Trauma Nursing: Case Study, Mechanism of Injury, Pathophysiology, Management
VerifiedAdded on 2022/11/18
|15
|3844
|68
AI Summary
This document discusses a case study of a patient with head and leg injuries due to a motorcycle accident. It covers the mechanism of injury, pathophysiology, and management of subarachnoid hemorrhage, subdural hematoma, anterior dislocation of the ankle joint, and instability in the ankle syndesmosis.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: TRAUMA NURSING
Trauma Nursing
Name of the student
Name of the university
Author’s name
Trauma Nursing
Name of the student
Name of the university
Author’s name
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1TRAUMA NURSING
Table of Contents
Case Study.......................................................................................................................................2
Mechanism of Injury........................................................................................................................4
Pathophysiology..............................................................................................................................5
Management....................................................................................................................................7
Subarachnoid hemorrhage (SAH)............................................................................................7
Subdural hematoma.................................................................................................................7
Anterior dislocation of the ankle joint.....................................................................................8
Instability in the ankle syndesmosis........................................................................................8
Futuristic Considerations.................................................................................................................9
Conclusion.....................................................................................................................................10
Reference.......................................................................................................................................11
Table of Contents
Case Study.......................................................................................................................................2
Mechanism of Injury........................................................................................................................4
Pathophysiology..............................................................................................................................5
Management....................................................................................................................................7
Subarachnoid hemorrhage (SAH)............................................................................................7
Subdural hematoma.................................................................................................................7
Anterior dislocation of the ankle joint.....................................................................................8
Instability in the ankle syndesmosis........................................................................................8
Futuristic Considerations.................................................................................................................9
Conclusion.....................................................................................................................................10
Reference.......................................................................................................................................11
2TRAUMA NURSING
Case Study
Steve Smith is a 27-year-old male, and he was admitted to the emergency department in
an unconscious condition as he had a severe head injury and an open fracture in the right leg due
to a motorcycle accident. After the crash, he was left untreated for 45 minutes, and after that,
pedestrians kept him to the emergency department of the local hospital. After assessing the
patient, it was revealed that the patient had a GCS (Glascow Coma Scale) of 3T along with with
4mm bilaterally fixed pupils. The nursing personnel reported that the patient negatively
responded to the corneal assessment. The CT (Computed tomography) assessment of the patient
showed that the person had already developed a subarachnoid haemorrhage with left frontal and
temporal subdural damage. The nurses also reported that the patient had developed right-sided
hemi-paralysis, facial dropping.
Moreover, the CT scan showed that there is a left frontal/temporal and parietal hematoma
along with mass effect and a 5.38-mm left to right midline shift was also observed in the CT
imaging due to cerebral oedema. In the right temporal bone of the patient, there was a non-
displaced comminuted fracture. When the injury of the open fracture of the right leg was
assessed, it was demonstrated as Gustilo IIIA which is the fractures that consist of high-energy
fractures as shown by the severe bone injury (segmental or highly comminuted fractures) often
contaminated soft-tissue wounds. The nurses helped Smith clean his wounds, lavage of the
damage, removing tissue lesions, and assisted in fixing the trans-articular external leg bones at
the ankle joint in regarding deliver treatment for the injury.
The vital sign assessment of the patient stated that the person was a bradycardic and
hypertension was also reported by his family members. The recorded blood pressure of the
Case Study
Steve Smith is a 27-year-old male, and he was admitted to the emergency department in
an unconscious condition as he had a severe head injury and an open fracture in the right leg due
to a motorcycle accident. After the crash, he was left untreated for 45 minutes, and after that,
pedestrians kept him to the emergency department of the local hospital. After assessing the
patient, it was revealed that the patient had a GCS (Glascow Coma Scale) of 3T along with with
4mm bilaterally fixed pupils. The nursing personnel reported that the patient negatively
responded to the corneal assessment. The CT (Computed tomography) assessment of the patient
showed that the person had already developed a subarachnoid haemorrhage with left frontal and
temporal subdural damage. The nurses also reported that the patient had developed right-sided
hemi-paralysis, facial dropping.
Moreover, the CT scan showed that there is a left frontal/temporal and parietal hematoma
along with mass effect and a 5.38-mm left to right midline shift was also observed in the CT
imaging due to cerebral oedema. In the right temporal bone of the patient, there was a non-
displaced comminuted fracture. When the injury of the open fracture of the right leg was
assessed, it was demonstrated as Gustilo IIIA which is the fractures that consist of high-energy
fractures as shown by the severe bone injury (segmental or highly comminuted fractures) often
contaminated soft-tissue wounds. The nurses helped Smith clean his wounds, lavage of the
damage, removing tissue lesions, and assisted in fixing the trans-articular external leg bones at
the ankle joint in regarding deliver treatment for the injury.
The vital sign assessment of the patient stated that the person was a bradycardic and
hypertension was also reported by his family members. The recorded blood pressure of the
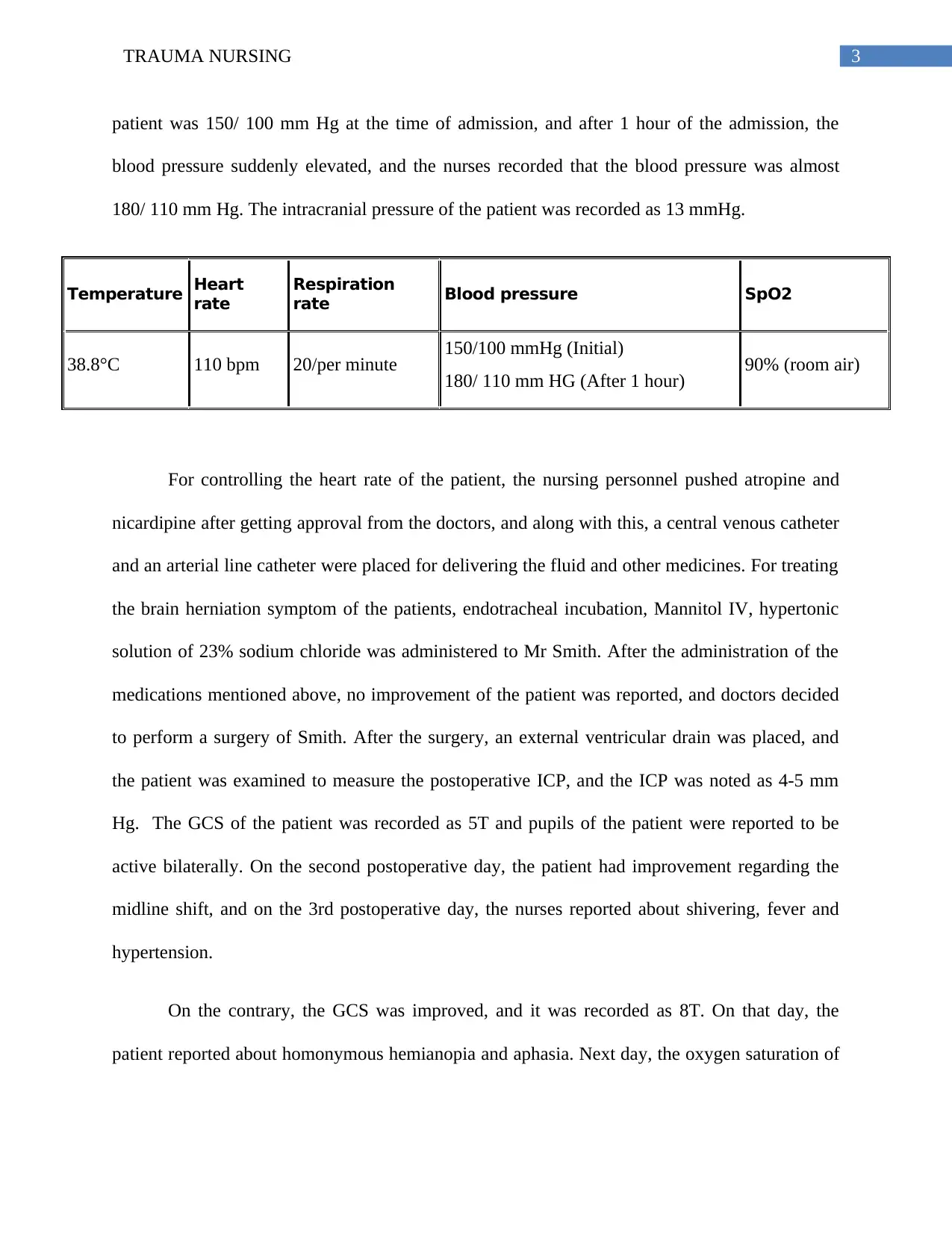
3TRAUMA NURSING
patient was 150/ 100 mm Hg at the time of admission, and after 1 hour of the admission, the
blood pressure suddenly elevated, and the nurses recorded that the blood pressure was almost
180/ 110 mm Hg. The intracranial pressure of the patient was recorded as 13 mmHg.
