Law, Policy and Ethical Practice in Health and Social Care
VerifiedAdded on 2023/01/13
|18
|4338
|39
AI Summary
This document explores the legal and policy landscape for health and social care practitioners. It discusses the roles of legislature, executive, and judiciary in setting the framework for healthcare. It also highlights key legislation and its impact on healthcare professionals. The document emphasizes the importance of following laws and regulations in providing fair treatment and maintaining equality in healthcare.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Unit 1 Law, Policy and Ethical Practice in Health and Social
Care.
1
Care.
1
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Contents
Title Page
Alexandra Acute hospital. Redditch 3
Task 1 4
Task 2 8
Task 3 10
Task 4 13
Conclusion 15
References 16
2
Title Page
Alexandra Acute hospital. Redditch 3
Task 1 4
Task 2 8
Task 3 10
Task 4 13
Conclusion 15
References 16
2

Alexandra Acute hospital. Redditch
This booklet is aimed at new healthcare assistants. The booklet explains and defines
the three arms of government which are: the Judiciary, the Executive and Legislature. It will
explain how these three branches with separate powers collaborate in the health and social
care. Alexandra Acute hospital based in Redditch was opened in 1985 and is the major centre
for urology service in the country. It caters for an annual footfall of approximately 200 000
walk-in patients a year and has about 300 beds. The hospital has 8 operating theatres, MRI,
CT scanners and cancer unit status for breast, lung, urology, gynaecology and colorectal
cancers (Worcsacute.nhs.uk)
3
This booklet is aimed at new healthcare assistants. The booklet explains and defines
the three arms of government which are: the Judiciary, the Executive and Legislature. It will
explain how these three branches with separate powers collaborate in the health and social
care. Alexandra Acute hospital based in Redditch was opened in 1985 and is the major centre
for urology service in the country. It caters for an annual footfall of approximately 200 000
walk-in patients a year and has about 300 beds. The hospital has 8 operating theatres, MRI,
CT scanners and cancer unit status for breast, lung, urology, gynaecology and colorectal
cancers (Worcsacute.nhs.uk)
3
TASK 1
Describe how the legislature, the executive and the judiciary set the legal and policy
landscape for health and social care practitioners.
Legislature
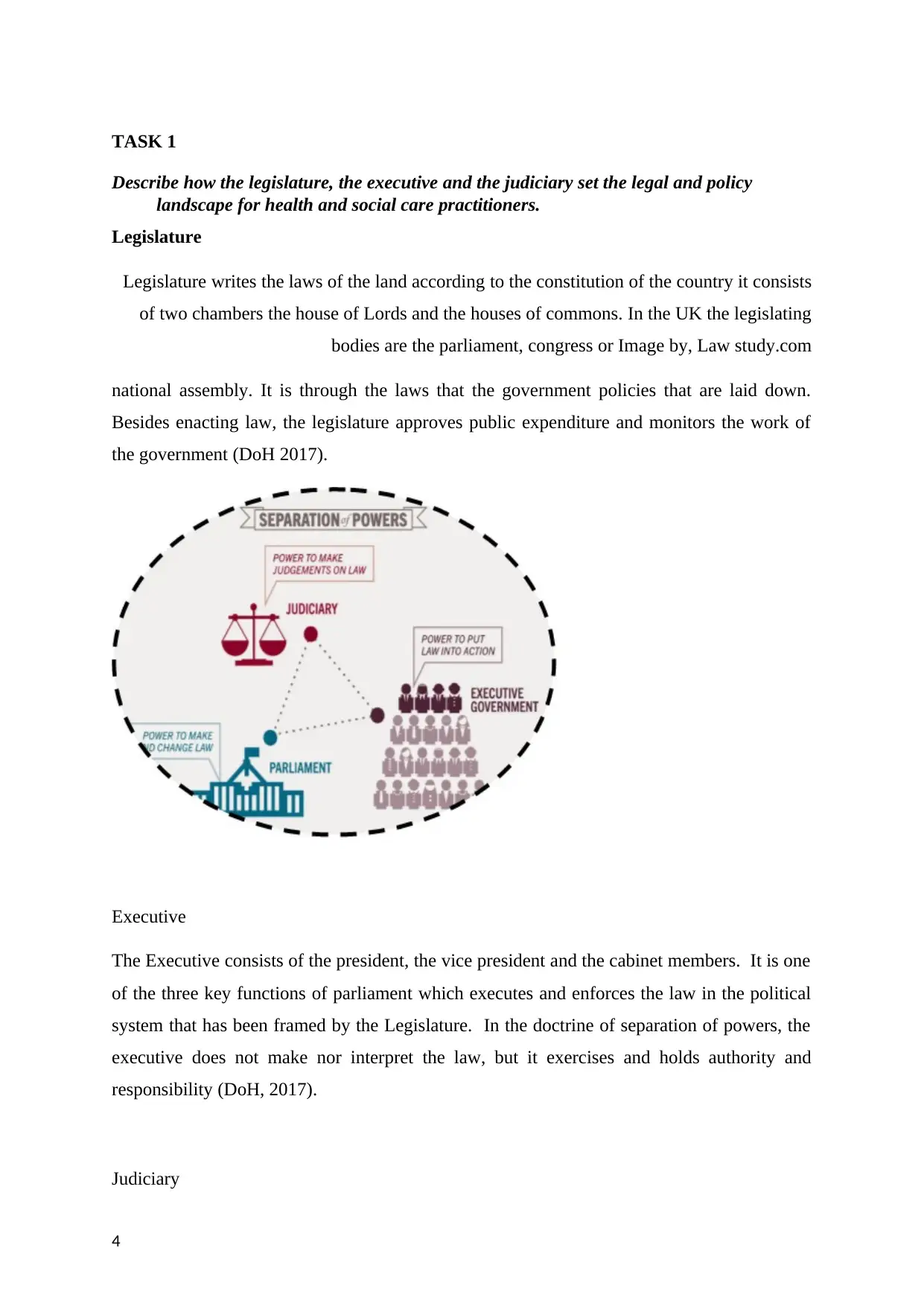
Legislature writes the laws of the land according to the constitution of the country it consists
of two chambers the house of Lords and the houses of commons. In the UK the legislating
bodies are the parliament, congress or Image by, Law study.com
national assembly. It is through the laws that the government policies that are laid down.
