Case Study Analysis: Inquiry Based Learning Approach for Amanda's Care
VerifiedAdded on 2022/10/11
|19
|5245
|22
Case Study
AI Summary
This case study focuses on Amanda, a 28-year-old woman with bipolar disorder, who attempted suicide after a relapse. The assignment requires an inquiry-based learning approach to analyze the case study documents, including medical records, and family narratives, to identify key issues, formulate relevant questions, and investigate the disorder, its clinical manifestations, and treatment options. The analysis includes the application of NMBA Registered Nurse Standards for Practice, exploring nursing interventions, and addressing patient safety concerns. The case study highlights the importance of a recovery and person-centered approach to care, particularly in addressing non-adherence to treatment plans and substance abuse issues. The assignment emphasizes critical thinking, clinical skills, and the development of effective nursing interventions to support Amanda's recovery and prevent future suicide attempts. The case study also examines the role of community interventions and support systems in managing bipolar disorder and preventing relapse.
Assessment 3 – Case Study 2019
Using an Inquiry Based Learning Approach
Learning strategy
What you need to do
to critically analyse
the Case Study
Thought processes
What you need to demonstrate to your
lecturer in terms of your critical thinking
about this Case Study
Learning Outcomes Section
Demonstrate your learning in each section by presenting the
information that you have examined to improve your knowledge and
understanding of this particular Case Study
STEP 1 - CONNECT
Analyse each of the
case study documents
Amanda is a 28 years old high-school part-
time teacher, living with roommate in
Adelaide, suffering from bipolar disorder, and
having suicidal tendencies from past few
weeks, after relapse. She is having mixed
episodes of bipolar disorder currently, having
excessive mood fluctuations, with high
energy, yet low-self esteem and depression
caused by workload. She is continuing with
Lithium Carbonate XR 600mg and low doses
of Quetiapine, along with occasional drinking,
which was again one reason for starting
suicidal thoughts. She has several episodes
wherein she had intake Diazepam and
marijuana. After initial intake of marijuana,
Amanda had undergone previous treatments in public and private hospitals
along with drug-rehab programs, but she was not provided support after
discharge as her mother suggested which has increased the suicidal trends in
Amanda. Moreover, the mood stabilisers, anti-psychotic medications and
tranquilisers given to Amanda always made her susceptible to side effects,
making her lethargic, unmotivated and low-concentration. She is now under
addiction control means, but feels light and happy when she goes into manic
phase or euphoria induced by drugs.
Using an Inquiry Based Learning Approach
Learning strategy
What you need to do
to critically analyse
the Case Study
Thought processes
What you need to demonstrate to your
lecturer in terms of your critical thinking
about this Case Study
Learning Outcomes Section
Demonstrate your learning in each section by presenting the
information that you have examined to improve your knowledge and
understanding of this particular Case Study
STEP 1 - CONNECT
Analyse each of the
case study documents
Amanda is a 28 years old high-school part-
time teacher, living with roommate in
Adelaide, suffering from bipolar disorder, and
having suicidal tendencies from past few
weeks, after relapse. She is having mixed
episodes of bipolar disorder currently, having
excessive mood fluctuations, with high
energy, yet low-self esteem and depression
caused by workload. She is continuing with
Lithium Carbonate XR 600mg and low doses
of Quetiapine, along with occasional drinking,
which was again one reason for starting
suicidal thoughts. She has several episodes
wherein she had intake Diazepam and
marijuana. After initial intake of marijuana,
Amanda had undergone previous treatments in public and private hospitals
along with drug-rehab programs, but she was not provided support after
discharge as her mother suggested which has increased the suicidal trends in
Amanda. Moreover, the mood stabilisers, anti-psychotic medications and
tranquilisers given to Amanda always made her susceptible to side effects,
making her lethargic, unmotivated and low-concentration. She is now under
addiction control means, but feels light and happy when she goes into manic
phase or euphoria induced by drugs.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
she had first suicidal episode, after which she
started exploring new amphetamines and
different drugs, which is one of the major risk
factors behind her suicidal tendencies.
STEP 2 - QUESTION
What are some of the
questions about this
Case Study that you
want to know more
information?
Identify the additional
information you need
to know about so that
you can plan your
care
Some questions are required to assess
information from the case study which seems
insufficient. For planning care interventions
such questions are vital in understanding the
patient’s responses and certain background to
improve intervention plans.
1. What are the thoughts that run through
Amanda’s mind before she attempts
suicide?
2. Did the hospital or nursing
interventions beforehand support
Amanda after being discharged from
hospital?
3. Had Amanda planned to be discovered
after suicide or was it accidental
These questions will provide extra information for understanding the
perspective from Amanda’s point of view. The thoughts pertaining to
suicide, and previous nursing interventions have been asked in detail, so that
the new nurses finds loopholes and improves the care provided to Amanda.
The suicidal tendencies, intentions, and feelings of the patient will be asked
to generate an answer about her perception of the whole episode, and her
reaction to the situation, whether she wants to improve her condition.
Moreover, previous care unit, the support system provided has also been
analysed to find criteria which will help Amanda develop her condition
better in future.
started exploring new amphetamines and
different drugs, which is one of the major risk
factors behind her suicidal tendencies.
