Maternal and Neonatal Health: Importance, Determinants and Intervention Strategies
VerifiedAdded on 2022/10/06
|13
|3116
|263
AI Summary
This article discusses the importance of maternal and neonatal health, determinants affecting their health, and intervention strategies to improve their health outcomes. It also highlights the role of community-based interventions and increasing awareness to promote maternal and neonatal health.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.
Running head:WOMEN'S AND CHILD WELFARE
WOMEN'S AND CHILD WELFARE
Name of the student
Name of the university
Author’s name
WOMEN'S AND CHILD WELFARE
Name of the student
Name of the university
Author’s name
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
WOMEN'S AND CHILD WELFARE
Introduction
There is an increasing number of evidence on the relationship between maternal and
neonatal health. The treatment women received in their pre-pregnancy, during the course of
pregnancy and during childbirth have a strong impact on the health of the newborn. According to
the study by Lassi et al., (2013), the strategies to improve maternal and newborn health are
therefore interlinked. Evidences have shown that an estimated 250000-280000 women dies every
year worldwide and over 15 million women suffers from chronic diseases because of the
complications due to pregnancy and child birth. Maternal health complications have been found
to be contributing to 1.5 million neonatal deaths in their first week of life and a 1.4 million
miscarriages (Lassi et al., 2013). It was found from the evidences on the role of community
based settings in improving maternal and neonatal health. Even though, the strategies vary
significantly, interventions planned based on community settings are believed to encourage a
healthier practice of care incorporating and employing local community members in the
provision of services including diagnosis and treatment and referral (Black et al., 2016).
Discussion
Why are maternal and neonatal Health important?
Wellbeing of mothers and early neonatal helps to determine and predict the next
generation health status and future family and community health problems (Healthypeople.gov,
2019). A neonatal's health is an important factor for his health and well-being during his lifespan.
Maternal health and the neonatal wellbeing influence variables such as education, public stability
and their sensitivity to negative actions. In Australia, more than 300,000 babies born each year is
Introduction
There is an increasing number of evidence on the relationship between maternal and
neonatal health. The treatment women received in their pre-pregnancy, during the course of
pregnancy and during childbirth have a strong impact on the health of the newborn. According to
the study by Lassi et al., (2013), the strategies to improve maternal and newborn health are
therefore interlinked. Evidences have shown that an estimated 250000-280000 women dies every
year worldwide and over 15 million women suffers from chronic diseases because of the
complications due to pregnancy and child birth. Maternal health complications have been found
to be contributing to 1.5 million neonatal deaths in their first week of life and a 1.4 million
miscarriages (Lassi et al., 2013). It was found from the evidences on the role of community
based settings in improving maternal and neonatal health. Even though, the strategies vary
significantly, interventions planned based on community settings are believed to encourage a
healthier practice of care incorporating and employing local community members in the
provision of services including diagnosis and treatment and referral (Black et al., 2016).
Discussion
Why are maternal and neonatal Health important?
Wellbeing of mothers and early neonatal helps to determine and predict the next
generation health status and future family and community health problems (Healthypeople.gov,
2019). A neonatal's health is an important factor for his health and well-being during his lifespan.
Maternal health and the neonatal wellbeing influence variables such as education, public stability
and their sensitivity to negative actions. In Australia, more than 300,000 babies born each year is
WOMEN'S AND CHILD WELFARE
increasing rapidly. Therefore, for mothers it is important to keep themselves healthy by
maintaining a healthy lifestyle that will attending regular neonatal care services in order to get
improved heath outcome for both the mother and child. Pregnancy provides opportunity for
identifying health risks and preventing health problems for women and neonates. The health
risks includes diabetes, depression, genetic disorders, tobacco, alcohol or substance abuse,
unhealthy weight, sexually transmitted disease and heart diseases(Healthypeople.gov, 2019). The
risk and mortality associated with pregnancy can be reduced by making quality preconception
more accessible before pregnancy and during the course of pregnancy. In addition to that health
outcomes, early diagnosis and treatment of disability and delays and other related health
conditions can promote health and prevent death and disability among the neonates.
Neonate’s health are impacted by sociodemographic and behavioural factors like
education, family income and breast feeding are strongly linked to physical health of the
mother(Healthypeople.gov, 2019).
