Bone Mineral Density, Status of Vitamin D and Intake of Calcium for Ileostomy Patient Analysis
VerifiedAdded on 2023/04/21
|10
|3696
|467
AI Summary
This study aims to determine the status of vitamin D, dietary intake of calcium, and bone mineral density for patients who have undergone ileostomy. The study will include participants within the age group of 18 to 70 years who have undergone ileostomy for 2+ years. Data will be collected from part of the C-TRIC and Ulster University study. The value of this research lies in its enhancement of future evidence-based clinical practice for health professionals.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Ulster University School of Biomedical Sciences
MSc RESEARCH PROPOSAL
(NUT814: Research Methods & Biostatistics for Nutritional Sciences)
Proposal Application Form
3. PROJECT DETAILS
Bone Mineral Density, Status of Vitamin D and Intake of Calcium for
Ileostomy Patient Analysis
Scientific abstract(maximum 250 words)
The surgical procedure of ileostomy, involving extensionfromthe small intestine to the skin surface, is
done on patients who are suffering from familial adenomatous polyposis or ulcerative colitis. The aim of
this study is to determine the status of vitamin D, dietary intake of calcium and bone mineral density for
patients who have undergone an ileostomy.Patients within the age group of 18 to 70 years, being male or
female, but not pregnant, who have underwent ileostomy for 2+ years for any reason will be included as
participants for this study. Prior to the commencement of the study, informed consent will be obtained
from the subjects. The decision of voluntary participation in the study, will not affect the quality of clinical
care provided to the subjects. Data will be collected from part of the C-TRIC and ulster university study
followed by data assessment. Ileostomy assessment will include screening tests of vitamin D status, dietary
calcium intake andbone mineral density. The patients will be required to questionnaires.There is a lack of
scientific evidence concerning the evaluation of the status of vitamin D, dietary intake of calcium and bone
mineral densityfor patients who have undergone ileostomy. The value of this research lies in its
enhancement of future evidence based clinical practice for health professionals concerning the
determination of vitamin D status, dietary intake of calcium and bone mineral density of patients who
have undergone ileostomy.
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
Office use only
:
MSc RESEARCH PROPOSAL
(NUT814: Research Methods & Biostatistics for Nutritional Sciences)
Proposal Application Form
3. PROJECT DETAILS
Bone Mineral Density, Status of Vitamin D and Intake of Calcium for
Ileostomy Patient Analysis
Scientific abstract(maximum 250 words)
The surgical procedure of ileostomy, involving extensionfromthe small intestine to the skin surface, is
done on patients who are suffering from familial adenomatous polyposis or ulcerative colitis. The aim of
this study is to determine the status of vitamin D, dietary intake of calcium and bone mineral density for
patients who have undergone an ileostomy.Patients within the age group of 18 to 70 years, being male or
female, but not pregnant, who have underwent ileostomy for 2+ years for any reason will be included as
participants for this study. Prior to the commencement of the study, informed consent will be obtained
from the subjects. The decision of voluntary participation in the study, will not affect the quality of clinical
care provided to the subjects. Data will be collected from part of the C-TRIC and ulster university study
followed by data assessment. Ileostomy assessment will include screening tests of vitamin D status, dietary
calcium intake andbone mineral density. The patients will be required to questionnaires.There is a lack of
scientific evidence concerning the evaluation of the status of vitamin D, dietary intake of calcium and bone
mineral densityfor patients who have undergone ileostomy. The value of this research lies in its
enhancement of future evidence based clinical practice for health professionals concerning the
determination of vitamin D status, dietary intake of calcium and bone mineral density of patients who
have undergone ileostomy.
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
Office use only
:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Ulster University School of Biomedical Sciences
Abstract word count = 250
Lay summary (maximum 150 words)
Describe your proposed research in a way that will be clear to members the public who do not
have a grasp of medical or scientific terminology
A total of 120, 000 patients in the United States and 13, 000 patients in United Kingdom undergo stoma
creation surgery every year with an estimated annual increase of three percent (3%). Poor state of Vitamin
D in the human body, increases one’s chances of acquiring reduced bone strength, increased joint stiffness
and greater susceptibility of fractures resulting from falls. (Broeet al.2016).
Hence, this researchaims at undertaking analysis which will determine the status of vitamin D and the
intake of calcium for a patient who has undergone ileostomy. The research will evaluate the presence of an
association between the implantation of an artificial pouch and the status of vitamin D, absorption of
calcium and bone mineral densities in such patients. In some patients, vitamin intake tends to alter due to
alteration in their diet, hence increasing their risk of nutritional deficiencies.
Lay summary word count = 144
4. PROPOSED INVESTIGATION
To include background, hypothesis, project aims, proposed methods (including statistical
approaches and power calculation),aproject timeline (e.g. Gantt chart) and references.Expand
this section as necessary to include all required information. Take note of individual word
counts specified throughout.
Background (maximum 750words)
Inflammatory bowel disease (IBD) is divided into 2 major disease entities: Crohn's disease and ulcerative
colitis. Studies have reported that 60% of patients with Crohn's disease and 15%–30% of patients with
ulcerative colitis require surgical intervention for the management of their disease (Peyrin-Biroulet 2004,
Targownik 2012).
It was uncovered that a 29% ofUnited States patients suffered from low bone mineral density, especially
those who had the ileostomy and inflammatory bowel disease for more than five years. Some of the
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
Abstract word count = 250
Lay summary (maximum 150 words)
Describe your proposed research in a way that will be clear to members the public who do not
have a grasp of medical or scientific terminology
A total of 120, 000 patients in the United States and 13, 000 patients in United Kingdom undergo stoma
creation surgery every year with an estimated annual increase of three percent (3%). Poor state of Vitamin
D in the human body, increases one’s chances of acquiring reduced bone strength, increased joint stiffness
and greater susceptibility of fractures resulting from falls. (Broeet al.2016).
Hence, this researchaims at undertaking analysis which will determine the status of vitamin D and the
intake of calcium for a patient who has undergone ileostomy. The research will evaluate the presence of an
association between the implantation of an artificial pouch and the status of vitamin D, absorption of
calcium and bone mineral densities in such patients. In some patients, vitamin intake tends to alter due to
alteration in their diet, hence increasing their risk of nutritional deficiencies.
Lay summary word count = 144
4. PROPOSED INVESTIGATION
To include background, hypothesis, project aims, proposed methods (including statistical
approaches and power calculation),aproject timeline (e.g. Gantt chart) and references.Expand
this section as necessary to include all required information. Take note of individual word
counts specified throughout.
Background (maximum 750words)
Inflammatory bowel disease (IBD) is divided into 2 major disease entities: Crohn's disease and ulcerative
colitis. Studies have reported that 60% of patients with Crohn's disease and 15%–30% of patients with
ulcerative colitis require surgical intervention for the management of their disease (Peyrin-Biroulet 2004,
Targownik 2012).
