Radiographer Screening for Pulmonary Emboli in Cancer Patients: Study
VerifiedAdded on 2022/09/07
|7
|4604
|29
Report
AI Summary
This report details a study conducted at The Christie NHS Foundation Trust evaluating a radiographer-led screening program for incidental pulmonary emboli on routine contrast-enhanced computed tomography (CT) scans within a cancer center. The study aimed to assess the effectiveness of the program in terms of detection rates, time to treatment initiation, and radiographer satisfaction. The training program involved 32 radiographers, and the screening service was implemented with monthly quality assurance. Results indicated a high detection rate of pulmonary emboli (92% after full implementation), a significant reduction in the time interval between the scan and clinical consultation for anticoagulant prescription (from a mean of 1.5 days to 26 minutes), and high radiographer satisfaction with the extended role. The study concludes that radiographer screening is an effective and accurate method for detecting incidental pulmonary emboli, leading to immediate communication with physicians and timely initiation of anticoagulation therapy, creating a "one-stop" service and improving patient outcomes.
Radiographer screening for incidental pulmonary
emboli on routine contrast-enhanced
computerised tomography scans at a cancer
centre
A. Kilburn*, S.I.Iddles,B.M. Carrington
Department of Radiology, The Christie NHS Foundation Trust, Wilmslow Road, Withington, Manchester M20 4BX, UK
article information
Article history:
Received 12 December 2016
Received in revised form
16 June 2017
Accepted 11 July 2017
AIM: To introduce and assess effectiveness of a radiographer-led screening programme for
the detection of unsuspected pulmonary emboli on routine contrast-enhanced computed to-
mography (CT),and to evaluate radiographer response to this extended role.
MATERIALS AND METHODS:A training programme was devised for allradiographic staff
working in CT. The screening service was introduced and monthly quality assurance performe
with cumulative analysis of the first 2 years. Clinical effectiveness before and after screening
evaluated by comparing the time interval between the scan and the start of a clinical consulta
for anticoagulant prescription. A satisfaction survey was sent to all participating staff.
RESULTS: Thirty-two radiographers completed the training.During the training period,the
radiographer detection rate of incidental pulmonary emboli was 89%.Main, lobar,segmental,
and subsegmental emboli were detected.The overall detection rate after full introduction of
the programme was 92% for the first 2 years.The time interval between the scan and clinical
consultation for anticoagulant prescription dropped from a mean of 1.5 days to a mean of 26
minutes and ensured that treatment was commenced at the same patient attendance. Eighty
four percent of staff completed the satisfaction survey and all were satisfied with the extende
role.
CONCLUSION: Radiographer screening for incidentalpulmonary emboliwas effective and
accurate.It resulted in immediate communication with the responsible physician and
commencement of anticoagulation therapy at the same hospital attendance,creating a “one-
stop” service.Radiographer satisfaction with the extended role was high.
Crown Copyright Ó 2017 Published by Elsevier Ltd on behalf of The Royal College of
Radiologists.All rights reserved.
Introduction
The incidence of pulmonary emboli is four- to six-times
greater in an oncology population than the general
medical population,1 and the diagnosis of an incidental
pulmonary embolus is associated with the same adverse
survival in cancer patients as in patients with symptomatic
pulmonary emboli.2 Technologicaladvances in computed
tomography (CT) image quality have resulted in increased
recognition of incidental pulmonary emboli on routine
intravenous contrast-enhanced thoracic CT.3 The main aim
of the present study was to introduce a radiographer-led
* Guarantor and correspondent: A. Kilburn,Department of Radiology, The
Christie NHS Foundation Trust,Wilmslow Road,Withington M20 4BX,UK.
Tel.: þ44 0161 446 8555.
E-mail address: alison.kilburn@christie.nhs.uk (A.Kilburn).
Contents lists available at ScienceDirect
Clinical Radiology
j o u r n a lhomepage: w w w . c l i n i c a l r a d i o l o g y o n l i n e . n e t
http://dx.doi.org/10.1016/j.crad.2017.07.010
0009-9260/Crown Copyright Ó 2017 Published by Elsevier Ltd on behalf of The Royal College of Radiologists.All rights reserved.
Clinical Radiology xxx (2017) 1e7
Please cite this article in press as: Kilburn A,et al.,Radiographer screening for incidental pulmonary emboli on routine contrast-enhanced
computerised tomography scans at a cancer centre, Clinical Radiology (2017),http://dx.doi.org/10.1016/j.crad.2017.07.010
emboli on routine contrast-enhanced
computerised tomography scans at a cancer
centre
A. Kilburn*, S.I.Iddles,B.M. Carrington
Department of Radiology, The Christie NHS Foundation Trust, Wilmslow Road, Withington, Manchester M20 4BX, UK
article information
Article history:
Received 12 December 2016
Received in revised form
16 June 2017
Accepted 11 July 2017
AIM: To introduce and assess effectiveness of a radiographer-led screening programme for
the detection of unsuspected pulmonary emboli on routine contrast-enhanced computed to-
mography (CT),and to evaluate radiographer response to this extended role.
MATERIALS AND METHODS:A training programme was devised for allradiographic staff
working in CT. The screening service was introduced and monthly quality assurance performe
with cumulative analysis of the first 2 years. Clinical effectiveness before and after screening
evaluated by comparing the time interval between the scan and the start of a clinical consulta
for anticoagulant prescription. A satisfaction survey was sent to all participating staff.
RESULTS: Thirty-two radiographers completed the training.During the training period,the
radiographer detection rate of incidental pulmonary emboli was 89%.Main, lobar,segmental,
and subsegmental emboli were detected.The overall detection rate after full introduction of
the programme was 92% for the first 2 years.The time interval between the scan and clinical
consultation for anticoagulant prescription dropped from a mean of 1.5 days to a mean of 26
minutes and ensured that treatment was commenced at the same patient attendance. Eighty
four percent of staff completed the satisfaction survey and all were satisfied with the extende
role.
CONCLUSION: Radiographer screening for incidentalpulmonary emboliwas effective and
accurate.It resulted in immediate communication with the responsible physician and
commencement of anticoagulation therapy at the same hospital attendance,creating a “one-
stop” service.Radiographer satisfaction with the extended role was high.
Crown Copyright Ó 2017 Published by Elsevier Ltd on behalf of The Royal College of
Radiologists.All rights reserved.
Introduction
The incidence of pulmonary emboli is four- to six-times
greater in an oncology population than the general
medical population,1 and the diagnosis of an incidental
pulmonary embolus is associated with the same adverse
survival in cancer patients as in patients with symptomatic
pulmonary emboli.2 Technologicaladvances in computed
tomography (CT) image quality have resulted in increased
recognition of incidental pulmonary emboli on routine
intravenous contrast-enhanced thoracic CT.3 The main aim
of the present study was to introduce a radiographer-led
* Guarantor and correspondent: A. Kilburn,Department of Radiology, The
Christie NHS Foundation Trust,Wilmslow Road,Withington M20 4BX,UK.
Tel.: þ44 0161 446 8555.
E-mail address: alison.kilburn@christie.nhs.uk (A.Kilburn).
Contents lists available at ScienceDirect
Clinical Radiology
j o u r n a lhomepage: w w w . c l i n i c a l r a d i o l o g y o n l i n e . n e t
http://dx.doi.org/10.1016/j.crad.2017.07.010
0009-9260/Crown Copyright Ó 2017 Published by Elsevier Ltd on behalf of The Royal College of Radiologists.All rights reserved.
Clinical Radiology xxx (2017) 1e7
Please cite this article in press as: Kilburn A,et al.,Radiographer screening for incidental pulmonary emboli on routine contrast-enhanced
computerised tomography scans at a cancer centre, Clinical Radiology (2017),http://dx.doi.org/10.1016/j.crad.2017.07.010
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser

screening programme forthe detection of unsuspected
pulmonary emboli and to assess its effectiveness in terms of
detection and time to patient treatment.To the authors’
knowledge, this is the first study to assess training efficacy
across a large cohort of radiographers working in CT on a
rotational basis, and to document the change in time taken
to institute treatment.A secondary aim was to assess staff
satisfaction with the extended role.
