Wound Management Plans for Different Types of Wounds
VerifiedAdded on 2023/06/08
|23
|6159
|132
AI Summary
This article provides a comprehensive guide on wound management plans for different types of wounds. It covers the holistic assessment of the patient, wound bed status, wound characteristics, expected healing process, and pain management. The article also includes case studies and investigations required for the wounds. Subject: Medicine, Course Code: MED101, College/University: Not mentioned.
Contribute Materials
Your contribution can guide someone’s learning journey. Share your
documents today.

Running head: WOUND MANAGEMENT PLANS
WOUND MANAGEMENT PLANS
Name of the Student
Name of the University
Author’s Note
WOUND MANAGEMENT PLANS
Name of the Student
Name of the University
Author’s Note
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
1WOUND MANAGEMENT PLANS
Table of Contents
A. Holistic assessment of the patient.................................................................................5
i. Medical history and examination of the patient.......................................................5
ii. The wounds..............................................................................................................6
iii. Type of wounds........................................................................................................6
iv. The cause of the wounds.........................................................................................7
v. Investigations required for the wounds....................................................................7
vi. Wound management principles...............................................................................8
B. Evaluation of the wound................................................................................................9
1. Wound bed status....................................................................................................9
2. Wound characteristics............................................................................................10
iv. Wound measurements..........................................................................................10
v. Condition of the surrounding skin..........................................................................11
vi. Wound exudates....................................................................................................11
vii. Further assessment...............................................................................................11
C. Expected healing process...........................................................................................12
i. Health factors.........................................................................................................12
ii. Timeline.................................................................................................................13
D. Health education for the patient regarding the wound................................................14
i. Nutrition..................................................................................................................14
Table of Contents
A. Holistic assessment of the patient.................................................................................5
i. Medical history and examination of the patient.......................................................5
ii. The wounds..............................................................................................................6
iii. Type of wounds........................................................................................................6
iv. The cause of the wounds.........................................................................................7
v. Investigations required for the wounds....................................................................7
vi. Wound management principles...............................................................................8
B. Evaluation of the wound................................................................................................9
1. Wound bed status....................................................................................................9
2. Wound characteristics............................................................................................10
iv. Wound measurements..........................................................................................10
v. Condition of the surrounding skin..........................................................................11
vi. Wound exudates....................................................................................................11
vii. Further assessment...............................................................................................11
C. Expected healing process...........................................................................................12
i. Health factors.........................................................................................................12
ii. Timeline.................................................................................................................13
D. Health education for the patient regarding the wound................................................14
i. Nutrition..................................................................................................................14
2WOUND MANAGEMENT PLANS
ii. Mobility...................................................................................................................14
iii. Preventative measures.......................................................................................14
E. Wound management plan...........................................................................................15
1. The diabetic foot ulcer..............................................................................................15
i. Moist wound healing...............................................................................................15
ii. Risk assessment......................................................................................................15
iii. Wound cleansing.....................................................................................................15
iv. Pressure support & relieving device.......................................................................15
v. Dressing product and primary dressing................................................................15
vi. Secondary dressing................................................................................................16
2. The arterial ulcer......................................................................................................16
i. Moist wound healing.............................................................................................16
ii. Risk assessment...................................................................................................16
iii. Wound cleansing.....................................................................................................16
iv. Pressure support & relieving device.......................................................................16
v. Dressing product and primary dressing................................................................17
vi. Secondary dressing................................................................................................17
vii. Pain management..............................................................................................17
3. The stage 3 pressure ulcer......................................................................................17
i. Moist wound healing.............................................................................................17
ii. Risk assessment...................................................................................................17
ii. Mobility...................................................................................................................14
iii. Preventative measures.......................................................................................14
E. Wound management plan...........................................................................................15
1. The diabetic foot ulcer..............................................................................................15
i. Moist wound healing...............................................................................................15
ii. Risk assessment......................................................................................................15
iii. Wound cleansing.....................................................................................................15
iv. Pressure support & relieving device.......................................................................15
v. Dressing product and primary dressing................................................................15
vi. Secondary dressing................................................................................................16
2. The arterial ulcer......................................................................................................16
i. Moist wound healing.............................................................................................16
ii. Risk assessment...................................................................................................16
iii. Wound cleansing.....................................................................................................16
iv. Pressure support & relieving device.......................................................................16
v. Dressing product and primary dressing................................................................17
vi. Secondary dressing................................................................................................17
vii. Pain management..............................................................................................17
3. The stage 3 pressure ulcer......................................................................................17
i. Moist wound healing.............................................................................................17
ii. Risk assessment...................................................................................................17
3WOUND MANAGEMENT PLANS
iii. Wound cleansing.....................................................................................................17
iv. Pressure support & relieving device...................................................................17
v. Dressing product and primary dressing................................................................18
vi. Secondary dressing............................................................................................18
vii. Pain management..............................................................................................18
4. The malignant groin wound......................................................................................18
i. Moist wound healing.............................................................................................18
ii. Risk assessment...................................................................................................18
iii. Wound cleansing................................................................................................18
iv. Pressure support & relieving device...................................................................19
v. Dressing product and primary dressing................................................................19
vi. Secondary dressing............................................................................................19
vii. Pain Management..............................................................................................19
5. The venous ulcer......................................................................................................19
i. Moist wound healing.............................................................................................19
ii. Risk assessment...................................................................................................19
iii. Wound cleansing................................................................................................19
iv. Pressure support & relieving device...................................................................20
v. Dressing product and primary dressing.............................................................20
vi. Secondary dressing............................................................................................20
vii. Pain management..............................................................................................20
iii. Wound cleansing.....................................................................................................17
iv. Pressure support & relieving device...................................................................17
v. Dressing product and primary dressing................................................................18
vi. Secondary dressing............................................................................................18
vii. Pain management..............................................................................................18
4. The malignant groin wound......................................................................................18
i. Moist wound healing.............................................................................................18
ii. Risk assessment...................................................................................................18
iii. Wound cleansing................................................................................................18
iv. Pressure support & relieving device...................................................................19
v. Dressing product and primary dressing................................................................19
vi. Secondary dressing............................................................................................19
vii. Pain Management..............................................................................................19
5. The venous ulcer......................................................................................................19
i. Moist wound healing.............................................................................................19
ii. Risk assessment...................................................................................................19
iii. Wound cleansing................................................................................................19
iv. Pressure support & relieving device...................................................................20
v. Dressing product and primary dressing.............................................................20
vi. Secondary dressing............................................................................................20
vii. Pain management..............................................................................................20
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
4WOUND MANAGEMENT PLANS
F. Pain management of the wound..................................................................................20
i. Medication..............................................................................................................20
ii. Frequency and dose..............................................................................................20
iii. Justification for the medication................................................................................21
G. Conclusion..................................................................................................................21
H. References..................................................................................................................22
F. Pain management of the wound..................................................................................20
i. Medication..............................................................................................................20
ii. Frequency and dose..............................................................................................20
iii. Justification for the medication................................................................................21
G. Conclusion..................................................................................................................21
H. References..................................................................................................................22
5WOUND MANAGEMENT PLANS
A. Holistic assessment of the patient
i. Medical history and examination of the patient
Case Study 1:
The first case study is on Mr. Will Jackson, a 77 year old who had been
diagnosed with rectal cancer five years ago. He has a clinical history of ischemic heart
disease (IHD) which attributed to his coronary artery bypass grafting (CABG) two years
ago. He also has Chronic Obstructive Pulmonary Disease (COPD) along with Gastro-
oesophageal reflux disease (GORD) and a history of alcohol abuse. He also suffers
from postural hypotension and takes insulin to control his type 2 diabetes mellitus. He
also suffers from intermittent confusion and mild lack of cognitive integrity at times. He
lives alone in a retirement village since his wife passed away a year ago. His urine
output is incontinent and requires pad in situ. He can walk a few steps for a short
distance with help however requires wheelchair assistance for longer distances.
Mr. Jackson has been admitted with pain, shortness of breath and for
management of his wounds. Prior to his admission, he had struck his head during a fall
at home and had a substantially large bruise over his face. The CT scan of Mr.
Jackson’s head did not reveal any significant damage; however the doctor stopped his
warfarin dose for a week due to this massive bruise as warfarin was being used to
reduce blood clots thereby aiding his CABG.
Case Study 2:
The second case study is on an 85 year old Mrs. Miriam Gold who has been
admitted with fluids overload problem and has pneumonia along with metastatic cervical
cancer. Mrs. Gold has a rectovaginal fistula due to her progressed cancer and
radiotherapy. Additionally, the patient has a long standing venous ulcer that is not
healing. Mrs. Gold has a medical history of Chronic Obstructive Pulmonary Disease
(COPD) and Gastro-oesophageal reflux disease (GORD) along with presence of
coronary artery bypass graft (CABG). Her mobility is restricted to resting in bed and is
cognitively drowsy and vague. She is on a semi liquid diet, comprised of mild thick fluids
and is incontinent, requiring pad in situ.
