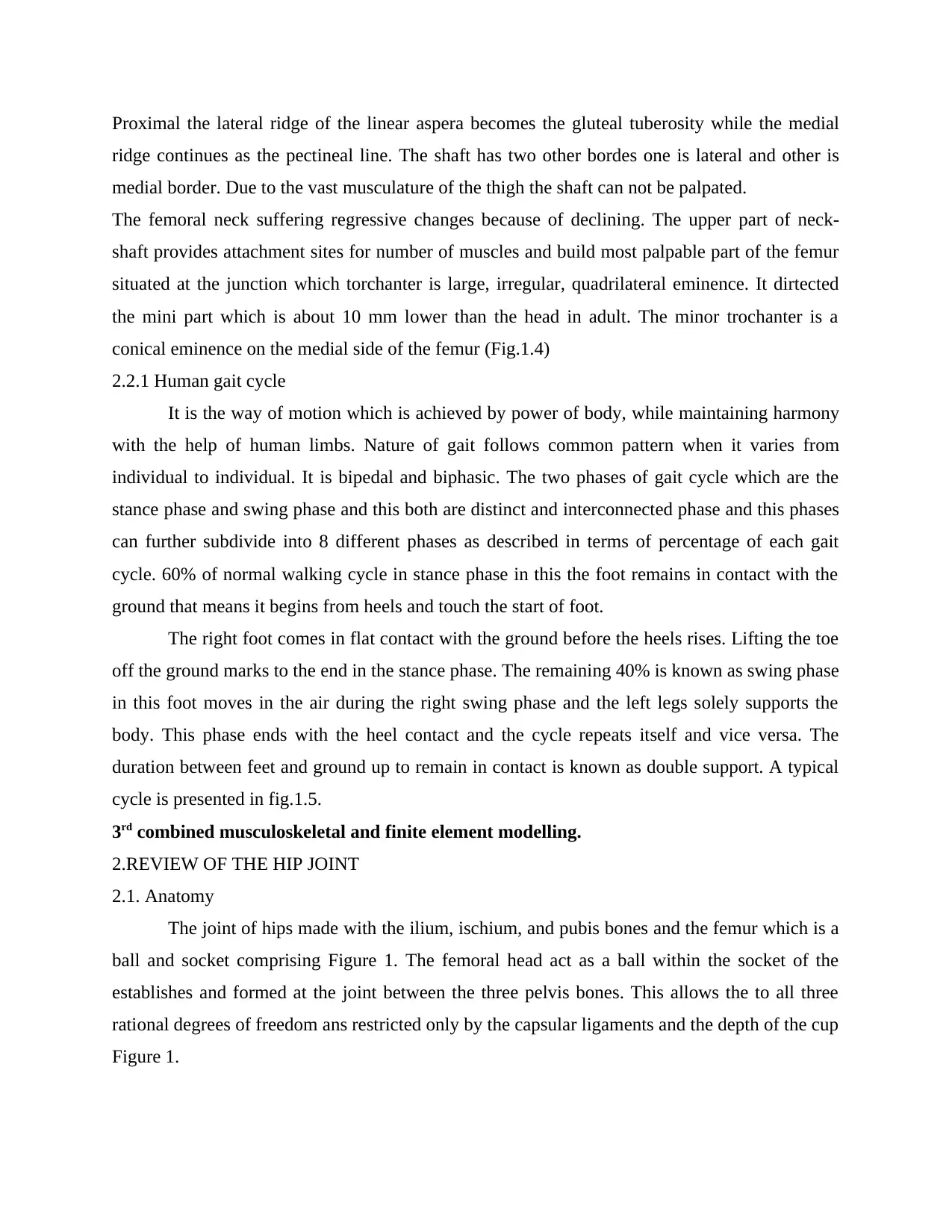
1.2.2 Hip anatomy
The hip joint forms the primary connection between the bones of the lower and upper limbs of
the human skeletal system, which is scientifically referred as the acetabulofemoral joint. The
hip-joint is said to support weight of the body and transfer load from upper limb to the lower
limb. A ball (femoral head) and a hemi-spherical socket (acetabulum) (Fig. 1.3) form the main
parts of this joint.
number of stem shapes may be assessed in a relatively small period, and one which is most
suited may be selected on basis of its predicted outcomes of design. Therefore, a combination of
suitable design optimization strategy with a solid modeling and FE analysis may result in a more
improved prosthesis design.
Optimization of shape (or geometry) is said to be a particular stage in structural optimization,
which deals with the search of the design domain with optimal configuration of it. (Fraternali et
al., 2011). In optimization of shape, introduction of design variables is done to control the
geometry of the structure and an FE model is required for methodology that changes during
optimization process. The growth in interest of optimization of shapes reflects a realization made
by the effectiveness of changes in shape for improvement in the structural performance. By
employing shape optimization as a design tool, evaluation of stem geometries can be done based
on bio-mechanical cost functions, framed on failure principles taken as a base. Therefore, a
suitable cost function must be formed, representing the effects on global level of these failure
mechanisms. It is necessary in order to search for optimal designs of the cement-less femoral
implant that would enhance prosthesis durability. However, for a priori and understanding the
failures associated with THA practically, a study on the hip joint's bio-mechanics is required.