Understanding maternal and early neonatal health
Identifying health risks in women and prevent the occurrence of future problem that can
impact both the mother and the child. There are strong evidences on the relationship between the
mother and the child. The major causes and health risks of mother and the child are interlinked
and the fundamental time points of mother and neonatal health overlaps making childbirth the
most sensitive time period for both mother and the new born child.
Maternal chronic illnesses like diabetes, kidney diseases, hypertension and infections
such as STDs, malaria can impact neonatal health. Diseases caused due to nutrient deficiency
also impacts health of the neonatal significantly. The treatment or interventions that women
increasing rapidly. Therefore, for mothers it is important to keep themselves healthy by
maintaining a healthy lifestyle that will attending regular neonatal care services in order to get
improved heath outcome for both the mother and child. Pregnancy provides opportunity for
identifying health risks and preventing health problems for women and neonates. The health
risks includes diabetes, depression, genetic disorders, tobacco, alcohol or substance abuse,
unhealthy weight, sexually transmitted disease and heart diseases(Healthypeople.gov, 2019). The
risk and mortality associated with pregnancy can be reduced by making quality preconception
more accessible before pregnancy and during the course of pregnancy. In addition to that health
outcomes, early diagnosis and treatment of disability and delays and other related health
conditions can promote health and prevent death and disability among the neonates.
Neonate’s health are impacted by sociodemographic and behavioural factors like
education, family income and breast feeding are strongly linked to physical health of the
mother(Healthypeople.gov, 2019).
Understanding maternal and early neonatal health
Identifying health risks in women and prevent the occurrence of future problem that can
impact both the mother and the child. There are strong evidences on the relationship between the
mother and the child. The major causes and health risks of mother and the child are interlinked
and the fundamental time points of mother and neonatal health overlaps making childbirth the
most sensitive time period for both mother and the new born child.
Maternal chronic illnesses like diabetes, kidney diseases, hypertension and infections
such as STDs, malaria can impact neonatal health. Diseases caused due to nutrient deficiency
also impacts health of the neonatal significantly. The treatment or interventions that women
WOMEN'S AND CHILD WELFARE
receive during pregnancy and childbirth have an impact on the neonatal health. For instance,
antenatal care and skilled birth attendance (SBA) addresses the major causes of both maternal
morbidity with excessive bleeding, infections and hypertensive diseases as well as neonatal
morbidity through infections, intrapartum related deaths and other complications related to with
preterm birth.
Why and how maternal and early neonatal health are strongly interrelated?
Evidences have shown that maternal health and early neonatal health are strongly inter-
related. Studies have identified maternal health risks that impacts neonatal health. The risks vary
by maternal age, maternal health status and past medical and social history, delivery process,
birth weight and gestational age. It has been found that male fetuses are at an increasing risk
when compared to female fetuses(Yego et al., 2013).
The health issues that contribute to the factors affecting woman’s health relates to
reproductive health and ante and post-partum healthcare and sexually transmitted disease
(STDs). Evidences have shown the prevalence of different diseases and other health factors of
the mother that affects the child during the early neonatal period. Maternal health issues,
particularly severe health conditions and chronic diseases like diabetes, kidney diseases,
hypertension, heart diseases and other related comorbidities significantly impacts early neonatal
health. It has also been found that lifestyle choices and dietary or nutritional choice of the mother
affects neonatal heath. Poor nutritional choice prior to pregnancy, during pregnancy and post
pregnancy have significant effect on the foetal development and therefore affects the neonatal
health. Maternal nutrition is found to be one of the most common and prevalent cause of child’s
mortality and therefore during pregnancy and post pregnancy woman are recommended to
consume foods with high nutritive value that improves both maternal and neonatal health.
receive during pregnancy and childbirth have an impact on the neonatal health. For instance,
antenatal care and skilled birth attendance (SBA) addresses the major causes of both maternal
morbidity with excessive bleeding, infections and hypertensive diseases as well as neonatal
morbidity through infections, intrapartum related deaths and other complications related to with
preterm birth.
Why and how maternal and early neonatal health are strongly interrelated?
Evidences have shown that maternal health and early neonatal health are strongly inter-
related. Studies have identified maternal health risks that impacts neonatal health. The risks vary
by maternal age, maternal health status and past medical and social history, delivery process,
birth weight and gestational age. It has been found that male fetuses are at an increasing risk
when compared to female fetuses(Yego et al., 2013).