A. Holistic assessment of the patient
i. Medical history and examination of the patient
Case Study 1:
The first case study is on Mr. Will Jackson, a 77 year old who had been
diagnosed with rectal cancer five years ago. He has a clinical history of ischemic heart
disease (IHD) which attributed to his coronary artery bypass grafting (CABG) two years
ago. He also has Chronic Obstructive Pulmonary Disease (COPD) along with Gastro-
oesophageal reflux disease (GORD) and a history of alcohol abuse. He also suffers
from postural hypotension and takes insulin to control his type 2 diabetes mellitus. He
also suffers from intermittent confusion and mild lack of cognitive integrity at times. He
lives alone in a retirement village since his wife passed away a year ago. His urine
output is incontinent and requires pad in situ. He can walk a few steps for a short
distance with help however requires wheelchair assistance for longer distances.
Mr. Jackson has been admitted with pain, shortness of breath and for
management of his wounds. Prior to his admission, he had struck his head during a fall
at home and had a substantially large bruise over his face. The CT scan of Mr.
Jackson’s head did not reveal any significant damage; however the doctor stopped his
warfarin dose for a week due to this massive bruise as warfarin was being used to
reduce blood clots thereby aiding his CABG.
Case Study 2:
The second case study is on an 85 year old Mrs. Miriam Gold who has been
admitted with fluids overload problem and has pneumonia along with metastatic cervical
cancer. Mrs. Gold has a rectovaginal fistula due to her progressed cancer and
radiotherapy. Additionally, the patient has a long standing venous ulcer that is not
healing. Mrs. Gold has a medical history of Chronic Obstructive Pulmonary Disease
(COPD) and Gastro-oesophageal reflux disease (GORD) along with presence of
coronary artery bypass graft (CABG). Her mobility is restricted to resting in bed and is
cognitively drowsy and vague. She is on a semi liquid diet, comprised of mild thick fluids
and is incontinent, requiring pad in situ.
6WOUND MANAGEMENT PLANS
The patient has been admitted for palliative care treatment as the patient is in a
lot of pain due to her malignant wound on her left groin and her family comprised of
husband and children are not coping well with her health issues.
ii. The wounds
Case Study 1:
Mr. Jackson was admitted with three wounds; however he now has four wounds
as follows;
1. One foot ulcer behind his left toe
2. One ulcer on his right lower leg
3. One ulcer on his sacrum bone
4. Bruise on left arm was after admittance to the ward.
Case Study 2:
Mrs Miriam Gold has two wound which require proper management.
1. One wound on the groin
2. One ulcer
iii. Type of wounds
Case Study 1:
The different wounds on Mr. Jackson are categorised below.
1. The foot ulcer behind his left toe is a diabetic ulcer.
2. The ulcer on his right lower leg is an arterial ulcer.
3. The ulcer on his sacrum bone is a stage 3 pressure ulcer.
4. The bruise on the patient’s left arm is a second degree burn bruise.
Case Study 2:
The two wounds on Mrs. Gold are categorised below
1. The wound on the left groin is malignant.
2. The ulcer is a venous ulcer.
The patient has been admitted for palliative care treatment as the patient is in a
lot of pain due to her malignant wound on her left groin and her family comprised of
husband and children are not coping well with her health issues.
ii. The wounds
Case Study 1:
Mr. Jackson was admitted with three wounds; however he now has four wounds
as follows;
1. One foot ulcer behind his left toe
2. One ulcer on his right lower leg
3. One ulcer on his sacrum bone
4. Bruise on left arm was after admittance to the ward.
Case Study 2:
Mrs Miriam Gold has two wound which require proper management.
1. One wound on the groin
2. One ulcer
iii. Type of wounds
Case Study 1:
The different wounds on Mr. Jackson are categorised below.
1. The foot ulcer behind his left toe is a diabetic ulcer.
2. The ulcer on his right lower leg is an arterial ulcer.
3. The ulcer on his sacrum bone is a stage 3 pressure ulcer.
4. The bruise on the patient’s left arm is a second degree burn bruise.
Case Study 2:
The two wounds on Mrs. Gold are categorised below
1. The wound on the left groin is malignant.
2. The ulcer is a venous ulcer.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
7WOUND MANAGEMENT PLANS
iv. The cause of the wounds
Case Study 1:
1. The patient’s diabetic foot ulcer along with the arterial ulcer is both due to
his hyperglycaemic condition as he is a patient diagnosed with type 2 diabetes
mellitus.
2. The arterial ulcer has formed due damage to the arteries caused by
reduced blood flow or lack of blood flow to the tissue.
3. The stage 3 pressure ulcer on his sacrum bone has developed due to
unrelieved pressure on the underlying tissue from the strain from the sacrum bone
because of lying for long intervals in a fixed supine position.
4. Mr. Jackson sustained a second degree burn bruise on his left arm on the
3rd day of hospital stay due to accidental hot coffee spillage.
Case Study 2:
The two wounds of Mrs Gold require attention.
1. The malignant wound on the left groin is a rectovaginal fistula due to her
progressed cervical cancer and radiotherapy.
2. The venous ulcer has developed due to venous valves not functioning
properly.
v. Investigations required for the wounds
Case Study 1:
Mr. Jackson’s blood glucose level needs to be investigated at the earliest to
determine the effect of diabetes on the wounds.
An USG must also be performed on the surrounding tissues of the diabetic foot
ulcer and arterial ulcer along with the stage 3 pressure ulcer to determine the
extent of the ulcers and health of the nearby tissues. pH of the wounds must also
be checked to assess the infections properly.
Wound swabs of the diabetic foot ulcer and arterial ulcer microbial culture
examination are also recommended.
Haemoglobin count, white cell count and platelet count assessment is also vital
to diagnose infections and expected healing time.
iv. The cause of the wounds
Case Study 1:
1. The patient’s diabetic foot ulcer along with the arterial ulcer is both due to
his hyperglycaemic condition as he is a patient diagnosed with type 2 diabetes
mellitus.
2. The arterial ulcer has formed due damage to the arteries caused by
reduced blood flow or lack of blood flow to the tissue.
3. The stage 3 pressure ulcer on his sacrum bone has developed due to
unrelieved pressure on the underlying tissue from the strain from the sacrum bone
because of lying for long intervals in a fixed supine position.
4. Mr. Jackson sustained a second degree burn bruise on his left arm on the
3rd day of hospital stay due to accidental hot coffee spillage.
Case Study 2:
The two wounds of Mrs Gold require attention.
1. The malignant wound on the left groin is a rectovaginal fistula due to her
progressed cervical cancer and radiotherapy.
2. The venous ulcer has developed due to venous valves not functioning
properly.
v. Investigations required for the wounds
Case Study 1:
Mr. Jackson’s blood glucose level needs to be investigated at the earliest to
determine the effect of diabetes on the wounds.
An USG must also be performed on the surrounding tissues of the diabetic foot
ulcer and arterial ulcer along with the stage 3 pressure ulcer to determine the
extent of the ulcers and health of the nearby tissues. pH of the wounds must also
be checked to assess the infections properly.
Wound swabs of the diabetic foot ulcer and arterial ulcer microbial culture
examination are also recommended.
Haemoglobin count, white cell count and platelet count assessment is also vital
to diagnose infections and expected healing time.
8WOUND MANAGEMENT PLANS
The pH of the malignant wound must be assessed to determine the infection and
administer medicines accordingly.
Case Study 2:
Wound swabs of the venous ulcer and malignant groin wound to detect the
specific microbes infecting the wounds or that microbe specific treatment can be
advised.
White cell count, haemoglobin count, and platelet count is required to analyse the
level of infection and assess the healing time.
A biopsy of her groin malignant wound must be done to assess the status of her
cervical cancer.
The pH of the malignant wound must be assessed to determine the infection and
administer medicines accordingly.
vi. Wound management principles
Case Study 1:
The basic wound management principle for diabetic foot ulcer would encompass
debridement of the ulcer, proper therapeutic management of infection, revascularization
measures along with off-loading of the ulcer.
The management of the arterial ulcer on his right lower leg must involve
treatment of the infection while enhancing autolytic debridement along with controlled
exudation of pus, pain reduction and maintenance of a moist sterile healing
environment.
The treatment for pressure ulcer on the patient’s sacrum bone needs
involvement of infection management along with removal of the necrotic tissue, and
proper maintenance of moist environment for rapid wound healing. Repositioning of the
patient is the key to treat pressure ulcers (Moore & Cowman, 2015).
The wound management principle for the second degree burn would include
loose wrapping of a hydrogel based dressing over the bruise which will allow aeration
for fastens the healing process along with application of antibiotic ointment to prevent
infection.