It was uncovered that a 29% ofUnited States patients suffered from low bone mineral density, especially
those who had the ileostomy and inflammatory bowel disease for more than five years. Some of the
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
Ulster University School of Biomedical Sciences
risksthat patient with ileostomy and inflammatory bowel disease have , in addition to low bone mineral
density include malnutrition, malabsorption, and inflations further increasing the susceptibility of
additional severe bowel associated disorders. The above factors further lead to reduced absorption of the
vitamins (D & B) and other nutrients, which results in serious nutritional associated health complications
such as low lean body mass and low BMI. According to the study by Broeet al. 2016), It was reported that
patient who were suffering from a prolonged status of inflammatory bowel disease and had underwent
ileostomy surgery to attach the pouch suffered from low levels of Vitamin D.Gupta and colleagues (2014)
recently highlighted a 29.4% prevalence of low bone mineral density (BMD) in a cohort of US patients
with IBD and ileostomy who were >5 years postoperative. Possible risk factors for bone loss in patients
with IBD and ileostomy are considered to include malabsorption secondary to bowel resection,
malnutrition and more aggressive disease and inflammation which led to bowel resection in the first place
(Gupta 2013). These factors also contribute to reduced intestinal absorption of nutrients and vitamins
including B & D (Vavricka et al. 2012) subsequently leading to potential health complications including
low BMI and low lean body mass (Ng et al. 2013). Although the study by Gupta and colleagues did not
assess vitamin D status directly, it has been reported that IBD patients who have surgical intervention to
create ileal pouches also have low levels of vitamin D (Khanna et al. 2013).
The two main forms of vitamin D are vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Vitamin
D from plant sources is in the form of vitamin D2 and that from animal sources is vitamin D3. Vitamin D3
is also produced in the human skin by 7-dehydroxycholesterol after absorption of ultraviolet B light from
the sun (Borel, Caillaud and Cano 2015).Vitamin D from dietary sources is incorporated into chylomicrons
and absorbed mostly from the proximal small bowel, and transported via the gut lymphatics into the
venous circulation after being bound to vitamin D binding protein, an alpha-globulin produced in the liver
(Christakos et al. 2015).Vitamin D is then hydroxylated in the liver by cytochrome P450-like enzymes to
form 25-hydroxyvitamin D [25(OH)D], which is the major circulating and storage form of vitamin D.
Further hydroxylation of vitamin D to form 1,25-dihydroxyvitamin D [1,25(OH)2D] occurs mainly in the
kidney. This last step in the kidney is stimulated by parathyroid hormone (PTH), whereas calcium and
1,25(OH)2D itself inhibits it (Goncalves et al. 2015).Calcium absorption via the intestine occurs via active
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
risksthat patient with ileostomy and inflammatory bowel disease have , in addition to low bone mineral
density include malnutrition, malabsorption, and inflations further increasing the susceptibility of
additional severe bowel associated disorders. The above factors further lead to reduced absorption of the
vitamins (D & B) and other nutrients, which results in serious nutritional associated health complications
such as low lean body mass and low BMI. According to the study by Broeet al. 2016), It was reported that
patient who were suffering from a prolonged status of inflammatory bowel disease and had underwent
ileostomy surgery to attach the pouch suffered from low levels of Vitamin D.Gupta and colleagues (2014)
recently highlighted a 29.4% prevalence of low bone mineral density (BMD) in a cohort of US patients
with IBD and ileostomy who were >5 years postoperative. Possible risk factors for bone loss in patients
with IBD and ileostomy are considered to include malabsorption secondary to bowel resection,
malnutrition and more aggressive disease and inflammation which led to bowel resection in the first place
(Gupta 2013). These factors also contribute to reduced intestinal absorption of nutrients and vitamins
including B & D (Vavricka et al. 2012) subsequently leading to potential health complications including
low BMI and low lean body mass (Ng et al. 2013). Although the study by Gupta and colleagues did not
assess vitamin D status directly, it has been reported that IBD patients who have surgical intervention to
create ileal pouches also have low levels of vitamin D (Khanna et al. 2013).
The two main forms of vitamin D are vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Vitamin
D from plant sources is in the form of vitamin D2 and that from animal sources is vitamin D3. Vitamin D3
is also produced in the human skin by 7-dehydroxycholesterol after absorption of ultraviolet B light from
the sun (Borel, Caillaud and Cano 2015).Vitamin D from dietary sources is incorporated into chylomicrons
and absorbed mostly from the proximal small bowel, and transported via the gut lymphatics into the
venous circulation after being bound to vitamin D binding protein, an alpha-globulin produced in the liver
(Christakos et al. 2015).Vitamin D is then hydroxylated in the liver by cytochrome P450-like enzymes to
form 25-hydroxyvitamin D [25(OH)D], which is the major circulating and storage form of vitamin D.
Further hydroxylation of vitamin D to form 1,25-dihydroxyvitamin D [1,25(OH)2D] occurs mainly in the
kidney. This last step in the kidney is stimulated by parathyroid hormone (PTH), whereas calcium and
1,25(OH)2D itself inhibits it (Goncalves et al. 2015).Calcium absorption via the intestine occurs via active
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
Ulster University School of Biomedical Sciences
(transcellular) and passive (paracellular) processes. Active absorption, which is the main mechanism, is
controlled by 1,25(OH)2D. Active calcium absorption also occurs mainly in the proximal small bowel;
however some calcium absorption occurs in other segments of the small bowel. Optimal calcium
absorption requires the presence of gastric acid(Schafer et al. 2015).
Surgical procedures such as an ileostomy alter the normal anatomy and physiology of the small intestine.
Bile acid (BA) malabsorption which is common to IBD is caused by impaired conjugated BA reabsorption
and a consequence, numerous pathological sequelae may occur, including the malfunction of lipid
digestion (Vitek 2015). Further, bacterial overgrowth can lead to deconjugation of bile salts, leading to
formation of free bile acids, again inducing dietary fat malabsorption, which in turn can lead to vitamin D
deficiency (Naysmith et al. 1989; Natori et al. 1992, Salemans et al. 1993). As vitamin D is a fat-soluble
vitamin, malfunction of lipid digestion or absorption is problematic. Moreover as researched by Caviezel
et al. (2017), recent ex vivo studies in biopsies from IBD patients and healthy controls reported vitamin D
and its derivatives significantly decreased adhesion molecules and metalloproteinase, commonly up-
regulated in IBD patients. While the Vitamin D receptor (VDR) may play an important role in maintaining
gastrointestinal mucosal integrity, as VDR-knockout mice have been shown to develop severe colitis
(Martinessi et al. 2014).
Given the paucity of data in the area of ileostomy patients BMD, vitamin D status and calcium intake, we
will establish baseline observations within the Northern Ireland (NI) population.
Background word count = 745
Hypothesis(maximum 100 words)
Patients who have undergone ileostomy surgery have low status of vitamin D, reduced intake of dietary
calcium and decreased levels of bone mineral density in accordance to standard values.
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
(transcellular) and passive (paracellular) processes. Active absorption, which is the main mechanism, is
controlled by 1,25(OH)2D. Active calcium absorption also occurs mainly in the proximal small bowel;
however some calcium absorption occurs in other segments of the small bowel. Optimal calcium
absorption requires the presence of gastric acid(Schafer et al. 2015).
Surgical procedures such as an ileostomy alter the normal anatomy and physiology of the small intestine.