STEP 2 - QUESTION
What are some of the
questions about this
Case Study that you
want to know more
information?
Identify the additional
information you need
to know about so that
you can plan your
care
Some questions are required to assess
information from the case study which seems
insufficient. For planning care interventions
such questions are vital in understanding the
patient’s responses and certain background to
improve intervention plans.
1. What are the thoughts that run through
Amanda’s mind before she attempts
suicide?
2. Did the hospital or nursing
interventions beforehand support
Amanda after being discharged from
hospital?
3. Had Amanda planned to be discovered
after suicide or was it accidental
These questions will provide extra information for understanding the
perspective from Amanda’s point of view. The thoughts pertaining to
suicide, and previous nursing interventions have been asked in detail, so that
the new nurses finds loopholes and improves the care provided to Amanda.
The suicidal tendencies, intentions, and feelings of the patient will be asked
to generate an answer about her perception of the whole episode, and her
reaction to the situation, whether she wants to improve her condition.
Moreover, previous care unit, the support system provided has also been
analysed to find criteria which will help Amanda develop her condition
better in future.
finding?
4. What was the feelings of Amanda
after waking up in hospital and not
perform the suicide successfully ?
5. What was the immediate cause of
suicide, and what happened later on?
6. Are there any feelings of guilt within
Amanda, or she blames herself over
some issue?
7. Were previous care providers
monitoring her situation even after
being discharged, and was she joining
any community interventions for
mitigating suicidal thoughts?
STEP 3 -
INVESTIGATE
Review your current
Research this disorder further. Record the
references at the end of this template
Describe the disorder presented in this scenario and include in-text
referencing
Bipolar disorder-
Bipolar disorder is a form of mood disorder characterised by fluctuations in
mood, and energy levels (Grande et al., 2016). About more than 1.8%,
Australians experience this disorder every year, through two episodes,
4. What was the feelings of Amanda
after waking up in hospital and not
perform the suicide successfully ?
5. What was the immediate cause of
suicide, and what happened later on?
6. Are there any feelings of guilt within
Amanda, or she blames herself over
some issue?
7. Were previous care providers
monitoring her situation even after
being discharged, and was she joining
any community interventions for
mitigating suicidal thoughts?
STEP 3 -
INVESTIGATE
Review your current
Research this disorder further. Record the
references at the end of this template
Describe the disorder presented in this scenario and include in-text
referencing
Bipolar disorder-
Bipolar disorder is a form of mood disorder characterised by fluctuations in
mood, and energy levels (Grande et al., 2016). About more than 1.8%,
Australians experience this disorder every year, through two episodes,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
knowledge about the
clients mental illness
in this Case Study
Answer the questions in the
Learning Outcomes Section on the right
namely depression episodes and manic episodes. Depressive episodes are
characterised by hopelessness, low mood, sadness, lack of interest, whereas,
the manic episodes are characterised by high energy, euphoria, more
agitation, little sleep, hasty speech patterns etc. In the case study, Amanda is
suffering from Bipolar disorder, from the age of 15, initially diagnosed as
unipolar disorder, with depression levels. However, consumption of
amphetamines and marijuana also influenced the bipolar changes in mood
patterns, displaying depressive, manic and mixed episodes until now. Every
patient undergoes through mixed episodes once during their bipolar course.
After being sober for some months, patients may started showing relapse
behaviour, with loss in focus and hasty speech. However, with mixed
episodes, patients start having various feelings namely, sadness, emptiness,
loss of interest, speaking irregularly, loss of concentration, having high
energy levels sometimes, irritation, fatigue, feeling worthless and low self-
esteem, and getting more suicidal tendencies through de-motivation (Aas et
al., 2016).
In mixed episodes patients may become more elevated or expansive, inflated
self-esteem, being talkative, fleeting ideas, increased energy levels, risk-
taking behaviour, and decrease in sleep. Likewise, they might also get
depressed over trivial matters, with low self-esteem, demotivation and
suicidal tendencies. Impulsivity is one characteristic feature common in all
bipolar patients, which leads them to take inappropriate actions without
clients mental illness
in this Case Study
Answer the questions in the
Learning Outcomes Section on the right
namely depression episodes and manic episodes. Depressive episodes are
characterised by hopelessness, low mood, sadness, lack of interest, whereas,
the manic episodes are characterised by high energy, euphoria, more
agitation, little sleep, hasty speech patterns etc. In the case study, Amanda is
suffering from Bipolar disorder, from the age of 15, initially diagnosed as
unipolar disorder, with depression levels. However, consumption of
amphetamines and marijuana also influenced the bipolar changes in mood
patterns, displaying depressive, manic and mixed episodes until now. Every
patient undergoes through mixed episodes once during their bipolar course.
After being sober for some months, patients may started showing relapse
behaviour, with loss in focus and hasty speech. However, with mixed
episodes, patients start having various feelings namely, sadness, emptiness,
loss of interest, speaking irregularly, loss of concentration, having high
energy levels sometimes, irritation, fatigue, feeling worthless and low self-
esteem, and getting more suicidal tendencies through de-motivation (Aas et
al., 2016).