1.2.1 Anatomical planes and directions
Hip joint bio-mechanics may form a basic understanding of the human anatomy. Typical
orientations of the human body of different anatomical planes are presented in the Fig. 1.2a. The
transverse (axial or horizontal) plane which is noted to be parallel to the ground, apart the
superior (top) from the inferior (bottom) part of the human body. The coronal (frontal) plane,
with perpendicular anatomy towards the ground, separates the anterior (front) from the posterior
(back).
The sagittal (median) plane is noted to be perpendicular to the transverse and coronal plane, and
it separates the left part of the body from the right part. The medial and lateral directions refers to
the direction towards and away from the mid-line of the body respectively (Fig. 1.2b). The
direction towards the front and the back side of the body are termed as The ‘anterior’ and
‘posterior’ directions respectively. The term ‘proximal’ describes the direction which is towards
the limbs origin, while the part which is away from the origin of the limbs is known as the
‘distal’.
This clinical definition done is based on their proximity with their respect to the head. The
‘superior’ and ‘inferior’ directions point towards the top and the bottom parts of the body,
respectively.
Fig. 1.2:
1.2.2 Hip anatomy
The hip joint forms the primary connection between the bones of the lower and upper limbs of
the human skeletal system, which is scientifically referred as the acetabulofemoral joint. The
hip-joint is said to support weight of the body and transfer load from upper limb to the lower
limb. A ball (femoral head) and a hemi-spherical socket (acetabulum) (Fig. 1.3) form the main
parts of this joint.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Fig. 1.3:
The femoral head is located at the top of the thigh bone (femur) and it is made to fit into the
acetabulum in the pelvis by means ligaments (hip capsule), a band of tissue. The function of
ligaments is also to provide stability to the joint.
The movement process is facilitated by a smooth durable cover of articular cartilage (a protein
substance) which cushions the ends of the bones between the two bones ‘surfaces (femoral head
and acetabulum).
The hip joint's remaining surface is covered by a thin, smooth tissue called the synovial
membrane. In a healthy hip, this membrane's function is to generate a small amount of fluid that
lubricates and improves frictional resistance in the hip joint. All of these parts of the hip-joint
work in simultaneously, allowing easy, painless moving of hip.
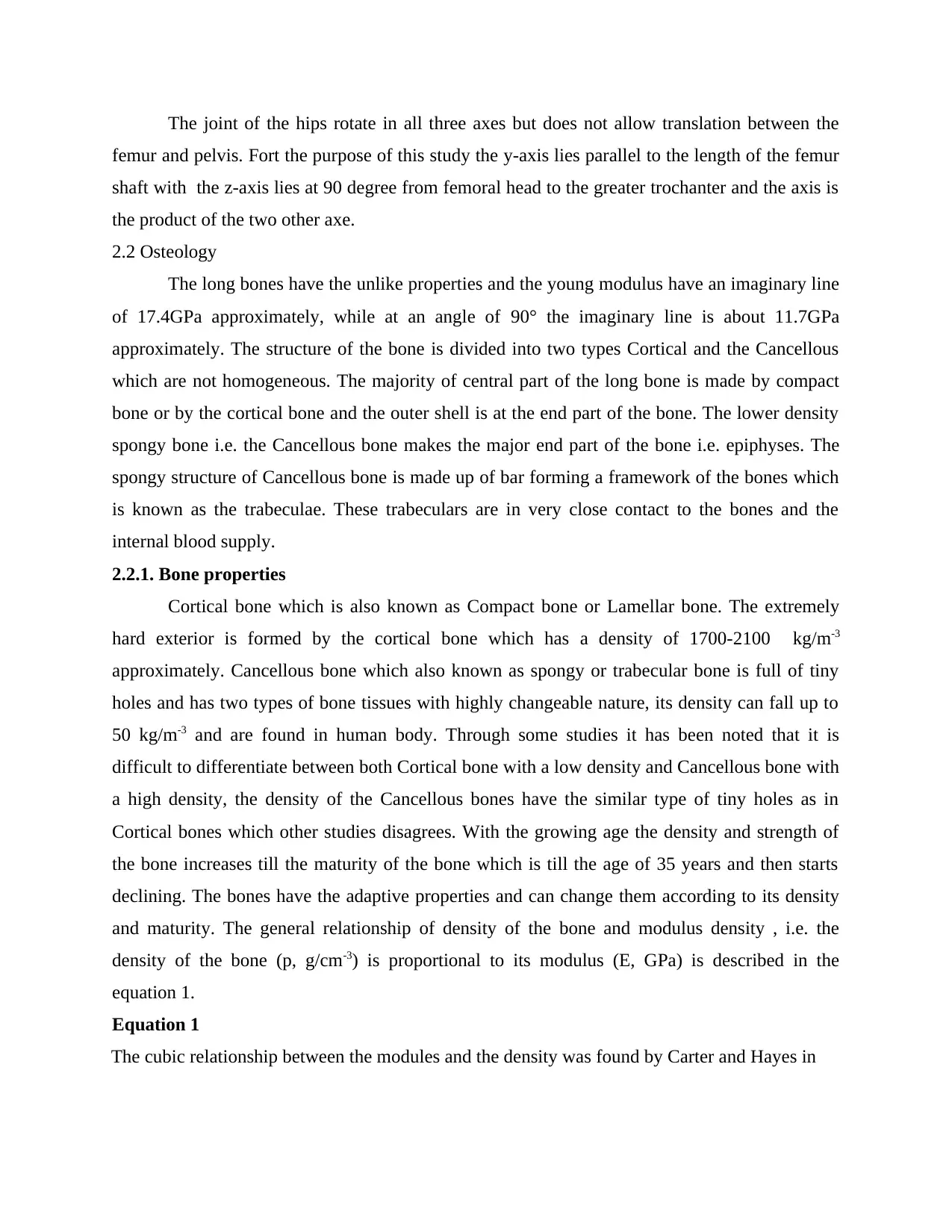
1.2.3 STRUCTURE OF FEMUR
It is the longest and stronger bone in the human skeletal system. Body weight is
supported by the femurs during many activities like running, jumping, walking, standing etc. It
consists two part, the primarily part is diaphysis or central shaft and two wider and rounded
bulges known as epiphyses (figure.1.4). Each epiphysis attach with diaphysis through conical
regions known as metaphysis. The diaphysis is generally belonged to hard cortical bone with a
small spongy core while the epiphyses and metaphysis contain mostly cancellous or spongy bone
within a thin shell of cortical bone. A head, a neck, a greater trochanter and lesser trochanter are
the nearest part of the femur the transition area between the head and neck is quite rough due the
attachment of muscles and hips joint capsule.(figure.1.4).
