Understanding Depression/Overdose with Psychosis: A Case Study of Jenna Taylor, 18 years old
VerifiedAdded on 2023/04/22
|11
|2782
|142
AI Summary
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
© 2016 Keith Rischer/www.KeithRN.com
Depression/Overdose with Psychosis
UNFOLDING Reasoning
Jenna Taylor, 18 years old
Primary Concept
Mood and Affect
Interrelated Concepts (In order of emphasis)
1. Safety
2. Psychosis
3. Clinical Judgment
4. Communication
5. Collaboration
Depression/Overdose with Psychosis
UNFOLDING Reasoning
Jenna Taylor, 18 years old
Primary Concept
Mood and Affect
Interrelated Concepts (In order of emphasis)
1. Safety
2. Psychosis
3. Clinical Judgment
4. Communication
5. Collaboration
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
© 2016 Keith Rischer/www.KeithRN.com
Depression/Overdose with Psychosis
PART 1:
History of Present Problem:
Jenna Taylor is an 18-year-old woman who is brought to the emergency department by ambulance after she admitted to
her mother that she had taken a “handful” of dextroamphetamine/amphetamine (Adderall) this morning. Mom noted that
there are 20 tablets missing. Jenna admits that she has been hearing voices telling her that she is worthless and would be
better off dead. She denies visual hallucinations.
As the primary nurse explores these comments further, Jenna states, “The devil is in the place! I can feel it! The
voices are telling me that I am going to hell forever.” Jenna appears fearful, anxious and does not maintain eye contact.
When she briefly glances and looks your way, she appears to be looking through you.
Personal/Social History:
She was hospitalized three weeks ago for depression and suicidal ideation and was discharged ten days ago. Jenna lives
with her mother. Her parents were divorced 12 years ago. She graduated from high school, has few close friends, and has
no current plans for her future.
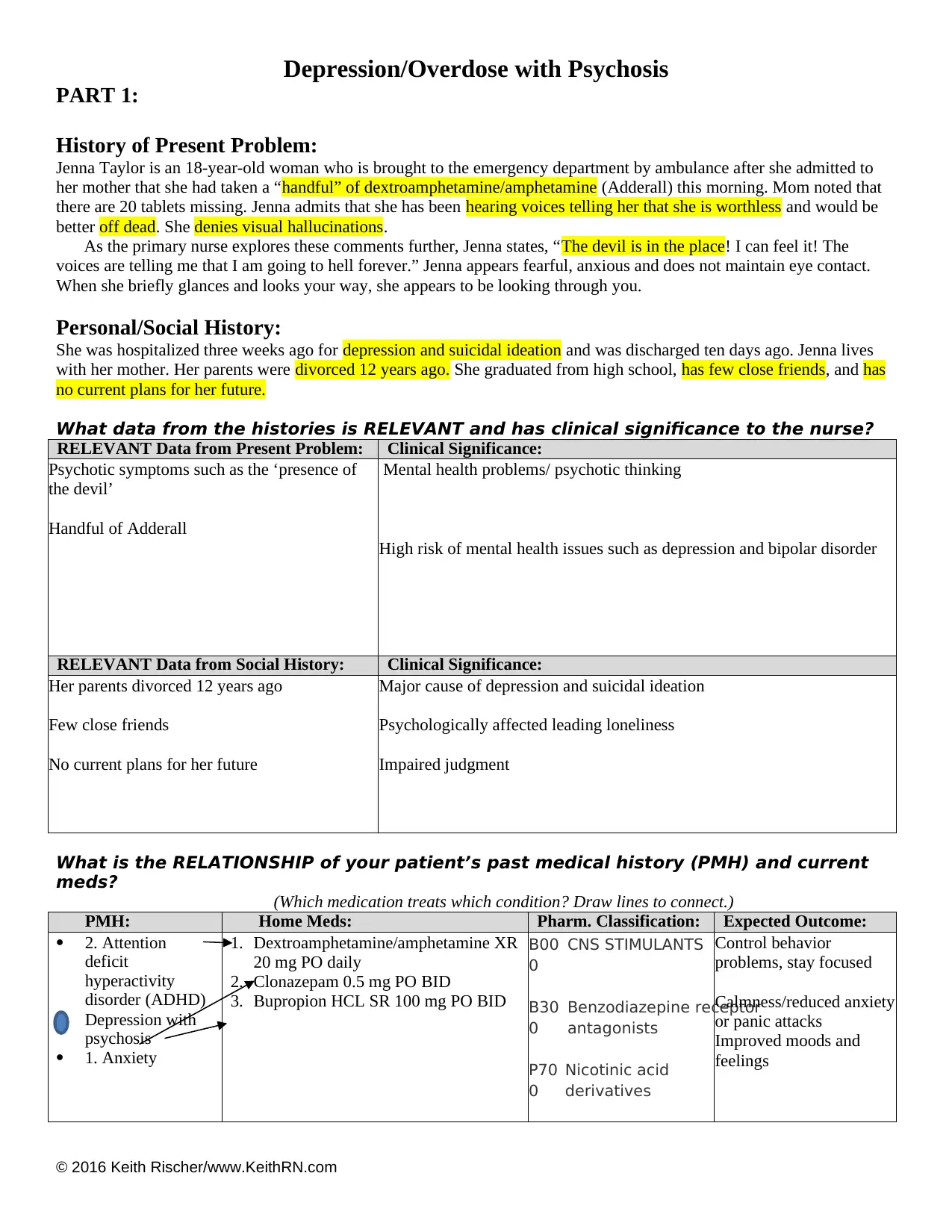
What data from the histories is RELEVANT and has clinical significance to the nurse?
RELEVANT Data from Present Problem: Clinical Significance:
Psychotic symptoms such as the ‘presence of
the devil’
Handful of Adderall
Mental health problems/ psychotic thinking
High risk of mental health issues such as depression and bipolar disorder
RELEVANT Data from Social History: Clinical Significance:
Her parents divorced 12 years ago
Few close friends
No current plans for her future
Major cause of depression and suicidal ideation
Psychologically affected leading loneliness
Impaired judgment
What is the RELATIONSHIP of your patient’s past medical history (PMH) and current
meds?
(Which medication treats which condition? Draw lines to connect.)
PMH: Home Meds: Pharm. Classification: Expected Outcome:
2. Attention
deficit
hyperactivity
disorder (ADHD)
Depression with
psychosis
1. Anxiety
1. Dextroamphetamine/amphetamine XR
20 mg PO daily
2. Clonazepam 0.5 mg PO BID
3. Bupropion HCL SR 100 mg PO BID
B00
0
CNS STIMULANTS
B30
0
Benzodiazepine receptor
antagonists
P70
0
Nicotinic acid
derivatives
Control behavior
problems, stay focused
Calmness/reduced anxiety
or panic attacks
Improved moods and
feelings
Depression/Overdose with Psychosis
PART 1:
History of Present Problem:
Jenna Taylor is an 18-year-old woman who is brought to the emergency department by ambulance after she admitted to
her mother that she had taken a “handful” of dextroamphetamine/amphetamine (Adderall) this morning. Mom noted that
there are 20 tablets missing. Jenna admits that she has been hearing voices telling her that she is worthless and would be
better off dead. She denies visual hallucinations.
