Professional Practice: Inter, Intra, and Transprofessional Evaluation
VerifiedAdded on 2023/06/10
|7
|6897
|348
Essay
AI Summary
This essay critically evaluates the main themes in professional practice literature, focusing on interprofessional, intraprofessional, and transprofessional models, and discusses their application to the author's professional practice. It explores an aspect of the author's professional practice that presents challenges and concerns, and considers potential solutions to enhance it. The essay likely draws upon research, theory, and emerging practice models to provide a comprehensive analysis of the chosen aspect, aiming to improve understanding and effectiveness in a real-world healthcare setting. Desklib is a platform where students can find similar assignments and study tools to aid their learning.
Full Terms & Conditions of access and use can be found at
http://www.tandfonline.com/action/journalInformation?journalCode=ijic20
Journal of Interprofessional Care
ISSN: 1356-1820 (Print) 1469-9567 (Online) Journal homepage: http://www.tandfonline.com/loi/ijic20
Using transprofessional care in the emergency
department to reduce patient admissions: A
retrospective audit of medical histories
Julia Morphet, Debra Lee Griffiths, Kimberley Crawford, Allison Williams,
Tamsin Jones, Belinda Berry & Kelli Innes
To cite this article: Julia Morphet, Debra Lee Griffiths, Kimberley Crawford, Allison Williams,
Tamsin Jones, Belinda Berry & Kelli Innes (2016) Using transprofessional care in the emergency
department to reduce patient admissions: A retrospective audit of medical histories, Journal of
Interprofessional Care, 30:2, 226-231, DOI: 10.3109/13561820.2015.1115394
To link to this article: http://dx.doi.org/10.3109/13561820.2015.1115394
Published online: 08 Mar 2016.
Submit your article to this journal
Article views: 58
View related articles
View Crossmark data
http://www.tandfonline.com/action/journalInformation?journalCode=ijic20
Journal of Interprofessional Care
ISSN: 1356-1820 (Print) 1469-9567 (Online) Journal homepage: http://www.tandfonline.com/loi/ijic20
Using transprofessional care in the emergency
department to reduce patient admissions: A
retrospective audit of medical histories
Julia Morphet, Debra Lee Griffiths, Kimberley Crawford, Allison Williams,
Tamsin Jones, Belinda Berry & Kelli Innes
To cite this article: Julia Morphet, Debra Lee Griffiths, Kimberley Crawford, Allison Williams,
Tamsin Jones, Belinda Berry & Kelli Innes (2016) Using transprofessional care in the emergency
department to reduce patient admissions: A retrospective audit of medical histories, Journal of
Interprofessional Care, 30:2, 226-231, DOI: 10.3109/13561820.2015.1115394
To link to this article: http://dx.doi.org/10.3109/13561820.2015.1115394
Published online: 08 Mar 2016.
Submit your article to this journal
Article views: 58
View related articles
View Crossmark data
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
ORIGINAL ARTICLE
Using transprofessional care in the emergency department to reduce patient
admissions:A retrospective audit of medical histories
Julia Morpheta, Debra Lee Griffithsa, Kimberley Crawfordb, Allison Williamsb, Tamsin Jonesa, Belinda Berryc,
and KelliInnesa
aSchool of Nursing and Midwifery,Monash University,Frankston,Victoria,Australia;bSchool of Nursing and Midwifery,Monash University,Clayton,
Victoria,Australia;cHospitalAdmission Risk Program (HARP),Peninsula Health,Frankston,Victoria,Australia
ABSTRACT
The demand for emergency department (ED) services has increased significantly,due to our increasingly
ageing population and limited access to primary care.This article reports outcomes from a transprofes-
sionalmodel of care in an ED in Victoria,Australia.Nurses,physiotherapists,socialworkers,and
occupationaltherapists undertook additionaleducation to increase the range ofservices they could
provide and thereby expedite patient flow through the ED.One hundred patients who received this
service were matched against 50 patients who did not. The most common reasons for patient admission
were limb injury/limb pain (n = 47,23.5%)and falls (n = 46,23.0%).Transprofessionalinterventions
included applying supportive bandages, slings, zimmer splints and controlled ankle motion (CAM) boots,
and referralto new services such as case management and mentalhealth teams.The rate of hospital
admissions was significantly lower in the transprofessionalgroup (n = 27,18.0%) than in the reference
group (n = 19,38%,p = 0.005).This group also had a slightly lower re-presentation rate (n = 4,2.7%)
than patients in the reference group (n = 2,4.0%).There are many benefits that support this modelof
care thatin turn reduces ED overcrowding and work stress.A transprofessionalmodelmay offera
creative solution to meeting the varied needs of patients presenting for emergency care.
ARTICLE HISTORY
Received 30 May 2014
Revised 16 August 2015
Accepted 29 October 2015
KEYWORDS
Collaboration;emergency
department;patient
outcomes;teamwork;
transprofessional
Introduction
Emergency departments (EDs)globally are experiencing an
ever-increasing demand on services(Lowthian etal., 2012;
Trzeciak & Rivers,2003).This increase isattributed to a
growingand increasinglyaged population (AIHW,2011;
Pallin,Allen, Espinola,Camargo,& Stephen Bohan,2013)
and increasingchronic illness (NSW Health, 2007;
Productivity Commission,2005).Limited access to primary
care results in many people attending EDs as a way to access
healthcare (NSW Health,2007).Another factor contributing
to service demand in the ED is access block. Access block is a
state in which ED patients awaiting admission are unable to
be transferred to the wards within a reasonable time frame, as
there are no availablebeds (AustralasianCollege for
Emergency Medicine, 2009). Access block has been well-docu-
mented to contribute to ED overcrowding, which has negative
implicationsfor both patientsand staff.ED overcrowding
results in delays to treatment,increased errors and increased
mortality(Kulstad & Kelley,2009;Kulstad,Sikka,Sweis,
Kelley,& Rzechula,2010;Pines et al.,2007;Sills,Fairclough,
Ranade,& Kahn,2011;Sprivulis,Da Silva,Jacobs,Frazer,&
Jelinek,2006).ED overcrowding also contributesto work
stress and job dissatisfaction for ED staff (Pines et al.,2007).
Given the ageing population,and increase in chronic illness,
globaldemand on EDsis expected to continueto grow,
increasing the workload for ED staff.
Many strategies have been introduced to address the grow
ing service demand on EDs.Typically,these strategies aim to
improve patient flow and reduce access block and overcrow
ing.Examples of such strategies include waiting room nurses
streaming,rapid assessment teams,short stay units and care
coordination programs(Crawford etal., 2014).A recent
reform to emergency care in Australia aimed atimproving
patient flow was the introduction of a key performance indi-
cator (KPI) based on patientlength ofstay in the ED.The
National Emergency Access Target (NEAT) requires that 90%
of patients be discharged from or transferred out ofthe ED
within 4 hours of arrival(Department of Health and Ageing,
2012). Finally, another strategy to address growing ED servi
demand isa transprofessionalcare model,which hasbeen
introduced in the ED of a Victorian (Australia) health service
(Innes et al.,2015).
A transprofessionalgroup consistsof membersdrawn
from a rangeof professions(Rosenfield,1992;Thylefors,
Persson,& Hellström,2005),in this case,occupationalther-
apy, physiotherapy,nursing and speech pathology.
Transprofessional teams are a unique way of drawing togeth
the skills ofdifferentprofessions into a cohesive unitwho
work togethertoward acommon goal(Rosenfield,1992;
Thistlethwaite,Jackson,& Moran, 2013;Thyleforset al.,
2005).In a multiprofessionalmodel,individuals from varied
professionswork in parallelto perform profession-specific
CONTACT Julia Morphet julia.morphet@monash.eduSchoolof Nursing and Midwifery,Monash University,PO Box 527,Frankston,VIC 3199,Australia.
Color versions of one or more figures in the article can be found online at http://www.tandfonline.com/ijic.
JOURNAL OF INTERPROFESSIONAL CARE
2016,VOL.30,NO.2,226–231
http://dx.doi.org/10.3109/13561820.2015.1115394
© 2016 Taylor & Francis
Downloaded by [Library Services City University London] at 18:00 04 April 2016
Using transprofessional care in the emergency department to reduce patient
admissions:A retrospective audit of medical histories
Julia Morpheta, Debra Lee Griffithsa, Kimberley Crawfordb, Allison Williamsb, Tamsin Jonesa, Belinda Berryc,
and KelliInnesa
aSchool of Nursing and Midwifery,Monash University,Frankston,Victoria,Australia;bSchool of Nursing and Midwifery,Monash University,Clayton,
Victoria,Australia;cHospitalAdmission Risk Program (HARP),Peninsula Health,Frankston,Victoria,Australia
ABSTRACT
The demand for emergency department (ED) services has increased significantly,due to our increasingly
ageing population and limited access to primary care.This article reports outcomes from a transprofes-
sionalmodel of care in an ED in Victoria,Australia.Nurses,physiotherapists,socialworkers,and
occupationaltherapists undertook additionaleducation to increase the range ofservices they could
provide and thereby expedite patient flow through the ED.One hundred patients who received this
service were matched against 50 patients who did not. The most common reasons for patient admission
were limb injury/limb pain (n = 47,23.5%)and falls (n = 46,23.0%).Transprofessionalinterventions
included applying supportive bandages, slings, zimmer splints and controlled ankle motion (CAM) boots,
and referralto new services such as case management and mentalhealth teams.The rate of hospital
admissions was significantly lower in the transprofessionalgroup (n = 27,18.0%) than in the reference
group (n = 19,38%,p = 0.005).This group also had a slightly lower re-presentation rate (n = 4,2.7%)
than patients in the reference group (n = 2,4.0%).There are many benefits that support this modelof
care thatin turn reduces ED overcrowding and work stress.A transprofessionalmodelmay offera
creative solution to meeting the varied needs of patients presenting for emergency care.
ARTICLE HISTORY
Received 30 May 2014
Revised 16 August 2015
Accepted 29 October 2015
KEYWORDS
Collaboration;emergency
department;patient
outcomes;teamwork;
transprofessional
Introduction
Emergency departments (EDs)globally are experiencing an
ever-increasing demand on services(Lowthian etal., 2012;
Trzeciak & Rivers,2003).This increase isattributed to a
growingand increasinglyaged population (AIHW,2011;
Pallin,Allen, Espinola,Camargo,& Stephen Bohan,2013)
and increasingchronic illness (NSW Health, 2007;
Productivity Commission,2005).Limited access to primary
care results in many people attending EDs as a way to access
healthcare (NSW Health,2007).Another factor contributing
to service demand in the ED is access block. Access block is a
state in which ED patients awaiting admission are unable to
be transferred to the wards within a reasonable time frame, as
there are no availablebeds (AustralasianCollege for
Emergency Medicine, 2009). Access block has been well-docu-
mented to contribute to ED overcrowding, which has negative
implicationsfor both patientsand staff.ED overcrowding
results in delays to treatment,increased errors and increased
mortality(Kulstad & Kelley,2009;Kulstad,Sikka,Sweis,
Kelley,& Rzechula,2010;Pines et al.,2007;Sills,Fairclough,
Ranade,& Kahn,2011;Sprivulis,Da Silva,Jacobs,Frazer,&
Jelinek,2006).ED overcrowding also contributesto work
stress and job dissatisfaction for ED staff (Pines et al.,2007).