The head is conducted upward, medial-ward, and a little ahead and it designs 2/3 of a
sphere and surface of it is smooth and cover with ossein tissue in the fresh condition excluding
depression, clinically known as fovea capitis femoris. The flattened pyramidal part of the bone is
neck which connecting the head with femoral shaft and assemble with the recent wide corner
opening medial ward. The angle of affection of neck to the pole in the front of plane is known as
neck-shaft angle. The neck jutting a little ahead due to change in femur body by projecting
upward and middle side. The angle of inclination of the neck shaft in cross plan is also known as
the angle of interversion. Femur bone of neck has an irregular cross-section and spheroid at the
upper end and approximately ovoid with major and minor axes in the ratio about 1.6 at the lower
end which is close to femoral shaft.
The body of femur is long, slender and almost cylindrical in form. It is little arched, to be
convex in front, and concave behind, where it is strengthened by a prominent longitudinal ridge.
The femoral head is located at the top of the thigh bone (femur) and it is made to fit into the
acetabulum in the pelvis by means ligaments (hip capsule), a band of tissue. The function of
ligaments is also to provide stability to the joint.
The movement process is facilitated by a smooth durable cover of articular cartilage (a protein
substance) which cushions the ends of the bones between the two bones ‘surfaces (femoral head
and acetabulum).
The hip joint's remaining surface is covered by a thin, smooth tissue called the synovial
membrane. In a healthy hip, this membrane's function is to generate a small amount of fluid that
lubricates and improves frictional resistance in the hip joint. All of these parts of the hip-joint
work in simultaneously, allowing easy, painless moving of hip.
1.2.3 STRUCTURE OF FEMUR
It is the longest and stronger bone in the human skeletal system. Body weight is
supported by the femurs during many activities like running, jumping, walking, standing etc. It
consists two part, the primarily part is diaphysis or central shaft and two wider and rounded
bulges known as epiphyses (figure.1.4). Each epiphysis attach with diaphysis through conical
regions known as metaphysis. The diaphysis is generally belonged to hard cortical bone with a
small spongy core while the epiphyses and metaphysis contain mostly cancellous or spongy bone
within a thin shell of cortical bone. A head, a neck, a greater trochanter and lesser trochanter are
the nearest part of the femur the transition area between the head and neck is quite rough due the
attachment of muscles and hips joint capsule.(figure.1.4).
The head is conducted upward, medial-ward, and a little ahead and it designs 2/3 of a
sphere and surface of it is smooth and cover with ossein tissue in the fresh condition excluding
depression, clinically known as fovea capitis femoris. The flattened pyramidal part of the bone is
neck which connecting the head with femoral shaft and assemble with the recent wide corner
opening medial ward. The angle of affection of neck to the pole in the front of plane is known as
neck-shaft angle. The neck jutting a little ahead due to change in femur body by projecting
upward and middle side. The angle of inclination of the neck shaft in cross plan is also known as
the angle of interversion. Femur bone of neck has an irregular cross-section and spheroid at the
upper end and approximately ovoid with major and minor axes in the ratio about 1.6 at the lower
end which is close to femoral shaft.
The body of femur is long, slender and almost cylindrical in form. It is little arched, to be
convex in front, and concave behind, where it is strengthened by a prominent longitudinal ridge.
Proximal the lateral ridge of the linear aspera becomes the gluteal tuberosity while the medial
ridge continues as the pectineal line. The shaft has two other bordes one is lateral and other is
medial border. Due to the vast musculature of the thigh the shaft can not be palpated.
The femoral neck suffering regressive changes because of declining. The upper part of neck-
shaft provides attachment sites for number of muscles and build most palpable part of the femur
situated at the junction which torchanter is large, irregular, quadrilateral eminence. It dirtected
the mini part which is about 10 mm lower than the head in adult. The minor trochanter is a
conical eminence on the medial side of the femur (Fig.1.4)
2.2.1 Human gait cycle
It is the way of motion which is achieved by power of body, while maintaining harmony
with the help of human limbs. Nature of gait follows common pattern when it varies from
individual to individual. It is bipedal and biphasic. The two phases of gait cycle which are the
stance phase and swing phase and this both are distinct and interconnected phase and this phases
can further subdivide into 8 different phases as described in terms of percentage of each gait
cycle. 60% of normal walking cycle in stance phase in this the foot remains in contact with the
ground that means it begins from heels and touch the start of foot.