The pH of the malignant wound must be assessed to determine the infection and
administer medicines accordingly.
Case Study 2:
Wound swabs of the venous ulcer and malignant groin wound to detect the
specific microbes infecting the wounds or that microbe specific treatment can be
advised.
White cell count, haemoglobin count, and platelet count is required to analyse the
level of infection and assess the healing time.
A biopsy of her groin malignant wound must be done to assess the status of her
cervical cancer.
The pH of the malignant wound must be assessed to determine the infection and
administer medicines accordingly.
vi. Wound management principles
Case Study 1:
The basic wound management principle for diabetic foot ulcer would encompass
debridement of the ulcer, proper therapeutic management of infection, revascularization
measures along with off-loading of the ulcer.
The management of the arterial ulcer on his right lower leg must involve
treatment of the infection while enhancing autolytic debridement along with controlled
exudation of pus, pain reduction and maintenance of a moist sterile healing
environment.
The treatment for pressure ulcer on the patient’s sacrum bone needs
involvement of infection management along with removal of the necrotic tissue, and
proper maintenance of moist environment for rapid wound healing. Repositioning of the
patient is the key to treat pressure ulcers (Moore & Cowman, 2015).
The wound management principle for the second degree burn would include
loose wrapping of a hydrogel based dressing over the bruise which will allow aeration
for fastens the healing process along with application of antibiotic ointment to prevent
infection.
9WOUND MANAGEMENT PLANS
Case Study 2:
Gentle exudation of pus of the malignant wound on the left groin needs to be
performed after warm compression which would also relieve some pain. Therapeutic
treatment of the infection with warm compression with hydrogen borate is required to
treat the malignant wound followed by proper dressing of the wound.
The venous ulcer requires gentle debridement followed by proper management
of infection along with accurate maintenance of moisture to assure that the fresh healthy
tissue does not dry out.
B. Evaluation of the wound
1. Wound bed status
Case Study 1:
i. The wound bed of the diabetic foot ulcer behind the left toe of the patient
contains yellow slough tissue with bone visible at the base and almost no visible
pink healthy tissue and looks like an undermined ulcer.
ii. The wound bed of the arterial ulcer on his right lower leg contains unhealthy
granulation with yellow slough tissue which looks like it will bleed on contact and
looks like sloping edge ulcer and is infected.
iii. The wound bed of the stage 3 pressure ulcer on the sacrum bone on the
patient’s back looks infected with excessive unhealthy granulation and is dark red
in colour and looks like a punched out ulcer. The wound base of the ulcer
consists of 70% slough tissue and 30% granulation tissue.
Case Study 2:
i. The bed of the malignant wound contains pus and the exudate is yellowish white
along with a bit of blackish necrotic tissue. No pink or healthy tissue is visible.
ii. The wound bed of the venous ulcer is of unhealthy granulation with yellow slough
tissue
Case Study 2:
Gentle exudation of pus of the malignant wound on the left groin needs to be
performed after warm compression which would also relieve some pain. Therapeutic
treatment of the infection with warm compression with hydrogen borate is required to
treat the malignant wound followed by proper dressing of the wound.
The venous ulcer requires gentle debridement followed by proper management
of infection along with accurate maintenance of moisture to assure that the fresh healthy
tissue does not dry out.
B. Evaluation of the wound
1. Wound bed status
Case Study 1:
i. The wound bed of the diabetic foot ulcer behind the left toe of the patient
contains yellow slough tissue with bone visible at the base and almost no visible
pink healthy tissue and looks like an undermined ulcer.
ii. The wound bed of the arterial ulcer on his right lower leg contains unhealthy
granulation with yellow slough tissue which looks like it will bleed on contact and
looks like sloping edge ulcer and is infected.
iii. The wound bed of the stage 3 pressure ulcer on the sacrum bone on the
patient’s back looks infected with excessive unhealthy granulation and is dark red
in colour and looks like a punched out ulcer. The wound base of the ulcer
consists of 70% slough tissue and 30% granulation tissue.
Case Study 2:
i. The bed of the malignant wound contains pus and the exudate is yellowish white
along with a bit of blackish necrotic tissue. No pink or healthy tissue is visible.
ii. The wound bed of the venous ulcer is of unhealthy granulation with yellow slough
tissue
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
10WOUND MANAGEMENT PLANS
2. Wound characteristics
Case Study 1:
i. The wound characteristics of the foot ulcer behind the left toe of the patient is a
diabetic ulcer, undermined, unhealthy granulation with yellow slough tissue, with
the bone visible at the base and almost no visible pink healthy tissue.
ii. The wound characteristics of the ulcer on the right lower leg of the patient is an
arterial sloping edge ulcer with yellow slough tissue and unhealthy granulation
with presence of infection.
iii. The wound characteristics of the ulcer on the sacrum bone is a stage 3 pressure
punched out ulcer on the patient’s back which is very painful and looks infected
with excessive unhealthy granulation and is dark red in colour.
Case Study 2:
i. The malignant wound on the left groin is exudating pus and is giving out
extremely strong odour. It is causing the patient extreme pain and has also
developed a sinus tract which is a narrow passageway under the skin that may
extend in any direction, through the soft tissue, therefore resulting in a dead gap
with high probability for abscess formation. The progress of the wound causes a
burning sensation in the groin and peri-anal area which gets aggravated due to
bowel incontinence & discharge from her cervical cancer.
ii. The venous ulcer is a long standing wound with reduced healing probably due to
radiotherapy and her old age.
iv. Wound measurements
For better assessment of the wounds, the proper area and depth of the wounds
need to be measured. Various techniques and protocols are present for accurate wound
measurement namely the ruler method, water fill technique, the volumetric method,
Acetate Tracing Method, 3D scanner method; however studies have shown that 3D
scanner protocol gives the most accurate result, consistently. The measurements taken
by the 3D scanner are 11% better compared to the water fill technique, 75% better than
the ruler method, 41% better than the acetate tracing method and 52% better in
comparison to other 2D planimetric techniques in average. Consistent accurate
2. Wound characteristics
Case Study 1:
i. The wound characteristics of the foot ulcer behind the left toe of the patient is a
diabetic ulcer, undermined, unhealthy granulation with yellow slough tissue, with
the bone visible at the base and almost no visible pink healthy tissue.
ii. The wound characteristics of the ulcer on the right lower leg of the patient is an
arterial sloping edge ulcer with yellow slough tissue and unhealthy granulation
with presence of infection.
iii. The wound characteristics of the ulcer on the sacrum bone is a stage 3 pressure
punched out ulcer on the patient’s back which is very painful and looks infected
with excessive unhealthy granulation and is dark red in colour.
Case Study 2:
i. The malignant wound on the left groin is exudating pus and is giving out
extremely strong odour. It is causing the patient extreme pain and has also
developed a sinus tract which is a narrow passageway under the skin that may
extend in any direction, through the soft tissue, therefore resulting in a dead gap
with high probability for abscess formation. The progress of the wound causes a
burning sensation in the groin and peri-anal area which gets aggravated due to
bowel incontinence & discharge from her cervical cancer.
ii. The venous ulcer is a long standing wound with reduced healing probably due to
radiotherapy and her old age.
iv. Wound measurements
For better assessment of the wounds, the proper area and depth of the wounds
need to be measured. Various techniques and protocols are present for accurate wound
measurement namely the ruler method, water fill technique, the volumetric method,
Acetate Tracing Method, 3D scanner method; however studies have shown that 3D
scanner protocol gives the most accurate result, consistently. The measurements taken
by the 3D scanner are 11% better compared to the water fill technique, 75% better than
the ruler method, 41% better than the acetate tracing method and 52% better in
comparison to other 2D planimetric techniques in average. Consistent accurate
11WOUND MANAGEMENT PLANS
measurements were observed with the 3D scanner and such is required to measure
wounds precisely and treat the wound accordingly.
v. Condition of the surrounding skin
Case Study 1
1. The periwound skin surrounding the diabetic foot ulcer behind the left toe is swollen,
whitish yellow in color with no visible pink healthy tissue and contains pus and slough
tissue.
2. The periwound around the arterial ulcer on his right lower is dry and scaly and pinkish
in colour.
3. The stage 3 pressure ulcer’s periwound is extremely inflamed and pink in colour.
Case Study 2:
1. The periwound region of the patient’s malignant wound on the left groin is pink in
colour and inflamed.
2. The periwound of the venous ulcer is yellowish in color with no visible pink healthy
tissue
vi. Wound exudates
Case Study 1:
1. The diabetic foot ulcer behind the left toe has seropurulent wound exudate.
2. The arterial ulcer on the right lower leg has serous wound drainage.
3. The stage 3 pressure ulcer on the sacrum bone has serosanguineous exudates.
Case Study 2:
1. The malignant wound on the left groin is exudating pus and is giving out strong foul
odour.