Given the ageing population,and increase in chronic illness,
globaldemand on EDsis expected to continueto grow,
increasing the workload for ED staff.
Many strategies have been introduced to address the grow
ing service demand on EDs.Typically,these strategies aim to
improve patient flow and reduce access block and overcrow
ing.Examples of such strategies include waiting room nurses
streaming,rapid assessment teams,short stay units and care
coordination programs(Crawford etal., 2014).A recent
reform to emergency care in Australia aimed atimproving
patient flow was the introduction of a key performance indi-
cator (KPI) based on patientlength ofstay in the ED.The
National Emergency Access Target (NEAT) requires that 90%
of patients be discharged from or transferred out ofthe ED
within 4 hours of arrival(Department of Health and Ageing,
2012). Finally, another strategy to address growing ED servi
demand isa transprofessionalcare model,which hasbeen
introduced in the ED of a Victorian (Australia) health service
(Innes et al.,2015).
A transprofessionalgroup consistsof membersdrawn
from a rangeof professions(Rosenfield,1992;Thylefors,
Persson,& Hellström,2005),in this case,occupationalther-
apy, physiotherapy,nursing and speech pathology.
Transprofessional teams are a unique way of drawing togeth
the skills ofdifferentprofessions into a cohesive unitwho
work togethertoward acommon goal(Rosenfield,1992;
Thistlethwaite,Jackson,& Moran, 2013;Thyleforset al.,
2005).In a multiprofessionalmodel,individuals from varied
professionswork in parallelto perform profession-specific
CONTACT Julia Morphet julia.morphet@monash.eduSchoolof Nursing and Midwifery,Monash University,PO Box 527,Frankston,VIC 3199,Australia.
Color versions of one or more figures in the article can be found online at http://www.tandfonline.com/ijic.
JOURNAL OF INTERPROFESSIONAL CARE
2016,VOL.30,NO.2,226–231
http://dx.doi.org/10.3109/13561820.2015.1115394
© 2016 Taylor & Francis
Downloaded by [Library Services City University London] at 18:00 04 April 2016
assessment, planning and delivery of care to address common
goals (Rosenfield, 1992; Smart & Smith, 2013; Thylefors et al.,
2005).Interprofessionalteams are more collaborative,work-
ing together to address common goals and sharing commu-
nication,but still working from a profession-specific basis
(Dyer,2003;Rosenfield,1992;Thylefors etal., 2005;Tran,
2012).By comparison,transprofessionalteamscross the
boundaries of professions (Rosenfield,1992;Thylefors et al.,
2005),completing training in other professions,which allows
flexibility in workload,or whatsome have defined asrole
blurring(Sims,Hewitt,& Harris, 2015;Thyleforset al.,
2005).Team membershave sharedresponsibilities,and
work collaboratively,sharing knowledge and skills,and sup-
porting each otherto solve problemsand deliverservices
(Dyer,2003;Thyleforset al., 2005).The transprofessional
skills of team membersallow them to providewhichever
services and skills are required at any given time.This is an
importantadvantageof the transprofessionalmodel,as it
avoids the delays associated with waiting for multiple specia-
lised assessments (Innes et al.,2015;King et al.,2009).Thus,
consulting timesare decreased,as duplication isremoved
(Thylefors etal.,2005).As a result,discharge from the ED
can be expedited (Innes etal.,2015;King etal.,2009).For
example,instead of waiting for an occupational health assess-
ment,a physiotherapy assessmentand a socialwork assess-
ment,one transprofessionalteam membercan complete a
comprehensive assessment and deliver allrequired interven-
tions.The use of transprofessionalteams has been described
internationallyin paediatricdisability units (Stepans,
Thompson,& Buchanan,2002),rehabilitation(Cartmill,
Soklaridis,& Cassidy,2011;Reilly,2001) and palliative care
(Daly & Matzel, 2013). However, there is a paucity of research
examiningthe outcomesof transprofessionalteamsin
healthcare.
It is hypothesised that the transprofessionalteam provide
efficient,effective and economic patientcare (King etal.,
2009;Thyleforset al., 2005).One study hasshown thata
transprofessionalteam provided an essentialservice in ED,
ensuring safe discharge and patient follow-up,and improving
ED efficiency (Innes et al.,2015),yet no other formal evalua-
tion ofthe transprofessionalteam has been published.This
study aimed to critically evaluate the following important
outcomesarising from the transprofessionalmodelof care
in the ED:patient admission rates;length ofstay in the ED
and patientre-presentation ratesto the ED following dis-
charge home.
Background
The study was undertaken in a metropolitan hospital in Victoria,
Australia. In 2012, there were 56,286 patient presentations to the
ED (Australian Institute ofHealth and Welfare,2013).The
transprofessionalteam consistsof nurses,physiotherapists,
socialworkersand occupationaltherapists.Each transprofes-
sionalteam membercompleted 20 competenciesto increase
their educationalpreparedness to extend the services and care
they can provide,effectively enabling them to provide health
services which may typically reside within a different profess
(Table 1) (Goonan,2011).For example,while not traditionally
the domain of a physiotherapist or occupationaltherapist,grief
counselling iswithin the skillsetof all team members.The
services provided by transprofessionalteam members is broad,
includingphysical,cognitiveand socialassessments,fitting
splints,developing care plans,referrals to internaland external
services and providing care after discharge. The transprofes
team treats approximately 400 patients per month in the ED
studied (7% of the ED patient population).It is estimated that
more than 40% of patients who are treated by the transprof
sionalteam have complex needsand chronic illnessessuch
as diabetes,heartdisease,respiratoryconditionsand renal
impairment (Goonan, 2011).
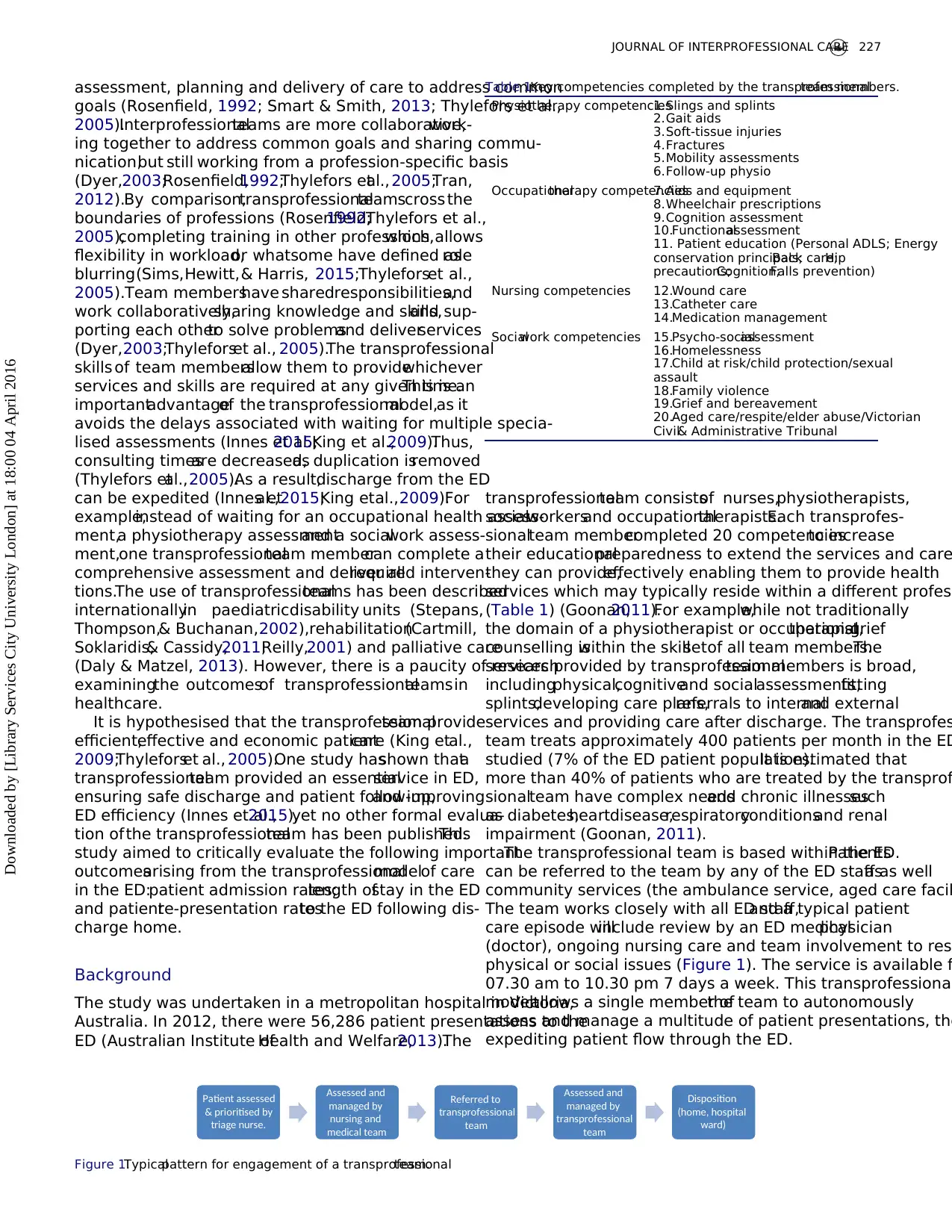
The transprofessional team is based within the ED.Patients
can be referred to the team by any of the ED staff as wellas
community services (the ambulance service, aged care facil
The team works closely with all ED staff,and a typical patient
care episode willinclude review by an ED medicalphysician
(doctor), ongoing nursing care and team involvement to reso
physical or social issues (Figure 1). The service is available f
07.30 am to 10.30 pm 7 days a week. This transprofessional
modelallows a single member ofthe team to autonomously
assess and manage a multitude of patient presentations, the
expediting patient flow through the ED.
Table 1.Key competencies completed by the transprofessionalteam members.