Bile acid (BA) malabsorption which is common to IBD is caused by impaired conjugated BA reabsorption
and a consequence, numerous pathological sequelae may occur, including the malfunction of lipid
digestion (Vitek 2015). Further, bacterial overgrowth can lead to deconjugation of bile salts, leading to
formation of free bile acids, again inducing dietary fat malabsorption, which in turn can lead to vitamin D
deficiency (Naysmith et al. 1989; Natori et al. 1992, Salemans et al. 1993). As vitamin D is a fat-soluble
vitamin, malfunction of lipid digestion or absorption is problematic. Moreover as researched by Caviezel
et al. (2017), recent ex vivo studies in biopsies from IBD patients and healthy controls reported vitamin D
and its derivatives significantly decreased adhesion molecules and metalloproteinase, commonly up-
regulated in IBD patients. While the Vitamin D receptor (VDR) may play an important role in maintaining
gastrointestinal mucosal integrity, as VDR-knockout mice have been shown to develop severe colitis
(Martinessi et al. 2014).
Given the paucity of data in the area of ileostomy patients BMD, vitamin D status and calcium intake, we
will establish baseline observations within the Northern Ireland (NI) population.
Background word count = 745
Hypothesis(maximum 100 words)
Patients who have undergone ileostomy surgery have low status of vitamin D, reduced intake of dietary
calcium and decreased levels of bone mineral density in accordance to standard values.
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Ulster University School of Biomedical Sciences
Hypothesis word count = 19
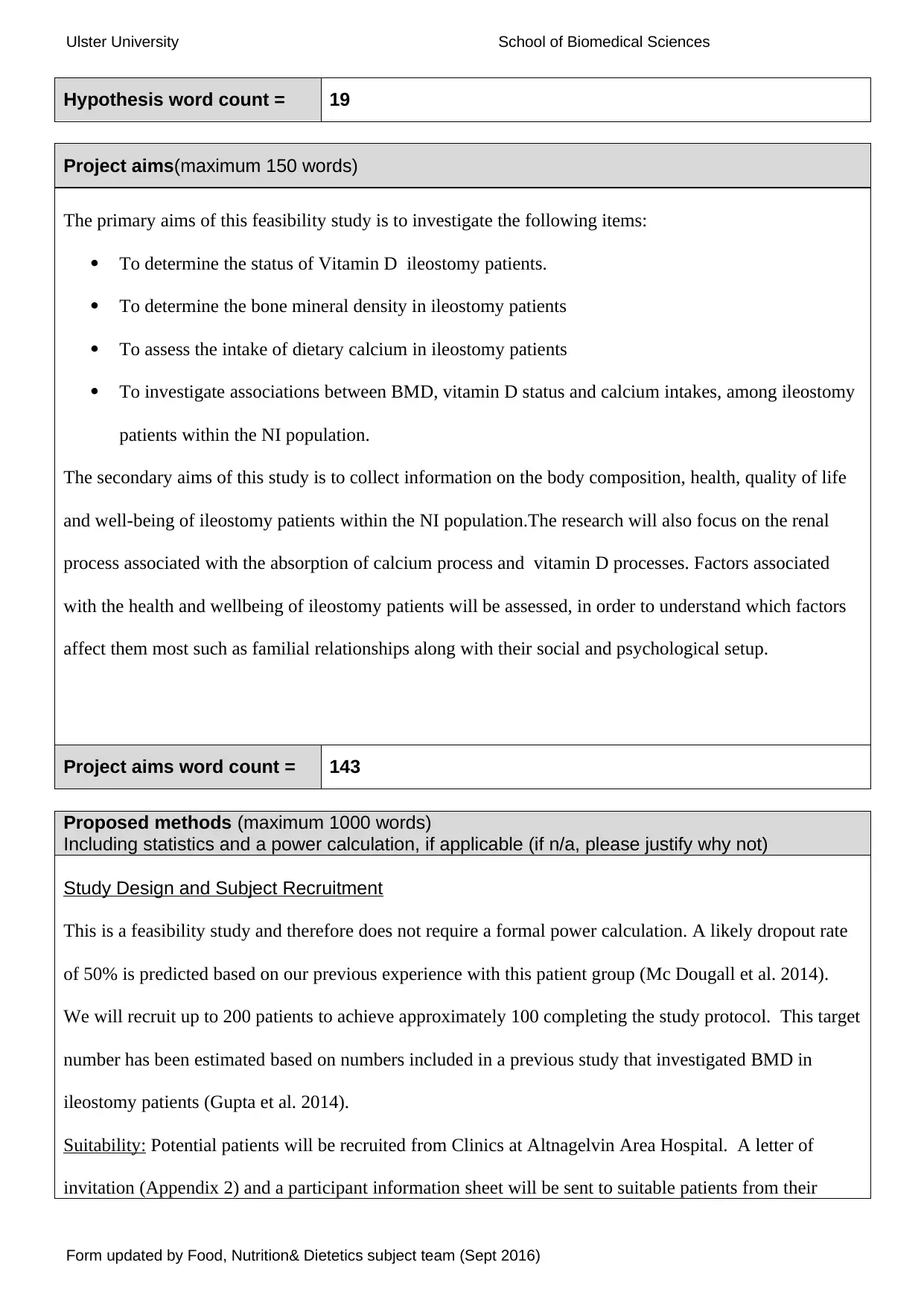
Project aims(maximum 150 words)
The primary aims of this feasibility study is to investigate the following items:
To determine the status of Vitamin D ileostomy patients.
To determine the bone mineral density in ileostomy patients
To assess the intake of dietary calcium in ileostomy patients
To investigate associations between BMD, vitamin D status and calcium intakes, among ileostomy
patients within the NI population.
The secondary aims of this study is to collect information on the body composition, health, quality of life
and well-being of ileostomy patients within the NI population.The research will also focus on the renal
process associated with the absorption of calcium process and vitamin D processes. Factors associated
with the health and wellbeing of ileostomy patients will be assessed, in order to understand which factors
affect them most such as familial relationships along with their social and psychological setup.
Project aims word count = 143
Proposed methods (maximum 1000 words)
Including statistics and a power calculation, if applicable (if n/a, please justify why not)
Study Design and Subject Recruitment
This is a feasibility study and therefore does not require a formal power calculation. A likely dropout rate
of 50% is predicted based on our previous experience with this patient group (Mc Dougall et al. 2014).
We will recruit up to 200 patients to achieve approximately 100 completing the study protocol. This target
number has been estimated based on numbers included in a previous study that investigated BMD in
ileostomy patients (Gupta et al. 2014).
Suitability: Potential patients will be recruited from Clinics at Altnagelvin Area Hospital. A letter of
invitation (Appendix 2) and a participant information sheet will be sent to suitable patients from their
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
Hypothesis word count = 19
Project aims(maximum 150 words)
The primary aims of this feasibility study is to investigate the following items:
To determine the status of Vitamin D ileostomy patients.
To determine the bone mineral density in ileostomy patients
To assess the intake of dietary calcium in ileostomy patients
To investigate associations between BMD, vitamin D status and calcium intakes, among ileostomy
patients within the NI population.
The secondary aims of this study is to collect information on the body composition, health, quality of life
and well-being of ileostomy patients within the NI population.The research will also focus on the renal
process associated with the absorption of calcium process and vitamin D processes. Factors associated
with the health and wellbeing of ileostomy patients will be assessed, in order to understand which factors
affect them most such as familial relationships along with their social and psychological setup.