In mixed episodes patients may become more elevated or expansive, inflated
self-esteem, being talkative, fleeting ideas, increased energy levels, risk-
taking behaviour, and decrease in sleep. Likewise, they might also get
depressed over trivial matters, with low self-esteem, demotivation and
suicidal tendencies. Impulsivity is one characteristic feature common in all
bipolar patients, which leads them to take inappropriate actions without
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
level-headedness (Solé et al., 2016).
What are the clinical manifestations associated with this disorder?
Include in-text referencing
Clinical manifestations:
Some clinical manifestations of bipolar disorder include manic episodes,
depressive episodes, and mixed episodes. Manic episodes include symptoms
like jumpy, weird and upbeat mood, increased energy, high self-confidence,
decreased sleep, talkativeness, hasty thoughts, distraction, and low
concentration (Wang et al., 2016). Depressive episode symptoms include
feeling empty, sad, loss of interest, weight loss, decrease in appetite,
insomnia, sleeping too much, slow actions, loss of energy, low
concentration, planning to attempt suicide. As per Grande et al., (2017),
other clinical manifestations include anxiety, distress, psychosis,
melancholia, mixed symptoms, stressed, feeling unrealistic, acting
impulsively, delusions or hallucinations in some cases. In some cases of
mixed symptoms both manic, depressive phases are found, with agitation,
anxiety, irritability, distraction, insomnia, hasty thoughts, along with high
and low mood interchange rising chances of suicidal trends.
Suicidal indications due to certain factors can be understood through
What are the clinical manifestations associated with this disorder?
Include in-text referencing
Clinical manifestations:
Some clinical manifestations of bipolar disorder include manic episodes,
depressive episodes, and mixed episodes. Manic episodes include symptoms
like jumpy, weird and upbeat mood, increased energy, high self-confidence,
decreased sleep, talkativeness, hasty thoughts, distraction, and low
concentration (Wang et al., 2016). Depressive episode symptoms include
feeling empty, sad, loss of interest, weight loss, decrease in appetite,
insomnia, sleeping too much, slow actions, loss of energy, low
concentration, planning to attempt suicide. As per Grande et al., (2017),
other clinical manifestations include anxiety, distress, psychosis,
melancholia, mixed symptoms, stressed, feeling unrealistic, acting
impulsively, delusions or hallucinations in some cases. In some cases of
mixed symptoms both manic, depressive phases are found, with agitation,
anxiety, irritability, distraction, insomnia, hasty thoughts, along with high
and low mood interchange rising chances of suicidal trends.
Suicidal indications due to certain factors can be understood through
helplessness, hopelessness, depressive symptoms, loss of appetite, low-self
esteem, low motivation which Amanda was suffering from. Suicidal people
might organise their suicide, either through self-harm by hanging, or self-
infliction using weapon, withdrawing from social interactions and finding
plausible ways in which to attempt suicide (Malhi, 2014).
What are the common treatment options for this disorder? Include in-
text referencing
Treatment options:
The best manner of conventional treatment for bipolar patients is
medications, treatment programs, substance abuse treatment and
hospitalisation. Medications according to Alda (2015), includes mood
stabilisers, antipsychotic drugs, anti-depressants, antidepressant-
antipsychotic, and anti-anxiety medicines. Within therapy treatment plans,
psychotherapy through interpersonal and social rhythm therapy IPSRT,
cognitive-behavioural therapy, psycho education, family-focused therapy are
widely accepted. Other options for conventional treatment as Ashok et al.,
(2017) suggests, includes electroconvulsive therapy ECT, and trans-cranial
magnetic stimulation TMS.
Home remedies for improving self-management of mood swings include,
esteem, low motivation which Amanda was suffering from. Suicidal people
might organise their suicide, either through self-harm by hanging, or self-
infliction using weapon, withdrawing from social interactions and finding
plausible ways in which to attempt suicide (Malhi, 2014).
What are the common treatment options for this disorder? Include in-
text referencing
Treatment options:
The best manner of conventional treatment for bipolar patients is
medications, treatment programs, substance abuse treatment and
hospitalisation. Medications according to Alda (2015), includes mood
stabilisers, antipsychotic drugs, anti-depressants, antidepressant-
antipsychotic, and anti-anxiety medicines. Within therapy treatment plans,
psychotherapy through interpersonal and social rhythm therapy IPSRT,
cognitive-behavioural therapy, psycho education, family-focused therapy are
widely accepted. Other options for conventional treatment as Ashok et al.,
(2017) suggests, includes electroconvulsive therapy ECT, and trans-cranial
magnetic stimulation TMS.
Home remedies for improving self-management of mood swings include,
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
quitting taking drugs, amphetamines, narcotics or marijuana. Forming
healthy relationships at home, generating a healthy plan or routine, and
keeping mood charts. Reducing substance abuse through community
intervention programs, going to doctors for treating substance abuse are
other forms of treatment for people with drug-induced suicidal tendencies
with bipolar disorder.