Materials and methods
The purpose of the training programme was to provide a
fast and effective radiographer-led screening programme
for incidental pulmonary embolism detection using routine
contrast-enhanced CT.As the responsibility for confirming
and reporting the presence of a pulmonary embolism
remained with the radiologist,there was no requirement
for formal ethics approval.
The intention was to integrate the screening programme
into the normalworking practices ofthe CT service with
radiographer screening taking place at the point of care in
the CT control room. CT lists included patients with all
histological types of cancer and were undertaken for stag-
ing, treatment response or follow-up.Apart from CT pul-
monary angiograms (CTPAs) and unenhanced studies, every
inpatient and outpatient contrast-enhanced CT thorax was
assessed,including patients with poor venous access or
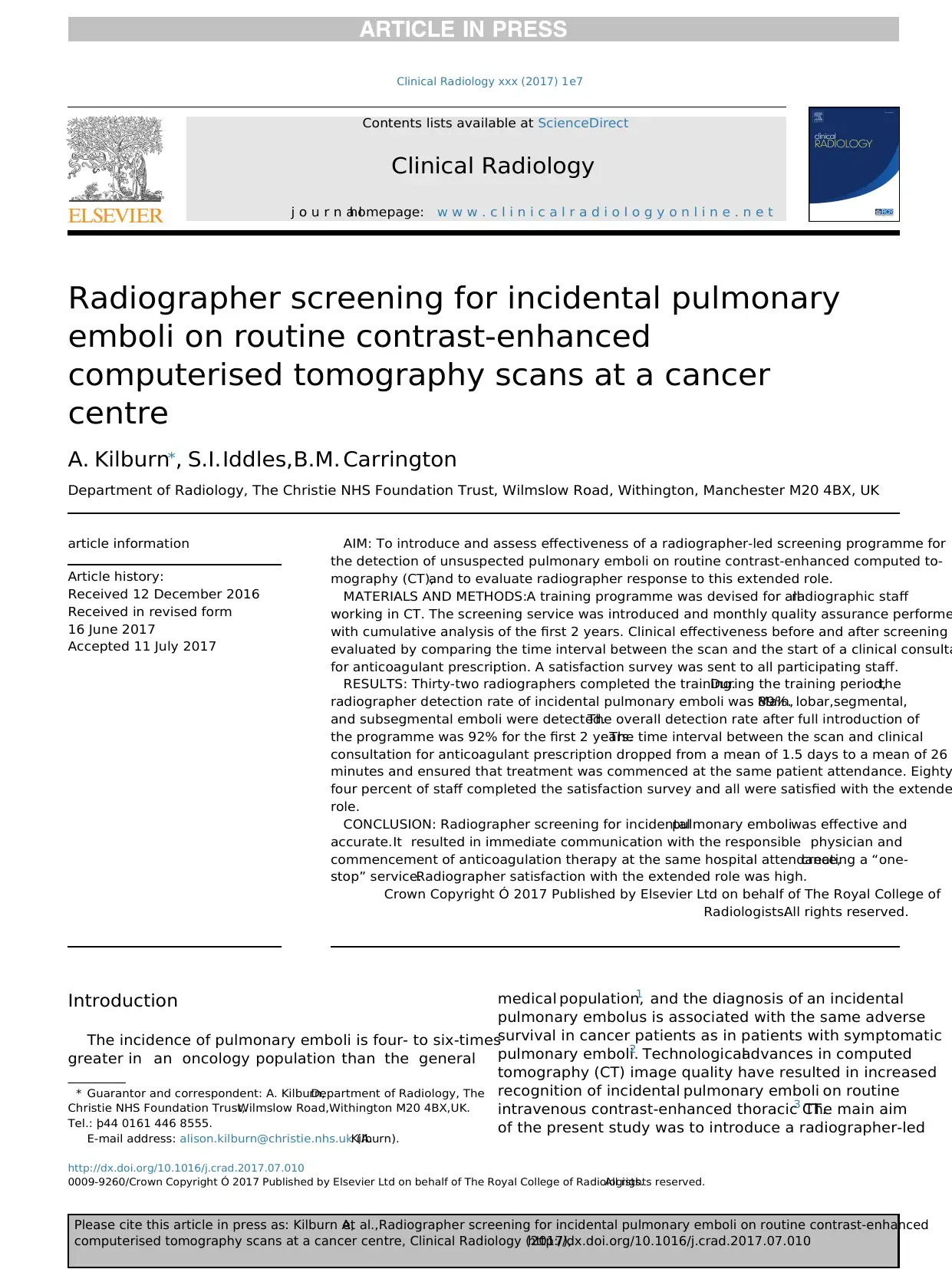
suboptimal contrast enhancement. A flow-chart illustrating
the proposed patient journey through CT following a
contrast-enhanced thorax scan is included in Fig 1.
A pilot cohort of six cross-sectionalradiographers un-
derwent training.They read relevant literature on pulmo-
nary embolism prevalence,imaging criteria for detection,
and clinical management. They attended a series of prepared
lectures on the epidemiology and pathophysiology of pul-
monary embolism,normal intravenous contrast-enhanced
thoracic CT anatomy, the CT appearance of acute and
chronic pulmonary emboli, and potential reasons for
misdiagnosis.The radiographers then reviewed 20 cases
individually, followed by a group discussion. Thereafter, each
radiographer completed a log book of 100 cases, which were
all reviewed by the training radiologist.A post-training
standard of 90% detection was decided upon and audit of
the pilot cohort confirmed that the standard had been met.
The same training programme was then extended to include
all radiographic staff working in and rotating through the CT
department, irrespective of seniority and extent of previous
CT experience and the post-training standard was met by all.
Training of the entire radiographic stafftook 2 years 4
months before fullimplementation ofthe screening pro-
gramme was possible. Before that time, trained staff
screened all the patients they scanned. Several posters were
designed and placed in the CT control room to remind staff of
key CT imaging features of pulmonary emboli.
CT acquisition and review
CT images were acquired on all three CT systems including
a 16-multidetector CT system and two 64-multidetector
CT systems (Somatom Sensation 16 and Somatom AS Defi-
nition 64, Siemens, Erlangen Germany). Imaging parameters
on the 16 section system were standardised for all routine
protocols with 1.5 mm beam collimation,pitch 0.75,0.5
second rotation time, and 3 mm reconstructed section
thickness.On the 64-section system,the imaging parame-
ters were 0.6 mm beam collimation,pitch 1.2,0.5 second
rotation time, and 3 mm reconstructed section thickness.
According to body weight,70 or 85 ml of an iodinated
intravenous contrast medium iopamidol(300 mg iodine/
ml; Niopam 300,Bracco imaging Germany) was adminis-
tered at a rate of1e3 ml/s depending on venous access.
Scans were performed using a bolus-tracking technique
with a trigger threshold of 120 HU units.The imaging pro-
tocol was standardised for all patients who had an arterial
phase contrast-enhanced thorax scan.All images were
screened immediately following scan acquisition by the
radiographer performing the scan using the scanner work-
stations (Wizard,Navigator and Syngo Acquisition Work-
place,Siemens,Erlangen Germany).
Implementation of screening programme
Prior to full implementation of the screening programme,
a standard operating procedure (SOP)was developed to
support and integrate the screening programme into the
daily work of the CT department.This outlined governance
arrangements and detailed the roles and responsibilities of
all staff groups,pathways of communication,quality assur-
ance and continued radiographer training and audit.Pro-
cedures were also introduced for training new employees
and for management of an incidentally discovered pulmo-
nary embolus when no radiologist was immediately avail-
able,for example,at weekends.Signs were produced for
waiting areas to inform the patients thatthe screening
programme was in operation and that there might be an
additional wait if a pulmonary embolus was detected.