Physiotherapy competencies1.Slings and splints
2.Gait aids
3.Soft-tissue injuries
4.Fractures
5.Mobility assessments
6.Follow-up physio
Occupationaltherapy competencies7.Aids and equipment
8.Wheelchair prescriptions
9.Cognition assessment
10.Functionalassessment
11. Patient education (Personal ADLS; Energy
conservation principals;Back care;Hip
precautions;Cognition;Falls prevention)
Nursing competencies 12.Wound care
13.Catheter care
14.Medication management
Socialwork competencies 15.Psycho-socialassessment
16.Homelessness
17.Child at risk/child protection/sexual
assault
18.Family violence
19.Grief and bereavement
20.Aged care/respite/elder abuse/Victorian
Civil& Administrative Tribunal
Patient assessed
& prioritised by
triage nurse.
Assessed and
managed by
nursing and
medical team
Referred to
transprofessional
team
Assessed and
managed by
transprofessional
team
Disposition
(home, hospital
ward)
Figure 1.Typicalpattern for engagement of a transprofessionalteam.
JOURNAL OF INTERPROFESSIONAL CARE 227
Downloaded by [Library Services City University London] at 18:00 04 April 2016
goals (Rosenfield, 1992; Smart & Smith, 2013; Thylefors et al.,
2005).Interprofessionalteams are more collaborative,work-
ing together to address common goals and sharing commu-
nication,but still working from a profession-specific basis
(Dyer,2003;Rosenfield,1992;Thylefors etal., 2005;Tran,
2012).By comparison,transprofessionalteamscross the
boundaries of professions (Rosenfield,1992;Thylefors et al.,
2005),completing training in other professions,which allows
flexibility in workload,or whatsome have defined asrole
blurring(Sims,Hewitt,& Harris, 2015;Thyleforset al.,
2005).Team membershave sharedresponsibilities,and
work collaboratively,sharing knowledge and skills,and sup-
porting each otherto solve problemsand deliverservices
(Dyer,2003;Thyleforset al., 2005).The transprofessional
skills of team membersallow them to providewhichever
services and skills are required at any given time.This is an
importantadvantageof the transprofessionalmodel,as it
avoids the delays associated with waiting for multiple specia-
lised assessments (Innes et al.,2015;King et al.,2009).Thus,
consulting timesare decreased,as duplication isremoved
(Thylefors etal.,2005).As a result,discharge from the ED
can be expedited (Innes etal.,2015;King etal.,2009).For
example,instead of waiting for an occupational health assess-
ment,a physiotherapy assessmentand a socialwork assess-
ment,one transprofessionalteam membercan complete a
comprehensive assessment and deliver allrequired interven-
tions.The use of transprofessionalteams has been described
internationallyin paediatricdisability units (Stepans,
Thompson,& Buchanan,2002),rehabilitation(Cartmill,
Soklaridis,& Cassidy,2011;Reilly,2001) and palliative care
(Daly & Matzel, 2013). However, there is a paucity of research
examiningthe outcomesof transprofessionalteamsin
healthcare.
It is hypothesised that the transprofessionalteam provide
efficient,effective and economic patientcare (King etal.,
2009;Thyleforset al., 2005).One study hasshown thata
transprofessionalteam provided an essentialservice in ED,
ensuring safe discharge and patient follow-up,and improving
ED efficiency (Innes et al.,2015),yet no other formal evalua-
tion ofthe transprofessionalteam has been published.This
study aimed to critically evaluate the following important
outcomesarising from the transprofessionalmodelof care
in the ED:patient admission rates;length ofstay in the ED
and patientre-presentation ratesto the ED following dis-
charge home.
Background
The study was undertaken in a metropolitan hospital in Victoria,
Australia. In 2012, there were 56,286 patient presentations to the
ED (Australian Institute ofHealth and Welfare,2013).The
transprofessionalteam consistsof nurses,physiotherapists,
socialworkersand occupationaltherapists.Each transprofes-
sionalteam membercompleted 20 competenciesto increase
their educationalpreparedness to extend the services and care
they can provide,effectively enabling them to provide health
services which may typically reside within a different profess
(Table 1) (Goonan,2011).For example,while not traditionally
the domain of a physiotherapist or occupationaltherapist,grief
counselling iswithin the skillsetof all team members.The
services provided by transprofessionalteam members is broad,
includingphysical,cognitiveand socialassessments,fitting
splints,developing care plans,referrals to internaland external
services and providing care after discharge. The transprofes
team treats approximately 400 patients per month in the ED
studied (7% of the ED patient population).It is estimated that
more than 40% of patients who are treated by the transprof
sionalteam have complex needsand chronic illnessessuch
as diabetes,heartdisease,respiratoryconditionsand renal
impairment (Goonan, 2011).
The transprofessional team is based within the ED.Patients
can be referred to the team by any of the ED staff as wellas
community services (the ambulance service, aged care facil
The team works closely with all ED staff,and a typical patient
care episode willinclude review by an ED medicalphysician
(doctor), ongoing nursing care and team involvement to reso
physical or social issues (Figure 1). The service is available f
07.30 am to 10.30 pm 7 days a week. This transprofessional
modelallows a single member ofthe team to autonomously
assess and manage a multitude of patient presentations, the
expediting patient flow through the ED.
Table 1.Key competencies completed by the transprofessionalteam members.
Physiotherapy competencies1.Slings and splints
2.Gait aids
3.Soft-tissue injuries
4.Fractures
5.Mobility assessments
6.Follow-up physio
Occupationaltherapy competencies7.Aids and equipment
8.Wheelchair prescriptions
9.Cognition assessment
10.Functionalassessment
11. Patient education (Personal ADLS; Energy
conservation principals;Back care;Hip
precautions;Cognition;Falls prevention)
Nursing competencies 12.Wound care
13.Catheter care
14.Medication management
Socialwork competencies 15.Psycho-socialassessment
16.Homelessness
17.Child at risk/child protection/sexual
assault
18.Family violence
19.Grief and bereavement
20.Aged care/respite/elder abuse/Victorian
Civil& Administrative Tribunal
Patient assessed
& prioritised by
triage nurse.
Assessed and
managed by
nursing and
medical team
Referred to
transprofessional
team
Assessed and
managed by
transprofessional
team
Disposition
(home, hospital
ward)
Figure 1.Typicalpattern for engagement of a transprofessionalteam.
JOURNAL OF INTERPROFESSIONAL CARE 227
Downloaded by [Library Services City University London] at 18:00 04 April 2016
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
Methods
A retrospective audit of medicalhistories with matched con-
trols was employed to examine key outcomes associated with
a transprofessionalmodel of care delivery.
Data collection
The medical histories of 150 patients who had received trans-
professionalteam services in 2012 were identified using the
patientmanagementsystem,and then 150 medicalhistories
were randomly selected and examined.The medicalhistories
of 50 patients who did not receive transprofessionalservices,
but presented in the same time period (month,day,hour),
were then matched by presenting complaint,triage category,
end diagnosis,age and gender,and were also audited.The
triage category determines how long a patient can wait before
medicalassessment(AustralasianCollegefor Emergency
Medicine,2006).These data provided a baseline for compar-
ison of outcomes.For the purpose of this article,the baseline
cohort has been labelled the “reference group” (RG).
Patientdata extracted from the records included date of
birth, presenting complaint,relevantpastmedicalhistory,
socialsupportsand living arrangements,interventionsand
investigations undertaken within the ED,end diagnosis and
disposition (i.e.admitted,discharged and where they were
discharged to).Outcome measures included hospitaladmis-
sion rates,patient length of stay in the ED (which was com-
pared against the 4 hours NEAT) and unscheduled patient re-
presentation to ED within 72 hours.
Data were manually extracted from patienthistoriesby
staff from within the health service and audited for accuracy
by one of the research team members– an experienced
emergency nurse.This involved the researcher re-examining
10% of the patientmedicalhistoriesand comparingthe
extracted data with the data in the medical history.No errors
were identified.Data were then imported into SPSS V.20
(Armonk,NY: IBM Corp 2011) for statisticalanalysis.
Data analysis
Descriptive statistics(frequencies,percentages,median and
interquartilerange)havebeen used to describethe data.
Inferentialstatistics (Mann–Whitney U-test,Chi-square test
for independence) were used to make comparisons between
transprofessionalteam and RG cohorts(Brace,Kemp,&
Snelgar,2003;Pallant,2013).
Ethical considerations
Ethics approvalwas obtained before the study commenced
(HREC/12/PH/96). The data were collected by staff employed
in the hospital,who have access to this data as part of their
employment.The data collected were notidentifiable.Data
have only been presented in aggregate form.Ethical approval
was sought and received from the health service and univer-
sity prior to the study being conducted.
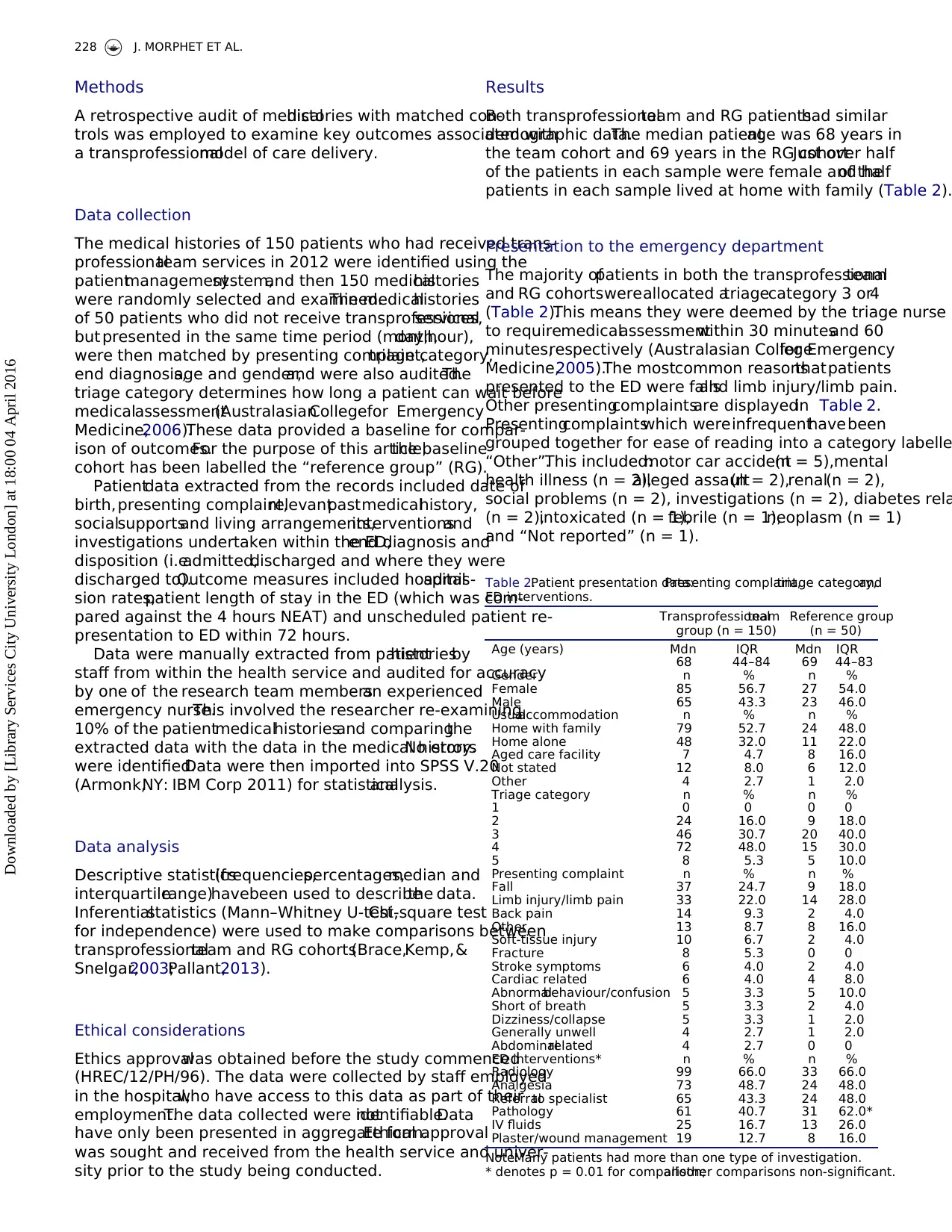
Results
Both transprofessionalteam and RG patientshad similar
demographic data.The median patientage was 68 years in
the team cohort and 69 years in the RG cohort.Just over half
of the patients in each sample were female and halfof the
patients in each sample lived at home with family (Table 2).
