Transfer of Care
VerifiedAdded on 2023/04/23
|11
|2635
|80
AI Summary
This document explains the importance of transfer of care in healthcare delivery. It covers the goals and course of action for transfer of care, care core principles, and ethical and legal principles of decision making. It also provides insights into cultural safe care and services provided by Tasmania Community.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Transfer of Care 1
Transfer of Care
By
Student Name
Course Name
Institute Name
Date
Transfer of care
Transfer of Care
By
Student Name
Course Name
Institute Name
Date
Transfer of care
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Transfer of Care 2
Introduction
Transfer of care can be defined as the process of coordinating continuity of healthcare
delivery to patients between different care settings for example between hospital wards or from
hospital to home-based care. Transfer of care is usually done according to changes of patients
health and needs which require a different approach and in a unique environment. Firstly, this
paper will explain course of action and goals of transfer of care according to Joseph´s case.
Secondly, there will be an explanation of care core principles and how they are incorporated in
strengths-based nursing. Thirdly, the paper will describe established goals and comprehensive
course of action for Joseph and his family care requirements. Lastly, there will be an explanation
of ethical and legal principles of decision making and cultural safe care when developmenting
patient plan of action.
Goals and course of action of transfer or care
The purpose of transfer of care is to move a patient from one healthcare environment to
another healthcare setting which meets optimal conditions and needs of that patient. It involves
taking care and training of the patient to be able to take care of their own health by observing
medication and allowing them to understand signs and symptoms of a disease or condition
affecting (Anhang et al. 2014, pp.522). Considering Joseph condition, the immediate family need
proper management training to be able to understand the behaviors of an affected person
including signs and symptoms of the condition. Awareness about the patient condition is
intended to create a better understanding between patients and his caregivers while at home
(Aebersold and Tschannen 2013, p.2).
A well structure transfer of care action plan for a patient like Joseph should be designed
to cover a duration of 30 days. This is to ensure proper interventions to handle post-discharge
Introduction
Transfer of care can be defined as the process of coordinating continuity of healthcare
delivery to patients between different care settings for example between hospital wards or from
hospital to home-based care. Transfer of care is usually done according to changes of patients
health and needs which require a different approach and in a unique environment. Firstly, this
paper will explain course of action and goals of transfer of care according to Joseph´s case.
Secondly, there will be an explanation of care core principles and how they are incorporated in
strengths-based nursing. Thirdly, the paper will describe established goals and comprehensive
course of action for Joseph and his family care requirements. Lastly, there will be an explanation
of ethical and legal principles of decision making and cultural safe care when developmenting
patient plan of action.
Goals and course of action of transfer or care
The purpose of transfer of care is to move a patient from one healthcare environment to
another healthcare setting which meets optimal conditions and needs of that patient. It involves
taking care and training of the patient to be able to take care of their own health by observing
medication and allowing them to understand signs and symptoms of a disease or condition
affecting (Anhang et al. 2014, pp.522). Considering Joseph condition, the immediate family need
proper management training to be able to understand the behaviors of an affected person
including signs and symptoms of the condition. Awareness about the patient condition is
intended to create a better understanding between patients and his caregivers while at home
(Aebersold and Tschannen 2013, p.2).
A well structure transfer of care action plan for a patient like Joseph should be designed
to cover a duration of 30 days. This is to ensure proper interventions to handle post-discharge
Transfer of Care 3
needs and issues that may be experienced by the patient. During this period, the patient will
receive medical support from his daughter Emma to manage and understand the condition. This
will help to reduce both emotional and physical risks to the patient and caregivers (Braithwaite,
Wears and Hollnagel 2015, pp.418).
Transfer of care core principles
It is a responsibility of nurses to help patients and their family members to develop
strength that can promote quick recovery and facilitate healing after discharge. Nurses are
required to incorporate Strengths-Based Nursing Care and transfer of care core principle when
planning discharge of a patient. Below are the transfer of care core principles that should be
considered before patient discharge is made (Dale, and Hvalvik 2013, p.379).
Evidence-based quality services. There should be a good working relationship between
family caregivers and healthcare providers to help in designing an effective action plan that
meets the patient needs.
Equity in access to care. The environment where the patient is being transferred to should
allow him to have easy access to medical services. Joseph and the family members should be
able to access medical services from local health facilities anytime they need.
Strengths-based approach. This approach focuses on identifying abilities of the patient
after discharge and enabling them to achieve their desired outcomes.