The right foot comes in flat contact with the ground before the heels rises. Lifting the toe
off the ground marks to the end in the stance phase. The remaining 40% is known as swing phase
in this foot moves in the air during the right swing phase and the left legs solely supports the
body. This phase ends with the heel contact and the cycle repeats itself and vice versa. The
duration between feet and ground up to remain in contact is known as double support. A typical
cycle is presented in fig.1.5.
3rd combined musculoskeletal and finite element modelling.
2.REVIEW OF THE HIP JOINT
2.1. Anatomy
The joint of hips made with the ilium, ischium, and pubis bones and the femur which is a
ball and socket comprising Figure 1. The femoral head act as a ball within the socket of the
establishes and formed at the joint between the three pelvis bones. This allows the to all three
rational degrees of freedom ans restricted only by the capsular ligaments and the depth of the cup
Figure 1.
ridge continues as the pectineal line. The shaft has two other bordes one is lateral and other is
medial border. Due to the vast musculature of the thigh the shaft can not be palpated.
The femoral neck suffering regressive changes because of declining. The upper part of neck-
shaft provides attachment sites for number of muscles and build most palpable part of the femur
situated at the junction which torchanter is large, irregular, quadrilateral eminence. It dirtected
the mini part which is about 10 mm lower than the head in adult. The minor trochanter is a
conical eminence on the medial side of the femur (Fig.1.4)
2.2.1 Human gait cycle
It is the way of motion which is achieved by power of body, while maintaining harmony
with the help of human limbs. Nature of gait follows common pattern when it varies from
individual to individual. It is bipedal and biphasic. The two phases of gait cycle which are the
stance phase and swing phase and this both are distinct and interconnected phase and this phases
can further subdivide into 8 different phases as described in terms of percentage of each gait
cycle. 60% of normal walking cycle in stance phase in this the foot remains in contact with the
ground that means it begins from heels and touch the start of foot.
The right foot comes in flat contact with the ground before the heels rises. Lifting the toe
off the ground marks to the end in the stance phase. The remaining 40% is known as swing phase
in this foot moves in the air during the right swing phase and the left legs solely supports the
body. This phase ends with the heel contact and the cycle repeats itself and vice versa. The
duration between feet and ground up to remain in contact is known as double support. A typical
cycle is presented in fig.1.5.
3rd combined musculoskeletal and finite element modelling.
2.REVIEW OF THE HIP JOINT
2.1. Anatomy
The joint of hips made with the ilium, ischium, and pubis bones and the femur which is a
ball and socket comprising Figure 1. The femoral head act as a ball within the socket of the
establishes and formed at the joint between the three pelvis bones. This allows the to all three
rational degrees of freedom ans restricted only by the capsular ligaments and the depth of the cup
Figure 1.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
The joint of the hips rotate in all three axes but does not allow translation between the
femur and pelvis. Fort the purpose of this study the y-axis lies parallel to the length of the femur
shaft with the z-axis lies at 90 degree from femoral head to the greater trochanter and the axis is
the product of the two other axe.
2.2 Osteology
The long bones have the unlike properties and the young modulus have an imaginary line
of 17.4GPa approximately, while at an angle of 90° the imaginary line is about 11.7GPa
approximately. The structure of the bone is divided into two types Cortical and the Cancellous
which are not homogeneous. The majority of central part of the long bone is made by compact
bone or by the cortical bone and the outer shell is at the end part of the bone. The lower density
spongy bone i.e. the Cancellous bone makes the major end part of the bone i.e. epiphyses. The
spongy structure of Cancellous bone is made up of bar forming a framework of the bones which
is known as the trabeculae. These trabeculars are in very close contact to the bones and the
internal blood supply.
2.2.1. Bone properties
Cortical bone which is also known as Compact bone or Lamellar bone. The extremely
hard exterior is formed by the cortical bone which has a density of 1700-2100 kg/m-3
approximately. Cancellous bone which also known as spongy or trabecular bone is full of tiny
holes and has two types of bone tissues with highly changeable nature, its density can fall up to
50 kg/m-3 and are found in human body. Through some studies it has been noted that it is
difficult to differentiate between both Cortical bone with a low density and Cancellous bone with
a high density, the density of the Cancellous bones have the similar type of tiny holes as in
Cortical bones which other studies disagrees. With the growing age the density and strength of
the bone increases till the maturity of the bone which is till the age of 35 years and then starts
declining. The bones have the adaptive properties and can change them according to its density
and maturity. The general relationship of density of the bone and modulus density , i.e. the
density of the bone (p, g/cm-3) is proportional to its modulus (E, GPa) is described in the
equation 1.
Equation 1
The cubic relationship between the modules and the density was found by Carter and Hayes in
femur and pelvis. Fort the purpose of this study the y-axis lies parallel to the length of the femur
shaft with the z-axis lies at 90 degree from femoral head to the greater trochanter and the axis is
the product of the two other axe.
2.2 Osteology
The long bones have the unlike properties and the young modulus have an imaginary line
of 17.4GPa approximately, while at an angle of 90° the imaginary line is about 11.7GPa
approximately. The structure of the bone is divided into two types Cortical and the Cancellous
which are not homogeneous. The majority of central part of the long bone is made by compact
bone or by the cortical bone and the outer shell is at the end part of the bone. The lower density
spongy bone i.e. the Cancellous bone makes the major end part of the bone i.e. epiphyses. The
spongy structure of Cancellous bone is made up of bar forming a framework of the bones which
is known as the trabeculae. These trabeculars are in very close contact to the bones and the
internal blood supply.