STEP 4 - CONSTRUCT
Using a recovery and
person-centred
approach, explore the
issues raised in this
case study and how
you can support this
person during your
early shift
Consider the NMBA Registered Nurse
Standards for Practice
You do not need to write anything here
Consider the nursing interventions and
clinical skills that are required for this Case
Study
You do not need to write anything here
Identify the appropriate NMBA Registered Nurse Standards for
Practice that would be applicable for you as an RN in supporting the
person in this Case Study
The main issue highlighted from the case study is non-adherence to proper
treatment plans for Amanda, due to which she is coming out from relapse
and entering a new phase in the disorder. Due to non-adherence and
improper substance abuse treatment, her alcohol intake is raising her chances
of suicidal attempts, thereby increasing her risk factors. During long-term
treatment, most patients and caregivers become non-adherent to the
treatment pattern. Hence, a person centric recovery approach must be
adopted to make patients recover from substance abuse, and increase their
adherence to the treatment plans (Murray et al., 2017).
The NMBA guidelines specify 7 basic standards of nursing for registered
healthy relationships at home, generating a healthy plan or routine, and
keeping mood charts. Reducing substance abuse through community
intervention programs, going to doctors for treating substance abuse are
other forms of treatment for people with drug-induced suicidal tendencies
with bipolar disorder.
STEP 4 - CONSTRUCT
Using a recovery and
person-centred
approach, explore the
issues raised in this
case study and how
you can support this
person during your
early shift
Consider the NMBA Registered Nurse
Standards for Practice
You do not need to write anything here
Consider the nursing interventions and
clinical skills that are required for this Case
Study
You do not need to write anything here
Identify the appropriate NMBA Registered Nurse Standards for
Practice that would be applicable for you as an RN in supporting the
person in this Case Study
The main issue highlighted from the case study is non-adherence to proper
treatment plans for Amanda, due to which she is coming out from relapse
and entering a new phase in the disorder. Due to non-adherence and
improper substance abuse treatment, her alcohol intake is raising her chances
of suicidal attempts, thereby increasing her risk factors. During long-term
treatment, most patients and caregivers become non-adherent to the
treatment pattern. Hence, a person centric recovery approach must be
adopted to make patients recover from substance abuse, and increase their
adherence to the treatment plans (Murray et al., 2017).
The NMBA guidelines specify 7 basic standards of nursing for registered
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
Consider the patient safety concerns related
to this Case Study
You do not need to write anything here
nurses, which involves:
Standard 1: ability to think critically and analyse various nursing practices
Standard 2: more involvement in therapeutic and qualified relations
Standard 3: having the capacity to practice
Standard 4: conducting assessments conducive
Standard 5: developing own nursing practice plans
Standard 6: providing able, justified, safe, and responsive nursing practices
Standard 7: evaluating the outcomes from care to improve nursing practice
Mental health nurses acknowledge the variety in culture, beliefs, values and
promotes dignity in nursing mental patients (Hagen et al., 2017). Through
collaborative partnerships, nurses provide support to mental patients for
improving their care. Through therapeutic and interpersonal-professional
relationships, nurses generate a holistic environment for providing
appropriate mental health services. To reduce prejudice and stigma in mental
care nurses improve social inclusion and community interventions for mental
patients. Through evidence based practices, innovative practice dissipation
by professional development, education, research, and reflective practices
are undertaken. The nurses work within the ambit of common law and code
of conduct, ethics integrating local, national and international protocols of
to this Case Study
You do not need to write anything here
nurses, which involves:
Standard 1: ability to think critically and analyse various nursing practices
Standard 2: more involvement in therapeutic and qualified relations
Standard 3: having the capacity to practice
Standard 4: conducting assessments conducive
Standard 5: developing own nursing practice plans
Standard 6: providing able, justified, safe, and responsive nursing practices
Standard 7: evaluating the outcomes from care to improve nursing practice
Mental health nurses acknowledge the variety in culture, beliefs, values and
promotes dignity in nursing mental patients (Hagen et al., 2017). Through
collaborative partnerships, nurses provide support to mental patients for
improving their care. Through therapeutic and interpersonal-professional
relationships, nurses generate a holistic environment for providing
appropriate mental health services. To reduce prejudice and stigma in mental
care nurses improve social inclusion and community interventions for mental
patients. Through evidence based practices, innovative practice dissipation
by professional development, education, research, and reflective practices
are undertaken. The nurses work within the ambit of common law and code
of conduct, ethics integrating local, national and international protocols of
mental nursing. Moreover, the nurses have specialist knowledge in taking
care of mentally ill patients, along with skills and practices to improve
mental health an capacity of patients (Hsiao et al., 2015).