Project aims word count = 143
Proposed methods (maximum 1000 words)
Including statistics and a power calculation, if applicable (if n/a, please justify why not)
Study Design and Subject Recruitment
This is a feasibility study and therefore does not require a formal power calculation. A likely dropout rate
of 50% is predicted based on our previous experience with this patient group (Mc Dougall et al. 2014).
We will recruit up to 200 patients to achieve approximately 100 completing the study protocol. This target
number has been estimated based on numbers included in a previous study that investigated BMD in
ileostomy patients (Gupta et al. 2014).
Suitability: Potential patients will be recruited from Clinics at Altnagelvin Area Hospital. A letter of
invitation (Appendix 2) and a participant information sheet will be sent to suitable patients from their
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
Ulster University School of Biomedical Sciences
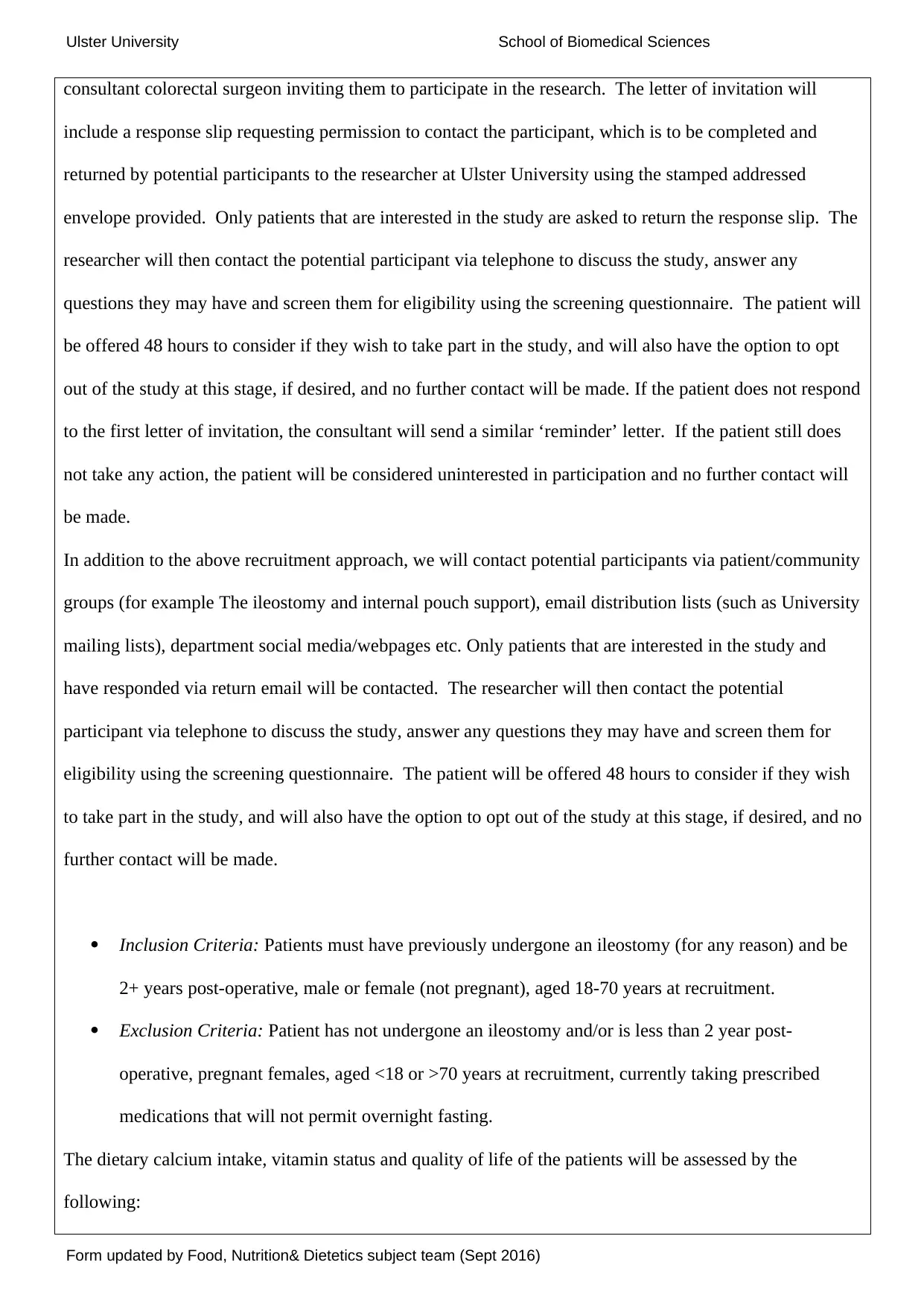
consultant colorectal surgeon inviting them to participate in the research. The letter of invitation will
include a response slip requesting permission to contact the participant, which is to be completed and
returned by potential participants to the researcher at Ulster University using the stamped addressed
envelope provided. Only patients that are interested in the study are asked to return the response slip. The
researcher will then contact the potential participant via telephone to discuss the study, answer any
questions they may have and screen them for eligibility using the screening questionnaire. The patient will
be offered 48 hours to consider if they wish to take part in the study, and will also have the option to opt
out of the study at this stage, if desired, and no further contact will be made. If the patient does not respond
to the first letter of invitation, the consultant will send a similar ‘reminder’ letter. If the patient still does
not take any action, the patient will be considered uninterested in participation and no further contact will
be made.
In addition to the above recruitment approach, we will contact potential participants via patient/community
groups (for example The ileostomy and internal pouch support), email distribution lists (such as University
mailing lists), department social media/webpages etc. Only patients that are interested in the study and
have responded via return email will be contacted. The researcher will then contact the potential
participant via telephone to discuss the study, answer any questions they may have and screen them for
eligibility using the screening questionnaire. The patient will be offered 48 hours to consider if they wish
to take part in the study, and will also have the option to opt out of the study at this stage, if desired, and no
further contact will be made.
Inclusion Criteria: Patients must have previously undergone an ileostomy (for any reason) and be
2+ years post-operative, male or female (not pregnant), aged 18-70 years at recruitment.
Exclusion Criteria: Patient has not undergone an ileostomy and/or is less than 2 year post-
operative, pregnant females, aged <18 or >70 years at recruitment, currently taking prescribed
medications that will not permit overnight fasting.
The dietary calcium intake, vitamin status and quality of life of the patients will be assessed by the
following:
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
consultant colorectal surgeon inviting them to participate in the research. The letter of invitation will
include a response slip requesting permission to contact the participant, which is to be completed and
returned by potential participants to the researcher at Ulster University using the stamped addressed
envelope provided. Only patients that are interested in the study are asked to return the response slip. The
researcher will then contact the potential participant via telephone to discuss the study, answer any
questions they may have and screen them for eligibility using the screening questionnaire. The patient will
be offered 48 hours to consider if they wish to take part in the study, and will also have the option to opt
out of the study at this stage, if desired, and no further contact will be made. If the patient does not respond
to the first letter of invitation, the consultant will send a similar ‘reminder’ letter. If the patient still does
not take any action, the patient will be considered uninterested in participation and no further contact will
be made.