Presentation to the emergency department
The majority ofpatients in both the transprofessionalteam
and RG cohortswereallocated atriagecategory 3 or4
(Table 2).This means they were deemed by the triage nurse
to requiremedicalassessmentwithin 30 minutesand 60
minutes,respectively (Australasian Collegefor Emergency
Medicine,2005).The mostcommon reasonsthatpatients
presented to the ED were fallsand limb injury/limb pain.
Other presentingcomplaintsare displayedin Table 2.
Presentingcomplaintswhich wereinfrequenthavebeen
grouped together for ease of reading into a category labelle
“Other”.This included:motor car accident(n = 5),mental
health illness (n = 2),alleged assault(n = 2),renal(n = 2),
social problems (n = 2), investigations (n = 2), diabetes rela
(n = 2),intoxicated (n = 1),febrile (n = 1),neoplasm (n = 1)
and “Not reported” (n = 1).
Table 2.Patient presentation data:Presenting complaint,triage category,and
ED interventions.
Transprofessionalteam
group (n = 150)
Reference group
(n = 50)
Age (years) Mdn IQR Mdn IQR
68 44–84 69 44–83
Gender n % n %
Female 85 56.7 27 54.0
Male 65 43.3 23 46.0
Usualaccommodation n % n %
Home with family 79 52.7 24 48.0
Home alone 48 32.0 11 22.0
Aged care facility 7 4.7 8 16.0
Not stated 12 8.0 6 12.0
Other 4 2.7 1 2.0
Triage category n % n %
1 0 0 0 0
2 24 16.0 9 18.0
3 46 30.7 20 40.0
4 72 48.0 15 30.0
5 8 5.3 5 10.0
Presenting complaint n % n %
Fall 37 24.7 9 18.0
Limb injury/limb pain 33 22.0 14 28.0
Back pain 14 9.3 2 4.0
Other 13 8.7 8 16.0
Soft-tissue injury 10 6.7 2 4.0
Fracture 8 5.3 0 0
Stroke symptoms 6 4.0 2 4.0
Cardiac related 6 4.0 4 8.0
Abnormalbehaviour/confusion 5 3.3 5 10.0
Short of breath 5 3.3 2 4.0
Dizziness/collapse 5 3.3 1 2.0
Generally unwell 4 2.7 1 2.0
Abdominalrelated 4 2.7 0 0
ED interventions* n % n %
Radiology 99 66.0 33 66.0
Analgesia 73 48.7 24 48.0
Referralto specialist 65 43.3 24 48.0
Pathology 61 40.7 31 62.0*
IV fluids 25 16.7 13 26.0
Plaster/wound management 19 12.7 8 16.0
Note:Many patients had more than one type of investigation.
* denotes p = 0.01 for comparison;allother comparisons non-significant.
228 J. MORPHET ET AL.
Downloaded by [Library Services City University London] at 18:00 04 April 2016
A retrospective audit of medicalhistories with matched con-
trols was employed to examine key outcomes associated with
a transprofessionalmodel of care delivery.
Data collection
The medical histories of 150 patients who had received trans-
professionalteam services in 2012 were identified using the
patientmanagementsystem,and then 150 medicalhistories
were randomly selected and examined.The medicalhistories
of 50 patients who did not receive transprofessionalservices,
but presented in the same time period (month,day,hour),
were then matched by presenting complaint,triage category,
end diagnosis,age and gender,and were also audited.The
triage category determines how long a patient can wait before
medicalassessment(AustralasianCollegefor Emergency
Medicine,2006).These data provided a baseline for compar-
ison of outcomes.For the purpose of this article,the baseline
cohort has been labelled the “reference group” (RG).
Patientdata extracted from the records included date of
birth, presenting complaint,relevantpastmedicalhistory,
socialsupportsand living arrangements,interventionsand
investigations undertaken within the ED,end diagnosis and
disposition (i.e.admitted,discharged and where they were
discharged to).Outcome measures included hospitaladmis-
sion rates,patient length of stay in the ED (which was com-
pared against the 4 hours NEAT) and unscheduled patient re-
presentation to ED within 72 hours.
Data were manually extracted from patienthistoriesby
staff from within the health service and audited for accuracy
by one of the research team members– an experienced
emergency nurse.This involved the researcher re-examining
10% of the patientmedicalhistoriesand comparingthe
extracted data with the data in the medical history.No errors
were identified.Data were then imported into SPSS V.20
(Armonk,NY: IBM Corp 2011) for statisticalanalysis.
Data analysis
Descriptive statistics(frequencies,percentages,median and
interquartilerange)havebeen used to describethe data.
Inferentialstatistics (Mann–Whitney U-test,Chi-square test
for independence) were used to make comparisons between
transprofessionalteam and RG cohorts(Brace,Kemp,&
Snelgar,2003;Pallant,2013).
Ethical considerations
Ethics approvalwas obtained before the study commenced
(HREC/12/PH/96). The data were collected by staff employed
in the hospital,who have access to this data as part of their
employment.The data collected were notidentifiable.Data
have only been presented in aggregate form.Ethical approval
was sought and received from the health service and univer-
sity prior to the study being conducted.
Results
Both transprofessionalteam and RG patientshad similar
demographic data.The median patientage was 68 years in
the team cohort and 69 years in the RG cohort.Just over half
of the patients in each sample were female and halfof the
patients in each sample lived at home with family (Table 2).
Presentation to the emergency department
The majority ofpatients in both the transprofessionalteam
and RG cohortswereallocated atriagecategory 3 or4
(Table 2).This means they were deemed by the triage nurse
to requiremedicalassessmentwithin 30 minutesand 60
minutes,respectively (Australasian Collegefor Emergency
Medicine,2005).The mostcommon reasonsthatpatients
presented to the ED were fallsand limb injury/limb pain.
Other presentingcomplaintsare displayedin Table 2.
Presentingcomplaintswhich wereinfrequenthavebeen
grouped together for ease of reading into a category labelle
“Other”.This included:motor car accident(n = 5),mental
health illness (n = 2),alleged assault(n = 2),renal(n = 2),
social problems (n = 2), investigations (n = 2), diabetes rela
(n = 2),intoxicated (n = 1),febrile (n = 1),neoplasm (n = 1)
and “Not reported” (n = 1).
Table 2.Patient presentation data:Presenting complaint,triage category,and
ED interventions.
Transprofessionalteam
group (n = 150)
Reference group
(n = 50)
Age (years) Mdn IQR Mdn IQR
68 44–84 69 44–83
Gender n % n %
Female 85 56.7 27 54.0
Male 65 43.3 23 46.0
Usualaccommodation n % n %
Home with family 79 52.7 24 48.0
Home alone 48 32.0 11 22.0
Aged care facility 7 4.7 8 16.0
Not stated 12 8.0 6 12.0
Other 4 2.7 1 2.0
Triage category n % n %
1 0 0 0 0
2 24 16.0 9 18.0
3 46 30.7 20 40.0
4 72 48.0 15 30.0
5 8 5.3 5 10.0
Presenting complaint n % n %
Fall 37 24.7 9 18.0
Limb injury/limb pain 33 22.0 14 28.0
Back pain 14 9.3 2 4.0
Other 13 8.7 8 16.0
Soft-tissue injury 10 6.7 2 4.0
Fracture 8 5.3 0 0
Stroke symptoms 6 4.0 2 4.0
Cardiac related 6 4.0 4 8.0
Abnormalbehaviour/confusion 5 3.3 5 10.0
Short of breath 5 3.3 2 4.0
Dizziness/collapse 5 3.3 1 2.0
Generally unwell 4 2.7 1 2.0
Abdominalrelated 4 2.7 0 0
ED interventions* n % n %
Radiology 99 66.0 33 66.0
Analgesia 73 48.7 24 48.0
Referralto specialist 65 43.3 24 48.0
Pathology 61 40.7 31 62.0*
IV fluids 25 16.7 13 26.0
Plaster/wound management 19 12.7 8 16.0
Note:Many patients had more than one type of investigation.
* denotes p = 0.01 for comparison;allother comparisons non-significant.
228 J. MORPHET ET AL.
Downloaded by [Library Services City University London] at 18:00 04 April 2016
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Patient journey through the emergency department
The median time patientsspentwaiting to see a medical
officerwas 62 minutes (IQR = 28–139 minutes).There was
no significantdifference in the time thattransprofessional
team (TT) and RG patients waited to see a medicalofficer
(TT Mdn = 67 minutes,IQR = 28–139;RG Mdn = 45
minutes,IQR = 22–103,p = 0.15).
Emergency department interventions
Patients in both cohorts had similar investigations and inter-
ventionswithin the ED.Almost halfof the patients in both
the transprofessional team and RG cohorts received analgesia.
Two-thirds of patients in each cohort had radiologicalinves-
tigations and less than one-fifth ofpatients needed wound
managementor a plaster ofParis castapplied.Significantly
more RG patients had pathology collected (i.e.blood investi-
gations) (p = 0.01) (Table 2).