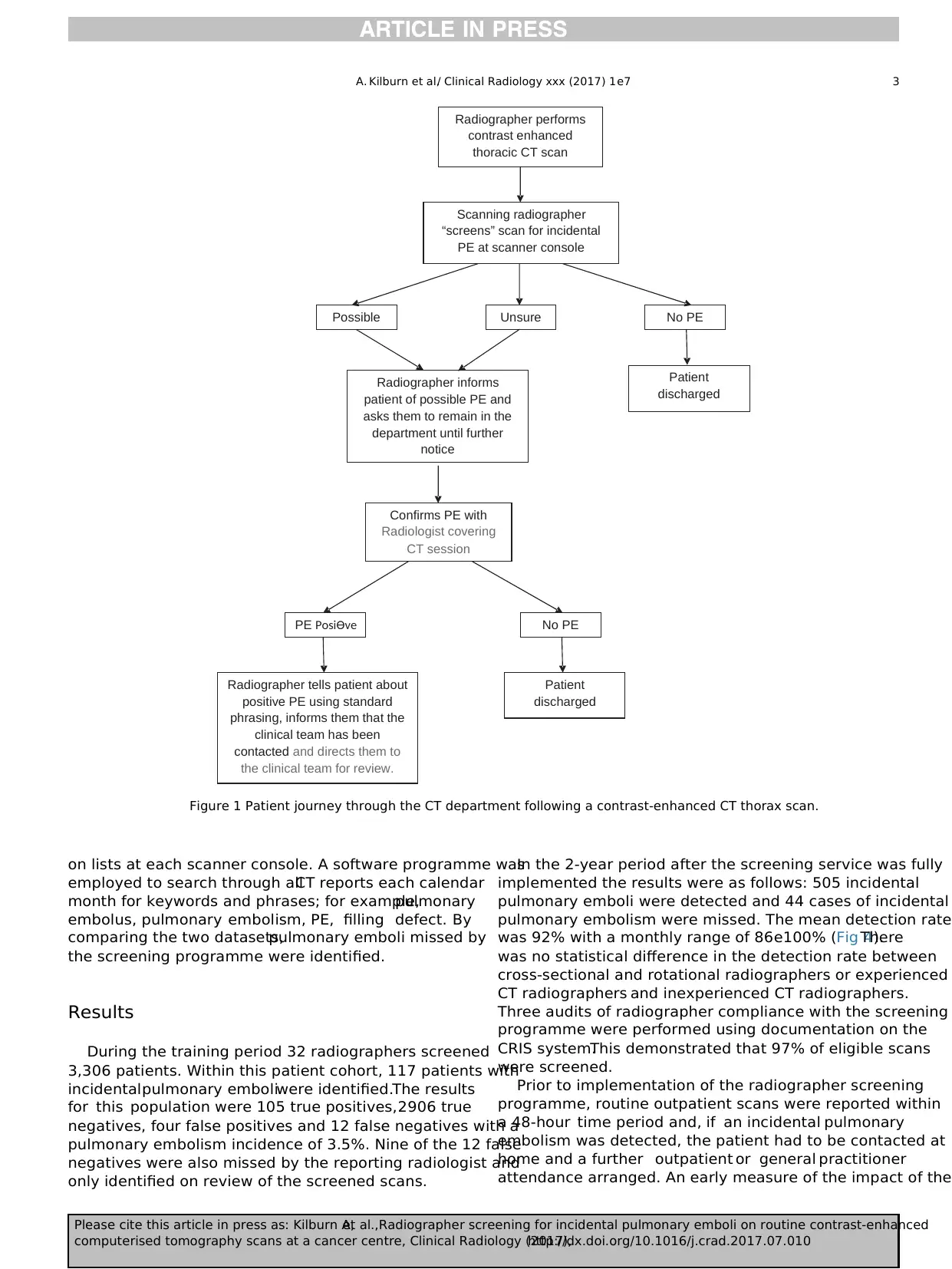
Robust lines of communication were essentialfor the
success ofthe screening programme.Radiographers and
radiologists had to understand and adhere to the stand-
ardised management of incidental pulmonary emboli (see
Figs 2e3).This included:
Radiographers asking the attending radiologist to
confirm a pulmonary embolus,informing the patient that
the scan was being reviewed and then informing the patient
when a pulmonary embolus was confirmed by the radiol-
ogist. They also told the patient where to go and who would
assess them for anticoagulant prescription.
Radiologists contacting the clinicalteam when a pul-
monary embolus was detected and making a note on the
picture archiving communication system (PACS) about the
pulmonary embolus if they were not responsible for issuing
the final CT report (to ensure that the finding was included
in the written report).
Quality assurance for the screening programme
All screen-detected pulmonary emboli were recorded on
the Computerised Radiology Information System (CRIS) and
A. Kilburn et al./ Clinical Radiology xxx (2017) 1e72
Please cite this article in press as: Kilburn A,et al.,Radiographer screening for incidental pulmonary emboli on routine contrast-enhanced
computerised tomography scans at a cancer centre, Clinical Radiology (2017), http://dx.doi.org/10.1016/j.crad.2017.07.010
pulmonary emboli and to assess its effectiveness in terms of
detection and time to patient treatment.To the authors’
knowledge, this is the first study to assess training efficacy
across a large cohort of radiographers working in CT on a
rotational basis, and to document the change in time taken
to institute treatment.A secondary aim was to assess staff
satisfaction with the extended role.
Materials and methods
The purpose of the training programme was to provide a
fast and effective radiographer-led screening programme
for incidental pulmonary embolism detection using routine
contrast-enhanced CT.As the responsibility for confirming
and reporting the presence of a pulmonary embolism
remained with the radiologist,there was no requirement
for formal ethics approval.
The intention was to integrate the screening programme
into the normalworking practices ofthe CT service with
radiographer screening taking place at the point of care in
the CT control room. CT lists included patients with all
histological types of cancer and were undertaken for stag-
ing, treatment response or follow-up.Apart from CT pul-
monary angiograms (CTPAs) and unenhanced studies, every
inpatient and outpatient contrast-enhanced CT thorax was
assessed,including patients with poor venous access or
suboptimal contrast enhancement. A flow-chart illustrating
the proposed patient journey through CT following a
contrast-enhanced thorax scan is included in Fig 1.
A pilot cohort of six cross-sectionalradiographers un-
derwent training.They read relevant literature on pulmo-
nary embolism prevalence,imaging criteria for detection,
and clinical management. They attended a series of prepared
lectures on the epidemiology and pathophysiology of pul-
monary embolism,normal intravenous contrast-enhanced
thoracic CT anatomy, the CT appearance of acute and
chronic pulmonary emboli, and potential reasons for
misdiagnosis.The radiographers then reviewed 20 cases
individually, followed by a group discussion. Thereafter, each
radiographer completed a log book of 100 cases, which were
all reviewed by the training radiologist.A post-training
standard of 90% detection was decided upon and audit of
the pilot cohort confirmed that the standard had been met.
The same training programme was then extended to include
all radiographic staff working in and rotating through the CT
department, irrespective of seniority and extent of previous
CT experience and the post-training standard was met by all.
Training of the entire radiographic stafftook 2 years 4
months before fullimplementation ofthe screening pro-
gramme was possible. Before that time, trained staff
screened all the patients they scanned. Several posters were
designed and placed in the CT control room to remind staff of
key CT imaging features of pulmonary emboli.
CT acquisition and review
CT images were acquired on all three CT systems including
a 16-multidetector CT system and two 64-multidetector
CT systems (Somatom Sensation 16 and Somatom AS Defi-
nition 64, Siemens, Erlangen Germany). Imaging parameters
on the 16 section system were standardised for all routine
protocols with 1.5 mm beam collimation,pitch 0.75,0.5
second rotation time, and 3 mm reconstructed section
thickness.On the 64-section system,the imaging parame-
ters were 0.6 mm beam collimation,pitch 1.2,0.5 second
rotation time, and 3 mm reconstructed section thickness.
According to body weight,70 or 85 ml of an iodinated
intravenous contrast medium iopamidol(300 mg iodine/
ml; Niopam 300,Bracco imaging Germany) was adminis-
tered at a rate of1e3 ml/s depending on venous access.
Scans were performed using a bolus-tracking technique
with a trigger threshold of 120 HU units.The imaging pro-
tocol was standardised for all patients who had an arterial
phase contrast-enhanced thorax scan.All images were
screened immediately following scan acquisition by the
radiographer performing the scan using the scanner work-
stations (Wizard,Navigator and Syngo Acquisition Work-
place,Siemens,Erlangen Germany).
