Assessment 1: Developing a COPD Care Plan in UR250, Semester 1, 2019
VerifiedAdded on 2023/01/16
|11
|4987
|99
Report
AI Summary
This report focuses on the holistic care of a 44-year-old male patient, Mr. Peter Newman, admitted to the hospital with an infective exacerbation of Chronic Obstructive Pulmonary Disease (COPD). The assignment requires the application of the clinical reasoning cycle to develop and plan nursing care. The report begins with a consideration of the patient's condition, highlighting the impact of smoking and occupational exposure on COPD. It then identifies and explains three priority nursing assessments, including respiration rate, spirometry, and arterial blood gas measurement. The report proceeds to identify three priority nursing diagnoses, emphasizing airway clearance, breathing pattern improvement, and activity tolerance. For each nursing diagnosis, relevant interventions are proposed, such as medication therapy, breathing exercises, and oxygen therapy. The report also includes evaluations to assess the effectiveness of the interventions. The report adheres to APA 6th referencing style, providing a comprehensive approach to the care of a patient with COPD.
UR250 Medical Surgical Nursing 2Assessment 1 Semester 1 2019
Description/Focus: Care of the person with a medical condition
Value: 40%
Due date: Friday 12th April 2019 by 1300 ACST
Length: 1800 - 2000 words
This assignment requires you to focus on the holistic care of a patient admitted to
hospital with an acute presentation of a chronic condition and to demonstrate your
ability to apply the clinical reasoning cycle to develop and plan nursing care.
Select one of the following case scenarios:
Mr. Peter Newman is a 44-year-old man admitted to the ward with infective
exacerbation of Chronic Obstructive Pulmonary Disease (COPD). Mr Newman is a heavy
smoker and social drinker. Mr Newman is a Fly-In-Fly-Out (FIFO) truck driver with a
remote mining company and is finding it difficult to meet work responsibilities due to
increasing breathlessness.
Mr Newman lives with his wife Marcy and 2 teenage children in a southern capital city and
works a 2 weeks on/2 weeks off roster.
Or
Miss Violet Paterson is a 77-year-old woman admitted to the ward following an Acute
Myocardial Infarction (AMI). Miss Paterson is currently in a stable condition. She has a
history of primary hypertension and longstanding osteoarthritis. Over the last few
months the arthritic pain has increased significantly, and both her blood pressure and
osteoarthritis are impacting on her ability to meet her daily living needs. Miss Paterson
lives alone in an apartment on the 3rd floor (with no lift access) with her cat Molly and
has no extended family.
1
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
Description/Focus: Care of the person with a medical condition
Value: 40%
Due date: Friday 12th April 2019 by 1300 ACST
Length: 1800 - 2000 words
This assignment requires you to focus on the holistic care of a patient admitted to
hospital with an acute presentation of a chronic condition and to demonstrate your
ability to apply the clinical reasoning cycle to develop and plan nursing care.
Select one of the following case scenarios:
Mr. Peter Newman is a 44-year-old man admitted to the ward with infective
exacerbation of Chronic Obstructive Pulmonary Disease (COPD). Mr Newman is a heavy
smoker and social drinker. Mr Newman is a Fly-In-Fly-Out (FIFO) truck driver with a
remote mining company and is finding it difficult to meet work responsibilities due to
increasing breathlessness.
Mr Newman lives with his wife Marcy and 2 teenage children in a southern capital city and
works a 2 weeks on/2 weeks off roster.
Or
Miss Violet Paterson is a 77-year-old woman admitted to the ward following an Acute
Myocardial Infarction (AMI). Miss Paterson is currently in a stable condition. She has a
history of primary hypertension and longstanding osteoarthritis. Over the last few
months the arthritic pain has increased significantly, and both her blood pressure and
osteoarthritis are impacting on her ability to meet her daily living needs. Miss Paterson
lives alone in an apartment on the 3rd floor (with no lift access) with her cat Molly and
has no extended family.
1
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
UR250 Medical Surgical Nursing 2Assessment 1 Semester 1 2019
Based on the information provided in the above case scenarios complete the following
tasks.
Task 1. Consider the patient
What will you consider when preparing the care plan for your chosen patient?
Clinical reasoning process can be explained as the cognitive process where the healthcare
professionals are seen to utilize both the formal as well as the informal thinking strategies for
gathering as well as analysing the patient information. Studies opine that this study is reliant on the
healthcare professionals that use both the intuition as well as the knowledge that influence the
decision-making for individual client circumstances (Weldam et al., 2017). The first step would be
collecting important cues and analyzing the symptoms presented to the healthcare center by Peter.
Peter is a 44 year old man who lives with his wife and two teenage children and has the occupation
of a Fly-In-Fly-Out (FIFO) truck driver on 2 weeks on/2 weeks off roster. He had been admitted to the
ward with the condition of exacerbated Chronic Obstructive Pulmonary Disease (COPD). He is a
heavy smoker as well as a social drinker and works in the remote mining company. He is presently
suffering issues at work because of the symptoms of increased breathlessness.
Studies are of the opinion that excessive smoking can be one of the most important risk
factor that increases the chance of occurrence of COPD among the patients (Weldam et al., 2015).
Peter is suffering from symptoms of COPD and he is also a smoker. Hence, nurses would first need to
know how Peter’s habit of smoking is exposing him to COPD occurrence. Under abnormal condition,
during the time of breathing, oxygen from the air is seen to travel through the windpipe and
ultimately into the bronchioles from which it moves to the alveoli. These are minuscule clusters of
air sacs, which allow the oxygen to get diffuse into its capillaries and from this region to different
parts of the body (Kaufman, 2013). Accordingly, carbon dioxide is seen to be transported from the
capillaries into the alveoli by being collected from different parts of the body from which it is
removed during exhalation. The elasticity of the air sacs mainly helps in the exchange to occur in a
smooth manner. However, in people like Peter, who are regular smokers, cigarette smokes affect the
physiology of the lungs affecting this entire process of gaseous exchange. Cigarette smokes contain
of harmful toxins that affect the lung functionality as they result in severe lung irritation that triggers
the onset of the disorder and hence Peter is also seen to be suffering from the symptoms of COPD.
With time, the lung becomes more and more damaged causing inflammation as well as degradation
affecting respiration (Rodgers et al., 2018). Hence, Peter was seen to suffer from breathless as easy
exchange of gases was disrupted in him. This allows less air in and out of the airways because of four
important occurrences. These are stiffening of the air sacs, deterioration of the walls between the air
sacs, inflammation as well as thickening of the airway walls and increased production of mucus in
the airways causing air obstruction (ANMJ, 2018). Studies also opine that occupational exposure to
dusts as well as chemicals also increase the risk for COPD. Long term exposure to different types of
chemical fumes, vapors as well as dusts in the workplace can irritate as well as inflame the lungs
2
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
Based on the information provided in the above case scenarios complete the following
tasks.
Task 1. Consider the patient
What will you consider when preparing the care plan for your chosen patient?