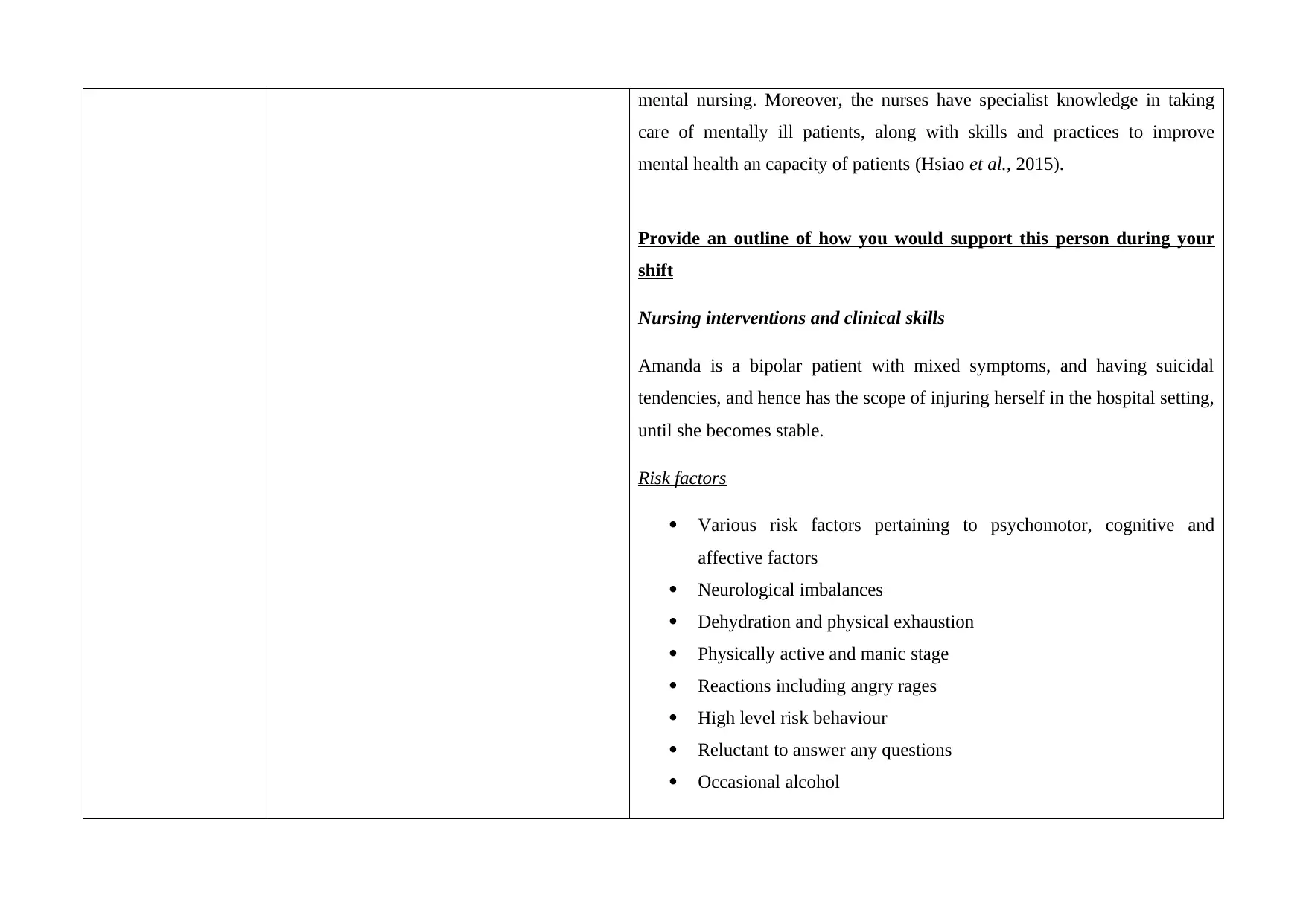
Provide an outline of how you would support this person during your
shift
Nursing interventions and clinical skills
Amanda is a bipolar patient with mixed symptoms, and having suicidal
tendencies, and hence has the scope of injuring herself in the hospital setting,
until she becomes stable.
Risk factors
Various risk factors pertaining to psychomotor, cognitive and
affective factors
Neurological imbalances
Dehydration and physical exhaustion
Physically active and manic stage
Reactions including angry rages
High level risk behaviour
Reluctant to answer any questions
Occasional alcohol
care of mentally ill patients, along with skills and practices to improve
mental health an capacity of patients (Hsiao et al., 2015).
Provide an outline of how you would support this person during your
shift
Nursing interventions and clinical skills
Amanda is a bipolar patient with mixed symptoms, and having suicidal
tendencies, and hence has the scope of injuring herself in the hospital setting,
until she becomes stable.