Implementation of screening programme
Prior to full implementation of the screening programme,
a standard operating procedure (SOP)was developed to
support and integrate the screening programme into the
daily work of the CT department.This outlined governance
arrangements and detailed the roles and responsibilities of
all staff groups,pathways of communication,quality assur-
ance and continued radiographer training and audit.Pro-
cedures were also introduced for training new employees
and for management of an incidentally discovered pulmo-
nary embolus when no radiologist was immediately avail-
able,for example,at weekends.Signs were produced for
waiting areas to inform the patients thatthe screening
programme was in operation and that there might be an
additional wait if a pulmonary embolus was detected.
Robust lines of communication were essentialfor the
success ofthe screening programme.Radiographers and
radiologists had to understand and adhere to the stand-
ardised management of incidental pulmonary emboli (see
Figs 2e3).This included:
Radiographers asking the attending radiologist to
confirm a pulmonary embolus,informing the patient that
the scan was being reviewed and then informing the patient
when a pulmonary embolus was confirmed by the radiol-
ogist. They also told the patient where to go and who would
assess them for anticoagulant prescription.
Radiologists contacting the clinicalteam when a pul-
monary embolus was detected and making a note on the
picture archiving communication system (PACS) about the
pulmonary embolus if they were not responsible for issuing
the final CT report (to ensure that the finding was included
in the written report).
Quality assurance for the screening programme
All screen-detected pulmonary emboli were recorded on
the Computerised Radiology Information System (CRIS) and
A. Kilburn et al./ Clinical Radiology xxx (2017) 1e72
Please cite this article in press as: Kilburn A,et al.,Radiographer screening for incidental pulmonary emboli on routine contrast-enhanced
computerised tomography scans at a cancer centre, Clinical Radiology (2017), http://dx.doi.org/10.1016/j.crad.2017.07.010
on lists at each scanner console. A software programme was
employed to search through allCT reports each calendar
month for keywords and phrases; for example,pulmonary
embolus, pulmonary embolism, PE, filling defect. By
comparing the two datasets,pulmonary emboli missed by
the screening programme were identified.
Results
During the training period 32 radiographers screened
3,306 patients. Within this patient cohort, 117 patients with
incidentalpulmonary emboliwere identified.The results
for this population were 105 true positives,2906 true
negatives, four false positives and 12 false negatives with a
pulmonary embolism incidence of 3.5%. Nine of the 12 false
negatives were also missed by the reporting radiologist and
only identified on review of the screened scans.
In the 2-year period after the screening service was fully
implemented the results were as follows: 505 incidental
pulmonary emboli were detected and 44 cases of incidental
pulmonary embolism were missed. The mean detection rate
was 92% with a monthly range of 86e100% (Fig 4).There
was no statistical difference in the detection rate between
cross-sectional and rotational radiographers or experienced
CT radiographers and inexperienced CT radiographers.
Three audits of radiographer compliance with the screening
programme were performed using documentation on the
CRIS system.This demonstrated that 97% of eligible scans
were screened.
Prior to implementation of the radiographer screening
programme, routine outpatient scans were reported within
a 48-hour time period and, if an incidental pulmonary
embolism was detected, the patient had to be contacted at
home and a further outpatient or general practitioner
attendance arranged. An early measure of the impact of the
Radiographer performs
contrast enhanced
thoracic CT scan
Scanning radiographer
“screens” scan for incidental
PE at scanner console
Possible No PEUnsure
Patient
discharged
Radiographer informs
patient of possible PE and
asks them to remain in the
department until further
notice
Patient
discharged
Confirms PE with
Radiologist covering
CT session
PE PosiƟve No PE
Radiographer tells patient about
positive PE using standard
phrasing, informs them that the
clinical team has been
contacted and directs them to
the clinical team for review.
Figure 1 Patient journey through the CT department following a contrast-enhanced CT thorax scan.
A. Kilburn et al./ Clinical Radiology xxx (2017) 1e7 3
Please cite this article in press as: Kilburn A,et al.,Radiographer screening for incidental pulmonary emboli on routine contrast-enhanced
computerised tomography scans at a cancer centre, Clinical Radiology (2017),http://dx.doi.org/10.1016/j.crad.2017.07.010
employed to search through allCT reports each calendar
month for keywords and phrases; for example,pulmonary
embolus, pulmonary embolism, PE, filling defect. By
comparing the two datasets,pulmonary emboli missed by
the screening programme were identified.
Results
During the training period 32 radiographers screened
3,306 patients. Within this patient cohort, 117 patients with
incidentalpulmonary emboliwere identified.The results
for this population were 105 true positives,2906 true
negatives, four false positives and 12 false negatives with a
pulmonary embolism incidence of 3.5%. Nine of the 12 false
negatives were also missed by the reporting radiologist and
only identified on review of the screened scans.
In the 2-year period after the screening service was fully
implemented the results were as follows: 505 incidental
pulmonary emboli were detected and 44 cases of incidental
pulmonary embolism were missed. The mean detection rate
was 92% with a monthly range of 86e100% (Fig 4).There
was no statistical difference in the detection rate between
cross-sectional and rotational radiographers or experienced
CT radiographers and inexperienced CT radiographers.
Three audits of radiographer compliance with the screening
programme were performed using documentation on the
CRIS system.This demonstrated that 97% of eligible scans
were screened.
Prior to implementation of the radiographer screening
programme, routine outpatient scans were reported within
a 48-hour time period and, if an incidental pulmonary
embolism was detected, the patient had to be contacted at
home and a further outpatient or general practitioner
attendance arranged. An early measure of the impact of the
Radiographer performs
contrast enhanced
thoracic CT scan
Scanning radiographer
“screens” scan for incidental
PE at scanner console
Possible No PEUnsure
Patient
discharged
Radiographer informs
patient of possible PE and
asks them to remain in the
department until further
notice
Patient
discharged
Confirms PE with
Radiologist covering
CT session
PE PosiƟve No PE
Radiographer tells patient about
positive PE using standard
phrasing, informs them that the
clinical team has been
contacted and directs them to
the clinical team for review.
Figure 1 Patient journey through the CT department following a contrast-enhanced CT thorax scan.
A. Kilburn et al./ Clinical Radiology xxx (2017) 1e7 3
Please cite this article in press as: Kilburn A,et al.,Radiographer screening for incidental pulmonary emboli on routine contrast-enhanced
computerised tomography scans at a cancer centre, Clinical Radiology (2017),http://dx.doi.org/10.1016/j.crad.2017.07.010
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
screening programme on patient management involved a
direct comparison of the time from the scan to the clinical
consultation for anticoagulant prescription.This was done
for 30 patients imaged before the screening programme
began and 30 patients imaged after screening was intro-
duced (Table 1).Seven patients in the pre-screening group
and six in the screened group were already on anticoagu-
lants. In the screened group, each of these patients had their
anticoagulant therapy reviewed at the same attendance. Of
the six patients already on anticoagulants, two were found
to have been inadequately anticoagulated and medication
was increased immediately.Two patients went on to have
an inferior vena cava (IVC) filter inserted.
Of the patients not receiving anticoagulation therapy
scanned prior to implementation of screening,two of 23
(8.7%) patients received treatment on the same day as the
scan, compared to 19 of 24 patients identified by screening
(79%).Of the five screened patients who did not receive
anticoagulants on the same day, one received treatment the
following day,although the reason for this was not docu-
mented. Three received no anticoagulation despite the
screen-detected pulmonary embolus for the following rea-
sons: significant disease progression with referralto a
hospice (n¼1),sepsis and a haemorrhagic brain metastasis
(n¼1), a small pulmonary embolus felt to be chronic (n¼1).
No record was found in the notes of one patient regarding
any treatment decisions regarding the pulmonary
embolism.
Following full implementation of the screening pro-
gramme, a retrospective study of 100 patients also
PE FLOWCHART
RADIOGRAPHERS
On anticoagulants
?PE Radiologist ?PE Radiologist Known PE Radiologists No PE
No Yes Yes
)
Add to list outside CT rooms
Enter into CRIS notes:
Annotate patient questionnaire
Add to list outside CT rooms
Enter into CRIS notes:
Annotate patient questionnaire
Annotate patient
questionnaire
Annotate patient
questionnaire
Figure 2 Radiographer flow chart for management of possible incidental pulmonary emboli.