Besides enacting law, the legislature approves public expenditure and monitors the work of
the government (DoH 2017).
Executive
The Executive consists of the president, the vice president and the cabinet members. It is one
of the three key functions of parliament which executes and enforces the law in the political
system that has been framed by the Legislature. In the doctrine of separation of powers, the
executive does not make nor interpret the law, but it exercises and holds authority and
responsibility (DoH, 2017).
Judiciary
4
Describe how the legislature, the executive and the judiciary set the legal and policy
landscape for health and social care practitioners.
Legislature
Legislature writes the laws of the land according to the constitution of the country it consists
of two chambers the house of Lords and the houses of commons. In the UK the legislating
bodies are the parliament, congress or Image by, Law study.com
national assembly. It is through the laws that the government policies that are laid down.
Besides enacting law, the legislature approves public expenditure and monitors the work of
the government (DoH 2017).
Executive
The Executive consists of the president, the vice president and the cabinet members. It is one
of the three key functions of parliament which executes and enforces the law in the political
system that has been framed by the Legislature. In the doctrine of separation of powers, the
executive does not make nor interpret the law, but it exercises and holds authority and
responsibility (DoH, 2017).
Judiciary
4
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
These are the courts that interpret and apply the law. This helps to keep the country in order
without people resorting to violence. Different types of cases are dealt with in different
courts. The magistrate court, the high court, the court of appeal and the supreme court of law
for criminal cases. Civil cases are dealt with in the magistrate and county courts. Appeals are
directed to the high court and then court of appeal. The tribunal system has its own structure
that deals with cases and appeals from different chambers e.g. upper tribunal and employers
in the health care system. Legislation.gov.uk, (2017)
Legislature, Executive and Judiciary Functions.
There are three organs of the government, that are formulated as, the parliament is the
legislature and it makes the laws. It works House of Lords and House of Commons.
The executive which compromises the Prime minister and the cabinet enforces the law. The
executive works with 29 agencies including the Care Quality Commission (CQC), controls
health and social care services in United Kingdom. It ensures the quality and safety of care in
ambulances, care homes, in dentists, hospitals including care given in people’s own homes.
The judiciary comprises the courts of law and judges. It applies law to specific cases that are
in breach of the law. It also interprets the law. Legislation.gov.uk, (2017)
The law helps practitioners by protecting them and the people that practitioners look after. It
also helps standardise the care that is provided to vulnerable patients governed by the Care
Quality Commission (CQC 2018). Within an institution when a practitioner does not follow
policies and procedures and something goes wrong, according to CQC, an internal
investigation begins. If there is a need for escalation, the case is investigated externally
which might be done by the CQC and if they don’t give an expected verdict the case is then
taken to court, with the end result of it going in the media. In that instance, the company will
not stand in support of the practitioner at court but, the practitioner will face the charges on
his/her own because you have failed to follow the policies and procedures that the company
has put in place. In the cases that the company has failed to put policies and guidelines in
place then it is the company that might end up in court and being fined large sums of money.
Care Quality Commission (2010)
Key Legislation
5
without people resorting to violence. Different types of cases are dealt with in different
courts. The magistrate court, the high court, the court of appeal and the supreme court of law
for criminal cases. Civil cases are dealt with in the magistrate and county courts. Appeals are
directed to the high court and then court of appeal. The tribunal system has its own structure
that deals with cases and appeals from different chambers e.g. upper tribunal and employers
in the health care system. Legislation.gov.uk, (2017)
Legislature, Executive and Judiciary Functions.
There are three organs of the government, that are formulated as, the parliament is the
legislature and it makes the laws. It works House of Lords and House of Commons.
The executive which compromises the Prime minister and the cabinet enforces the law. The
executive works with 29 agencies including the Care Quality Commission (CQC), controls
health and social care services in United Kingdom. It ensures the quality and safety of care in
ambulances, care homes, in dentists, hospitals including care given in people’s own homes.