Temperature Heart
rate
Respiration
rate Blood pressure SpO2
38.8°C 110 bpm 20/per minute 150/100 mmHg (Initial)
180/ 110 mm HG (After 1 hour) 90% (room air)
For controlling the heart rate of the patient, the nursing personnel pushed atropine and
nicardipine after getting approval from the doctors, and along with this, a central venous catheter
and an arterial line catheter were placed for delivering the fluid and other medicines. For treating
the brain herniation symptom of the patients, endotracheal incubation, Mannitol IV, hypertonic
solution of 23% sodium chloride was administered to Mr Smith. After the administration of the
medications mentioned above, no improvement of the patient was reported, and doctors decided
to perform a surgery of Smith. After the surgery, an external ventricular drain was placed, and
the patient was examined to measure the postoperative ICP, and the ICP was noted as 4-5 mm
Hg. The GCS of the patient was recorded as 5T and pupils of the patient were reported to be
active bilaterally. On the second postoperative day, the patient had improvement regarding the
midline shift, and on the 3rd postoperative day, the nurses reported about shivering, fever and
hypertension.
On the contrary, the GCS was improved, and it was recorded as 8T. On that day, the
patient reported about homonymous hemianopia and aphasia. Next day, the oxygen saturation of
patient was 150/ 100 mm Hg at the time of admission, and after 1 hour of the admission, the
blood pressure suddenly elevated, and the nurses recorded that the blood pressure was almost
180/ 110 mm Hg. The intracranial pressure of the patient was recorded as 13 mmHg.
Temperature Heart
rate
Respiration
rate Blood pressure SpO2
38.8°C 110 bpm 20/per minute 150/100 mmHg (Initial)
180/ 110 mm HG (After 1 hour) 90% (room air)
For controlling the heart rate of the patient, the nursing personnel pushed atropine and
nicardipine after getting approval from the doctors, and along with this, a central venous catheter
and an arterial line catheter were placed for delivering the fluid and other medicines. For treating
the brain herniation symptom of the patients, endotracheal incubation, Mannitol IV, hypertonic
solution of 23% sodium chloride was administered to Mr Smith. After the administration of the
medications mentioned above, no improvement of the patient was reported, and doctors decided
to perform a surgery of Smith. After the surgery, an external ventricular drain was placed, and
the patient was examined to measure the postoperative ICP, and the ICP was noted as 4-5 mm
Hg. The GCS of the patient was recorded as 5T and pupils of the patient were reported to be
active bilaterally. On the second postoperative day, the patient had improvement regarding the
midline shift, and on the 3rd postoperative day, the nurses reported about shivering, fever and
hypertension.
On the contrary, the GCS was improved, and it was recorded as 8T. On that day, the
patient reported about homonymous hemianopia and aphasia. Next day, the oxygen saturation of
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4TRAUMA NURSING
the patient was dropped to 87% from 90%. The chest x-ray and respiratory culture revealed that
there was a severe bipolar opacity.
the patient was dropped to 87% from 90%. The chest x-ray and respiratory culture revealed that
there was a severe bipolar opacity.
5TRAUMA NURSING
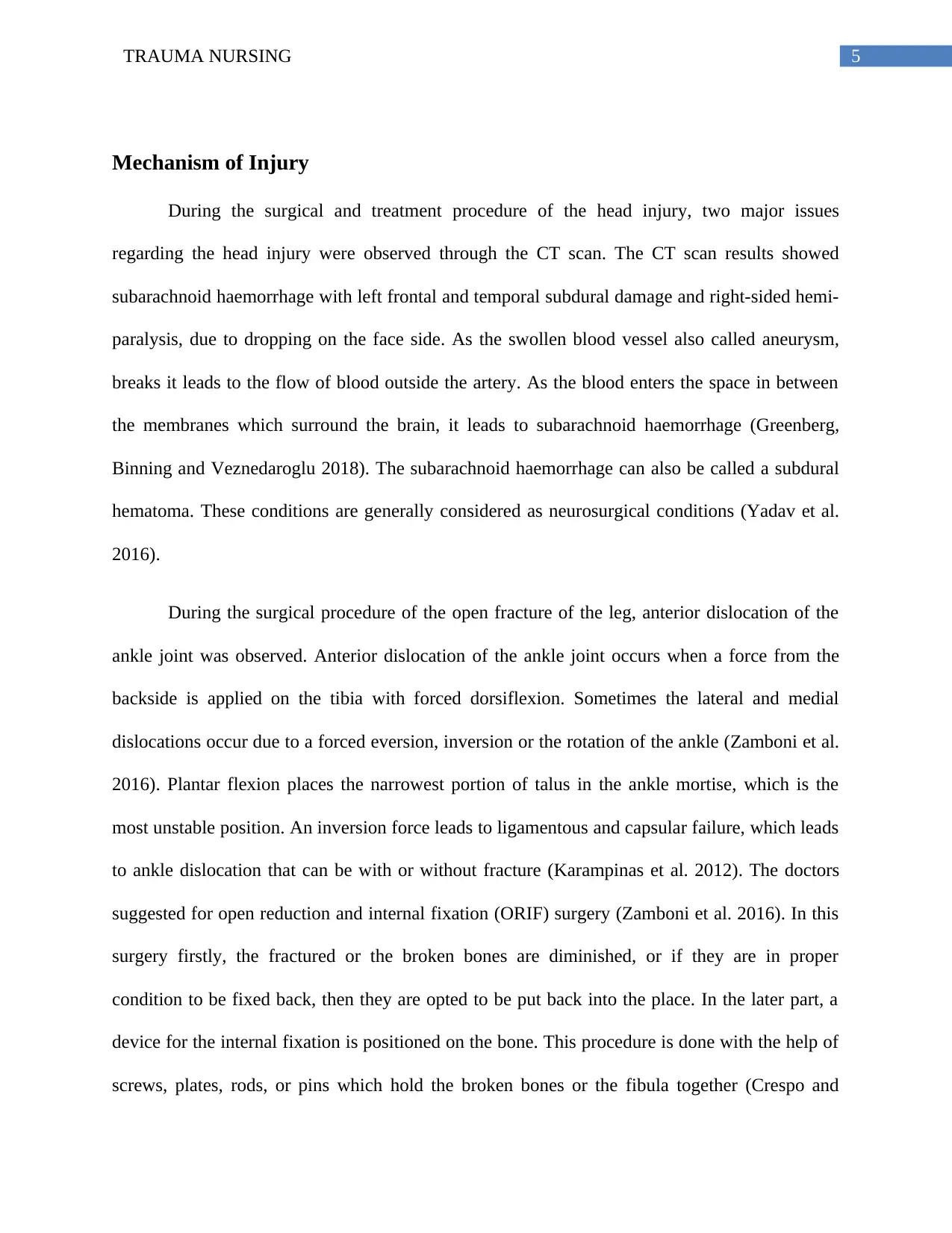
Mechanism of Injury
During the surgical and treatment procedure of the head injury, two major issues
regarding the head injury were observed through the CT scan. The CT scan results showed
subarachnoid haemorrhage with left frontal and temporal subdural damage and right-sided hemi-
paralysis, due to dropping on the face side. As the swollen blood vessel also called aneurysm,
breaks it leads to the flow of blood outside the artery. As the blood enters the space in between
the membranes which surround the brain, it leads to subarachnoid haemorrhage (Greenberg,
Binning and Veznedaroglu 2018). The subarachnoid haemorrhage can also be called a subdural
hematoma. These conditions are generally considered as neurosurgical conditions (Yadav et al.
2016).
During the surgical procedure of the open fracture of the leg, anterior dislocation of the
ankle joint was observed. Anterior dislocation of the ankle joint occurs when a force from the
backside is applied on the tibia with forced dorsiflexion. Sometimes the lateral and medial
dislocations occur due to a forced eversion, inversion or the rotation of the ankle (Zamboni et al.