The health issues that contribute to the factors affecting woman’s health relates to
reproductive health and ante and post-partum healthcare and sexually transmitted disease
(STDs). Evidences have shown the prevalence of different diseases and other health factors of
the mother that affects the child during the early neonatal period. Maternal health issues,
particularly severe health conditions and chronic diseases like diabetes, kidney diseases,
hypertension, heart diseases and other related comorbidities significantly impacts early neonatal
health. It has also been found that lifestyle choices and dietary or nutritional choice of the mother
affects neonatal heath. Poor nutritional choice prior to pregnancy, during pregnancy and post
pregnancy have significant effect on the foetal development and therefore affects the neonatal
health. Maternal nutrition is found to be one of the most common and prevalent cause of child’s
mortality and therefore during pregnancy and post pregnancy woman are recommended to
consume foods with high nutritive value that improves both maternal and neonatal health.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
WOMEN'S AND CHILD WELFARE
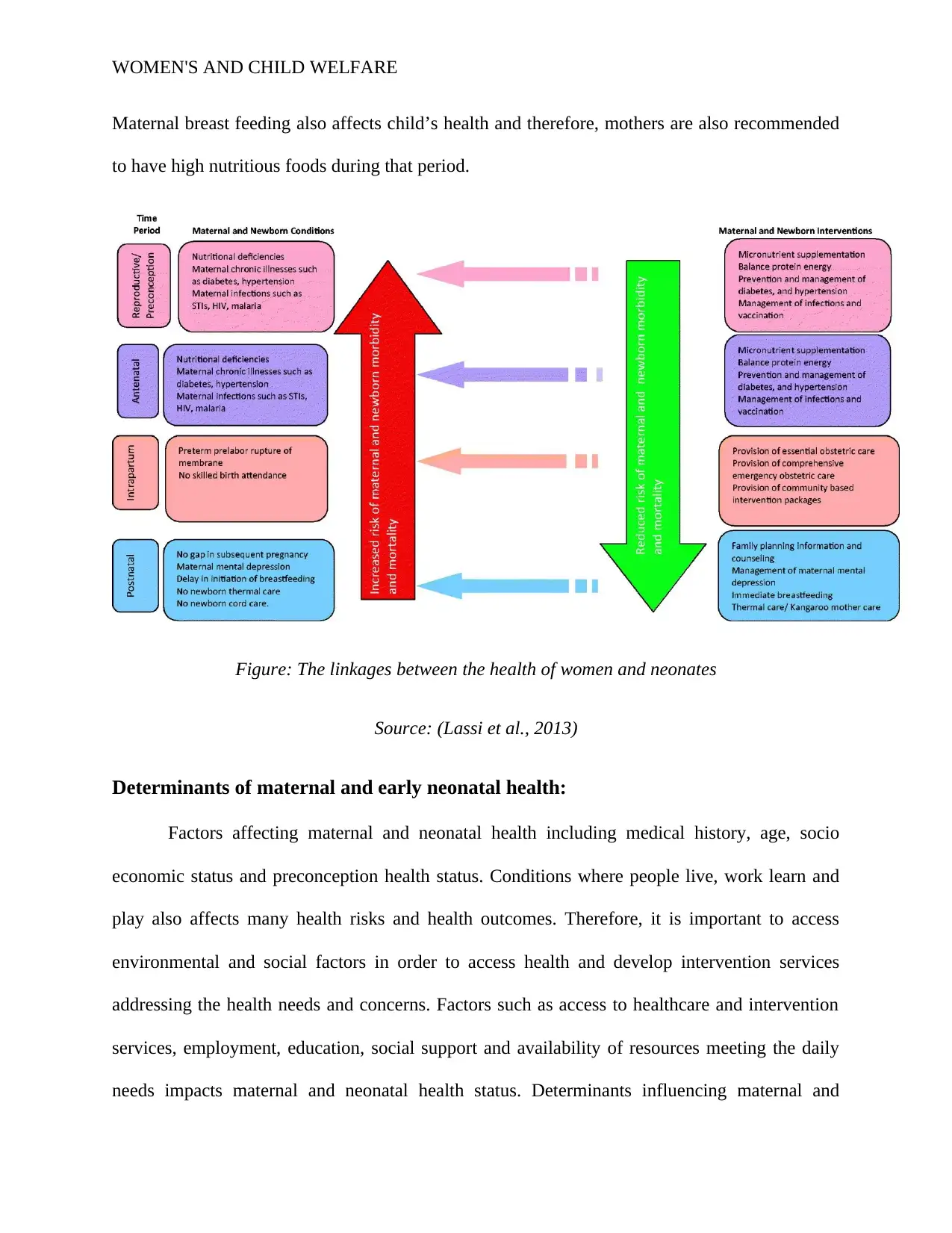
Maternal breast feeding also affects child’s health and therefore, mothers are also recommended
to have high nutritious foods during that period.