2. The venous ulcer has no visible exudate.
vii. Further assessment
Case Study 1:
measurements were observed with the 3D scanner and such is required to measure
wounds precisely and treat the wound accordingly.
v. Condition of the surrounding skin
Case Study 1
1. The periwound skin surrounding the diabetic foot ulcer behind the left toe is swollen,
whitish yellow in color with no visible pink healthy tissue and contains pus and slough
tissue.
2. The periwound around the arterial ulcer on his right lower is dry and scaly and pinkish
in colour.
3. The stage 3 pressure ulcer’s periwound is extremely inflamed and pink in colour.
Case Study 2:
1. The periwound region of the patient’s malignant wound on the left groin is pink in
colour and inflamed.
2. The periwound of the venous ulcer is yellowish in color with no visible pink healthy
tissue
vi. Wound exudates
Case Study 1:
1. The diabetic foot ulcer behind the left toe has seropurulent wound exudate.
2. The arterial ulcer on the right lower leg has serous wound drainage.
3. The stage 3 pressure ulcer on the sacrum bone has serosanguineous exudates.
Case Study 2:
1. The malignant wound on the left groin is exudating pus and is giving out strong foul
odour.
2. The venous ulcer has no visible exudate.
vii. Further assessment
Case Study 1:
12WOUND MANAGEMENT PLANS
Besides measuring and characterising the wounds of Mr. Jackson, his blood
glucose level also needs to be investigated at the earliest to determine the effect of
diabetes on the wounds (Wang et al., 2016). Hyperglycemia obstructs the curative
process therefore leading to delayed healing. An ultrasonography could also be
performed on the surrounding tissues of the diabetic foot ulcer and arterial ulcer along
with the stage 3 pressure ulcer to determine the extent of the wound beneath the upper
tissue layers and health of the nearby tissues. If a lot of dead, necrotic or infected
tissues are found, then debridement is recommended to remove the wasted tissue and
allowing the healthy tissues to heal faster. Wound swabs of the diabetic foot ulcer and
arterial ulcer microbial culture examination are also recommended to assess microbial
infections (Rondas et al., 2015). Haemoglobin count, white cell count and platelet count
assessment is also vital to diagnose infections and judge the expected healing time.
The pH of wounds must also be assessed to have a holistic approach during wound
management.
Case Study 2:
A blood glucose test is recommended to assess the delayed healing of the
venous wound. Wound swabs of both the malignant and venous wound are required to
assess the microbial infection and the exact nature of infection. Biopsy of the malignant
wound needs to be performed also along with a pH assay to accurately evaluate the
condition of the wound.
C. Expected healing process
i. Health factors
Case Study 1:
The patient Mr. Jackson is a hyperglycemic with a clinical history of ischemic
heart disease (IHD) which attributed to his coronary artery bypass grafting (CABG) two
years ago and was also diagnosed with rectal cancer five years ago. He also has
Chronic Obstructive Pulmonary Disease (COPD) along with Gastro-oesophageal reflux
disease (GORD) and a history of alcohol abuse. He also suffers from postural
hypotension and takes insulin to control his type 2 diabetes mellitus. He also suffers
Besides measuring and characterising the wounds of Mr. Jackson, his blood
glucose level also needs to be investigated at the earliest to determine the effect of
diabetes on the wounds (Wang et al., 2016). Hyperglycemia obstructs the curative
process therefore leading to delayed healing. An ultrasonography could also be
performed on the surrounding tissues of the diabetic foot ulcer and arterial ulcer along
with the stage 3 pressure ulcer to determine the extent of the wound beneath the upper
tissue layers and health of the nearby tissues. If a lot of dead, necrotic or infected
tissues are found, then debridement is recommended to remove the wasted tissue and
allowing the healthy tissues to heal faster. Wound swabs of the diabetic foot ulcer and
arterial ulcer microbial culture examination are also recommended to assess microbial
infections (Rondas et al., 2015). Haemoglobin count, white cell count and platelet count
assessment is also vital to diagnose infections and judge the expected healing time.
The pH of wounds must also be assessed to have a holistic approach during wound
management.
Case Study 2:
A blood glucose test is recommended to assess the delayed healing of the
venous wound. Wound swabs of both the malignant and venous wound are required to
assess the microbial infection and the exact nature of infection. Biopsy of the malignant
wound needs to be performed also along with a pH assay to accurately evaluate the
condition of the wound.
C. Expected healing process
i. Health factors
Case Study 1:
The patient Mr. Jackson is a hyperglycemic with a clinical history of ischemic
heart disease (IHD) which attributed to his coronary artery bypass grafting (CABG) two
years ago and was also diagnosed with rectal cancer five years ago. He also has
Chronic Obstructive Pulmonary Disease (COPD) along with Gastro-oesophageal reflux
disease (GORD) and a history of alcohol abuse. He also suffers from postural
hypotension and takes insulin to control his type 2 diabetes mellitus. He also suffers
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
13WOUND MANAGEMENT PLANS
from intermittent confusion and mild lack of cognitive integrity at times. Mr. Jackson’s
diet is also poor and for the last 2 weeks he has reduced his oral intake.
Case Study 2:
Mrs Gold has renal issues which required regular dialysis, attributing to the fluid
overload problem. She is also suffering from pneumonia along with metastatic cervical
cancer. Mrs. Gold has a rectovaginal fistula due to her progressed cancer and
radiotherapy. She is often vague and is drowsy due to old age and medication. Her
mobility is restricted to resting in bed and is on a semi liquid diet, comprised of mild thick
fluids and her urine output is incontinent and requires pad in situ.
ii. Timeline
Case Study 1:
The timeline for wound healing for Mr. Jackson is tentatively prolonged due to his
hyperglycaemic condition along with cardiac and pulmonary diseases added with
hypotension. Hyperglycemia leads to excess glucose build up in the blood vessels due
to lack or resistance to the insulin hormone leading to poor circulation along with
preventing the nutrients and the oxygen from vitalizing the cells and increases
inflammation. Hyperglycemia delays healing and restricts the immune system from
functioning properly therefore increases the chance of the wounds getting infected
(Federman et al., 2016). Peripheral neuropathy which causes reduced sensation is also
attributed to hyperglygemia which decrease the pain developed from wound therefore
making the patient not understand the actual extent of harm and wound progress.
Case Study 2:
Radiotherapy to treat her metastatic cervical cancer has lead to the delayed
healing status of Mrs. Gold. The radiation received has an adverse impact on the
reconstitution and re-epithelialization of the wounded tissue therefore delaying the
healing progress (Jacobson et al., 2017). This radiotherapy along with old age delays
healing which in turn opened opportunity for infections to grow on the wounds, hindering
the repair process even further. Antibiotic resistance might have also contributed to
delayed healing process.
from intermittent confusion and mild lack of cognitive integrity at times. Mr. Jackson’s
diet is also poor and for the last 2 weeks he has reduced his oral intake.
Case Study 2:
Mrs Gold has renal issues which required regular dialysis, attributing to the fluid
overload problem. She is also suffering from pneumonia along with metastatic cervical
cancer. Mrs. Gold has a rectovaginal fistula due to her progressed cancer and
radiotherapy. She is often vague and is drowsy due to old age and medication. Her
mobility is restricted to resting in bed and is on a semi liquid diet, comprised of mild thick
fluids and her urine output is incontinent and requires pad in situ.
ii. Timeline
Case Study 1:
The timeline for wound healing for Mr. Jackson is tentatively prolonged due to his
hyperglycaemic condition along with cardiac and pulmonary diseases added with
hypotension. Hyperglycemia leads to excess glucose build up in the blood vessels due
to lack or resistance to the insulin hormone leading to poor circulation along with
preventing the nutrients and the oxygen from vitalizing the cells and increases
inflammation. Hyperglycemia delays healing and restricts the immune system from
functioning properly therefore increases the chance of the wounds getting infected
(Federman et al., 2016). Peripheral neuropathy which causes reduced sensation is also
attributed to hyperglygemia which decrease the pain developed from wound therefore
making the patient not understand the actual extent of harm and wound progress.
Case Study 2:
Radiotherapy to treat her metastatic cervical cancer has lead to the delayed
healing status of Mrs. Gold. The radiation received has an adverse impact on the
reconstitution and re-epithelialization of the wounded tissue therefore delaying the
healing progress (Jacobson et al., 2017). This radiotherapy along with old age delays
healing which in turn opened opportunity for infections to grow on the wounds, hindering
the repair process even further. Antibiotic resistance might have also contributed to
delayed healing process.
14WOUND MANAGEMENT PLANS
D. Health education for the patient regarding the wound
i. Nutrition
A balanced diet directly influences the blood sugar level thus maintenance of a
proper nutritional diet is the key factor in wound recovery. Regular monitoring and
proper maintenance of blood glucose level with accuracy and consistency would help
the wounds heal quickly (Quain & Khardori, 2015). Processed carbohydrates, fast
foods, sugars, soft drinks which the patient is very fond of must be restricted to maintain
the blood glucose level whereas consumption of fruits, legumes and vegetables with
high fibre and high levels of zinc, vitamin C and protein must be promoted as they
enhance the wound healing process.