Care is centered on the patient and their family. This principle requires effective
collaboration between caregivers at home and health professionals to ensure patient is at the
center of services and quality services are provided according to discharge guidelines
needs and issues that may be experienced by the patient. During this period, the patient will
receive medical support from his daughter Emma to manage and understand the condition. This
will help to reduce both emotional and physical risks to the patient and caregivers (Braithwaite,
Wears and Hollnagel 2015, pp.418).
Transfer of care core principles
It is a responsibility of nurses to help patients and their family members to develop
strength that can promote quick recovery and facilitate healing after discharge. Nurses are
required to incorporate Strengths-Based Nursing Care and transfer of care core principle when
planning discharge of a patient. Below are the transfer of care core principles that should be
considered before patient discharge is made (Dale, and Hvalvik 2013, p.379).
Evidence-based quality services. There should be a good working relationship between
family caregivers and healthcare providers to help in designing an effective action plan that
meets the patient needs.
Equity in access to care. The environment where the patient is being transferred to should
allow him to have easy access to medical services. Joseph and the family members should be
able to access medical services from local health facilities anytime they need.
Strengths-based approach. This approach focuses on identifying abilities of the patient
after discharge and enabling them to achieve their desired outcomes.
Care is centered on the patient and their family. This principle requires effective
collaboration between caregivers at home and health professionals to ensure patient is at the
center of services and quality services are provided according to discharge guidelines
Transfer of Care 4
Good coordination and linkages across sectors. The principle focuses on ensuring an
integrated approach that is well coordinated to make sure patient basic needs are provided for
example access to medical care from his local community setting.
Interdisciplinary approach. The principle requires healthcare providers and family
caregivers to ensure the patient receives holistic care.
Services That Can be received from Tasmania Community
Since Joseph had just been discharged from the hospital, Tasmania community would
provide the following services to him and the family:
● Helping the family to raise money for their basic needs such as food.
● Coordinating with Emma to help her in providing care to her parents who are all
sick through shift working.
● Provide both social and moral support to the family.
● Helping in the movement of the client from one point to another including when
going to the hospital for medical check-ups.
● Advising the family on best practices and issues involving patient care and
support.
● Helping the family in meeting the patient needs such as purchase of food and
medications.
● Helping the family to ensure patient environment is conducive and meets the
minimum standard requirements for easy recovery.
● Medical check up services from community health nursing team.
● Mental health services can also be provided by community health nursing team.
Good coordination and linkages across sectors. The principle focuses on ensuring an
integrated approach that is well coordinated to make sure patient basic needs are provided for
example access to medical care from his local community setting.
Interdisciplinary approach. The principle requires healthcare providers and family
caregivers to ensure the patient receives holistic care.
Services That Can be received from Tasmania Community
Since Joseph had just been discharged from the hospital, Tasmania community would
provide the following services to him and the family:
● Helping the family to raise money for their basic needs such as food.
● Coordinating with Emma to help her in providing care to her parents who are all
sick through shift working.
● Provide both social and moral support to the family.
● Helping in the movement of the client from one point to another including when
going to the hospital for medical check-ups.
● Advising the family on best practices and issues involving patient care and
support.
● Helping the family in meeting the patient needs such as purchase of food and
medications.
● Helping the family to ensure patient environment is conducive and meets the
minimum standard requirements for easy recovery.
● Medical check up services from community health nursing team.