Clinical reasoning process can be explained as the cognitive process where the healthcare
professionals are seen to utilize both the formal as well as the informal thinking strategies for
gathering as well as analysing the patient information. Studies opine that this study is reliant on the
healthcare professionals that use both the intuition as well as the knowledge that influence the
decision-making for individual client circumstances (Weldam et al., 2017). The first step would be
collecting important cues and analyzing the symptoms presented to the healthcare center by Peter.
Peter is a 44 year old man who lives with his wife and two teenage children and has the occupation
of a Fly-In-Fly-Out (FIFO) truck driver on 2 weeks on/2 weeks off roster. He had been admitted to the
ward with the condition of exacerbated Chronic Obstructive Pulmonary Disease (COPD). He is a
heavy smoker as well as a social drinker and works in the remote mining company. He is presently
suffering issues at work because of the symptoms of increased breathlessness.
Studies are of the opinion that excessive smoking can be one of the most important risk
factor that increases the chance of occurrence of COPD among the patients (Weldam et al., 2015).
Peter is suffering from symptoms of COPD and he is also a smoker. Hence, nurses would first need to
know how Peter’s habit of smoking is exposing him to COPD occurrence. Under abnormal condition,
during the time of breathing, oxygen from the air is seen to travel through the windpipe and
ultimately into the bronchioles from which it moves to the alveoli. These are minuscule clusters of
air sacs, which allow the oxygen to get diffuse into its capillaries and from this region to different
parts of the body (Kaufman, 2013). Accordingly, carbon dioxide is seen to be transported from the
capillaries into the alveoli by being collected from different parts of the body from which it is
removed during exhalation. The elasticity of the air sacs mainly helps in the exchange to occur in a
smooth manner. However, in people like Peter, who are regular smokers, cigarette smokes affect the
physiology of the lungs affecting this entire process of gaseous exchange. Cigarette smokes contain
of harmful toxins that affect the lung functionality as they result in severe lung irritation that triggers
the onset of the disorder and hence Peter is also seen to be suffering from the symptoms of COPD.
With time, the lung becomes more and more damaged causing inflammation as well as degradation
affecting respiration (Rodgers et al., 2018). Hence, Peter was seen to suffer from breathless as easy
exchange of gases was disrupted in him. This allows less air in and out of the airways because of four
important occurrences. These are stiffening of the air sacs, deterioration of the walls between the air
sacs, inflammation as well as thickening of the airway walls and increased production of mucus in
the airways causing air obstruction (ANMJ, 2018). Studies also opine that occupational exposure to
dusts as well as chemicals also increase the risk for COPD. Long term exposure to different types of
chemical fumes, vapors as well as dusts in the workplace can irritate as well as inflame the lungs
2
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
UR250 Medical Surgical Nursing 2Assessment 1 Semester 1 2019
(Kyngas et al., 2017). He works in a mining company and thereby he might be also exposed to coal
dusts and other fumes that have added to the exacerbation of the condition.
Task 2. Nursing assessments
Identify three (3) nursing assessments you will conduct and explain why they are a priority for you.
The nursing diagnosis should try to identify the highest nursing priorities so that the
professional can provide direct care to the patients. For Peter, the nurse should first try to measure
his respiration rate. The respiration rate measurement as a part of the vital sign measurement also
needs to be conducted. The respiration rate is the number of breaths taken by the patient in one
minute. This rate is mainly measured when an individual would be at rest. This would simply involve
counting the total number of times the chest would rise (Fitzsimmons et al., 2016). Normal
respiration rate for the adult persons are usually 12 to 16 breaths per minute. Changes in the
respiratory rate is found to be associated with asthma, anxiety, congestive heart failure, pneumonia,
lung disorder as well as the use of narcotics. Therefore, this should be the first assessment needed
to find out whether any such disorders are present in Peter or not. If the rate is found to be high in
Peter, then the following assessments are to be done.
For Peter, Spirometry test should also be conducted to develop about his conditions of the
lungs as Peter is suspected to be suffering from COPD. Spirometry is one of the diagnostic tools of
choice and helps in measuring the obstruction of the airflow. These tests are seen to include forced
expiratory volume in the first second (FEV1) and forced vital capacity (FVC). These have been found
to help in reflecting the changes in the lung volume from that of the total lung capacity through the
sustained expiration to residual volume (Moreira et al., 2017). The nurse would then try to calculate
the ratio of expired volume to vital capacity (FEV1/FVC). The normal ratio of FEV1/FVC should be
about 705 of greater than this. A lower ratio is mainly seen to indicate the airflow obstruction and is
considered to be the sensitive indicator for the COPD. Studies have also stated that the absolute
FEV1 found in the setting of that of the reduced FEV1/FVC ratio is mainly expressed as a percentage
of the predicted value. This can be helpful of the professional in assessing the severity of the
disorder (The Lung Foundation, 2018). Hence, the nurse attending Peter should first conduct the test
that would show the change the lung volume from total lung capacity and assess its severity.
Another diagnostic test that should be also conducted for Peter is the arterial blood gas
measurement. This measurement can help by providing information about the alteration of Ph as
well as hypercapnia, hypocapnia as well as hypoxia in Peter. This test is found to be useful in the
evaluation of acute dyspnea. They are also found to be helpful in the cases of diagnosis of patients
who have gradually become dyspneic or who suffer from chronic dyspneic. This blood test would be
helpful in measuring how well the lungs are bringing oxygen into the blood and removing the carbon
dioxide (Mulpuru et al., 2017). The patient named Peter is showing symptoms of dyspnea and hence,
this assessment would help nurses to develop an idea about how the lung is functioning.
3
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
(Kyngas et al., 2017). He works in a mining company and thereby he might be also exposed to coal
dusts and other fumes that have added to the exacerbation of the condition.
Task 2. Nursing assessments
Identify three (3) nursing assessments you will conduct and explain why they are a priority for you.
The nursing diagnosis should try to identify the highest nursing priorities so that the
professional can provide direct care to the patients. For Peter, the nurse should first try to measure
his respiration rate. The respiration rate measurement as a part of the vital sign measurement also
needs to be conducted. The respiration rate is the number of breaths taken by the patient in one
minute. This rate is mainly measured when an individual would be at rest. This would simply involve
counting the total number of times the chest would rise (Fitzsimmons et al., 2016). Normal
respiration rate for the adult persons are usually 12 to 16 breaths per minute. Changes in the
respiratory rate is found to be associated with asthma, anxiety, congestive heart failure, pneumonia,
lung disorder as well as the use of narcotics. Therefore, this should be the first assessment needed
to find out whether any such disorders are present in Peter or not. If the rate is found to be high in
Peter, then the following assessments are to be done.
For Peter, Spirometry test should also be conducted to develop about his conditions of the
lungs as Peter is suspected to be suffering from COPD. Spirometry is one of the diagnostic tools of
choice and helps in measuring the obstruction of the airflow. These tests are seen to include forced
expiratory volume in the first second (FEV1) and forced vital capacity (FVC). These have been found
to help in reflecting the changes in the lung volume from that of the total lung capacity through the
sustained expiration to residual volume (Moreira et al., 2017). The nurse would then try to calculate
the ratio of expired volume to vital capacity (FEV1/FVC). The normal ratio of FEV1/FVC should be
about 705 of greater than this. A lower ratio is mainly seen to indicate the airflow obstruction and is
considered to be the sensitive indicator for the COPD. Studies have also stated that the absolute
FEV1 found in the setting of that of the reduced FEV1/FVC ratio is mainly expressed as a percentage
of the predicted value. This can be helpful of the professional in assessing the severity of the
disorder (The Lung Foundation, 2018). Hence, the nurse attending Peter should first conduct the test
that would show the change the lung volume from total lung capacity and assess its severity.