2.2.1. Bone properties
Cortical bone which is also known as Compact bone or Lamellar bone. The extremely
hard exterior is formed by the cortical bone which has a density of 1700-2100 kg/m-3
approximately. Cancellous bone which also known as spongy or trabecular bone is full of tiny
holes and has two types of bone tissues with highly changeable nature, its density can fall up to
50 kg/m-3 and are found in human body. Through some studies it has been noted that it is
difficult to differentiate between both Cortical bone with a low density and Cancellous bone with
a high density, the density of the Cancellous bones have the similar type of tiny holes as in
Cortical bones which other studies disagrees. With the growing age the density and strength of
the bone increases till the maturity of the bone which is till the age of 35 years and then starts
declining. The bones have the adaptive properties and can change them according to its density
and maturity. The general relationship of density of the bone and modulus density , i.e. the
density of the bone (p, g/cm-3) is proportional to its modulus (E, GPa) is described in the
equation 1.
Equation 1
The cubic relationship between the modules and the density was found by Carter and Hayes in
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

(1977). Rice et a. (Rice et al. 1988) a slightly better correlation was found with a squared
relationship and also it was found in other studies the power, p, is slightly less than 2
(Hodgskinson and Currey 1992 ; Morgan et al. 2003). According to the equation 2 it was also
found by Carter and Hayes that the modulus – density was marked for a effect by the strain rate.
Equation 2
While it should be noted that this is one of the many relationships to found be between modulus
and density. A large degree of variation between studies was found between variation and studies
when a review of the potential relationship of modulus and density of bone was conducted by
Helgason et al. 2008)
The dependency of the bone density has been shown to depend on the tensile strength and yield
strength of the bone (Figure 4) (carter and Hayes 1977; Kopperdahl and keaveny 1998; cowin
2001). The bone strength is considered to be dependent on its density, whereas the yield strain is
noted to be independent of elastic modulus, yield stress and density (Cowin 2001; Morgan and
keaveny 2001), however a variation has been reported in the vaiues of yield strain. Across
severai anatomicai sites it researches conducted by kopperdahl et al. (1998) the yield
compression for cancellous bone was found to be 8400pe (± 1000 s.d.) and between 7000pe
(±500 s.d.) and 8500pe (±1000 s.d.) by Morgan rt al. (2001). kopperdahl et al. found the yield
strain of cancellous bone to be 7800pe and for Morgan et al. it varied between 6100pe (±500 s.d.)
and 7000pe (±500 s.d.) in tension. In Ebacher et al. (2007) research it was found that cancellous
bone is more ductile than cortical bone with an Ultimate strain of approx 10000-15000pe. The
cortical bone was found to be having a yield strain of approx 4000pe in tension and yield strain
was higher and more variable in compression than in tension, between 6500pe and 10000pe.
Figure 4
Strain gauges were attached to human tibia by Lanyon et a. (1975) to measure the surface strain
during normal walking. A variation was noted in the surface strain through gait cycle from 640pe
(±70) to 2370pe (±180) in tension and it peaked in the strain when the foot left the floor. The
compressive strain measured a hike as the load carried by the subject was increased and strain
hiked to highest when the subject was seen running on a treadmill 8470pe (±590). the bone on
relationship and also it was found in other studies the power, p, is slightly less than 2
(Hodgskinson and Currey 1992 ; Morgan et al. 2003). According to the equation 2 it was also
found by Carter and Hayes that the modulus – density was marked for a effect by the strain rate.
Equation 2
While it should be noted that this is one of the many relationships to found be between modulus
and density. A large degree of variation between studies was found between variation and studies
when a review of the potential relationship of modulus and density of bone was conducted by
Helgason et al. 2008)
The dependency of the bone density has been shown to depend on the tensile strength and yield
strength of the bone (Figure 4) (carter and Hayes 1977; Kopperdahl and keaveny 1998; cowin
2001). The bone strength is considered to be dependent on its density, whereas the yield strain is
noted to be independent of elastic modulus, yield stress and density (Cowin 2001; Morgan and
keaveny 2001), however a variation has been reported in the vaiues of yield strain. Across
severai anatomicai sites it researches conducted by kopperdahl et al. (1998) the yield
compression for cancellous bone was found to be 8400pe (± 1000 s.d.) and between 7000pe
(±500 s.d.) and 8500pe (±1000 s.d.) by Morgan rt al. (2001). kopperdahl et al. found the yield
strain of cancellous bone to be 7800pe and for Morgan et al. it varied between 6100pe (±500 s.d.)
and 7000pe (±500 s.d.) in tension. In Ebacher et al. (2007) research it was found that cancellous
bone is more ductile than cortical bone with an Ultimate strain of approx 10000-15000pe. The
cortical bone was found to be having a yield strain of approx 4000pe in tension and yield strain
was higher and more variable in compression than in tension, between 6500pe and 10000pe.
Figure 4
Strain gauges were attached to human tibia by Lanyon et a. (1975) to measure the surface strain
during normal walking. A variation was noted in the surface strain through gait cycle from 640pe
(±70) to 2370pe (±180) in tension and it peaked in the strain when the foot left the floor. The
compressive strain measured a hike as the load carried by the subject was increased and strain
hiked to highest when the subject was seen running on a treadmill 8470pe (±590). the bone on

the surface of tibia is cortical bone during the walking process the strain noted was lower than
the yield strain. In an investigation Keyak and Rossi (2000) investigated which failure criteria
could most accurately predict the failure of bone using finite element models. A finite element
model was taken to compare the experimental results of different failure criteria which included
maximum and normal strain, stress and shear strain. The predictions made by all the failure
criteria included the load which caused femoral fracture in the vitro, when using different loading
scenarios the shear strain and hoffmann criterion was found to be robust. Schileo et al. (2008)
also compared failure criteria; von Mises stress, maximum principle stress and principal strain.
