Wound Assessment: Burn, Skin Tear, and Ulcer
VerifiedAdded on 2023/01/19
|10
|2785
|93
AI Summary
This essay provides a comprehensive assessment of different types of wounds including burn, skin tear, and ulcer. It discusses the evaluation criteria, wound characteristics, pain assessment, and recommended treatment for each case study. The aim is to promote optimal wound healing and faster recovery.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: WOUND ASSESSMENT
WOUND ASSESSMENT
Name of the Student
Name of the University
Author’s Note:
WOUND ASSESSMENT
Name of the Student
Name of the University
Author’s Note:
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1WOUND ASSESSMENT
Introduction:
Most injuries heal without complexity from any aetiology. However, some wounds are
subject to cures, although they do not stop remedy if the injuries are handled properly.
Although, in minor cases, some wound will become non- healing and chronic. The ultimate
goal in these cases is to manage side effects and inhibit complications rather than heal the
wound (Mukherjee et al., 2014). Accurate evaluation of wounds and effective wound
management require knowledge of wound healing physiology in combination with an
awareness of the actions regarding dressing products. An ongoing evaluation, clinical
decision making, intervention and documentation process is crucial to promote optimal
wound healing (Vowden & Vowden, 2017). Various local and general factors such as
underlying disease, pressure, moisture imbalance, malnutrition, impaired perfusion may delay
or affect healing of wounds (Greatrex‐White & Moxey, 2015). An important part of the
wound management process is the integral evaluation of the patient and holistic approach.
Hence, this essay utilizes the MEASURE assessment criteria for wound assessment which are
Measure, Exudate, Appearance, Suffering, Undermining, Re-evaluate, and Edge. Therefore,
the aim of this essay is to provide a wound management for the supplied case studies.
Discussion:
In this wound assessment will be provided for three case studies of Patient A, Patient B, and
Patient C.
Wound Assessment of Patient A:
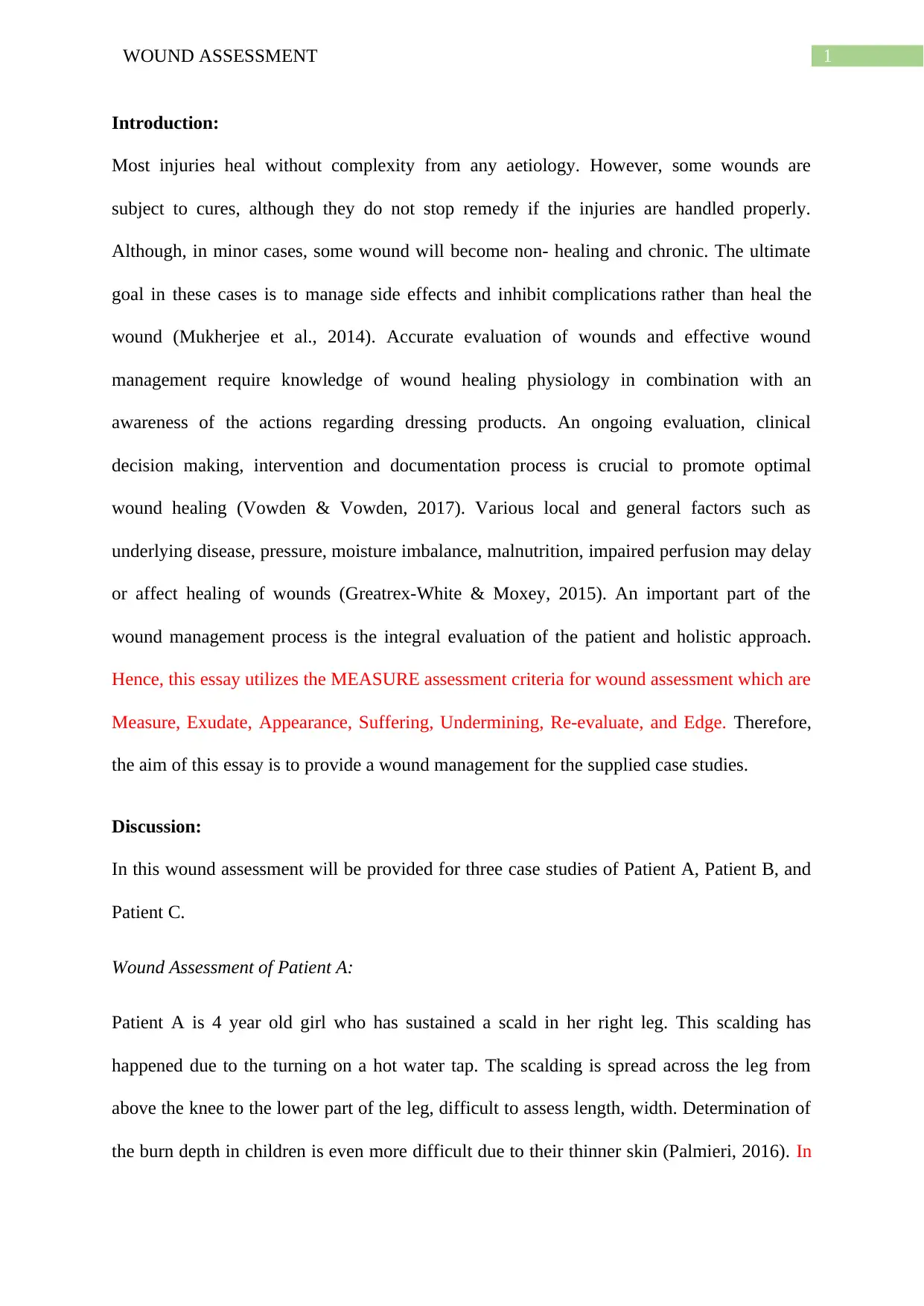
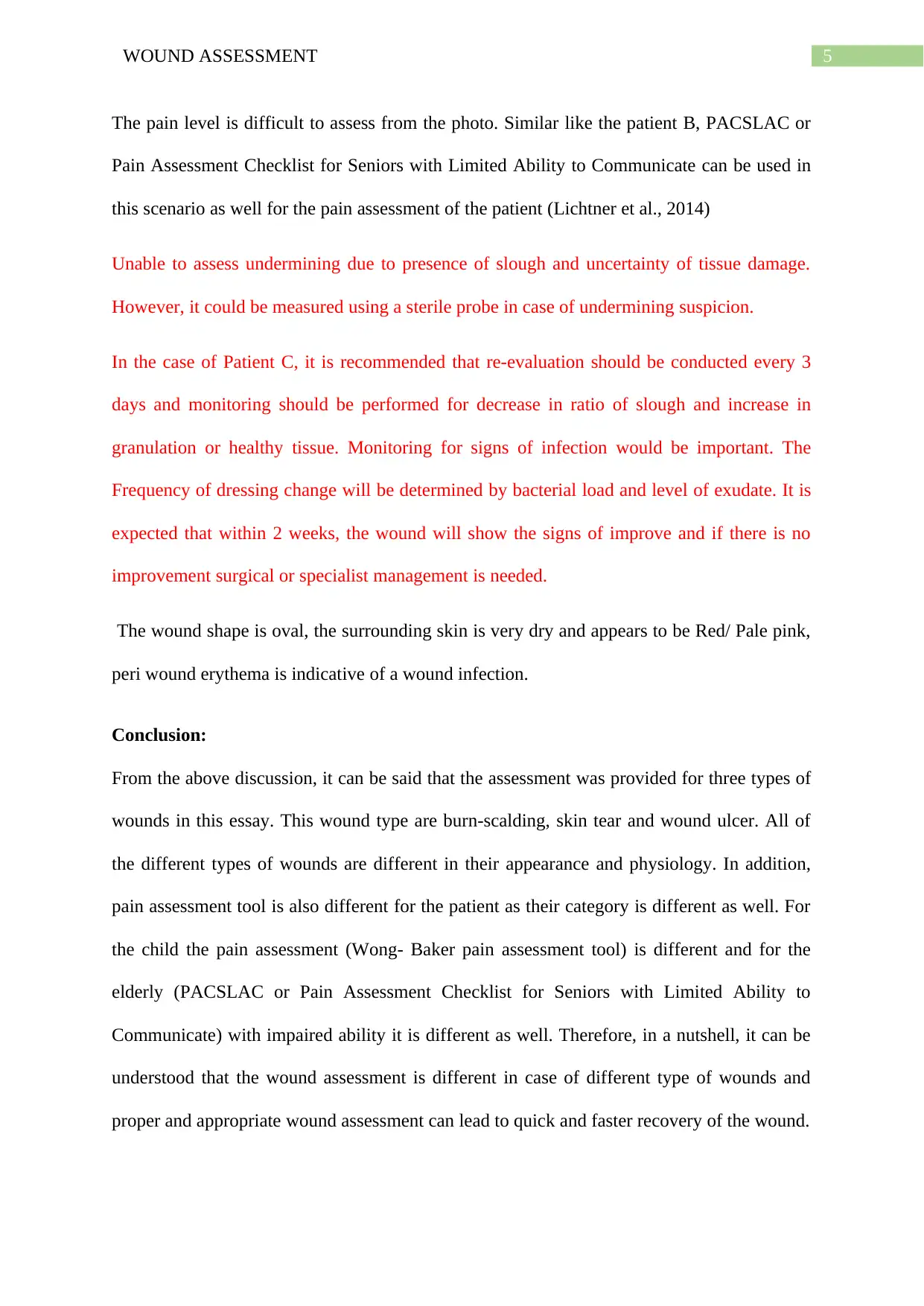
Patient A is 4 year old girl who has sustained a scald in her right leg. This scalding has
happened due to the turning on a hot water tap. The scalding is spread across the leg from
above the knee to the lower part of the leg, difficult to assess length, width. Determination of
the burn depth in children is even more difficult due to their thinner skin (Palmieri, 2016). In
Introduction:
Most injuries heal without complexity from any aetiology. However, some wounds are
subject to cures, although they do not stop remedy if the injuries are handled properly.
Although, in minor cases, some wound will become non- healing and chronic. The ultimate
goal in these cases is to manage side effects and inhibit complications rather than heal the