Mrs Gold is on a semi solid, liquid based diet therefore all the vital supplements
consisting of minerals, vitamins must be added to the food mixture to ensure the
required nourishment (Barchitta et al., 2019).
ii. Mobility
Mr. Jackson can walk a few steps for a short distance with help; however
requires wheelchair assistance for longer distance. As exercise improves insulin
sensitivity and increases blood circulation, it promotes sugar entering the cells thereby
increasing the efficiency of the cell, thus enhancing the healing process. Therefore,
guided physical activity along with physiotherapy must be prescribed for Mr. Jackson.
Mrs. Gold on the other hand is restricted to bed as she requires complete bed
rest. Physiotherapy can be recommended for her to ensure better circulation and blood
flow, thereby reducing pain and might hasten the healing of wounds.
iii. Preventative measures
Case Study 1:
As the healing process is delayed, extra precaution must be taken to stop further
infection of the open wounds. Additionally the patient’s urine output is incontinent and
requires pad in situ. This heightens the chances of microbial infections of the wound, if
care is not taken and urine touches the wounds.
Case Study 2:
D. Health education for the patient regarding the wound
i. Nutrition
A balanced diet directly influences the blood sugar level thus maintenance of a
proper nutritional diet is the key factor in wound recovery. Regular monitoring and
proper maintenance of blood glucose level with accuracy and consistency would help
the wounds heal quickly (Quain & Khardori, 2015). Processed carbohydrates, fast
foods, sugars, soft drinks which the patient is very fond of must be restricted to maintain
the blood glucose level whereas consumption of fruits, legumes and vegetables with
high fibre and high levels of zinc, vitamin C and protein must be promoted as they
enhance the wound healing process.
Mrs Gold is on a semi solid, liquid based diet therefore all the vital supplements
consisting of minerals, vitamins must be added to the food mixture to ensure the
required nourishment (Barchitta et al., 2019).
ii. Mobility
Mr. Jackson can walk a few steps for a short distance with help; however
requires wheelchair assistance for longer distance. As exercise improves insulin
sensitivity and increases blood circulation, it promotes sugar entering the cells thereby
increasing the efficiency of the cell, thus enhancing the healing process. Therefore,
guided physical activity along with physiotherapy must be prescribed for Mr. Jackson.
Mrs. Gold on the other hand is restricted to bed as she requires complete bed
rest. Physiotherapy can be recommended for her to ensure better circulation and blood
flow, thereby reducing pain and might hasten the healing of wounds.
iii. Preventative measures
Case Study 1:
As the healing process is delayed, extra precaution must be taken to stop further
infection of the open wounds. Additionally the patient’s urine output is incontinent and
requires pad in situ. This heightens the chances of microbial infections of the wound, if
care is not taken and urine touches the wounds.
Case Study 2:
15WOUND MANAGEMENT PLANS
Proper covering and care needs to be taken of the wounds so that no further
infection can grow on the wounds. Care had to be taken to prevent injury around the
wounded regions which might delay the healing.
E. Wound management plan
Case Study 1:
The wound management plans for Mr. Jackson’s wounds are discussed below.
1. The diabetic foot ulcer.
i. Moist wound healing
Moist wound healing promotes faster healing in comparison to dry conditions as
moist wound healing prevents formation of crusty scab (Gethin, McIntosh & Probst,
2016). The circulation and migration of new cells are enhanced in moist wound healing
along with growth promotion and increased transport of nutrients and proteins required
for the repair healing process.
ii. Risk assessment
Assessment of the risk elements is the key factor required in treatment and
prevention of wounds. In case of diabetic foot ulcer, the main aim is to prevent the
spread of the wound and thereby, reduce chances of amputation.
iii. Wound cleansing
The diabetic foot ulcer of Mr. Jackson requires wound debridement for the
removal of dead, necrotic and infected tissues allowing the healthy tissues to grow and
heal the wound faster. Effervescent cleansing action helps to lift debris from the wound
surface when used at full strength along with irrigation with normal saline.
iv. Pressure support & relieving device
Use of therapeutic shoes might be used to reduce formation of unwanted
pressure points and proper management of the diabetic ulcer is crucial.
v. Dressing product and primary dressing
Gauges are generally used as dressing product. The wound must be properly
dressed to avoid infection and minimize further harm that might be caused on touch.
Primary wound dressing is when dressing is placed directly on the wound itself. A thin
Proper covering and care needs to be taken of the wounds so that no further
infection can grow on the wounds. Care had to be taken to prevent injury around the
wounded regions which might delay the healing.
E. Wound management plan
Case Study 1:
The wound management plans for Mr. Jackson’s wounds are discussed below.
1. The diabetic foot ulcer.
i. Moist wound healing
Moist wound healing promotes faster healing in comparison to dry conditions as
moist wound healing prevents formation of crusty scab (Gethin, McIntosh & Probst,
2016). The circulation and migration of new cells are enhanced in moist wound healing
along with growth promotion and increased transport of nutrients and proteins required
for the repair healing process.
ii. Risk assessment
Assessment of the risk elements is the key factor required in treatment and
prevention of wounds. In case of diabetic foot ulcer, the main aim is to prevent the
spread of the wound and thereby, reduce chances of amputation.
iii. Wound cleansing
The diabetic foot ulcer of Mr. Jackson requires wound debridement for the
removal of dead, necrotic and infected tissues allowing the healthy tissues to grow and
heal the wound faster. Effervescent cleansing action helps to lift debris from the wound
surface when used at full strength along with irrigation with normal saline.
iv. Pressure support & relieving device
Use of therapeutic shoes might be used to reduce formation of unwanted
pressure points and proper management of the diabetic ulcer is crucial.
v. Dressing product and primary dressing
Gauges are generally used as dressing product. The wound must be properly
dressed to avoid infection and minimize further harm that might be caused on touch.
Primary wound dressing is when dressing is placed directly on the wound itself. A thin
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
16WOUND MANAGEMENT PLANS
film of anti bacterial ointment is recommended to reduce infection (Gethin, McIntosh &
Probst, 2016). The dressing must be kept wet to ensure proper moisture content which
attributes to faster healing. Hydrocolloid dressing is recommended for Mr. Jackson’s low
exudating diabetic foot wound.
vi. Secondary dressing
Secondary dressing is required either to hold the primary dressing in the correct
place or to absorb extra exudates leaking from the wound through the primary dressing.
Here a tape is recommended to keep the primary dressing in place so that it doesn’t fall
off during movement.
vii. Pain management
Pain management includes use of analgesic, painkillers along with controlling the
infection growth.
2. The arterial ulcer.
i. Moist wound healing
The arterial ulcer on the patient’s right low leg must be kept moist to promote
faster healing and pain relief while changing the dressing. Dry wound break or tear at
the edges while change of dressing. Therefore, the arterial ulcer must be kept moist for
better healing.
ii. Risk assessment
The risk assessment of the arterial ulcer should be performed using the Brady
scale to establish the progress of the arterial ulcer.
iii. Wound cleansing
Conservative debridement followed by effervescent cleaning might be used to lift
debris from the wound surface followed by irrigation with normal saline. This must be
followed by application of antibiotic, micro-biocidal ointment.
iv. Pressure support & relieving device
The leg can be kept a bit elevated with the help of pillow for better blood flow
and pain also might be relieved. Care must be maintained to avoid application of any
pressure or contact with the wound.
film of anti bacterial ointment is recommended to reduce infection (Gethin, McIntosh &
Probst, 2016). The dressing must be kept wet to ensure proper moisture content which
attributes to faster healing. Hydrocolloid dressing is recommended for Mr. Jackson’s low
exudating diabetic foot wound.
vi. Secondary dressing
Secondary dressing is required either to hold the primary dressing in the correct
place or to absorb extra exudates leaking from the wound through the primary dressing.
Here a tape is recommended to keep the primary dressing in place so that it doesn’t fall
off during movement.
vii. Pain management
Pain management includes use of analgesic, painkillers along with controlling the
infection growth.
2. The arterial ulcer.
i. Moist wound healing
The arterial ulcer on the patient’s right low leg must be kept moist to promote
faster healing and pain relief while changing the dressing. Dry wound break or tear at
the edges while change of dressing. Therefore, the arterial ulcer must be kept moist for
better healing.
ii. Risk assessment
The risk assessment of the arterial ulcer should be performed using the Brady
scale to establish the progress of the arterial ulcer.
iii. Wound cleansing
Conservative debridement followed by effervescent cleaning might be used to lift
debris from the wound surface followed by irrigation with normal saline. This must be
followed by application of antibiotic, micro-biocidal ointment.
iv. Pressure support & relieving device
The leg can be kept a bit elevated with the help of pillow for better blood flow
and pain also might be relieved. Care must be maintained to avoid application of any
pressure or contact with the wound.