2016). Plantar flexion places the narrowest portion of talus in the ankle mortise, which is the
most unstable position. An inversion force leads to ligamentous and capsular failure, which leads
to ankle dislocation that can be with or without fracture (Karampinas et al. 2012). The doctors
suggested for open reduction and internal fixation (ORIF) surgery (Zamboni et al. 2016). In this
surgery firstly, the fractured or the broken bones are diminished, or if they are in proper
condition to be fixed back, then they are opted to be put back into the place. In the later part, a
device for the internal fixation is positioned on the bone. This procedure is done with the help of
screws, plates, rods, or pins which hold the broken bones or the fibula together (Crespo and
Mechanism of Injury
During the surgical and treatment procedure of the head injury, two major issues
regarding the head injury were observed through the CT scan. The CT scan results showed
subarachnoid haemorrhage with left frontal and temporal subdural damage and right-sided hemi-
paralysis, due to dropping on the face side. As the swollen blood vessel also called aneurysm,
breaks it leads to the flow of blood outside the artery. As the blood enters the space in between
the membranes which surround the brain, it leads to subarachnoid haemorrhage (Greenberg,
Binning and Veznedaroglu 2018). The subarachnoid haemorrhage can also be called a subdural
hematoma. These conditions are generally considered as neurosurgical conditions (Yadav et al.
2016).
During the surgical procedure of the open fracture of the leg, anterior dislocation of the
ankle joint was observed. Anterior dislocation of the ankle joint occurs when a force from the
backside is applied on the tibia with forced dorsiflexion. Sometimes the lateral and medial
dislocations occur due to a forced eversion, inversion or the rotation of the ankle (Zamboni et al.
2016). Plantar flexion places the narrowest portion of talus in the ankle mortise, which is the
most unstable position. An inversion force leads to ligamentous and capsular failure, which leads
to ankle dislocation that can be with or without fracture (Karampinas et al. 2012). The doctors
suggested for open reduction and internal fixation (ORIF) surgery (Zamboni et al. 2016). In this
surgery firstly, the fractured or the broken bones are diminished, or if they are in proper
condition to be fixed back, then they are opted to be put back into the place. In the later part, a
device for the internal fixation is positioned on the bone. This procedure is done with the help of
screws, plates, rods, or pins which hold the broken bones or the fibula together (Crespo and
6TRAUMA NURSING
Tejwani 2019). Later a Cotton test was done, which showed a positive outcome which leads to
instability in the ankle syndesmosis (Zamboni et al. 2016). Cotton tests are the tests that use
manual stress to detect the extent of lateral translation of the talus within the ankle mortise. The
examiner or the doctor steadies the proximal ankle while moving the talus sideways. A positive
test result in high motion comparative to the uninvolved side and indicates the symptom of
sprain of the distal tibiofibular syndesmosis or the subtalar joint (Großterlinden et al. 2016).
When there is a rupture in the anterior tibiofibular ligament (ATiFL), it causes instability in the
ankle mortise. Furthermore, an injury in the syndesmosis causes pain during any activity, which
further raises a feeling of instability and weakness of the ankle (Wagener, Beumer and Swierstra
2011).
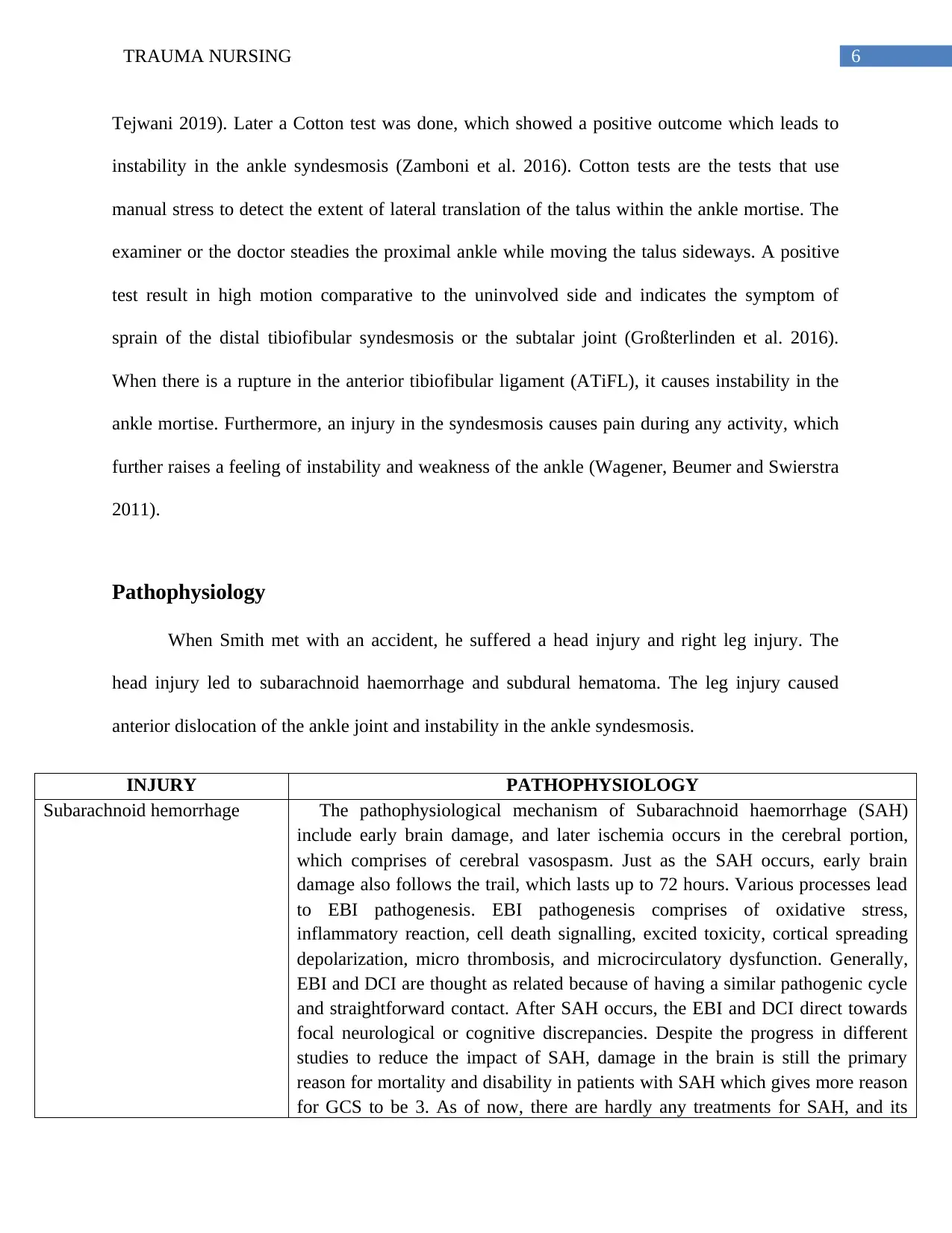
Pathophysiology
When Smith met with an accident, he suffered a head injury and right leg injury. The
head injury led to subarachnoid haemorrhage and subdural hematoma. The leg injury caused
anterior dislocation of the ankle joint and instability in the ankle syndesmosis.
INJURY PATHOPHYSIOLOGY
Subarachnoid hemorrhage The pathophysiological mechanism of Subarachnoid haemorrhage (SAH)
include early brain damage, and later ischemia occurs in the cerebral portion,
which comprises of cerebral vasospasm. Just as the SAH occurs, early brain
damage also follows the trail, which lasts up to 72 hours. Various processes lead
to EBI pathogenesis. EBI pathogenesis comprises of oxidative stress,
inflammatory reaction, cell death signalling, excited toxicity, cortical spreading
depolarization, micro thrombosis, and microcirculatory dysfunction. Generally,
EBI and DCI are thought as related because of having a similar pathogenic cycle
and straightforward contact. After SAH occurs, the EBI and DCI direct towards
focal neurological or cognitive discrepancies. Despite the progress in different
studies to reduce the impact of SAH, damage in the brain is still the primary
reason for mortality and disability in patients with SAH which gives more reason
for GCS to be 3. As of now, there are hardly any treatments for SAH, and its
Tejwani 2019). Later a Cotton test was done, which showed a positive outcome which leads to
instability in the ankle syndesmosis (Zamboni et al. 2016). Cotton tests are the tests that use
manual stress to detect the extent of lateral translation of the talus within the ankle mortise. The
examiner or the doctor steadies the proximal ankle while moving the talus sideways. A positive
test result in high motion comparative to the uninvolved side and indicates the symptom of
sprain of the distal tibiofibular syndesmosis or the subtalar joint (Großterlinden et al. 2016).