In addition to the above recruitment approach, we will contact potential participants via patient/community
groups (for example The ileostomy and internal pouch support), email distribution lists (such as University
mailing lists), department social media/webpages etc. Only patients that are interested in the study and
have responded via return email will be contacted. The researcher will then contact the potential
participant via telephone to discuss the study, answer any questions they may have and screen them for
eligibility using the screening questionnaire. The patient will be offered 48 hours to consider if they wish
to take part in the study, and will also have the option to opt out of the study at this stage, if desired, and no
further contact will be made.
Inclusion Criteria: Patients must have previously undergone an ileostomy (for any reason) and be
2+ years post-operative, male or female (not pregnant), aged 18-70 years at recruitment.
Exclusion Criteria: Patient has not undergone an ileostomy and/or is less than 2 year post-
operative, pregnant females, aged <18 or >70 years at recruitment, currently taking prescribed
medications that will not permit overnight fasting.
The dietary calcium intake, vitamin status and quality of life of the patients will be assessed by the
following:
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
Ulster University School of Biomedical Sciences
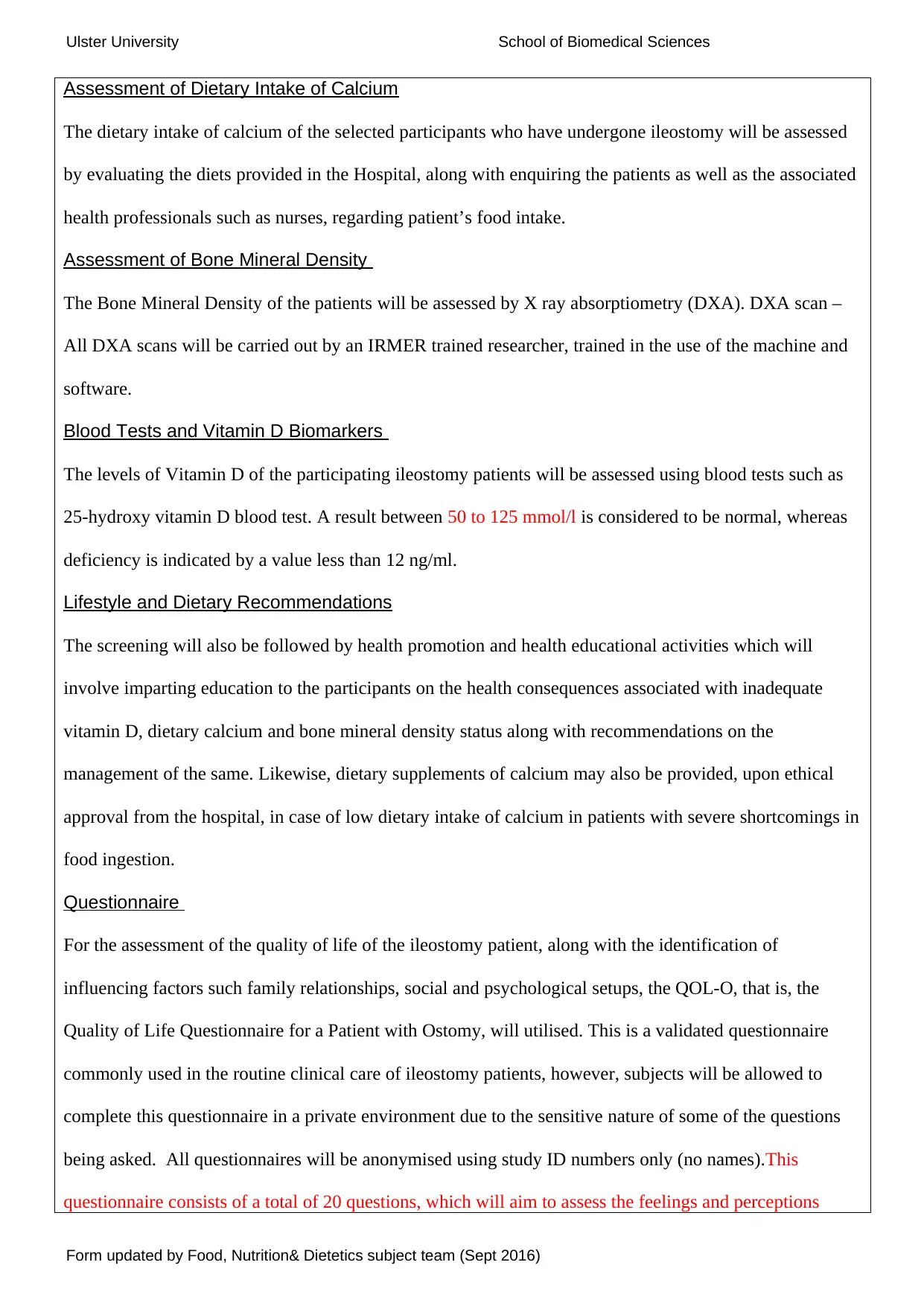
Assessment of Dietary Intake of Calcium
The dietary intake of calcium of the selected participants who have undergone ileostomy will be assessed
by evaluating the diets provided in the Hospital, along with enquiring the patients as well as the associated
health professionals such as nurses, regarding patient’s food intake.
Assessment of Bone Mineral Density
The Bone Mineral Density of the patients will be assessed by X ray absorptiometry (DXA). DXA scan –
All DXA scans will be carried out by an IRMER trained researcher, trained in the use of the machine and
software.
Blood Tests and Vitamin D Biomarkers
The levels of Vitamin D of the participating ileostomy patients will be assessed using blood tests such as
25-hydroxy vitamin D blood test. A result between 50 to 125 mmol/l is considered to be normal, whereas
deficiency is indicated by a value less than 12 ng/ml.
Lifestyle and Dietary Recommendations
The screening will also be followed by health promotion and health educational activities which will
involve imparting education to the participants on the health consequences associated with inadequate
vitamin D, dietary calcium and bone mineral density status along with recommendations on the
management of the same. Likewise, dietary supplements of calcium may also be provided, upon ethical
approval from the hospital, in case of low dietary intake of calcium in patients with severe shortcomings in
food ingestion.
Questionnaire
For the assessment of the quality of life of the ileostomy patient, along with the identification of
influencing factors such family relationships, social and psychological setups, the QOL-O, that is, the
Quality of Life Questionnaire for a Patient with Ostomy, will utilised. This is a validated questionnaire
commonly used in the routine clinical care of ileostomy patients, however, subjects will be allowed to
complete this questionnaire in a private environment due to the sensitive nature of some of the questions
being asked. All questionnaires will be anonymised using study ID numbers only (no names).This
questionnaire consists of a total of 20 questions, which will aim to assess the feelings and perceptions
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
Assessment of Dietary Intake of Calcium
The dietary intake of calcium of the selected participants who have undergone ileostomy will be assessed
by evaluating the diets provided in the Hospital, along with enquiring the patients as well as the associated
health professionals such as nurses, regarding patient’s food intake.
Assessment of Bone Mineral Density
The Bone Mineral Density of the patients will be assessed by X ray absorptiometry (DXA). DXA scan –
All DXA scans will be carried out by an IRMER trained researcher, trained in the use of the machine and
software.
Blood Tests and Vitamin D Biomarkers
The levels of Vitamin D of the participating ileostomy patients will be assessed using blood tests such as
25-hydroxy vitamin D blood test. A result between 50 to 125 mmol/l is considered to be normal, whereas
deficiency is indicated by a value less than 12 ng/ml.
