University Wound Care Management Guidelines: A Comparative Critique
VerifiedAdded on 2023/06/03
|17
|3928
|314
Report
AI Summary
This report critically appraises two wound care management guidelines: one developed by NHS Foundation Trust and another by HSE. The analysis utilizes the AGREE II tool to evaluate the guidelines across several domains including scope and purpose, stakeholder involvement, rigor of development, clarity of presentation, and applicability. The report identifies the HSE guidelines as superior due to its comprehensive approach, explicit details regarding evidence search strategies, and clear presentation of recommendations categorized by wound type, unlike the NHS guidelines. The report highlights the importance of stakeholder involvement and transparent reporting to ensure the credibility and practical application of clinical practice guidelines. It also discusses the differences in quality, emphasizing the completeness of information and consideration of all necessary information for application of evidence into practice. The study concludes with recommendations for developing evidence-based clinical practice guidelines and promoting transparency of evidence.

0Running head: WOUND CARE MANAGEMENT
Wound care management
Name of the student:
Name of the University:
Author’s note
Wound care management
Name of the student:
Name of the University:
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1WOUND CARE MANAGEMENT
Introduction:
Chronic wound like pressure ulcers and neuropathic ulcers posed unique challenges for
wound care professionals. To ensure that uniform policy exists regarding treating acute wounds
in all setting, many evidenced based guidelines have been developed. These guidelines have
played a role in reducing barriers for wound healing and promoting consistency in the
documentation of wound care. Interdisciplinary communication is also enhanced by the
development of wound care management guidelines (Ubbink et al., 2015). The main purpose of
this paper is to critique two wound care management guidelines using the AGREE 11 tool and
comparatively evaluate the strength and weakness of the two tools. The first tool that will be
used in this paper include the ‘Guideline for the Assessment & Management of Wounds’
developed by NHS foundation trust for the Northamptonshire Trust. This guideline gives idea
about measures that can be taken when normal wound healing fails (NHS Foundation Trust
2017). In addition, the second tool that will be analyzed include the ‘HSE National Wound
Management Guidelines 2018’ developed for Irish health care setting. This guideline is an
updated guideline that provides evidence based approach for wound care management (Wynne
2018).
Critique of the 2 clinical practice guideline using the AGREE 11 tool:
The critique of the tools and results obtained using the AGREE 11 tool has been provided
in appendix.
Introduction:
Chronic wound like pressure ulcers and neuropathic ulcers posed unique challenges for
wound care professionals. To ensure that uniform policy exists regarding treating acute wounds
in all setting, many evidenced based guidelines have been developed. These guidelines have
played a role in reducing barriers for wound healing and promoting consistency in the
documentation of wound care. Interdisciplinary communication is also enhanced by the
development of wound care management guidelines (Ubbink et al., 2015). The main purpose of
this paper is to critique two wound care management guidelines using the AGREE 11 tool and
comparatively evaluate the strength and weakness of the two tools. The first tool that will be
used in this paper include the ‘Guideline for the Assessment & Management of Wounds’
developed by NHS foundation trust for the Northamptonshire Trust. This guideline gives idea
about measures that can be taken when normal wound healing fails (NHS Foundation Trust
2017). In addition, the second tool that will be analyzed include the ‘HSE National Wound
Management Guidelines 2018’ developed for Irish health care setting. This guideline is an
updated guideline that provides evidence based approach for wound care management (Wynne
2018).
Critique of the 2 clinical practice guideline using the AGREE 11 tool:
The critique of the tools and results obtained using the AGREE 11 tool has been provided
in appendix.
2WOUND CARE MANAGEMENT
Discussion on why one of the guideline is better than the other:
Based on the critique of the two wound care management guidelines, it can be said that
the ‘HSE National Wound Management Guidelines 2018’ is better than the ‘Guideline for the
Assessment & Management of Wounds’ because of completeness of information and
consideration of all important information that is needed for application of evidence into
practice. The discussion regarding the recommendations mentioned by each tool and the method
of reporting can give idea regarding the difference in quality of both tools. The ‘Guideline for the
Assessment & Management of Wounds’ will be defined as guideline 1 and the ‘HSE National
Wound Management Guidelines 2018’ will be described as guideline 2 from this section.
While reviewing the reporting methods for both the guidelines, it can be said that
guideline 2 provides complete information with information not just on the key recommendation
but also on the method of developing the guideline. While critically appraising the guideline 1
using the AGREE tool, it has been found that the document lacks rigor of development. The
purpose and scope section of the document mentions that the wound care management guidance
is based on evidence based care principles. However, this information is not considered reliable
because no information has been provided regarding the method adapted to search for evidence
and critically evaluation them before framing it as a recommendation. Majid et al (2018) argues
that while engaging in evidence based practice, it is necessary to adapt an appropriate search
strategy and retrieve current and relevant evidence. Hence, presence of information related to
search strategy and process used to critically evaluate research evidence would have increased
the rigour and reliability of the guideline. The guideline 1 by NHS Foundation Trust (2017) has
not reported about search strategy and this seriously impedes the reliability as well as the
application of evidence. In contrast, the guideline 2 by Wynne (2018) gave information about the
Discussion on why one of the guideline is better than the other:
Based on the critique of the two wound care management guidelines, it can be said that
the ‘HSE National Wound Management Guidelines 2018’ is better than the ‘Guideline for the
Assessment & Management of Wounds’ because of completeness of information and
consideration of all important information that is needed for application of evidence into
practice. The discussion regarding the recommendations mentioned by each tool and the method
of reporting can give idea regarding the difference in quality of both tools. The ‘Guideline for the
Assessment & Management of Wounds’ will be defined as guideline 1 and the ‘HSE National
Wound Management Guidelines 2018’ will be described as guideline 2 from this section.