The judiciary comprises the courts of law and judges. It applies law to specific cases that are
in breach of the law. It also interprets the law. Legislation.gov.uk, (2017)
The law helps practitioners by protecting them and the people that practitioners look after. It
also helps standardise the care that is provided to vulnerable patients governed by the Care
Quality Commission (CQC 2018). Within an institution when a practitioner does not follow
policies and procedures and something goes wrong, according to CQC, an internal
investigation begins. If there is a need for escalation, the case is investigated externally
which might be done by the CQC and if they don’t give an expected verdict the case is then
taken to court, with the end result of it going in the media. In that instance, the company will
not stand in support of the practitioner at court but, the practitioner will face the charges on
his/her own because you have failed to follow the policies and procedures that the company
has put in place. In the cases that the company has failed to put policies and guidelines in
place then it is the company that might end up in court and being fined large sums of money.
Care Quality Commission (2010)
Key Legislation
5
The Health and Social Care Act 2012 introduced the first legal duties about health
inequalities. It included specific duties for health bodies including the Department of Health,
Public Health England, Clinical Commissioning Groups, and NHS England which require the
bodies to have due regard to reducing health inequalities between the people of England. The
Act also brought in changes for local authorities on public health functions. The Equality Act
2010 established equality duties for all public sector bodies which aim to integrate
consideration of the advancement of equality into the day-to-day business of all bodies
subject to the duty. NHS England has produced a document for NHS commissioners on the
duties covered by both of these Acts. Care Quality Commission (2010)
These pieces of legislation are complementary in setting a framework for the public sector to
act and reduce inequalities within England at local and national levels. National health and
social care legislations are Care standard acts of the parliament in the United Kingdom. It
provides for the administrations of a variety of different care institutions which consist of the
legislation and policies. There are a few national legislations that are in place and these
include Human Rights Act 1998. Policies like dignity, choices, grievance, discrimination are
put in place in the health and social care to allow patients to have fair treatment (Ali et al
2013). When dealing with a service user or giving personal care, it is important always to
seek consent before any medical intervention on their person and also maintaining their
dignity like shutting the door or drawing the curtains. Age UK (2011)
The Health and Safety Act,1974 at work ensures that staff have Personal Protective
Equipment (PPE) and exercise correct manual handling. This covers the correct and safe use
of the manual moving equipment of service users in the institution. It also deals with the
Control of Substances Hazardous to Health (COSHH). This is the safe storage of clearly
labelled chemicals which are carefully stored and kept securely
locked away at all times. The Reporting of Injuries, Diseases,
Dangerous Occurrence Regulations (RIDDOR) is a policy that
demands the documentation and reporting of deaths, sickness
and injuries in the work place. Health and Safety at Work
website, (2018). Image
by HSAW website
6
inequalities. It included specific duties for health bodies including the Department of Health,
Public Health England, Clinical Commissioning Groups, and NHS England which require the
bodies to have due regard to reducing health inequalities between the people of England. The
Act also brought in changes for local authorities on public health functions. The Equality Act
2010 established equality duties for all public sector bodies which aim to integrate
consideration of the advancement of equality into the day-to-day business of all bodies
subject to the duty. NHS England has produced a document for NHS commissioners on the
duties covered by both of these Acts. Care Quality Commission (2010)
These pieces of legislation are complementary in setting a framework for the public sector to
act and reduce inequalities within England at local and national levels. National health and
social care legislations are Care standard acts of the parliament in the United Kingdom. It
provides for the administrations of a variety of different care institutions which consist of the
legislation and policies. There are a few national legislations that are in place and these
include Human Rights Act 1998. Policies like dignity, choices, grievance, discrimination are
put in place in the health and social care to allow patients to have fair treatment (Ali et al
2013). When dealing with a service user or giving personal care, it is important always to
seek consent before any medical intervention on their person and also maintaining their
dignity like shutting the door or drawing the curtains. Age UK (2011)
The Health and Safety Act,1974 at work ensures that staff have Personal Protective
Equipment (PPE) and exercise correct manual handling. This covers the correct and safe use
of the manual moving equipment of service users in the institution. It also deals with the
Control of Substances Hazardous to Health (COSHH). This is the safe storage of clearly
labelled chemicals which are carefully stored and kept securely
locked away at all times. The Reporting of Injuries, Diseases,
Dangerous Occurrence Regulations (RIDDOR) is a policy that
demands the documentation and reporting of deaths, sickness
and injuries in the work place. Health and Safety at Work
website, (2018). Image
by HSAW website
6
Equality Act 2010 protects people from discrimination from employers’ businesses and
organisations that provide goods or services, like banks, shops and utility companies health
and care providers, such as hospitals and care homes housing. (Government Equalities Office
(2010),)
The Mental Health Act 1983 allows compulsory action to be taken, where necessary, to make
sure that people with mental disorders get the care and treatment they need for their own
health or safety, or for the protection of other people. It protects people without mental
capacity and empowers them to make decisions about their care and treatment. Care Act
2014, covers safeguarding and improves well-being and independence. Principles of the Care
Act 2014
The Care Act 2014 encourages caregivers to take a person-centred approach when
safeguarding vulnerable adults. When you follow the principles, you too place the vulnerable
person’s wellbeing and needs at the forefront of safeguarding processes.