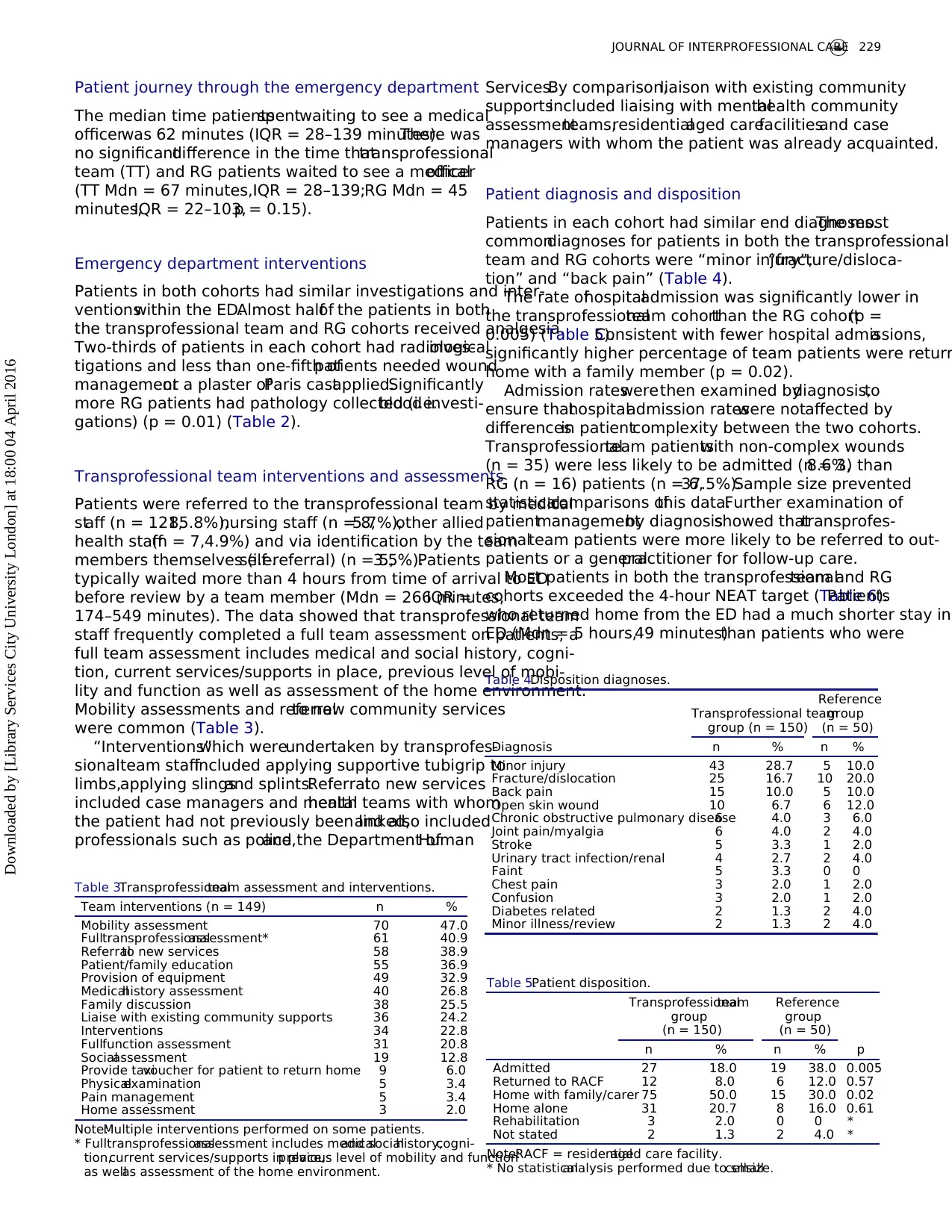
Transprofessional team interventions and assessments
Patients were referred to the transprofessional team by medical
staff (n = 121,85.8%),nursing staff (n = 8,5.7%),other allied
health staff(n = 7,4.9%) and via identification by the team
members themselves (i.e.self-referral) (n = 5,3.5%).Patients
typically waited more than 4 hours from time of arrival to ED
before review by a team member (Mdn = 266 minutes,IQR =
174–549 minutes). The data showed that transprofessional team
staff frequently completed a full team assessment on patients; a
full team assessment includes medical and social history, cogni-
tion, current services/supports in place, previous level of mobi-
lity and function as well as assessment of the home environment.
Mobility assessments and referralto new community services
were common (Table 3).
“Interventions”which wereundertaken by transprofes-
sionalteam staffincluded applying supportive tubigrip to
limbs,applying slingsand splints.Referralto new services
included case managers and mentalhealth teams with whom
the patient had not previously been linked,and also included
professionals such as police,and the Department ofHuman
Services.By comparison,liaison with existing community
supportsincluded liaising with mentalhealth community
assessmentteams,residentialaged carefacilitiesand case
managers with whom the patient was already acquainted.
Patient diagnosis and disposition
Patients in each cohort had similar end diagnoses.The most
commondiagnoses for patients in both the transprofessional
team and RG cohorts were “minor injury”,“fracture/disloca-
tion” and “back pain” (Table 4).
The rate ofhospitaladmission was significantly lower in
the transprofessionalteam cohortthan the RG cohort(p =
0.005) (Table 5).Consistent with fewer hospital admissions,a
significantly higher percentage of team patients were return
home with a family member (p = 0.02).
Admission rateswerethen examined bydiagnosis,to
ensure thathospitaladmission rateswere notaffected by
differencesin patientcomplexity between the two cohorts.
Transprofessionalteam patientswith non-complex wounds
(n = 35) were less likely to be admitted (n = 3,8.6%) than
RG (n = 16) patients (n = 6,37.5%).Sample size prevented
statisticalcomparisons ofthis data.Further examination of
patientmanagementby diagnosisshowed thattransprofes-
sionalteam patients were more likely to be referred to out-
patients or a generalpractitioner for follow-up care.
Most patients in both the transprofessionalteam and RG
cohorts exceeded the 4-hour NEAT target (Table 6).Patients
who returned home from the ED had a much shorter stay in
ED (Mdn = 5 hours,49 minutes)than patients who were
Table 3.Transprofessionalteam assessment and interventions.
Team interventions (n = 149) n %
Mobility assessment 70 47.0
Fulltransprofessionalassessment* 61 40.9
Referralto new services 58 38.9
Patient/family education 55 36.9
Provision of equipment 49 32.9
Medicalhistory assessment 40 26.8
Family discussion 38 25.5
Liaise with existing community supports 36 24.2
Interventions 34 22.8
Fullfunction assessment 31 20.8
Socialassessment 19 12.8
Provide taxivoucher for patient to return home 9 6.0
Physicalexamination 5 3.4
Pain management 5 3.4
Home assessment 3 2.0
Note:Multiple interventions performed on some patients.
* Fulltransprofessionalassessment includes medicaland socialhistory,cogni-
tion,current services/supports in place,previous level of mobility and function
as wellas assessment of the home environment.
Table 4.Disposition diagnoses.
Transprofessional team
group (n = 150)
Reference
group
(n = 50)
Diagnosis n % n %
Minor injury 43 28.7 5 10.0
Fracture/dislocation 25 16.7 10 20.0
Back pain 15 10.0 5 10.0
Open skin wound 10 6.7 6 12.0
Chronic obstructive pulmonary disease6 4.0 3 6.0
Joint pain/myalgia 6 4.0 2 4.0
Stroke 5 3.3 1 2.0
Urinary tract infection/renal 4 2.7 2 4.0
Faint 5 3.3 0 0
Chest pain 3 2.0 1 2.0
Confusion 3 2.0 1 2.0
Diabetes related 2 1.3 2 4.0
Minor illness/review 2 1.3 2 4.0
Table 5.Patient disposition.
Transprofessionalteam
group
(n = 150)
Reference
group
(n = 50)
n % n % p
Admitted 27 18.0 19 38.0 0.005
Returned to RACF 12 8.0 6 12.0 0.57
Home with family/carer 75 50.0 15 30.0 0.02
Home alone 31 20.7 8 16.0 0.61
Rehabilitation 3 2.0 0 0 *
Not stated 2 1.3 2 4.0 *
Note:RACF = residentialaged care facility.
* No statisticalanalysis performed due to smallcellsize.
JOURNAL OF INTERPROFESSIONAL CARE 229
Downloaded by [Library Services City University London] at 18:00 04 April 2016
The median time patientsspentwaiting to see a medical
officerwas 62 minutes (IQR = 28–139 minutes).There was
no significantdifference in the time thattransprofessional
team (TT) and RG patients waited to see a medicalofficer
(TT Mdn = 67 minutes,IQR = 28–139;RG Mdn = 45
minutes,IQR = 22–103,p = 0.15).
Emergency department interventions
Patients in both cohorts had similar investigations and inter-
ventionswithin the ED.Almost halfof the patients in both
the transprofessional team and RG cohorts received analgesia.
Two-thirds of patients in each cohort had radiologicalinves-
tigations and less than one-fifth ofpatients needed wound
managementor a plaster ofParis castapplied.Significantly
more RG patients had pathology collected (i.e.blood investi-
gations) (p = 0.01) (Table 2).
Transprofessional team interventions and assessments
Patients were referred to the transprofessional team by medical
staff (n = 121,85.8%),nursing staff (n = 8,5.7%),other allied
health staff(n = 7,4.9%) and via identification by the team
members themselves (i.e.self-referral) (n = 5,3.5%).Patients
typically waited more than 4 hours from time of arrival to ED
before review by a team member (Mdn = 266 minutes,IQR =
174–549 minutes). The data showed that transprofessional team
staff frequently completed a full team assessment on patients; a
full team assessment includes medical and social history, cogni-
tion, current services/supports in place, previous level of mobi-
lity and function as well as assessment of the home environment.
Mobility assessments and referralto new community services
were common (Table 3).
“Interventions”which wereundertaken by transprofes-
sionalteam staffincluded applying supportive tubigrip to
limbs,applying slingsand splints.Referralto new services
included case managers and mentalhealth teams with whom
the patient had not previously been linked,and also included
professionals such as police,and the Department ofHuman
Services.By comparison,liaison with existing community
supportsincluded liaising with mentalhealth community
assessmentteams,residentialaged carefacilitiesand case
managers with whom the patient was already acquainted.
Patient diagnosis and disposition
Patients in each cohort had similar end diagnoses.The most
commondiagnoses for patients in both the transprofessional
team and RG cohorts were “minor injury”,“fracture/disloca-
tion” and “back pain” (Table 4).
The rate ofhospitaladmission was significantly lower in
the transprofessionalteam cohortthan the RG cohort(p =
0.005) (Table 5).Consistent with fewer hospital admissions,a
significantly higher percentage of team patients were return
home with a family member (p = 0.02).
Admission rateswerethen examined bydiagnosis,to
ensure thathospitaladmission rateswere notaffected by
differencesin patientcomplexity between the two cohorts.