Risk factors
Various risk factors pertaining to psychomotor, cognitive and
affective factors
Neurological imbalances
Dehydration and physical exhaustion
Physically active and manic stage
Reactions including angry rages
High level risk behaviour
Reluctant to answer any questions
Occasional alcohol
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
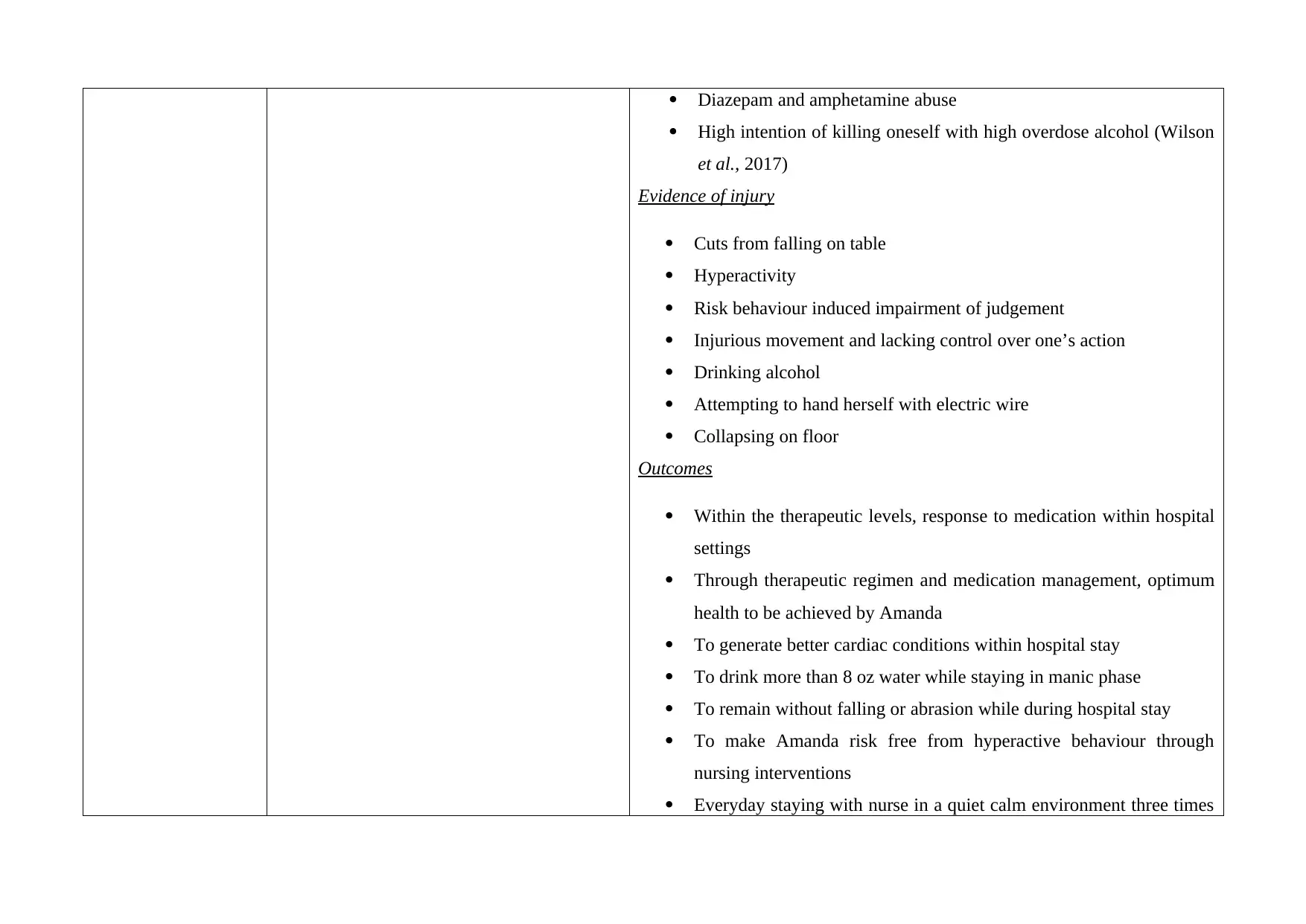
Diazepam and amphetamine abuse
High intention of killing oneself with high overdose alcohol (Wilson
et al., 2017)
Evidence of injury
Cuts from falling on table
Hyperactivity
Risk behaviour induced impairment of judgement
Injurious movement and lacking control over one’s action
Drinking alcohol
Attempting to hand herself with electric wire
Collapsing on floor
Outcomes
Within the therapeutic levels, response to medication within hospital
settings
Through therapeutic regimen and medication management, optimum
health to be achieved by Amanda
To generate better cardiac conditions within hospital stay
To drink more than 8 oz water while staying in manic phase
To remain without falling or abrasion while during hospital stay
To make Amanda risk free from hyperactive behaviour through
nursing interventions
Everyday staying with nurse in a quiet calm environment three times
High intention of killing oneself with high overdose alcohol (Wilson
et al., 2017)
Evidence of injury
Cuts from falling on table
Hyperactivity
Risk behaviour induced impairment of judgement
Injurious movement and lacking control over one’s action
Drinking alcohol
Attempting to hand herself with electric wire
Collapsing on floor
Outcomes
Within the therapeutic levels, response to medication within hospital
settings
Through therapeutic regimen and medication management, optimum
health to be achieved by Amanda
To generate better cardiac conditions within hospital stay