They help you directly involve the vulnerable people, and any nominated people who can
help reach decisions in the vulnerable adult’s best interest, when managing safeguarding
concerns and care plans.
The six principles of the Care Act are:
Empowerment.
Protection.
Prevention
Proportionality.
Partnership.
Accountability. Image by, Caring Mind
Most of these policies are regulated by specific bodies which oversee the professional
conduct of practitioners. The umbrella enforcing body is the CQC. The General Medical
Council (GMC) is responsible for doctors, the Nurses and Midwifery Council (NMC)
oversees nurses and midwives. The General dental Council (GDC) is for dentists, Health and
safety Executive enforces workplace health and welfare (Garland 2019)
7
organisations that provide goods or services, like banks, shops and utility companies health
and care providers, such as hospitals and care homes housing. (Government Equalities Office
(2010),)
The Mental Health Act 1983 allows compulsory action to be taken, where necessary, to make
sure that people with mental disorders get the care and treatment they need for their own
health or safety, or for the protection of other people. It protects people without mental
capacity and empowers them to make decisions about their care and treatment. Care Act
2014, covers safeguarding and improves well-being and independence. Principles of the Care
Act 2014
The Care Act 2014 encourages caregivers to take a person-centred approach when
safeguarding vulnerable adults. When you follow the principles, you too place the vulnerable
person’s wellbeing and needs at the forefront of safeguarding processes.
They help you directly involve the vulnerable people, and any nominated people who can
help reach decisions in the vulnerable adult’s best interest, when managing safeguarding
concerns and care plans.
The six principles of the Care Act are:
Empowerment.
Protection.
Prevention
Proportionality.
Partnership.
Accountability. Image by, Caring Mind
Most of these policies are regulated by specific bodies which oversee the professional
conduct of practitioners. The umbrella enforcing body is the CQC. The General Medical
Council (GMC) is responsible for doctors, the Nurses and Midwifery Council (NMC)
oversees nurses and midwives. The General dental Council (GDC) is for dentists, Health and
safety Executive enforces workplace health and welfare (Garland 2019)
7
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
M1.
In present scenario, healthcare practitioner plays the crucial role where they simply
have to perform the duty through which they can cure any of the patient. Talking about the
ethical code and conducts, it simply guides the practitioner that how patient can recover for
their health issues. In addition, code of ethics say that any of the practitioner is not allowed to
take any of those decision which can create issues for patient. For example: If patient is not
willing to share his or her medical issues with any of the other person then, in that respective
situation practitioner is not allowed to disclose any of the information.
D1.
In any of the nation role of government increases automatically as they are the one who
decides that how any of the work is required to be done. While talking about the UK, their
government has formed number of laws and regulation which are very effective in current
period of time. The main motive behind the formation of law is just to ensure that all of the
people will get fair treatment. For example: NHS has formed the law that in any of the
situation any of the practitioner will not be allowed to disclose any of the information related
to patient which will not allow other person to point out any of question against any of the
respective patient. It is one of the example which shows that there is a huge involvement
within the healthcare for positive outcomes.
8
In present scenario, healthcare practitioner plays the crucial role where they simply
have to perform the duty through which they can cure any of the patient. Talking about the
ethical code and conducts, it simply guides the practitioner that how patient can recover for
their health issues. In addition, code of ethics say that any of the practitioner is not allowed to
take any of those decision which can create issues for patient. For example: If patient is not
willing to share his or her medical issues with any of the other person then, in that respective
situation practitioner is not allowed to disclose any of the information.
D1.
In any of the nation role of government increases automatically as they are the one who
decides that how any of the work is required to be done. While talking about the UK, their
government has formed number of laws and regulation which are very effective in current
period of time. The main motive behind the formation of law is just to ensure that all of the
people will get fair treatment. For example: NHS has formed the law that in any of the
situation any of the practitioner will not be allowed to disclose any of the information related
to patient which will not allow other person to point out any of question against any of the
respective patient. It is one of the example which shows that there is a huge involvement
within the healthcare for positive outcomes.
8
Task2
9
9
10
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Task 3
P5.
In recent time period, I was working for Airdri Ltd, which is one of the manufacturing
organisation. It was the organisation where I was given the responsibility to manage the team
of 15 workers. Suddenly, one day a accident took place just because of the failure of
machineries. According to the laws and regulation, I had been taken to hospital and compete
payment was made by the side of organisation as per the law. The main reason of doing the
final payment within the hospital from the side of organisation was necessary because the
place of accident was within the premisses of organisation. In addition, various benefits will
be provided such as National Health Service Injury benefit. Here, laws like Care Standard
Act, 2000 & Community Care Direct Payment Act, 1996 will be also applicable. All of this
laws will allow to deliver the human rights as per the criteria set by international level.
It is one of the case where legal laws has been followed as a greater level which has
allowed them to maintain the level of equality within the premisses of an organisation. As
employee got injured within the premisses of organisation and it was found that no
discrimination had been done from the side of business organisation. All of the required steps
has been considered so that health level can be improved as soon as possible which shows
11
P5.