When there is a rupture in the anterior tibiofibular ligament (ATiFL), it causes instability in the
ankle mortise. Furthermore, an injury in the syndesmosis causes pain during any activity, which
further raises a feeling of instability and weakness of the ankle (Wagener, Beumer and Swierstra
2011).
Pathophysiology
When Smith met with an accident, he suffered a head injury and right leg injury. The
head injury led to subarachnoid haemorrhage and subdural hematoma. The leg injury caused
anterior dislocation of the ankle joint and instability in the ankle syndesmosis.
INJURY PATHOPHYSIOLOGY
Subarachnoid hemorrhage The pathophysiological mechanism of Subarachnoid haemorrhage (SAH)
include early brain damage, and later ischemia occurs in the cerebral portion,
which comprises of cerebral vasospasm. Just as the SAH occurs, early brain
damage also follows the trail, which lasts up to 72 hours. Various processes lead
to EBI pathogenesis. EBI pathogenesis comprises of oxidative stress,
inflammatory reaction, cell death signalling, excited toxicity, cortical spreading
depolarization, micro thrombosis, and microcirculatory dysfunction. Generally,
EBI and DCI are thought as related because of having a similar pathogenic cycle
and straightforward contact. After SAH occurs, the EBI and DCI direct towards
focal neurological or cognitive discrepancies. Despite the progress in different
studies to reduce the impact of SAH, damage in the brain is still the primary
reason for mortality and disability in patients with SAH which gives more reason
for GCS to be 3. As of now, there are hardly any treatments for SAH, and its
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7TRAUMA NURSING
consequences are devastating known so far (Reis et al. 2017).
Subdural hematoma A slight shock initiates the development of a chronic subdural haematoma
(CSDH). Trauma leads to stress that slightly slices the border cells of the dural
following which cerebrospinal fluid and blood are interrupted among the pathway
of the border lining of the dural. The damaged dural border lining discharge
cytokines which attract the inflammatory cells, that infiltrates specifically
neutrophils and eosinophils. A little number of fibroblasts turn to myofibroblasts
and produce chemokines, engaging more inflammatory cells. Prostaglandins and
chemokines persuade the expression of vascular endothelial growth factor
(VEGF). The juvenile vessels not having basal membrane are exposed to high
compression. These lead to extravasation of vascular components into the
hematoma hollow. Gradually additional eosinophils, plasminogen and thrombin,
are discharged in hollow. Fibrin clots are fragmented; platelets fail in combining,
causing cell damage and an upsurge in inflammatory cells and VEGF
manufacture. The pathway continues, which changes hygroma to turn into a
chronic subdural hematoma. The CSDH increases to a size that hampers the CBF
and breakdown of brain structures leads to indications, like hemiparesis or mental
disorder (Holl et al. 2018).
Anterior dislocation of the
ankle joint
Ankle joint comprises articulation of tibia, fibula, and talus. The joint is
balanced by three ligamentous systems: a complex of the lateral ligament, the
medial deltoid ligament, and the syndesmotic ligaments. Common ankle injury
occurs with inversion of the ankle and stressing the lateral ligament complex. The
anterior talofibular (ATFL) is the frailest ligament, and around 70% of lateral
ankle sprains comprise of only this ligament. The distal tibiofibular syndesmotic
ligaments bind the tibia and fibula together, and injuries to this complex have
been referred to as “high ankle sprains” and are much less common than other
sprains. Given the amount of force required to injure this ligamentous complex,
this injury is usually uncommon in a population and generally occur in
competitive athletes. The most common mechanism of high ankle injuries is the
external rotation and ankle dorsiflexion (Melanson and Shuman 2018).
Instability in the ankle
syndesmosis
A syndesmosis is a fibrous articulation where ligaments join the opposite joints.
Syndesmotic wounds are generally linked with Weber C/pronation exterior
turning or pronation abduction and less frequent with Weber B/supination
exterior turning ankle fractures. Syndesmotic wounds also occur in isolation due
to an exorotation trauma or in relation with damage to the lateral ankle ligaments
after traumatic supination. During exterior turning of the feet, the fibula is
interpreted posteriorly and turned outwards, resulting in stiffness of the ATiFL
portion, which contributes to breakage of the ATiFL portion (Bekerom 2011).
Breakage of ATiFL leads to instability and weakness in the ankle mortise. A
wound in syndesmosis results in a feeling of instability and weakness of the
consequences are devastating known so far (Reis et al. 2017).
Subdural hematoma A slight shock initiates the development of a chronic subdural haematoma
(CSDH). Trauma leads to stress that slightly slices the border cells of the dural
following which cerebrospinal fluid and blood are interrupted among the pathway
of the border lining of the dural. The damaged dural border lining discharge
cytokines which attract the inflammatory cells, that infiltrates specifically
neutrophils and eosinophils. A little number of fibroblasts turn to myofibroblasts
and produce chemokines, engaging more inflammatory cells. Prostaglandins and
chemokines persuade the expression of vascular endothelial growth factor
(VEGF). The juvenile vessels not having basal membrane are exposed to high
compression. These lead to extravasation of vascular components into the
hematoma hollow. Gradually additional eosinophils, plasminogen and thrombin,
are discharged in hollow. Fibrin clots are fragmented; platelets fail in combining,
causing cell damage and an upsurge in inflammatory cells and VEGF
manufacture. The pathway continues, which changes hygroma to turn into a
chronic subdural hematoma. The CSDH increases to a size that hampers the CBF
and breakdown of brain structures leads to indications, like hemiparesis or mental
disorder (Holl et al. 2018).
Anterior dislocation of the
ankle joint
Ankle joint comprises articulation of tibia, fibula, and talus. The joint is
balanced by three ligamentous systems: a complex of the lateral ligament, the
medial deltoid ligament, and the syndesmotic ligaments. Common ankle injury
occurs with inversion of the ankle and stressing the lateral ligament complex. The
anterior talofibular (ATFL) is the frailest ligament, and around 70% of lateral
ankle sprains comprise of only this ligament. The distal tibiofibular syndesmotic
ligaments bind the tibia and fibula together, and injuries to this complex have
been referred to as “high ankle sprains” and are much less common than other
sprains. Given the amount of force required to injure this ligamentous complex,
this injury is usually uncommon in a population and generally occur in
competitive athletes. The most common mechanism of high ankle injuries is the
external rotation and ankle dorsiflexion (Melanson and Shuman 2018).
Instability in the ankle
syndesmosis
A syndesmosis is a fibrous articulation where ligaments join the opposite joints.
Syndesmotic wounds are generally linked with Weber C/pronation exterior
turning or pronation abduction and less frequent with Weber B/supination
exterior turning ankle fractures. Syndesmotic wounds also occur in isolation due
to an exorotation trauma or in relation with damage to the lateral ankle ligaments
after traumatic supination. During exterior turning of the feet, the fibula is
interpreted posteriorly and turned outwards, resulting in stiffness of the ATiFL
portion, which contributes to breakage of the ATiFL portion (Bekerom 2011).
Breakage of ATiFL leads to instability and weakness in the ankle mortise. A
wound in syndesmosis results in a feeling of instability and weakness of the
8TRAUMA NURSING
ankle. Also, tenderness of ATiFL and swelling of the syndesmosis causes a high
sprain type symptom (Wagener, Beumer and Swierstra 2011).