As the primary nurse explores these comments further, Jenna states, “The devil is in the place! I can feel it! The
voices are telling me that I am going to hell forever.” Jenna appears fearful, anxious and does not maintain eye contact.
When she briefly glances and looks your way, she appears to be looking through you.
Personal/Social History:
She was hospitalized three weeks ago for depression and suicidal ideation and was discharged ten days ago. Jenna lives
with her mother. Her parents were divorced 12 years ago. She graduated from high school, has few close friends, and has
no current plans for her future.
What data from the histories is RELEVANT and has clinical significance to the nurse?
RELEVANT Data from Present Problem: Clinical Significance:
Psychotic symptoms such as the ‘presence of
the devil’
Handful of Adderall
Mental health problems/ psychotic thinking
High risk of mental health issues such as depression and bipolar disorder
RELEVANT Data from Social History: Clinical Significance:
Her parents divorced 12 years ago
Few close friends
No current plans for her future
Major cause of depression and suicidal ideation
Psychologically affected leading loneliness
Impaired judgment
What is the RELATIONSHIP of your patient’s past medical history (PMH) and current
meds?
(Which medication treats which condition? Draw lines to connect.)
PMH: Home Meds: Pharm. Classification: Expected Outcome:
2. Attention
deficit
hyperactivity
disorder (ADHD)
Depression with
psychosis
1. Anxiety
1. Dextroamphetamine/amphetamine XR
20 mg PO daily
2. Clonazepam 0.5 mg PO BID
3. Bupropion HCL SR 100 mg PO BID
B00
0
CNS STIMULANTS
B30
0
Benzodiazepine receptor
antagonists
P70
0
Nicotinic acid
derivatives
Control behavior
problems, stay focused
Calmness/reduced anxiety
or panic attacks
Improved moods and
feelings
© 2016 Keith Rischer/www.KeithRN.com
(Butcher, Bulechek, Dochterman, & Wagner, 2018).
One disease process often influences the development of other illnesses. Based on your knowledge of
pathophysiology, (if applicable), which disease likely developed FIRST, then initiated a “domino effect” in Jenna’s
life?
Circle the PMH problem that likely started FIRST.
Numbr the PMH problem(s) that FOLLOWED as domino(s).
Patient Care Begins:
Current VS: WILDA Pain Assessment (5th VS):
T: 99.2 F (37.3 C) oral Words: Denies
P: 92 (regular) Intensity: Moderate
R: 20 (regular) Location: Head
BP: 118/70 Duration: Episodic
O2 sat: 98% RA Aggravate:
Alleviate:
Overdose, divorced parents, few friends
Correct Adderall dosage
(Murray & Barker, 2018).
What VS data is RELEVANT and must be recognized as clinically significant by the nurse?
RELEVANT VS Data: Clinical Significance:
R: 20 (regular)
O2 sat: 98% RA
The location of pain will help ascertain the cause of the disease and prioritized treatment of the
most affected areas.
Ascertaining aggravating and alleviating factors helps in determining the cause and treatment
options
Current Assessment:
GENERAL
APPEARANCE:
Appears comfortable, no acute distress
RESP: Breath sounds clear with equal aeration bilaterally, nonlabored respiratory effort
CARDIAC: Pink, warm and dry, no edema, heart sounds regular with no abnormal beats, pulses
strong, equal with palpation at radial/pedal/post-tibial landmarks
NEURO: Alert and oriented to person, place, time, and situation (x4), flat affect
GI: Abdomen soft/nontender, bowel sounds audible per auscultation in all four
quadrants
GU: Voiding without difficulty, urine clear/yellow
SKIN: Skin integrity intact
What assessment data is RELEVANT and must be recognized as clinically significant by the
nurse?
RELEVANT Assessment Data: Clinical Significance:
RESP
CARDIAC:
Ascertaining any airway blockage, evaluation of the response of the medication
that affects the respiratory system.
Possibility of any heart disease
Mental Status Examination (MSE):
APPEARANCE: Dressed in casual clothes, no make-up; no body odor; appears tired and appears stated age;
cooperative during interview
MOTOR BEHAVIOR: Psychomotor agitation, restless
(Butcher, Bulechek, Dochterman, & Wagner, 2018).
One disease process often influences the development of other illnesses. Based on your knowledge of
pathophysiology, (if applicable), which disease likely developed FIRST, then initiated a “domino effect” in Jenna’s
life?
Circle the PMH problem that likely started FIRST.
Numbr the PMH problem(s) that FOLLOWED as domino(s).
Patient Care Begins:
Current VS: WILDA Pain Assessment (5th VS):
T: 99.2 F (37.3 C) oral Words: Denies
P: 92 (regular) Intensity: Moderate
R: 20 (regular) Location: Head
BP: 118/70 Duration: Episodic
O2 sat: 98% RA Aggravate:
Alleviate:
Overdose, divorced parents, few friends
Correct Adderall dosage
(Murray & Barker, 2018).
What VS data is RELEVANT and must be recognized as clinically significant by the nurse?
RELEVANT VS Data: Clinical Significance:
R: 20 (regular)
O2 sat: 98% RA
The location of pain will help ascertain the cause of the disease and prioritized treatment of the
most affected areas.
Ascertaining aggravating and alleviating factors helps in determining the cause and treatment
options
Current Assessment:
GENERAL
APPEARANCE:
Appears comfortable, no acute distress
RESP: Breath sounds clear with equal aeration bilaterally, nonlabored respiratory effort
CARDIAC: Pink, warm and dry, no edema, heart sounds regular with no abnormal beats, pulses
strong, equal with palpation at radial/pedal/post-tibial landmarks
NEURO: Alert and oriented to person, place, time, and situation (x4), flat affect
GI: Abdomen soft/nontender, bowel sounds audible per auscultation in all four
quadrants
GU: Voiding without difficulty, urine clear/yellow
SKIN: Skin integrity intact
What assessment data is RELEVANT and must be recognized as clinically significant by the
nurse?
RELEVANT Assessment Data: Clinical Significance:
RESP
CARDIAC:
Ascertaining any airway blockage, evaluation of the response of the medication
that affects the respiratory system.