In recent time period, I was working for Airdri Ltd, which is one of the manufacturing
organisation. It was the organisation where I was given the responsibility to manage the team
of 15 workers. Suddenly, one day a accident took place just because of the failure of
machineries. According to the laws and regulation, I had been taken to hospital and compete
payment was made by the side of organisation as per the law. The main reason of doing the
final payment within the hospital from the side of organisation was necessary because the
place of accident was within the premisses of organisation. In addition, various benefits will
be provided such as National Health Service Injury benefit. Here, laws like Care Standard
Act, 2000 & Community Care Direct Payment Act, 1996 will be also applicable. All of this
laws will allow to deliver the human rights as per the criteria set by international level.
It is one of the case where legal laws has been followed as a greater level which has
allowed them to maintain the level of equality within the premisses of an organisation. As
employee got injured within the premisses of organisation and it was found that no
discrimination had been done from the side of business organisation. All of the required steps
has been considered so that health level can be improved as soon as possible which shows
11
that human rights by the company has been considered at a national and international level.
Additional, it can be said that international human right has enforced that each of the person
should be treated equal as it falls under the category of human rights. This international laws
says that environment should be diversified where all of the person should get equal rights
that how they are needed to perform any of their work. In any of the situation, it is necessary
to understand that the main purpose of providing fair treatment each of the person is very
simply which means that every has the right to improve their health where practitioner must
treat them equally.
P6.
In current scenario, laws and regulations plays the crucial role as guidelines can be
provided easily in it. For the purpose of delivering of safe & healthy social care facility, it is
essential that they must follow different laws and regulations.
Health and Social Care Act, 2012: It is among one of those law which simply
explains about the duty and roles of each and every medical practitioner because it is one of
the way through which equality can be introduced in the sector of fair treatment to every
individual. Power is given to local body where they are required to commence new policies
through which equality can be delivered with in the organisation. It will enhance the outcome
for patient as they will get better opportunity for fair treatment.
Social value Act, 2012: It is the act where major focus is on the development of
healthcare facility in context of economic, social and environmental connection. The main
area which laws focus is that treatment for patient should be based on local the background
which they belong because it will directly allow to reduce the chances of inequality.
In present scenario, any of the policies which are being formed on daily basis for the
better healthcare facility of patient, it will be necessary that they must be formed by giving
focus on international level of laws and policies.
M3
In current situation, laws and regulations are being changed on a regular basis where
major focus is on the guidelines which is being provided to practitioner. Different laws and
legalisation are being formed for practitioner and they are needed to consider them. The law
says that it is the responsibility of that practitioner to provide detail to patient as per the
guidelines of right to practitioner. Also, it is essential that whenever any of the changes occur
12
Additional, it can be said that international human right has enforced that each of the person
should be treated equal as it falls under the category of human rights. This international laws
says that environment should be diversified where all of the person should get equal rights
that how they are needed to perform any of their work. In any of the situation, it is necessary
to understand that the main purpose of providing fair treatment each of the person is very
simply which means that every has the right to improve their health where practitioner must
treat them equally.
P6.
In current scenario, laws and regulations plays the crucial role as guidelines can be
provided easily in it. For the purpose of delivering of safe & healthy social care facility, it is
essential that they must follow different laws and regulations.
Health and Social Care Act, 2012: It is among one of those law which simply
explains about the duty and roles of each and every medical practitioner because it is one of
the way through which equality can be introduced in the sector of fair treatment to every
individual. Power is given to local body where they are required to commence new policies
through which equality can be delivered with in the organisation. It will enhance the outcome
for patient as they will get better opportunity for fair treatment.
Social value Act, 2012: It is the act where major focus is on the development of
healthcare facility in context of economic, social and environmental connection. The main
area which laws focus is that treatment for patient should be based on local the background
which they belong because it will directly allow to reduce the chances of inequality.
In present scenario, any of the policies which are being formed on daily basis for the
better healthcare facility of patient, it will be necessary that they must be formed by giving
focus on international level of laws and policies.
M3
In current situation, laws and regulations are being changed on a regular basis where
major focus is on the guidelines which is being provided to practitioner. Different laws and
legalisation are being formed for practitioner and they are needed to consider them. The law
says that it is the responsibility of that practitioner to provide detail to patient as per the
guidelines of right to practitioner. Also, it is essential that whenever any of the changes occur
12
with the medical services it should be well informed for effective outcomes. The recent
changes in HSCS where they mainly focuses on the setting of regulations and care where
involvement of social care will be necessity.
D3
It is essential for each and every practitioner that they must taken any of the decision
by reviewing each and every activity in a systematic manner. As per the recent changes of
Health and Social Care Standards, it simply explains that it is the responsibilities of
practitioner that they must take any of the action according to the legal laws and regulations.
Also, medical laws can ensure that which types of medicines must be given to patient
whenever they suffers from any of the problem. This are some of the important criteria which
helps practitioner to take and review that correct compliances has been followed for effective
result. All this will allow them to generate healthy revenue and goodwill can also be
developed through which name can be develop for future period of time.
Task 4
Law, policy and ethics on many occasions have always not agreed, but comprise has worked
and sometimes the law supersedes ethics.