Another diagnostic test that should be also conducted for Peter is the arterial blood gas
measurement. This measurement can help by providing information about the alteration of Ph as
well as hypercapnia, hypocapnia as well as hypoxia in Peter. This test is found to be useful in the
evaluation of acute dyspnea. They are also found to be helpful in the cases of diagnosis of patients
who have gradually become dyspneic or who suffer from chronic dyspneic. This blood test would be
helpful in measuring how well the lungs are bringing oxygen into the blood and removing the carbon
dioxide (Mulpuru et al., 2017). The patient named Peter is showing symptoms of dyspnea and hence,
this assessment would help nurses to develop an idea about how the lung is functioning.
3
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
UR250 Medical Surgical Nursing 2Assessment 1 Semester 1 2019
Task 3. Care planning
Identify three (3) priority nursing diagnoses for your chosen case scenario and explain why they are
relevant.
The nurse should set the first nursing priority. It is importance for the nurse to help Peter
achieve airway clearance as he is facing breathlessness, which might be because of mucus
formation, and blocking of the airways by the mucus. Then interventions need to be set. The nurse
must initiate medication therapy for appropriately administering the bronchodilators as well as
corticosteroids and thereby become alert for any potential side effects for Peter. Bronchodilators
mainly help in relieving bronchospasms mainly by alteration of the smooth muscles tones and
thereby reducing the airway obstruction by allowing increased oxygen distribution throughout the
lungs thereby improving alveolar ventilation (Weldam et al., 2017). Corticosteroids on the other
hand can also be also initiated. Studies are of the opinion that for people who have moderate or
severe acute exacerbation, short courses of oral corticosteroids like that, for five days can help in
preventing the worsening of COPD. Even nowadays, evidence based studies have opined the
application of the phosphodiesterase-4 inhibitor to relieve people from reducing the symptoms of
COPD. The nurse should also teach Peter about the concept of direct as well as indirect
coughing. The nurse should be instructing Peter in direct as well as controlled coughing. This
is found to be more effective and would help in the reduction of fatigue associated with
undirected forceful coughing (Korpenshoek et al., 2016). Then evaluation needs to be done.
The nurse should ausculate the breath sounds and no down the adventitious breath sounds.
The nurse should also assess and monitor respirations as well as breath sounds, noting the
rate and other sounds in Peter. This would help nurses to understand the efficiency of
interventions in maintaining clearance of the airways in Peter.
The nurse should set the second nursing priority. The second goal of the nurse would be to
develop the breathing pattern of Peter. Then interventions need to be set. The nurse should first
integrate inspiratory muscle training, as this would help the patient in developing the breathing
pattern in Peter. The nurse can also undertake diaphragmatic breathing. This form of breathing helps
in education of the respiratory rate and increases the alveolar ventilation. It also sometimes helps in
expelling as much air as possible during the time of expiration (Sobeh et al., 2019). The nurse may
also introduce pursed lip breathing to Peter. This form of breathing can help in slowing down the
expiration and helps in preventing the collapse of the small airways. It would also help in controlling
the rate as well as depth of the respiration. The nurse can introduce oxygen therapies. When
there is not enough oxygen in the blood, supplemental oxygen can be provided to the
patients through different devices like delivering oxygen to your lungs, including lightweight,
portable units. Studies suggest that this therapy helps in extending the lives and developing
the quality of lives (Hazizadeh et al., 2015). Then evaluation needs to be done. Vital signs
should be done from time to time which would also help the nurse to undertake
assessments for saturated oxygen level and this would help them in understanding the
breathing pattern.
4
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
Task 3. Care planning
Identify three (3) priority nursing diagnoses for your chosen case scenario and explain why they are
relevant.
The nurse should set the first nursing priority. It is importance for the nurse to help Peter
achieve airway clearance as he is facing breathlessness, which might be because of mucus
formation, and blocking of the airways by the mucus. Then interventions need to be set. The nurse
must initiate medication therapy for appropriately administering the bronchodilators as well as
corticosteroids and thereby become alert for any potential side effects for Peter. Bronchodilators
mainly help in relieving bronchospasms mainly by alteration of the smooth muscles tones and
thereby reducing the airway obstruction by allowing increased oxygen distribution throughout the
lungs thereby improving alveolar ventilation (Weldam et al., 2017). Corticosteroids on the other
hand can also be also initiated. Studies are of the opinion that for people who have moderate or
severe acute exacerbation, short courses of oral corticosteroids like that, for five days can help in
preventing the worsening of COPD. Even nowadays, evidence based studies have opined the
application of the phosphodiesterase-4 inhibitor to relieve people from reducing the symptoms of
COPD. The nurse should also teach Peter about the concept of direct as well as indirect
coughing. The nurse should be instructing Peter in direct as well as controlled coughing. This
is found to be more effective and would help in the reduction of fatigue associated with
undirected forceful coughing (Korpenshoek et al., 2016). Then evaluation needs to be done.
The nurse should ausculate the breath sounds and no down the adventitious breath sounds.
The nurse should also assess and monitor respirations as well as breath sounds, noting the
rate and other sounds in Peter. This would help nurses to understand the efficiency of
interventions in maintaining clearance of the airways in Peter.
The nurse should set the second nursing priority. The second goal of the nurse would be to
develop the breathing pattern of Peter. Then interventions need to be set. The nurse should first
integrate inspiratory muscle training, as this would help the patient in developing the breathing
pattern in Peter. The nurse can also undertake diaphragmatic breathing. This form of breathing helps
in education of the respiratory rate and increases the alveolar ventilation. It also sometimes helps in
expelling as much air as possible during the time of expiration (Sobeh et al., 2019). The nurse may
also introduce pursed lip breathing to Peter. This form of breathing can help in slowing down the
expiration and helps in preventing the collapse of the small airways. It would also help in controlling
the rate as well as depth of the respiration. The nurse can introduce oxygen therapies. When
there is not enough oxygen in the blood, supplemental oxygen can be provided to the
patients through different devices like delivering oxygen to your lungs, including lightweight,
portable units. Studies suggest that this therapy helps in extending the lives and developing
the quality of lives (Hazizadeh et al., 2015). Then evaluation needs to be done. Vital signs
should be done from time to time which would also help the nurse to undertake
assessments for saturated oxygen level and this would help them in understanding the
breathing pattern.