17WOUND MANAGEMENT PLANS
v. Dressing product and primary dressing
The primary dressing gauge must have a thin film of anti bacterial ointment to
reduce infection. Proper moisture content must be maintained which attributes to faster
healing.
vi. Secondary dressing
A secondary dressing might be required to absorb any exudates leaking through
the primary dressing along with usage of an adhesive tape to keep the dressing i
position.
vii. Pain management
The patient is being treated with Endone and Hydromorphone which are pain
relievers.
3. The stage 3 pressure ulcer.
i. Moist wound healing
The stage 3 pressure ulcer on the sacrum bone must be treated under Moist
wound healing process as it promotes faster healing by increasing the transport of
nutrients and proteins required for the repair healing process along with preventing the
newly formed cells from drying out.
ii. Risk assessment
The pressure ulcers that develop from lying in similar position for long period of
time have a high chance of getting infected and that infection travelling to deep tissues
and also the surrounding periwound region. Therefore, proper control and management
of the wound is necessary to prevent such a spread.
iii. Wound cleansing
Infected pressure wounds must be cleaned with antiseptic saline solutions along
with gentle debridement of the wound. This must be followed by application of antibiotic,
microbiocidal ointment.
iv. Pressure support & relieving device
Mr. Jackson is under a lot of pain as he has a stage 3 pressure ulcer on his back
on his sacrum region and the pain aggravates when he lies in supine position. Hence,
repositioning is the best technique to relieve pain and pressure support must be used by
v. Dressing product and primary dressing
The primary dressing gauge must have a thin film of anti bacterial ointment to
reduce infection. Proper moisture content must be maintained which attributes to faster
healing.
vi. Secondary dressing
A secondary dressing might be required to absorb any exudates leaking through
the primary dressing along with usage of an adhesive tape to keep the dressing i
position.
vii. Pain management
The patient is being treated with Endone and Hydromorphone which are pain
relievers.
3. The stage 3 pressure ulcer.
i. Moist wound healing
The stage 3 pressure ulcer on the sacrum bone must be treated under Moist
wound healing process as it promotes faster healing by increasing the transport of
nutrients and proteins required for the repair healing process along with preventing the
newly formed cells from drying out.
ii. Risk assessment
The pressure ulcers that develop from lying in similar position for long period of
time have a high chance of getting infected and that infection travelling to deep tissues
and also the surrounding periwound region. Therefore, proper control and management
of the wound is necessary to prevent such a spread.
iii. Wound cleansing
Infected pressure wounds must be cleaned with antiseptic saline solutions along
with gentle debridement of the wound. This must be followed by application of antibiotic,
microbiocidal ointment.
iv. Pressure support & relieving device
Mr. Jackson is under a lot of pain as he has a stage 3 pressure ulcer on his back
on his sacrum region and the pain aggravates when he lies in supine position. Hence,
repositioning is the best technique to relieve pain and pressure support must be used by
18WOUND MANAGEMENT PLANS
providing correct mattress so that pressure distribution is equilibrated all over and
allowing proper healing (Moore & Cowman, 2015).
v. Dressing product and primary dressing
A thin film of anti bacterial ointment is recommended to reduce infection. The
primary dressing must be kept moist so that tissue injury is reduced during change of
dressing.
vi. Secondary dressing
Secondary dressing is required to absorb the extra exudate leaking from the
wound through the primary dressing along with a tape to maintain the position of the
dressing.
vii. Pain management
Endone and Hydromorphone are being administered regularly for management
of his pain.
4. The malignant groin wound.
i. Moist wound healing
The patient, Mrs Gold, requires pain relieve before dressing procedure, therefore
accurate moisture content must be maintained for the malignant wound to reduce tissue
breakage or injury that might aggravate the pain.
ii. Risk assessment
The wound is already malignant and is filled with pus and has developed a sinus
tract. So proper assessment is required to judge the risk factor as the malignancy might
have reached the deep seated tissues and might affect the internal muscles and
organs. An ultrasonography might be performed to assess the depth of the infection.
iii. Wound cleansing
Malignant wounds is caused by the invasion of the cancerous cells into the skin
and the adjoining blood vessels and lymph causing death of the tissue that leads to
inflammation resulting in infection, odour and pus exudation from the wound. Warm
compression followed by gentle exudation by applying pressure followed by thorough
cleaning with antiseptic saline solution is recommended.
providing correct mattress so that pressure distribution is equilibrated all over and
allowing proper healing (Moore & Cowman, 2015).
v. Dressing product and primary dressing
A thin film of anti bacterial ointment is recommended to reduce infection. The
primary dressing must be kept moist so that tissue injury is reduced during change of
dressing.
vi. Secondary dressing
Secondary dressing is required to absorb the extra exudate leaking from the
wound through the primary dressing along with a tape to maintain the position of the
dressing.
vii. Pain management
Endone and Hydromorphone are being administered regularly for management
of his pain.
4. The malignant groin wound.
i. Moist wound healing
The patient, Mrs Gold, requires pain relieve before dressing procedure, therefore
accurate moisture content must be maintained for the malignant wound to reduce tissue
breakage or injury that might aggravate the pain.
ii. Risk assessment
The wound is already malignant and is filled with pus and has developed a sinus
tract. So proper assessment is required to judge the risk factor as the malignancy might
have reached the deep seated tissues and might affect the internal muscles and
organs. An ultrasonography might be performed to assess the depth of the infection.
iii. Wound cleansing
Malignant wounds is caused by the invasion of the cancerous cells into the skin
and the adjoining blood vessels and lymph causing death of the tissue that leads to
inflammation resulting in infection, odour and pus exudation from the wound. Warm
compression followed by gentle exudation by applying pressure followed by thorough
cleaning with antiseptic saline solution is recommended.
Paraphrase This Document
Need a fresh take? Get an instant paraphrase of this document with our AI Paraphraser
19WOUND MANAGEMENT PLANS
iv. Pressure support & relieving device
Mrs. Gold is under a lot of pain from her malignant wound. Hence, equilibrated
pressure mattress might be used to relieve the pain (Moore & Cowman, 2015).
v. Dressing product and primary dressing
Alginate dressing with a film of antibiotic ointment is recommended for Mrs.
Gold’s malignant wound on her left groin as her wound is a highly exudating wound and
alginate dressing will prevent the pus and exudates from coming in contact with her
clothes, or urine or faecal matter.
vi. Secondary dressing
Mrs. Gold requires secondary dressing to hold the primary dressing in the correct
place and to absorb exudates leaking from the wound through the primary dressing and
also to prevent urine and faecal matter coming in contact with the wound which
increases the pain and burning sensation of the patient.
vii. Pain Management
Due to old age and added pain from the malignant wound, fewer dressing
changes are recommended to reduce chances of injury and manage pain.
5. The venous ulcer.
i. Moist wound healing
Compression therapy is the cornerstone of venous ulcer treatment. The venous
ulcer must be kept moist so that it does not become dry and scaly. Keeping the wound
accurately moistened will help in the repair of the dead or damaged tissues.
ii. Risk assessment
The risk assessment of the venous ulcer with the help of Brady scale is
recommended to establish the progress of the venous ulcer.
iii. Wound cleansing
Wound cleansing for the venous ulcer must follow conservative debridement
along with cleaning to lift debris from the wound surface followed by irrigation with
normal saline. This must be followed by application of antibiotic, micro-biocidal
ointment.
iv. Pressure support & relieving device
Mrs. Gold is under a lot of pain from her malignant wound. Hence, equilibrated
pressure mattress might be used to relieve the pain (Moore & Cowman, 2015).
v. Dressing product and primary dressing
Alginate dressing with a film of antibiotic ointment is recommended for Mrs.
Gold’s malignant wound on her left groin as her wound is a highly exudating wound and
alginate dressing will prevent the pus and exudates from coming in contact with her
clothes, or urine or faecal matter.
vi. Secondary dressing
Mrs. Gold requires secondary dressing to hold the primary dressing in the correct
place and to absorb exudates leaking from the wound through the primary dressing and
also to prevent urine and faecal matter coming in contact with the wound which
increases the pain and burning sensation of the patient.
vii. Pain Management
Due to old age and added pain from the malignant wound, fewer dressing
changes are recommended to reduce chances of injury and manage pain.
5. The venous ulcer.
i. Moist wound healing
Compression therapy is the cornerstone of venous ulcer treatment. The venous
ulcer must be kept moist so that it does not become dry and scaly. Keeping the wound
accurately moistened will help in the repair of the dead or damaged tissues.
ii. Risk assessment
The risk assessment of the venous ulcer with the help of Brady scale is
recommended to establish the progress of the venous ulcer.
iii. Wound cleansing
Wound cleansing for the venous ulcer must follow conservative debridement
along with cleaning to lift debris from the wound surface followed by irrigation with
normal saline. This must be followed by application of antibiotic, micro-biocidal
ointment.