James (not his real name) was a 73-year-old man who lived alone, but was admitted to the
local elderly mental health assessment unit after being found wandering along a main road at
one o’clock in the morning. He was very confused and agitated, dehydrated, malnourished
and showing some signs of poor short-term memory function. He had been prescribed
medication in the form of a syrup to reduce his agitation. At the beginning he was happy to
take the medication.
During handover, the ward manager, Carol, told the staff nurse to put the syrup in James’ cup
of coffee. This was the correct ethical procedure. Nurses can help patients to exercise their
autonomy and provide them with information they need to make informed choices consistent
with their interests and goals (Tingle and Cribb 2002). Autonomy is one of the ethical
principles in nursing. Gillon (1994) contends that autonomy means the capacity to think,
decide and act on the basis of such thought and decision freely and independently without
hindrance. Therefore, the nurse felt it was her duty to give James chance to earn and
understand more about the treatment he was about to undertake, thus playing the role of an
educator. She acted as an advocate to the patient by deciding what she should be disclosed.
13
changes in HSCS where they mainly focuses on the setting of regulations and care where
involvement of social care will be necessity.
D3
It is essential for each and every practitioner that they must taken any of the decision
by reviewing each and every activity in a systematic manner. As per the recent changes of
Health and Social Care Standards, it simply explains that it is the responsibilities of
practitioner that they must take any of the action according to the legal laws and regulations.
Also, medical laws can ensure that which types of medicines must be given to patient
whenever they suffers from any of the problem. This are some of the important criteria which
helps practitioner to take and review that correct compliances has been followed for effective
result. All this will allow them to generate healthy revenue and goodwill can also be
developed through which name can be develop for future period of time.
Task 4
Law, policy and ethics on many occasions have always not agreed, but comprise has worked
and sometimes the law supersedes ethics.
James (not his real name) was a 73-year-old man who lived alone, but was admitted to the
local elderly mental health assessment unit after being found wandering along a main road at
one o’clock in the morning. He was very confused and agitated, dehydrated, malnourished
and showing some signs of poor short-term memory function. He had been prescribed
medication in the form of a syrup to reduce his agitation. At the beginning he was happy to
take the medication.
During handover, the ward manager, Carol, told the staff nurse to put the syrup in James’ cup
of coffee. This was the correct ethical procedure. Nurses can help patients to exercise their
autonomy and provide them with information they need to make informed choices consistent
with their interests and goals (Tingle and Cribb 2002). Autonomy is one of the ethical
principles in nursing. Gillon (1994) contends that autonomy means the capacity to think,
decide and act on the basis of such thought and decision freely and independently without
hindrance. Therefore, the nurse felt it was her duty to give James chance to earn and
understand more about the treatment he was about to undertake, thus playing the role of an
educator. She acted as an advocate to the patient by deciding what she should be disclosed.
13
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
However, on the other hand there is the principle of
beneficence (Bloch etal 1991). This principle
conflicts with the principle of autonomy in the sense
that by acting in the client’s best interest NMC code
of professional conduct one would be depriving the
client to have option. The principle of beneficence
requires nurses to help others to further their important
legitimate interests often by preventing or removing
possible harm. (Bloch etal 1991).
Although James was well informed about his medication he did not fully comprehend.
Reeves and Orford (2007) state that a person with a mental disorder is not autonomous,
meaning that they cannot govern themselves. This meant that James’ autonomy was taken
away and, in that health, professionals acted paternalistic. Paternalism refers to treating or
acting using your judgement to the best interest of someone, limiting or overriding someone’s
autonomy. Paternalism involves force. James was observed and detained without his consent.
His freedom of choice was taken away from him (Dimond 1990).
A person can be compulsorily detained for treatment, health and safety and for their
protection and others. It appears that James was not fully given options due to his personal
care. It is therefore evident that health professionals do not give all the information, however,
the ethical principle of autonomy puts emphasis on an individual's right to choose their
preferred care (Beauchamp and Childress,1994) Disclosing certain forms of information can
cause harm to patients. However, on the other hand Hendricks (2002) argues that we should
ensure that people are able to make informed decisions and be self-determining. In James’s
case, there is clear evidence that there was duty of care when he was put under observation
for his own good and to prevent harm.
Hendricks (2000), states that the duty of care creates moral obligations to act in ways that
promote a service user's wellbeing and autonomy. This is non-malfeasance. According to
Beauchamp and Childress (1994) non-malfeasance is seen as an act of not doing any harm.
However, they go on to argue that it is justifiable to override non-malfeasance in mental
health situations, meaning it is justifiable to harm someone by compulsorily detaining them
so as to protect the society at large. In James’ incident the duty of non-malfeasance is seen as
14
beneficence (Bloch etal 1991). This principle
conflicts with the principle of autonomy in the sense
that by acting in the client’s best interest NMC code
of professional conduct one would be depriving the
client to have option. The principle of beneficence
requires nurses to help others to further their important
legitimate interests often by preventing or removing
possible harm. (Bloch etal 1991).
Although James was well informed about his medication he did not fully comprehend.