4
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
UR250 Medical Surgical Nursing 2Assessment 1 Semester 1 2019
The third nursing priority needs to be set. Peter is also facing issues while conducting
different activities mainly at work. Therefore, the third goal would be to improve to activity
tolerance and manage other potential complications. Then interventions need to be set. The
nurse should help the patient in managing the daily activities. Experts suggest that the daily activities
need to be paced throughout the day as well as supporting devices that can be also used in
decreasing the energy expenditure. The nurse should also help in exercise training as this can help in
strengthening of the muscles of both the upper and lower extremities and thereby would help in
improving exercise tolerance as well as endurance (Tobiano et al., 2015). The nurse should also
provide the patient with walking aids as this might be recommended in improving the activity levels
as well as ambulation (Shah et al., 2016). The nurse should also try to check for the cognitive
changes as studies opine that the symptoms of the disorder are associated with personality and
behaviour changes and memory impairment. The nurse should also try to prevent any infections
in Peter and should thereby encourage Peter to be immunized with influenza and
S. pneumonia. Peter with this disorder might become prone to respiratory infection with
this disorder. Then evaluation needs to be done. The nurse should try to measure patient
satisfaction and his quality of life through informal discussion about his activity tolerance
issues. As per the feedback of the patient, further interventions can be changed
Task 4: Patient education
Identify specific education your chosen case scenario will require to effectively manage their
condition post discharge.
The nurse should try to develop the health literacy level of the patient named Peter. He
should be discussed about the disorder, the risks factors as well as the complications that may arise
if his disorder is not managed effectively. He should be taught about how cigarette smoking is
contributing to ill health and therefore should advise him to reduce smoking or quit smoking
altogether. He should be also told how his working place is resulting in dust and fumes that are
contributing to the disorders. Peter should be advised with important aspects in his discharge plan.
The nurse should set achievable goals for the patient to help him in increasing the exercise tolerance
and help in preventing the further loss of pulmonary functions (Efraimsson et al., 2015). Another
important aspect would be to instruct the patient about the importance of temperature control. The
nurse should advise the patient in avoiding extremes of heat and cold because heat would result in
increasing the temperature and thereby because rising of the oxygen requirements. The nurse
should also advise the patient in activity moderation where the patient would be adapting a lifestyle
of moderate activities and should thereby avoid any emotional disturbances and stressful situation,
which would increase coughing episodes. Another important component of the training episode
would be breathing retraining. Here the home care nurses should be providing education as well as
breathing retraining to Peter that are found to be necessary in optimizing the functional status of the
patients. Besides, Peter should be also educated about how to take inhaled steroids using the
inhalers in order to make the medication reach lungs appropriately
5
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
The third nursing priority needs to be set. Peter is also facing issues while conducting
different activities mainly at work. Therefore, the third goal would be to improve to activity
tolerance and manage other potential complications. Then interventions need to be set. The
nurse should help the patient in managing the daily activities. Experts suggest that the daily activities
need to be paced throughout the day as well as supporting devices that can be also used in
decreasing the energy expenditure. The nurse should also help in exercise training as this can help in
strengthening of the muscles of both the upper and lower extremities and thereby would help in
improving exercise tolerance as well as endurance (Tobiano et al., 2015). The nurse should also
provide the patient with walking aids as this might be recommended in improving the activity levels
as well as ambulation (Shah et al., 2016). The nurse should also try to check for the cognitive
changes as studies opine that the symptoms of the disorder are associated with personality and
behaviour changes and memory impairment. The nurse should also try to prevent any infections
in Peter and should thereby encourage Peter to be immunized with influenza and
S. pneumonia. Peter with this disorder might become prone to respiratory infection with
this disorder. Then evaluation needs to be done. The nurse should try to measure patient
satisfaction and his quality of life through informal discussion about his activity tolerance
issues. As per the feedback of the patient, further interventions can be changed
Task 4: Patient education
Identify specific education your chosen case scenario will require to effectively manage their
condition post discharge.
The nurse should try to develop the health literacy level of the patient named Peter. He
should be discussed about the disorder, the risks factors as well as the complications that may arise
if his disorder is not managed effectively. He should be taught about how cigarette smoking is
contributing to ill health and therefore should advise him to reduce smoking or quit smoking
altogether. He should be also told how his working place is resulting in dust and fumes that are
contributing to the disorders. Peter should be advised with important aspects in his discharge plan.
The nurse should set achievable goals for the patient to help him in increasing the exercise tolerance
and help in preventing the further loss of pulmonary functions (Efraimsson et al., 2015). Another
important aspect would be to instruct the patient about the importance of temperature control. The
nurse should advise the patient in avoiding extremes of heat and cold because heat would result in
increasing the temperature and thereby because rising of the oxygen requirements. The nurse
should also advise the patient in activity moderation where the patient would be adapting a lifestyle
of moderate activities and should thereby avoid any emotional disturbances and stressful situation,
which would increase coughing episodes. Another important component of the training episode
would be breathing retraining. Here the home care nurses should be providing education as well as
breathing retraining to Peter that are found to be necessary in optimizing the functional status of the
patients. Besides, Peter should be also educated about how to take inhaled steroids using the
inhalers in order to make the medication reach lungs appropriately
5
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
UR250 Medical Surgical Nursing 2Assessment 1 Semester 1 2019
Task 5: Team care
Identify and define the Allied Health team members that should be involved in the patient’s care
during admission and in preparation for discharge
One of the most important people in the team is the dietician. Patients are seen to benefit
from nutritional education, which includes information about how COPD effects their eating.
Nutritional depletion is one of the most common issues in COPD and this has negative impact on
both respiratory as well as skeletal muscle function. Therefore, dieticians would be developing the
food chart for Peter to maintain his weight properly. The nurse might develop a smoking cessation
goal and set of strategies for Peter while educating him to how to adhere to the goals. She might
also refer Peter to community smoking cessation programs. Cardiopulmonary healthcare experts
would be attending Peter and nurses need to report the conditions of the patient regularly to the
experts so as to ensure best interventions. The rehabilitation program should also comprise of the
set of physical exercises for effectively managing conditions like COPD by physiotherapists (Deravin
et al., 2016). They teach the patients about the right breathing as well as relaxation techniques as
well as chest clearance techniques. This helps in managing the disorder as well. Besides, a substance
abuse counsellor can also be allocated for him where he would be included in the talk therapies to
make him motivated to quit the behaviours and counsel him accordingly. Thereby, all individuals
would be working together as a team and would involve Peter and his family in decision-making and
care planning process to provide him person-centred care.
6
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
Task 5: Team care
Identify and define the Allied Health team members that should be involved in the patient’s care
during admission and in preparation for discharge
One of the most important people in the team is the dietician. Patients are seen to benefit
from nutritional education, which includes information about how COPD effects their eating.
Nutritional depletion is one of the most common issues in COPD and this has negative impact on
both respiratory as well as skeletal muscle function. Therefore, dieticians would be developing the
food chart for Peter to maintain his weight properly. The nurse might develop a smoking cessation
goal and set of strategies for Peter while educating him to how to adhere to the goals. She might
also refer Peter to community smoking cessation programs. Cardiopulmonary healthcare experts
would be attending Peter and nurses need to report the conditions of the patient regularly to the
experts so as to ensure best interventions. The rehabilitation program should also comprise of the
set of physical exercises for effectively managing conditions like COPD by physiotherapists (Deravin
et al., 2016). They teach the patients about the right breathing as well as relaxation techniques as
well as chest clearance techniques. This helps in managing the disorder as well. Besides, a substance
abuse counsellor can also be allocated for him where he would be included in the talk therapies to
make him motivated to quit the behaviours and counsel him accordingly. Thereby, all individuals
would be working together as a team and would involve Peter and his family in decision-making and
care planning process to provide him person-centred care.