Transprofessionalteam patientswith non-complex wounds
(n = 35) were less likely to be admitted (n = 3,8.6%) than
RG (n = 16) patients (n = 6,37.5%).Sample size prevented
statisticalcomparisons ofthis data.Further examination of
patientmanagementby diagnosisshowed thattransprofes-
sionalteam patients were more likely to be referred to out-
patients or a generalpractitioner for follow-up care.
Most patients in both the transprofessionalteam and RG
cohorts exceeded the 4-hour NEAT target (Table 6).Patients
who returned home from the ED had a much shorter stay in
ED (Mdn = 5 hours,49 minutes)than patients who were
Table 3.Transprofessionalteam assessment and interventions.
Team interventions (n = 149) n %
Mobility assessment 70 47.0
Fulltransprofessionalassessment* 61 40.9
Referralto new services 58 38.9
Patient/family education 55 36.9
Provision of equipment 49 32.9
Medicalhistory assessment 40 26.8
Family discussion 38 25.5
Liaise with existing community supports 36 24.2
Interventions 34 22.8
Fullfunction assessment 31 20.8
Socialassessment 19 12.8
Provide taxivoucher for patient to return home 9 6.0
Physicalexamination 5 3.4
Pain management 5 3.4
Home assessment 3 2.0
Note:Multiple interventions performed on some patients.
* Fulltransprofessionalassessment includes medicaland socialhistory,cogni-
tion,current services/supports in place,previous level of mobility and function
as wellas assessment of the home environment.
Table 4.Disposition diagnoses.
Transprofessional team
group (n = 150)
Reference
group
(n = 50)
Diagnosis n % n %
Minor injury 43 28.7 5 10.0
Fracture/dislocation 25 16.7 10 20.0
Back pain 15 10.0 5 10.0
Open skin wound 10 6.7 6 12.0
Chronic obstructive pulmonary disease6 4.0 3 6.0
Joint pain/myalgia 6 4.0 2 4.0
Stroke 5 3.3 1 2.0
Urinary tract infection/renal 4 2.7 2 4.0
Faint 5 3.3 0 0
Chest pain 3 2.0 1 2.0
Confusion 3 2.0 1 2.0
Diabetes related 2 1.3 2 4.0
Minor illness/review 2 1.3 2 4.0
Table 5.Patient disposition.
Transprofessionalteam
group
(n = 150)
Reference
group
(n = 50)
n % n % p
Admitted 27 18.0 19 38.0 0.005
Returned to RACF 12 8.0 6 12.0 0.57
Home with family/carer 75 50.0 15 30.0 0.02
Home alone 31 20.7 8 16.0 0.61
Rehabilitation 3 2.0 0 0 *
Not stated 2 1.3 2 4.0 *
Note:RACF = residentialaged care facility.
* No statisticalanalysis performed due to smallcellsize.
JOURNAL OF INTERPROFESSIONAL CARE 229
Downloaded by [Library Services City University London] at 18:00 04 April 2016
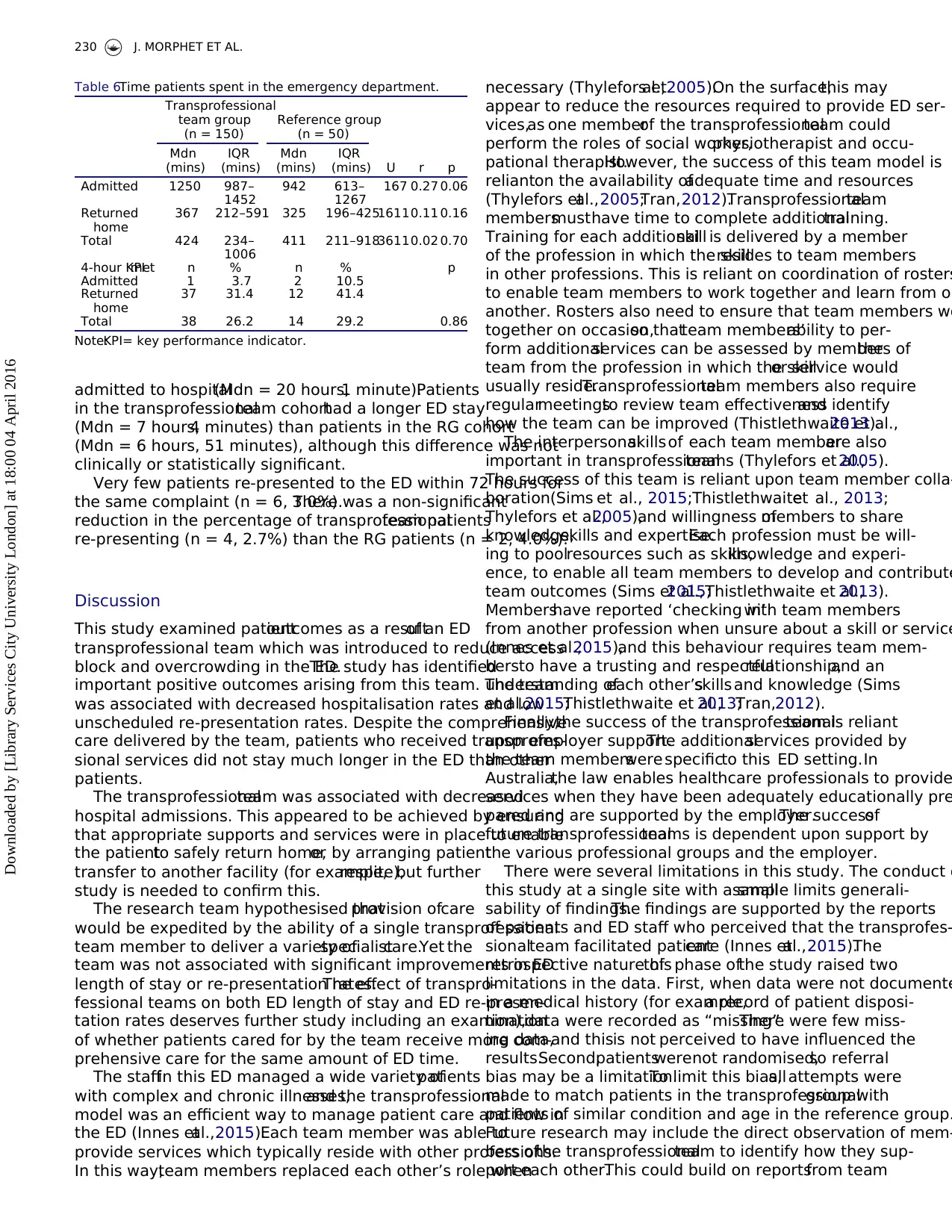
admitted to hospital(Mdn = 20 hours,1 minute).Patients
in the transprofessionalteam cohorthad a longer ED stay
(Mdn = 7 hours,4 minutes) than patients in the RG cohort
(Mdn = 6 hours, 51 minutes), although this difference was not
clinically or statistically significant.
Very few patients re-presented to the ED within 72 hours for
the same complaint (n = 6, 3.0%).There was a non-significant
reduction in the percentage of transprofessionalteam patients
re-presenting (n = 4, 2.7%) than the RG patients (n = 2, 4.0%).
Discussion
This study examined patientoutcomes as a resultof an ED
transprofessional team which was introduced to reduce access
block and overcrowding in the ED.The study has identified
important positive outcomes arising from this team. The team
was associated with decreased hospitalisation rates and low
unscheduled re-presentation rates. Despite the comprehensive
care delivered by the team, patients who received transprofes-
sional services did not stay much longer in the ED than other
patients.
The transprofessionalteam was associated with decreased
hospital admissions. This appeared to be achieved by ensuring
that appropriate supports and services were in place to enable
the patientto safely return home,or by arranging patient
transfer to another facility (for example,respite),but further
study is needed to confirm this.
The research team hypothesised thatprovision ofcare
would be expedited by the ability of a single transprofessional
team member to deliver a variety ofspecialistcare.Yet the
team was not associated with significant improvements in ED
length of stay or re-presentation rates.The effect of transpro-
fessional teams on both ED length of stay and ED re-presen-
tation rates deserves further study including an examination
of whether patients cared for by the team receive more com-
prehensive care for the same amount of ED time.
The staffin this ED managed a wide variety ofpatients
with complex and chronic illnesses,and the transprofessional
model was an efficient way to manage patient care and flow in
the ED (Innes etal.,2015).Each team member was able to
provide services which typically reside with other professions.
In this way,team members replaced each other’s role when
necessary (Thylefors etal.,2005).On the surface,this may
appear to reduce the resources required to provide ED ser-
vices,as one memberof the transprofessionalteam could
perform the roles of social worker,physiotherapist and occu-
pational therapist.However, the success of this team model is
relianton the availability ofadequate time and resources
(Thylefors etal.,2005;Tran,2012).Transprofessionalteam
membersmusthave time to complete additionaltraining.
Training for each additionalskill is delivered by a member
of the profession in which the skillresides to team members
in other professions. This is reliant on coordination of rosters
to enable team members to work together and learn from on
another. Rosters also need to ensure that team members wo
together on occasion,so thatteam members’ability to per-
form additionalservices can be assessed by members ofthe
team from the profession in which the skillor service would
usually reside.Transprofessionalteam members also require
regularmeetingsto review team effectivenessand identify
how the team can be improved (Thistlethwaite et al.,2013).
The interpersonalskillsof each team memberare also
important in transprofessionalteams (Thylefors et al.,2005).
The success of this team is reliant upon team member colla-
boration(Sims et al., 2015;Thistlethwaiteet al., 2013;
Thylefors et al.,2005),and willingness ofmembers to share
knowledge,skills and expertise.Each profession must be will-
ing to poolresources such as skills,knowledge and experi-
ence, to enable all team members to develop and contribute
team outcomes (Sims et al.,2015;Thistlethwaite et al.,2013).
Membershave reported ‘checking in’with team members
from another profession when unsure about a skill or service
(Innes et al.,2015),and this behaviour requires team mem-
bersto have a trusting and respectfulrelationship,and an
understanding ofeach other’sskills and knowledge (Sims
et al.,2015;Thistlethwaite et al.,2013;Tran,2012).
Finally,the success of the transprofessionalteam is reliant
upon employer support.The additionalservices provided by
the team memberswere specificto this ED setting.In
Australia,the law enables healthcare professionals to provide
services when they have been adequately educationally pre
pared and are supported by the employer.The successof
future transprofessionalteams is dependent upon support by
the various professional groups and the employer.
There were several limitations in this study. The conduct o
this study at a single site with a smallsample limits generali-
sability of findings.The findings are supported by the reports
of patients and ED staff who perceived that the transprofes-
sionalteam facilitated patientcare (Innes etal.,2015).The
retrospective nature ofthis phase ofthe study raised two
limitations in the data. First, when data were not documente
in a medical history (for example,a record of patient disposi-
tion),data were recorded as “missing”.There were few miss-
ing data,and thisis not perceived to have influenced the
results.Second,patientswerenot randomised,so referral
bias may be a limitation.To limit this bias,all attempts were
made to match patients in the transprofessionalgroup with
patients of similar condition and age in the reference group.