To drink more than 8 oz water while staying in manic phase
To remain without falling or abrasion while during hospital stay
To make Amanda risk free from hyperactive behaviour through
nursing interventions
Everyday staying with nurse in a quiet calm environment three times
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
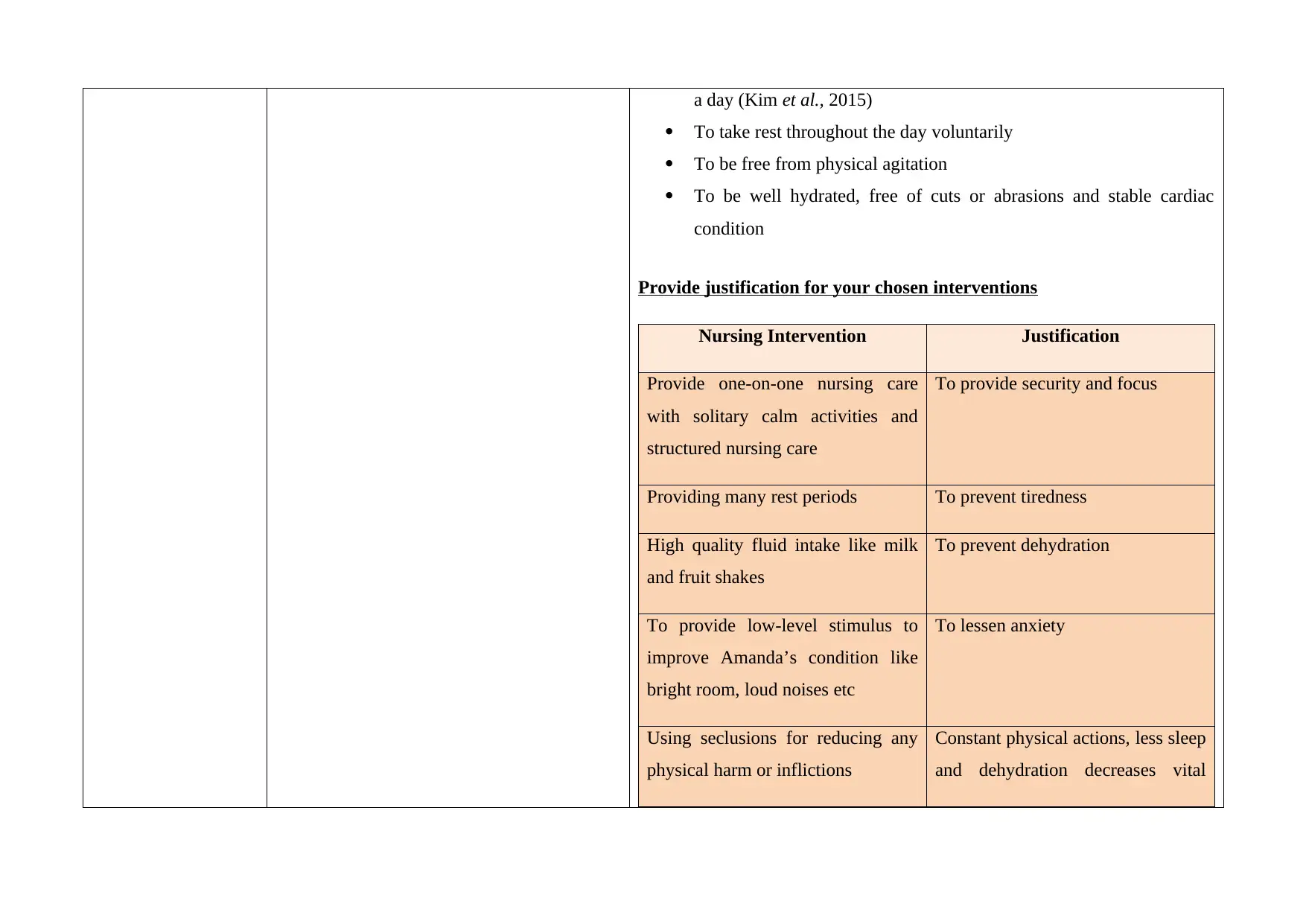
a day (Kim et al., 2015)
To take rest throughout the day voluntarily
To be free from physical agitation
To be well hydrated, free of cuts or abrasions and stable cardiac
condition
Provide justification for your chosen interventions
Nursing Intervention Justification
Provide one-on-one nursing care
with solitary calm activities and
structured nursing care
To provide security and focus
Providing many rest periods To prevent tiredness
High quality fluid intake like milk
and fruit shakes
To prevent dehydration
To provide low-level stimulus to
improve Amanda’s condition like
bright room, loud noises etc
To lessen anxiety
Using seclusions for reducing any
physical harm or inflictions
Constant physical actions, less sleep
and dehydration decreases vital
To take rest throughout the day voluntarily
To be free from physical agitation
To be well hydrated, free of cuts or abrasions and stable cardiac
condition
Provide justification for your chosen interventions
Nursing Intervention Justification
Provide one-on-one nursing care
with solitary calm activities and
structured nursing care
To provide security and focus
Providing many rest periods To prevent tiredness
High quality fluid intake like milk
and fruit shakes
To prevent dehydration
To provide low-level stimulus to
improve Amanda’s condition like
bright room, loud noises etc
To lessen anxiety
Using seclusions for reducing any
physical harm or inflictions
Constant physical actions, less sleep
