HLTENN006 Wound Management Plan: Diabetic Foot Ulcer Case Study
VerifiedAdded on 2023/06/11
|9
|1813
|430
Report
AI Summary
This report details a comprehensive wound management plan for a 70-year-old patient with type 2 diabetes and a diabetic foot ulcer. It includes the patient's diagnosis, medical history, and nutritional status. The plan covers wound evaluation, including wound bed status, measurements, surrounding skin condition, and exudate analysis. It addresses the actual and potential impacts of the wound, such as peripheral neuropathy and mobility issues, and discusses the physiology of the healing process in diabetic patients, including factors like hyperglycemia and impaired growth factor expression. The wound management plan outlines specific interventions such as sucrose octasulfate dressings, cleaning protocols, infection control measures, and moisture balance techniques. It also emphasizes health education for the patient, pain management strategies, and a wound care assessment plan, with adjustments made based on the wound's progress. The report concludes with relevant references to support the outlined strategies. Desklib provides access to similar solved assignments.

Running head: WOUND CARE PLAN
WOUND CARE PLAN
Name of the Student
Name of the university
Author’s note
WOUND CARE PLAN
Name of the Student
Name of the university
Author’s note
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
1
WOUND CARE PLAN
Wound care plan
1. Diagnosis of chosen individual including
Presenting problem: Seventy year old patient with type 2 diabetes and an injured diabetic
foot is admitted in to the hospital.
Other medical conditions: The patient is obese and high risks of cardiovascular diseases.
Current or past nutritional status: The patient was a chain smoker and also consumed
alcohol frequently when he used to work but has abstained from alcohol now. Smokes 4-
6 cigarettes a day. The patient has mostly survived on coffee and deep fried junk foods
while at work and still do not stick to the treatment regimen set for him. Misses the
medication doses and forgets to refill the empty doses.
The type of wound: diabetic foot injury after the use of prolonged, improperly shaped
footwear. The wound is painful.
2. Evaluation of the wound including:
Wound bed status (include color/s): The wound bed was neuro-ischemic, pale and slough
with poor granulation. Gangrene in the second to the 4th digit in the left foot. The callus
present is thick. The wound is cool with absent pulses. The temperature of the patient was
102 ◦ F, BP was 124/80 mm Hg.
Wound measurements: The area of the wound is about 3.5 cm2.
Condition of surrounding skin: The patient has developed flap necrosis.
WOUND CARE PLAN
Wound care plan
1. Diagnosis of chosen individual including
Presenting problem: Seventy year old patient with type 2 diabetes and an injured diabetic
foot is admitted in to the hospital.
Other medical conditions: The patient is obese and high risks of cardiovascular diseases.
Current or past nutritional status: The patient was a chain smoker and also consumed
alcohol frequently when he used to work but has abstained from alcohol now. Smokes 4-
6 cigarettes a day. The patient has mostly survived on coffee and deep fried junk foods
while at work and still do not stick to the treatment regimen set for him. Misses the
medication doses and forgets to refill the empty doses.
The type of wound: diabetic foot injury after the use of prolonged, improperly shaped
footwear. The wound is painful.
2. Evaluation of the wound including:
Wound bed status (include color/s): The wound bed was neuro-ischemic, pale and slough
with poor granulation. Gangrene in the second to the 4th digit in the left foot. The callus
present is thick. The wound is cool with absent pulses. The temperature of the patient was
102 ◦ F, BP was 124/80 mm Hg.
Wound measurements: The area of the wound is about 3.5 cm2.
Condition of surrounding skin: The patient has developed flap necrosis.
2
WOUND CARE PLAN
Wound exudate (color, consistency, odour): The discharge from the wound is thick, fowl
smelling and yellowish in color. The bad smell of the exudates determines infections.
3. Actual or potential impacts of the wound:
Peripheral neuropathy can give rise to excessive diabetic foot pain. The patient was having a
burning sensation. A complex combination of oxidative stress, micro-vascular disease,
cytokine deficiency and disturbances in the inflammatory combines at various degrees for
producing the painful aspect of neuropathy (Matsuzaki & Upton, 2013). The foot
complications have already affected the ways of living of the patient by affecting its
mobility. The patient was having difficulties in moving and accomplishing his daily chores.
Further deterioration of the gangrene in the digits have increased the risk of digit amputation.
This has brought about depression and anxiety in the patient for being dependent for every
single things.