PE FLOWCHART
RADIOLOGISTS
PE NO PE YES PE YES PE YES Radiographers have missed PE
(Big, Medium & Small)
END Reporting scan Not reporting scan Known PE
Contact Clinical Team
Contact Clinical Team Contact Clinical Team Already on anticoagulants
Mark PE on image
Make PACS note:
“PE detected, clinical
team contacted”
Include in report
Add case to missed
pulmonary emboli folder
Mark PE on image
Make PACS note:
“Known PE detected,
already on anticoagulants”
Include in report
Figure 3 Radiologist flow chart for management of possible incidental pulmonary emboli.
A. Kilburn et al./ Clinical Radiology xxx (2017) 1e74
Please cite this article in press as: Kilburn A,et al.,Radiographer screening for incidental pulmonary emboli on routine contrast-enhanced
computerised tomography scans at a cancer centre, Clinical Radiology (2017), http://dx.doi.org/10.1016/j.crad.2017.07.010
direct comparison of the time from the scan to the clinical
consultation for anticoagulant prescription.This was done
for 30 patients imaged before the screening programme
began and 30 patients imaged after screening was intro-
duced (Table 1).Seven patients in the pre-screening group
and six in the screened group were already on anticoagu-
lants. In the screened group, each of these patients had their
anticoagulant therapy reviewed at the same attendance. Of
the six patients already on anticoagulants, two were found
to have been inadequately anticoagulated and medication
was increased immediately.Two patients went on to have
an inferior vena cava (IVC) filter inserted.
Of the patients not receiving anticoagulation therapy
scanned prior to implementation of screening,two of 23
(8.7%) patients received treatment on the same day as the
scan, compared to 19 of 24 patients identified by screening
(79%).Of the five screened patients who did not receive
anticoagulants on the same day, one received treatment the
following day,although the reason for this was not docu-
mented. Three received no anticoagulation despite the
screen-detected pulmonary embolus for the following rea-
sons: significant disease progression with referralto a
hospice (n¼1),sepsis and a haemorrhagic brain metastasis
(n¼1), a small pulmonary embolus felt to be chronic (n¼1).
No record was found in the notes of one patient regarding
any treatment decisions regarding the pulmonary
embolism.
Following full implementation of the screening pro-
gramme, a retrospective study of 100 patients also
PE FLOWCHART
RADIOGRAPHERS
On anticoagulants
?PE Radiologist ?PE Radiologist Known PE Radiologists No PE
No Yes Yes
)
Add to list outside CT rooms
Enter into CRIS notes:
Annotate patient questionnaire
Add to list outside CT rooms
Enter into CRIS notes:
Annotate patient questionnaire
Annotate patient
questionnaire
Annotate patient
questionnaire
Figure 2 Radiographer flow chart for management of possible incidental pulmonary emboli.
PE FLOWCHART
RADIOLOGISTS
PE NO PE YES PE YES PE YES Radiographers have missed PE
(Big, Medium & Small)
END Reporting scan Not reporting scan Known PE
Contact Clinical Team
Contact Clinical Team Contact Clinical Team Already on anticoagulants
Mark PE on image
Make PACS note:
“PE detected, clinical
team contacted”
Include in report
Add case to missed
pulmonary emboli folder
Mark PE on image
Make PACS note:
“Known PE detected,
already on anticoagulants”
Include in report
Figure 3 Radiologist flow chart for management of possible incidental pulmonary emboli.
A. Kilburn et al./ Clinical Radiology xxx (2017) 1e74
Please cite this article in press as: Kilburn A,et al.,Radiographer screening for incidental pulmonary emboli on routine contrast-enhanced
computerised tomography scans at a cancer centre, Clinical Radiology (2017), http://dx.doi.org/10.1016/j.crad.2017.07.010
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
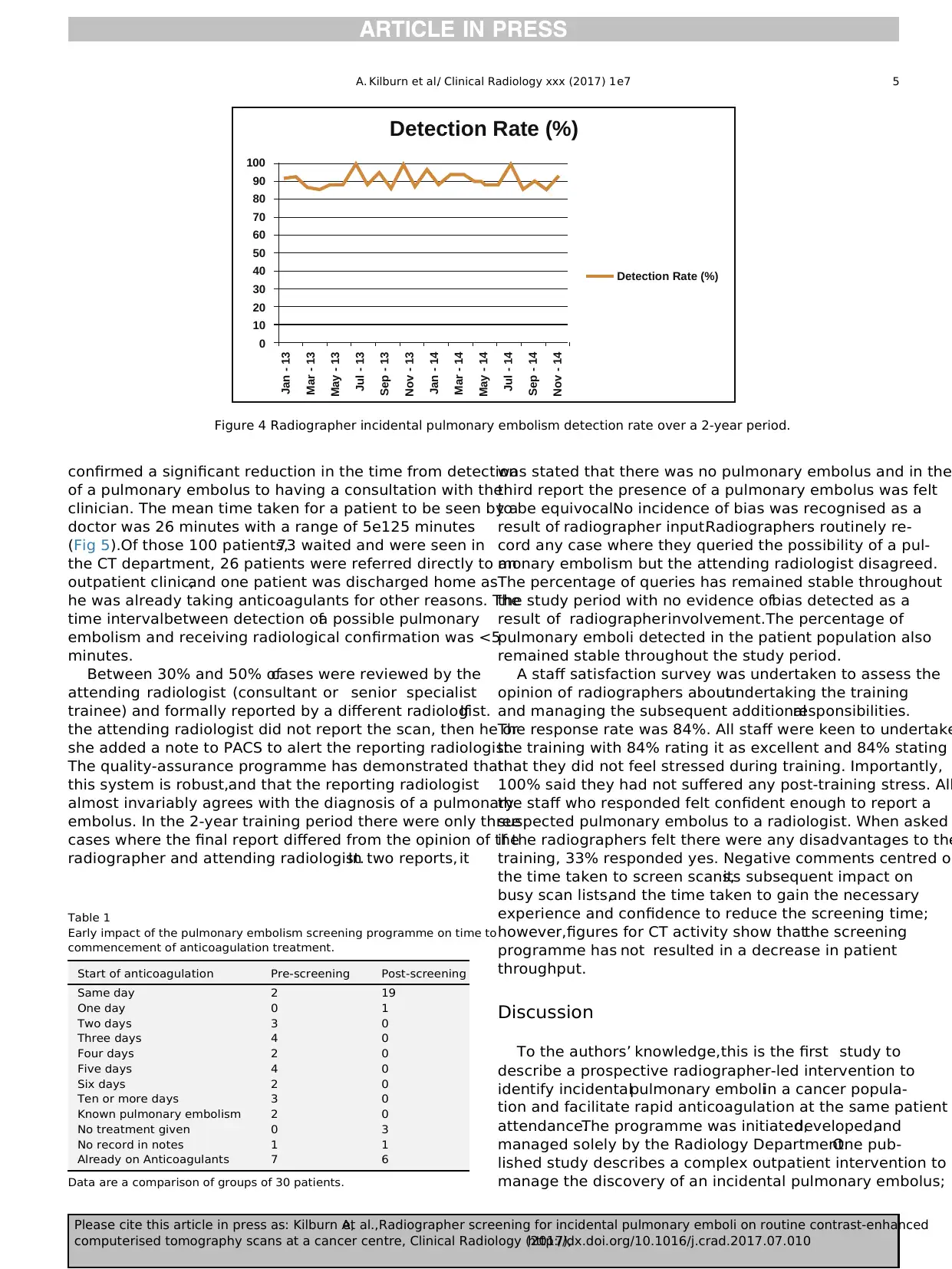
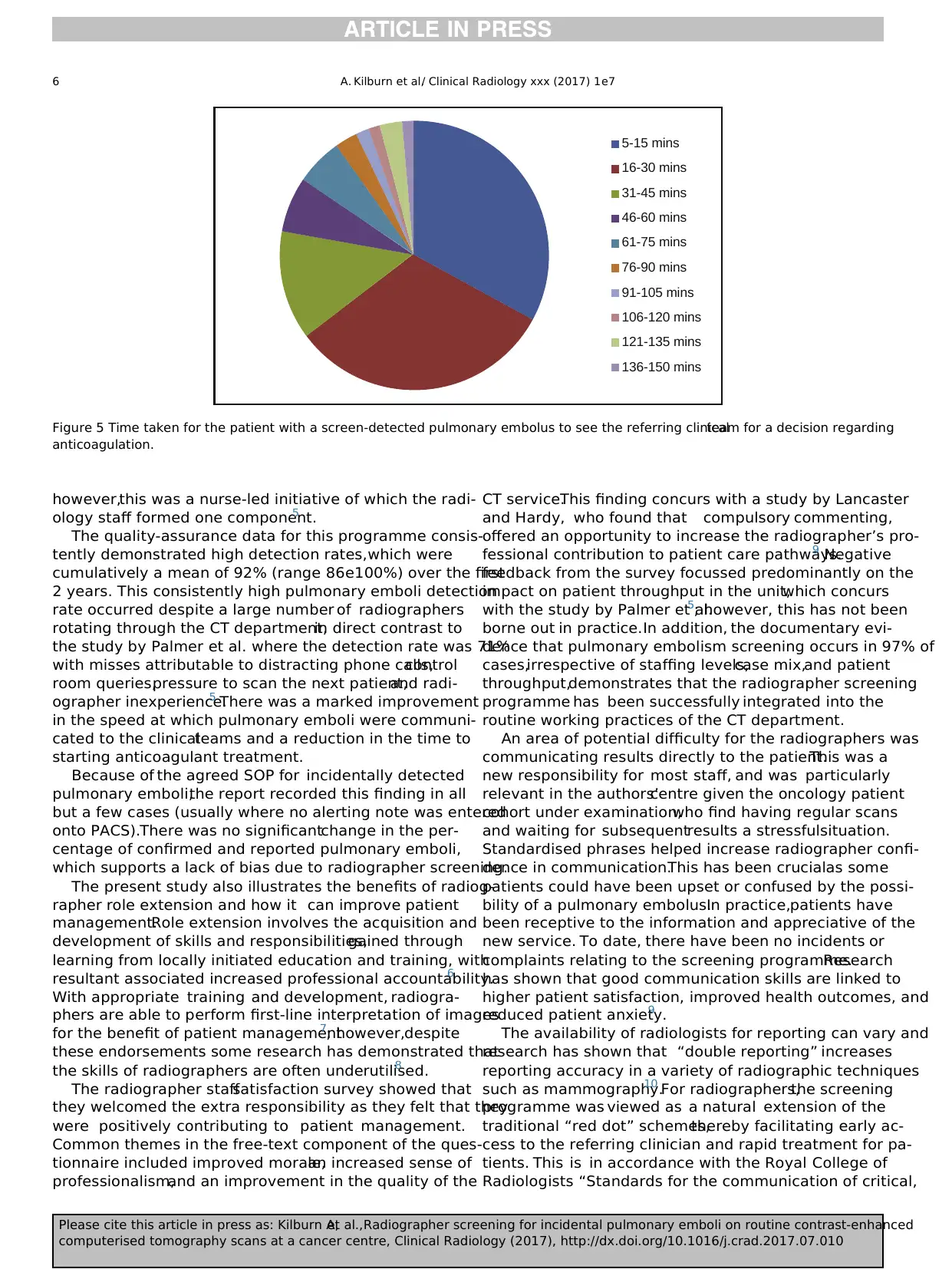
confirmed a significant reduction in the time from detection
of a pulmonary embolus to having a consultation with the
clinician. The mean time taken for a patient to be seen by a
doctor was 26 minutes with a range of 5e125 minutes
(Fig 5).Of those 100 patients,73 waited and were seen in
the CT department, 26 patients were referred directly to an
outpatient clinic,and one patient was discharged home as
he was already taking anticoagulants for other reasons. The
time intervalbetween detection ofa possible pulmonary
embolism and receiving radiological confirmation was <5
minutes.
Between 30% and 50% ofcases were reviewed by the
attending radiologist (consultant or senior specialist
trainee) and formally reported by a different radiologist.If
the attending radiologist did not report the scan, then he or
she added a note to PACS to alert the reporting radiologist.
The quality-assurance programme has demonstrated that