Possibility of any heart disease
Mental Status Examination (MSE):
APPEARANCE: Dressed in casual clothes, no make-up; no body odor; appears tired and appears stated age;
cooperative during interview
MOTOR BEHAVIOR: Psychomotor agitation, restless
© 2016 Keith Rischer/www.KeithRN.com
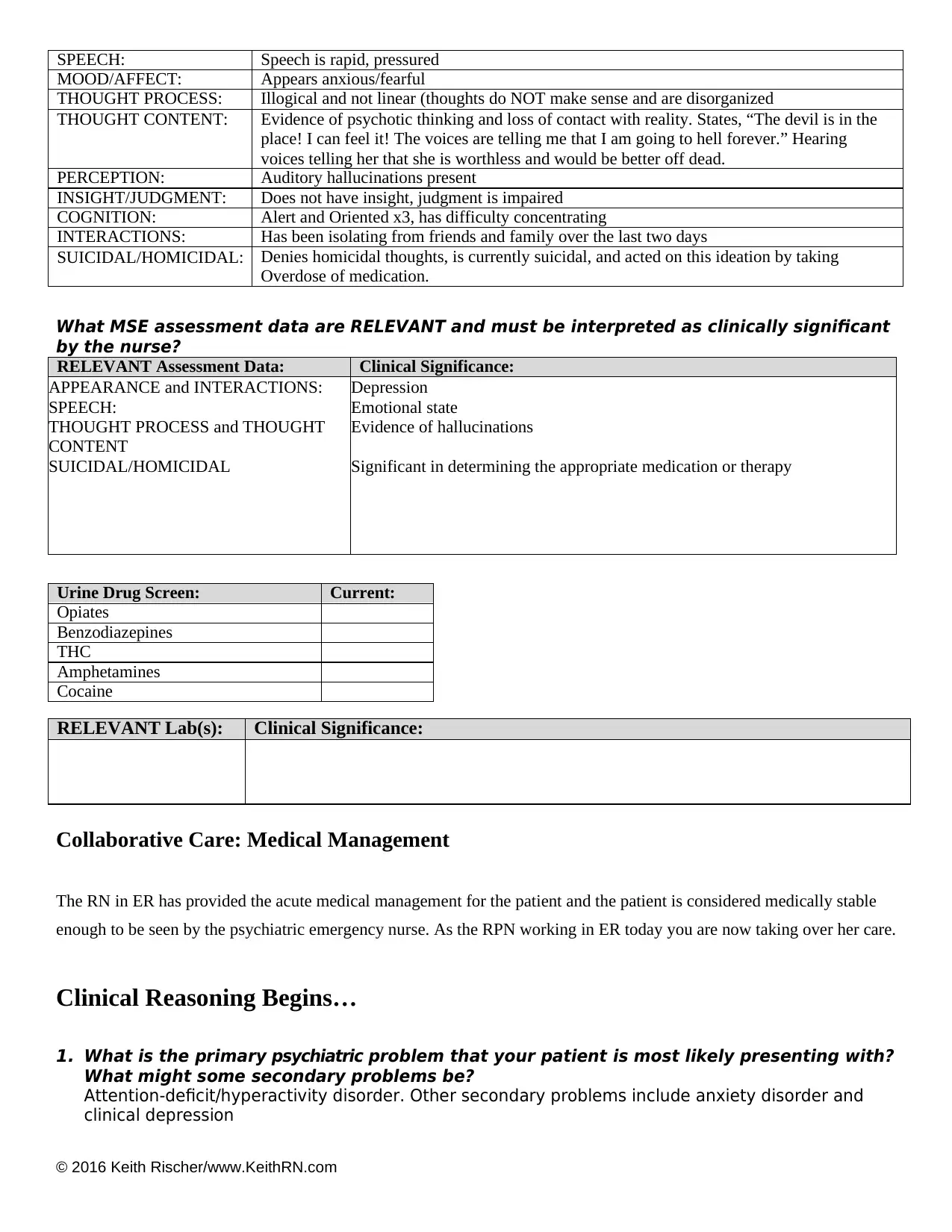
SPEECH: Speech is rapid, pressured
MOOD/AFFECT: Appears anxious/fearful
THOUGHT PROCESS: Illogical and not linear (thoughts do NOT make sense and are disorganized
THOUGHT CONTENT: Evidence of psychotic thinking and loss of contact with reality. States, “The devil is in the
place! I can feel it! The voices are telling me that I am going to hell forever.” Hearing
voices telling her that she is worthless and would be better off dead.
PERCEPTION: Auditory hallucinations present
INSIGHT/JUDGMENT: Does not have insight, judgment is impaired
COGNITION: Alert and Oriented x3, has difficulty concentrating
INTERACTIONS: Has been isolating from friends and family over the last two days
SUICIDAL/HOMICIDAL: Denies homicidal thoughts, is currently suicidal, and acted on this ideation by taking
Overdose of medication.
What MSE assessment data are RELEVANT and must be interpreted as clinically significant
by the nurse?
RELEVANT Assessment Data: Clinical Significance:
APPEARANCE and INTERACTIONS:
SPEECH:
THOUGHT PROCESS and THOUGHT
CONTENT
SUICIDAL/HOMICIDAL
Depression
Emotional state
Evidence of hallucinations
Significant in determining the appropriate medication or therapy
Urine Drug Screen: Current:
Opiates
Benzodiazepines
THC
Amphetamines
Cocaine
RELEVANT Lab(s): Clinical Significance:
Collaborative Care: Medical Management
The RN in ER has provided the acute medical management for the patient and the patient is considered medically stable
enough to be seen by the psychiatric emergency nurse. As the RPN working in ER today you are now taking over her care.
Clinical Reasoning Begins…
1. What is the primary psychiatric problem that your patient is most likely presenting with?
What might some secondary problems be?
Attention-deficit/hyperactivity disorder. Other secondary problems include anxiety disorder and
clinical depression
SPEECH: Speech is rapid, pressured
MOOD/AFFECT: Appears anxious/fearful
THOUGHT PROCESS: Illogical and not linear (thoughts do NOT make sense and are disorganized
THOUGHT CONTENT: Evidence of psychotic thinking and loss of contact with reality. States, “The devil is in the
place! I can feel it! The voices are telling me that I am going to hell forever.” Hearing
voices telling her that she is worthless and would be better off dead.
PERCEPTION: Auditory hallucinations present
INSIGHT/JUDGMENT: Does not have insight, judgment is impaired
COGNITION: Alert and Oriented x3, has difficulty concentrating
INTERACTIONS: Has been isolating from friends and family over the last two days
SUICIDAL/HOMICIDAL: Denies homicidal thoughts, is currently suicidal, and acted on this ideation by taking
Overdose of medication.
What MSE assessment data are RELEVANT and must be interpreted as clinically significant
by the nurse?
RELEVANT Assessment Data: Clinical Significance:
APPEARANCE and INTERACTIONS:
SPEECH:
THOUGHT PROCESS and THOUGHT
CONTENT
SUICIDAL/HOMICIDAL
Depression
Emotional state
Evidence of hallucinations
Significant in determining the appropriate medication or therapy
Urine Drug Screen: Current:
Opiates
Benzodiazepines
THC
Amphetamines
Cocaine
RELEVANT Lab(s): Clinical Significance:
Collaborative Care: Medical Management
The RN in ER has provided the acute medical management for the patient and the patient is considered medically stable
enough to be seen by the psychiatric emergency nurse. As the RPN working in ER today you are now taking over her care.