● Mental health services can also be provided by community health nursing team.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Transfer of Care 5
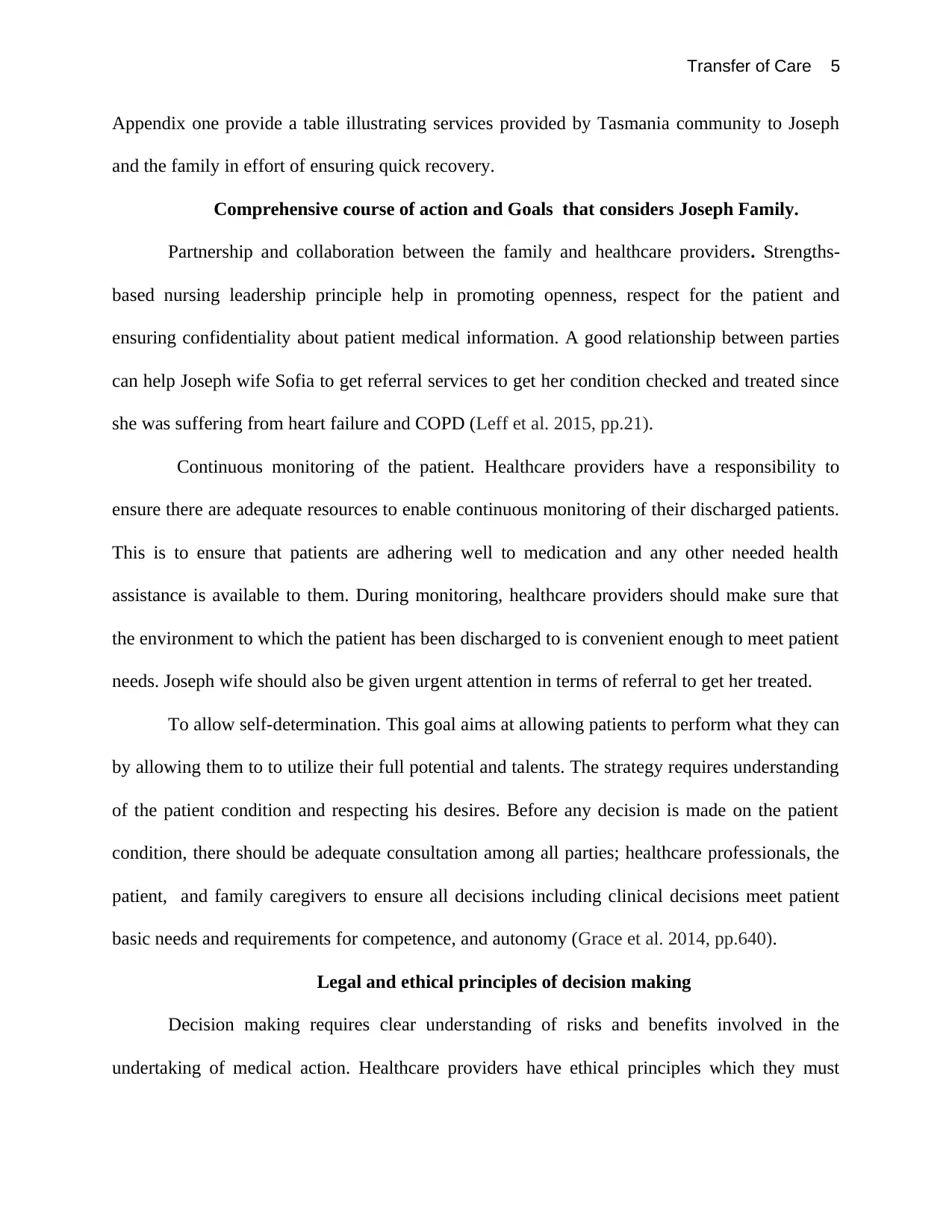