Reeves and Orford (2007) state that a person with a mental disorder is not autonomous,
meaning that they cannot govern themselves. This meant that James’ autonomy was taken
away and, in that health, professionals acted paternalistic. Paternalism refers to treating or
acting using your judgement to the best interest of someone, limiting or overriding someone’s
autonomy. Paternalism involves force. James was observed and detained without his consent.
His freedom of choice was taken away from him (Dimond 1990).
A person can be compulsorily detained for treatment, health and safety and for their
protection and others. It appears that James was not fully given options due to his personal
care. It is therefore evident that health professionals do not give all the information, however,
the ethical principle of autonomy puts emphasis on an individual's right to choose their
preferred care (Beauchamp and Childress,1994) Disclosing certain forms of information can
cause harm to patients. However, on the other hand Hendricks (2002) argues that we should
ensure that people are able to make informed decisions and be self-determining. In James’s
case, there is clear evidence that there was duty of care when he was put under observation
for his own good and to prevent harm.
Hendricks (2000), states that the duty of care creates moral obligations to act in ways that
promote a service user's wellbeing and autonomy. This is non-malfeasance. According to
Beauchamp and Childress (1994) non-malfeasance is seen as an act of not doing any harm.
However, they go on to argue that it is justifiable to override non-malfeasance in mental
health situations, meaning it is justifiable to harm someone by compulsorily detaining them
so as to protect the society at large. In James’ incident the duty of non-malfeasance is seen as
14
causing harm intentionally because during handover staff were not fully informed about the
treatment as expected by the law. By intentionally doing this they breached the duty of non-
malfeasance.
Furthermore, looking at the legal principle, this can be described as negligence (Beauchamp
et al 1994). In most situations when faced with a moral dilemma, people almost act according
to their own set of rules and values. A nurse is under legal duty to act carefully towards
patients. If a nurse fails to exercise sufficient care, and by so doing causes injury or harm to
the patient they will be held liable in the tort of negligence. Michele and Tingle (2003)
further explain that a nurse is not negligent if she acts in accordance with a practice accepted
as proper by a responsible body of nursing opinion. Policies and procedures enforce the law
and guidelines pertaining to mental health. In this case the nurse did her duty by informing
the patient about his medication to meet the individual needs concerned.
15
treatment as expected by the law. By intentionally doing this they breached the duty of non-
malfeasance.
Furthermore, looking at the legal principle, this can be described as negligence (Beauchamp
et al 1994). In most situations when faced with a moral dilemma, people almost act according
to their own set of rules and values. A nurse is under legal duty to act carefully towards
patients. If a nurse fails to exercise sufficient care, and by so doing causes injury or harm to
the patient they will be held liable in the tort of negligence. Michele and Tingle (2003)
further explain that a nurse is not negligent if she acts in accordance with a practice accepted
as proper by a responsible body of nursing opinion. Policies and procedures enforce the law
and guidelines pertaining to mental health. In this case the nurse did her duty by informing
the patient about his medication to meet the individual needs concerned.
15
Conclusion
Finally, in conclusion, its vital to note that, the life of a healthcare provider is very
important in their life and its critically important that they apply the law where its relevant.
There is a wide range of contradiction between law and ethics which requires rationale
application by care providers and a holistic approach to ensure the patient receives utmost
care they require. Induction for any new staff must be done efficiently and effectively at the
earliest opportunity so that they hit the ground running and making sure there is little or no
disruption on the ongoing work by providers.
References
Addicott, R. and Ashton, R., eds. (2010). 'Delivering better care at end of life: The next
steps.' London: The King's Fund.
16
Finally, in conclusion, its vital to note that, the life of a healthcare provider is very
important in their life and its critically important that they apply the law where its relevant.
There is a wide range of contradiction between law and ethics which requires rationale
application by care providers and a holistic approach to ensure the patient receives utmost
care they require. Induction for any new staff must be done efficiently and effectively at the
earliest opportunity so that they hit the ground running and making sure there is little or no
disruption on the ongoing work by providers.
References
Addicott, R. and Ashton, R., eds. (2010). 'Delivering better care at end of life: The next
steps.' London: The King's Fund.
16
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
Age UK (2011) Older People and Human Rights: a reference guide for professionals working
with older people
Billings, J. A. (2008). 'Dignity.' Journal of Palliative Medicine 11(2): 138–9.
Birrell, J., Thomas, D. & Jones, C. A. (2006) 'Promoting privacy and dignity for older
patients in hospital'. Nursing Standard 20 41–46.
Beauchamp, T. and Childress (2014) Principles of Biomedical Ethics. (4thedition), Oxford
University press. New York.
Bloch, S. (2013) An Introduction to Psychotherapies. (3rd edition) Oxford Medical
Publications, New York.
‘Changing Lives’ The British Institute for Human Rights, report (2008)
Dimond, B. (2015) Legal Aspects of Nursing. London
Caring Mind (20141). Available on https://caringmindblog.com/2017/08/27/the-care-act-
2014/, Cited on 17 Dec 2019
Chochinov, H. (2017). 'Dignity and the essence of medicine – the A, B, C, and D of dignity
conserving care.' British Medical Journal 335(7612): pp 184–187.
Clark, A. (2009). 'Ageism and age discrimination in social care in the United Kingdom. A
review from the literature.' Centre for Policy on Ageing.