6
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
UR250 Medical Surgical Nursing 2Assessment 1 Semester 1 2019
References
Anmj.org.au (2018) Chest Pain Assessment And Management, Australian Nursing and Midwifery
journal, Retrieved from: https://anmj.org.au/anmfs-continuing-education-acute-coronary-
syndromes/
Copdx.org.au , (2018), The COPD-X Plan: Australian and New Zealand Guidelines for the
management of Chronic Obstructive Pulmonary Disease 2018, The Lung Foundation
Australia, Retrieved from: https://copdx.org.au/
Deravin-Malone, L., & Anderson, J. (2016). Chronic Care Nursing. Cambridge University Press.
https://books.google.co.in/books?
hl=en&lr=&id=fFWJDAAAQBAJ&oi=fnd&pg=PR15&dq=nursing+care+for+COPD&ots=DuxcT1
VUtN&sig=bEyLNCqRvUOMnLi4Jj5QkFQdisg#v=onepage&q=nursing%20care%20for
%20COPD&f=false
Efraimsson, E. Ö., Klang, B., Ehrenberg, A., Larsson, K., Fossum, B., & Olai, L. (2015). Nurses’ and
patients’ communication in smoking cessation at nurse-led COPD clinics in primary health
care. European clinical respiratory journal, 2(1), 27915.
https://doi.org/10.3402/ecrj.v2.27915
Fitzsimmons, D. A., Thompson, J., Bentley, C. L., & Mountain, G. A. (2016). Comparison of patient
perceptions of Telehealth-supported and specialist nursing interventions for early stage
COPD: a qualitative study. BMC health services research, 16(1), 420.
https://doi.org/10.1186/s12913-016-1623-z
Ghosh, S., OKelly, N., Roberts, E. J., Barker, C., & Swift, J. (2016). The clinical and economic impact of
the combined interventions of telehealth, specialist respiratory nursing care and health
coaching interventions for COPD admissions within an urban setting.
DOI: 10.1183/13993003.congress-2016.PA3958
Hajizadeh, N., Goldfeld, K., & Crothers, K. (2015). What happens to patients with COPD with long-
term oxygen treatment who receive mechanical ventilation for COPD exacerbation? A 1-year
retrospective follow-up study. Thorax, 70(3), 294-296. http://dx.doi.org/10.1136/thoraxjnl-
2014-205248
Kaufman, G. (2013). Chronic obstructive pulmonary disease:: diagnosis and management, Nursing
Standard (through 2013), 27(21), 53. Retrieved from:
https://search.proquest.com/openview/86f38bb47a863bf3ca9bc572f09cb272/1?pq-
origsite=gscholar&cbl=30130
Korpershoek, Y. J. G., Vervoort, S. C. J. M., Nijssen, L. I. T., Schuurmans, M. J., & Trappenburg, J. C. A.
(2016). Factors influencing exacerbation-related self-management behavior in patients with
COPD. Journal of Advanced Nursing, 72(Suppl. S1), 89-89.
https://dspace.library.uu.nl/bitstream/handle/1874/344004/89.pdf?sequence=1
7
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
References
Anmj.org.au (2018) Chest Pain Assessment And Management, Australian Nursing and Midwifery
journal, Retrieved from: https://anmj.org.au/anmfs-continuing-education-acute-coronary-
syndromes/
Copdx.org.au , (2018), The COPD-X Plan: Australian and New Zealand Guidelines for the
management of Chronic Obstructive Pulmonary Disease 2018, The Lung Foundation
Australia, Retrieved from: https://copdx.org.au/
Deravin-Malone, L., & Anderson, J. (2016). Chronic Care Nursing. Cambridge University Press.
https://books.google.co.in/books?
hl=en&lr=&id=fFWJDAAAQBAJ&oi=fnd&pg=PR15&dq=nursing+care+for+COPD&ots=DuxcT1
VUtN&sig=bEyLNCqRvUOMnLi4Jj5QkFQdisg#v=onepage&q=nursing%20care%20for
%20COPD&f=false
Efraimsson, E. Ö., Klang, B., Ehrenberg, A., Larsson, K., Fossum, B., & Olai, L. (2015). Nurses’ and
patients’ communication in smoking cessation at nurse-led COPD clinics in primary health
care. European clinical respiratory journal, 2(1), 27915.
https://doi.org/10.3402/ecrj.v2.27915
Fitzsimmons, D. A., Thompson, J., Bentley, C. L., & Mountain, G. A. (2016). Comparison of patient
perceptions of Telehealth-supported and specialist nursing interventions for early stage
COPD: a qualitative study. BMC health services research, 16(1), 420.
https://doi.org/10.1186/s12913-016-1623-z
Ghosh, S., OKelly, N., Roberts, E. J., Barker, C., & Swift, J. (2016). The clinical and economic impact of
the combined interventions of telehealth, specialist respiratory nursing care and health
coaching interventions for COPD admissions within an urban setting.
DOI: 10.1183/13993003.congress-2016.PA3958
Hajizadeh, N., Goldfeld, K., & Crothers, K. (2015). What happens to patients with COPD with long-
term oxygen treatment who receive mechanical ventilation for COPD exacerbation? A 1-year
retrospective follow-up study. Thorax, 70(3), 294-296. http://dx.doi.org/10.1136/thoraxjnl-
2014-205248
Kaufman, G. (2013). Chronic obstructive pulmonary disease:: diagnosis and management, Nursing
Standard (through 2013), 27(21), 53. Retrieved from:
https://search.proquest.com/openview/86f38bb47a863bf3ca9bc572f09cb272/1?pq-
origsite=gscholar&cbl=30130
Korpershoek, Y. J. G., Vervoort, S. C. J. M., Nijssen, L. I. T., Schuurmans, M. J., & Trappenburg, J. C. A.
(2016). Factors influencing exacerbation-related self-management behavior in patients with
COPD. Journal of Advanced Nursing, 72(Suppl. S1), 89-89.
https://dspace.library.uu.nl/bitstream/handle/1874/344004/89.pdf?sequence=1
7
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
UR250 Medical Surgical Nursing 2Assessment 1 Semester 1 2019
Kyngäs, H., Kanste, O., Patala-Pudas, L., & Kaakinen, P. (2017). COPD-patients adherence to care and
quality of counselling. J Nurs Educ Pract, 7(3), 32-39. DOI: 10.5430/jnep.v7n3p32
Moreira, F. C., Teixeira, C., Vieira, S. R. R., Berto, P. P., Martins, L. D. F. G., Hervé, B. B., ... & Robinson,
C. C. (2017). Quality of life after intensive care unit discharge based on the GOLD
classification. Journal of Critical Care, 42, 403.