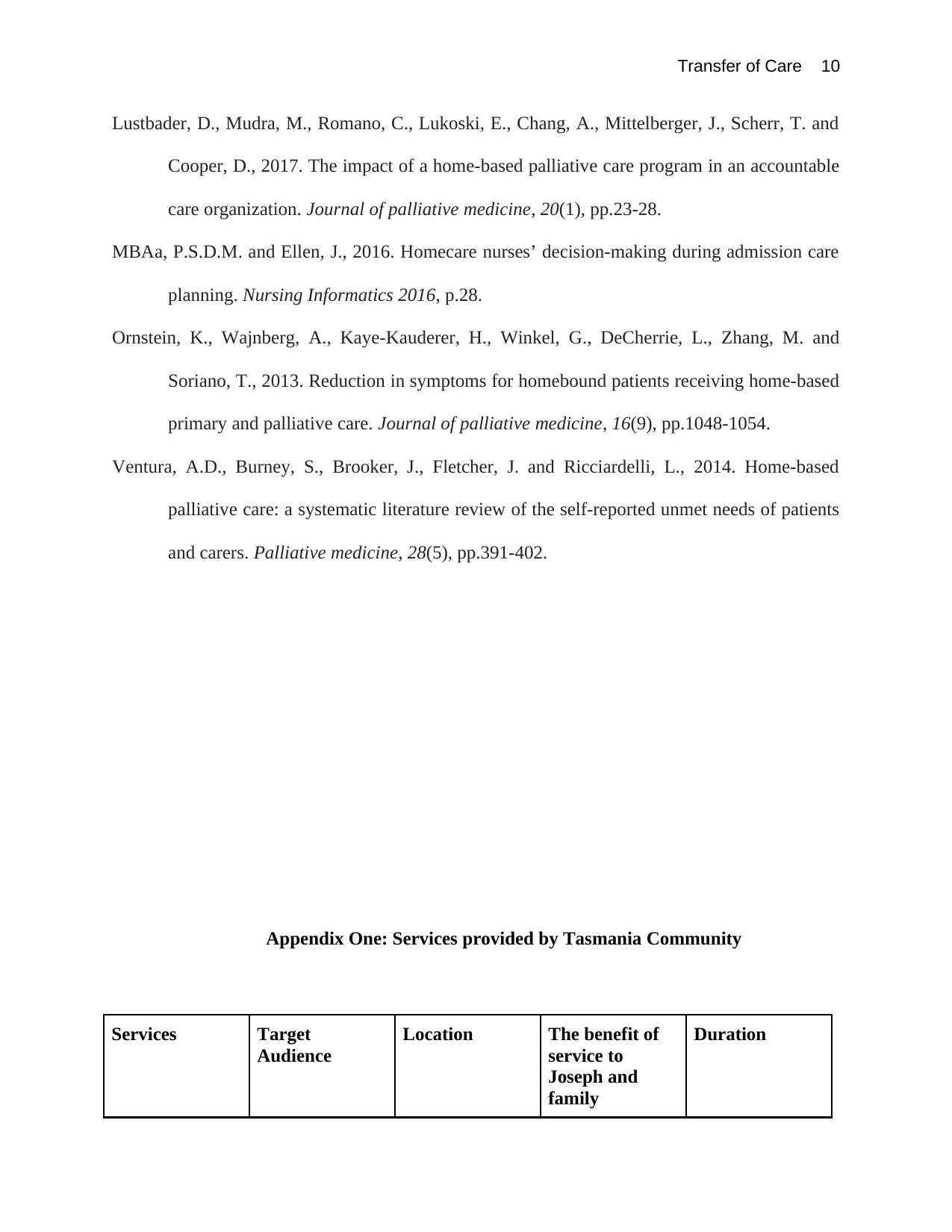
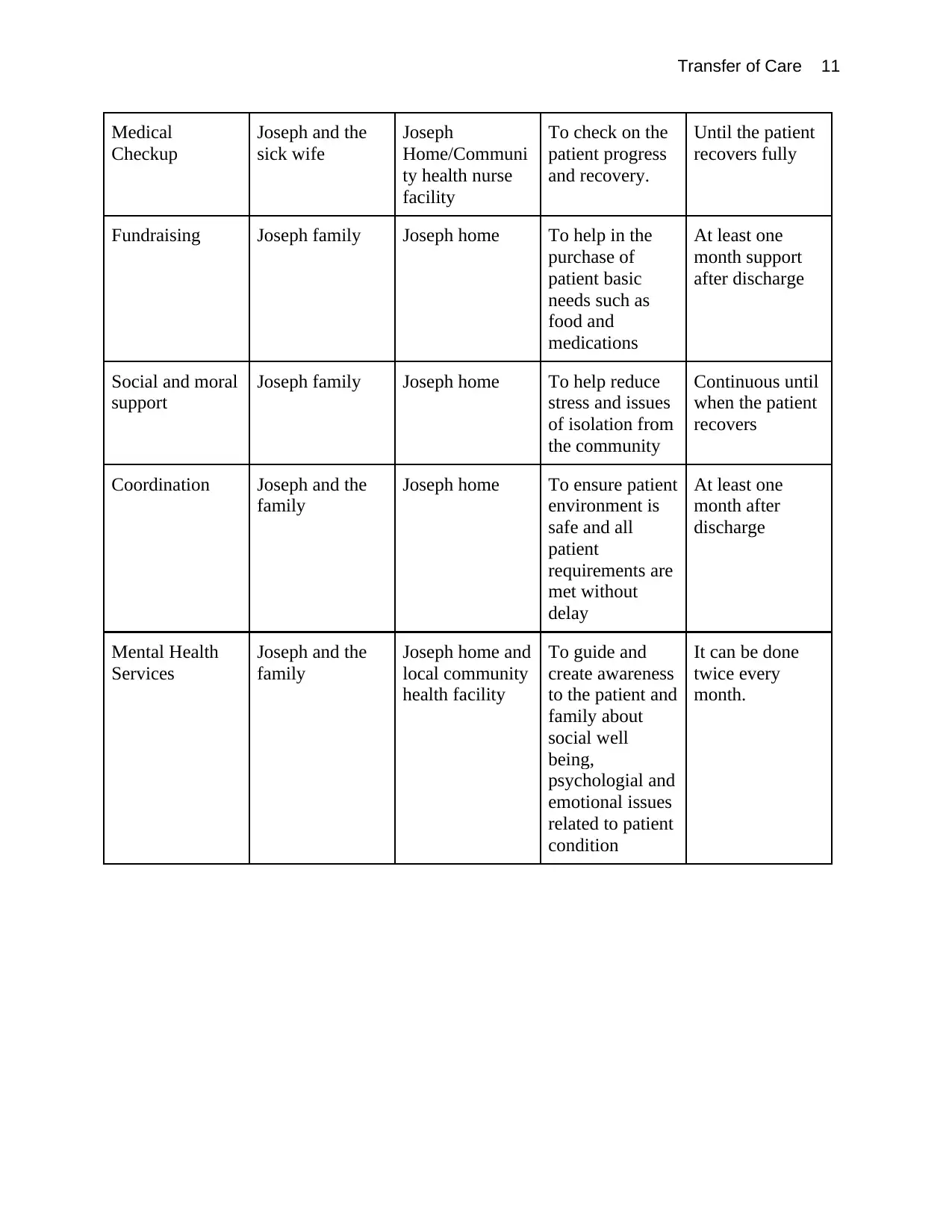
Appendix one provide a table illustrating services provided by Tasmania community to Joseph
and the family in effort of ensuring quick recovery.