wound (Mukherjee et al., 2014). Accurate evaluation of wounds and effective wound
management require knowledge of wound healing physiology in combination with an
awareness of the actions regarding dressing products. An ongoing evaluation, clinical
decision making, intervention and documentation process is crucial to promote optimal
wound healing (Vowden & Vowden, 2017). Various local and general factors such as
underlying disease, pressure, moisture imbalance, malnutrition, impaired perfusion may delay
or affect healing of wounds (Greatrex‐White & Moxey, 2015). An important part of the
wound management process is the integral evaluation of the patient and holistic approach.
Hence, this essay utilizes the MEASURE assessment criteria for wound assessment which are
Measure, Exudate, Appearance, Suffering, Undermining, Re-evaluate, and Edge. Therefore,
the aim of this essay is to provide a wound management for the supplied case studies.
Discussion:
In this wound assessment will be provided for three case studies of Patient A, Patient B, and
Patient C.
Wound Assessment of Patient A:
Patient A is 4 year old girl who has sustained a scald in her right leg. This scalding has
happened due to the turning on a hot water tap. The scalding is spread across the leg from
above the knee to the lower part of the leg, difficult to assess length, width. Determination of
the burn depth in children is even more difficult due to their thinner skin (Palmieri, 2016). In
2WOUND ASSESSMENT
case of burn, it is paramount to assess depth, including capillary refill. Additionally, other key
aspects which are important in case of this type of burn assessment are the source and
mechanism of injury and the type of first aid provided to reduce the destruction of deep layers
of skin. Due to the spreading nature of this wound it is very difficult to calculate the length of
the wound. However, Total Body surface area can be calculated using the Lunder and
Browder burn chart and the affected area is around 7 percent (Vic Burns, 2019).
Given the significant surface area and the appearance of the wound bed, it can be expected
that large amount of exudate will ooze in the first 72 hour post injury (Aci.health.nsw.gov.au,
2019). It is also expected that the wound exudate will be clear. There is no sign of
contamination is noticed, hence, there will not be any malodour in the wound. At the current
state, there is no presence of exudates in the wound and the wound appears to be dry.
The wound bed comprises of 60 percent pinkish red, 30 percent pale pink, 10 percent pale red
granulation tissue. In some area of the wound, the epidermis isn’t present which might have
happened due to break of blisters. Presence of red tissue can be seen directly above the knee.
The colours and the presence of blister can aid in determination of depth of burn and without
the capillary refill, it can be deduced that the wound depth is limited to superficial dermal or
mid dermal. There is no visible signs of tendon, ligament, muscle, or bone exposure.