https://www.annalsthoracicsurgery.org/article/S0883-9441(17)31443-0/abstract
Mulpuru, S., McKay, J., Ronksley, P. E., Thavorn, K., Kobewka, D. M., & Forster, A. J. (2017). Factors
contributing to high-cost hospital care for patients with COPD. International journal of
chronic obstructive pulmonary disease, 12, 989. doi: 10.2147/COPD.S126607
Rodgers, J., Stanton, M., & Jackson, J. (2018). Providing care to COPD patients using in-home visits by
nurse practitioners. Journal of nursing care quality, 33(3), 208-212. doi:
10.1097/NCQ.0000000000000295
Shah, T., Press, V. G., Huisingh-Scheetz, M., & White, S. R. (2016). COPD readmissions: addressing
COPD in the era of value-based health care. Chest, 150(4), 916-926.
https://doi.org/10.1016/j.chest.2016.05.002
Sobeh, D. E., Hafez, F. E., & Mohammed, A. (2019). The Effect of Nursing Care Protocol on Health
Outcomes of Patients with Chronic Obstructive Pulmonary Disease (COPD). International
journal of Nursing Didactics, 9(03), 49-56.
http://www.innovativejournal.net/index.php/ijnd/article/view/2499
Tobiano, G., Marshall, A., Bucknall, T., & Chaboyer, W. (2015). Patient participation in nursing care
on medical wards: an integrative review. International Journal of Nursing Studies, 52(6),
1107-1120. https://doi.org/10.1016/j.ijnurstu.2015.02.010
Weldam, S. W., Lammers, J. W. J., Zwakman, M., & Schuurmans, M. J. (2017). Nurses' perspectives of
a new individualized nursing care intervention for COPD patients in primary care settings: a
mixed method study. Applied nursing research, 33, 85-92.
https://doi.org/10.1016/j.apnr.2016.10.010
Weldam, S. W., Schuurmans, M. J., Zanen, P., Heijmans, M. J., Sachs, A. P., & Lammers, J. W. J.
(2017). The effectiveness of a nurse-led illness perception intervention in COPD patients: a
cluster randomised trial in primary care. ERJ open research, 3(4), 00115-2016.
DOI: 10.1183/23120541.00115-2016
Weldam, S., Lammers, J. W., Zwakman, M., & Schuurmans, M. (2015). Feasibility of a new
individualized nursing care intervention in COPD, the COPD-GRIP intervention.
DOI: 10.1183/13993003.congress-2015.PA327
8
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
Kyngäs, H., Kanste, O., Patala-Pudas, L., & Kaakinen, P. (2017). COPD-patients adherence to care and
quality of counselling. J Nurs Educ Pract, 7(3), 32-39. DOI: 10.5430/jnep.v7n3p32
Moreira, F. C., Teixeira, C., Vieira, S. R. R., Berto, P. P., Martins, L. D. F. G., Hervé, B. B., ... & Robinson,
C. C. (2017). Quality of life after intensive care unit discharge based on the GOLD
classification. Journal of Critical Care, 42, 403.
https://www.annalsthoracicsurgery.org/article/S0883-9441(17)31443-0/abstract
Mulpuru, S., McKay, J., Ronksley, P. E., Thavorn, K., Kobewka, D. M., & Forster, A. J. (2017). Factors
contributing to high-cost hospital care for patients with COPD. International journal of
chronic obstructive pulmonary disease, 12, 989. doi: 10.2147/COPD.S126607
Rodgers, J., Stanton, M., & Jackson, J. (2018). Providing care to COPD patients using in-home visits by
nurse practitioners. Journal of nursing care quality, 33(3), 208-212. doi:
10.1097/NCQ.0000000000000295
Shah, T., Press, V. G., Huisingh-Scheetz, M., & White, S. R. (2016). COPD readmissions: addressing
COPD in the era of value-based health care. Chest, 150(4), 916-926.
https://doi.org/10.1016/j.chest.2016.05.002
Sobeh, D. E., Hafez, F. E., & Mohammed, A. (2019). The Effect of Nursing Care Protocol on Health
Outcomes of Patients with Chronic Obstructive Pulmonary Disease (COPD). International
journal of Nursing Didactics, 9(03), 49-56.
http://www.innovativejournal.net/index.php/ijnd/article/view/2499
Tobiano, G., Marshall, A., Bucknall, T., & Chaboyer, W. (2015). Patient participation in nursing care
on medical wards: an integrative review. International Journal of Nursing Studies, 52(6),
1107-1120. https://doi.org/10.1016/j.ijnurstu.2015.02.010
Weldam, S. W., Lammers, J. W. J., Zwakman, M., & Schuurmans, M. J. (2017). Nurses' perspectives of
a new individualized nursing care intervention for COPD patients in primary care settings: a
mixed method study. Applied nursing research, 33, 85-92.
https://doi.org/10.1016/j.apnr.2016.10.010
Weldam, S. W., Schuurmans, M. J., Zanen, P., Heijmans, M. J., Sachs, A. P., & Lammers, J. W. J.
(2017). The effectiveness of a nurse-led illness perception intervention in COPD patients: a
cluster randomised trial in primary care. ERJ open research, 3(4), 00115-2016.
DOI: 10.1183/23120541.00115-2016
Weldam, S., Lammers, J. W., Zwakman, M., & Schuurmans, M. (2015). Feasibility of a new
individualized nursing care intervention in COPD, the COPD-GRIP intervention.