Lifestyle and Dietary Recommendations
The screening will also be followed by health promotion and health educational activities which will
involve imparting education to the participants on the health consequences associated with inadequate
vitamin D, dietary calcium and bone mineral density status along with recommendations on the
management of the same. Likewise, dietary supplements of calcium may also be provided, upon ethical
approval from the hospital, in case of low dietary intake of calcium in patients with severe shortcomings in
food ingestion.
Questionnaire
For the assessment of the quality of life of the ileostomy patient, along with the identification of
influencing factors such family relationships, social and psychological setups, the QOL-O, that is, the
Quality of Life Questionnaire for a Patient with Ostomy, will utilised. This is a validated questionnaire
commonly used in the routine clinical care of ileostomy patients, however, subjects will be allowed to
complete this questionnaire in a private environment due to the sensitive nature of some of the questions
being asked. All questionnaires will be anonymised using study ID numbers only (no names).This
questionnaire consists of a total of 20 questions, which will aim to assess the feelings and perceptions
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Ulster University School of Biomedical Sciences
overcome by patients with a stoma at the moment, through a 4 point scale.
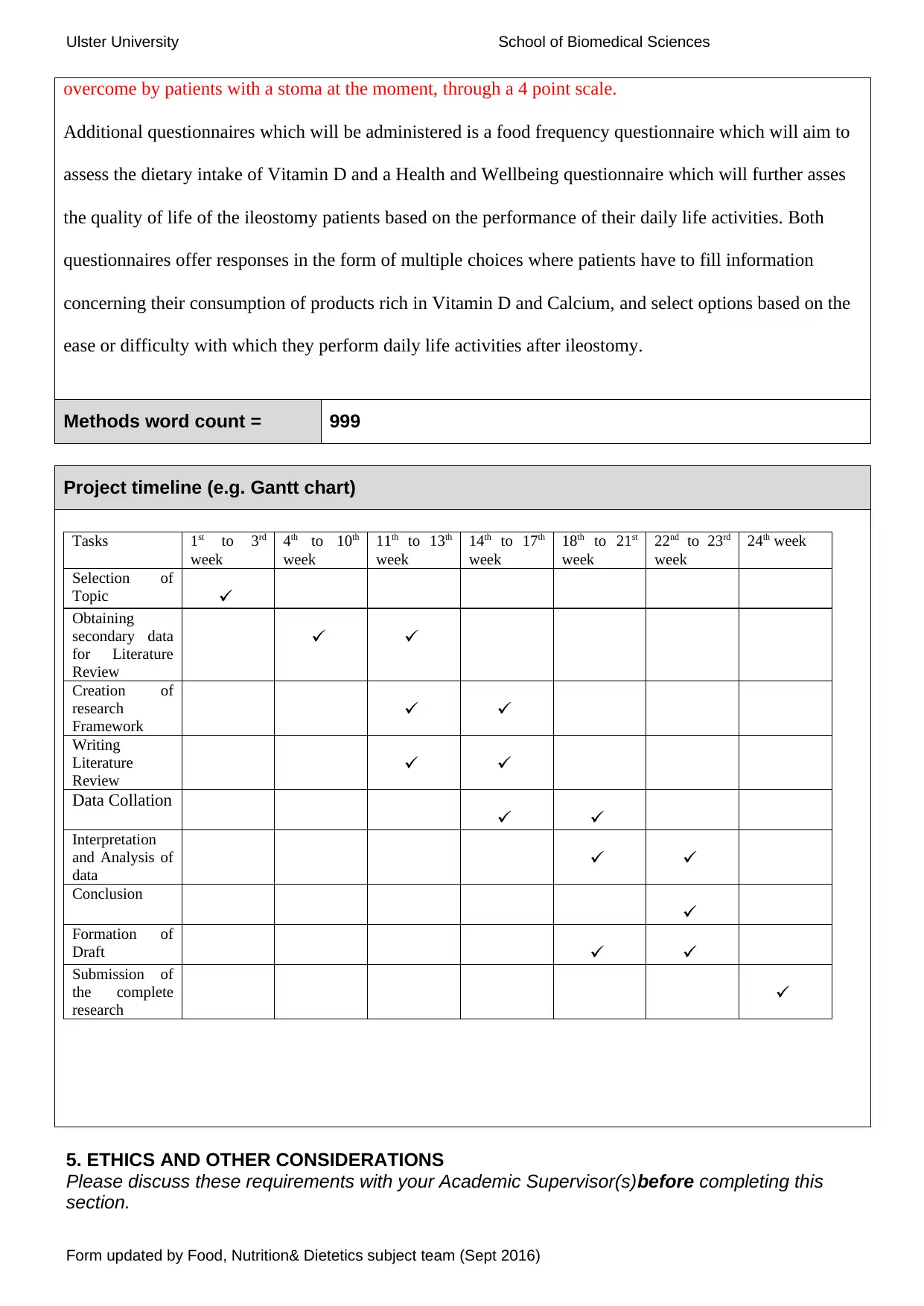
Additional questionnaires which will be administered is a food frequency questionnaire which will aim to
assess the dietary intake of Vitamin D and a Health and Wellbeing questionnaire which will further asses
the quality of life of the ileostomy patients based on the performance of their daily life activities. Both
questionnaires offer responses in the form of multiple choices where patients have to fill information
concerning their consumption of products rich in Vitamin D and Calcium, and select options based on the
ease or difficulty with which they perform daily life activities after ileostomy.
Methods word count = 999
Project timeline (e.g. Gantt chart)
Tasks 1st to 3rd
week
4th to 10th
week
11th to 13th
week
14th to 17th
week
18th to 21st
week
22nd to 23rd
week
24th week
Selection of
Topic
Obtaining
secondary data
for Literature
Review
Creation of
research
Framework
Writing
Literature
Review
Data Collation
Interpretation
and Analysis of
data
Conclusion
Formation of
Draft
Submission of
the complete
research
5. ETHICS AND OTHER CONSIDERATIONS
Please discuss these requirements with your Academic Supervisor(s)before completing this
section.
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
overcome by patients with a stoma at the moment, through a 4 point scale.
Additional questionnaires which will be administered is a food frequency questionnaire which will aim to
assess the dietary intake of Vitamin D and a Health and Wellbeing questionnaire which will further asses
the quality of life of the ileostomy patients based on the performance of their daily life activities. Both
questionnaires offer responses in the form of multiple choices where patients have to fill information
concerning their consumption of products rich in Vitamin D and Calcium, and select options based on the
ease or difficulty with which they perform daily life activities after ileostomy.
Methods word count = 999
Project timeline (e.g. Gantt chart)
Tasks 1st to 3rd
week
4th to 10th
week
11th to 13th
week
14th to 17th
week
18th to 21st
week
22nd to 23rd
week
24th week
Selection of
Topic
Obtaining
secondary data
for Literature
Review
Creation of
research
Framework
Writing
Literature
Review
Data Collation
Interpretation
and Analysis of
data
Conclusion
Formation of
Draft
Submission of
the complete
research
5. ETHICS AND OTHER CONSIDERATIONS
Please discuss these requirements with your Academic Supervisor(s)before completing this
section.