Clinical Reasoning Begins…
1. What is the primary psychiatric problem that your patient is most likely presenting with?
What might some secondary problems be?
Attention-deficit/hyperactivity disorder. Other secondary problems include anxiety disorder and
clinical depression
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
© 2016 Keith Rischer/www.KeithRN.com
2. What is the underlying cause/pathophysiology of your primary and secondary concerns?
Causes of ADHD
Genetics-ADHD tends to run in families
Brain disorder or injury-damage to the frontal lobe leading to difficulties in controlling
emotions and impulses
Toxins such as incorrect medication or overdose of central nervous system drugs (Killeen,
Tannock, & Sagvolden, 2011).
Cause of anxiety disorder
Drug misuse or withdrawal, heart disease or diabetes. It can also be caused by trauma,
stress as a result of sickness, drugs or alcohol (Lader, 2015).
Clinical depression
Caused by stressful life event such as divorce and build-up of pressure (Beck & Alford, 2009).
Collaborative Care: Nursing
3. What psychiatric nursing priority(s) will guide your plan of care? (if more than one-list in order
of PRIORITY)
Self-concept - Disturbed body image – 00118
Mood regulation - Impaired mood regulation – 00241
Comfort - Anxiety – 00146
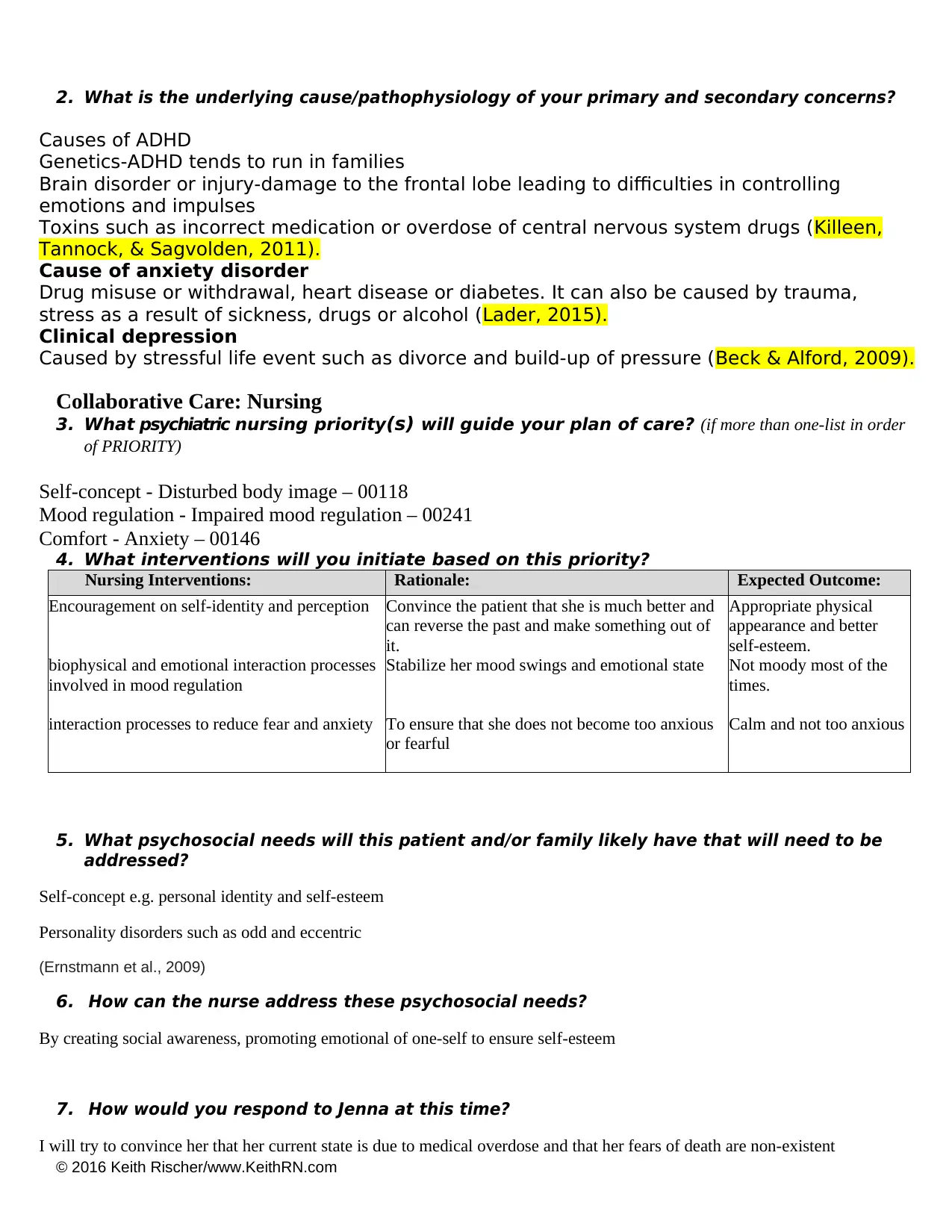
4. What interventions will you initiate based on this priority?
Nursing Interventions: Rationale: Expected Outcome:
Encouragement on self-identity and perception
biophysical and emotional interaction processes
involved in mood regulation
interaction processes to reduce fear and anxiety
Convince the patient that she is much better and
can reverse the past and make something out of
it.
Stabilize her mood swings and emotional state
To ensure that she does not become too anxious
or fearful
Appropriate physical
appearance and better
self-esteem.
Not moody most of the
times.
Calm and not too anxious
5. What psychosocial needs will this patient and/or family likely have that will need to be
addressed?
Self-concept e.g. personal identity and self-esteem
Personality disorders such as odd and eccentric
(Ernstmann et al., 2009)
6. How can the nurse address these psychosocial needs?
By creating social awareness, promoting emotional of one-self to ensure self-esteem
7. How would you respond to Jenna at this time?
I will try to convince her that her current state is due to medical overdose and that her fears of death are non-existent
2. What is the underlying cause/pathophysiology of your primary and secondary concerns?
Causes of ADHD
Genetics-ADHD tends to run in families
Brain disorder or injury-damage to the frontal lobe leading to difficulties in controlling
emotions and impulses
Toxins such as incorrect medication or overdose of central nervous system drugs (Killeen,
Tannock, & Sagvolden, 2011).
Cause of anxiety disorder
Drug misuse or withdrawal, heart disease or diabetes. It can also be caused by trauma,
stress as a result of sickness, drugs or alcohol (Lader, 2015).
Clinical depression
Caused by stressful life event such as divorce and build-up of pressure (Beck & Alford, 2009).