While reviewing the reporting methods for both the guidelines, it can be said that
guideline 2 provides complete information with information not just on the key recommendation
but also on the method of developing the guideline. While critically appraising the guideline 1
using the AGREE tool, it has been found that the document lacks rigor of development. The
purpose and scope section of the document mentions that the wound care management guidance
is based on evidence based care principles. However, this information is not considered reliable
because no information has been provided regarding the method adapted to search for evidence
and critically evaluation them before framing it as a recommendation. Majid et al (2018) argues
that while engaging in evidence based practice, it is necessary to adapt an appropriate search
strategy and retrieve current and relevant evidence. Hence, presence of information related to
search strategy and process used to critically evaluate research evidence would have increased
the rigour and reliability of the guideline. The guideline 1 by NHS Foundation Trust (2017) has
not reported about search strategy and this seriously impedes the reliability as well as the
application of evidence. In contrast, the guideline 2 by Wynne (2018) gave information about the
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3WOUND CARE MANAGEMENT
development of guidelines by giving explicit details related to the clinical question, literature
search strategy, data extraction and data analysis technique and quality appraisal. Wynne (2018)
also considered grading all the recommendation after developing grading scheme. This technique
is commendable as it used the hierarchy of evidence types from which the information was
sourced to grade the recommendation. Hierarchical system of classifying evidence is the
cornerstone of evidence based medicine and understanding the level of evidence can help to
interpret and prioritize information (Burns, Rohrich and Chung 2011).
Another major difference between the protocol is the clarity of presentation. The
recommendations proposed is the most vital component of the two wound management
guidelines and the quality of presentation can determine whether it is useful for the target setting
or not. In terms of presentation of content, it can be said that there is stark difference between the
two guidelines. For example, the presentation of recommendation by Wynne (2018) is very
focused and relevant to the main challenges faced during wound management in clinical setting.
For example, burden of care increase due to hospitalization for non-healing wounds like surgical
wound, pressure ulcers and foot ulcers. Hence, those guideline would be useful that categorise
different types of wound and then suggest specific advice for clinical practice. Accordingly,
guideline 2 by Wynne (2018) considered different wound management situation and classified
the recommendation by discussing about general wound care, diabetic foot ulcers, pressure
ulcers, leg ulcer and palliatiave wound care separately. For each area, recommendation was
proposed for risk assessment, assessment tool and recommendation. Compared to guideline 2,
guideline 1 by NHS Foundation Trust (2017) has very ambiguous information related to wound
care management. This is because it defines the process of wound healing, documentation of
wound care and different dressing types but not separate process for management of different
development of guidelines by giving explicit details related to the clinical question, literature
search strategy, data extraction and data analysis technique and quality appraisal. Wynne (2018)
also considered grading all the recommendation after developing grading scheme. This technique
is commendable as it used the hierarchy of evidence types from which the information was
sourced to grade the recommendation. Hierarchical system of classifying evidence is the
cornerstone of evidence based medicine and understanding the level of evidence can help to
interpret and prioritize information (Burns, Rohrich and Chung 2011).
Another major difference between the protocol is the clarity of presentation. The
recommendations proposed is the most vital component of the two wound management
guidelines and the quality of presentation can determine whether it is useful for the target setting
or not. In terms of presentation of content, it can be said that there is stark difference between the
two guidelines. For example, the presentation of recommendation by Wynne (2018) is very
focused and relevant to the main challenges faced during wound management in clinical setting.
For example, burden of care increase due to hospitalization for non-healing wounds like surgical
wound, pressure ulcers and foot ulcers. Hence, those guideline would be useful that categorise
different types of wound and then suggest specific advice for clinical practice. Accordingly,
guideline 2 by Wynne (2018) considered different wound management situation and classified
the recommendation by discussing about general wound care, diabetic foot ulcers, pressure
ulcers, leg ulcer and palliatiave wound care separately. For each area, recommendation was
proposed for risk assessment, assessment tool and recommendation. Compared to guideline 2,
guideline 1 by NHS Foundation Trust (2017) has very ambiguous information related to wound
care management. This is because it defines the process of wound healing, documentation of
wound care and different dressing types but not separate process for management of different
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4WOUND CARE MANAGEMENT
wounds. This is a major limitation of the guideline as health care professionals would not be able
to apply the guidelines in clinical practice. It does not present any systematic recommendations
such as type of risk assessment and management process needed for different types of wound.