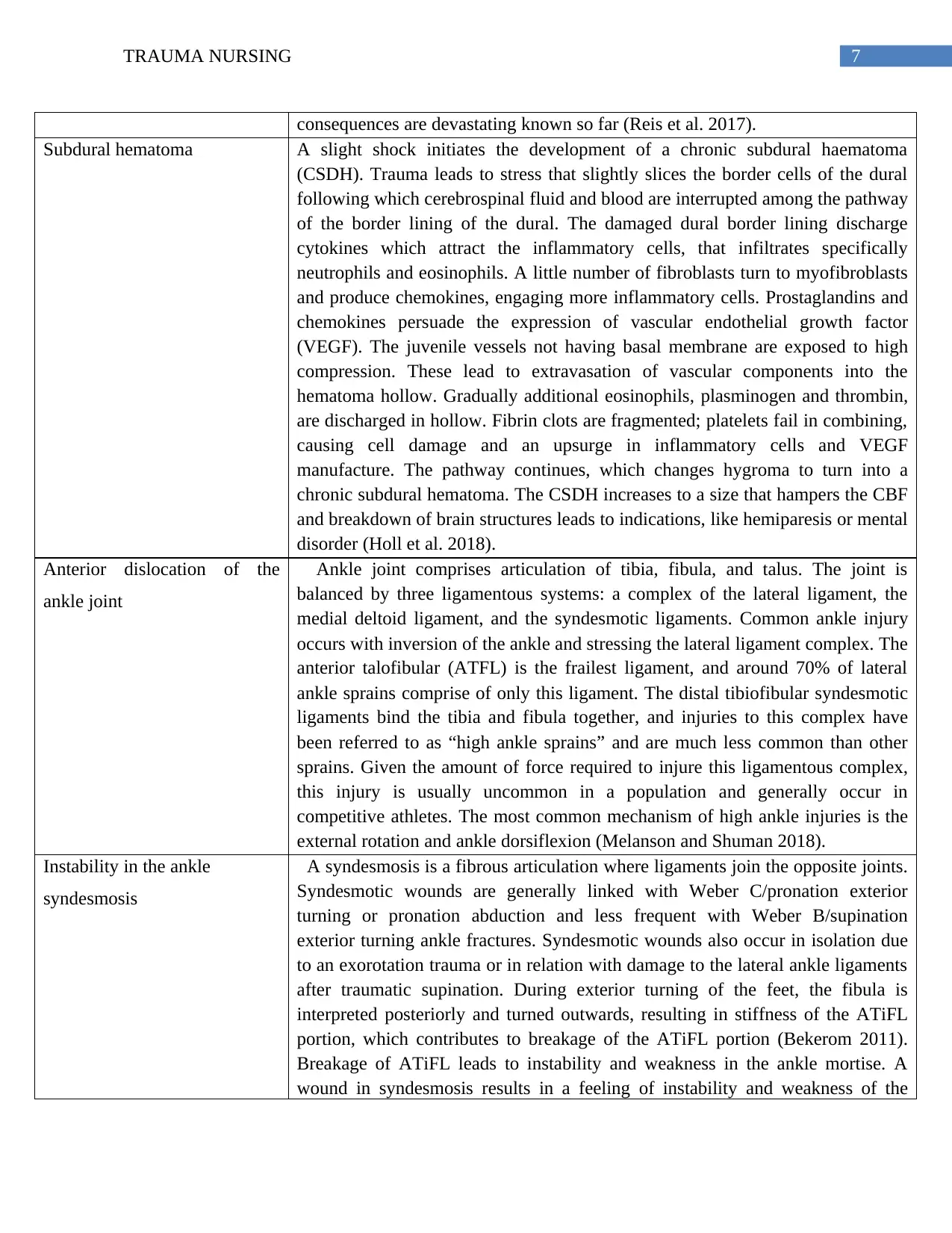
Management
Subarachnoid hemorrhage (SAH)
Management Complications
There are various methods through which the (SAH) can
be managed, including open surgery or endovascular
treatment.
Open surgery Techniques includes clipping and
vessel bypass.
Endovascular surgery includes coiling and
stenting or flow diversion (Cleveland Clinic,
2018).
There are certain complications from subarachnoid
haemorrhage after the treatment of brain aneurysm.
Like,
There can be brain swelling and hydrocephalus.
Sometimes a patient can also have a seizure due
to the sudden increase in brain pressure.
Sometimes patients require External ventricular
drain (EVD) for temporary till the brain resumes
the normal flow and absorption of CSF
(Cleveland Clinic, 2018).
Subdural hematoma
Management Complication
To treat subdural hematoma, a surgical process
called craniotomy can be used. In this process,
the surgical team through incision brings out a
part of the skull in to access the hematoma. Later
through the use of suction and irrigation, the
hematoma is removed.
Another method is through the utilization of a
small hole which drains all chronic and acute
subdural hematomas that are smaller than one
The complications relating to the subdural hematoma
can arise just after the injury or can also occur after
post-surgery (Iorio et al. 2018). The complications can
vary –
Brain herniation, which puts pressure on the
brain and can cause a coma or death.
Seizures or shock due to brain pressure.
Brain muscle weakness or numbness.
ankle. Also, tenderness of ATiFL and swelling of the syndesmosis causes a high
sprain type symptom (Wagener, Beumer and Swierstra 2011).
Management
Subarachnoid hemorrhage (SAH)
Management Complications
There are various methods through which the (SAH) can
be managed, including open surgery or endovascular
treatment.
Open surgery Techniques includes clipping and
vessel bypass.
Endovascular surgery includes coiling and
stenting or flow diversion (Cleveland Clinic,
2018).
There are certain complications from subarachnoid
haemorrhage after the treatment of brain aneurysm.
Like,
There can be brain swelling and hydrocephalus.
Sometimes a patient can also have a seizure due
to the sudden increase in brain pressure.
Sometimes patients require External ventricular