The pain level is indeterminable from the photo. The Wong- Baker pain assessment tool will
be used for the measurement of the pain in this scenario as Wong- Baker pain assessment tool
is particularly helpful for assessment of pain among children (Savino et al., 2013). Patient
A’s wound shows no signs of undermining.
The Agency for Clinical Innovation (2019) recommended review in every 3-7 days for the
assessment of wound healing and ongoing risk of infection. In the case of Patient A, it is
recommend that the initial dressing to be left in tact for 3-7 days and monitoring for the
case of burn, it is paramount to assess depth, including capillary refill. Additionally, other key
aspects which are important in case of this type of burn assessment are the source and
mechanism of injury and the type of first aid provided to reduce the destruction of deep layers
of skin. Due to the spreading nature of this wound it is very difficult to calculate the length of
the wound. However, Total Body surface area can be calculated using the Lunder and
Browder burn chart and the affected area is around 7 percent (Vic Burns, 2019).
Given the significant surface area and the appearance of the wound bed, it can be expected
that large amount of exudate will ooze in the first 72 hour post injury (Aci.health.nsw.gov.au,
2019). It is also expected that the wound exudate will be clear. There is no sign of
contamination is noticed, hence, there will not be any malodour in the wound. At the current
state, there is no presence of exudates in the wound and the wound appears to be dry.
The wound bed comprises of 60 percent pinkish red, 30 percent pale pink, 10 percent pale red
granulation tissue. In some area of the wound, the epidermis isn’t present which might have
happened due to break of blisters. Presence of red tissue can be seen directly above the knee.
The colours and the presence of blister can aid in determination of depth of burn and without
the capillary refill, it can be deduced that the wound depth is limited to superficial dermal or
mid dermal. There is no visible signs of tendon, ligament, muscle, or bone exposure.
The pain level is indeterminable from the photo. The Wong- Baker pain assessment tool will
be used for the measurement of the pain in this scenario as Wong- Baker pain assessment tool
is particularly helpful for assessment of pain among children (Savino et al., 2013). Patient
A’s wound shows no signs of undermining.
The Agency for Clinical Innovation (2019) recommended review in every 3-7 days for the
assessment of wound healing and ongoing risk of infection. In the case of Patient A, it is
recommend that the initial dressing to be left in tact for 3-7 days and monitoring for the
3WOUND ASSESSMENT
wound progression and infection. The frequency of dressing changes will be determined by