Hence, this justified why guideline 1 is inferior to guideline 2 in terms of quality and content of
the presentation. The purpose of developing clinical guideline is defeated due to lack of clarity in
presentation and poor relevance of the guideline in the context of real practice (Yaşar et al.
2016).
Shekelle et al. (2012) suggest that while developing any clinical practice guideline, it is
important to develop strategies to increase uptake of the guideline. For example, this would be
possible by taking steps to identify potential barriers of recommendation, using specific
language, identification of resource implication and use of data collection tool. Similar type of
technique has been considered by Wynne (2018) for developing the guideline too. For example,
guideline 2 covered all details regarding potential barriers for each recommendation. In addition,
the overall facilitators to the implementation of the guideline were also identified. The clarity in
reporting about barrier and facilitators is also understood from the fact that the developer also
reported about strategies to address the barrier and defining facilitators that would improve
uptake of the guideline. Throughout the reporting about recommendations for wound care,
resource implication was discussed too. In contrast, tool 1 by NHS Foundation Trust (2017) also
identified barriers to the application of the evidence. However, resource implication and specific
training needs were missing. For this reason, guideline 2 is considered better than guideline 1.
Fischer et al. (2016) also supports the fact the success of the implementation of guidelines is
dependent on the consideration of barriers and strategies to address them. This can promote
adherence to the guideline and development of strategies tailored to the specific health setting.
wounds. This is a major limitation of the guideline as health care professionals would not be able
to apply the guidelines in clinical practice. It does not present any systematic recommendations
such as type of risk assessment and management process needed for different types of wound.
Hence, this justified why guideline 1 is inferior to guideline 2 in terms of quality and content of
the presentation. The purpose of developing clinical guideline is defeated due to lack of clarity in
presentation and poor relevance of the guideline in the context of real practice (Yaşar et al.
2016).
Shekelle et al. (2012) suggest that while developing any clinical practice guideline, it is
important to develop strategies to increase uptake of the guideline. For example, this would be
possible by taking steps to identify potential barriers of recommendation, using specific
language, identification of resource implication and use of data collection tool. Similar type of
technique has been considered by Wynne (2018) for developing the guideline too. For example,
guideline 2 covered all details regarding potential barriers for each recommendation. In addition,
the overall facilitators to the implementation of the guideline were also identified. The clarity in
reporting about barrier and facilitators is also understood from the fact that the developer also
reported about strategies to address the barrier and defining facilitators that would improve
uptake of the guideline. Throughout the reporting about recommendations for wound care,
resource implication was discussed too. In contrast, tool 1 by NHS Foundation Trust (2017) also
identified barriers to the application of the evidence. However, resource implication and specific
training needs were missing. For this reason, guideline 2 is considered better than guideline 1.
Fischer et al. (2016) also supports the fact the success of the implementation of guidelines is
dependent on the consideration of barriers and strategies to address them. This can promote
adherence to the guideline and development of strategies tailored to the specific health setting.
5WOUND CARE MANAGEMENT
On comparison of the two wound care management guideline, another difference has
been found in the reporting about stakeholder involvement. According to Massoni, Ricci and
Ricci (2014), review of stakeholder involvement is necessary in evidence based medicine as this
has an impact on the formulation of the recommendation and operational applicability of the
evidence. The guideline 1 gave no details about stakeholder involvement and guideline 2 gave all
details related to types of stakeholders involved and approach taken to critically appraise the
recommendations identified from different research papers related to wound care. Hence, as no
details have been provided regarding stakeholder involvement, it has affected the quality of
recommendation and direct application of the guideline in clinical practice too. In contrast, the
guideline presented by Wynne (2018) is very reliable because of transparent reporting and it can
be easily applied in clinical setting.
Possible reasons for difference in the quality of the two tools:
The above discussion on the quality of the two selected wound management guidelines
reveals several differences in the quality of the protocol. Such differences might have occurred
because of lack of engagement of appropriate stakeholders during the development of tool 1.
This can be said because both the guidelines were backed by renowned agencies like HSE and
the NHS, but still the desired level of recommendation was not found for guideline 1. This could
be explained by lack of involvement of experienced stakeholders from the field of wound care
and management while developing guideline 1. In contrast, guideline 1 was framed based on the
clinical judgment and decision making done by stakeholders from relevant field of interest. The
quality of the guideline 1 might have been compromised because of personal factors like lack of
agreement and efficacy of the key stakeholders too. Individualized audit and feedback was also
not done which might have affected the quality of the guideline.
On comparison of the two wound care management guideline, another difference has
been found in the reporting about stakeholder involvement. According to Massoni, Ricci and
Ricci (2014), review of stakeholder involvement is necessary in evidence based medicine as this
has an impact on the formulation of the recommendation and operational applicability of the
evidence. The guideline 1 gave no details about stakeholder involvement and guideline 2 gave all
details related to types of stakeholders involved and approach taken to critically appraise the
recommendations identified from different research papers related to wound care. Hence, as no
details have been provided regarding stakeholder involvement, it has affected the quality of
recommendation and direct application of the guideline in clinical practice too. In contrast, the
guideline presented by Wynne (2018) is very reliable because of transparent reporting and it can
be easily applied in clinical setting.