The failure of bone was found in all three criteria at the location of fracture. When a compressive
principle strain limit 10400pe nad tensile limit 7300pe was used, maximum principle strain
criteria had a prediction of localised failure, in the femur, which corresponded to experiments.
Wolff's law states that in response to mechanical stimulus the bone density and orientation of
trabeculae changes. Remodelling of bone adapt is based on Wolff's law and is used to predict
where bone will be deposited due to stress stimulus. The density in the bone is increased by
deposition and the bone is resorbed In area of low stress and density lowered (figure 5). between
the threshold values high and low there is lazy or dead zone in which change in stress rate doesnt
change the bone. It was found by Beaupre et al. (1990) that the DSS was approximately
50MP/day which generates a cyclic normal strain of approx 400pe assuming 10000 walking
cycles a day. Based on the adaptive model in fig 5 using 20% stress stimulus as the width of lazy
zone a calculation was on done on change in bone density and predicted a bone density
distribution consistent with that found in vivo.
Figure 5
Myology
2.3.1.Structure
Ligament, a fibrous tissue that connect bones together, and muscle are responsible for movement
and control in the body. The whole of the joint of hip ligament is covered by capsular ligament.
Movement of the skeleton is created by skeletal muscle. Perimsysuim (figure 6) is a collectively
wrapped sheath of muscle belly fibers bundled together. Tendons are made to provide connection
between the muscle belly and the bones on which they act. Spiral cord contain neurons tha fire
the yield strain. In an investigation Keyak and Rossi (2000) investigated which failure criteria
could most accurately predict the failure of bone using finite element models. A finite element
model was taken to compare the experimental results of different failure criteria which included
maximum and normal strain, stress and shear strain. The predictions made by all the failure
criteria included the load which caused femoral fracture in the vitro, when using different loading
scenarios the shear strain and hoffmann criterion was found to be robust. Schileo et al. (2008)
also compared failure criteria; von Mises stress, maximum principle stress and principal strain.
The failure of bone was found in all three criteria at the location of fracture. When a compressive
principle strain limit 10400pe nad tensile limit 7300pe was used, maximum principle strain
criteria had a prediction of localised failure, in the femur, which corresponded to experiments.
Wolff's law states that in response to mechanical stimulus the bone density and orientation of
trabeculae changes. Remodelling of bone adapt is based on Wolff's law and is used to predict
where bone will be deposited due to stress stimulus. The density in the bone is increased by
deposition and the bone is resorbed In area of low stress and density lowered (figure 5). between
the threshold values high and low there is lazy or dead zone in which change in stress rate doesnt
change the bone. It was found by Beaupre et al. (1990) that the DSS was approximately
50MP/day which generates a cyclic normal strain of approx 400pe assuming 10000 walking
cycles a day. Based on the adaptive model in fig 5 using 20% stress stimulus as the width of lazy
zone a calculation was on done on change in bone density and predicted a bone density
distribution consistent with that found in vivo.
Figure 5
Myology
2.3.1.Structure
Ligament, a fibrous tissue that connect bones together, and muscle are responsible for movement
and control in the body. The whole of the joint of hip ligament is covered by capsular ligament.
Movement of the skeleton is created by skeletal muscle. Perimsysuim (figure 6) is a collectively
wrapped sheath of muscle belly fibers bundled together. Tendons are made to provide connection
between the muscle belly and the bones on which they act. Spiral cord contain neurons tha fire
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

electrical impulses down the pathways called axons to muscle fibers. There can be increase on
muscle fibers when additional motor units are activated. (Whiting and zernicke 1998).
Figure 6/ Figure 7
Twenty muscle cross the hip joint approx (Figure 7). All these muscles have different attachment
points in the skeleton which allows different actions and muscles functions to take place Table 1.
Normally a skeleton muscle is attached to bone in the body by tendons minimum two points,
known as origin and insertion points. The origin point end is attached to a relatively stationary
part of the body muscle. The area which is moved by contraction muscle is called insertion point.
It is noted that a muscle may not always have two specific points that they are attached to, many
muscles have large area on the bone on to which the tendon is attached. Such a muscle is gluteus
maximus.
Figure 7
2.3.2 Generation of muscle Force
Figure 8
The muscle strength is directly related to the intellectual cross sectional area of muscle
and alignment of muscle fibres. Further, the muscle fibre direction is vertical to the cross
sectional area of muscle. Moreover, there are two elements of muscle tension which are, the
active tension and the passive tension. Whereas, the active tension is produced by the activity of
muscle fibre while the passive tension is generated by the physical lengthening of tendon and
muscle. Therefore, when the length of tension increases by the force of muscle it leads to
increase the strength of muscle and then continuously decrease the muscle extension till there is
an increase in passive tension. The muscle force is also equivalent to the velocity of the
contraction. Hence, the Hill’s muscle model related to velocity and force was experimentally
figured by Bressler and Clinch (1974) using the sartorii muscle from a toad.