DOI: 10.1183/13993003.congress-2015.PA327
8
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1

UR250 Medical Surgical Nursing 2Assessment 1 Semester 1 2019
9
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
9
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
UR250 Medical Surgical Nursing 2Assessment 1 Semester 1 2019
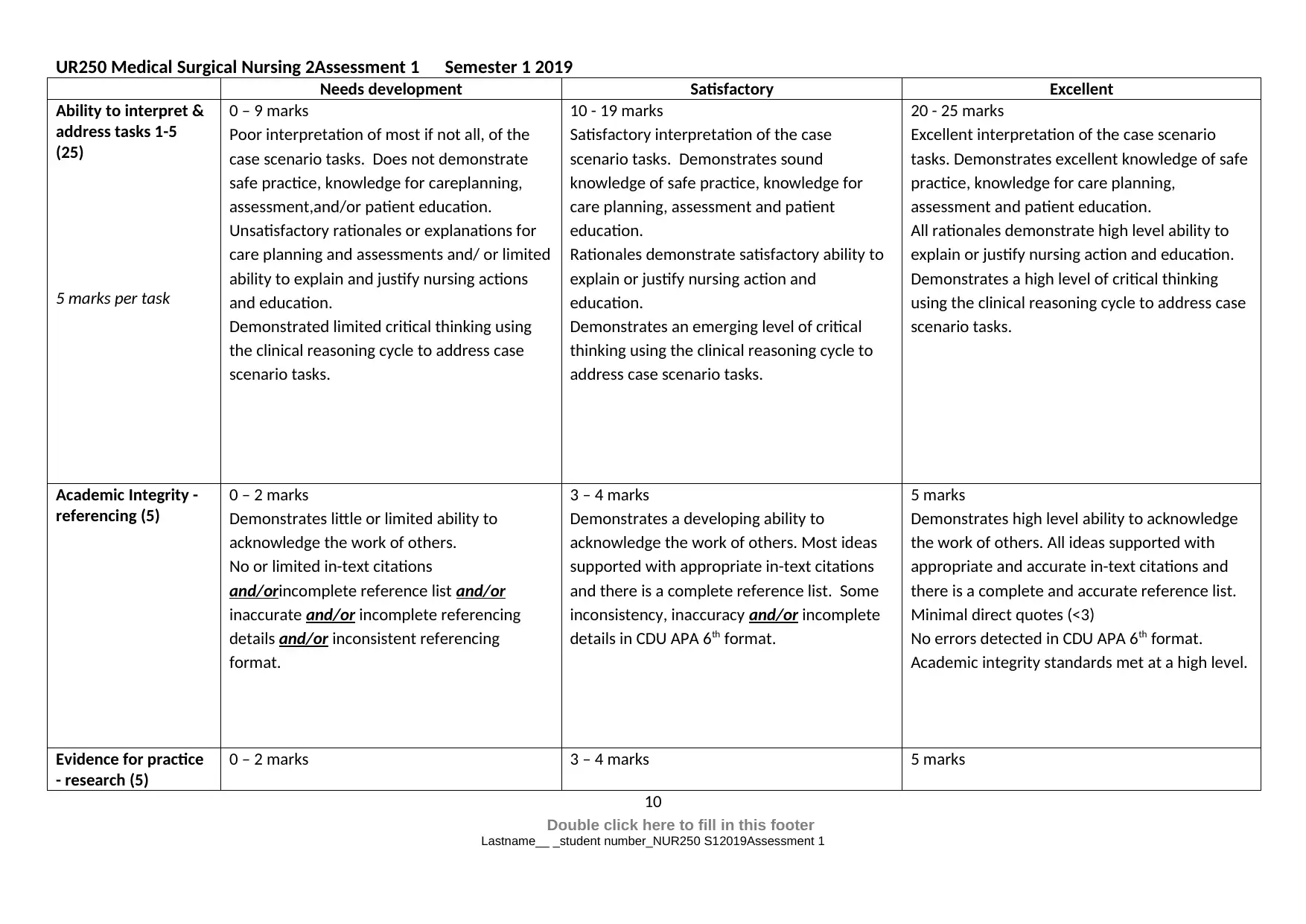
Needs development Satisfactory Excellent
Ability to interpret &
address tasks 1-5
(25)
5 marks per task
0 – 9 marks
Poor interpretation of most if not all, of the
case scenario tasks. Does not demonstrate
safe practice, knowledge for careplanning,
assessment,and/or patient education.
Unsatisfactory rationales or explanations for
care planning and assessments and/ or limited
ability to explain and justify nursing actions
and education.
Demonstrated limited critical thinking using
the clinical reasoning cycle to address case
scenario tasks.
10 - 19 marks
Satisfactory interpretation of the case
scenario tasks. Demonstrates sound
knowledge of safe practice, knowledge for
care planning, assessment and patient
education.
Rationales demonstrate satisfactory ability to
explain or justify nursing action and
education.
Demonstrates an emerging level of critical
thinking using the clinical reasoning cycle to
address case scenario tasks.
20 - 25 marks
Excellent interpretation of the case scenario
tasks. Demonstrates excellent knowledge of safe
practice, knowledge for care planning,
assessment and patient education.
All rationales demonstrate high level ability to
explain or justify nursing action and education.
Demonstrates a high level of critical thinking
using the clinical reasoning cycle to address case
scenario tasks.
Academic Integrity -
referencing (5)
0 – 2 marks
Demonstrates little or limited ability to
acknowledge the work of others.
No or limited in-text citations
and/orincomplete reference list and/or
inaccurate and/or incomplete referencing
details and/or inconsistent referencing
format.
3 – 4 marks
Demonstrates a developing ability to
acknowledge the work of others. Most ideas
supported with appropriate in-text citations
and there is a complete reference list. Some
inconsistency, inaccuracy and/or incomplete
details in CDU APA 6th format.
5 marks
Demonstrates high level ability to acknowledge
the work of others. All ideas supported with
appropriate and accurate in-text citations and
there is a complete and accurate reference list.
Minimal direct quotes (<3)
No errors detected in CDU APA 6th format.
Academic integrity standards met at a high level.
Evidence for practice
- research (5)
0 – 2 marks 3 – 4 marks 5 marks
10
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
Needs development Satisfactory Excellent
Ability to interpret &
address tasks 1-5
(25)
5 marks per task
0 – 9 marks
Poor interpretation of most if not all, of the
case scenario tasks. Does not demonstrate
safe practice, knowledge for careplanning,
assessment,and/or patient education.
Unsatisfactory rationales or explanations for
care planning and assessments and/ or limited
ability to explain and justify nursing actions
and education.
Demonstrated limited critical thinking using
the clinical reasoning cycle to address case
scenario tasks.
10 - 19 marks
Satisfactory interpretation of the case
scenario tasks. Demonstrates sound
knowledge of safe practice, knowledge for
care planning, assessment and patient
education.
Rationales demonstrate satisfactory ability to
explain or justify nursing action and
education.
Demonstrates an emerging level of critical
thinking using the clinical reasoning cycle to
address case scenario tasks.
20 - 25 marks
Excellent interpretation of the case scenario
tasks. Demonstrates excellent knowledge of safe
practice, knowledge for care planning,
assessment and patient education.
All rationales demonstrate high level ability to
explain or justify nursing action and education.
Demonstrates a high level of critical thinking
using the clinical reasoning cycle to address case
scenario tasks.
Academic Integrity -
referencing (5)
0 – 2 marks
Demonstrates little or limited ability to
acknowledge the work of others.
No or limited in-text citations
and/orincomplete reference list and/or
inaccurate and/or incomplete referencing
details and/or inconsistent referencing
format.
3 – 4 marks
Demonstrates a developing ability to
acknowledge the work of others. Most ideas
supported with appropriate in-text citations
and there is a complete reference list. Some
inconsistency, inaccuracy and/or incomplete
details in CDU APA 6th format.
5 marks
Demonstrates high level ability to acknowledge
the work of others. All ideas supported with
appropriate and accurate in-text citations and
there is a complete and accurate reference list.
Minimal direct quotes (<3)
No errors detected in CDU APA 6th format.
Academic integrity standards met at a high level.