Figure: The linkages between the health of women and neonates
Source: (Lassi et al., 2013)
Determinants of maternal and early neonatal health:
Factors affecting maternal and neonatal health including medical history, age, socio
economic status and preconception health status. Conditions where people live, work learn and
play also affects many health risks and health outcomes. Therefore, it is important to access
environmental and social factors in order to access health and develop intervention services
addressing the health needs and concerns. Factors such as access to healthcare and intervention
services, employment, education, social support and availability of resources meeting the daily
needs impacts maternal and neonatal health status. Determinants influencing maternal and
Maternal breast feeding also affects child’s health and therefore, mothers are also recommended
to have high nutritious foods during that period.
Figure: The linkages between the health of women and neonates
Source: (Lassi et al., 2013)
Determinants of maternal and early neonatal health:
Factors affecting maternal and neonatal health including medical history, age, socio
economic status and preconception health status. Conditions where people live, work learn and
play also affects many health risks and health outcomes. Therefore, it is important to access
environmental and social factors in order to access health and develop intervention services
addressing the health needs and concerns. Factors such as access to healthcare and intervention
services, employment, education, social support and availability of resources meeting the daily
needs impacts maternal and neonatal health status. Determinants influencing maternal and
WOMEN'S AND CHILD WELFARE
neonatal health also include pregnancy outcomes and lifestyle choice before and during
pregnancy.
Issues identified in this area:
In the developing countries, it has been found that more than 9 million infants die each
year at stillbirth and during the early neonatal period due to the complications arising during
pregnancy. It has been reported that often these morbidities can be prevented by accessing the
health needs of the mother, identifying the risk factors contributing to the same and developing
intervention strategies beneficial for both maternal and early neonatal health. A majority of the
early neonatal death has been identified owing to pregnancy risks (Yego et al., 2013). Therefore,
the continuum of care given throughout the course of pregnancy and post pregnancy contributes
to the reduction in maternal and neonatal mortality deaths. There is an increasing number of
evidences showing that maximum maternal and neonatal deaths can be prevented by giving
adequate care and a continuous care during pregnancy, delivery of the child and in the
postpartum period (Yego et al., 2013). During the antenatal period, health care providers
addresses and accesses the risks and treat the health conditions that affects both maternal and
neonatal health.
Maternal health complications have been found to be contributing to 1.5 million neonatal
deaths in their first week of life and a 1.4 million miscarriages (Lassi et al., 2013). Maternal
health is strongly associated with neonatal health and has been found to significantly impact
neonatal health. A study by Mohsin, Bauman and Jalaludin (2006), has identified the influences
of maternal factors on stillbirths and neonatal deaths in New South Wales in Australia. The
research findings show that stillbirth and neonatal deaths varies with neonatal sex,
socioeconomic status, maternal smoking, antenatal care, plurality of birth, low weight, delivery
neonatal health also include pregnancy outcomes and lifestyle choice before and during
pregnancy.
Issues identified in this area:
In the developing countries, it has been found that more than 9 million infants die each
year at stillbirth and during the early neonatal period due to the complications arising during
pregnancy. It has been reported that often these morbidities can be prevented by accessing the
health needs of the mother, identifying the risk factors contributing to the same and developing
intervention strategies beneficial for both maternal and early neonatal health. A majority of the
early neonatal death has been identified owing to pregnancy risks (Yego et al., 2013). Therefore,
the continuum of care given throughout the course of pregnancy and post pregnancy contributes
to the reduction in maternal and neonatal mortality deaths. There is an increasing number of
evidences showing that maximum maternal and neonatal deaths can be prevented by giving
adequate care and a continuous care during pregnancy, delivery of the child and in the
postpartum period (Yego et al., 2013). During the antenatal period, health care providers
addresses and accesses the risks and treat the health conditions that affects both maternal and
neonatal health.