Future research may include the direct observation of mem-
bers ofthe transprofessionalteam to identify how they sup-
port each other.This could build on reportsfrom team
Table 6.Time patients spent in the emergency department.
Transprofessional
team group
(n = 150)
Reference group
(n = 50)
Mdn
(mins)
IQR
(mins)
Mdn
(mins)
IQR
(mins) U r p
Admitted 1250 987–
1452
942 613–
1267
167 0.27 0.06
Returned
home
367 212–591 325 196–42516110.11 0.16
Total 424 234–
1006
411 211–91836110.02 0.70
4-hour KPImet n % n % p
Admitted 1 3.7 2 10.5
Returned
home
37 31.4 12 41.4
Total 38 26.2 14 29.2 0.86
Note:KPI= key performance indicator.
230 J. MORPHET ET AL.
Downloaded by [Library Services City University London] at 18:00 04 April 2016
in the transprofessionalteam cohorthad a longer ED stay
(Mdn = 7 hours,4 minutes) than patients in the RG cohort
(Mdn = 6 hours, 51 minutes), although this difference was not
clinically or statistically significant.
Very few patients re-presented to the ED within 72 hours for
the same complaint (n = 6, 3.0%).There was a non-significant
reduction in the percentage of transprofessionalteam patients
re-presenting (n = 4, 2.7%) than the RG patients (n = 2, 4.0%).
Discussion
This study examined patientoutcomes as a resultof an ED
transprofessional team which was introduced to reduce access
block and overcrowding in the ED.The study has identified
important positive outcomes arising from this team. The team
was associated with decreased hospitalisation rates and low
unscheduled re-presentation rates. Despite the comprehensive
care delivered by the team, patients who received transprofes-
sional services did not stay much longer in the ED than other
patients.
The transprofessionalteam was associated with decreased
hospital admissions. This appeared to be achieved by ensuring
that appropriate supports and services were in place to enable
the patientto safely return home,or by arranging patient
transfer to another facility (for example,respite),but further
study is needed to confirm this.
The research team hypothesised thatprovision ofcare
would be expedited by the ability of a single transprofessional
team member to deliver a variety ofspecialistcare.Yet the
team was not associated with significant improvements in ED
length of stay or re-presentation rates.The effect of transpro-
fessional teams on both ED length of stay and ED re-presen-
tation rates deserves further study including an examination
of whether patients cared for by the team receive more com-
prehensive care for the same amount of ED time.
The staffin this ED managed a wide variety ofpatients
with complex and chronic illnesses,and the transprofessional
model was an efficient way to manage patient care and flow in
the ED (Innes etal.,2015).Each team member was able to
provide services which typically reside with other professions.
In this way,team members replaced each other’s role when
necessary (Thylefors etal.,2005).On the surface,this may
appear to reduce the resources required to provide ED ser-
vices,as one memberof the transprofessionalteam could
perform the roles of social worker,physiotherapist and occu-
pational therapist.However, the success of this team model is
relianton the availability ofadequate time and resources
(Thylefors etal.,2005;Tran,2012).Transprofessionalteam
membersmusthave time to complete additionaltraining.
Training for each additionalskill is delivered by a member
of the profession in which the skillresides to team members
in other professions. This is reliant on coordination of rosters
to enable team members to work together and learn from on
another. Rosters also need to ensure that team members wo
together on occasion,so thatteam members’ability to per-
form additionalservices can be assessed by members ofthe
team from the profession in which the skillor service would
usually reside.Transprofessionalteam members also require
regularmeetingsto review team effectivenessand identify
how the team can be improved (Thistlethwaite et al.,2013).
The interpersonalskillsof each team memberare also
important in transprofessionalteams (Thylefors et al.,2005).
The success of this team is reliant upon team member colla-
boration(Sims et al., 2015;Thistlethwaiteet al., 2013;
Thylefors et al.,2005),and willingness ofmembers to share
knowledge,skills and expertise.Each profession must be will-
ing to poolresources such as skills,knowledge and experi-
ence, to enable all team members to develop and contribute
team outcomes (Sims et al.,2015;Thistlethwaite et al.,2013).
Membershave reported ‘checking in’with team members
from another profession when unsure about a skill or service
(Innes et al.,2015),and this behaviour requires team mem-
bersto have a trusting and respectfulrelationship,and an
understanding ofeach other’sskills and knowledge (Sims
et al.,2015;Thistlethwaite et al.,2013;Tran,2012).
Finally,the success of the transprofessionalteam is reliant
upon employer support.The additionalservices provided by
the team memberswere specificto this ED setting.In
Australia,the law enables healthcare professionals to provide
services when they have been adequately educationally pre
pared and are supported by the employer.The successof
future transprofessionalteams is dependent upon support by
the various professional groups and the employer.
There were several limitations in this study. The conduct o
this study at a single site with a smallsample limits generali-
sability of findings.The findings are supported by the reports
of patients and ED staff who perceived that the transprofes-
sionalteam facilitated patientcare (Innes etal.,2015).The
retrospective nature ofthis phase ofthe study raised two
limitations in the data. First, when data were not documente
in a medical history (for example,a record of patient disposi-
tion),data were recorded as “missing”.There were few miss-
ing data,and thisis not perceived to have influenced the
results.Second,patientswerenot randomised,so referral
bias may be a limitation.To limit this bias,all attempts were
made to match patients in the transprofessionalgroup with
patients of similar condition and age in the reference group.
Future research may include the direct observation of mem-
bers ofthe transprofessionalteam to identify how they sup-
port each other.This could build on reportsfrom team
Table 6.Time patients spent in the emergency department.
Transprofessional
team group
(n = 150)
Reference group
(n = 50)
Mdn
(mins)
IQR
(mins)
Mdn
(mins)
IQR
(mins) U r p
Admitted 1250 987–
1452
942 613–
1267
167 0.27 0.06
Returned
home
367 212–591 325 196–42516110.11 0.16
Total 424 234–
1006
411 211–91836110.02 0.70
4-hour KPImet n % n % p
Admitted 1 3.7 2 10.5
Returned
home
37 31.4 12 41.4
Total 38 26.2 14 29.2 0.86
Note:KPI= key performance indicator.
230 J. MORPHET ET AL.
Downloaded by [Library Services City University London] at 18:00 04 April 2016
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
members who have indicated that they work closely together,
sharing knowledge and training each other in the skillsof
their own profession (Innes et al.,2015).
Concluding comments
Transprofessional teams offer a unique solution to meeting the
varied specialist care needs of patients in the ED. This ED team
are making a substantial contribution to the ED management of
patients.Transprofessional team services in the ED were asso-
ciated with lower hospital admission rates and less unscheduled
re-presentation rates, which reduces overcrowding.
Acknowledgements
The research team gratefully acknowledge the support of the
ED staff, particularly thetransprofessionalteam members
who supported this study.
Declaration of interest
The authors report no conflicts of interest.The authors alone
are responsible for the content and writing of this article.
Funding
This study wasfunded by a Monash University Peninsula
Campus Research Grant.
References
Australasian College for Emergency Medicine.(2005).Guidelines on the
implementation ofthe Australasian triage scale in emergency depart-
ments.Melbourne,Australia:Australasian Collegefor Emergency
Medicine.
Australasian Collegefor Emergency Medicine.(2006).Policy on the
Australasian triage scale.Melbourne,Australia:Australasian College
for Emergency Medicine.
Australasian College for Emergency Medicine.(2009).ACEM policy on
standard terminology.Melbourne,Australia:ACEM.
Australian Institute ofHealth and Welfare.(2011).Australian hospital
statistics.Retrieved from www.aihw.gov.au/publication-detail/?id=
10737418863
Australian Instituteof Health and Welfare.(2013).My hospitals.
Retrieved from http://www.myhospitals.gov.au/
Brace,N., Kemp,R., & Snelgar,R. (2003).SPSS for psychologists (2nd
ed.).New York,NY: Palgrave Macmillan.
Cartmill,C., Soklaridis,S.,& Cassidy,J. (2011).Transdisciplinary team-
work: The experience of clinicians at a functional restoration program.
Journal of Occupational Rehabilitation,21(1),1–8.
Crawford,K., Morphet,J., Jones,T., Innes,K., Griffiths,D.,& Williams,
A. (2014).Initiativesto reduce overcrowding and accessblock in
Australian emergency departments:A literaturereview.Collegian.
21,359–366.
Daly, D., & Matzel, S. C. (2013). Building a transdisciplinary approach to
palliative care in an acute care setting.Omega (United States),67(1–
2),43–51.
Departmentof Health and Ageing.(2012).Nationalemergency access
target.Retrieved from http://www.health.gov.au/internet/yourhealth/
publishing.nsf/Content/npa-improvingpublichospitals-agreement-
toc~schedule-c
Dyer,J. A. (2003).Multidisciplinary,interdisciplinary,and transdisci-
plinary: Educationalmodels and nursing education.Nursing
Education Perspectives,24(4),186–188.
Goonan,S. (2011).Trans-disciplinaryserviceprovision.Frankston,
Australia:Peninsula Health.
Innes,K., Crawford,K., Jones,T., Blight,R., Trenham,C., Williams,
A.,. . .Morphet,J. (2015).Transdisciplinary care in the emergency
department:A qualitative analysis.InternationalEmergency Nursing.
Advance online publication.doi:10.1016/j.ienj.2015.07.003
King, G., Strachan, D., Tucker, M., Duwyn, B., Desserud, S., & Shillingto
M. (2009).The application of a transdisciplinary model for early inter-
vention services. Infants and Young Children, 22(3), 211–223.
Kulstad, E., & Kelley, K. M. (2009). Overcrowding is associated with de
in percutaneous coronary intervention for acute myocardial infarctio
International Journal of Emergency Medicine, 2(3), 149–154.
Kulstad, E., Sikka, R., Sweis, R. T., Kelley, K. M., & Rzechula, K. H. (201
ED overcrowding is associated with an increased frequency of medic
tion errors. American Journal of Emergency Medicine, 28(3), 304–30
Lowthian, J. A., Curtis, A. J., Jolley, D. J., Stoelwinder, J. U., McNeil, J. J.,
& Cameron, P. A. (2012). Demand at the emergency department fro
door:10-year trends in presentations.MedicalJournalof Australia,
196(2),128–132.
New South Wales Health. (2007). Key drivers of demand in the emerge
department:A hypothesisdriven approach to analysedemand and
supply.Sydney,Australia:New South Wales Health.
Pallant,J. (2013).SPSS survivalmanual(5th ed.).Sydney,Australia:
Allen & Unwin.