Collaborative Care: Nursing
3. What psychiatric nursing priority(s) will guide your plan of care? (if more than one-list in order
of PRIORITY)
Self-concept - Disturbed body image – 00118
Mood regulation - Impaired mood regulation – 00241
Comfort - Anxiety – 00146
4. What interventions will you initiate based on this priority?
Nursing Interventions: Rationale: Expected Outcome:
Encouragement on self-identity and perception
biophysical and emotional interaction processes
involved in mood regulation
interaction processes to reduce fear and anxiety
Convince the patient that she is much better and
can reverse the past and make something out of
it.
Stabilize her mood swings and emotional state
To ensure that she does not become too anxious
or fearful
Appropriate physical
appearance and better
self-esteem.
Not moody most of the
times.
Calm and not too anxious
5. What psychosocial needs will this patient and/or family likely have that will need to be
addressed?
Self-concept e.g. personal identity and self-esteem
Personality disorders such as odd and eccentric
(Ernstmann et al., 2009)
6. How can the nurse address these psychosocial needs?
By creating social awareness, promoting emotional of one-self to ensure self-esteem
7. How would you respond to Jenna at this time?
I will try to convince her that her current state is due to medical overdose and that her fears of death are non-existent
© 2016 Keith Rischer/www.KeithRN.com
8. How could you use attentive listening and presence with this patient and her mother?
I will lean forward and maintain eye contact in addition to head nodding as an indication that I am interested in their problem
and thus would like to provide a solution
9. What barriers to effective communication do you anticipate? How might these barriers be
eliminated?
Lack of the willingness to disclose vital information.
Unwillingness to listen to the nurse
Solution
These barriers can be eliminated by first winning the confidence of the patient by assuring her that I
have handled previous incidences like hers and in some case worse than hers, but this will require
maximum cooperation.
I will also try to show interest by the use of active listening skills mentioned in question 8 above
10. What are useful communication strategies to use when Jenna is demonstrating
hallucinations and delusional beliefs?
Keep a non-judgmental attitude
Develop a rapport
Be mindful of non-verbal communication
8. How could you use attentive listening and presence with this patient and her mother?
I will lean forward and maintain eye contact in addition to head nodding as an indication that I am interested in their problem
and thus would like to provide a solution
9. What barriers to effective communication do you anticipate? How might these barriers be
eliminated?
Lack of the willingness to disclose vital information.
Unwillingness to listen to the nurse
Solution
These barriers can be eliminated by first winning the confidence of the patient by assuring her that I
have handled previous incidences like hers and in some case worse than hers, but this will require
maximum cooperation.
I will also try to show interest by the use of active listening skills mentioned in question 8 above
10. What are useful communication strategies to use when Jenna is demonstrating
hallucinations and delusional beliefs?
Keep a non-judgmental attitude
Develop a rapport
Be mindful of non-verbal communication
© 2016 Keith Rischer/www.KeithRN.com
PART 2:
Evaluation: Two hours later…
Jenna has become more restless with increased pacing in room. She cries out loudly in a shriek.
As you enter the room, Jenna is sitting on the bed and states fearfully, “I told you the devil is in
this place! Please help me!” Jenna begins to cry, yelling “Devil get out, devil get out!” and
holding her head in her hands and curling up into the fetal position on the couch.
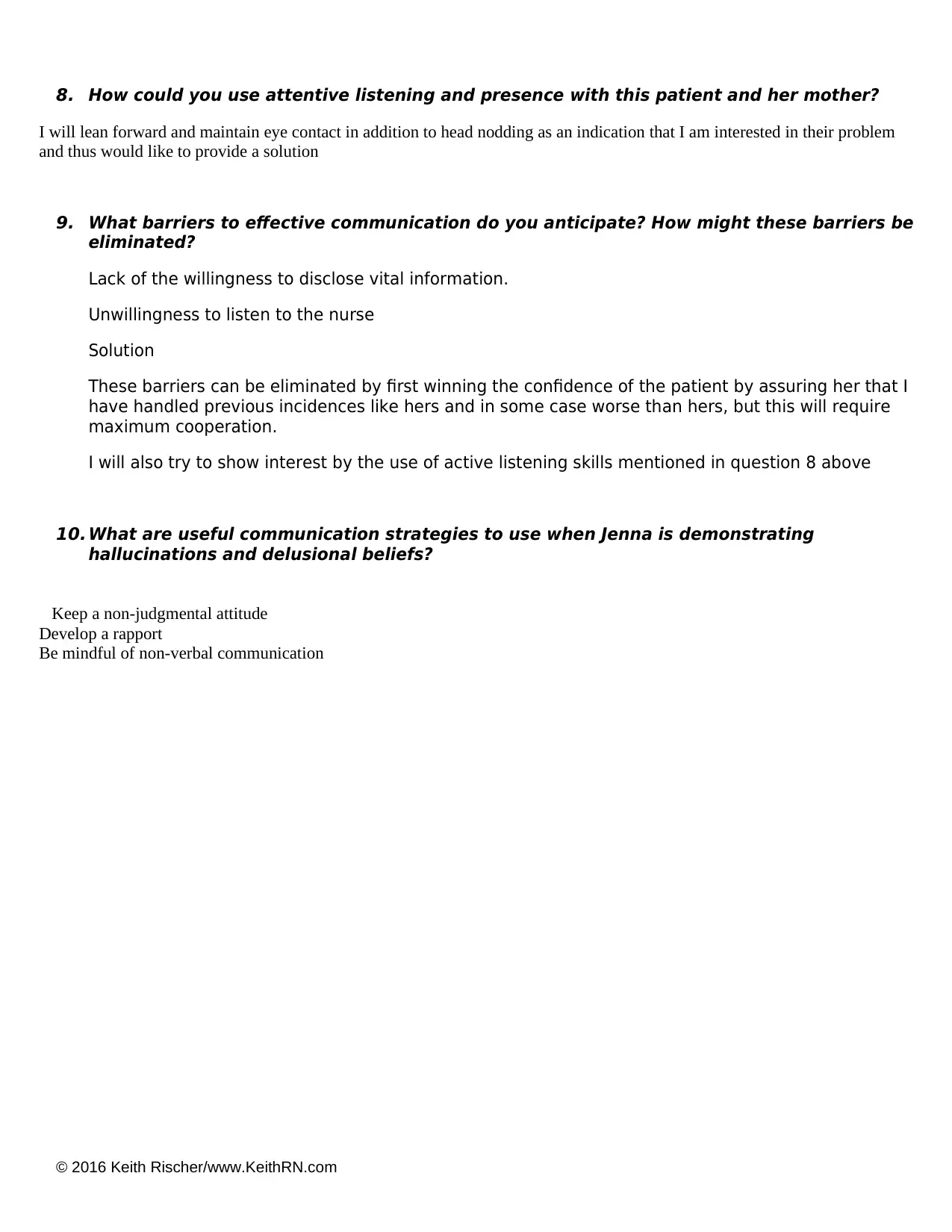
1. What clinical data is RELEVANT that must be recognized as clinically significant?
RELEVANT VS Data: Clinical Significance:
More restless and increased pacing Advanced depression
RELEVANT Assessment Data: Clinical Significance:
Hallucinations Mental disorder
2. Has her psychiatric status improved or not as expected to this point?
It has actually increased
3. Does your nursing priority or plan of care need to be modified in any way after this
evaluation assessment?