Maternal health complications have been found to be contributing to 1.5 million neonatal
deaths in their first week of life and a 1.4 million miscarriages (Lassi et al., 2013). Maternal
health is strongly associated with neonatal health and has been found to significantly impact
neonatal health. A study by Mohsin, Bauman and Jalaludin (2006), has identified the influences
of maternal factors on stillbirths and neonatal deaths in New South Wales in Australia. The
research findings show that stillbirth and neonatal deaths varies with neonatal sex,
socioeconomic status, maternal smoking, antenatal care, plurality of birth, low weight, delivery
WOMEN'S AND CHILD WELFARE
type and other complications arising pregnancy and delivery of the child (Sisay et al., 2014).
Evidences have shown that the most common causes of stillbirths originates during the prenatal
period due to hypoxia, intrauterine and asphyxia (Mohsin, Bauman &Jalaludin, 2006).
Intervention strategies to improve maternal and neonatal health:
Evidences have shown that during 1990-2015, the global mortality rate has been dropped
by 53% from 90.6 deaths per 1,000 live births in the year 1990to 42.5 in 2015. There is also a
rapid decline in the maternal mortality globally (Liu et al., 2015). Although a huge progress has
been found in this area, morality remains to be higher in countries with a lower and middle
income. The data found suggested by WHO, 2015, shows that approximately, 303,000 women
have died due to pregnancy and childbirth complications (Who.int, 2019).
Improving maternal and neonatal health by accessing health risks and complications:The
maternal and neonatal health and wellbeing are strongly interrelated. If mothers are
malnourished, sick, have chronic diseases and other health complications and received
inadequate care, their neonatal are at an increasing risk of developing illnesses and premature
death. The maternal health greatly influences the probability and risks of diseases in the new
born. It has been found in a study that maternal death during birth of the child significantly
increases the risk of mortality of the newborn (Ronsmans et al., 2010). Studies have suggested
that woman and children must have proper access to health services from conception, to
pregnancy, delivery, postnatal period in the neonatal period. Issues like sexually transmitted
infections, HIV/AIDS, malaria, malnutrition and severe complications during pregnancy and
child delivery and an insufficient or inadequate care must be accessed and addressed in order to
improve both maternal and neonatal heath (Yego et al.., 2014). A coordinating care with a
type and other complications arising pregnancy and delivery of the child (Sisay et al., 2014).
Evidences have shown that the most common causes of stillbirths originates during the prenatal
period due to hypoxia, intrauterine and asphyxia (Mohsin, Bauman &Jalaludin, 2006).
Intervention strategies to improve maternal and neonatal health:
Evidences have shown that during 1990-2015, the global mortality rate has been dropped
by 53% from 90.6 deaths per 1,000 live births in the year 1990to 42.5 in 2015. There is also a
rapid decline in the maternal mortality globally (Liu et al., 2015). Although a huge progress has
been found in this area, morality remains to be higher in countries with a lower and middle
income. The data found suggested by WHO, 2015, shows that approximately, 303,000 women
have died due to pregnancy and childbirth complications (Who.int, 2019).
Improving maternal and neonatal health by accessing health risks and complications:The
maternal and neonatal health and wellbeing are strongly interrelated. If mothers are
malnourished, sick, have chronic diseases and other health complications and received
inadequate care, their neonatal are at an increasing risk of developing illnesses and premature
death. The maternal health greatly influences the probability and risks of diseases in the new
born. It has been found in a study that maternal death during birth of the child significantly
increases the risk of mortality of the newborn (Ronsmans et al., 2010). Studies have suggested
that woman and children must have proper access to health services from conception, to
pregnancy, delivery, postnatal period in the neonatal period. Issues like sexually transmitted
infections, HIV/AIDS, malaria, malnutrition and severe complications during pregnancy and
child delivery and an insufficient or inadequate care must be accessed and addressed in order to
improve both maternal and neonatal heath (Yego et al.., 2014). A coordinating care with a
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
WOMEN'S AND CHILD WELFARE
multidisciplinary approach from preconception to child delivery has found to be effective for
improving maternal and neonatal heath (Black et al., 2016).
The risk factors for prenatal and neonatal fatalities, which lead to elevated neonatal
mortality worldwide, must be identified and obtained. Neonatal mortality is a strong maternal
health predictor (Euro.who.int, 2019). Health service factors have found to be associated with
early neonatal deaths, especially in the countries with low resource settings where quality of care
services is generally poor and insufficient. Conditions that act as risk factors for neonatal
mortality include maternal complications such as premature rupture of membranes (PROM),
dystocia, and haemorrhage. Mothers with PROM have shown to deliver preterm babies more
than those mothers without this condition, contributing to developing health risks for both
maternal and neonates (Yego et al., 2013).