Figure 9:
The result of force vector for a muscle can be analysed as the line of action which is
affected by the orientation of the fibres in the muscle and in the routes of the muscles presented
in the human body. The path of muscles in the body in not the direct route to joints instead it is
interrupted by the soft tissues or by the part of bones. Moreover, it can be said that when the
skeleton of body moves there are chances that the blocked parts of the body change its position
muscle fibers when additional motor units are activated. (Whiting and zernicke 1998).
Figure 6/ Figure 7
Twenty muscle cross the hip joint approx (Figure 7). All these muscles have different attachment
points in the skeleton which allows different actions and muscles functions to take place Table 1.
Normally a skeleton muscle is attached to bone in the body by tendons minimum two points,
known as origin and insertion points. The origin point end is attached to a relatively stationary
part of the body muscle. The area which is moved by contraction muscle is called insertion point.
It is noted that a muscle may not always have two specific points that they are attached to, many
muscles have large area on the bone on to which the tendon is attached. Such a muscle is gluteus
maximus.
Figure 7
2.3.2 Generation of muscle Force
Figure 8
The muscle strength is directly related to the intellectual cross sectional area of muscle
and alignment of muscle fibres. Further, the muscle fibre direction is vertical to the cross
sectional area of muscle. Moreover, there are two elements of muscle tension which are, the
active tension and the passive tension. Whereas, the active tension is produced by the activity of
muscle fibre while the passive tension is generated by the physical lengthening of tendon and
muscle. Therefore, when the length of tension increases by the force of muscle it leads to
increase the strength of muscle and then continuously decrease the muscle extension till there is
an increase in passive tension. The muscle force is also equivalent to the velocity of the
contraction. Hence, the Hill’s muscle model related to velocity and force was experimentally
figured by Bressler and Clinch (1974) using the sartorii muscle from a toad.
Figure 9:
The result of force vector for a muscle can be analysed as the line of action which is
affected by the orientation of the fibres in the muscle and in the routes of the muscles presented
in the human body. The path of muscles in the body in not the direct route to joints instead it is
interrupted by the soft tissues or by the part of bones. Moreover, it can be said that when the
skeleton of body moves there are chances that the blocked parts of the body change its position
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
with the relative changes in muscle which will affects the muscle's path. Besides, the Pennate
muscle in the body are made up of fibre which do not run in one line and further fluctuates the
strength of muscle. The angle made between the line of action of muscle and fibre is termed as
Pen nation angle. Therefore, the angle is used to compare the length of muscles fibres which is
used in a Hill type muscle model to calculate the strength of the muscle.
2.3.4. Muscle injury and repair
Muscles injury in minimizes the ability to produce force and during hip arthroplasty
muscles can be divided or dissected. Muscle lacerations heal but can be rebuilt with the use of
dense connective scar tissue instead of muscle tissue which minimizes the functions of muscle.
Lacerations which intersect the muscle fibres are the most harmful type of laceration for
recovery of muscle, specially when they dissect blood supply to areas of the muscle. Further,
there are three stages of muscle recovery; degeneration and inflammation, regeneration and
fibrosis. Hence, in fibrosis stage scar tissue is formed which minimizes the strength of the healed
muscle. Generally, this stage starts in two to three weeks after it is injured and it takes more than
6 weeks for normal functioning.
Besides, the mechanical and biological properties of a muscle can be identified to
investigating how the muscle is affected like by, laceration and healing. The test to is to find the
ways to recover from muscle injury, various methods used by doctors recovery of muscles after
laceration and also it will evaluate the weakest muscle in the skeleton. The elongation of the
healed muscles was measured by applying pressure to injured muscle. Scholars found a
minimizing technique in both type of lengths of muscle, the one which is injured and the non
operated muscle which is also termed as contralateral leg. Further, the failure load is identified
by recovering only to approximately 50% of the contralateral muscle which is attributed to the
atrophy of the muscle instead of damage caused by the laceration. Moreover, the minimization in
elongation is related to the scar tissue which is formed at the laceration site as the scar had a
higher elastic modulus.
In contrast to the fluctuation mechanical properties the biological response of a muscle
can also be affected by injured muscle. According to researcher the force of muscle can be
minimized by some injury so repair methods used by Huard et al., (2002) to measure the
strengths of muscle. Moreover, Garrett and Duncan (1988) used the extensor digitorum muscle
of the New Zealand white rabbit to identify the impact of full and partial laceration on strength
muscle in the body are made up of fibre which do not run in one line and further fluctuates the
strength of muscle. The angle made between the line of action of muscle and fibre is termed as
Pen nation angle. Therefore, the angle is used to compare the length of muscles fibres which is
used in a Hill type muscle model to calculate the strength of the muscle.
2.3.4. Muscle injury and repair
Muscles injury in minimizes the ability to produce force and during hip arthroplasty
muscles can be divided or dissected. Muscle lacerations heal but can be rebuilt with the use of
dense connective scar tissue instead of muscle tissue which minimizes the functions of muscle.
Lacerations which intersect the muscle fibres are the most harmful type of laceration for
recovery of muscle, specially when they dissect blood supply to areas of the muscle. Further,
there are three stages of muscle recovery; degeneration and inflammation, regeneration and
fibrosis. Hence, in fibrosis stage scar tissue is formed which minimizes the strength of the healed
muscle. Generally, this stage starts in two to three weeks after it is injured and it takes more than
6 weeks for normal functioning.