Possible reasons for difference in the quality of the two tools:
The above discussion on the quality of the two selected wound management guidelines
reveals several differences in the quality of the protocol. Such differences might have occurred
because of lack of engagement of appropriate stakeholders during the development of tool 1.
This can be said because both the guidelines were backed by renowned agencies like HSE and
the NHS, but still the desired level of recommendation was not found for guideline 1. This could
be explained by lack of involvement of experienced stakeholders from the field of wound care
and management while developing guideline 1. In contrast, guideline 1 was framed based on the
clinical judgment and decision making done by stakeholders from relevant field of interest. The
quality of the guideline 1 might have been compromised because of personal factors like lack of
agreement and efficacy of the key stakeholders too. Individualized audit and feedback was also
not done which might have affected the quality of the guideline.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6WOUND CARE MANAGEMENT
Conclusion:
The report summarized the results obtained based on the critical appraisal of two wound
care management guidelines using the AGREE tool. The AGREE tool evaluated the two
guideline based on the elements like scope and purpose, stakeholder involvement, rigor of
development, clarity of presentation and applicability of the evidence. The overall conclusion
from the critical appraisal is that guideline 2 (HSE National Wound Management Guidelines
2018’ is better than guideline 1 (NHS Foundation Trust 2017). The main rationale behind this is
that guideline 2 addressed all elements that were needed for increasing the reliability of the
recommendation, promoting transparency in reporting and enhancing the credibility of the
information. The reporting process was complete with detailed information about search
strategy, critical appraisal and grading of evidence, barriers to research application and resource
implication. In addition, wound care management recommendation was clearly specified by
categorizing types of wound care in guideline 2. However, guideline 1 could not be directly
applied for evidence based practice before of presence ambiguous information and many missing
information. It is recommended to follow the principles of evidence based practice while
developing clinical practice guidelines and consider factors to promote transparency of the
evidence.
Conclusion:
The report summarized the results obtained based on the critical appraisal of two wound
care management guidelines using the AGREE tool. The AGREE tool evaluated the two
guideline based on the elements like scope and purpose, stakeholder involvement, rigor of
development, clarity of presentation and applicability of the evidence. The overall conclusion
from the critical appraisal is that guideline 2 (HSE National Wound Management Guidelines
2018’ is better than guideline 1 (NHS Foundation Trust 2017). The main rationale behind this is
that guideline 2 addressed all elements that were needed for increasing the reliability of the
recommendation, promoting transparency in reporting and enhancing the credibility of the
information. The reporting process was complete with detailed information about search
strategy, critical appraisal and grading of evidence, barriers to research application and resource
implication. In addition, wound care management recommendation was clearly specified by
categorizing types of wound care in guideline 2. However, guideline 1 could not be directly
applied for evidence based practice before of presence ambiguous information and many missing
information. It is recommended to follow the principles of evidence based practice while
developing clinical practice guidelines and consider factors to promote transparency of the
evidence.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7WOUND CARE MANAGEMENT
References:
Burns, P.B., Rohrich, R.J. and Chung, K.C., 2011. The levels of evidence and their role in
evidence-based medicine. Plastic and reconstructive surgery, 128(1), p.305.
Fischer, F., Lange, K., Klose, K., Greiner, W. and Kraemer, A., 2016, June. Barriers and
strategies in guideline implementation—a scoping review. In Healthcare (Vol. 4, No. 3, p. 36).
Multidisciplinary Digital Publishing Institute.
Majid, S., Foo, S., Luyt, B., Zhang, X., Theng, Y.L., Chang, Y.K. and Mokhtar, I.A., 2011.
Adopting evidence-based practice in clinical decision making: nurses' perceptions, knowledge,
and barriers. Journal of the Medical Library Association: JMLA, 99(3), p.229.
Massoni, F., Ricci, P. and Ricci, S., 2014. Guidelines and evidence based medicine. The
importance of stakeholder involvement. Reviews in Health Care, 5(3), pp.109-115.
NHS Foundation Trust 2017. Guidelines for the assessment & management of wounds. Retrieved
from:
https://www.nhft.nhs.uk/download.cfm?doc=docm93jijm4n1793.pdf&ver=17402
Shekelle, P., Woolf, S., Grimshaw, J.M., Schünemann, H.J. and Eccles, M.P., 2012. Developing
clinical practice guidelines: reviewing, reporting, and publishing guidelines; updating guidelines;
and the emerging issues of enhancing guideline implementability and accounting for comorbid
conditions in guideline development. Implementation Science, 7(1), p.62.
Ubbink, D.T., Brölmann, F.E., Go, P.M. and Vermeulen, H., 2015. Evidence-based care of acute
wounds: a perspective. Advances in wound care, 4(5), pp.286-294.
References:
Burns, P.B., Rohrich, R.J. and Chung, K.C., 2011. The levels of evidence and their role in
evidence-based medicine. Plastic and reconstructive surgery, 128(1), p.305.