Department of Health (2010) Our health, our care, our say: a new direction for community
services. London, The Stationery Office, HM Government.
Department of Health (2010) Essence of care benchmarks for promoting health.
Department of Health (2007v). Review of the Health Inequalities Infant Mortality PSA
Target. London:
Diamond, B (2015) Legal aspects of nursing.4th edition, Harlow: Pearson Education Limited.
Garland, C. (2019) The Health and safety executive first aid bulletin 26th July 2019.
Gillon R. (2015) Principles of Health Care Ethics, Chichester: John Wiley.
Government Equalities Office (2010), Equality Act 2010: What Do I Need To Know?
Disability Quick Start Guide, Crown Copyright.
17
with older people
Billings, J. A. (2008). 'Dignity.' Journal of Palliative Medicine 11(2): 138–9.
Birrell, J., Thomas, D. & Jones, C. A. (2006) 'Promoting privacy and dignity for older
patients in hospital'. Nursing Standard 20 41–46.
Beauchamp, T. and Childress (2014) Principles of Biomedical Ethics. (4thedition), Oxford
University press. New York.
Bloch, S. (2013) An Introduction to Psychotherapies. (3rd edition) Oxford Medical
Publications, New York.
‘Changing Lives’ The British Institute for Human Rights, report (2008)
Dimond, B. (2015) Legal Aspects of Nursing. London
Caring Mind (20141). Available on https://caringmindblog.com/2017/08/27/the-care-act-
2014/, Cited on 17 Dec 2019
Chochinov, H. (2017). 'Dignity and the essence of medicine – the A, B, C, and D of dignity
conserving care.' British Medical Journal 335(7612): pp 184–187.
Clark, A. (2009). 'Ageism and age discrimination in social care in the United Kingdom. A
review from the literature.' Centre for Policy on Ageing.
Department of Health (2010) Our health, our care, our say: a new direction for community
services. London, The Stationery Office, HM Government.
Department of Health (2010) Essence of care benchmarks for promoting health.
Department of Health (2007v). Review of the Health Inequalities Infant Mortality PSA
Target. London:
Diamond, B (2015) Legal aspects of nursing.4th edition, Harlow: Pearson Education Limited.
Garland, C. (2019) The Health and safety executive first aid bulletin 26th July 2019.
Gillon R. (2015) Principles of Health Care Ethics, Chichester: John Wiley.
Government Equalities Office (2010), Equality Act 2010: What Do I Need To Know?
Disability Quick Start Guide, Crown Copyright.
17
Hendrick, J. (2009) Law and Ethics in Nursing and Health Care, Cheltenham: Nelson
Thomas.
Healthcare Commission, Audit Commission & Commission for Social Care Inspection
(2010) Good practice in services for older people (434kb PDF file)
Law Study .com. available on http://thelawstudy.blogspot.com/2014/11/separation-of-
powers-in-british.html. Cited 18 Dec 2019.
Michele, J. Fox, M (2013) Health Care Law: Text material, (2nd edition) London: Sweet and
Maxwell.
Nursing and Midwifery Council (2077) Code of Professional Practice: London
Royal College of Physicians. (2017). 'Assessment of pain in older people. National
guidelines.' Concise guidance to good practice 4th edition: Harlow Longman.
The Care Quality Commission (2010) Essential Standards of Quality and Safety
The Health and Safety at Work etc. Act 1974, Available at:
http://www.legislation.gov.uk/ukpga/1974/37/contents (Accessed 26 April 2017)
The Care Quality Commission (2010) Essential Standards of Quality and Safety
Available on www.house.government,house.co.uk. Cited 16 Dec 2019
http://rcnhca.org.uk/equality-diversity-and-rights/anti-discriminatory-practice/. Cited 2 Dec
2019
Thompson, T and Matthias, P. (2000) Lytle’s Mental Health Disorder (3rd edition)
18
Thomas.
Healthcare Commission, Audit Commission & Commission for Social Care Inspection
(2010) Good practice in services for older people (434kb PDF file)
Law Study .com. available on http://thelawstudy.blogspot.com/2014/11/separation-of-
powers-in-british.html. Cited 18 Dec 2019.
Michele, J. Fox, M (2013) Health Care Law: Text material, (2nd edition) London: Sweet and
Maxwell.
Nursing and Midwifery Council (2077) Code of Professional Practice: London
Royal College of Physicians. (2017). 'Assessment of pain in older people. National
guidelines.' Concise guidance to good practice 4th edition: Harlow Longman.
The Care Quality Commission (2010) Essential Standards of Quality and Safety
The Health and Safety at Work etc. Act 1974, Available at:
http://www.legislation.gov.uk/ukpga/1974/37/contents (Accessed 26 April 2017)
The Care Quality Commission (2010) Essential Standards of Quality and Safety
Available on www.house.government,house.co.uk. Cited 16 Dec 2019
http://rcnhca.org.uk/equality-diversity-and-rights/anti-discriminatory-practice/. Cited 2 Dec
2019
Thompson, T and Matthias, P. (2000) Lytle’s Mental Health Disorder (3rd edition)
18
1 out of 18
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.