20WOUND MANAGEMENT PLANS
iv. Pressure support & relieving device
The area must be kept a bit elevated with the help of pillow for better blood
circulation (Yim et al., 2015). This will help will relief and reduction of inflammation.
v. Dressing product and primary dressing
Antimicrobial dressing is recommended for Mrs. Gold’s venous ulcer. Gauge
with a thin layer of antimicrobial ointment is suggested to maintain the moisture content
along with effective treatment for possible infections.
vi. Secondary dressing
A tape might be used to keep the primary dressing in place.
vii. Pain management
The patient is being treated with Fentanyl which is a powerful pain relieving
opiod.
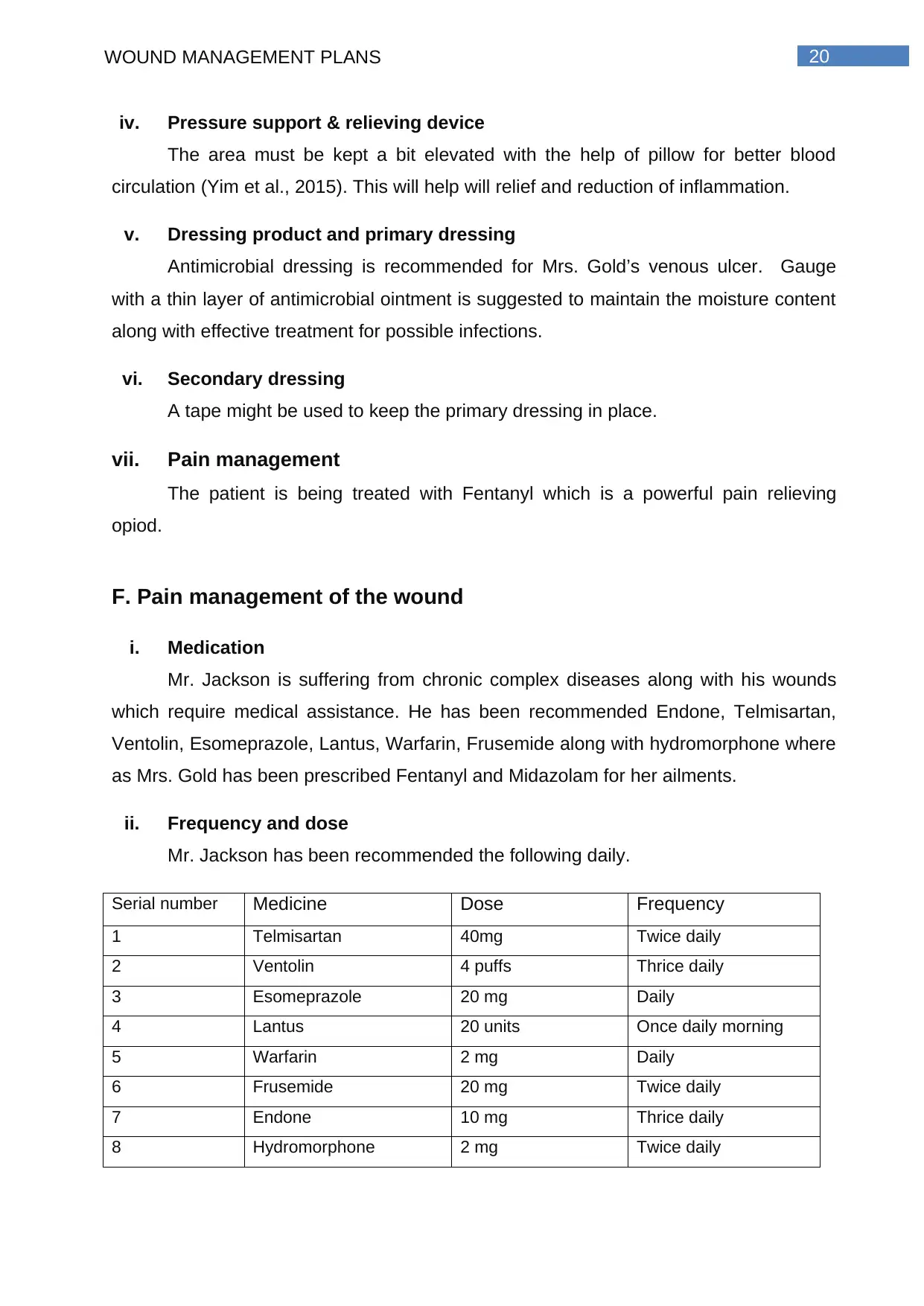
F. Pain management of the wound
i. Medication
Mr. Jackson is suffering from chronic complex diseases along with his wounds
which require medical assistance. He has been recommended Endone, Telmisartan,
Ventolin, Esomeprazole, Lantus, Warfarin, Frusemide along with hydromorphone where
as Mrs. Gold has been prescribed Fentanyl and Midazolam for her ailments.
ii. Frequency and dose
Mr. Jackson has been recommended the following daily.
Serial number Medicine Dose Frequency
1 Telmisartan 40mg Twice daily
2 Ventolin 4 puffs Thrice daily
3 Esomeprazole 20 mg Daily
4 Lantus 20 units Once daily morning
5 Warfarin 2 mg Daily
6 Frusemide 20 mg Twice daily
7 Endone 10 mg Thrice daily
8 Hydromorphone 2 mg Twice daily
iv. Pressure support & relieving device
The area must be kept a bit elevated with the help of pillow for better blood
circulation (Yim et al., 2015). This will help will relief and reduction of inflammation.
v. Dressing product and primary dressing
Antimicrobial dressing is recommended for Mrs. Gold’s venous ulcer. Gauge
with a thin layer of antimicrobial ointment is suggested to maintain the moisture content
along with effective treatment for possible infections.
vi. Secondary dressing
A tape might be used to keep the primary dressing in place.
vii. Pain management
The patient is being treated with Fentanyl which is a powerful pain relieving
opiod.
F. Pain management of the wound
i. Medication
Mr. Jackson is suffering from chronic complex diseases along with his wounds
which require medical assistance. He has been recommended Endone, Telmisartan,
Ventolin, Esomeprazole, Lantus, Warfarin, Frusemide along with hydromorphone where
as Mrs. Gold has been prescribed Fentanyl and Midazolam for her ailments.
ii. Frequency and dose
Mr. Jackson has been recommended the following daily.