Fischer, F., Lange, K., Klose, K., Greiner, W. and Kraemer, A., 2016, June. Barriers and
strategies in guideline implementation—a scoping review. In Healthcare (Vol. 4, No. 3, p. 36).
Multidisciplinary Digital Publishing Institute.
Majid, S., Foo, S., Luyt, B., Zhang, X., Theng, Y.L., Chang, Y.K. and Mokhtar, I.A., 2011.
Adopting evidence-based practice in clinical decision making: nurses' perceptions, knowledge,
and barriers. Journal of the Medical Library Association: JMLA, 99(3), p.229.
Massoni, F., Ricci, P. and Ricci, S., 2014. Guidelines and evidence based medicine. The
importance of stakeholder involvement. Reviews in Health Care, 5(3), pp.109-115.
NHS Foundation Trust 2017. Guidelines for the assessment & management of wounds. Retrieved
from:
https://www.nhft.nhs.uk/download.cfm?doc=docm93jijm4n1793.pdf&ver=17402
Shekelle, P., Woolf, S., Grimshaw, J.M., Schünemann, H.J. and Eccles, M.P., 2012. Developing
clinical practice guidelines: reviewing, reporting, and publishing guidelines; updating guidelines;
and the emerging issues of enhancing guideline implementability and accounting for comorbid
conditions in guideline development. Implementation Science, 7(1), p.62.
Ubbink, D.T., Brölmann, F.E., Go, P.M. and Vermeulen, H., 2015. Evidence-based care of acute
wounds: a perspective. Advances in wound care, 4(5), pp.286-294.
8WOUND CARE MANAGEMENT
Wynne, M. 2018. HSE National Wound Management Guidelines 2018. Retrieved from:
https://www.lenus.ie/handle/10147/623616
Yaşar, I., Kahveci, R., Artantaş, A. B., Başer, D. A., Cihan, F. G., Şencan, I., ... & Özkara, A.
(2016). Quality assessment of clinical practice guidelines developed by professional societies in
Turkey. PloS one, 11(6), e0156483.
Wynne, M. 2018. HSE National Wound Management Guidelines 2018. Retrieved from:
https://www.lenus.ie/handle/10147/623616
Yaşar, I., Kahveci, R., Artantaş, A. B., Başer, D. A., Cihan, F. G., Şencan, I., ... & Özkara, A.
(2016). Quality assessment of clinical practice guidelines developed by professional societies in
Turkey. PloS one, 11(6), e0156483.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
9WOUND CARE MANAGEMENT
Appendix:
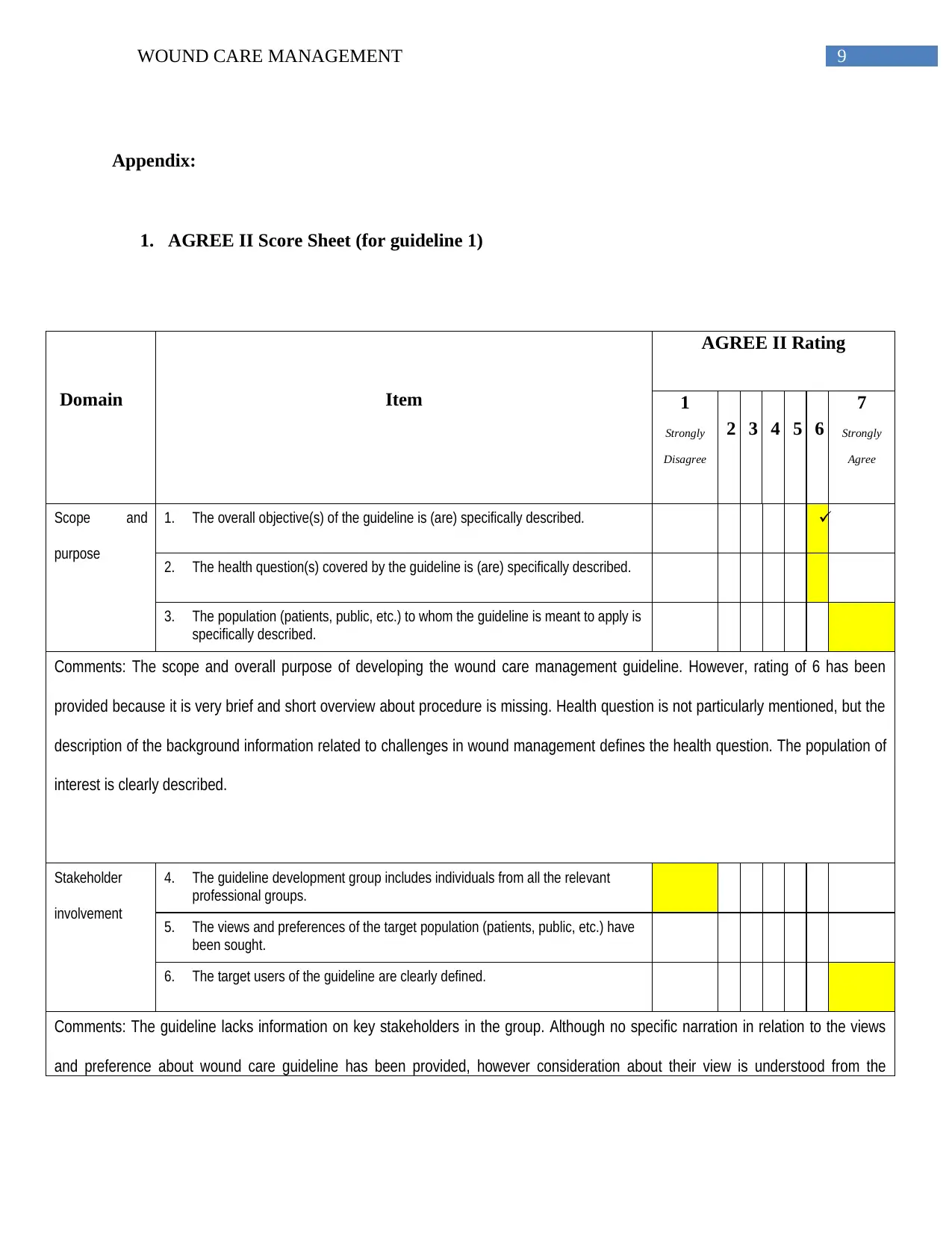
1. AGREE II Score Sheet (for guideline 1)
Domain Item
AGREE II Rating
1
Strongly
Disagree
2 3 4 5 6
7
Strongly
Agree
Scope and
purpose
1. The overall objective(s) of the guideline is (are) specifically described.
2. The health question(s) covered by the guideline is (are) specifically described.
3. The population (patients, public, etc.) to whom the guideline is meant to apply is
specifically described.
Comments: The scope and overall purpose of developing the wound care management guideline. However, rating of 6 has been
provided because it is very brief and short overview about procedure is missing. Health question is not particularly mentioned, but the
description of the background information related to challenges in wound management defines the health question. The population of
interest is clearly described.
Stakeholder
involvement
4. The guideline development group includes individuals from all the relevant
professional groups.
5. The views and preferences of the target population (patients, public, etc.) have
been sought.
6. The target users of the guideline are clearly defined.
Comments: The guideline lacks information on key stakeholders in the group. Although no specific narration in relation to the views
and preference about wound care guideline has been provided, however consideration about their view is understood from the
Appendix:
1. AGREE II Score Sheet (for guideline 1)
Domain Item
AGREE II Rating
1
Strongly
Disagree
2 3 4 5 6
7
Strongly
Agree
Scope and
purpose
1. The overall objective(s) of the guideline is (are) specifically described.
2. The health question(s) covered by the guideline is (are) specifically described.
3. The population (patients, public, etc.) to whom the guideline is meant to apply is
specifically described.
Comments: The scope and overall purpose of developing the wound care management guideline. However, rating of 6 has been
provided because it is very brief and short overview about procedure is missing. Health question is not particularly mentioned, but the
description of the background information related to challenges in wound management defines the health question. The population of
interest is clearly described.
Stakeholder
involvement
4. The guideline development group includes individuals from all the relevant
professional groups.
5. The views and preferences of the target population (patients, public, etc.) have
been sought.
6. The target users of the guideline are clearly defined.
Comments: The guideline lacks information on key stakeholders in the group. Although no specific narration in relation to the views
and preference about wound care guideline has been provided, however consideration about their view is understood from the
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
10WOUND CARE MANAGEMENT
Domain Item
AGREE II Rating
1
Strongly
Disagree
2 3 4 5 6
7
Strongly
Agree
introduction section.
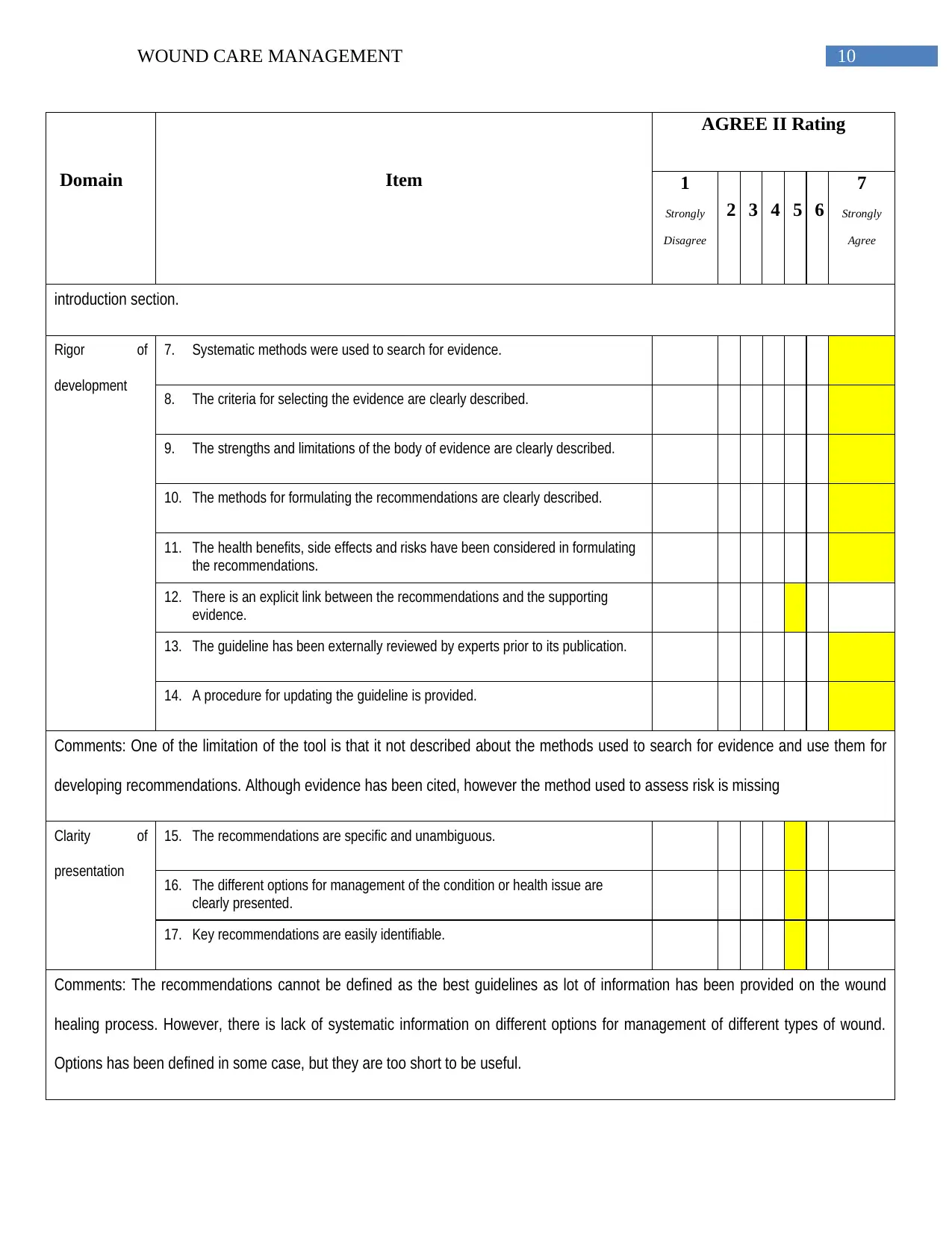