Community based interventions for improving maternal and neonatal health: Interventions
focused on community-based programs, including counselling or home visits may help reduce
mortality of mothers and neonates (Lassi et al., 2016). For women during their pregnancy and
postnatal period by the community health workers in the pre and post natal period for
counselling others, provide care to the newborn and facilitate referral may contribute to early
diagnosis and complications and health risks.
Community health workers (CHW) play a fundamental role in promoting maternal and
neonatal health outcome. Since 2000, it has been found that CHW have a great potential for
achieving health outcomes. Community based interventions encourages healthy practices and
care involving community members and families. The CHW is active in the provision of health
education, development and the distribution of services, the diagnosis and prevention of diseases
multidisciplinary approach from preconception to child delivery has found to be effective for
improving maternal and neonatal heath (Black et al., 2016).
The risk factors for prenatal and neonatal fatalities, which lead to elevated neonatal
mortality worldwide, must be identified and obtained. Neonatal mortality is a strong maternal
health predictor (Euro.who.int, 2019). Health service factors have found to be associated with
early neonatal deaths, especially in the countries with low resource settings where quality of care
services is generally poor and insufficient. Conditions that act as risk factors for neonatal
mortality include maternal complications such as premature rupture of membranes (PROM),
dystocia, and haemorrhage. Mothers with PROM have shown to deliver preterm babies more
than those mothers without this condition, contributing to developing health risks for both
maternal and neonates (Yego et al., 2013).
Community based interventions for improving maternal and neonatal health: Interventions
focused on community-based programs, including counselling or home visits may help reduce
mortality of mothers and neonates (Lassi et al., 2016). For women during their pregnancy and
postnatal period by the community health workers in the pre and post natal period for
counselling others, provide care to the newborn and facilitate referral may contribute to early
diagnosis and complications and health risks.
Community health workers (CHW) play a fundamental role in promoting maternal and
neonatal health outcome. Since 2000, it has been found that CHW have a great potential for
achieving health outcomes. Community based interventions encourages healthy practices and
care involving community members and families. The CHW is active in the provision of health
education, development and the distribution of services, the diagnosis and prevention of diseases
WOMEN'S AND CHILD WELFARE
and damage in primary health care. The CHW also provides guidance. Evidences have shown
that community based interventions are important for improving delivery of health care services
and outcomes (Lunze et al., 2015). Evidences have also suggested that CHWs perform neonatal
resuscitation effectively.
Increasing awareness: Lack of awareness and knowledge on the urgency of seeking medical
treatment can significantly affect maternal and neonatal health. Awareness, education,
employment and affordability are believed to negatively impact maternal and neonatal health.
Choice of seeking healthcare service is also impacted by social and cultural practices especially
for women who are from socially isolated or remote areas (Yadeta, 2018). Therefore, it can be
concluded that neonatal health is significantly impacted by the health and lifestyle choices.
Conclusion
Neonatal safety and morbidity have been shown to be closely related to mothers and
insufficient maternal care during and after the childbirth can affect neonate wellbeing as well.
Evidence has shown that exposure to obstetric emergencies and prenatal care can reduce
neonatal mortality by 10% to 15%. There are also evidences that 10% of the preterm and
intrapartum-related deaths can be decreased by conducting immediate assessments and
promoting the health of neonates. There are many approaches to enhance both maternal and
neonatal safety that have been shown to be successful. Antenatal corticosteroids were also used
to treat the neonatal deaths in general, especially for women who are diagnosed with premature
membrane rupture (PROM). Interventions to inform mothers in prenatal care, testing, evaluation,
tracking and management of maternal disorders via various approaches to mother- and neonate
health concerns should be improved during the prenatal era. Doctor’s active involvement and
and damage in primary health care. The CHW also provides guidance. Evidences have shown
that community based interventions are important for improving delivery of health care services
and outcomes (Lunze et al., 2015). Evidences have also suggested that CHWs perform neonatal
resuscitation effectively.
Increasing awareness: Lack of awareness and knowledge on the urgency of seeking medical
treatment can significantly affect maternal and neonatal health. Awareness, education,
employment and affordability are believed to negatively impact maternal and neonatal health.