drain (EVD) for temporary till the brain resumes
the normal flow and absorption of CSF
(Cleveland Clinic, 2018).
Subdural hematoma
Management Complication
To treat subdural hematoma, a surgical process
called craniotomy can be used. In this process,
the surgical team through incision brings out a
part of the skull in to access the hematoma. Later
through the use of suction and irrigation, the
hematoma is removed.
Another method is through the utilization of a
small hole which drains all chronic and acute
subdural hematomas that are smaller than one
The complications relating to the subdural hematoma
can arise just after the injury or can also occur after
post-surgery (Iorio et al. 2018). The complications can
vary –
Brain herniation, which puts pressure on the
brain and can cause a coma or death.
Seizures or shock due to brain pressure.
Brain muscle weakness or numbness.
9TRAUMA NURSING
centimetre at the thickest point (Iorio et al.
2018).
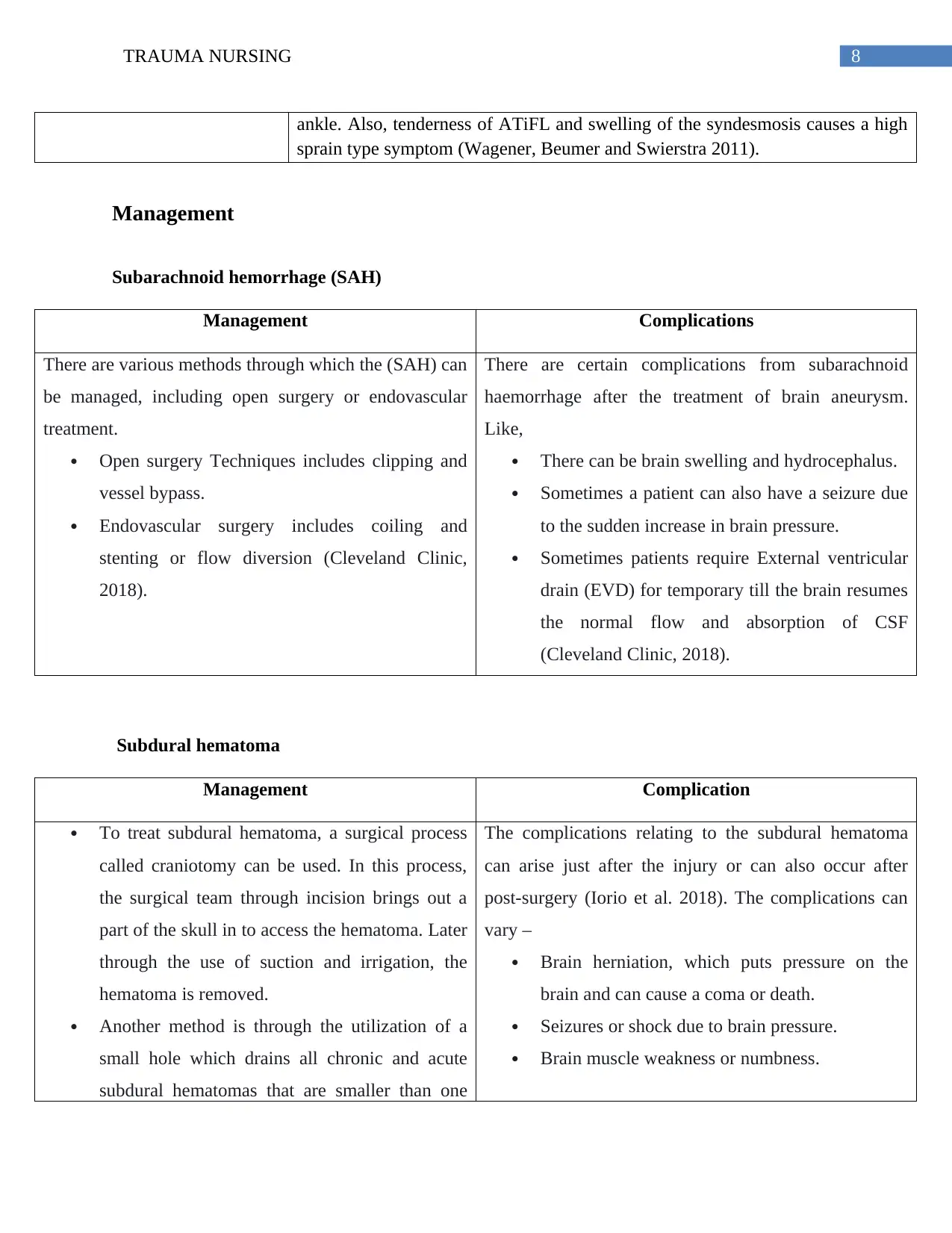
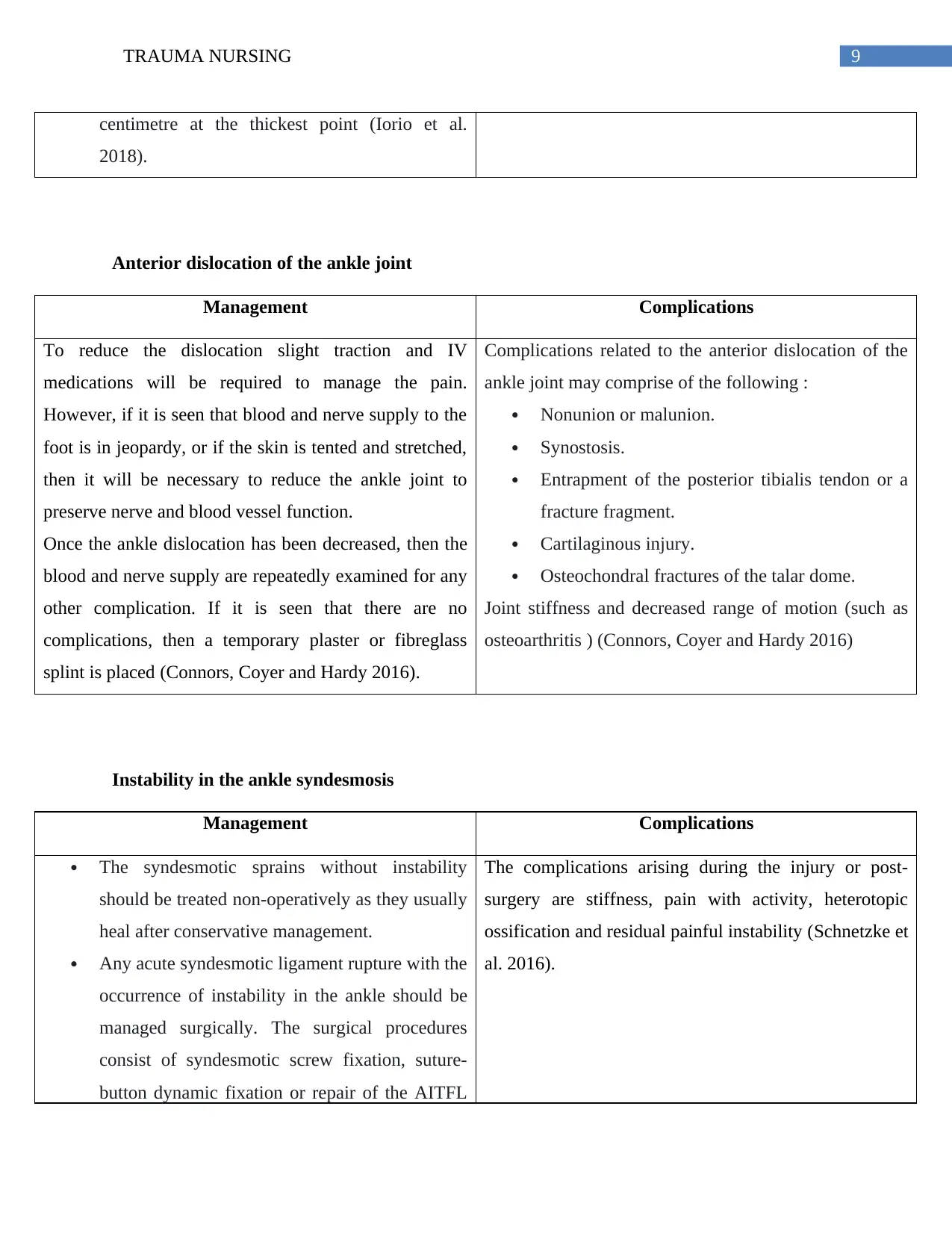
Anterior dislocation of the ankle joint
Management Complications
To reduce the dislocation slight traction and IV
medications will be required to manage the pain.
However, if it is seen that blood and nerve supply to the
foot is in jeopardy, or if the skin is tented and stretched,
then it will be necessary to reduce the ankle joint to
preserve nerve and blood vessel function.
Once the ankle dislocation has been decreased, then the
blood and nerve supply are repeatedly examined for any
other complication. If it is seen that there are no
complications, then a temporary plaster or fibreglass
splint is placed (Connors, Coyer and Hardy 2016).
Complications related to the anterior dislocation of the
ankle joint may comprise of the following :
Nonunion or malunion.
Synostosis.
Entrapment of the posterior tibialis tendon or a
fracture fragment.
Cartilaginous injury.
Osteochondral fractures of the talar dome.
Joint stiffness and decreased range of motion (such as
osteoarthritis ) (Connors, Coyer and Hardy 2016)
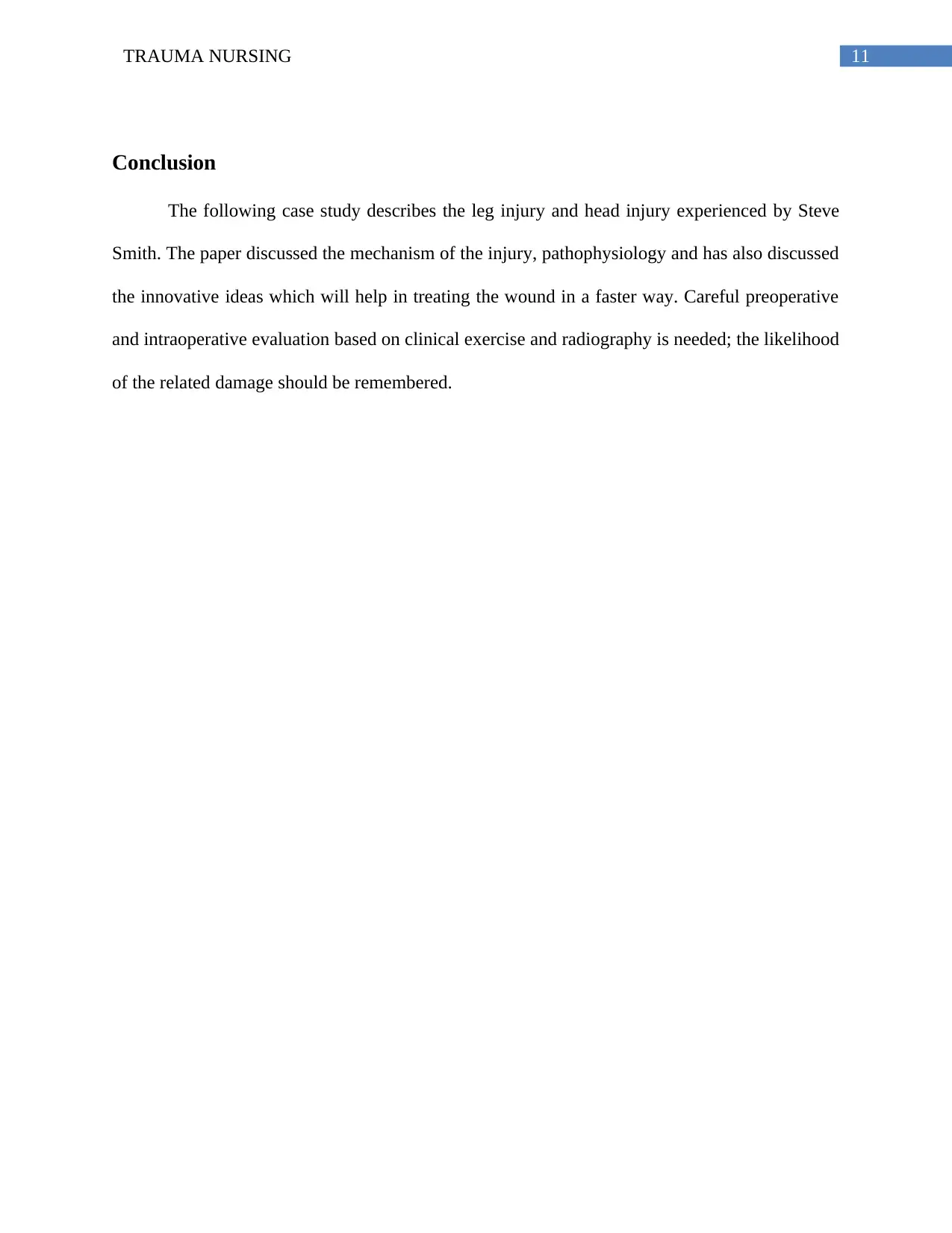
Instability in the ankle syndesmosis
Management Complications
The syndesmotic sprains without instability
should be treated non-operatively as they usually
heal after conservative management.