the presence of exudate.
In this scenario, the wound shaped is irregular, but consistent with scalding from hot water.
From the image of the wound, it can be deduced that the part of epidermis have been burnt
and large area of the burn reflect epidermal burn (erythema).
Wound Assessment of Patient B:
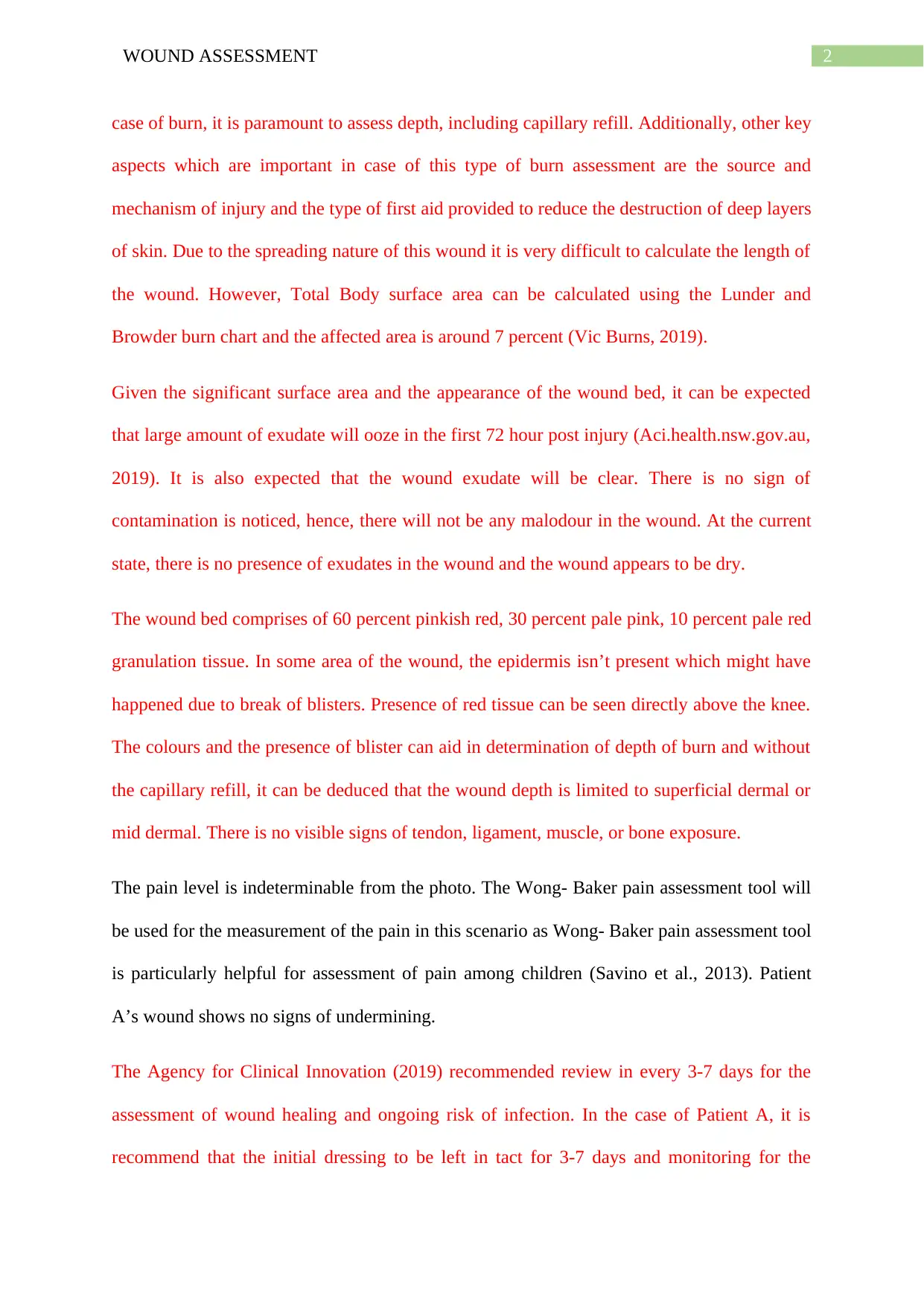
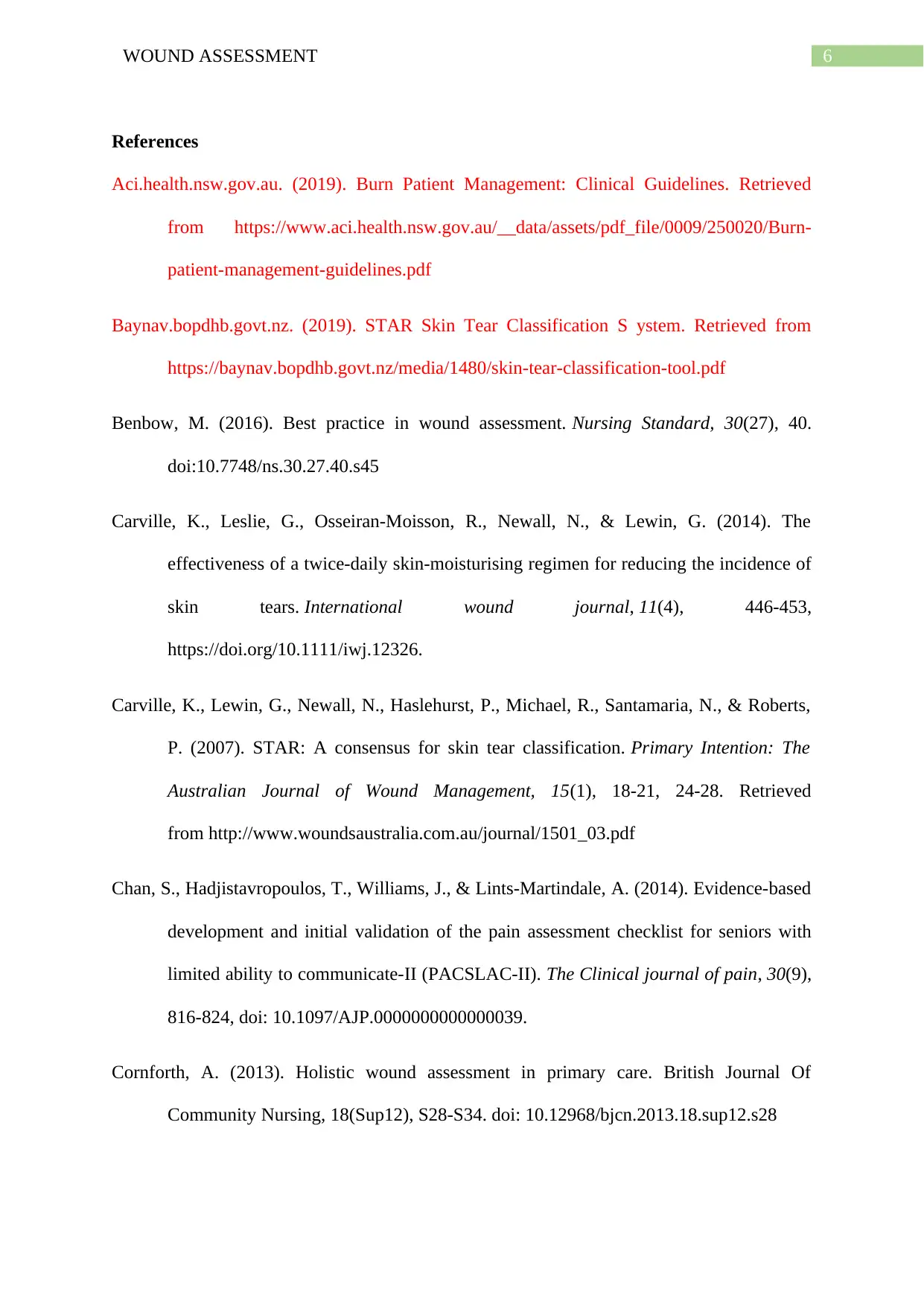
This is case study is regarding to the Patient B who is a 94-year-old woman. She has
sustained a skin tear recently.
The wound shape is in a triangular shape and the length is of the wound is 2 cm, width 3.5cm.
The depth of the wound is very minimal and only underlying skin tissues can be seen in this
wound. This is a category type 3 skin tear as the skin flap is completely absent (Carville et
al., 2014).
From this type of wound, it can be expected that the wound exudate will be present in large
quantity of serous exudate for the first 24 to 48 hours. As there is no signs of infection,
malodour is absent.
In addition, the skin colour is not pale but rather darkened or dusky (Carville et al., 2014).
Additionally, bruising can be seen around the skin tear. The wound bed is moist with red
coloration with slight white tinge. Most of the wound bed is covered with epithelial tissue and
it has covered almost 95 percent of the wound. The white tinge may signify the presence of
pus in the wound. This might also happen due to the skin granulation (Harries, Bosanquet &
Harding, 2016). PACSLAC or Pain Assessment Checklist for Seniors with Limited Ability to
Communicate can be used for the pain assessment in this scenario as the patient is elderly
(Chan et al., 2014). Undermining is absent in this wound.
wound progression and infection. The frequency of dressing changes will be determined by
the presence of exudate.
In this scenario, the wound shaped is irregular, but consistent with scalding from hot water.
From the image of the wound, it can be deduced that the part of epidermis have been burnt
and large area of the burn reflect epidermal burn (erythema).
Wound Assessment of Patient B:
This is case study is regarding to the Patient B who is a 94-year-old woman. She has
sustained a skin tear recently.
The wound shape is in a triangular shape and the length is of the wound is 2 cm, width 3.5cm.
The depth of the wound is very minimal and only underlying skin tissues can be seen in this
wound. This is a category type 3 skin tear as the skin flap is completely absent (Carville et
al., 2014).
From this type of wound, it can be expected that the wound exudate will be present in large
quantity of serous exudate for the first 24 to 48 hours. As there is no signs of infection,
malodour is absent.
In addition, the skin colour is not pale but rather darkened or dusky (Carville et al., 2014).