Evidence for practice
- research (5)
0 – 2 marks 3 – 4 marks 5 marks
10
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
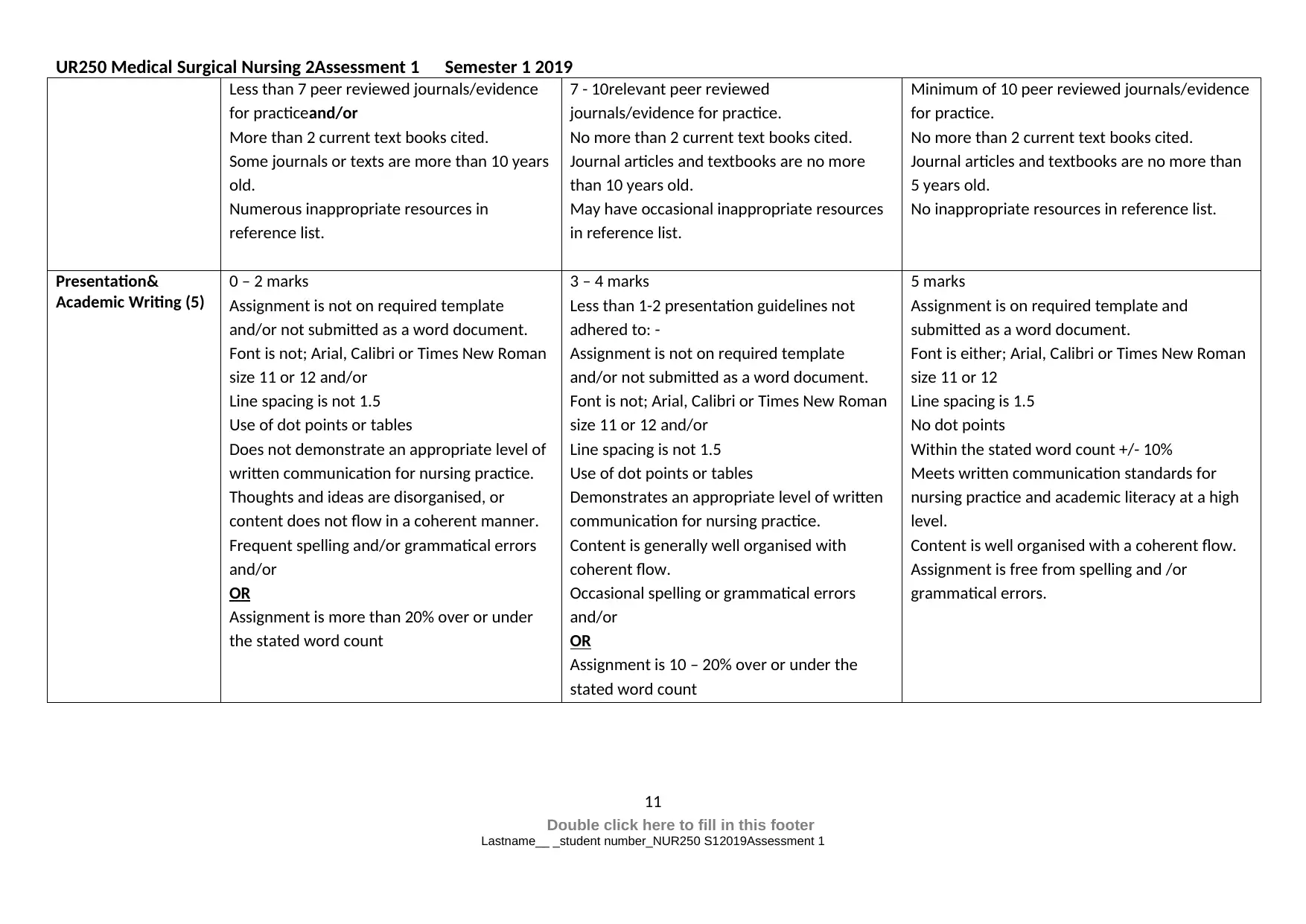
UR250 Medical Surgical Nursing 2Assessment 1 Semester 1 2019
Less than 7 peer reviewed journals/evidence
for practiceand/or
More than 2 current text books cited.
Some journals or texts are more than 10 years
old.
Numerous inappropriate resources in
reference list.
7 - 10relevant peer reviewed
journals/evidence for practice.
No more than 2 current text books cited.
Journal articles and textbooks are no more
than 10 years old.
May have occasional inappropriate resources
in reference list.
Minimum of 10 peer reviewed journals/evidence
for practice.
No more than 2 current text books cited.
Journal articles and textbooks are no more than
5 years old.
No inappropriate resources in reference list.
Presentation&
Academic Writing (5)
0 – 2 marks
Assignment is not on required template
and/or not submitted as a word document.
Font is not; Arial, Calibri or Times New Roman
size 11 or 12 and/or
Line spacing is not 1.5
Use of dot points or tables
Does not demonstrate an appropriate level of
written communication for nursing practice.
Thoughts and ideas are disorganised, or
content does not flow in a coherent manner.
Frequent spelling and/or grammatical errors
and/or
OR
Assignment is more than 20% over or under
the stated word count
3 – 4 marks
Less than 1-2 presentation guidelines not
adhered to: -
Assignment is not on required template
and/or not submitted as a word document.
Font is not; Arial, Calibri or Times New Roman
size 11 or 12 and/or
Line spacing is not 1.5
Use of dot points or tables
Demonstrates an appropriate level of written
communication for nursing practice.
Content is generally well organised with
coherent flow.
Occasional spelling or grammatical errors
and/or
OR
Assignment is 10 – 20% over or under the
stated word count
5 marks
Assignment is on required template and
submitted as a word document.
Font is either; Arial, Calibri or Times New Roman
size 11 or 12
Line spacing is 1.5
No dot points
Within the stated word count +/- 10%
Meets written communication standards for
nursing practice and academic literacy at a high
level.
Content is well organised with a coherent flow.
Assignment is free from spelling and /or
grammatical errors.
11
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
Less than 7 peer reviewed journals/evidence
for practiceand/or
More than 2 current text books cited.
Some journals or texts are more than 10 years
old.
Numerous inappropriate resources in
reference list.
7 - 10relevant peer reviewed
journals/evidence for practice.
No more than 2 current text books cited.
Journal articles and textbooks are no more
than 10 years old.
May have occasional inappropriate resources
in reference list.
Minimum of 10 peer reviewed journals/evidence
for practice.
No more than 2 current text books cited.
Journal articles and textbooks are no more than
5 years old.
No inappropriate resources in reference list.
Presentation&
Academic Writing (5)
0 – 2 marks
Assignment is not on required template
and/or not submitted as a word document.
Font is not; Arial, Calibri or Times New Roman
size 11 or 12 and/or
Line spacing is not 1.5
Use of dot points or tables
Does not demonstrate an appropriate level of
written communication for nursing practice.
Thoughts and ideas are disorganised, or
content does not flow in a coherent manner.
Frequent spelling and/or grammatical errors
and/or
OR
Assignment is more than 20% over or under
the stated word count
3 – 4 marks
Less than 1-2 presentation guidelines not
adhered to: -
Assignment is not on required template
and/or not submitted as a word document.
Font is not; Arial, Calibri or Times New Roman
size 11 or 12 and/or
Line spacing is not 1.5
Use of dot points or tables
Demonstrates an appropriate level of written
communication for nursing practice.
Content is generally well organised with
coherent flow.
Occasional spelling or grammatical errors
and/or
OR
Assignment is 10 – 20% over or under the
stated word count
5 marks
Assignment is on required template and
submitted as a word document.
Font is either; Arial, Calibri or Times New Roman
size 11 or 12
Line spacing is 1.5
No dot points
Within the stated word count +/- 10%
Meets written communication standards for
nursing practice and academic literacy at a high
level.
Content is well organised with a coherent flow.
Assignment is free from spelling and /or
grammatical errors.
11
Double click here to fill in this footer
Lastname__ _student number_NUR250 S12019Assessment 1
1 out of 11
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