Rigor of
development
7. Systematic methods were used to search for evidence.
8. The criteria for selecting the evidence are clearly described.
9. The strengths and limitations of the body of evidence are clearly described.
10. The methods for formulating the recommendations are clearly described.
11. The health benefits, side effects and risks have been considered in formulating
the recommendations.
12. There is an explicit link between the recommendations and the supporting
evidence.
13. The guideline has been externally reviewed by experts prior to its publication.
14. A procedure for updating the guideline is provided.
Comments: One of the limitation of the tool is that it not described about the methods used to search for evidence and use them for
developing recommendations. Although evidence has been cited, however the method used to assess risk is missing
Clarity of
presentation
15. The recommendations are specific and unambiguous.
16. The different options for management of the condition or health issue are
clearly presented.
17. Key recommendations are easily identifiable.
Comments: The recommendations cannot be defined as the best guidelines as lot of information has been provided on the wound
healing process. However, there is lack of systematic information on different options for management of different types of wound.
Options has been defined in some case, but they are too short to be useful.
Domain Item
AGREE II Rating
1
Strongly
Disagree
2 3 4 5 6
7
Strongly
Agree
introduction section.
Rigor of
development
7. Systematic methods were used to search for evidence.
8. The criteria for selecting the evidence are clearly described.
9. The strengths and limitations of the body of evidence are clearly described.
10. The methods for formulating the recommendations are clearly described.
11. The health benefits, side effects and risks have been considered in formulating
the recommendations.
12. There is an explicit link between the recommendations and the supporting
evidence.
13. The guideline has been externally reviewed by experts prior to its publication.
14. A procedure for updating the guideline is provided.
Comments: One of the limitation of the tool is that it not described about the methods used to search for evidence and use them for
developing recommendations. Although evidence has been cited, however the method used to assess risk is missing
Clarity of
presentation
15. The recommendations are specific and unambiguous.
16. The different options for management of the condition or health issue are
clearly presented.
17. Key recommendations are easily identifiable.
Comments: The recommendations cannot be defined as the best guidelines as lot of information has been provided on the wound
healing process. However, there is lack of systematic information on different options for management of different types of wound.
Options has been defined in some case, but they are too short to be useful.