Pallin,D. J., Allen,M. B., Espinola,J. A., Camargo,C. A., & Stephen
Bohan,J. (2013).The care span population aging and emergency
departments:Visits willnot increase,lengths-of-stay and hospitaliza-
tions will.Health Affairs,32(7),1306–1312.
Pines, J. M., Garson, C., Baxt, W. G., Rhodes, K. V., Shofer, F. S., & Holl
J. E. (2007).ED crowding is associated with variable perceptions of car
compromise. Academic Emergency Medicine, 14(12), 1176–1181.
Productivity Commission.(2005).Australia’s health workforce:Research
report.Canberra,Australia:Productivity Commission.
Reilly,C. (2001).Transdisciplinary approach:An atypicalstrategy for
improving outcomes in rehabilitative and long-term acute care set-
tings.Rehabilitation nursing:The officialjournalof the Association of
Rehabilitation Nurses,26(6),216–220,244.
Rosenfield,P. L. (1992).The potentialof transdisciplinary research for
sustaining and extending linkagesbetween thehealth and social
sciences.SocialScience and Medicine,35(11),1343–1357.
Sills, M. R., Fairclough,D., Ranade,D., & Kahn, M. G. (2011).
Emergency department crowding is associated with decreased qual
of care for children with acute asthma. Annals of Emergency Medici
57(3),191–200.e191–e197.
Sims,S., Hewitt,G., & Harris, R. (2015).Evidence ofcollaboration,
pooling ofresources,learning and role blurring in interprofessional
healthcare teams: A realist synthesis. Journal of Interprofessional Ca
29,20–25.doi:10.3109/13561820.2014.939745
Smart,C. J., & Smith,B. L. (2013).A transdisciplinary team approach to
perinatal loss. MCN The American Journal of Maternal/Child Nursing,
38(2),110–114.
Sprivulis, P. C., Da Silva, J. A., Jacobs, I. G., Frazer, A. R. L., & Jelinek, G
A. (2006).The association between hospitalovercrowding and mor-
tality among patientsadmitted via Western Australian emergency
departments.MedicalJournalof Australia,184(5),208–212.
Stepans,M. B.,Thompson,C. L.,& Buchanan,M. L. (2002).The role of
the nurse on a transdisciplinary early intervention assessment team
Public Health Nursing,19(4),238–245.
Thistlethwaite,J., Jackson,A., & Moran, M. (2013).Interprofessional
collaborative practice:A deconstruction.Journalof Interprofessional
Care,27,50–56.doi:10.3109/13561820.2012.730075
Thylefors, I.,Persson, O.,& Hellström,D. (2005). Team types, perceived
efficiency and team climate in Swedish cross-professionalteamwork.
Journal of InterprofessionalCare, 19, 102–114.doi:10.1080/
13561820400024159
Tran,A. (2012).Acute caring in the emergency department.Journalof
Interprofessional Care, 26, 505–507. doi:10.3109/13561820.2012.71
Trzeciak,S.,& Rivers,E. (2003).Emergency department overcrowding in
the United States: An emerging threat to patient safety and public h
Emergency Medicine Journal, 20, 402–405. doi:10.1136/emj.20.5.40
JOURNAL OF INTERPROFESSIONAL CARE 231
Downloaded by [Library Services City University London] at 18:00 04 April 2016
sharing knowledge and training each other in the skillsof
their own profession (Innes et al.,2015).
Concluding comments
Transprofessional teams offer a unique solution to meeting the
varied specialist care needs of patients in the ED. This ED team
are making a substantial contribution to the ED management of
patients.Transprofessional team services in the ED were asso-
ciated with lower hospital admission rates and less unscheduled
re-presentation rates, which reduces overcrowding.
Acknowledgements
The research team gratefully acknowledge the support of the
ED staff, particularly thetransprofessionalteam members
who supported this study.
Declaration of interest
The authors report no conflicts of interest.The authors alone
are responsible for the content and writing of this article.
Funding
This study wasfunded by a Monash University Peninsula
Campus Research Grant.
References
Australasian College for Emergency Medicine.(2005).Guidelines on the
implementation ofthe Australasian triage scale in emergency depart-
ments.Melbourne,Australia:Australasian Collegefor Emergency
Medicine.
Australasian Collegefor Emergency Medicine.(2006).Policy on the
Australasian triage scale.Melbourne,Australia:Australasian College
for Emergency Medicine.
Australasian College for Emergency Medicine.(2009).ACEM policy on
standard terminology.Melbourne,Australia:ACEM.
Australian Institute ofHealth and Welfare.(2011).Australian hospital
statistics.Retrieved from www.aihw.gov.au/publication-detail/?id=
10737418863
Australian Instituteof Health and Welfare.(2013).My hospitals.
Retrieved from http://www.myhospitals.gov.au/
Brace,N., Kemp,R., & Snelgar,R. (2003).SPSS for psychologists (2nd
ed.).New York,NY: Palgrave Macmillan.
Cartmill,C., Soklaridis,S.,& Cassidy,J. (2011).Transdisciplinary team-
work: The experience of clinicians at a functional restoration program.
Journal of Occupational Rehabilitation,21(1),1–8.
Crawford,K., Morphet,J., Jones,T., Innes,K., Griffiths,D.,& Williams,
A. (2014).Initiativesto reduce overcrowding and accessblock in
Australian emergency departments:A literaturereview.Collegian.
21,359–366.
Daly, D., & Matzel, S. C. (2013). Building a transdisciplinary approach to
palliative care in an acute care setting.Omega (United States),67(1–
2),43–51.
Departmentof Health and Ageing.(2012).Nationalemergency access
target.Retrieved from http://www.health.gov.au/internet/yourhealth/
publishing.nsf/Content/npa-improvingpublichospitals-agreement-
toc~schedule-c
Dyer,J. A. (2003).Multidisciplinary,interdisciplinary,and transdisci-
plinary: Educationalmodels and nursing education.Nursing
Education Perspectives,24(4),186–188.
Goonan,S. (2011).Trans-disciplinaryserviceprovision.Frankston,
Australia:Peninsula Health.
Innes,K., Crawford,K., Jones,T., Blight,R., Trenham,C., Williams,
A.,. . .Morphet,J. (2015).Transdisciplinary care in the emergency
department:A qualitative analysis.InternationalEmergency Nursing.
Advance online publication.doi:10.1016/j.ienj.2015.07.003
King, G., Strachan, D., Tucker, M., Duwyn, B., Desserud, S., & Shillingto
M. (2009).The application of a transdisciplinary model for early inter-
vention services. Infants and Young Children, 22(3), 211–223.
Kulstad, E., & Kelley, K. M. (2009). Overcrowding is associated with de
in percutaneous coronary intervention for acute myocardial infarctio
International Journal of Emergency Medicine, 2(3), 149–154.
Kulstad, E., Sikka, R., Sweis, R. T., Kelley, K. M., & Rzechula, K. H. (201
ED overcrowding is associated with an increased frequency of medic
tion errors. American Journal of Emergency Medicine, 28(3), 304–30
Lowthian, J. A., Curtis, A. J., Jolley, D. J., Stoelwinder, J. U., McNeil, J. J.,
& Cameron, P. A. (2012). Demand at the emergency department fro
door:10-year trends in presentations.MedicalJournalof Australia,
196(2),128–132.
New South Wales Health. (2007). Key drivers of demand in the emerge
department:A hypothesisdriven approach to analysedemand and
supply.Sydney,Australia:New South Wales Health.
Pallant,J. (2013).SPSS survivalmanual(5th ed.).Sydney,Australia:
Allen & Unwin.
Pallin,D. J., Allen,M. B., Espinola,J. A., Camargo,C. A., & Stephen
Bohan,J. (2013).The care span population aging and emergency
departments:Visits willnot increase,lengths-of-stay and hospitaliza-
tions will.Health Affairs,32(7),1306–1312.
Pines, J. M., Garson, C., Baxt, W. G., Rhodes, K. V., Shofer, F. S., & Holl
J. E. (2007).ED crowding is associated with variable perceptions of car
compromise. Academic Emergency Medicine, 14(12), 1176–1181.
Productivity Commission.(2005).Australia’s health workforce:Research
report.Canberra,Australia:Productivity Commission.
Reilly,C. (2001).Transdisciplinary approach:An atypicalstrategy for
improving outcomes in rehabilitative and long-term acute care set-
tings.Rehabilitation nursing:The officialjournalof the Association of
Rehabilitation Nurses,26(6),216–220,244.
Rosenfield,P. L. (1992).The potentialof transdisciplinary research for
sustaining and extending linkagesbetween thehealth and social
sciences.SocialScience and Medicine,35(11),1343–1357.
Sills, M. R., Fairclough,D., Ranade,D., & Kahn, M. G. (2011).
Emergency department crowding is associated with decreased qual
of care for children with acute asthma. Annals of Emergency Medici
57(3),191–200.e191–e197.
Sims,S., Hewitt,G., & Harris, R. (2015).Evidence ofcollaboration,
pooling ofresources,learning and role blurring in interprofessional
healthcare teams: A realist synthesis. Journal of Interprofessional Ca
29,20–25.doi:10.3109/13561820.2014.939745
Smart,C. J., & Smith,B. L. (2013).A transdisciplinary team approach to
perinatal loss. MCN The American Journal of Maternal/Child Nursing,
38(2),110–114.
Sprivulis, P. C., Da Silva, J. A., Jacobs, I. G., Frazer, A. R. L., & Jelinek, G
A. (2006).The association between hospitalovercrowding and mor-
tality among patientsadmitted via Western Australian emergency
departments.MedicalJournalof Australia,184(5),208–212.
Stepans,M. B.,Thompson,C. L.,& Buchanan,M. L. (2002).The role of
the nurse on a transdisciplinary early intervention assessment team
Public Health Nursing,19(4),238–245.
Thistlethwaite,J., Jackson,A., & Moran, M. (2013).Interprofessional
collaborative practice:A deconstruction.Journalof Interprofessional
Care,27,50–56.doi:10.3109/13561820.2012.730075
Thylefors, I.,Persson, O.,& Hellström,D. (2005). Team types, perceived
efficiency and team climate in Swedish cross-professionalteamwork.
Journal of InterprofessionalCare, 19, 102–114.doi:10.1080/
13561820400024159
Tran,A. (2012).Acute caring in the emergency department.Journalof
Interprofessional Care, 26, 505–507. doi:10.3109/13561820.2012.71
Trzeciak,S.,& Rivers,E. (2003).Emergency department overcrowding in
the United States: An emerging threat to patient safety and public h
Emergency Medicine Journal, 20, 402–405. doi:10.1136/emj.20.5.40
JOURNAL OF INTERPROFESSIONAL CARE 231
Downloaded by [Library Services City University London] at 18:00 04 April 2016
1 out of 7
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.