and dehydration decreases vital
stats
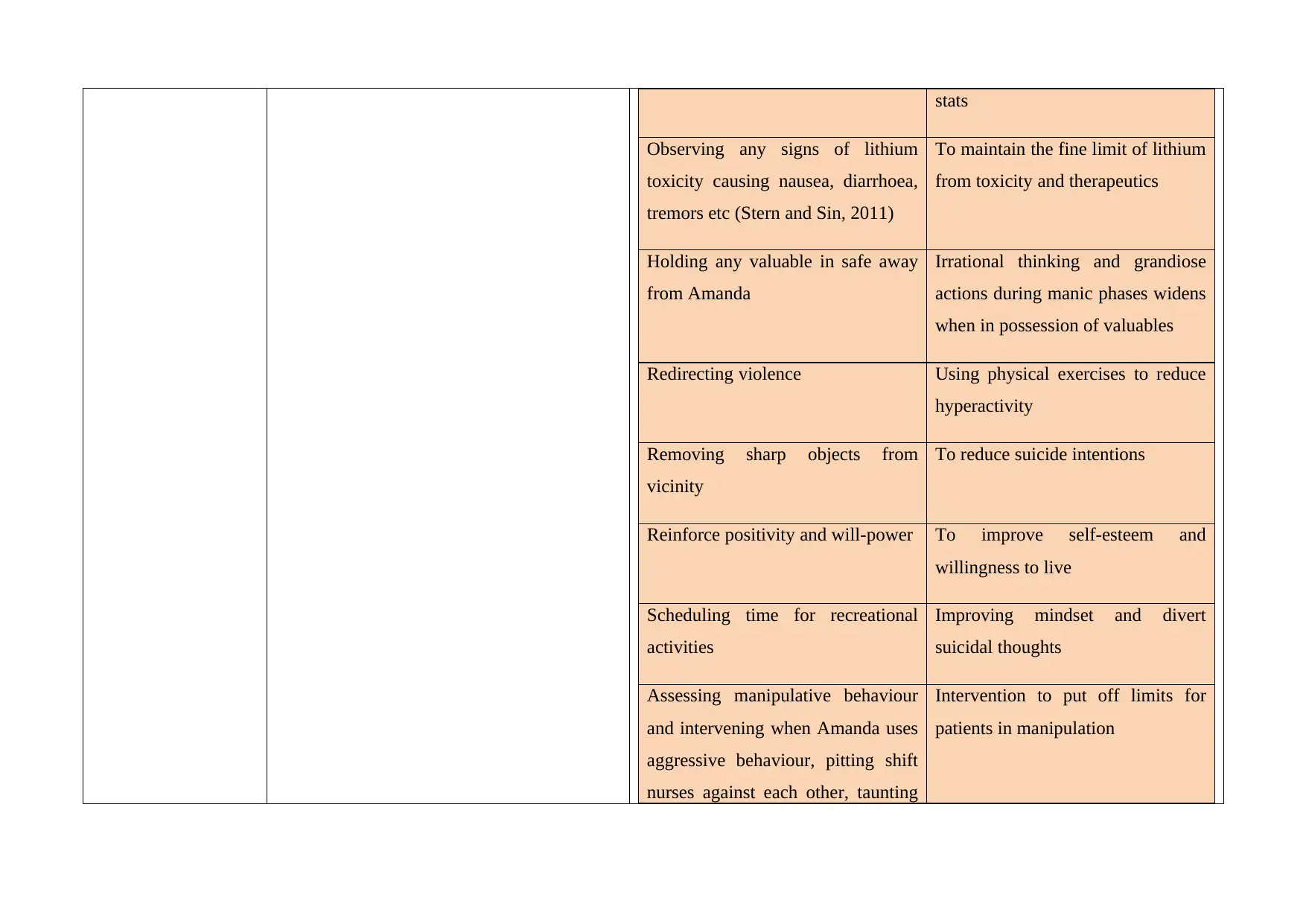
Observing any signs of lithium
toxicity causing nausea, diarrhoea,
tremors etc (Stern and Sin, 2011)
To maintain the fine limit of lithium
from toxicity and therapeutics
Holding any valuable in safe away
from Amanda
Irrational thinking and grandiose
actions during manic phases widens
when in possession of valuables
Redirecting violence Using physical exercises to reduce
hyperactivity
Removing sharp objects from
vicinity
To reduce suicide intentions
Reinforce positivity and will-power To improve self-esteem and
willingness to live
Scheduling time for recreational
activities
Improving mindset and divert
suicidal thoughts
Assessing manipulative behaviour
and intervening when Amanda uses
aggressive behaviour, pitting shift
nurses against each other, taunting
Intervention to put off limits for
patients in manipulation
Observing any signs of lithium
toxicity causing nausea, diarrhoea,
tremors etc (Stern and Sin, 2011)
To maintain the fine limit of lithium
from toxicity and therapeutics
Holding any valuable in safe away
from Amanda
Irrational thinking and grandiose
actions during manic phases widens
when in possession of valuables
Redirecting violence Using physical exercises to reduce
hyperactivity
Removing sharp objects from
vicinity
To reduce suicide intentions
Reinforce positivity and will-power To improve self-esteem and
willingness to live
Scheduling time for recreational
activities
Improving mindset and divert
suicidal thoughts
Assessing manipulative behaviour
and intervening when Amanda uses
aggressive behaviour, pitting shift
nurses against each other, taunting
Intervention to put off limits for
patients in manipulation
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 19
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.