Additionally, bruising can be seen around the skin tear. The wound bed is moist with red
coloration with slight white tinge. Most of the wound bed is covered with epithelial tissue and
it has covered almost 95 percent of the wound. The white tinge may signify the presence of
pus in the wound. This might also happen due to the skin granulation (Harries, Bosanquet &
Harding, 2016). PACSLAC or Pain Assessment Checklist for Seniors with Limited Ability to
Communicate can be used for the pain assessment in this scenario as the patient is elderly
(Chan et al., 2014). Undermining is absent in this wound.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4WOUND ASSESSMENT
In this scenario, it is recommend that the initial dressing should be left intact for 3 -7 days
and monitoring for wound progression and risk of infection. Special caution must be taken
while removing the dressing. The frequency of dressing changes will be determined by the
presence of exudate. It is expected for this type of wound to heal in 21 days, however,
consultation ius needed from appropriate specialist (Baynav.bopdhb.govt.nz, 2019).
The edges of the wound are intact and no breaking is present in the wound.
Wound Assessment of Patient C:
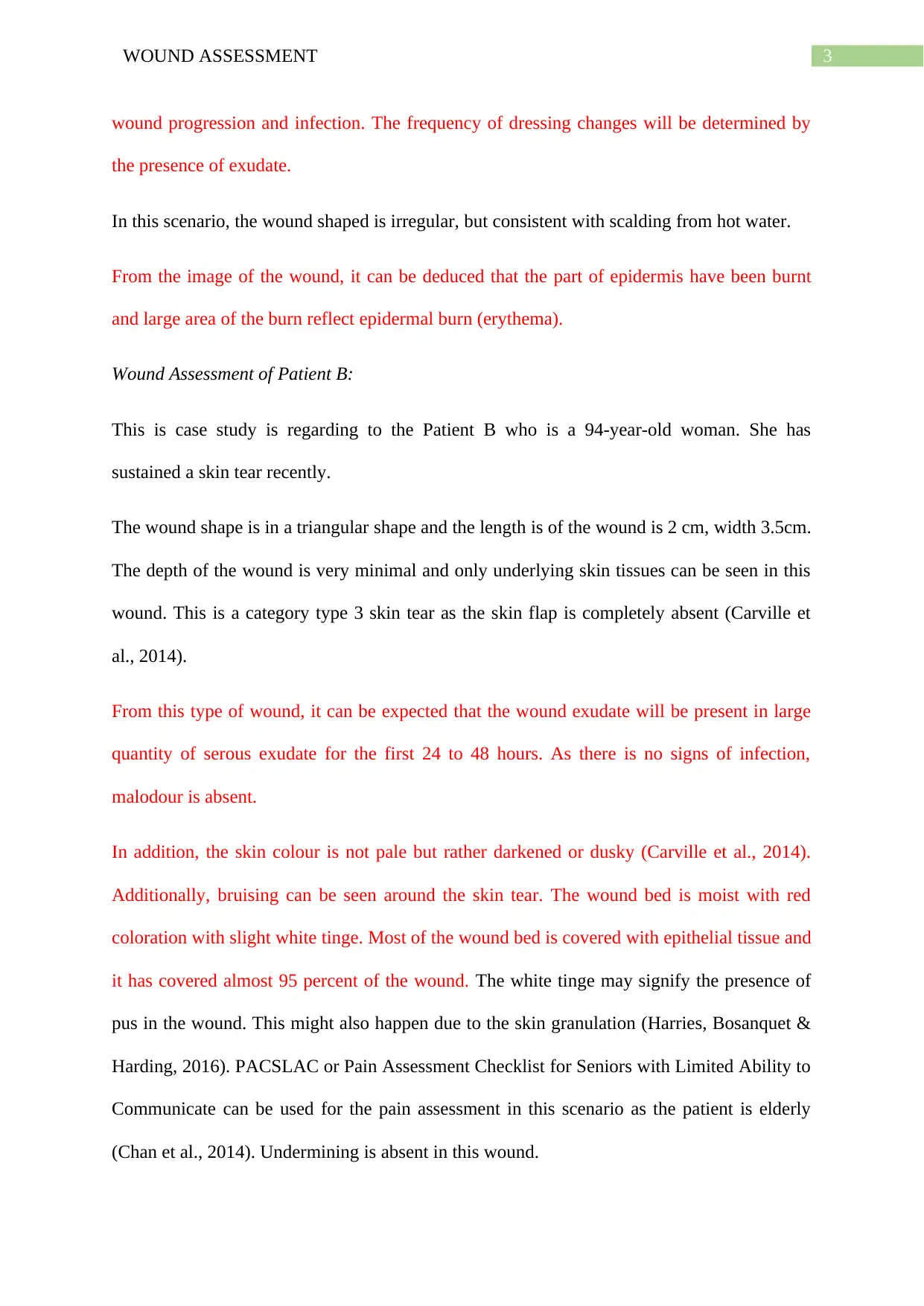
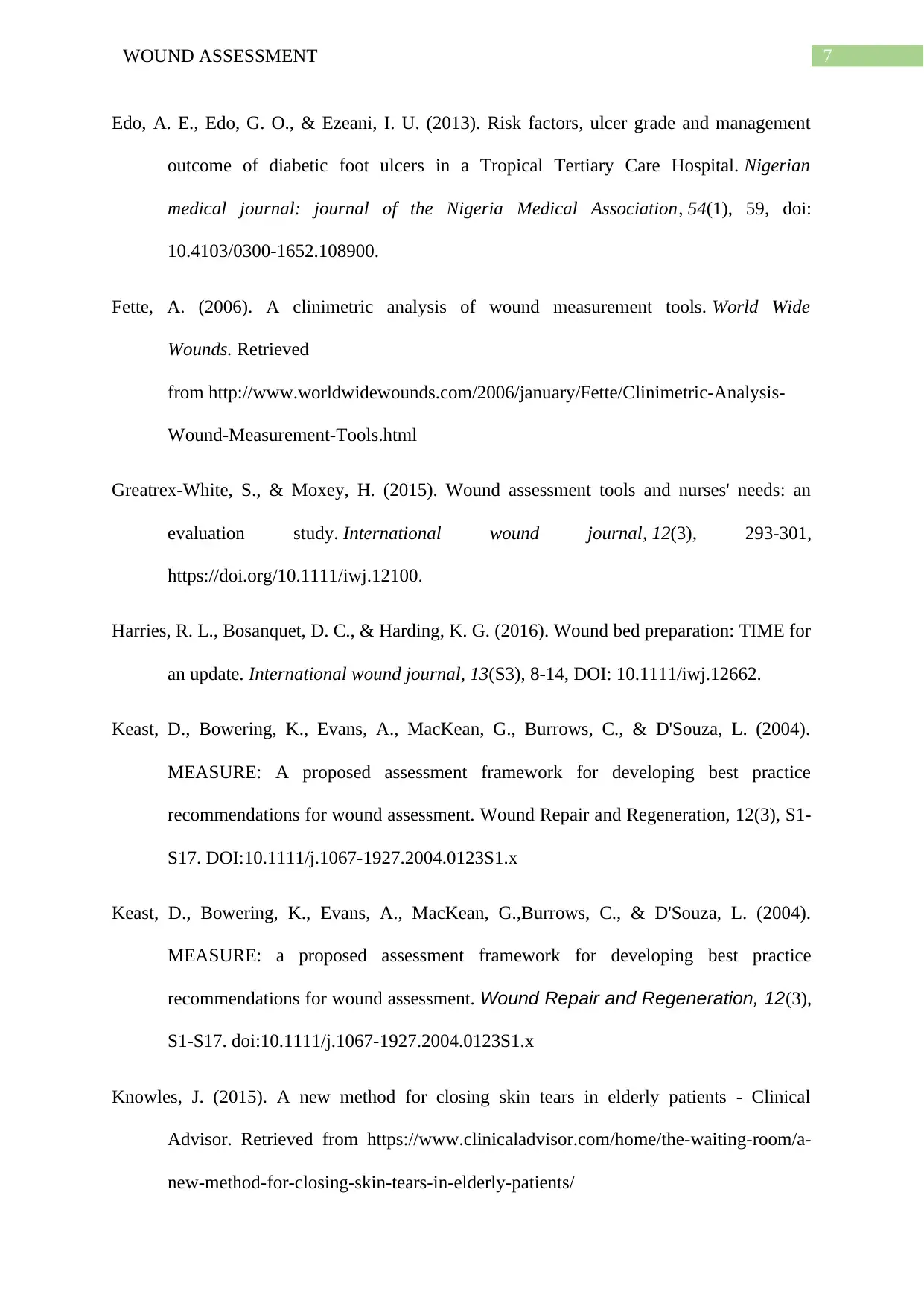
Patient C is an 80-year-old woman. She has developed an ulcer about 10 weeks ago which
has not healed and this is the reason for her visit to the hospital. The patient has impaired
cognitive ability as she is an Alzheimer’s patient.
The ulcer wound of this patient is around 2.5 in length and 1.5 cm long in width. From the
picture, it is difficult to assess depth as the base of the wound cannot be visualized due to
slough and eschar.
Based on the significant amount of hyperkeratosis present in the peri wound and the
appearance of yellow slough, it is expected that large amount of exudate will present. It is
also expected that the wound exudate to be purulent in consistent with a wound infection.
Additionally, it is expected that the wound to have a pungent odour.
The wound bed of this ulcer is moist, and islands of skin granulation can be seen in the
wound. Almost 15 percent of wound is covered with healthy granulation and the 85 percent
of the wound is yellow slough covered with biofilm and due to the presence of biofilm, it is
difficult to determine how much tissue loss present. There might be the presence of pus and
for that reason the wound should be checked for bacterial infection. The peri wound area
pinkish in colour.
In this scenario, it is recommend that the initial dressing should be left intact for 3 -7 days
and monitoring for wound progression and risk of infection. Special caution must be taken
while removing the dressing. The frequency of dressing changes will be determined by the
presence of exudate. It is expected for this type of wound to heal in 21 days, however,
consultation ius needed from appropriate specialist (Baynav.bopdhb.govt.nz, 2019).
The edges of the wound are intact and no breaking is present in the wound.
Wound Assessment of Patient C:
Patient C is an 80-year-old woman. She has developed an ulcer about 10 weeks ago which
has not healed and this is the reason for her visit to the hospital. The patient has impaired
cognitive ability as she is an Alzheimer’s patient.