Comprehensive course of action and Goals that considers Joseph Family.
Partnership and collaboration between the family and healthcare providers. Strengths-
based nursing leadership principle help in promoting openness, respect for the patient and
ensuring confidentiality about patient medical information. A good relationship between parties
can help Joseph wife Sofia to get referral services to get her condition checked and treated since
she was suffering from heart failure and COPD (Leff et al. 2015, pp.21).
Continuous monitoring of the patient. Healthcare providers have a responsibility to
ensure there are adequate resources to enable continuous monitoring of their discharged patients.
This is to ensure that patients are adhering well to medication and any other needed health
assistance is available to them. During monitoring, healthcare providers should make sure that
the environment to which the patient has been discharged to is convenient enough to meet patient
needs. Joseph wife should also be given urgent attention in terms of referral to get her treated.
To allow self-determination. This goal aims at allowing patients to perform what they can
by allowing them to to utilize their full potential and talents. The strategy requires understanding
of the patient condition and respecting his desires. Before any decision is made on the patient
condition, there should be adequate consultation among all parties; healthcare professionals, the
patient, and family caregivers to ensure all decisions including clinical decisions meet patient
basic needs and requirements for competence, and autonomy (Grace et al. 2014, pp.640).
Legal and ethical principles of decision making
Decision making requires clear understanding of risks and benefits involved in the
undertaking of medical action. Healthcare providers have ethical principles which they must
Appendix one provide a table illustrating services provided by Tasmania community to Joseph
and the family in effort of ensuring quick recovery.
Comprehensive course of action and Goals that considers Joseph Family.
Partnership and collaboration between the family and healthcare providers. Strengths-
based nursing leadership principle help in promoting openness, respect for the patient and
ensuring confidentiality about patient medical information. A good relationship between parties
can help Joseph wife Sofia to get referral services to get her condition checked and treated since
she was suffering from heart failure and COPD (Leff et al. 2015, pp.21).
Continuous monitoring of the patient. Healthcare providers have a responsibility to
ensure there are adequate resources to enable continuous monitoring of their discharged patients.
This is to ensure that patients are adhering well to medication and any other needed health
assistance is available to them. During monitoring, healthcare providers should make sure that
the environment to which the patient has been discharged to is convenient enough to meet patient
needs. Joseph wife should also be given urgent attention in terms of referral to get her treated.
To allow self-determination. This goal aims at allowing patients to perform what they can
by allowing them to to utilize their full potential and talents. The strategy requires understanding
of the patient condition and respecting his desires. Before any decision is made on the patient
condition, there should be adequate consultation among all parties; healthcare professionals, the
patient, and family caregivers to ensure all decisions including clinical decisions meet patient
basic needs and requirements for competence, and autonomy (Grace et al. 2014, pp.640).
Legal and ethical principles of decision making
Decision making requires clear understanding of risks and benefits involved in the
undertaking of medical action. Healthcare providers have ethical principles which they must
Transfer of Care 6
adhere to while taking care of patients. There are four basic principles which healthcare
providers must follow to ensure optimal patient care and safety (Butts, and Rich, 2019).