Yes
4. Based on your current evaluation, what are your nursing priorities and plan of
care?
She should be admitted to the psychiatric intensive care unit and More emphasis should be placed on addressing self-concept,
then mood regulation and comfort or assurance
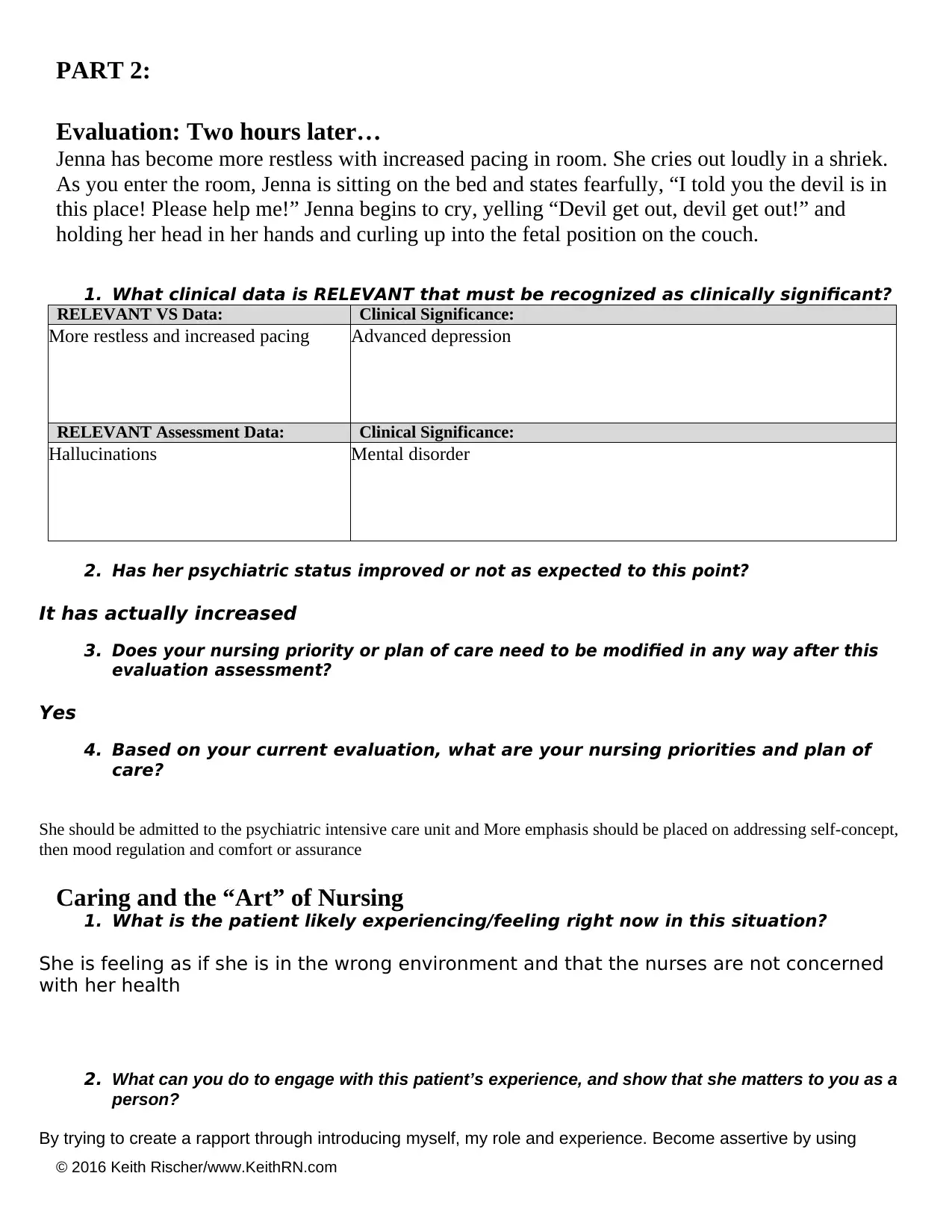
Caring and the “Art” of Nursing
1. What is the patient likely experiencing/feeling right now in this situation?
She is feeling as if she is in the wrong environment and that the nurses are not concerned
with her health
2. What can you do to engage with this patient’s experience, and show that she matters to you as a
person?
By trying to create a rapport through introducing myself, my role and experience. Become assertive by using
PART 2:
Evaluation: Two hours later…
Jenna has become more restless with increased pacing in room. She cries out loudly in a shriek.
As you enter the room, Jenna is sitting on the bed and states fearfully, “I told you the devil is in
this place! Please help me!” Jenna begins to cry, yelling “Devil get out, devil get out!” and
holding her head in her hands and curling up into the fetal position on the couch.
1. What clinical data is RELEVANT that must be recognized as clinically significant?
RELEVANT VS Data: Clinical Significance:
More restless and increased pacing Advanced depression
RELEVANT Assessment Data: Clinical Significance:
Hallucinations Mental disorder
2. Has her psychiatric status improved or not as expected to this point?
It has actually increased
3. Does your nursing priority or plan of care need to be modified in any way after this
evaluation assessment?
Yes
4. Based on your current evaluation, what are your nursing priorities and plan of
care?
She should be admitted to the psychiatric intensive care unit and More emphasis should be placed on addressing self-concept,
then mood regulation and comfort or assurance
Caring and the “Art” of Nursing
1. What is the patient likely experiencing/feeling right now in this situation?
She is feeling as if she is in the wrong environment and that the nurses are not concerned
with her health
2. What can you do to engage with this patient’s experience, and show that she matters to you as a
person?
By trying to create a rapport through introducing myself, my role and experience. Become assertive by using
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
© 2016 Keith Rischer/www.KeithRN.com
statements such as ‘I’. Exercising keen listening skills and not rushing to conclusions. Giving an illustration of a
similar incidence that I successfully handled before in order to win her confidence and establish a rapport.