The ulcer wound of this patient is around 2.5 in length and 1.5 cm long in width. From the
picture, it is difficult to assess depth as the base of the wound cannot be visualized due to
slough and eschar.
Based on the significant amount of hyperkeratosis present in the peri wound and the
appearance of yellow slough, it is expected that large amount of exudate will present. It is
also expected that the wound exudate to be purulent in consistent with a wound infection.
Additionally, it is expected that the wound to have a pungent odour.
The wound bed of this ulcer is moist, and islands of skin granulation can be seen in the
wound. Almost 15 percent of wound is covered with healthy granulation and the 85 percent
of the wound is yellow slough covered with biofilm and due to the presence of biofilm, it is
difficult to determine how much tissue loss present. There might be the presence of pus and
for that reason the wound should be checked for bacterial infection. The peri wound area
pinkish in colour.
5WOUND ASSESSMENT
The pain level is difficult to assess from the photo. Similar like the patient B, PACSLAC or
Pain Assessment Checklist for Seniors with Limited Ability to Communicate can be used in
this scenario as well for the pain assessment of the patient (Lichtner et al., 2014)
Unable to assess undermining due to presence of slough and uncertainty of tissue damage.
However, it could be measured using a sterile probe in case of undermining suspicion.
In the case of Patient C, it is recommended that re-evaluation should be conducted every 3
days and monitoring should be performed for decrease in ratio of slough and increase in
granulation or healthy tissue. Monitoring for signs of infection would be important. The
Frequency of dressing change will be determined by bacterial load and level of exudate. It is
expected that within 2 weeks, the wound will show the signs of improve and if there is no
improvement surgical or specialist management is needed.
The wound shape is oval, the surrounding skin is very dry and appears to be Red/ Pale pink,
peri wound erythema is indicative of a wound infection.
Conclusion:
From the above discussion, it can be said that the assessment was provided for three types of
wounds in this essay. This wound type are burn-scalding, skin tear and wound ulcer. All of
the different types of wounds are different in their appearance and physiology. In addition,
pain assessment tool is also different for the patient as their category is different as well. For
the child the pain assessment (Wong- Baker pain assessment tool) is different and for the
elderly (PACSLAC or Pain Assessment Checklist for Seniors with Limited Ability to
Communicate) with impaired ability it is different as well. Therefore, in a nutshell, it can be
understood that the wound assessment is different in case of different type of wounds and
proper and appropriate wound assessment can lead to quick and faster recovery of the wound.
The pain level is difficult to assess from the photo. Similar like the patient B, PACSLAC or
Pain Assessment Checklist for Seniors with Limited Ability to Communicate can be used in
this scenario as well for the pain assessment of the patient (Lichtner et al., 2014)
Unable to assess undermining due to presence of slough and uncertainty of tissue damage.
However, it could be measured using a sterile probe in case of undermining suspicion.