Any acute syndesmotic ligament rupture with the
occurrence of instability in the ankle should be
managed surgically. The surgical procedures
consist of syndesmotic screw fixation, suture-
button dynamic fixation or repair of the AITFL
The complications arising during the injury or post-
surgery are stiffness, pain with activity, heterotopic
ossification and residual painful instability (Schnetzke et
al. 2016).
centimetre at the thickest point (Iorio et al.
2018).
Anterior dislocation of the ankle joint
Management Complications
To reduce the dislocation slight traction and IV
medications will be required to manage the pain.
However, if it is seen that blood and nerve supply to the
foot is in jeopardy, or if the skin is tented and stretched,
then it will be necessary to reduce the ankle joint to
preserve nerve and blood vessel function.
Once the ankle dislocation has been decreased, then the
blood and nerve supply are repeatedly examined for any
other complication. If it is seen that there are no
complications, then a temporary plaster or fibreglass
splint is placed (Connors, Coyer and Hardy 2016).
Complications related to the anterior dislocation of the
ankle joint may comprise of the following :
Nonunion or malunion.
Synostosis.
Entrapment of the posterior tibialis tendon or a
fracture fragment.
Cartilaginous injury.
Osteochondral fractures of the talar dome.
Joint stiffness and decreased range of motion (such as
osteoarthritis ) (Connors, Coyer and Hardy 2016)
Instability in the ankle syndesmosis
Management Complications
The syndesmotic sprains without instability
should be treated non-operatively as they usually
heal after conservative management.
Any acute syndesmotic ligament rupture with the
occurrence of instability in the ankle should be
managed surgically. The surgical procedures
consist of syndesmotic screw fixation, suture-
button dynamic fixation or repair of the AITFL
The complications arising during the injury or post-
surgery are stiffness, pain with activity, heterotopic
ossification and residual painful instability (Schnetzke et
al. 2016).
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.

10TRAUMA NURSING
with direct sutures, suture anchors or screws
with washers. These surgical operations help in
reducing and maintaining the structures in the
correct position so that the ligaments can heal
properly (Heras et al. 2017).
Futuristic Considerations
Wound healing is generally referred as tissue repair which starts with the formation of a
clot, and successively degranulation of the platelets which releases platelet growth factors which
are the basic necessity for the well-regulated procedures for wound healing. During this case
study, we neglected to analyze the infections at the site of the wound. Even though the surgeons
treated the internal wounds, there was negligence in the evaluation of the infections at the wound
site. Infections can cause side effects, such as the formation of pus at the inner membrane that
can infect the blood and also increase pain for the patient, making his health condition severe.
According to some researchers at the University of Cincinnati, the blood of a person contains a
topical gel that helps in the prevention of the infection at the wound site and also helps in
increasing the healing process. In the distant future, an individual’s blood can be used to dress
wounds, specifically patients who have been diagnosed with diabetes or any other disease that
can slow the healing process (Chu 2019).
with direct sutures, suture anchors or screws
with washers. These surgical operations help in
reducing and maintaining the structures in the
correct position so that the ligaments can heal
properly (Heras et al. 2017).
Futuristic Considerations
Wound healing is generally referred as tissue repair which starts with the formation of a
clot, and successively degranulation of the platelets which releases platelet growth factors which
are the basic necessity for the well-regulated procedures for wound healing. During this case
study, we neglected to analyze the infections at the site of the wound. Even though the surgeons
treated the internal wounds, there was negligence in the evaluation of the infections at the wound
site. Infections can cause side effects, such as the formation of pus at the inner membrane that
can infect the blood and also increase pain for the patient, making his health condition severe.
According to some researchers at the University of Cincinnati, the blood of a person contains a
topical gel that helps in the prevention of the infection at the wound site and also helps in
increasing the healing process. In the distant future, an individual’s blood can be used to dress
wounds, specifically patients who have been diagnosed with diabetes or any other disease that
can slow the healing process (Chu 2019).
11TRAUMA NURSING
Conclusion
The following case study describes the leg injury and head injury experienced by Steve
Smith. The paper discussed the mechanism of the injury, pathophysiology and has also discussed
the innovative ideas which will help in treating the wound in a faster way. Careful preoperative
and intraoperative evaluation based on clinical exercise and radiography is needed; the likelihood
of the related damage should be remembered.
Conclusion
The following case study describes the leg injury and head injury experienced by Steve
Smith. The paper discussed the mechanism of the injury, pathophysiology and has also discussed
the innovative ideas which will help in treating the wound in a faster way. Careful preoperative
and intraoperative evaluation based on clinical exercise and radiography is needed; the likelihood
of the related damage should be remembered.
12TRAUMA NURSING
Reference
Cleveland Clinic. (2018). Subarachnoid Hemorrhage (SAH) Management and Treatment.
[online] Available at: https://my.clevelandclinic.org/health/diseases/17871-subarachnoid-
hemorrhage-sah/management-and-treatment [Accessed 13 Sep. 2019].
Connors, J.C., Coyer, M.A. and Hardy, M.A., 2016. Irreducible ankle fracture dislocation due to
tibialis posterior tendon interposition: a case report. The Journal of Foot and Ankle
Surgery, 55(6), pp.1276-1281.
Crespo, A.M. and Tejwani, N.C., 2019. Radial Head and Neck Fractures: Open Reduction and
Internal Fixation. In Fractures of the Elbow (pp. 133-140). Springer, Cham.
de-las-Heras Romero, J., Alvarez, A.M.L., Sanchez, F.M., Garcia, A.P., Porcel, P.A.G., Sarabia,
R.V. and Torralba, M.H., 2017. Management of syndesmotic injuries of the ankle. EFORT open
reviews, 2(9), pp.403-409.
Greenberg, K., Binning, M.J. and Veznedaroglu, E., 2018. Severe Headache and Diagnosis of
Subarachnoid Hemorrhage in the Emergency Department. In Intracranial Aneurysms (pp. 99-
113). Academic Press.
Großterlinden, L.G., Hartel, M., Yamamura, J., Schoennagel, B., Bürger, N., Krause, M., Spiro,
A., Hoffmann, M., Lehmann, W., Rueger, J.M. and Rupprecht, M., 2016. Isolated syndesmotic
injuries in acute ankle sprains: diagnostic significance of clinical examination and MRI. Knee
Surgery, Sports Traumatology, Arthroscopy, 24(4), pp.1180-1186.
Reference
Cleveland Clinic. (2018). Subarachnoid Hemorrhage (SAH) Management and Treatment.
[online] Available at: https://my.clevelandclinic.org/health/diseases/17871-subarachnoid-
hemorrhage-sah/management-and-treatment [Accessed 13 Sep. 2019].
Connors, J.C., Coyer, M.A. and Hardy, M.A., 2016. Irreducible ankle fracture dislocation due to
tibialis posterior tendon interposition: a case report. The Journal of Foot and Ankle
Surgery, 55(6), pp.1276-1281.
Crespo, A.M. and Tejwani, N.C., 2019. Radial Head and Neck Fractures: Open Reduction and
Internal Fixation. In Fractures of the Elbow (pp. 133-140). Springer, Cham.
de-las-Heras Romero, J., Alvarez, A.M.L., Sanchez, F.M., Garcia, A.P., Porcel, P.A.G., Sarabia,
R.V. and Torralba, M.H., 2017. Management of syndesmotic injuries of the ankle. EFORT open
reviews, 2(9), pp.403-409.