Autonomy. This principle requires healthcare providers not to coerce patients to make
decisions on matters they have suggested to them but rather allow patients right to retain control
over his or her body. Decisions made by patients should be respected by healthcare providers and
consider them as the best interest of patient according to his or her beliefs and values. For
example, before Joseph discharge is done, he should be explained why he is being moved to
home care and allow him to accept the suggestion or not (MBAa, P.S.D.M. and Ellen 2016,
p.28).
Beneficence. The principle requires medical professionals to make sure all actions they
undertake to are of benefit to the patient. Healthcare providers have to provide Joseph family
with a clear guideline on how the patient will be managed while at home. Clear explanations are
required to enable the family to understand patient needs for quick recovery from his medical
condition (Ventura et al. 2014, pp.391).
Non-Maleficence. The principles requires medical practitioners to do no harm. In
reference to Joseph case, discharge of a patient from hospital to home care should be of high
benefit to the patient. A clear analysis should be conducted before deciding on discharge about
the patient status after discharge. Healthcare providers have to ensure the environment where the
patient is being transferred to meets the minimum standards of the patient needs for easy
management of his or her condition.
Justice. This principle requires fairs when making medical decisions and equal
distribution of scarce resources. Transfer of care action plan should ensure patient medical needs
will be met while at home. Resources should be allocated for monitoring of patients discharged
adhere to while taking care of patients. There are four basic principles which healthcare
providers must follow to ensure optimal patient care and safety (Butts, and Rich, 2019).
Autonomy. This principle requires healthcare providers not to coerce patients to make
decisions on matters they have suggested to them but rather allow patients right to retain control
over his or her body. Decisions made by patients should be respected by healthcare providers and
consider them as the best interest of patient according to his or her beliefs and values. For
example, before Joseph discharge is done, he should be explained why he is being moved to
home care and allow him to accept the suggestion or not (MBAa, P.S.D.M. and Ellen 2016,
p.28).
Beneficence. The principle requires medical professionals to make sure all actions they
undertake to are of benefit to the patient. Healthcare providers have to provide Joseph family
with a clear guideline on how the patient will be managed while at home. Clear explanations are
required to enable the family to understand patient needs for quick recovery from his medical
condition (Ventura et al. 2014, pp.391).
Non-Maleficence. The principles requires medical practitioners to do no harm. In
reference to Joseph case, discharge of a patient from hospital to home care should be of high
benefit to the patient. A clear analysis should be conducted before deciding on discharge about
the patient status after discharge. Healthcare providers have to ensure the environment where the
patient is being transferred to meets the minimum standards of the patient needs for easy
management of his or her condition.
Justice. This principle requires fairs when making medical decisions and equal
distribution of scarce resources. Transfer of care action plan should ensure patient medical needs
will be met while at home. Resources should be allocated for monitoring of patients discharged
Transfer of Care 7
for home care to ensure there is a good record of their health status and to ensure the patient is
improving while he or she is out of a hospital setting (Ornstein et al. 2013, pp.1048).
Cultural safe care in the development of an action plan
Observation of cultural safe care is important in ensuring continuous care support and
understanding between healthcare providers and the family receiving medical services.
Healthcare professionals providing home-based care for patients like Joseph should be able to
identify cultural norms to understand behaviors among their patients and help in preserving
dignity. Development of an effective action plan for the discharge of Joseph from hospital to
home care requires good collaboration between healthcare providers who will be monitoring him
while at home, his immediate family (his daughter) and willing friends who will support the
family (Dixon-Woods et al. 2014, pp.106).
Achievement of culturally safe care depends on knowledge and mutual respect shared
between healthcare providers and the patient with an aim of safeguarding the dignity of a patient.
Joseph is a migrant to a new society with different cultural norms and this can affect his
willingness to seek medical attention from the local community health facility due to long-
established cultural norms. His discharge action plan should consider cultural norms and how
care maybe affected to ensure quick recovery of the patient or achieved (Lustbader et al. 2017,
pp.23).
Conclusion
Transfer of care for a patient should involve all parties in a collaborative manner. The use
of interventions such as collaborative partnership and self determination should be encouraged to
for home care to ensure there is a good record of their health status and to ensure the patient is
improving while he or she is out of a hospital setting (Ornstein et al. 2013, pp.1048).
Cultural safe care in the development of an action plan
Observation of cultural safe care is important in ensuring continuous care support and
understanding between healthcare providers and the family receiving medical services.
Healthcare professionals providing home-based care for patients like Joseph should be able to
identify cultural norms to understand behaviors among their patients and help in preserving
dignity. Development of an effective action plan for the discharge of Joseph from hospital to
home care requires good collaboration between healthcare providers who will be monitoring him
while at home, his immediate family (his daughter) and willing friends who will support the
family (Dixon-Woods et al. 2014, pp.106).