In the case of Patient C, it is recommended that re-evaluation should be conducted every 3
days and monitoring should be performed for decrease in ratio of slough and increase in
granulation or healthy tissue. Monitoring for signs of infection would be important. The
Frequency of dressing change will be determined by bacterial load and level of exudate. It is
expected that within 2 weeks, the wound will show the signs of improve and if there is no
improvement surgical or specialist management is needed.
The wound shape is oval, the surrounding skin is very dry and appears to be Red/ Pale pink,
peri wound erythema is indicative of a wound infection.
Conclusion:
From the above discussion, it can be said that the assessment was provided for three types of
wounds in this essay. This wound type are burn-scalding, skin tear and wound ulcer. All of
the different types of wounds are different in their appearance and physiology. In addition,
pain assessment tool is also different for the patient as their category is different as well. For
the child the pain assessment (Wong- Baker pain assessment tool) is different and for the
elderly (PACSLAC or Pain Assessment Checklist for Seniors with Limited Ability to
Communicate) with impaired ability it is different as well. Therefore, in a nutshell, it can be
understood that the wound assessment is different in case of different type of wounds and
proper and appropriate wound assessment can lead to quick and faster recovery of the wound.
6WOUND ASSESSMENT
References
Aci.health.nsw.gov.au. (2019). Burn Patient Management: Clinical Guidelines. Retrieved
from https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0009/250020/Burn-
patient-management-guidelines.pdf
Baynav.bopdhb.govt.nz. (2019). STAR Skin Tear Classification S ystem. Retrieved from
https://baynav.bopdhb.govt.nz/media/1480/skin-tear-classification-tool.pdf
Benbow, M. (2016). Best practice in wound assessment. Nursing Standard, 30(27), 40.
doi:10.7748/ns.30.27.40.s45
Carville, K., Leslie, G., Osseiran‐Moisson, R., Newall, N., & Lewin, G. (2014). The
effectiveness of a twice‐daily skin‐moisturising regimen for reducing the incidence of
skin tears. International wound journal, 11(4), 446-453,
https://doi.org/10.1111/iwj.12326.
Carville, K., Lewin, G., Newall, N., Haslehurst, P., Michael, R., Santamaria, N., & Roberts,
P. (2007). STAR: A consensus for skin tear classification. Primary Intention: The
Australian Journal of Wound Management, 15(1), 18-21, 24-28. Retrieved
from http://www.woundsaustralia.com.au/journal/1501_03.pdf
Chan, S., Hadjistavropoulos, T., Williams, J., & Lints-Martindale, A. (2014). Evidence-based
development and initial validation of the pain assessment checklist for seniors with
limited ability to communicate-II (PACSLAC-II). The Clinical journal of pain, 30(9),
816-824, doi: 10.1097/AJP.0000000000000039.
Cornforth, A. (2013). Holistic wound assessment in primary care. British Journal Of
Community Nursing, 18(Sup12), S28-S34. doi: 10.12968/bjcn.2013.18.sup12.s28
References
Aci.health.nsw.gov.au. (2019). Burn Patient Management: Clinical Guidelines. Retrieved
from https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0009/250020/Burn-
patient-management-guidelines.pdf
Baynav.bopdhb.govt.nz. (2019). STAR Skin Tear Classification S ystem. Retrieved from
https://baynav.bopdhb.govt.nz/media/1480/skin-tear-classification-tool.pdf
Benbow, M. (2016). Best practice in wound assessment. Nursing Standard, 30(27), 40.
doi:10.7748/ns.30.27.40.s45
Carville, K., Leslie, G., Osseiran‐Moisson, R., Newall, N., & Lewin, G. (2014). The
effectiveness of a twice‐daily skin‐moisturising regimen for reducing the incidence of
skin tears. International wound journal, 11(4), 446-453,
https://doi.org/10.1111/iwj.12326.
Carville, K., Lewin, G., Newall, N., Haslehurst, P., Michael, R., Santamaria, N., & Roberts,
P. (2007). STAR: A consensus for skin tear classification. Primary Intention: The
Australian Journal of Wound Management, 15(1), 18-21, 24-28. Retrieved
from http://www.woundsaustralia.com.au/journal/1501_03.pdf
Chan, S., Hadjistavropoulos, T., Williams, J., & Lints-Martindale, A. (2014). Evidence-based
development and initial validation of the pain assessment checklist for seniors with
limited ability to communicate-II (PACSLAC-II). The Clinical journal of pain, 30(9),
816-824, doi: 10.1097/AJP.0000000000000039.
Cornforth, A. (2013). Holistic wound assessment in primary care. British Journal Of
Community Nursing, 18(Sup12), S28-S34. doi: 10.12968/bjcn.2013.18.sup12.s28
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7WOUND ASSESSMENT
Edo, A. E., Edo, G. O., & Ezeani, I. U. (2013). Risk factors, ulcer grade and management
outcome of diabetic foot ulcers in a Tropical Tertiary Care Hospital. Nigerian
medical journal: journal of the Nigeria Medical Association, 54(1), 59, doi:
10.4103/0300-1652.108900.
Fette, A. (2006). A clinimetric analysis of wound measurement tools. World Wide
Wounds. Retrieved
from http://www.worldwidewounds.com/2006/january/Fette/Clinimetric-Analysis-
Wound-Measurement-Tools.html
Greatrex‐White, S., & Moxey, H. (2015). Wound assessment tools and nurses' needs: an
evaluation study. International wound journal, 12(3), 293-301,
https://doi.org/10.1111/iwj.12100.
Harries, R. L., Bosanquet, D. C., & Harding, K. G. (2016). Wound bed preparation: TIME for
an update. International wound journal, 13(S3), 8-14, DOI: 10.1111/iwj.12662.
Keast, D., Bowering, K., Evans, A., MacKean, G., Burrows, C., & D'Souza, L. (2004).
MEASURE: A proposed assessment framework for developing best practice
recommendations for wound assessment. Wound Repair and Regeneration, 12(3), S1-
S17. DOI:10.1111/j.1067-1927.2004.0123S1.x
Keast, D., Bowering, K., Evans, A., MacKean, G.,Burrows, C., & D'Souza, L. (2004).