Besides, the mechanical and biological properties of a muscle can be identified to
investigating how the muscle is affected like by, laceration and healing. The test to is to find the
ways to recover from muscle injury, various methods used by doctors recovery of muscles after
laceration and also it will evaluate the weakest muscle in the skeleton. The elongation of the
healed muscles was measured by applying pressure to injured muscle. Scholars found a
minimizing technique in both type of lengths of muscle, the one which is injured and the non
operated muscle which is also termed as contralateral leg. Further, the failure load is identified
by recovering only to approximately 50% of the contralateral muscle which is attributed to the
atrophy of the muscle instead of damage caused by the laceration. Moreover, the minimization in
elongation is related to the scar tissue which is formed at the laceration site as the scar had a
higher elastic modulus.
In contrast to the fluctuation mechanical properties the biological response of a muscle
can also be affected by injured muscle. According to researcher the force of muscle can be
minimized by some injury so repair methods used by Huard et al., (2002) to measure the
strengths of muscle. Moreover, Garrett and Duncan (1988) used the extensor digitorum muscle
of the New Zealand white rabbit to identify the impact of full and partial laceration on strength
and shortening ability of muscle. It was examined that the partial cut of 50 to 75 percent and the
full dip cut along the width of the widest section of the belly muscle is made. Further, when the
muscles were allowed to heal for 3 months in order to provide muscles the ability stiff and
shorten. Garrett and Duncan stated that full deep cut only recover by 54 percent of strength while
the partial cut regain 62 percent of control. The muscle ability of shortening is also affected by
the cutting method because that minimizes the stiffness. In contrary partially cut muscles attain
80 percent of stiffness and control. Hence, it was examined that the proximal section that is the
origin point and cut point performs the similar functions of healing. Further, due to the limited in
vivo data on shortening ability of the sections of full wide cut in muscle has not been included
into models assuming muscle strength.
Crow et al., (2007) has carried a study over rabbits to examine several repair methods of
dividing the belly muscle in the extensor digitorum longus. Scholars compared various methods
of recovering the dip cut in muscle by testing the force produced by electric stimulus or by
performing tensile test. Further, the electrical stimuli chosen by the researchers needed twice and
ten times the threshold voltage to establish involuntary contraction between muscle. Moreover,
scholars found that using ten times the threshold, 1 0T, after 3 months of healing sutured muscles
had majorly 75% of the muscle strength compared to control. However, when the scholar tested
twice the threshold, 2T, gave only 40% of the strength of the control over healed muscles.
Hence, the study states that the minimization of strength on injured muscle is not constant over
the pressure on muscles and that is the reason why lacerating muscle is unable to recover full
strength. Henceforth, the muscle which were ignored and left unpaired after 3 months at 10 T
attained 61 percent over the control muscle strength and at 2T the unrepaired muscle had greater
strength of approximately 56% of the control.
Therefore, muscles that get injured do not recover their full strength when cured. Various
factors that include the way of improvement and the level of damage determine the strength of
wounded muscle. Partially healed muscle have more strength as compared to completely
compound muscle and it is possible that the part of body that is effected by partial wound might
also affect the whole strength. However, no literature studies have been found that compare
different levels of laceration and therefore the variation in muscle strength caused by different
quantities of laceration cannot yet be determined. During hip arthroplasty surgery many of the
muscles are divided along the line of the muscle fibers rather than lacerated. This will affect the
full dip cut along the width of the widest section of the belly muscle is made. Further, when the
muscles were allowed to heal for 3 months in order to provide muscles the ability stiff and
shorten. Garrett and Duncan stated that full deep cut only recover by 54 percent of strength while
the partial cut regain 62 percent of control. The muscle ability of shortening is also affected by
the cutting method because that minimizes the stiffness. In contrary partially cut muscles attain
80 percent of stiffness and control. Hence, it was examined that the proximal section that is the
origin point and cut point performs the similar functions of healing. Further, due to the limited in
vivo data on shortening ability of the sections of full wide cut in muscle has not been included
into models assuming muscle strength.
Crow et al., (2007) has carried a study over rabbits to examine several repair methods of
dividing the belly muscle in the extensor digitorum longus. Scholars compared various methods
of recovering the dip cut in muscle by testing the force produced by electric stimulus or by
performing tensile test. Further, the electrical stimuli chosen by the researchers needed twice and
ten times the threshold voltage to establish involuntary contraction between muscle. Moreover,
scholars found that using ten times the threshold, 1 0T, after 3 months of healing sutured muscles
had majorly 75% of the muscle strength compared to control. However, when the scholar tested
twice the threshold, 2T, gave only 40% of the strength of the control over healed muscles.
Hence, the study states that the minimization of strength on injured muscle is not constant over
the pressure on muscles and that is the reason why lacerating muscle is unable to recover full
strength. Henceforth, the muscle which were ignored and left unpaired after 3 months at 10 T
attained 61 percent over the control muscle strength and at 2T the unrepaired muscle had greater
strength of approximately 56% of the control.
Therefore, muscles that get injured do not recover their full strength when cured. Various
factors that include the way of improvement and the level of damage determine the strength of
wounded muscle. Partially healed muscle have more strength as compared to completely
compound muscle and it is possible that the part of body that is effected by partial wound might
also affect the whole strength. However, no literature studies have been found that compare
different levels of laceration and therefore the variation in muscle strength caused by different
quantities of laceration cannot yet be determined. During hip arthroplasty surgery many of the
muscles are divided along the line of the muscle fibers rather than lacerated. This will affect the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 31
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.