Choice of seeking healthcare service is also impacted by social and cultural practices especially
for women who are from socially isolated or remote areas (Yadeta, 2018). Therefore, it can be
concluded that neonatal health is significantly impacted by the health and lifestyle choices.
Conclusion
Neonatal safety and morbidity have been shown to be closely related to mothers and
insufficient maternal care during and after the childbirth can affect neonate wellbeing as well.
Evidence has shown that exposure to obstetric emergencies and prenatal care can reduce
neonatal mortality by 10% to 15%. There are also evidences that 10% of the preterm and
intrapartum-related deaths can be decreased by conducting immediate assessments and
promoting the health of neonates. There are many approaches to enhance both maternal and
neonatal safety that have been shown to be successful. Antenatal corticosteroids were also used
to treat the neonatal deaths in general, especially for women who are diagnosed with premature
membrane rupture (PROM). Interventions to inform mothers in prenatal care, testing, evaluation,
tracking and management of maternal disorders via various approaches to mother- and neonate
health concerns should be improved during the prenatal era. Doctor’s active involvement and
WOMEN'S AND CHILD WELFARE
attention during child delivery and for emergency situations on priority basis are crucial and
important for ensuring survival and improvement of early neonatalheath and prevent potential
risk factors contributing to maternal and neonatal mortality.
attention during child delivery and for emergency situations on priority basis are crucial and
important for ensuring survival and improvement of early neonatalheath and prevent potential
risk factors contributing to maternal and neonatal mortality.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
WOMEN'S AND CHILD WELFARE
References:
Black, R., Laxminarayan, R., Temmerman, M., & Walker, N. (Eds.). (2016). Disease control
priorities, (volume 2): reproductive, maternal, newborn, and child health. The World
Bank.
Euro.who.int. (2019). Maternal and newborn health. Retrieved 1 October 2019, from
http://www.euro.who.int/en/health-topics/Life-stages/maternal-and-newborn-health/
maternal-and-newborn-health
Healthypeople.gov. (2019). Maternal, Infant, and Child Health | Healthy People 2020. Retrieved
29 September 2019, from
https://www.healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-child-
health
Lassi, Z. S., Majeed, A., Rashid, S., Yakoob, M. Y., &Bhutta, Z. A. (2013). The interconnections
between maternal and newborn health–evidence and implications for policy. The Journal
of Maternal-Fetal& Neonatal Medicine, 26(sup1), 3-53.
Lassi, Z. S., Middleton, P. F., Bhutta, Z. A., & Crowther, C. (2016). Strategies for improving
health care seeking for maternal and newborn illnesses in low-and middle-income
countries: a systematic review and meta-analysis. Global health action, 9(1), 31408.
Liu, L., Hill, K., Oza, S., Hogan, D., Chu, Y., Cousens, S., ...& Black, R. E. (2015). Levels and
causes of mortality under age five years. International Bank for Reconstruction and
Development, World Bank. Reproductive, maternal, newborn, and child health: disease
control priorities, 2, 71-83.
References:
Black, R., Laxminarayan, R., Temmerman, M., & Walker, N. (Eds.). (2016). Disease control
priorities, (volume 2): reproductive, maternal, newborn, and child health. The World
Bank.
Euro.who.int. (2019). Maternal and newborn health. Retrieved 1 October 2019, from
http://www.euro.who.int/en/health-topics/Life-stages/maternal-and-newborn-health/
maternal-and-newborn-health
Healthypeople.gov. (2019). Maternal, Infant, and Child Health | Healthy People 2020. Retrieved
29 September 2019, from
https://www.healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-child-
health
Lassi, Z. S., Majeed, A., Rashid, S., Yakoob, M. Y., &Bhutta, Z. A. (2013). The interconnections
between maternal and newborn health–evidence and implications for policy. The Journal
of Maternal-Fetal& Neonatal Medicine, 26(sup1), 3-53.
Lassi, Z. S., Middleton, P. F., Bhutta, Z. A., & Crowther, C. (2016). Strategies for improving
health care seeking for maternal and newborn illnesses in low-and middle-income
countries: a systematic review and meta-analysis. Global health action, 9(1), 31408.
Liu, L., Hill, K., Oza, S., Hogan, D., Chu, Y., Cousens, S., ...& Black, R. E. (2015). Levels and
causes of mortality under age five years. International Bank for Reconstruction and
Development, World Bank. Reproductive, maternal, newborn, and child health: disease
control priorities, 2, 71-83.