MEASURE: a proposed assessment framework for developing best practice
recommendations for wound assessment. Wound Repair and Regeneration, 12(3),
S1-S17. doi:10.1111/j.1067-1927.2004.0123S1.x
Knowles, J. (2015). A new method for closing skin tears in elderly patients - Clinical
Advisor. Retrieved from https://www.clinicaladvisor.com/home/the-waiting-room/a-
new-method-for-closing-skin-tears-in-elderly-patients/
Edo, A. E., Edo, G. O., & Ezeani, I. U. (2013). Risk factors, ulcer grade and management
outcome of diabetic foot ulcers in a Tropical Tertiary Care Hospital. Nigerian
medical journal: journal of the Nigeria Medical Association, 54(1), 59, doi:
10.4103/0300-1652.108900.
Fette, A. (2006). A clinimetric analysis of wound measurement tools. World Wide
Wounds. Retrieved
from http://www.worldwidewounds.com/2006/january/Fette/Clinimetric-Analysis-
Wound-Measurement-Tools.html
Greatrex‐White, S., & Moxey, H. (2015). Wound assessment tools and nurses' needs: an
evaluation study. International wound journal, 12(3), 293-301,
https://doi.org/10.1111/iwj.12100.
Harries, R. L., Bosanquet, D. C., & Harding, K. G. (2016). Wound bed preparation: TIME for
an update. International wound journal, 13(S3), 8-14, DOI: 10.1111/iwj.12662.
Keast, D., Bowering, K., Evans, A., MacKean, G., Burrows, C., & D'Souza, L. (2004).
MEASURE: A proposed assessment framework for developing best practice
recommendations for wound assessment. Wound Repair and Regeneration, 12(3), S1-
S17. DOI:10.1111/j.1067-1927.2004.0123S1.x
Keast, D., Bowering, K., Evans, A., MacKean, G.,Burrows, C., & D'Souza, L. (2004).
MEASURE: a proposed assessment framework for developing best practice
recommendations for wound assessment. Wound Repair and Regeneration, 12(3),
S1-S17. doi:10.1111/j.1067-1927.2004.0123S1.x
Knowles, J. (2015). A new method for closing skin tears in elderly patients - Clinical
Advisor. Retrieved from https://www.clinicaladvisor.com/home/the-waiting-room/a-
new-method-for-closing-skin-tears-in-elderly-patients/
8WOUND ASSESSMENT
LeBlanc, K., Woo, K., Christensen, D., Forest-Lalande, L., O’Dea,J., Varga, M., McSwiggan,
J. & van Ineveld, C. (2018). Best practice recommendations for the prevention and
management of skin tears. WoundsCanada. Retrieved
from https://www.woundscanada.ca/docman/public/health-care-professional/bpr-
workshop/552-bpr-prevention-and-management-of-skin-tears
Lichtner, V., Dowding, D., Esterhuizen, P., Closs, S. J., Long, A. F., Corbett, A., & Briggs,
M. (2014). Pain assessment for people with dementia: a systematic review of
systematic reviews of pain assessment tools. BMC geriatrics, 14(1), 138,
https://doi.org/10.1186/1471-2318-14-138.
Mukherjee, R., Manohar, D. D., Das, D. K., Achar, A., Mitra, A., & Chakraborty, C. (2014).
Automated tissue classification framework for reproducible chronic wound
assessment. BioMed research international, 2014.
Palmieri, T. L. (2016). Pediatric burn resuscitation. Crit Care Clin, 32(4), 547-59, doi:
10.1016/j.ccc.2016.06.004.
Savino, F., Vagliano, L., Ceratto, S., Viviani, F., Miniero, R., & Ricceri, F. (2013). Pain
assessment in children undergoing venipuncture: the Wong–Baker faces scale versus
skin conductance fluctuations. PeerJ, 1, e37, https://doi.org/10.7717/peerj.37.
Stephen-Haynes J, Carville K. Skin tears Made Easy. Wounds International 2011; 2(4):
Retrieved from http://www.woundsinternational.com
Vic Burns. (2019). Paediatric Burn Assessment - Vic Burns. Retrieved from
https://www.vicburns.org.au/burn-assessment-overview/burn-tbsa/lund-browder/
Vowden, K., & Vowden, P. (2017). Wound dressings: principles and practice. Surgery
(Oxford), 35(9), 489-494, https://doi.org/10.1016/j.mpsur.2017.06.005.
LeBlanc, K., Woo, K., Christensen, D., Forest-Lalande, L., O’Dea,J., Varga, M., McSwiggan,
J. & van Ineveld, C. (2018). Best practice recommendations for the prevention and
management of skin tears. WoundsCanada. Retrieved
from https://www.woundscanada.ca/docman/public/health-care-professional/bpr-
workshop/552-bpr-prevention-and-management-of-skin-tears
Lichtner, V., Dowding, D., Esterhuizen, P., Closs, S. J., Long, A. F., Corbett, A., & Briggs,
M. (2014). Pain assessment for people with dementia: a systematic review of
systematic reviews of pain assessment tools. BMC geriatrics, 14(1), 138,
https://doi.org/10.1186/1471-2318-14-138.
Mukherjee, R., Manohar, D. D., Das, D. K., Achar, A., Mitra, A., & Chakraborty, C. (2014).
Automated tissue classification framework for reproducible chronic wound
assessment. BioMed research international, 2014.
Palmieri, T. L. (2016). Pediatric burn resuscitation. Crit Care Clin, 32(4), 547-59, doi:
10.1016/j.ccc.2016.06.004.
Savino, F., Vagliano, L., Ceratto, S., Viviani, F., Miniero, R., & Ricceri, F. (2013). Pain
assessment in children undergoing venipuncture: the Wong–Baker faces scale versus
skin conductance fluctuations. PeerJ, 1, e37, https://doi.org/10.7717/peerj.37.
Stephen-Haynes J, Carville K. Skin tears Made Easy. Wounds International 2011; 2(4):
Retrieved from http://www.woundsinternational.com
Vic Burns. (2019). Paediatric Burn Assessment - Vic Burns. Retrieved from
https://www.vicburns.org.au/burn-assessment-overview/burn-tbsa/lund-browder/
Vowden, K., & Vowden, P. (2017). Wound dressings: principles and practice. Surgery
(Oxford), 35(9), 489-494, https://doi.org/10.1016/j.mpsur.2017.06.005.

9WOUND ASSESSMENT
Wounds UK (2018) Best Practice Statement maintaining skin integrity. London: Wounds
UK. Retrieved at www.wounds-uk.com
Wounds UK (2018) Best Practice Statement maintaining skin integrity. London: Wounds
UK. Retrieved at www.wounds-uk.com
1 out of 10
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