4. Physiology of the healing process
The wound healing in diabetes is governed by some intrinsic and extrinsic factors. The
extrinsic factors involve the stress and the repeated trauma applied to the foot that has been
rendered insensitive for the ischemia and neuropathy (Gordon et al., 2012). The basement
membrane of the capillaries and the arteries thicken in patients with diabetes that delays the
wound healing. Hyperglycemia has a delirious effect on the healing of wound by the
formation of advanced glycation end products, inducing the production of inflammatory
molecules. Tsourdi et al., (2013), have showed that the exposure to high levels of glucose is
associated with cellular morphological changes, abnormal division of the keratinocytes and
WOUND CARE PLAN
Wound exudate (color, consistency, odour): The discharge from the wound is thick, fowl
smelling and yellowish in color. The bad smell of the exudates determines infections.
3. Actual or potential impacts of the wound:
Peripheral neuropathy can give rise to excessive diabetic foot pain. The patient was having a
burning sensation. A complex combination of oxidative stress, micro-vascular disease,
cytokine deficiency and disturbances in the inflammatory combines at various degrees for
producing the painful aspect of neuropathy (Matsuzaki & Upton, 2013). The foot
complications have already affected the ways of living of the patient by affecting its
mobility. The patient was having difficulties in moving and accomplishing his daily chores.
Further deterioration of the gangrene in the digits have increased the risk of digit amputation.
This has brought about depression and anxiety in the patient for being dependent for every
single things.
4. Physiology of the healing process
The wound healing in diabetes is governed by some intrinsic and extrinsic factors. The
extrinsic factors involve the stress and the repeated trauma applied to the foot that has been
rendered insensitive for the ischemia and neuropathy (Gordon et al., 2012). The basement
membrane of the capillaries and the arteries thicken in patients with diabetes that delays the
wound healing. Hyperglycemia has a delirious effect on the healing of wound by the
formation of advanced glycation end products, inducing the production of inflammatory
molecules. Tsourdi et al., (2013), have showed that the exposure to high levels of glucose is
associated with cellular morphological changes, abnormal division of the keratinocytes and
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
3
WOUND CARE PLAN
the decreased proliferation. According to Mishra et al., (2017), decreased phagocytosis,
chemotaxis and bacterial killing and lessened production of the heat shock proteins leads
have been associated with the early stages of wound healing. Fahey et al (2012), have
demonstrated that the modified leukocyte infiltration and IL-6 involves delayed
inflammatory phase in wound healing in diabetes. Diabetic foot ulcers has been related to the
abnormal expression of the growth factors. Diabetes have been found to be linked with the
trapping of the growth factors by the macromolecules like fibrinogen, albumin that further
disrupts the healing of the wound (Tsourdi et al., 2013). The insulin degrading activity in the
wound fluid is has been found to be positively correlated with the with the HbA1c levels,
which supports the fact that glucose control plays an important role in wound healing. It is
evident from the case study that the patient is 70 years old. According to Andrews et al.,
(2015), reduced skin elasticity due to the degradation of the collagen fibers and the elastic
tissues, slower replacement of the damaged collagen fibers are the age related complications
that can hinder the wound healing.
5. Wound management plan
Interventions
Dressing Sucrose octasulfate dressing can be suitable for neuro-
ischemic wound (Edmonds et al., 2013).
Frequency of dressing
changes
How the wound is cleaned The cleaning of the wound involves:-
Hands are washed and protective clothing are donned.
The wound area is cleaned with normal saline or
WOUND CARE PLAN
the decreased proliferation. According to Mishra et al., (2017), decreased phagocytosis,
chemotaxis and bacterial killing and lessened production of the heat shock proteins leads
have been associated with the early stages of wound healing. Fahey et al (2012), have
demonstrated that the modified leukocyte infiltration and IL-6 involves delayed
inflammatory phase in wound healing in diabetes. Diabetic foot ulcers has been related to the
abnormal expression of the growth factors. Diabetes have been found to be linked with the
trapping of the growth factors by the macromolecules like fibrinogen, albumin that further
disrupts the healing of the wound (Tsourdi et al., 2013). The insulin degrading activity in the
wound fluid is has been found to be positively correlated with the with the HbA1c levels,
which supports the fact that glucose control plays an important role in wound healing. It is
evident from the case study that the patient is 70 years old. According to Andrews et al.,
(2015), reduced skin elasticity due to the degradation of the collagen fibers and the elastic
tissues, slower replacement of the damaged collagen fibers are the age related complications
that can hinder the wound healing.
5. Wound management plan
Interventions
Dressing Sucrose octasulfate dressing can be suitable for neuro-
ischemic wound (Edmonds et al., 2013).
Frequency of dressing
changes
How the wound is cleaned The cleaning of the wound involves:-
Hands are washed and protective clothing are donned.
The wound area is cleaned with normal saline or
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
4
WOUND CARE PLAN
chlorohexidine (Peters et al., 2012).