11WOUND CARE MANAGEMENT
Domain Item
AGREE II Rating
1
Strongly
Disagree
2 3 4 5 6
7
Strongly
Agree
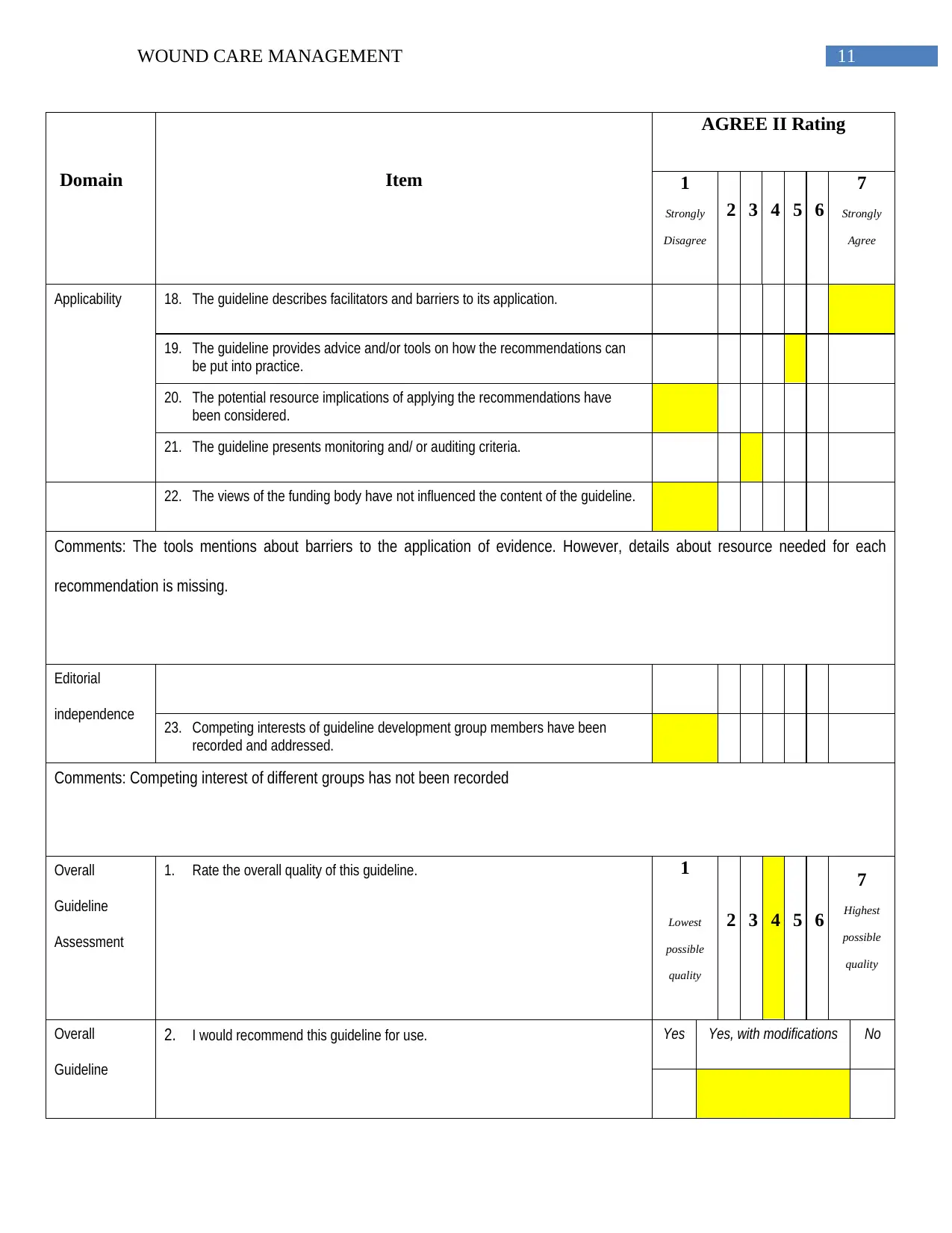
Applicability 18. The guideline describes facilitators and barriers to its application.
19. The guideline provides advice and/or tools on how the recommendations can
be put into practice.
20. The potential resource implications of applying the recommendations have
been considered.
21. The guideline presents monitoring and/ or auditing criteria.
22. The views of the funding body have not influenced the content of the guideline.
Comments: The tools mentions about barriers to the application of evidence. However, details about resource needed for each
recommendation is missing.
Editorial
independence 23. Competing interests of guideline development group members have been
recorded and addressed.
Comments: Competing interest of different groups has not been recorded
Overall
Guideline
Assessment
1. Rate the overall quality of this guideline. 1
Lowest
possible
quality
2 3 4 5 6
7
Highest
possible
quality
Overall
Guideline
2. I would recommend this guideline for use. Yes Yes, with modifications No
Domain Item
AGREE II Rating
1
Strongly
Disagree
2 3 4 5 6
7
Strongly
Agree
Applicability 18. The guideline describes facilitators and barriers to its application.
19. The guideline provides advice and/or tools on how the recommendations can
be put into practice.
20. The potential resource implications of applying the recommendations have
been considered.
21. The guideline presents monitoring and/ or auditing criteria.
22. The views of the funding body have not influenced the content of the guideline.
Comments: The tools mentions about barriers to the application of evidence. However, details about resource needed for each
recommendation is missing.
Editorial
independence 23. Competing interests of guideline development group members have been
recorded and addressed.
Comments: Competing interest of different groups has not been recorded
Overall
Guideline
Assessment
1. Rate the overall quality of this guideline. 1
Lowest
possible
quality
2 3 4 5 6
7
Highest
possible
quality
Overall
Guideline
2. I would recommend this guideline for use. Yes Yes, with modifications No
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 17
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