Achievement of culturally safe care depends on knowledge and mutual respect shared
between healthcare providers and the patient with an aim of safeguarding the dignity of a patient.
Joseph is a migrant to a new society with different cultural norms and this can affect his
willingness to seek medical attention from the local community health facility due to long-
established cultural norms. His discharge action plan should consider cultural norms and how
care maybe affected to ensure quick recovery of the patient or achieved (Lustbader et al. 2017,
pp.23).
Conclusion
Transfer of care for a patient should involve all parties in a collaborative manner. The use
of interventions such as collaborative partnership and self determination should be encouraged to
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

Transfer of Care 8
help patient utilize their potential during recovery period. Healthcare providers are required to
design an action plan that meets basic needs of a patient while observing transfer of care core
principles. Cultural safe care should be encouraged to create awareness to family and community
members about patient condition helping then to understand need to provide support to the
patient.
References
help patient utilize their potential during recovery period. Healthcare providers are required to
design an action plan that meets basic needs of a patient while observing transfer of care core
principles. Cultural safe care should be encouraged to create awareness to family and community
members about patient condition helping then to understand need to provide support to the
patient.
References
Transfer of Care 9
Aebersold, M. and Tschannen, D., 2013. Simulation in nursing practice: The impact on patient
care. The Online Journal of Issues in Nursing, 18(2).
Anhang Price, R., Elliott, M.N., Zaslavsky, A.M., Hays, R.D., Lehrman, W.G., Rybowski, L.,
Edgman-Levitan, S. and Cleary, P.D., 2014. Examining the role of patient experience
surveys in measuring health care quality. Medical Care Research and Review, 71(5),
pp.522-554.
Braithwaite, J., Wears, R.L. and Hollnagel, E., 2015. Resilient health care: turning patient safety
on its head. International Journal for Quality in Health Care, 27(5), pp.418-420.
Butts, J.B. and Rich, K.L., 2019. Nursing ethics. Jones & Bartlett Learning.
Dale, B. and Hvalvik, S., 2013. Administration of care to older patients in transition from
hospital to home care services: home nursing leaders’ experiences. Journal of
multidisciplinary healthcare, 6, p.379.
Dixon-Woods, M., Baker, R., Charles, K., Dawson, J., Jerzembek, G., Martin, G., McCarthy, I.,
McKee, L., Minion, J., Ozieranski, P. and Willars, J., 2014. Culture and behaviour in the
English National Health Service: overview of lessons from a large multimethod study.
BMJ Qual Saf, 23(2), pp.106-115.
Grace, P.J., Robinson, E.M., Jurchak, M., Zollfrank, A.A. and Lee, S.M., 2014. Clinical ethics
residency for nurses: An education model to decrease moral distress and strengthen nurse
retention in acute care. Journal of Nursing Administration, 44(12), pp.640-646.
Leff, B., Carlson, C.M., Saliba, D. and Ritchie, C., 2015. The invisible homebound: setting
quality-of-care standards for home-based primary and palliative care. Health Affairs,
34(1), pp.21-29.
Aebersold, M. and Tschannen, D., 2013. Simulation in nursing practice: The impact on patient
care. The Online Journal of Issues in Nursing, 18(2).
Anhang Price, R., Elliott, M.N., Zaslavsky, A.M., Hays, R.D., Lehrman, W.G., Rybowski, L.,
Edgman-Levitan, S. and Cleary, P.D., 2014. Examining the role of patient experience
surveys in measuring health care quality. Medical Care Research and Review, 71(5),
pp.522-554.
Braithwaite, J., Wears, R.L. and Hollnagel, E., 2015. Resilient health care: turning patient safety
on its head. International Journal for Quality in Health Care, 27(5), pp.418-420.
Butts, J.B. and Rich, K.L., 2019. Nursing ethics. Jones & Bartlett Learning.
Dale, B. and Hvalvik, S., 2013. Administration of care to older patients in transition from
hospital to home care services: home nursing leaders’ experiences. Journal of
multidisciplinary healthcare, 6, p.379.
Dixon-Woods, M., Baker, R., Charles, K., Dawson, J., Jerzembek, G., Martin, G., McCarthy, I.,
McKee, L., Minion, J., Ozieranski, P. and Willars, J., 2014. Culture and behaviour in the
English National Health Service: overview of lessons from a large multimethod study.