Tissue debriment- forceps, scalpels and scissors can be
used to remove the tissue debris. Forced beam of saline
solution can also be used (Andrews et al., 2015).
Infection control- Topical antimicrobial agents such as
Silver (silver containing dressing), Polyhexamethylene
biguanide (PHMB) (in the form of gel or solution), Iodine
(ointments and impregnated dressings), medical grade
honey (as ointments and impregnated dressings) (Lipsky et
al., 2016).
Moisture balance- Alginates and hydrocolloid dressings
can be used to control moisture and the debriment of the
devitalized tissues.
Advancements of the epithelial edge- The edges of the
ulcers should be debrided for removing the potential
barriers to the growth of the new epithelium.
Choosing the appropriate dressing- Sucrose octasulfate
dressing, alginate, foams.
Progress being made The wound should attain closure within 6 weeks. This can be
measured by measuring the diameter of the wound and the
exudate status.
Any changes made With the shrinkage of the wound diameter the alginate
WOUND CARE PLAN
chlorohexidine (Peters et al., 2012).
Tissue debriment- forceps, scalpels and scissors can be
used to remove the tissue debris. Forced beam of saline
solution can also be used (Andrews et al., 2015).
Infection control- Topical antimicrobial agents such as
Silver (silver containing dressing), Polyhexamethylene
biguanide (PHMB) (in the form of gel or solution), Iodine
(ointments and impregnated dressings), medical grade
honey (as ointments and impregnated dressings) (Lipsky et
al., 2016).
Moisture balance- Alginates and hydrocolloid dressings
can be used to control moisture and the debriment of the
devitalized tissues.
Advancements of the epithelial edge- The edges of the
ulcers should be debrided for removing the potential
barriers to the growth of the new epithelium.
Choosing the appropriate dressing- Sucrose octasulfate
dressing, alginate, foams.
Progress being made The wound should attain closure within 6 weeks. This can be
measured by measuring the diameter of the wound and the
exudate status.
Any changes made With the shrinkage of the wound diameter the alginate
5
WOUND CARE PLAN
dressing was changed to hydrogels for rehydrating the wound
bed. Previously Ceftazidime was used as an antibiotic, but the
medicine was having an adverse effect on the nervous system.
This lead to the shifting to Amoxicillin-Clavulanate that is a
broad spectrum antibiotic giving coverage to both
streptococcus and Staphylococcus species.
6. Health education
Patients should be well aware of his own medical status regarding the measurement of the
wound, the color of the exudates, pain or size of the wound. Patients should know whom to
contact if symptoms persists and should adhere to the medication and the cleanliness
regimen.
7. Pain management
Tricyclic agents, γ-aminobutyric acid (GABA) analogues (gabapentin or pregabalin),
serotonin–norepinephrine reuptake inhibitors (SNRIs) can be given as first line agents
followed by topical treatments and opoids (Javed et al., 2015). A topical 5% ketamine cream
can be used for painful diabetic neuropathy (Matsuzaki & Upton, 2013).
WOUND CARE PLAN
dressing was changed to hydrogels for rehydrating the wound
bed. Previously Ceftazidime was used as an antibiotic, but the
medicine was having an adverse effect on the nervous system.
This lead to the shifting to Amoxicillin-Clavulanate that is a
broad spectrum antibiotic giving coverage to both
streptococcus and Staphylococcus species.
6. Health education
Patients should be well aware of his own medical status regarding the measurement of the
wound, the color of the exudates, pain or size of the wound. Patients should know whom to
contact if symptoms persists and should adhere to the medication and the cleanliness
regimen.
7. Pain management
Tricyclic agents, γ-aminobutyric acid (GABA) analogues (gabapentin or pregabalin),
serotonin–norepinephrine reuptake inhibitors (SNRIs) can be given as first line agents
followed by topical treatments and opoids (Javed et al., 2015). A topical 5% ketamine cream
can be used for painful diabetic neuropathy (Matsuzaki & Upton, 2013).