this system is robust,and that the reporting radiologist
almost invariably agrees with the diagnosis of a pulmonary
embolus. In the 2-year training period there were only three
cases where the final report differed from the opinion of the
radiographer and attending radiologist.In two reports, it
was stated that there was no pulmonary embolus and in the
third report the presence of a pulmonary embolus was felt
to be equivocal.No incidence of bias was recognised as a
result of radiographer input.Radiographers routinely re-
cord any case where they queried the possibility of a pul-
monary embolism but the attending radiologist disagreed.
The percentage of queries has remained stable throughout
the study period with no evidence ofbias detected as a
result of radiographerinvolvement.The percentage of
pulmonary emboli detected in the patient population also
remained stable throughout the study period.
A staff satisfaction survey was undertaken to assess the
opinion of radiographers aboutundertaking the training
and managing the subsequent additionalresponsibilities.
The response rate was 84%. All staff were keen to undertake
the training with 84% rating it as excellent and 84% stating
that they did not feel stressed during training. Importantly,
100% said they had not suffered any post-training stress. All
the staff who responded felt confident enough to report a
suspected pulmonary embolus to a radiologist. When asked
if the radiographers felt there were any disadvantages to the
training, 33% responded yes. Negative comments centred on
the time taken to screen scans,its subsequent impact on
busy scan lists,and the time taken to gain the necessary
experience and confidence to reduce the screening time;
however,figures for CT activity show thatthe screening
programme has not resulted in a decrease in patient
throughput.
Discussion
To the authors’ knowledge,this is the first study to
describe a prospective radiographer-led intervention to
identify incidentalpulmonary emboliin a cancer popula-
tion and facilitate rapid anticoagulation at the same patient
attendance.The programme was initiated,developed,and
managed solely by the Radiology Department.One pub-
lished study describes a complex outpatient intervention to
manage the discovery of an incidental pulmonary embolus;
Detection Rate (%)
Detection Rate (%)
100
90
80
70
60
50
40
30
20
10
0
Jan - 13
Mar - 13
May - 13
Jul - 13
Sep - 13
Nov - 13
Jan - 14
Mar - 14
May - 14
Jul - 14
Sep - 14
Nov - 14
Figure 4 Radiographer incidental pulmonary embolism detection rate over a 2-year period.
Table 1
Early impact of the pulmonary embolism screening programme on time to
commencement of anticoagulation treatment.
Start of anticoagulation Pre-screening Post-screening
Same day 2 19
One day 0 1
Two days 3 0
Three days 4 0
Four days 2 0
Five days 4 0
Six days 2 0
Ten or more days 3 0
Known pulmonary embolism 2 0
No treatment given 0 3
No record in notes 1 1
Already on Anticoagulants 7 6
Data are a comparison of groups of 30 patients.
A. Kilburn et al./ Clinical Radiology xxx (2017) 1e7 5
Please cite this article in press as: Kilburn A,et al.,Radiographer screening for incidental pulmonary emboli on routine contrast-enhanced
computerised tomography scans at a cancer centre, Clinical Radiology (2017),http://dx.doi.org/10.1016/j.crad.2017.07.010
of a pulmonary embolus to having a consultation with the
clinician. The mean time taken for a patient to be seen by a
doctor was 26 minutes with a range of 5e125 minutes
(Fig 5).Of those 100 patients,73 waited and were seen in
the CT department, 26 patients were referred directly to an
outpatient clinic,and one patient was discharged home as
he was already taking anticoagulants for other reasons. The
time intervalbetween detection ofa possible pulmonary
embolism and receiving radiological confirmation was <5
minutes.
Between 30% and 50% ofcases were reviewed by the
attending radiologist (consultant or senior specialist
trainee) and formally reported by a different radiologist.If
the attending radiologist did not report the scan, then he or
she added a note to PACS to alert the reporting radiologist.
The quality-assurance programme has demonstrated that
this system is robust,and that the reporting radiologist
almost invariably agrees with the diagnosis of a pulmonary
embolus. In the 2-year training period there were only three
cases where the final report differed from the opinion of the
radiographer and attending radiologist.In two reports, it
was stated that there was no pulmonary embolus and in the
third report the presence of a pulmonary embolus was felt
to be equivocal.No incidence of bias was recognised as a
result of radiographer input.Radiographers routinely re-
cord any case where they queried the possibility of a pul-
monary embolism but the attending radiologist disagreed.