WOMEN'S AND CHILD WELFARE
Lunze, K., Higgins-Steele, A., Simen-Kapeu, A., Vesel, L., Kim, J., & Dickson, K. (2015).
Innovative approaches for improving maternal and newborn health-A landscape
analysis. BMC pregnancy and childbirth, 15(1), 337.
Mohsin, M., Bauman, A. E., &Jalaludin, B. (2006). The influence of antenatal and maternal
factors on stillbirths and neonatal deaths in New South Wales, Australia. Journal of
biosocial science, 38(5), 643-657.
Ronsmans, C., Chowdhury, M. E., Dasgupta, S. K., Ahmed, A., &Koblinsky, M. (2010). Effect
of parent's death on child survival in rural Bangladesh: a cohort study. The
Lancet, 375(9730), 2024-2031.
Sisay, M. M., Yirgu, R., Gobezayehu, A. G., & Sibley, L. M. (2014). A qualitative study of
attitudes and values surrounding stillbirth and neonatal mortality among grandmothers,
mothers, and unmarried girls in rural Amhara and Oromiya regions, Ethiopia: unheard
souls in the backyard. Journal of midwifery & women's health, 59(s1), S110-S117.
Who.int. (2019). Trends in maternal mortality: 1990 to 2015. Retrieved 1 October 2019, from
https://www.who.int/reproductivehealth/publications/monitoring/maternal-mortality-
2015/en/
Yadeta, T. A. (2018). Antenatal care utilization increase the odds of women knowledge on
neonatal danger sign: a community-based study, eastern Ethiopia. BMC research
notes, 11(1), 845.
Lunze, K., Higgins-Steele, A., Simen-Kapeu, A., Vesel, L., Kim, J., & Dickson, K. (2015).
Innovative approaches for improving maternal and newborn health-A landscape
analysis. BMC pregnancy and childbirth, 15(1), 337.
Mohsin, M., Bauman, A. E., &Jalaludin, B. (2006). The influence of antenatal and maternal
factors on stillbirths and neonatal deaths in New South Wales, Australia. Journal of
biosocial science, 38(5), 643-657.
Ronsmans, C., Chowdhury, M. E., Dasgupta, S. K., Ahmed, A., &Koblinsky, M. (2010). Effect
of parent's death on child survival in rural Bangladesh: a cohort study. The
Lancet, 375(9730), 2024-2031.
Sisay, M. M., Yirgu, R., Gobezayehu, A. G., & Sibley, L. M. (2014). A qualitative study of
attitudes and values surrounding stillbirth and neonatal mortality among grandmothers,
mothers, and unmarried girls in rural Amhara and Oromiya regions, Ethiopia: unheard
souls in the backyard. Journal of midwifery & women's health, 59(s1), S110-S117.
Who.int. (2019). Trends in maternal mortality: 1990 to 2015. Retrieved 1 October 2019, from
https://www.who.int/reproductivehealth/publications/monitoring/maternal-mortality-
2015/en/
Yadeta, T. A. (2018). Antenatal care utilization increase the odds of women knowledge on
neonatal danger sign: a community-based study, eastern Ethiopia. BMC research
notes, 11(1), 845.
WOMEN'S AND CHILD WELFARE
Yego, F., D’Este, C., Byles, J., Nyongesa, P., & Williams, J. S. (2014). A case-control study of
risk factors for fetal and early neonatal deaths in a tertiary hospital in Kenya. BMC
pregnancy and childbirth, 14(1), 389.
Yego, F., Williams, J. S., Byles, J., Nyongesa, P., Aruasa, W., &D'Este, C. (2013). A
retrospective analysis of maternal and neonatal mortality at a teaching and referral
hospital in Kenya. Reproductive health, 10(1), 13.
Yego, F., D’Este, C., Byles, J., Nyongesa, P., & Williams, J. S. (2014). A case-control study of
risk factors for fetal and early neonatal deaths in a tertiary hospital in Kenya. BMC
pregnancy and childbirth, 14(1), 389.
Yego, F., Williams, J. S., Byles, J., Nyongesa, P., Aruasa, W., &D'Este, C. (2013). A
retrospective analysis of maternal and neonatal mortality at a teaching and referral
hospital in Kenya. Reproductive health, 10(1), 13.
1 out of 13
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