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
6
WOUND CARE PLAN
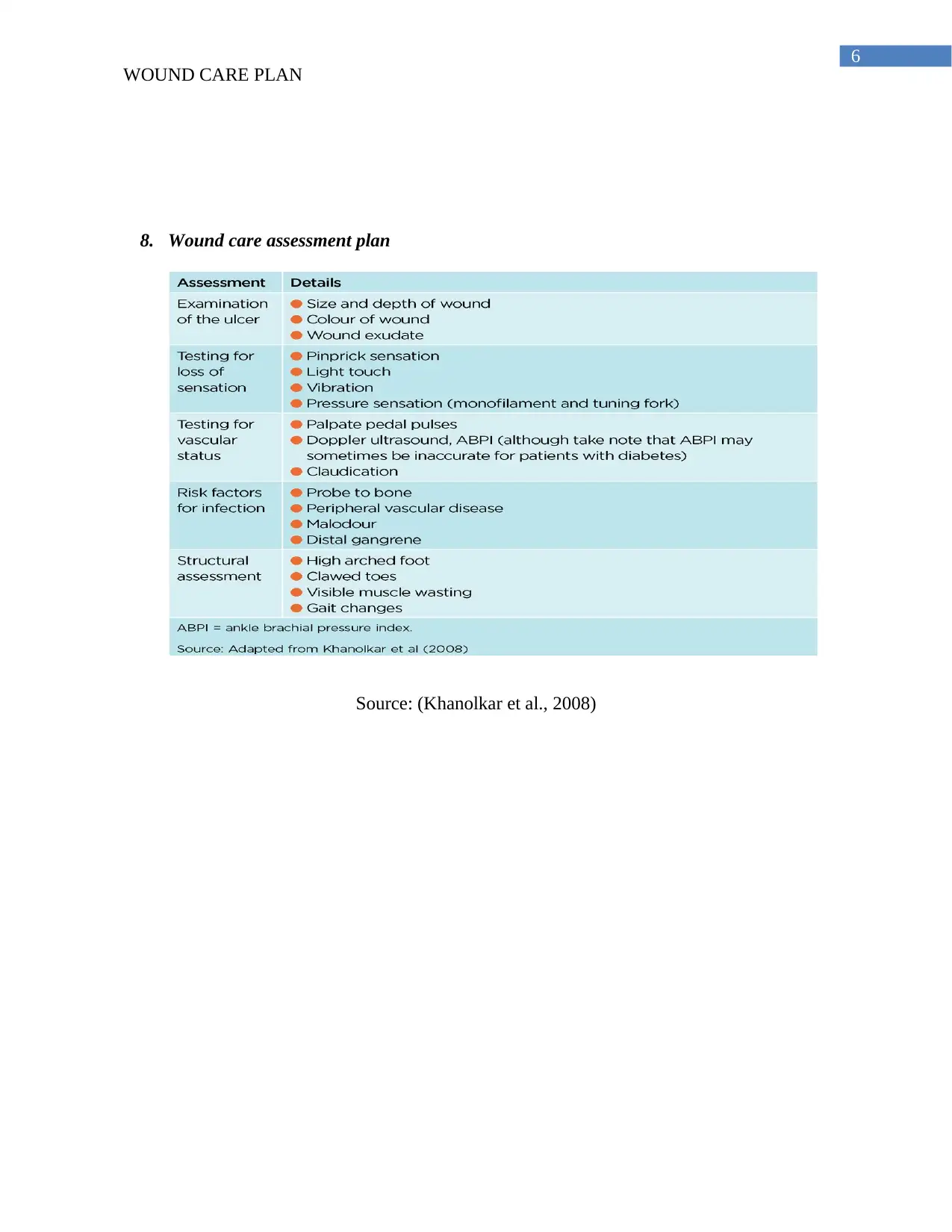
8. Wound care assessment plan
Source: (Khanolkar et al., 2008)
WOUND CARE PLAN
8. Wound care assessment plan
Source: (Khanolkar et al., 2008)
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7
WOUND CARE PLAN
References
Andrews, K. L., Houdek, M. T., & Kiemele, L. J. (2015). Wound management of chronic
diabetic foot ulcers: from the basics to regenerative medicine. Prosthetics and orthotics
international, 39(1), 29-39.
Edmonds, M., Lázaro-Martínez, J. L., Alfayate-García, J. M., Martini, J., Petit, J. M., Rayman,
G., ... & Kerihuel, J. C. (2017). Sucrose octasulfate dressing versus control dressing in
patients with neuroischaemic diabetic foot ulcers (Explorer): an international,
multicentre, double-blind, randomised, controlled trial. The Lancet Diabetes &
Endocrinology.
Fahey, T. J., Sadaty, A., Jones, W. G., Barber, A., Smoller, B., & Shires, G. T. (2014). Diabetes
impairs the late inflammatory response to wound healing. Journal of Surgical Research,
50(4), 308-313.
Gordon, K. A., Lebrun, E. A., Tomic-Canic, M., & Kirsner, R. S. (2012). The role of surgical
debridement in healing of diabetic foot ulcers. Skinmed, 10(1), 24-26.