The percentage of queries has remained stable throughout
the study period with no evidence ofbias detected as a
result of radiographerinvolvement.The percentage of
pulmonary emboli detected in the patient population also
remained stable throughout the study period.
A staff satisfaction survey was undertaken to assess the
opinion of radiographers aboutundertaking the training
and managing the subsequent additionalresponsibilities.
The response rate was 84%. All staff were keen to undertake
the training with 84% rating it as excellent and 84% stating
that they did not feel stressed during training. Importantly,
100% said they had not suffered any post-training stress. All
the staff who responded felt confident enough to report a
suspected pulmonary embolus to a radiologist. When asked
if the radiographers felt there were any disadvantages to the
training, 33% responded yes. Negative comments centred on
the time taken to screen scans,its subsequent impact on
busy scan lists,and the time taken to gain the necessary
experience and confidence to reduce the screening time;
however,figures for CT activity show thatthe screening
programme has not resulted in a decrease in patient
throughput.
Discussion
To the authors’ knowledge,this is the first study to
describe a prospective radiographer-led intervention to
identify incidentalpulmonary emboliin a cancer popula-
tion and facilitate rapid anticoagulation at the same patient
attendance.The programme was initiated,developed,and
managed solely by the Radiology Department.One pub-
lished study describes a complex outpatient intervention to
manage the discovery of an incidental pulmonary embolus;
Detection Rate (%)
Detection Rate (%)
100
90
80
70
60
50
40
30
20
10
0
Jan - 13
Mar - 13
May - 13
Jul - 13
Sep - 13
Nov - 13
Jan - 14
Mar - 14
May - 14
Jul - 14
Sep - 14
Nov - 14
Figure 4 Radiographer incidental pulmonary embolism detection rate over a 2-year period.
Table 1
Early impact of the pulmonary embolism screening programme on time to
commencement of anticoagulation treatment.
Start of anticoagulation Pre-screening Post-screening
Same day 2 19
One day 0 1
Two days 3 0
Three days 4 0
Four days 2 0
Five days 4 0
Six days 2 0
Ten or more days 3 0
Known pulmonary embolism 2 0
No treatment given 0 3
No record in notes 1 1
Already on Anticoagulants 7 6
Data are a comparison of groups of 30 patients.
A. Kilburn et al./ Clinical Radiology xxx (2017) 1e7 5
Please cite this article in press as: Kilburn A,et al.,Radiographer screening for incidental pulmonary emboli on routine contrast-enhanced
computerised tomography scans at a cancer centre, Clinical Radiology (2017),http://dx.doi.org/10.1016/j.crad.2017.07.010
however,this was a nurse-led initiative of which the radi-
ology staff formed one component.5
The quality-assurance data for this programme consis-
tently demonstrated high detection rates,which were
cumulatively a mean of 92% (range 86e100%) over the first
2 years. This consistently high pulmonary emboli detection
rate occurred despite a large number of radiographers
rotating through the CT department,in direct contrast to
the study by Palmer et al. where the detection rate was 71%
with misses attributable to distracting phone calls,control
room queries,pressure to scan the next patient,and radi-
ographer inexperience.5 There was a marked improvement
in the speed at which pulmonary emboli were communi-
cated to the clinicalteams and a reduction in the time to
starting anticoagulant treatment.
Because of the agreed SOP for incidentally detected
pulmonary emboli,the report recorded this finding in all
but a few cases (usually where no alerting note was entered
onto PACS).There was no significantchange in the per-
centage of confirmed and reported pulmonary emboli,
which supports a lack of bias due to radiographer screening.
The present study also illustrates the benefits of radiog-
rapher role extension and how it can improve patient
management.Role extension involves the acquisition and
development of skills and responsibilities,gained through
learning from locally initiated education and training, with
resultant associated increased professional accountability.6
With appropriate training and development, radiogra-
phers are able to perform first-line interpretation of images
for the benefit of patient management7
; however,despite
these endorsements some research has demonstrated that
the skills of radiographers are often underutilised.8
The radiographer staffsatisfaction survey showed that
they welcomed the extra responsibility as they felt that they
were positively contributing to patient management.
Common themes in the free-text component of the ques-
tionnaire included improved morale,an increased sense of
professionalism,and an improvement in the quality of the
CT service.This finding concurs with a study by Lancaster
and Hardy, who found that compulsory commenting,
offered an opportunity to increase the radiographer’s pro-
fessional contribution to patient care pathways.9 Negative
feedback from the survey focussed predominantly on the
impact on patient throughput in the unit,which concurs
with the study by Palmer et al.5
; however, this has not been
borne out in practice.In addition, the documentary evi-
dence that pulmonary embolism screening occurs in 97% of
cases,irrespective of staffing levels,case mix,and patient
throughput,demonstrates that the radiographer screening
programme has been successfully integrated into the
routine working practices of the CT department.
An area of potential difficulty for the radiographers was
communicating results directly to the patient.This was a
new responsibility for most staff, and was particularly
relevant in the authors’centre given the oncology patient
cohort under examination,who find having regular scans
and waiting for subsequentresults a stressfulsituation.
Standardised phrases helped increase radiographer confi-
dence in communication.This has been crucialas some
patients could have been upset or confused by the possi-
bility of a pulmonary embolus.In practice,patients have
been receptive to the information and appreciative of the
new service. To date, there have been no incidents or
complaints relating to the screening programme.Research
has shown that good communication skills are linked to
higher patient satisfaction, improved health outcomes, and
reduced patient anxiety.9
The availability of radiologists for reporting can vary and
research has shown that “double reporting” increases
reporting accuracy in a variety of radiographic techniques
such as mammography.10 For radiographers,the screening
programme was viewed as a natural extension of the
traditional “red dot” schemes,thereby facilitating early ac-
cess to the referring clinician and rapid treatment for pa-
tients. This is in accordance with the Royal College of
Radiologists “Standards for the communication of critical,
5-15 mins
16-30 mins
31-45 mins
46-60 mins
61-75 mins
76-90 mins
91-105 mins
106-120 mins
121-135 mins
136-150 mins
Figure 5 Time taken for the patient with a screen-detected pulmonary embolus to see the referring clinicalteam for a decision regarding
anticoagulation.
A. Kilburn et al./ Clinical Radiology xxx (2017) 1e76
Please cite this article in press as: Kilburn A,et al.,Radiographer screening for incidental pulmonary emboli on routine contrast-enhanced
computerised tomography scans at a cancer centre, Clinical Radiology (2017), http://dx.doi.org/10.1016/j.crad.2017.07.010
ology staff formed one component.5
The quality-assurance data for this programme consis-
tently demonstrated high detection rates,which were
cumulatively a mean of 92% (range 86e100%) over the first
2 years. This consistently high pulmonary emboli detection
rate occurred despite a large number of radiographers
rotating through the CT department,in direct contrast to
the study by Palmer et al. where the detection rate was 71%
with misses attributable to distracting phone calls,control
room queries,pressure to scan the next patient,and radi-
ographer inexperience.5 There was a marked improvement
in the speed at which pulmonary emboli were communi-
cated to the clinicalteams and a reduction in the time to
starting anticoagulant treatment.
Because of the agreed SOP for incidentally detected
pulmonary emboli,the report recorded this finding in all
but a few cases (usually where no alerting note was entered
onto PACS).There was no significantchange in the per-
centage of confirmed and reported pulmonary emboli,
which supports a lack of bias due to radiographer screening.
The present study also illustrates the benefits of radiog-
rapher role extension and how it can improve patient
management.Role extension involves the acquisition and
development of skills and responsibilities,gained through
learning from locally initiated education and training, with
resultant associated increased professional accountability.6
With appropriate training and development, radiogra-
phers are able to perform first-line interpretation of images
for the benefit of patient management7
; however,despite
these endorsements some research has demonstrated that
the skills of radiographers are often underutilised.8
The radiographer staffsatisfaction survey showed that
they welcomed the extra responsibility as they felt that they
were positively contributing to patient management.