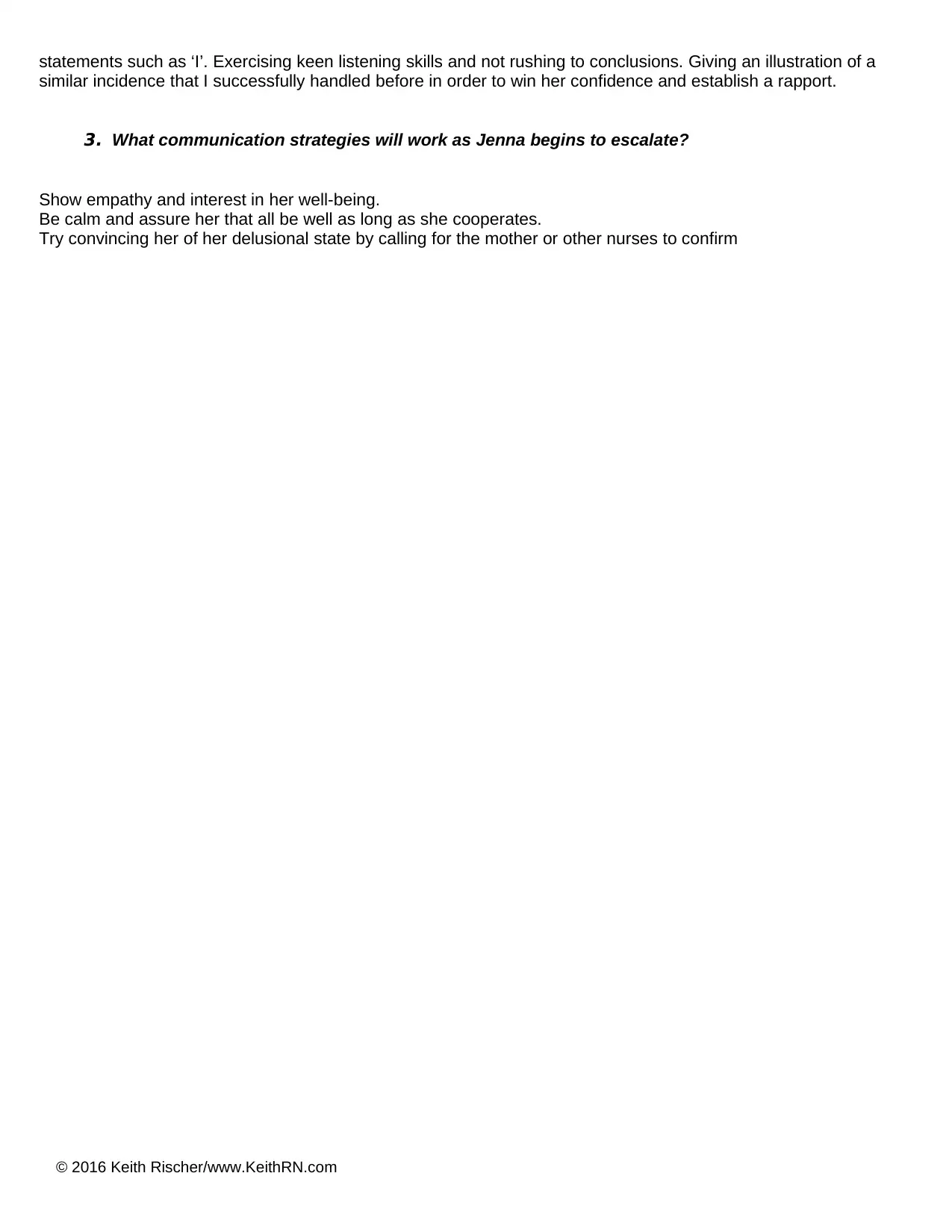
3. What communication strategies will work as Jenna begins to escalate?
Show empathy and interest in her well-being.
Be calm and assure her that all be well as long as she cooperates.
Try convincing her of her delusional state by calling for the mother or other nurses to confirm
statements such as ‘I’. Exercising keen listening skills and not rushing to conclusions. Giving an illustration of a
similar incidence that I successfully handled before in order to win her confidence and establish a rapport.
3. What communication strategies will work as Jenna begins to escalate?
Show empathy and interest in her well-being.
Be calm and assure her that all be well as long as she cooperates.
Try convincing her of her delusional state by calling for the mother or other nurses to confirm
© 2016 Keith Rischer/www.KeithRN.com
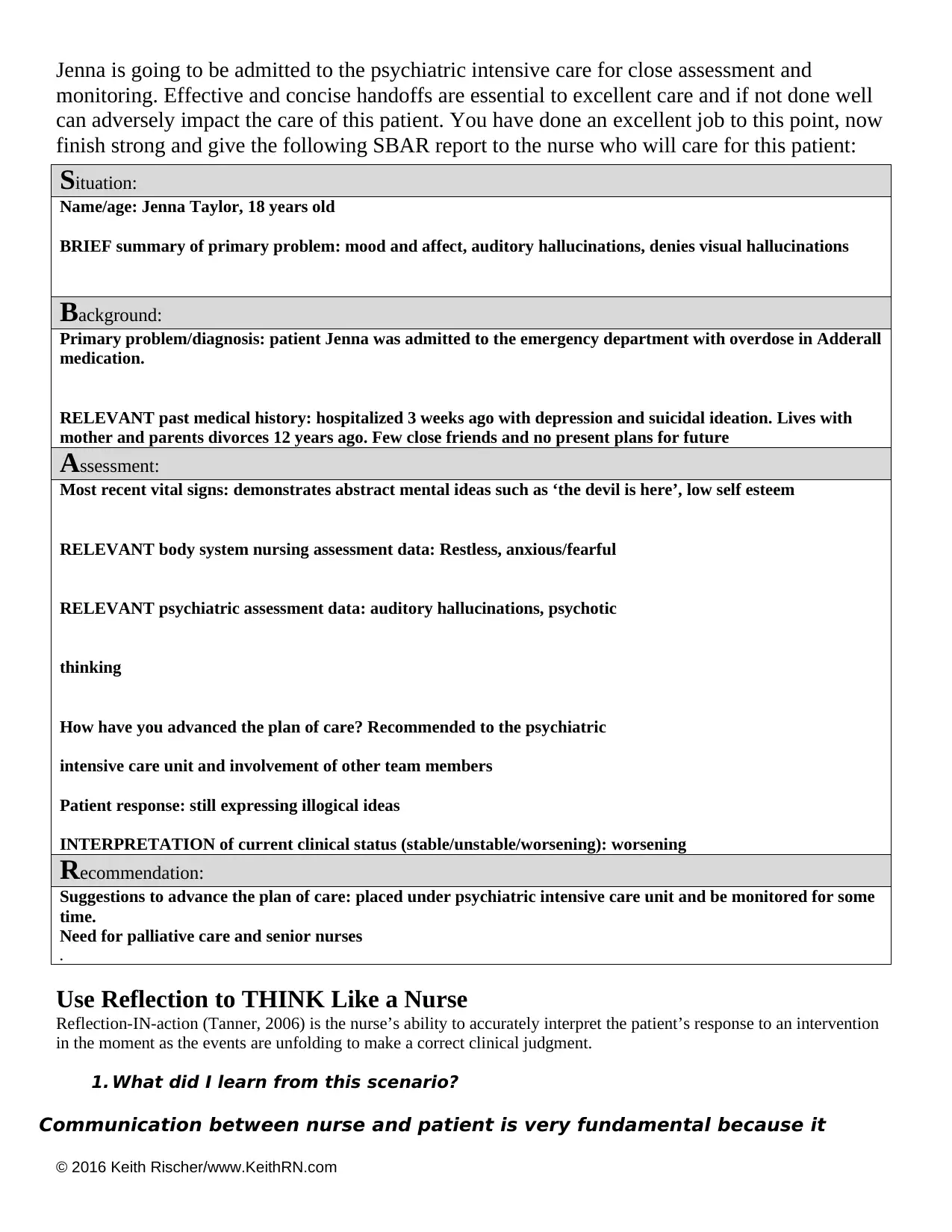
Jenna is going to be admitted to the psychiatric intensive care for close assessment and
monitoring. Effective and concise handoffs are essential to excellent care and if not done well
can adversely impact the care of this patient. You have done an excellent job to this point, now
finish strong and give the following SBAR report to the nurse who will care for this patient:
Situation:
Name/age: Jenna Taylor, 18 years old
BRIEF summary of primary problem: mood and affect, auditory hallucinations, denies visual hallucinations
Background:
Primary problem/diagnosis: patient Jenna was admitted to the emergency department with overdose in Adderall
medication.