Serial number Medicine Dose Frequency
1 Telmisartan 40mg Twice daily
2 Ventolin 4 puffs Thrice daily
3 Esomeprazole 20 mg Daily
4 Lantus 20 units Once daily morning
5 Warfarin 2 mg Daily
6 Frusemide 20 mg Twice daily
7 Endone 10 mg Thrice daily
8 Hydromorphone 2 mg Twice daily
21WOUND MANAGEMENT PLANS
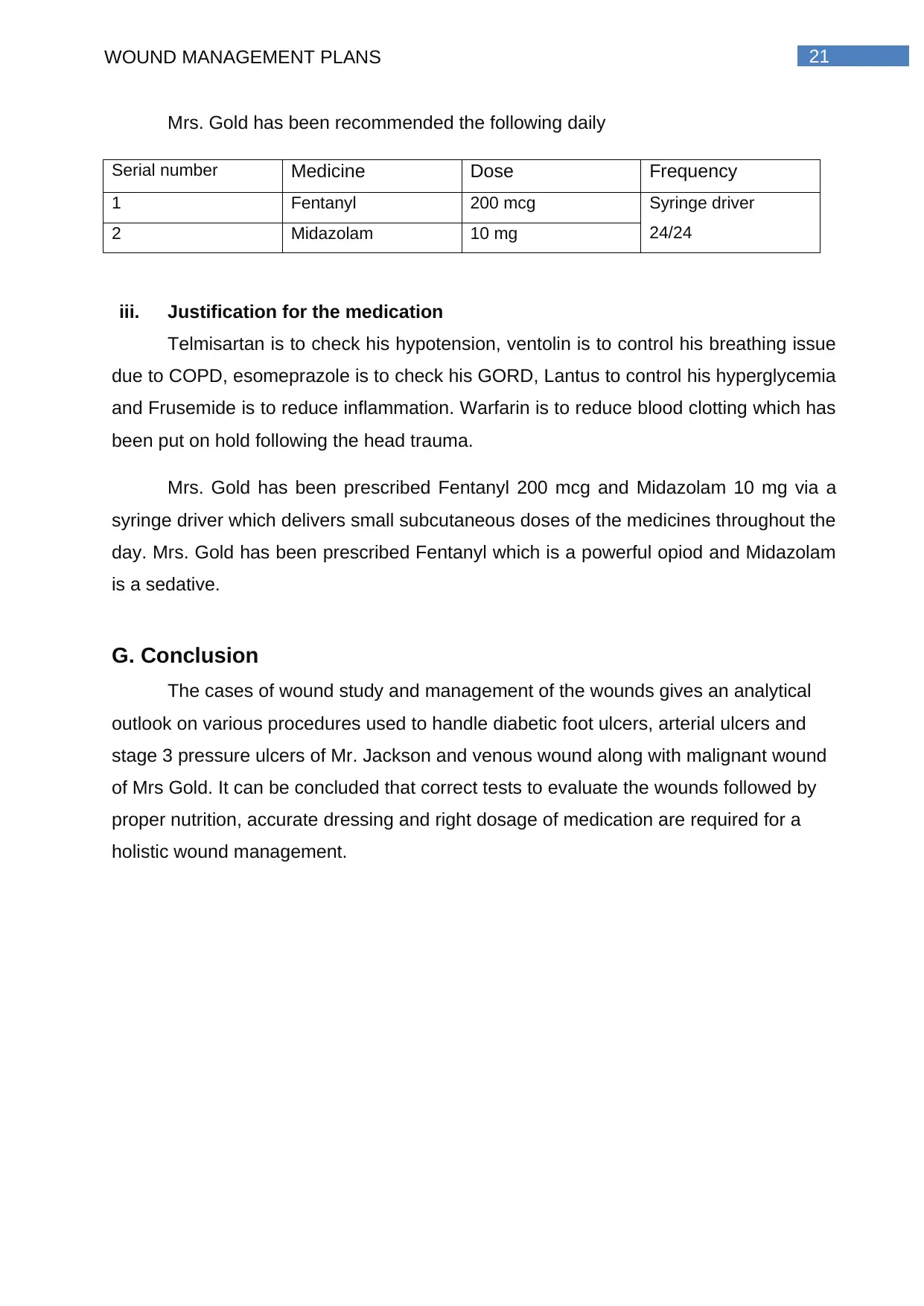
Mrs. Gold has been recommended the following daily
Serial number Medicine Dose Frequency
1 Fentanyl 200 mcg Syringe driver
24/242 Midazolam 10 mg
iii. Justification for the medication
Telmisartan is to check his hypotension, ventolin is to control his breathing issue
due to COPD, esomeprazole is to check his GORD, Lantus to control his hyperglycemia
and Frusemide is to reduce inflammation. Warfarin is to reduce blood clotting which has
been put on hold following the head trauma.
Mrs. Gold has been prescribed Fentanyl 200 mcg and Midazolam 10 mg via a
syringe driver which delivers small subcutaneous doses of the medicines throughout the
day. Mrs. Gold has been prescribed Fentanyl which is a powerful opiod and Midazolam
is a sedative.
G. Conclusion
The cases of wound study and management of the wounds gives an analytical
outlook on various procedures used to handle diabetic foot ulcers, arterial ulcers and
stage 3 pressure ulcers of Mr. Jackson and venous wound along with malignant wound
of Mrs Gold. It can be concluded that correct tests to evaluate the wounds followed by
proper nutrition, accurate dressing and right dosage of medication are required for a
holistic wound management.
Mrs. Gold has been recommended the following daily
Serial number Medicine Dose Frequency
1 Fentanyl 200 mcg Syringe driver
24/242 Midazolam 10 mg
iii. Justification for the medication
Telmisartan is to check his hypotension, ventolin is to control his breathing issue
due to COPD, esomeprazole is to check his GORD, Lantus to control his hyperglycemia
and Frusemide is to reduce inflammation. Warfarin is to reduce blood clotting which has
been put on hold following the head trauma.
Mrs. Gold has been prescribed Fentanyl 200 mcg and Midazolam 10 mg via a
syringe driver which delivers small subcutaneous doses of the medicines throughout the
day. Mrs. Gold has been prescribed Fentanyl which is a powerful opiod and Midazolam
is a sedative.
G. Conclusion
The cases of wound study and management of the wounds gives an analytical
outlook on various procedures used to handle diabetic foot ulcers, arterial ulcers and
stage 3 pressure ulcers of Mr. Jackson and venous wound along with malignant wound
of Mrs Gold. It can be concluded that correct tests to evaluate the wounds followed by
proper nutrition, accurate dressing and right dosage of medication are required for a
holistic wound management.
Secure Best Marks with AI Grader
Need help grading? Try our AI Grader for instant feedback on your assignments.
22WOUND MANAGEMENT PLANS
H. References
Barchitta, M., Maugeri, A., Favara, G., Magnano San Lio, R., Evola, G., Agodi, A., &
Basile, G. (2019). Nutrition and wound healing: an overview focusing on the
beneficial effects of curcumin. International journal of molecular sciences, 20(5),
1119.
Federman, D. G., Ladiiznski, B., Dardik, A., Kelly, M., Shapshak, D., Ueno, C. M., ... &
Hopf, H. W. (2016). Wound healing society 2014 update on guidelines for arterial
ulcers. Wound Repair and Regeneration, 24(1), 127-135.
Gethin, G., McIntosh, C., & Probst, S. (2016). Complementary and alternative therapies
for management of odor in malignant fungating wounds: a critical review. Chronic
Wound Care Management and Research, 3, 51.
Jacobson, L. K., Johnson, M. B., Dedhia, R. D., Niknam-Bienia, S., & Wong, A. K.
(2017). Impaired wound healing after radiation therapy: A systematic review of
pathogenesis and treatment. Jpras Open, 13, 92-105.
Moore, Z. E., & Cowman, S. (2015). Repositioning for treating pressure
ulcers. Cochrane Database of Systematic Reviews, (1).
Quain, A. M., & Khardori, N. M. (2015). Nutrition in Wound Care Management: A
Comprehensive Overview. Wounds: a compendium of clinical research and
practice, 27(12), 327-335.
Rondas, A. A., Halfens, R. J., Schols, J. M., Thiesen, K. P., Trienekens, T. A., &
Stobberingh, E. E. (2015). Is a wound swab for microbiological analysis
supportive in the clinical assessment of infection of a chronic wound?. Future
microbiology, 10(11), 1815-1824.
Wang, Z., Hasan, R., Firwana, B., Elraiyah, T., Tsapas, A., Prokop, L., ... & Murad, M.
H. (2016). A systematic review and meta-analysis of tests to predict wound
healing in diabetic foot. Journal of vascular surgery, 63(2), 29S-36S.
H. References
Barchitta, M., Maugeri, A., Favara, G., Magnano San Lio, R., Evola, G., Agodi, A., &
Basile, G. (2019). Nutrition and wound healing: an overview focusing on the
beneficial effects of curcumin. International journal of molecular sciences, 20(5),
1119.
Federman, D. G., Ladiiznski, B., Dardik, A., Kelly, M., Shapshak, D., Ueno, C. M., ... &
Hopf, H. W. (2016). Wound healing society 2014 update on guidelines for arterial
ulcers. Wound Repair and Regeneration, 24(1), 127-135.
Gethin, G., McIntosh, C., & Probst, S. (2016). Complementary and alternative therapies
for management of odor in malignant fungating wounds: a critical review. Chronic
Wound Care Management and Research, 3, 51.
Jacobson, L. K., Johnson, M. B., Dedhia, R. D., Niknam-Bienia, S., & Wong, A. K.
(2017). Impaired wound healing after radiation therapy: A systematic review of
pathogenesis and treatment. Jpras Open, 13, 92-105.
Moore, Z. E., & Cowman, S. (2015). Repositioning for treating pressure
ulcers. Cochrane Database of Systematic Reviews, (1).
Quain, A. M., & Khardori, N. M. (2015). Nutrition in Wound Care Management: A
Comprehensive Overview. Wounds: a compendium of clinical research and
practice, 27(12), 327-335.
Rondas, A. A., Halfens, R. J., Schols, J. M., Thiesen, K. P., Trienekens, T. A., &
Stobberingh, E. E. (2015). Is a wound swab for microbiological analysis
supportive in the clinical assessment of infection of a chronic wound?. Future
microbiology, 10(11), 1815-1824.
Wang, Z., Hasan, R., Firwana, B., Elraiyah, T., Tsapas, A., Prokop, L., ... & Murad, M.
H. (2016). A systematic review and meta-analysis of tests to predict wound
healing in diabetic foot. Journal of vascular surgery, 63(2), 29S-36S.
1 out of 23
Related Documents
Your All-in-One AI-Powered Toolkit for Academic Success.
+13062052269
info@desklib.com
Available 24*7 on WhatsApp / Email
![[object Object]](/_next/static/media/star-bottom.7253800d.svg)
Unlock your academic potential
© 2024 | Zucol Services PVT LTD | All rights reserved.