BMJ Qual Saf, 23(2), pp.106-115.
Grace, P.J., Robinson, E.M., Jurchak, M., Zollfrank, A.A. and Lee, S.M., 2014. Clinical ethics
residency for nurses: An education model to decrease moral distress and strengthen nurse
retention in acute care. Journal of Nursing Administration, 44(12), pp.640-646.
Leff, B., Carlson, C.M., Saliba, D. and Ritchie, C., 2015. The invisible homebound: setting
quality-of-care standards for home-based primary and palliative care. Health Affairs,
34(1), pp.21-29.
Transfer of Care 10
Lustbader, D., Mudra, M., Romano, C., Lukoski, E., Chang, A., Mittelberger, J., Scherr, T. and
Cooper, D., 2017. The impact of a home-based palliative care program in an accountable
care organization. Journal of palliative medicine, 20(1), pp.23-28.
MBAa, P.S.D.M. and Ellen, J., 2016. Homecare nurses’ decision-making during admission care
planning. Nursing Informatics 2016, p.28.
Ornstein, K., Wajnberg, A., Kaye-Kauderer, H., Winkel, G., DeCherrie, L., Zhang, M. and
Soriano, T., 2013. Reduction in symptoms for homebound patients receiving home-based
primary and palliative care. Journal of palliative medicine, 16(9), pp.1048-1054.
Ventura, A.D., Burney, S., Brooker, J., Fletcher, J. and Ricciardelli, L., 2014. Home-based
palliative care: a systematic literature review of the self-reported unmet needs of patients
and carers. Palliative medicine, 28(5), pp.391-402.
Appendix One: Services provided by Tasmania Community
Services Target
Audience
Location The benefit of
service to
Joseph and
family
Duration
Lustbader, D., Mudra, M., Romano, C., Lukoski, E., Chang, A., Mittelberger, J., Scherr, T. and
Cooper, D., 2017. The impact of a home-based palliative care program in an accountable
care organization. Journal of palliative medicine, 20(1), pp.23-28.
MBAa, P.S.D.M. and Ellen, J., 2016. Homecare nurses’ decision-making during admission care
planning. Nursing Informatics 2016, p.28.
Ornstein, K., Wajnberg, A., Kaye-Kauderer, H., Winkel, G., DeCherrie, L., Zhang, M. and
Soriano, T., 2013. Reduction in symptoms for homebound patients receiving home-based
primary and palliative care. Journal of palliative medicine, 16(9), pp.1048-1054.
Ventura, A.D., Burney, S., Brooker, J., Fletcher, J. and Ricciardelli, L., 2014. Home-based
palliative care: a systematic literature review of the self-reported unmet needs of patients
and carers. Palliative medicine, 28(5), pp.391-402.
Appendix One: Services provided by Tasmania Community
Services Target
Audience
Location The benefit of
service to
Joseph and
family
Duration
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Transfer of Care 11
Medical
Checkup
Joseph and the
sick wife
Joseph
Home/Communi
ty health nurse
facility
To check on the
patient progress
and recovery.
Until the patient
recovers fully
Fundraising Joseph family Joseph home To help in the
purchase of
patient basic
needs such as
food and
medications
At least one
month support
after discharge
Social and moral
support
Joseph family Joseph home To help reduce
stress and issues
of isolation from
the community
Continuous until
when the patient
recovers
Coordination Joseph and the
family
Joseph home To ensure patient
environment is
safe and all
patient
requirements are
met without
delay
At least one
month after
discharge
Mental Health
Services
Joseph and the
family
Joseph home and
local community
health facility
To guide and
create awareness
to the patient and
family about
social well
being,
psychologial and
emotional issues
related to patient
condition
It can be done
twice every
month.
Medical
Checkup
Joseph and the
sick wife
Joseph
Home/Communi
ty health nurse
facility
To check on the
patient progress
and recovery.
Until the patient
recovers fully
Fundraising Joseph family Joseph home To help in the
purchase of
patient basic
needs such as
food and
medications
At least one
month support
after discharge
Social and moral
support
Joseph family Joseph home To help reduce
stress and issues
of isolation from
the community
Continuous until
when the patient
recovers
Coordination Joseph and the
family
Joseph home To ensure patient
environment is
safe and all
patient
requirements are
met without
delay
At least one
month after
discharge
Mental Health
Services
Joseph and the
family
Joseph home and
local community
health facility
To guide and
create awareness
to the patient and
family about
social well
being,
psychologial and
emotional issues
related to patient
condition
It can be done
twice every
month.
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