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
Ulster University School of Biomedical Sciences
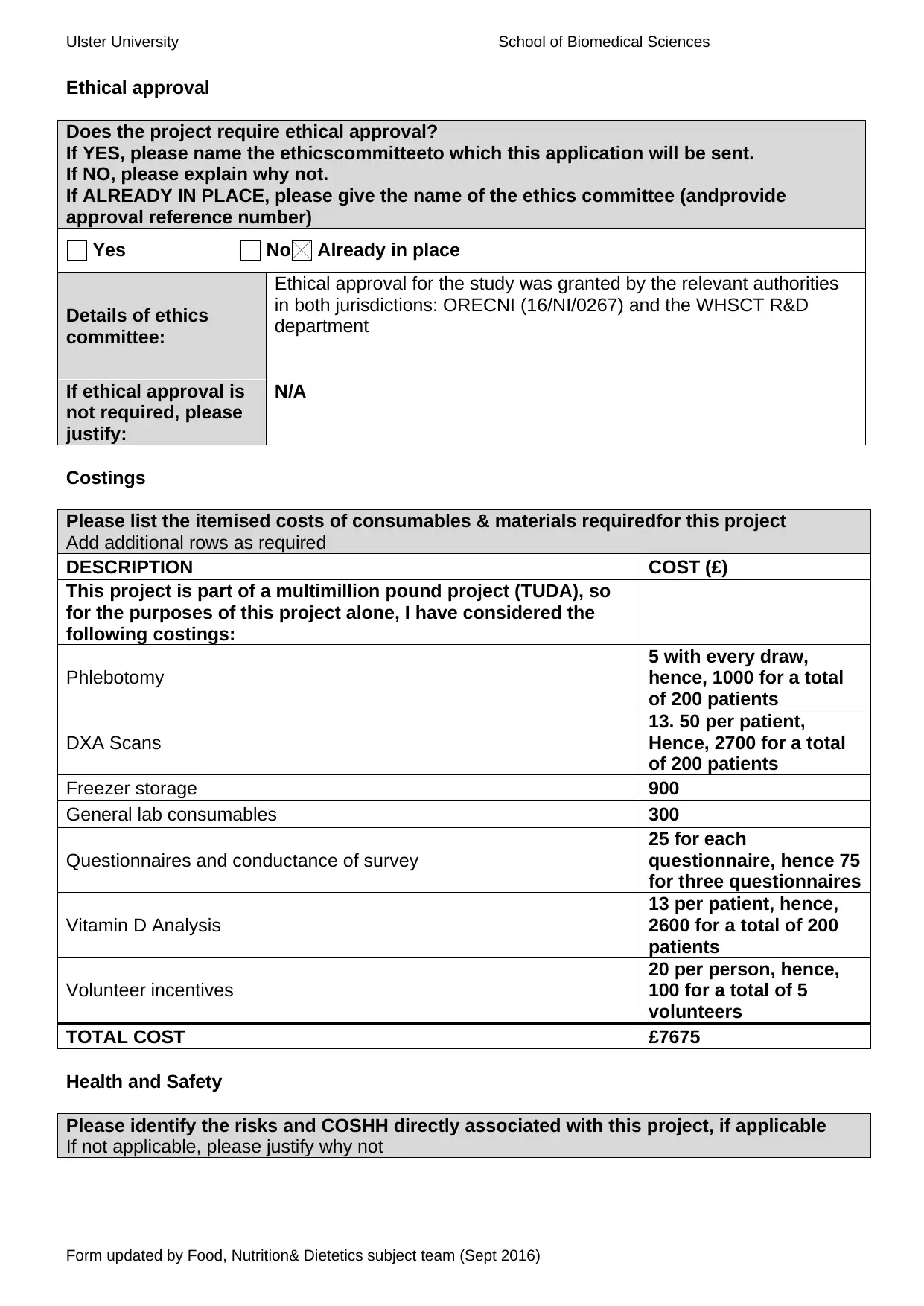
Ethical approval
Does the project require ethical approval?
If YES, please name the ethicscommitteeto which this application will be sent.
If NO, please explain why not.
If ALREADY IN PLACE, please give the name of the ethics committee (andprovide
approval reference number)
Yes No Already in place
Details of ethics
committee:
Ethical approval for the study was granted by the relevant authorities
in both jurisdictions: ORECNI (16/NI/0267) and the WHSCT R&D
department
If ethical approval is
not required, please
justify:
N/A
Costings
Please list the itemised costs of consumables & materials requiredfor this project
Add additional rows as required
DESCRIPTION COST (£)
This project is part of a multimillion pound project (TUDA), so
for the purposes of this project alone, I have considered the
following costings:
Phlebotomy
5 with every draw,
hence, 1000 for a total
of 200 patients
DXA Scans
13. 50 per patient,
Hence, 2700 for a total
of 200 patients
Freezer storage 900
General lab consumables 300
Questionnaires and conductance of survey
25 for each
questionnaire, hence 75
for three questionnaires
Vitamin D Analysis
13 per patient, hence,
2600 for a total of 200
patients
Volunteer incentives
20 per person, hence,
100 for a total of 5
volunteers
TOTAL COST £7675
Health and Safety
Please identify the risks and COSHH directly associated with this project, if applicable
If not applicable, please justify why not
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
Ethical approval
Does the project require ethical approval?
If YES, please name the ethicscommitteeto which this application will be sent.
If NO, please explain why not.