RELEVANT past medical history: hospitalized 3 weeks ago with depression and suicidal ideation. Lives with
mother and parents divorces 12 years ago. Few close friends and no present plans for future
Assessment:
Most recent vital signs: demonstrates abstract mental ideas such as ‘the devil is here’, low self esteem
RELEVANT body system nursing assessment data: Restless, anxious/fearful
RELEVANT psychiatric assessment data: auditory hallucinations, psychotic
thinking
How have you advanced the plan of care? Recommended to the psychiatric
intensive care unit and involvement of other team members
Patient response: still expressing illogical ideas
INTERPRETATION of current clinical status (stable/unstable/worsening): worsening
Recommendation:
Suggestions to advance the plan of care: placed under psychiatric intensive care unit and be monitored for some
time.
Need for palliative care and senior nurses
.
Use Reflection to THINK Like a Nurse
Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention
in the moment as the events are unfolding to make a correct clinical judgment.
1. What did I learn from this scenario?
Communication between nurse and patient is very fundamental because it
Jenna is going to be admitted to the psychiatric intensive care for close assessment and
monitoring. Effective and concise handoffs are essential to excellent care and if not done well
can adversely impact the care of this patient. You have done an excellent job to this point, now
finish strong and give the following SBAR report to the nurse who will care for this patient:
Situation:
Name/age: Jenna Taylor, 18 years old
BRIEF summary of primary problem: mood and affect, auditory hallucinations, denies visual hallucinations
Background:
Primary problem/diagnosis: patient Jenna was admitted to the emergency department with overdose in Adderall
medication.
RELEVANT past medical history: hospitalized 3 weeks ago with depression and suicidal ideation. Lives with
mother and parents divorces 12 years ago. Few close friends and no present plans for future
Assessment:
Most recent vital signs: demonstrates abstract mental ideas such as ‘the devil is here’, low self esteem
RELEVANT body system nursing assessment data: Restless, anxious/fearful
RELEVANT psychiatric assessment data: auditory hallucinations, psychotic
thinking
How have you advanced the plan of care? Recommended to the psychiatric
intensive care unit and involvement of other team members
Patient response: still expressing illogical ideas
INTERPRETATION of current clinical status (stable/unstable/worsening): worsening
Recommendation:
Suggestions to advance the plan of care: placed under psychiatric intensive care unit and be monitored for some
time.
Need for palliative care and senior nurses
.
Use Reflection to THINK Like a Nurse
Reflection-IN-action (Tanner, 2006) is the nurse’s ability to accurately interpret the patient’s response to an intervention
in the moment as the events are unfolding to make a correct clinical judgment.
1. What did I learn from this scenario?
Communication between nurse and patient is very fundamental because it
© 2016 Keith Rischer/www.KeithRN.com
determines the patient’s response to treatment.
Psychiatric cases require expert handling without with the patient may worsen to
extent of mental damage
2. How can I use what has been learned from this scenario to improve patient care in the
f uture?
The first initiative when offering treatment intervention to patients will be to first create a rapport and win their confidence
before engaging in any medical or palliative care
determines the patient’s response to treatment.
Psychiatric cases require expert handling without with the patient may worsen to
extent of mental damage
2. How can I use what has been learned from this scenario to improve patient care in the
f uture?
The first initiative when offering treatment intervention to patients will be to first create a rapport and win their confidence
before engaging in any medical or palliative care
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
© 2016 Keith Rischer/www.KeithRN.com
References
Beck, A. T., & Alford, B. A. (2009). Depression: Causes and treatment. University of
Pennsylvania Press.
Butcher, H. K., Bulechek, G. M., Dochterman, J. M. M., & Wagner, C. (2018). Nursing
Interventions classification (NIC)-E-Book. Elsevier Health Sciences.
Ernstmann, N., Neumann, M., Ommen, O., Galushko, M., Wirtz, M., Voltz, R., ... & Pfaff, H.
(2009). Determinants and implications of cancer patients’ psychosocial needs. Supportive care in
cancer, 17(11), 1417.
Killeen, P. R., Tannock, R., & Sagvolden, T. (2011). The four causes of ADHD: a
framework. In Behavioral neuroscience of attention deficit hyperactivity disorder and its treatment (pp. 391-
425). Springer, Berlin, Heidelberg.
Lader, M. (2015). Generalized anxiety disorder. In Encyclopedia of
psychopharmacology (pp. 699-702). Springer, Berlin, Heidelberg.
Murray, P., & Barker, D. (2018). C4 An Institutional Comprehensive Pain Assessment:
WILDA Revised. Pain Management Nursing, 19(2), 106.
References
Beck, A. T., & Alford, B. A. (2009). Depression: Causes and treatment. University of
Pennsylvania Press.
Butcher, H. K., Bulechek, G. M., Dochterman, J. M. M., & Wagner, C. (2018). Nursing
Interventions classification (NIC)-E-Book. Elsevier Health Sciences.
Ernstmann, N., Neumann, M., Ommen, O., Galushko, M., Wirtz, M., Voltz, R., ... & Pfaff, H.
(2009). Determinants and implications of cancer patients’ psychosocial needs. Supportive care in
cancer, 17(11), 1417.
Killeen, P. R., Tannock, R., & Sagvolden, T. (2011). The four causes of ADHD: a
framework. In Behavioral neuroscience of attention deficit hyperactivity disorder and its treatment (pp. 391-
425). Springer, Berlin, Heidelberg.
Lader, M. (2015). Generalized anxiety disorder. In Encyclopedia of
psychopharmacology (pp. 699-702). Springer, Berlin, Heidelberg.
Murray, P., & Barker, D. (2018). C4 An Institutional Comprehensive Pain Assessment:
WILDA Revised. Pain Management Nursing, 19(2), 106.
1 out of 11
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.