Common themes in the free-text component of the ques-
tionnaire included improved morale,an increased sense of
professionalism,and an improvement in the quality of the
CT service.This finding concurs with a study by Lancaster
and Hardy, who found that compulsory commenting,
offered an opportunity to increase the radiographer’s pro-
fessional contribution to patient care pathways.9 Negative
feedback from the survey focussed predominantly on the
impact on patient throughput in the unit,which concurs
with the study by Palmer et al.5
; however, this has not been
borne out in practice.In addition, the documentary evi-
dence that pulmonary embolism screening occurs in 97% of
cases,irrespective of staffing levels,case mix,and patient
throughput,demonstrates that the radiographer screening
programme has been successfully integrated into the
routine working practices of the CT department.
An area of potential difficulty for the radiographers was
communicating results directly to the patient.This was a
new responsibility for most staff, and was particularly
relevant in the authors’centre given the oncology patient
cohort under examination,who find having regular scans
and waiting for subsequentresults a stressfulsituation.
Standardised phrases helped increase radiographer confi-
dence in communication.This has been crucialas some
patients could have been upset or confused by the possi-
bility of a pulmonary embolus.In practice,patients have
been receptive to the information and appreciative of the
new service. To date, there have been no incidents or
complaints relating to the screening programme.Research
has shown that good communication skills are linked to
higher patient satisfaction, improved health outcomes, and
reduced patient anxiety.9
The availability of radiologists for reporting can vary and
research has shown that “double reporting” increases
reporting accuracy in a variety of radiographic techniques
such as mammography.10 For radiographers,the screening
programme was viewed as a natural extension of the
traditional “red dot” schemes,thereby facilitating early ac-
cess to the referring clinician and rapid treatment for pa-
tients. This is in accordance with the Royal College of
Radiologists “Standards for the communication of critical,
5-15 mins
16-30 mins
31-45 mins
46-60 mins
61-75 mins
76-90 mins
91-105 mins
106-120 mins
121-135 mins
136-150 mins
Figure 5 Time taken for the patient with a screen-detected pulmonary embolus to see the referring clinicalteam for a decision regarding
anticoagulation.
A. Kilburn et al./ Clinical Radiology xxx (2017) 1e76
Please cite this article in press as: Kilburn A,et al.,Radiographer screening for incidental pulmonary emboli on routine contrast-enhanced
computerised tomography scans at a cancer centre, Clinical Radiology (2017), http://dx.doi.org/10.1016/j.crad.2017.07.010
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide

urgent and unexpected significantradiologicalfindings”
where an incidental pulmonary embolus may be classed as
a significant finding where the reporting radiologist is con-
cerned that the image findings are significant for the patient
but may be unexpected by the referrer.11 The programme
model developed in this study is one that could be adopted
in other hospitals and offers more rapid management of
incidental pulmonary emboli discovered on routine CT.
In conclusion,radiographers were effective in first-line
screening for incidental pulmonary emboli on routine
contrast-enhanced thoracic CT. Screening led to a reduction
in delay in commencing anticoagulanttreatment,which
was prescribed at the same outpatientattendance.The
trained radiographers identified benefits including
increased knowledge and improved quality of service.
References
1. Sebastian AJ, Paddon AJ. Clinically unsuspected pulmonary embolism dan
important secondary finding in oncology CT. Clin Radiol 2006;61:81e5.
2. Den-Exter PL,Jimenez D, Kroft LJ, et al. Outcome of incidentally diag-
nosed pulmonary embolism in patients with malignancy. Curr Opin Pulm
Med 2012;18(5):399e405.
3. Den-Exter PL, Hooijer J, Dekkers OM, et al. Risk of recurrent venous
thromboembolism and mortality in patients with cancer incidentally
diagnosed with pulmonary embolism: a comparison with symptomatic
patients.J Clin Oncol 2011;29:2405e9.
5. Palmer J,Bozas G,Stephens A,et al.Developing a complex intervention
for the outpatient management ofincidentally diagnosed pulmonary
embolism in cancer patients. BMC Health Services Research 2013;13:235.
6. Hardy M, Snaith B.Role extension and role advancement d is there a
difference? A discussion paper.Radiography 2006;12.
7. Beardmore C.Preliminary clinicalevaluation and clinicalreporting by
radiographers:policy and practice guidance.The Society of Radiogra-
phers; 2013.p. 1e11.Available at: https://www.sor.org.Accessed 21/07/
2014
8. Hardy M, Hutton J,Snaith B.Is a radiographer led immediate reporting
service for emergency department referrals a cost effective initiative?
Radiography 2013;17:275e9.
9. LancasterM, Hardy M. An investigation into the opportunities and
barriers to participation in a radiographer comment scheme, in a multi-
centre NHS Trust.Radiography 2012;18:105e8.
10. Murphy R, Slater A,Uberoi R, et al. Reduction of perception error by
double reporting of minimal preparation CT colon. Br J Radiol
2010;83:331e5.
11. The Royal College of Radiologists.Standards for the communication of
critical, urgent and unexpected radiological findings. 2nd edn. London: The
Royal College of Radiologists; 2012.
A. Kilburn et al./ Clinical Radiology xxx (2017) 1e7 7
Please cite this article in press as: Kilburn A,et al.,Radiographer screening for incidental pulmonary emboli on routine contrast-enhanced
computerised tomography scans at a cancer centre, Clinical Radiology (2017),http://dx.doi.org/10.1016/j.crad.2017.07.010
where an incidental pulmonary embolus may be classed as
a significant finding where the reporting radiologist is con-
cerned that the image findings are significant for the patient
but may be unexpected by the referrer.11 The programme
model developed in this study is one that could be adopted
in other hospitals and offers more rapid management of
incidental pulmonary emboli discovered on routine CT.
In conclusion,radiographers were effective in first-line
screening for incidental pulmonary emboli on routine
contrast-enhanced thoracic CT. Screening led to a reduction
in delay in commencing anticoagulanttreatment,which
was prescribed at the same outpatientattendance.The
trained radiographers identified benefits including
increased knowledge and improved quality of service.
References
1. Sebastian AJ, Paddon AJ. Clinically unsuspected pulmonary embolism dan
important secondary finding in oncology CT. Clin Radiol 2006;61:81e5.
2. Den-Exter PL,Jimenez D, Kroft LJ, et al. Outcome of incidentally diag-
nosed pulmonary embolism in patients with malignancy. Curr Opin Pulm
Med 2012;18(5):399e405.
3. Den-Exter PL, Hooijer J, Dekkers OM, et al. Risk of recurrent venous
thromboembolism and mortality in patients with cancer incidentally
diagnosed with pulmonary embolism: a comparison with symptomatic
patients.J Clin Oncol 2011;29:2405e9.
5. Palmer J,Bozas G,Stephens A,et al.Developing a complex intervention
for the outpatient management ofincidentally diagnosed pulmonary
embolism in cancer patients. BMC Health Services Research 2013;13:235.
6. Hardy M, Snaith B.Role extension and role advancement d is there a
difference? A discussion paper.Radiography 2006;12.
7. Beardmore C.Preliminary clinicalevaluation and clinicalreporting by
radiographers:policy and practice guidance.The Society of Radiogra-
phers; 2013.p. 1e11.Available at: https://www.sor.org.Accessed 21/07/
2014
8. Hardy M, Hutton J,Snaith B.Is a radiographer led immediate reporting
service for emergency department referrals a cost effective initiative?
Radiography 2013;17:275e9.
9. LancasterM, Hardy M. An investigation into the opportunities and
barriers to participation in a radiographer comment scheme, in a multi-
centre NHS Trust.Radiography 2012;18:105e8.
10. Murphy R, Slater A,Uberoi R, et al. Reduction of perception error by
double reporting of minimal preparation CT colon. Br J Radiol
2010;83:331e5.
11. The Royal College of Radiologists.Standards for the communication of
critical, urgent and unexpected radiological findings. 2nd edn. London: The
Royal College of Radiologists; 2012.
A. Kilburn et al./ Clinical Radiology xxx (2017) 1e7 7
Please cite this article in press as: Kilburn A,et al.,Radiographer screening for incidental pulmonary emboli on routine contrast-enhanced
computerised tomography scans at a cancer centre, Clinical Radiology (2017),http://dx.doi.org/10.1016/j.crad.2017.07.010
1 out of 7
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2025 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.