If ALREADY IN PLACE, please give the name of the ethics committee (andprovide
approval reference number)
Yes No Already in place
Details of ethics
committee:
Ethical approval for the study was granted by the relevant authorities
in both jurisdictions: ORECNI (16/NI/0267) and the WHSCT R&D
department
If ethical approval is
not required, please
justify:
N/A
Costings
Please list the itemised costs of consumables & materials requiredfor this project
Add additional rows as required
DESCRIPTION COST (£)
This project is part of a multimillion pound project (TUDA), so
for the purposes of this project alone, I have considered the
following costings:
Phlebotomy
5 with every draw,
hence, 1000 for a total
of 200 patients
DXA Scans
13. 50 per patient,
Hence, 2700 for a total
of 200 patients
Freezer storage 900
General lab consumables 300
Questionnaires and conductance of survey
25 for each
questionnaire, hence 75
for three questionnaires
Vitamin D Analysis
13 per patient, hence,
2600 for a total of 200
patients
Volunteer incentives
20 per person, hence,
100 for a total of 5
volunteers
TOTAL COST £7675
Health and Safety
Please identify the risks and COSHH directly associated with this project, if applicable
If not applicable, please justify why not
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
Ulster University School of Biomedical Sciences
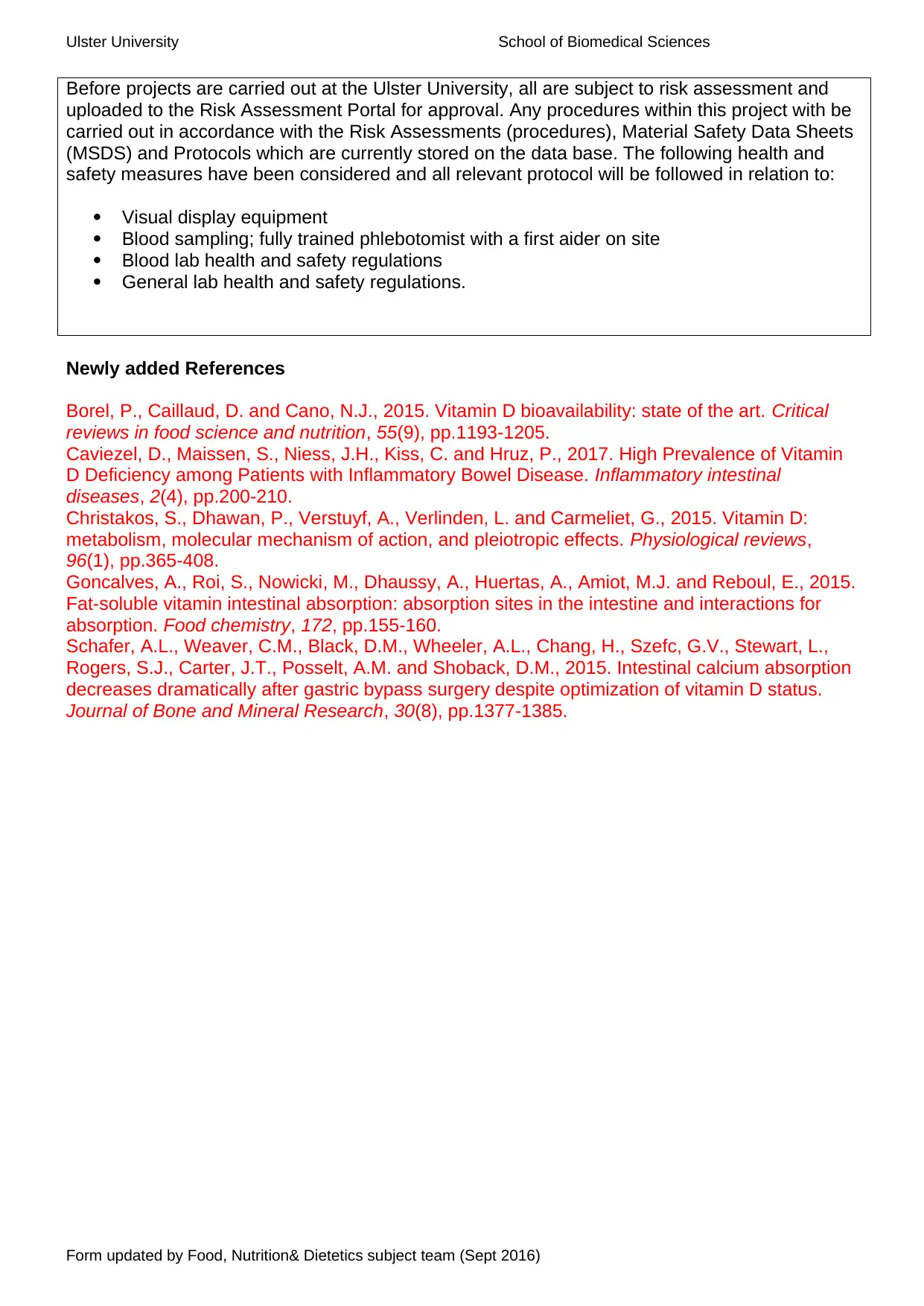
Before projects are carried out at the Ulster University, all are subject to risk assessment and
uploaded to the Risk Assessment Portal for approval. Any procedures within this project with be
carried out in accordance with the Risk Assessments (procedures), Material Safety Data Sheets
(MSDS) and Protocols which are currently stored on the data base. The following health and
safety measures have been considered and all relevant protocol will be followed in relation to:
Visual display equipment
Blood sampling; fully trained phlebotomist with a first aider on site
Blood lab health and safety regulations
General lab health and safety regulations.
Newly added References
Borel, P., Caillaud, D. and Cano, N.J., 2015. Vitamin D bioavailability: state of the art. Critical
reviews in food science and nutrition, 55(9), pp.1193-1205.
Caviezel, D., Maissen, S., Niess, J.H., Kiss, C. and Hruz, P., 2017. High Prevalence of Vitamin
D Deficiency among Patients with Inflammatory Bowel Disease. Inflammatory intestinal
diseases, 2(4), pp.200-210.
Christakos, S., Dhawan, P., Verstuyf, A., Verlinden, L. and Carmeliet, G., 2015. Vitamin D:
metabolism, molecular mechanism of action, and pleiotropic effects. Physiological reviews,
96(1), pp.365-408.
Goncalves, A., Roi, S., Nowicki, M., Dhaussy, A., Huertas, A., Amiot, M.J. and Reboul, E., 2015.
Fat-soluble vitamin intestinal absorption: absorption sites in the intestine and interactions for
absorption. Food chemistry, 172, pp.155-160.
Schafer, A.L., Weaver, C.M., Black, D.M., Wheeler, A.L., Chang, H., Szefc, G.V., Stewart, L.,
Rogers, S.J., Carter, J.T., Posselt, A.M. and Shoback, D.M., 2015. Intestinal calcium absorption
decreases dramatically after gastric bypass surgery despite optimization of vitamin D status.
Journal of Bone and Mineral Research, 30(8), pp.1377-1385.
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
Before projects are carried out at the Ulster University, all are subject to risk assessment and
uploaded to the Risk Assessment Portal for approval. Any procedures within this project with be
carried out in accordance with the Risk Assessments (procedures), Material Safety Data Sheets
(MSDS) and Protocols which are currently stored on the data base. The following health and
safety measures have been considered and all relevant protocol will be followed in relation to:
Visual display equipment
Blood sampling; fully trained phlebotomist with a first aider on site
Blood lab health and safety regulations
General lab health and safety regulations.
Newly added References
Borel, P., Caillaud, D. and Cano, N.J., 2015. Vitamin D bioavailability: state of the art. Critical
reviews in food science and nutrition, 55(9), pp.1193-1205.
Caviezel, D., Maissen, S., Niess, J.H., Kiss, C. and Hruz, P., 2017. High Prevalence of Vitamin
D Deficiency among Patients with Inflammatory Bowel Disease. Inflammatory intestinal
diseases, 2(4), pp.200-210.
Christakos, S., Dhawan, P., Verstuyf, A., Verlinden, L. and Carmeliet, G., 2015. Vitamin D:
metabolism, molecular mechanism of action, and pleiotropic effects. Physiological reviews,
96(1), pp.365-408.
Goncalves, A., Roi, S., Nowicki, M., Dhaussy, A., Huertas, A., Amiot, M.J. and Reboul, E., 2015.
Fat-soluble vitamin intestinal absorption: absorption sites in the intestine and interactions for
absorption. Food chemistry, 172, pp.155-160.
Schafer, A.L., Weaver, C.M., Black, D.M., Wheeler, A.L., Chang, H., Szefc, G.V., Stewart, L.,
Rogers, S.J., Carter, J.T., Posselt, A.M. and Shoback, D.M., 2015. Intestinal calcium absorption
decreases dramatically after gastric bypass surgery despite optimization of vitamin D status.
Journal of Bone and Mineral Research, 30(8), pp.1377-1385.
Form updated by Food, Nutrition& Dietetics subject team (Sept 2016)
1 out of 10
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.