Javed, S., Petropoulos, I. N., Alam, U., & Malik, R. A. (2015). Treatment of painful diabetic
neuropathy. Therapeutic Advances in Chronic Disease, 6(1), 15–28.
http://doi.org/10.1177/2040622314552071
Khanolkar, M. P., Bain, S. C., & Stephens, J. W. (2008). The diabetic foot. QJM: An
International Journal of Medicine, 101(9), 685-695.
WOUND CARE PLAN
References
Andrews, K. L., Houdek, M. T., & Kiemele, L. J. (2015). Wound management of chronic
diabetic foot ulcers: from the basics to regenerative medicine. Prosthetics and orthotics
international, 39(1), 29-39.
Edmonds, M., Lázaro-Martínez, J. L., Alfayate-García, J. M., Martini, J., Petit, J. M., Rayman,
G., ... & Kerihuel, J. C. (2017). Sucrose octasulfate dressing versus control dressing in
patients with neuroischaemic diabetic foot ulcers (Explorer): an international,
multicentre, double-blind, randomised, controlled trial. The Lancet Diabetes &
Endocrinology.
Fahey, T. J., Sadaty, A., Jones, W. G., Barber, A., Smoller, B., & Shires, G. T. (2014). Diabetes
impairs the late inflammatory response to wound healing. Journal of Surgical Research,
50(4), 308-313.
Gordon, K. A., Lebrun, E. A., Tomic-Canic, M., & Kirsner, R. S. (2012). The role of surgical
debridement in healing of diabetic foot ulcers. Skinmed, 10(1), 24-26.
Javed, S., Petropoulos, I. N., Alam, U., & Malik, R. A. (2015). Treatment of painful diabetic
neuropathy. Therapeutic Advances in Chronic Disease, 6(1), 15–28.
http://doi.org/10.1177/2040622314552071
Khanolkar, M. P., Bain, S. C., & Stephens, J. W. (2008). The diabetic foot. QJM: An
International Journal of Medicine, 101(9), 685-695.
8
WOUND CARE PLAN
Lipsky, B. A., Peters, E. J. G., Senneville, E., Berendt, A. R., Embil, J. M., Lavery, L. A., ... &
Jeffcoate, W. J. (2012). Expert opinion on the management of infections in the diabetic
foot. Diabetes/metabolism research and reviews, 28(S1), 163-178.
Matsuzaki, K., & Upton, D. (2013). Wound treatment and pain management: a stressful
time. International wound journal, 10(6), 638-644.
Mishra, S. C., Chhatbar, K. C., Kashikar, A., & Mehndiratta, A. (2017). Diabetic foot. BMJ, 359,
j5064.
Peters, E. J. G., Lipsky, B. A., Berendt, A. R., Embil, J. M., Lavery, L. A., Senneville, E., ... &
Jeffcoate, W. J. (2012). A systematic review of the effectiveness of interventions in the
management of infection in the diabetic foot. Diabetes/metabolism research and
reviews, 28(S1), 142-162.
Tsourdi, E., Barthel, A., Rietzsch, H., Reichel, A., & Bornstein, S. R. (2013). Current aspects in
the pathophysiology and treatment of chronic wounds in diabetes mellitus. BioMed
research international, 2013.
WOUND CARE PLAN
Lipsky, B. A., Peters, E. J. G., Senneville, E., Berendt, A. R., Embil, J. M., Lavery, L. A., ... &
Jeffcoate, W. J. (2012). Expert opinion on the management of infections in the diabetic
foot. Diabetes/metabolism research and reviews, 28(S1), 163-178.
Matsuzaki, K., & Upton, D. (2013). Wound treatment and pain management: a stressful
time. International wound journal, 10(6), 638-644.
Mishra, S. C., Chhatbar, K. C., Kashikar, A., & Mehndiratta, A. (2017). Diabetic foot. BMJ, 359,
j5064.
Peters, E. J. G., Lipsky, B. A., Berendt, A. R., Embil, J. M., Lavery, L. A., Senneville, E., ... &
Jeffcoate, W. J. (2012). A systematic review of the effectiveness of interventions in the
management of infection in the diabetic foot. Diabetes/metabolism research and
reviews, 28(S1), 142-162.
Tsourdi, E., Barthel, A., Rietzsch, H., Reichel, A., & Bornstein, S. R. (2013). Current aspects in
the pathophysiology and treatment of chronic wounds in diabetes mellitus. BioMed
research international, 2013.
⊘ This is a preview!⊘
Do you want full access?
Subscribe today to unlock all pages.

Trusted by 1+ million students worldwide
1 out of 9
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
Copyright © 2020–2026 A2Z Services. All Rights Reserved. Developed and managed by ZUCOL.