Greenberg, K., Binning, M.J. and Veznedaroglu, E., 2018. Severe Headache and Diagnosis of
Subarachnoid Hemorrhage in the Emergency Department. In Intracranial Aneurysms (pp. 99-
113). Academic Press.
Großterlinden, L.G., Hartel, M., Yamamura, J., Schoennagel, B., Bürger, N., Krause, M., Spiro,
A., Hoffmann, M., Lehmann, W., Rueger, J.M. and Rupprecht, M., 2016. Isolated syndesmotic
injuries in acute ankle sprains: diagnostic significance of clinical examination and MRI. Knee
Surgery, Sports Traumatology, Arthroscopy, 24(4), pp.1180-1186.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13TRAUMA NURSING
Holl, D.C., Volovici, V., Dirven, C.M., Peul, W.C., van Kooten, F., Jellema, K., van der Gaag,
N.A., Miah, I.P., Kho, K.H., den Hertog, H.M. and Lingsma, H.F., 2018. Pathophysiology and
nonsurgical treatment of chronic subdural hematoma: from past to present to future. World
neurosurgery, 116, pp.402-411.
Iorio-Morin, C., Touchette, C., Lévesque, M., Effendi, K., Fortin, D. and Mathieu, D., 2018.
Chronic subdural hematoma: toward a new management paradigm for an increasingly complex
population. Journal of neurotrauma, 35(16), pp.1882-1885.
Iorio-Morin, C., Touchette, C., Lévesque, M., Effendi, K., Fortin, D. and Mathieu, D., 2018.
Chronic subdural hematoma: toward a new management paradigm for an increasingly complex
population. Journal of neurotrauma, 35(16), pp.1882-1885.
Karampinas, P.K., Stathopoulos, I.P., Vlamis, J., Polyzois, V.D. and Pneumatikos, S.G., 2012.
Conservative treatment of an anterior-lateral ankle dislocation without an associated fracture in a
diabetic patient: a case report. Diabetic foot & ankle, 3(1), p.18411.
Melanson, S.W. and Shuman, V.L., 2018. Acute Ankle Sprain. In StatPearls [Internet].
StatPearls Publishing.
Reis, C., Ho, W.M., Akyol, O., Chen, S., Applegate II, R. and Zhang, J., 2017. Pathophysiology
of Subarachnoid Hemorrhage, Early Brain Injury, and Delayed Cerebral Ischemia. In Primer on
Cerebrovascular Diseases (pp. 125-130). Academic Press.
Schnetzke, M., Vetter, S.Y., Beisemann, N., Swartman, B., Grützner, P.A. and Franke, J., 2016.
Management of syndesmotic injuries: What is the evidence?. World journal of
orthopedics, 7(11), p.718.
Holl, D.C., Volovici, V., Dirven, C.M., Peul, W.C., van Kooten, F., Jellema, K., van der Gaag,
N.A., Miah, I.P., Kho, K.H., den Hertog, H.M. and Lingsma, H.F., 2018. Pathophysiology and
nonsurgical treatment of chronic subdural hematoma: from past to present to future. World
neurosurgery, 116, pp.402-411.
Iorio-Morin, C., Touchette, C., Lévesque, M., Effendi, K., Fortin, D. and Mathieu, D., 2018.
Chronic subdural hematoma: toward a new management paradigm for an increasingly complex
population. Journal of neurotrauma, 35(16), pp.1882-1885.
Iorio-Morin, C., Touchette, C., Lévesque, M., Effendi, K., Fortin, D. and Mathieu, D., 2018.
Chronic subdural hematoma: toward a new management paradigm for an increasingly complex
population. Journal of neurotrauma, 35(16), pp.1882-1885.
Karampinas, P.K., Stathopoulos, I.P., Vlamis, J., Polyzois, V.D. and Pneumatikos, S.G., 2012.
Conservative treatment of an anterior-lateral ankle dislocation without an associated fracture in a
diabetic patient: a case report. Diabetic foot & ankle, 3(1), p.18411.
Melanson, S.W. and Shuman, V.L., 2018. Acute Ankle Sprain. In StatPearls [Internet].
StatPearls Publishing.
Reis, C., Ho, W.M., Akyol, O., Chen, S., Applegate II, R. and Zhang, J., 2017. Pathophysiology
of Subarachnoid Hemorrhage, Early Brain Injury, and Delayed Cerebral Ischemia. In Primer on
Cerebrovascular Diseases (pp. 125-130). Academic Press.
Schnetzke, M., Vetter, S.Y., Beisemann, N., Swartman, B., Grützner, P.A. and Franke, J., 2016.
Management of syndesmotic injuries: What is the evidence?. World journal of
orthopedics, 7(11), p.718.
14TRAUMA NURSING
Shore, B.J. and Kramer, D.E., 2016. Management of syndesmotic ankle injuries in children and
adolescents. Journal of Pediatric Orthopaedics, 36, pp.S11-S14.
van den Bekerom, M.P., 2011. Diagnosing syndesmotic instability in ankle fractures. World
journal of orthopedics, 2(7), p.51.
van Dijk, C.N., Longo, U.G., Loppini, M., Florio, P., Maltese, L., Ciuffreda, M. and Denaro, V.,
2016. Conservative and surgical management of acute isolated syndesmotic injuries: ESSKA-
AFAS consensus and guidelines. Knee Surgery, Sports Traumatology, Arthroscopy, 24(4),
pp.1217-1227.
Wagener, M.L., Beumer, A. and Swierstra, B.A., 2011. Chronic instability of the anterior
tibiofibular syndesmosis of the ankle. Arthroscopic findings and results of anatomical
reconstruction. BMC musculoskeletal disorders, 12(1), p.212.
Wight, L., Owen, D., Goldbloom, D. and Knupp, M., 2017. Pure ankle dislocation: a systematic
review of the literature and estimation of incidence. Injury, 48(10), pp.2027-2034.
Yadav, Y.R., Parihar, V., Namdev, H. and Bajaj, J., 2016. Chronic subdural hematoma. Asian
journal of neurosurgery, 11(4), p.330.
Zamboni, C., Campos, F.A.G.D., Foni, N.O., Souza, R.C., Christian, R.W. and Mercadante,
M.T., 2016. Tibial shaft fracture and ankle injury-Case report. Revista Brasileira de
Ortopedia, 51(5), pp.597-600.
Chu, J. (2019). How to Heal Wounds Faster. [online] MIT Technology Review. Available at:
https://www.technologyreview.com/s/407975/how-to-heal-wounds-faster/ [Accessed 14 Sep.
2019].
Shore, B.J. and Kramer, D.E., 2016. Management of syndesmotic ankle injuries in children and
adolescents. Journal of Pediatric Orthopaedics, 36, pp.S11-S14.
van den Bekerom, M.P., 2011. Diagnosing syndesmotic instability in ankle fractures. World
journal of orthopedics, 2(7), p.51.
van Dijk, C.N., Longo, U.G., Loppini, M., Florio, P., Maltese, L., Ciuffreda, M. and Denaro, V.,
2016. Conservative and surgical management of acute isolated syndesmotic injuries: ESSKA-
AFAS consensus and guidelines. Knee Surgery, Sports Traumatology, Arthroscopy, 24(4),
pp.1217-1227.
Wagener, M.L., Beumer, A. and Swierstra, B.A., 2011. Chronic instability of the anterior
tibiofibular syndesmosis of the ankle. Arthroscopic findings and results of anatomical
reconstruction. BMC musculoskeletal disorders, 12(1), p.212.
Wight, L., Owen, D., Goldbloom, D. and Knupp, M., 2017. Pure ankle dislocation: a systematic
review of the literature and estimation of incidence. Injury, 48(10), pp.2027-2034.
Yadav, Y.R., Parihar, V., Namdev, H. and Bajaj, J., 2016. Chronic subdural hematoma. Asian
journal of neurosurgery, 11(4), p.330.
Zamboni, C., Campos, F.A.G.D., Foni, N.O., Souza, R.C., Christian, R.W. and Mercadante,
M.T., 2016. Tibial shaft fracture and ankle injury-Case report. Revista Brasileira de
Ortopedia, 51(5), pp.597-600.
Chu, J. (2019). How to Heal Wounds Faster. [online] MIT Technology Review. Available at:
https://www.technologyreview.com/s/407975/how-to-heal-wounds-faster/ [Accessed 14 Sep.
2019].
1 out of 15
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





